Lessons Learned from an Attempted Pragmatic Randomized Controlled Trial for Improvement of Chronic Pain-Associated Disability in Green Professions: Long-Term Effectiveness of a Guided Online-Based Acceptance and Commitment Therapy (PACT-A)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Inclusion and Exclusion Criteria
2.3. Recruitment
2.4. Procedure
2.5. Intervention
2.5.1. Control Group
2.5.2. Intervention Group
2.6. Outcome Measures
2.6.1. Primary Outcome
2.6.2. Pain-Related Secondary Outcomes
2.6.3. Mental Health–Related Secondary Outcomes
2.6.4. Intervention-Related Secondary Outcomes
2.7. Data Analysis
3. Results
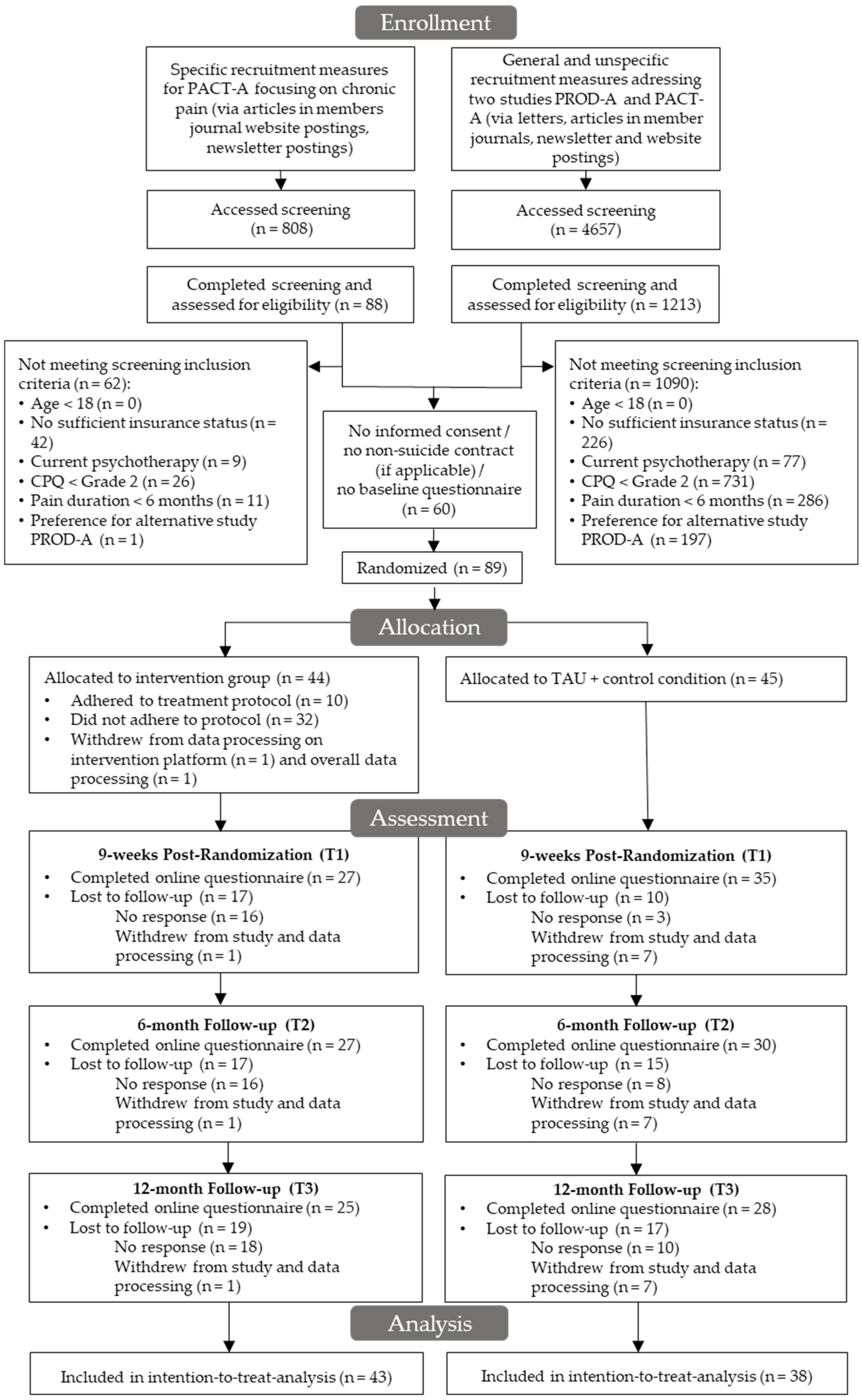
3.1. Participants
3.2. Primary Outcome
3.3. Pain-Related Secondary Outcomes
3.4. Mental Health–Related Secondary Outcomes
3.5. Intervention-Related Secondary Outcomes
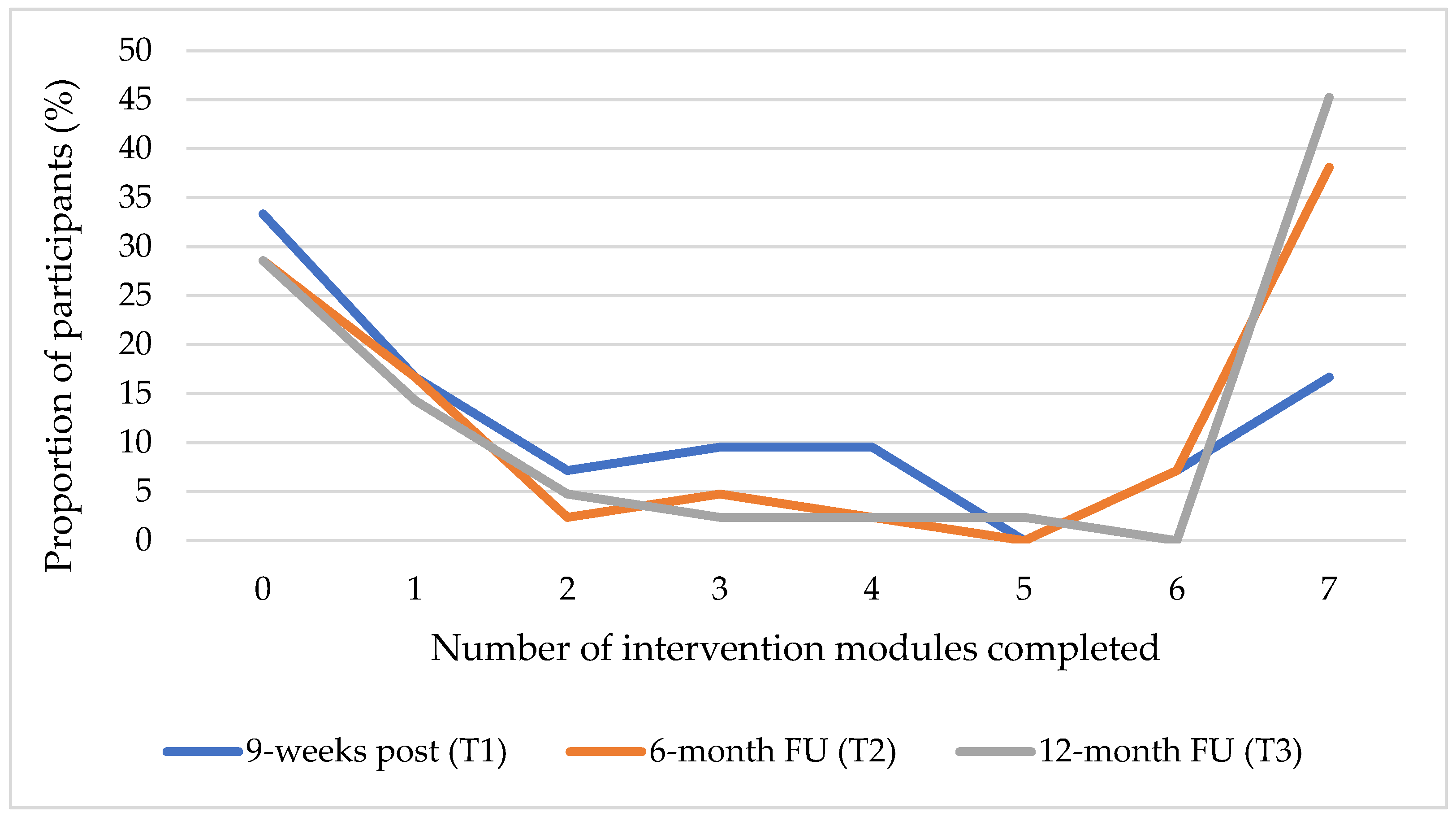
3.6. Use of and Adherence to the Online Intervention(s)
3.7. Negative Effects and Reliable Deterioration
4. Discussion
4.1. Principal Results
4.2. Comparison to Prior Work
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Deviations from Study Registration/Study Protocol
- The 24-month (T4) and 36-month (T5) FU measurement points: We refrained from analyzing and reporting of data for the 24-month FU (T4) due to limited statistical power following high study attrition. Data collection at the initially planned measurement point after 36 months (T5) was omitted.
- Per-protocol analysis: Due to preliminary recruitment stop, high study attrition and the low rate of intervention participants adhering to treatment protocol, no per-protocol analysis was performed. Statistical power is not sufficient to detect potential treatment effects in per-protocol analysis.
- Complete-case analysis: Instead, an additional complete-case analysis was conducted to examine the robustness of the ITT analysis against the background of high study attrition.
- Moderation analysis: As the study is substantially underpowered due to the reasons already stated, we have refrained from conducting a further analysis of possible moderating variables.
- Mediation analysis: We proposed to analyze the three facets of psychological flexibility (pain acceptance, cognitive fusion and committed action) as well as technological and therapeutic alliances as mediating variables in the study protocol. As no reduction of pain interference was observed by this ACT-based online intervention, we were not able to investigate possible mediating variables of this supposed treatment effect.
- Cost-effectiveness analysis: Due to the low statistical power, we also refrained from conducting a cost-effectiveness analysis.
References
- Husky, M.M.; Ferdous Farin, F.; Compagnone, P.; Fermanian, C.; Kovess-Masfety, V.; Scarth, R.D.; Stallones, L.; Zwerling, C.; Burmeister, L.F.; Thelin, A.; et al. Chronic back pain and its association with quality of life in a large French population survey. Health Qual. Life Outcomes 2018, 16, 195. [Google Scholar] [CrossRef] [PubMed]
- Bernfort, L.; Gerdle, B.; Rahmqvist, M.; Husberg, M.; Levin, L.Å. Severity of chronic pain in an elderly population in Sweden—Impact on costs and quality of life. Pain 2015, 156, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Merskey, H.; Bogduk, N. Classification of Chronic Pain, 2nd ed.; IASP Press: Seattle, WA, USA, 1994; ISBN 0-931092-05-1. [Google Scholar]
- Treede, R.-D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. A classification of chronic pain for ICD-11. Pain 2015, 156, 1003–1007. [Google Scholar] [CrossRef] [PubMed]
- Häuser, W.; Wolfe, F.; Henningsen, P.; Schmutzer, G.; Brähler, E.; Hinz, A. Untying chronic pain: Prevalence and societal burden of chronic pain stages in the general population—A cross-sectional survey. BMC Public Health 2014, 14, 352. [Google Scholar] [CrossRef] [PubMed]
- Leadley, R.M.; Armstrong, N.; Lee, Y.C.; Allen, A.; Kleijnen, J. Chronic diseases in the European Union: The prevalence and health cost implications of chronic pain. J. Pain Palliat. Care Pharmacother. 2012, 26, 310–325. [Google Scholar] [CrossRef]
- Dahlhamer, J.; Lucas, J.; Zelaya, C.; Nahin, R.; Mackey, S.; DeBar, L.; Kerns, R.; Von Korff, M.; Porter, L.; Helmick, C. Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults—United States, 2016. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 1001–1006. [Google Scholar] [CrossRef]
- Schneider, S.; Lipinski, S.; Schiltenwolf, M. Occupations associated with a high risk of self-reported back pain: Representative outcomes of a back pain prevalence study in the Federal Republic of Germany. Eur. Spine J. 2006, 15, 821–833. [Google Scholar] [CrossRef]
- Liebers, F.; Brendler, C.; Latza, U. Alters- und berufsgruppenabhängige Unterschiede in der Arbeitsunfähigkeit durch häufige Muskel-Skelett-Erkrankungen: Rückenschmerzen und Gonarthrose. Bundesgesundheitsblatt-Gesundheitsforsch.-Gesundh. 2013, 56, 367–380. [Google Scholar] [CrossRef]
- Yang, H.; Haldeman, S.; Lu, M.L.; Baker, D. Low Back Pain Prevalence and Related Workplace Psychosocial Risk Factors: A Study Using Data From the 2010 National Health Interview Survey. J. Manip. Physiol. Ther. 2016, 39, 459–472. [Google Scholar] [CrossRef]
- Holmberg, S.; Thelin, A.; Stiernström, E.L.; Svärdsudd, K. Low back pain comorbidity among male farmers and rural referents: A population-based study. Ann. Agric. Environ. Med. 2005, 12, 261–268. [Google Scholar]
- Holmberg, S.; Stiernström, E.-L.; Thelin, A.; Svärdsudd, K. Musculoskeletal Symptoms among Farmers and Non-farmers: A Population-based Study. Int. J. Occup. Environ. Health 2002, 8, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Kolstrup, C.L. Work-related musculoskeletal discomfort of dairy farmers and employed workers. J. Occup. Med. Toxicol. 2012, 7, 23. [Google Scholar] [CrossRef] [PubMed]
- Osborne, A.; Blake, C.; Fullen, B.M.; Meredith, D.; Phelan, J.; Mcnamara, J.; Cunningham, C. Risk factors for musculoskeletal disorders among farm owners and farm workers: A systematic review. Am. J. Ind. Med. 2012, 55, 376–389. [Google Scholar] [CrossRef] [PubMed]
- Walker-Bone, K.; Palmer, K.T. Musculoskeletal disorders in farmers and farm workers. Occup. Med. (Chic. Ill) 2002, 52, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Kolstrup, C.L.; Jakob, M. Epidemiology of Musculoskeletal Symptoms Among Milkers and Dairy Farm Characteristics in Sweden and Germany. J. Agromedicine 2016, 21, 43–55. [Google Scholar] [CrossRef]
- Thinius, M.; Jakob, M. Ergonomic workplace evaluation and epidemiology of musculoskeletal discomfort on German dairy farms. Work 2014, 49, 25–32. [Google Scholar] [CrossRef]
- Jadhav, R.; Achutan, C.; Haynatzki, G.; Rajaram, S.; Rautiainen, R. Risk Factors for Agricultural Injury: A Systematic Review and Meta-analysis. J. Agromedicine 2015, 20, 434–449. [Google Scholar] [CrossRef]
- Jakob, M.C. Evaluation of a Physical Ergonomic Intervention for Milking Parlor Operatives–A Case Study. J. Agromedicine 2019, 24, 215–223. [Google Scholar] [CrossRef]
- Kamioka, H.; Okuizumi, H.; Handa, S.; Kitayuguchi, J.; Machida, R. Effect of non-surgical interventions on pain relief and symptom improvement in farmers with diseases of the musculoskeletal system or connective tissue: An exploratory systematic review based on randomized controlled trials. J. Rural Med. 2022, 17, 1–13. [Google Scholar] [CrossRef]
- Kotowski, S.E.; Davis, K.G.; Waters, T.R. Investigation of select ergonomic interventions to farm youth. Part 1: Shovels. J. Agromedicine 2009, 14, 33–43. [Google Scholar] [CrossRef]
- Kotowski, S.E.; Davis, K.G.; Waters, T.R. Investigation of select ergonomic interventions for farm youth. Part 2: Wheelbarrows. J. Agromedicine 2009, 14, 44–57. [Google Scholar] [CrossRef] [PubMed]
- Severeijns, R.; Vlaeyen, J.W.S.; Van Den Hout, M.A.; Weber, W.E.J. Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. Clin. J. Pain 2001, 17, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Turner, J.A.; Jensen, M.P.; Warms, C.A.; Cardenas, D.D. Catastrophizing is associated with pain intensity, psychological distress, and pain-related disability among individuals with chronic pain after spinal cord injury. Pain 2002, 98, 127–134. [Google Scholar] [CrossRef]
- Trompetter, H.R.; Bohlmeijer, E.T.; Fox, J.P.; Schreurs, K.M.G. Psychological flexibility and catastrophizing as associated change mechanisms during online Acceptance & Commitment Therapy for chronic pain. Behav. Res. Ther. 2015, 74, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Åkerblom, S.; Perrin, S.; Rivano Fischer, M.; McCracken, L.M. The Mediating Role of Acceptance in Multidisciplinary Cognitive-Behavioral Therapy for Chronic Pain. J. Pain 2015, 16, 606–615. [Google Scholar] [CrossRef]
- Baranoff, J.; Hanrahan, S.J.; Kapur, D.; Connor, J.P. Acceptance as a process variable in relation to catastrophizing in multidisciplinary pain treatment. Eur. J. Pain 2013, 17, 101–110. [Google Scholar] [CrossRef]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change; Guilford Press: New York, NY, USA, 1999; ISBN 978-1572304819. [Google Scholar]
- Probst, T.; Baumeister, H.; McCracken, L.; Lin, J. Baseline Psychological Inflexibility Moderates the Outcome Pain Interference in a Randomized Controlled Trial on Internet-based Acceptance and Commitment Therapy for Chronic Pain. J. Clin. Med. 2018, 8, 24. [Google Scholar] [CrossRef]
- Veehof, M.M.; Trompetter, H.R.; Bohlmeijer, E.T.; Schreurs, K.M.G. Acceptance- and mindfulness-based interventions for the treatment of chronic pain: A meta-analytic review. Cogn. Behav. Ther. 2016, 45, 5–31. [Google Scholar] [CrossRef]
- Trindade, I.A.; Guiomar, R.; Carvalho, S.A.; Duarte, J.; Lapa, T.; Menezes, P.; Nogueira, M.R.; Patrão, B.; Pinto-Gouveia, J.; Castilho, P. Efficacy of Online-Based Acceptance and Commitment Therapy for Chronic Pain: A Systematic Review and Meta-Analysis. J. Pain 2021, 22, 1328–1342. [Google Scholar] [CrossRef]
- Lin, J.; Baumeister, H. Internet- und Mobilebasierte Interventionen in der Psychotherapie. Public Health Forum 2015, 23, 176–179. [Google Scholar] [CrossRef]
- Brew, B.; Inder, K.; Allen, J.; Thomas, M.; Kelly, B. The health and wellbeing of Australian farmers: A longitudinal cohort study. BMC Public Health 2016, 16, 988. [Google Scholar] [CrossRef] [PubMed]
- Hull, M.J.; Fennell, K.M.; Vallury, K.; Jones, M.; Dollman, J. A comparison of barriers to mental health support-seeking among farming and non-farming adults in rural South Australia. Aust. J. Rural Health 2017, 25, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Freund, J.; Titzler, I.; Thielecke, J.; Braun, L.; Baumeister, H.; Berking, M.; Ebert, D.D. Implementing internet- and tele-based interventions to prevent mental health disorders in farmers, foresters and gardeners (ImplementIT): Study protocol for the multi-level evaluation of a nationwide project. BMC Psychiatry 2020, 20, 424. [Google Scholar] [CrossRef] [PubMed]
- Thielecke, J.; Buntrock, C.; Titzler, I.; Braun, L.; Freund, J.; Berking, M.; Baumeister, H.; Ebert, D.D. Clinical and cost-effectiveness of personalized tele-based coaching for farmers, foresters and gardeners to prevent depression: Study protocol of an 18-month follow-up pragmatic randomized controlled trial (TEC-A). Front. Psychiatry 2020, 11, 125. [Google Scholar] [CrossRef]
- Braun, L.; Titzler, I.; Ebert, D.D.; Buntrock, C.; Terhorst, Y.; Freund, J.; Thielecke, J.; Baumeister, H. Clinical and cost-effectiveness of guided internet-based interventions in the indicated prevention of depression in green professions (PROD-A): Study protocol of a 36-months follow-up pragmatic randomized controlled trial. BMC Psychiatry 2019, 19, 278. [Google Scholar] [CrossRef]
- Braun, L.; Titzler, I.; Terhorst, Y.; Freund, J.; Thielecke, J.; Ebert, D.D.; Baumeister, H. Effectiveness of guided internet-based interventions in the indicated prevention of depression in green professions (PROD-A): Results of a pragmatic randomized controlled trial. J. Affect. Disord. 2021, 278, 658–671. [Google Scholar] [CrossRef]
- Braun, L.; Titzler, I.; Terhorst, Y.; Freund, J.; Thielecke, J.; Ebert, D.D.; Baumeister, H. Are guided internet-based interventions for the indicated prevention of depression in green professions effective in the long run? Longitudinal analysis of the 6- and 12-month follow-up of a pragmatic randomized controlled trial (PROD-A). Internet Interv. 2021, 26, 100455. [Google Scholar] [CrossRef]
- Thielecke, J.; Buntrock, C.; Titzler, I.; Braun, L.; Freund, J.; Berking, M.; Baumeister, H.; Ebert, D.D. Telephone coaching for the prevention of depression in depression in farmers: Results from a pragmatic from a pragmatic randomized controlled trial. J. Telemed. Telecare 2022. [Google Scholar] [CrossRef]
- Terhorst, Y.; Braun, L.; Titzler, I.; Buntrock, C.; Freund, J.; Thielecke, J.; Ebert, D.D.; Baumeister, H. Clinical and cost- effectiveness of a guided internet- based Acceptance and Commitment Therapy to improve chronic pain–related disability in green professions (PACT- A): Study protocol of a pragmatic randomised controlled trial. BMJ Open 2020, 10, e034271. [Google Scholar] [CrossRef]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gotzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c869. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef] [PubMed]
- Zwarenstein, M.; Treweek, S.; Gagnier, J.J.; Altman, D.G.; Tunis, S.; Haynes, B.; Oxman, A.D.; Moher, D. Improving the reporting of pragmatic trials: An extension of the CONSORT statement. BMJ 2008, 337, a2390. [Google Scholar] [CrossRef] [PubMed]
- Proudfoot, J.; Klein, B.; Barak, A.; Carlbring, P.; Cuijpers, P.; Lange, A.; Ritterband, L.; Andersson, G. Establishing Guidelines for Executing and Reporting Internet Intervention Research. Cogn. Behav. Ther. 2011, 40, 82–97. [Google Scholar] [CrossRef] [PubMed]
- Klasen, B.W.; Hallner, D.; Schaub, C.; Willburger, R.; Hasenbring, M. Validation and reliability of the German version of the Chronic Pain Grade questionnaire in primary care back pain patients. Psycho-Soc.-Med. 2004, 1, Doc07. [Google Scholar]
- Kühner, C.; Bürger, C.; Keller, F.; Hautzinger, M. Reliabilität und Validität des revidierten Beck- Depressionsinventars (BDI-II). Befunde aus deutschsprachigen Stichproben. Nervenarzt 2007, 78, 651–656. [Google Scholar] [CrossRef] [PubMed]
- Bouwmans, C.; De Jong, K.; Timman, R.; Zijlstra-Vlasveld, M.; Van der Feltz-Cornelis, C.; Tan, S.S.; Hakkaart-van Roijen, L. Feasibility, reliability and validity of a questionnaire on healthcare consumption and productivity loss in patients with a psychiatric disorder (TiC-P). BMC Health Serv. Res. 2013, 13, 217. [Google Scholar] [CrossRef]
- Lin, J.; Lüking, M.; Ebert, D.D.; Buhrman, M.; Andersson, G.; Baumeister, H. Effectiveness and cost-effectiveness of a guided and unguided internet-based Acceptance and Commitment Therapy for chronic pain: Study protocol for a three-armed randomised controlled trial. Internet Interv. 2015, 2, 7–16. [Google Scholar] [CrossRef]
- Lin, J.; Paganini, S.; Sander, L.; Lüking, M.; Ebert, D.D.; Buhrman, M.; Andersson, G.; Baumeister, H. An internet-based intervention for chronic pain. Dtsch. Arztebl. Int. 2017, 114, 681–688. [Google Scholar] [CrossRef]
- Nobis, S.; Lehr, D.; Ebert, D.D.; Berking, M.; Heber, E.; Baumeister, H.; Becker, A.; Snoek, F.; Riper, H. Efficacy and cost-effectiveness of a web-based intervention with mobile phone support to treat depressive symptoms in adults with diabetes mellitus type 1 and type 2: Design of a randomised controlled trial. BMC Psychiatry 2013, 13, 306. [Google Scholar] [CrossRef]
- Buntrock, C.; Ebert, D.D.; Lehr, D.; Cuijpers, P.; Riper, H.; Smit, F.; Berking, M. Evaluating the efficacy and cost-effectiveness of web-based indicated prevention of major depression: Design of a randomised controlled trial. BMC Psychiatry 2014, 14, 25. [Google Scholar] [CrossRef]
- Ebert, D.D.; Lehr, D.; Smit, F.; Zarski, A.C.; Riper, H.; Heber, E.; Cuijpers, P.; Berking, M. Efficacy and cost-effectiveness of minimal guided and unguided internet-based mobile supported stress-management in employees with occupational stress: A three-armed randomised controlled trial. BMC Public Health 2014, 14, 807. [Google Scholar] [CrossRef] [PubMed]
- Thiart, H.; Lehr, D.; Ebert, D.D.; Sieland, B.; Berking, M.; Riper, H. Log in and breathe out: Efficacy and cost-effectiveness of an online sleep training for teachers affected by work-related strain-study protocol for a randomized controlled trial. Trials 2013, 14, 169. [Google Scholar] [CrossRef] [PubMed]
- Boß, L.; Lehr, D.; Berking, M.; Riper, H.; Schaub, M.P.; Ebert, D.D. Evaluating the (cost-)effectiveness of guided and unguided Internet-based self-help for problematic alcohol use in employees-A three arm randomized controlled trial. BMC Public Health 2015, 15, 1043. [Google Scholar] [CrossRef] [PubMed]
- Ebenfeld, L.; Kleine Stegemann, S.; Lehr, D.; Ebert, D.D.; Jazaieri, H.; van Ballegooijen, W.; Funk, B.; Riper, H.; Berking, M. Efficacy of a hybrid online training for panic symptoms and agoraphobia: Study protocol for a randomized controlled trial. Trials 2014, 15, 427. [Google Scholar] [CrossRef]
- Kerns, R.D.; Turk, D.C.; Rudy, T.E. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI). Pain 1985, 23, 345–356. [Google Scholar] [CrossRef]
- Flor, H.; Rudy, T.E.; Birbaumer, N.; Streit, B.; Schugens, M.M. Zur Anwendbarkeit des West Haven-Yale Multidimensional Pain Inventory im deutschen Sprachraum-Daten zur Reliabilität und Validität des MPI-D. Der Schmerz 1990, 4, 82–87. [Google Scholar] [CrossRef]
- Radbruch, L.; Loick, G.; Kiencke, P.; Lindena, G.; Sabatowski, R.; Grond, S.; Lehmann, K.A.; Cleeland, C.S. Validation of the German version of the Brief Pain Inventory. J. Pain Symptom Manage. 1999, 18, 180–187. [Google Scholar] [CrossRef]
- Cleeland, C.S.; Ryan, K.M. Pain assessment: Global use of the Brief Pain Inventory. Ann. Acad. Med. Singap. 1994, 23, 129–138. [Google Scholar]
- Guy, W. Clinical global impression scale. In ECDEU Assessment Manual for Psychopharmacology; DHEW Publication: Rockville, MD, USA, 1976; pp. 218–222. [Google Scholar]
- Nilges, P.; Köster, B.; Schmidt, C.O. Schmerzakzeptanz-Konzept und Überprüfung einer deutschen Fassung des Chronic Aain Acceptance Questionnaire. Schmerz 2007, 21, 57–67. [Google Scholar] [CrossRef]
- China, C.; Hansen, L.B.; Gillanders, D.T.; Benninghoven, D. Concept and validation of the German version of the Cognitive Fusion Questionnaire (CFQ-D). J. Context. Behav. Sci. 2018, 9, 30–35. [Google Scholar] [CrossRef]
- Terhorst, Y.; Baumeister, H.; McCracken, L.M.; Lin, J. Further development in the assessment of psychological flexibility: Validation of the German committed action questionnaire. Health Qual. Life Outcomes 2020, 18, 260. [Google Scholar] [CrossRef] [PubMed]
- Rush, A.J.; Trivedi, M.H.; Ibrahim, H.M.; Carmody, T.J.; Arnow, B.; Klein, D.N.; Markowitz, J.C.; Ninan, P.T.; Kornstein, S.; Manber, R.; et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), Clinician Rating (QIDS-C), and Self-Report (QIDS-SR): A Psychometric Evaluation in Patients with Chronic Major Depression. Biol. Psychiatry 2003, 54, 573–583. [Google Scholar] [CrossRef]
- Auerbach, R.P.; Mortier, P.; Bruffaerts, R.; Alonso, J.; Benjet, C.; Cuijpers, P.; Demyttenaere, K.; Ebert, D.D.; Green, J.G.; Hasking, P.; et al. WHO World Mental Health Surveys International College Student Project: Prevalence and Distribution of Mental Disorders. J. Abnorm. Psychol. 2018, 127, 623–638. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and Standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the General Population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. In Journal of health and social behavior; Spacapan, S., Oskamp, S., Eds.; Sage: Newbury Park, CA, USA, 1983; Volume 24, pp. 385–396. ISBN 0-8039-3162-X (Hardcover)/0-8039-3163-8 (Paperback). [Google Scholar]
- Gerber, M.; Lang, C.; Lemola, S.; Colledge, F.; Kalak, N.; Holsboer-Trachsler, E.; Pühse, U.; Brand, S. Validation of the German version of the insomnia severity index in adolescents, young adults and adult workers: Results from three cross-sectional studies. BMC Psychiatry 2016, 16, 174. [Google Scholar] [CrossRef]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Saunders, J.B.; Aasland, O.G.; Amundsen, A.; Grant, M. Alcohol consumption and related problems among primary health care patients: WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-I. Addiction 1993, 88, 349–362. [Google Scholar] [CrossRef] [PubMed]
- Hays, R.D.; Merz, J.F.; Nicholas, R. Response burden, reliability, and validity of the CAGE, Short MAST, and AUDIT alcohol screening measures. Behav. Res. Methods Instrum. Comput. 1995, 27, 277–280. [Google Scholar] [CrossRef]
- Fleming, M.F.; Barry, K.L.; MacDonald, R. The Alcohol Use Disorders Identification Test (AUDIT) in a College Sample. Int. J. Addict. 1991, 26, 1173–1185. [Google Scholar] [CrossRef]
- Richardson, J.; Iezzi, A.; Khan, M.A.; Maxwell, A. Validity and Reliability of the Assessment of Quality of Life (AQoL)-8D Multi-Attribute Utility Instrument. Patient 2014, 7, 85–96. [Google Scholar] [CrossRef]
- Mittag, O.; Raspe, H. Eine kurze Skala zur Messung der subjektiven Prognose der Erwerbstätigkeit: Ergebnisse einer Untersuchung an 4279 Mitgliedern der gesetzlichen Arbeiterrentenversicherung zu Reliabilität (Guttman-Skalierung) und Validität der Skala. Rehabilitation 2003, 42, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Wilmers, F.; Munder, T.; Leonhart, R.; Herzog, T.; Plassmann, R.; Barth, J.; Linster, H.W. Die deutschsprachige Version des Working Alliance Inventory–short revised (WAI-SR)–Ein schulenübergreifendes, ökonomisches und empirisch validiertes Instrument zur Erfassung der therapeutischen Allianz. Klin. Diagn. Und Eval. 2008, 1, 343–358. [Google Scholar]
- Hatcher, R.L.; Lindqvist, K.; Falkenström, F. Psychometric evaluation of the Working Alliance Inventory—Therapist version: Current and new short forms. Psychother. Res. 2020, 30, 706–717. [Google Scholar] [CrossRef] [PubMed]
- Herrero, R.; Vara, M.D.; Miragall, M.; Botella, C.; García-Palacios, A.; Riper, H.; Kleiboer, A.; Baños, M.R. The Role of the Therapeutic Alliance between Patient and Online Program in Therapeutic Outcomes. Int. J. Environ. Res. Public Health 2020, 17, 6169. [Google Scholar] [CrossRef]
- Jasper, K.; Weise, C.; Conrad, I.; Andersson, G.; Hiller, W.; Kleinstäuber, M. The working alliance in a randomized controlled trial comparing Internet-based self-help and face-to-face cognitive behavior therapy for chronic tinnitus. Internet Interv. 2014, 1, 49–57. [Google Scholar] [CrossRef]
- Boß, L.; Lehr, D.; Reis, D.; Vis, C.; Riper, H.; Berking, M.; Ebert, D.D. Reliability and Validity of Assessing User Satisfaction With Web-Based Health Interventions. J. Med. Internet Res. 2016, 18, e234. [Google Scholar] [CrossRef]
- Ladwig, I.; Rief, W.; Nestoriuc, Y. What Are the Risks and Side Effects of Psychotherapy?–Development of an Inventory for the Assessment of Negative Effects of Psychotherapy (INEP). Verhaltenstherapie 2014, 24, 252–264. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2020. [Google Scholar]
- Buhrman, M.; Gordh, T.; Andersson, G. Internet interventions for chronic pain including headache: A systematic review. Internet Interv. 2016, 4, 17–34. [Google Scholar] [CrossRef]
- Melville, K.M.; Casey, L.M.; Kavanagh, D.J. Dropout from Internet-based treatment for psychological disorders. Br. J. Clin. Psychol. 2010, 49, 455–471. [Google Scholar] [CrossRef]
- van Buuren, S.; Groothuis-Oudshoorn, K. mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- Enders, C.K. Applied Missing Data Analysis; Guilford Press: New York, NY, USA, 2010; ISBN 978-1-60623-639-0. [Google Scholar]
- Graham, J.W.; Olchowski, A.E.; Gilreath, T.D. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prev. Sci. 2007, 8, 206–213. [Google Scholar] [CrossRef] [PubMed]
- Little, R.J.A. Missing-data adjustments in large surveys. J. Bus. Econ. Stat. 1988, 6, 287–296. [Google Scholar] [CrossRef]
- Rubin, D.B. Multiple Imputation after 18+ Years. J. Am. Stat. Assoc. 1996, 91, 473–489. [Google Scholar] [CrossRef]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; John Wiley & Sons, Ltd.: Chichester, UK, 1987; ISBN 9780471087052. [Google Scholar]
- Jacobson, N.S.; Truax, P. Clinical Significance: A Statistical Approach to Defining Meaningful Change in Psychotherapy Research. J. Consult. Clin. Psychol. 1991, 59, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Rozental, A.; Andersson, G.; Carlbring, P. In the absence of effects: An individual patient data meta-analysis of non-response and its predictors in internet-based cognitive behavior therapy. Front. Psychol. 2019, 10, 589. [Google Scholar] [CrossRef]
- Lamoureux, B.E.; Linardatos, E.; Fresco, D.M.; Bartko, D.; Logue, E.; Milo, L. Using the QIDS-SR16 to Identify Major Depressive Disorder in Primary Care Medical Patients. Behav. Ther. 2010, 41, 423–431. [Google Scholar] [CrossRef]
- Thabane, L.; Mbuagbaw, L.; Zhang, S.; Samaan, Z.; Marcucci, M.; Ye, C.; Thabane, M.; Giangregorio, L.; Dennis, B.; Kosa, D.; et al. A tutorial on sensitivity analyses in clinical trials: The what, why, when and how. BMC Med. Res. Methodol. 2013, 13, 92. [Google Scholar] [CrossRef]
- OECD; European Union; UNESCO-UIS. ISCED 2011 Operational Manual: Guidelines for Classifying National Education Programmes and Related Qualifications; OECD Publishing: Paris, France, 2015; ISBN 978-92-78-41240-1. [Google Scholar]
- Newcombe, R.G. Interval estimation for the difference between independent proportions: Comparison of eleven methods. Stat. Med. 1998, 17, 873–890. [Google Scholar] [CrossRef]
- Vugts, M.A.P.; Joosen, M.C.W.; van der Geer, J.E.; Zedlitz, A.M.E.E.; Vrijhoef, H.J.M. The effectiveness of various computer-based interventions for patients with chronic pain or functional somatic syndromes: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0196467. [Google Scholar] [CrossRef]
- Baumeister, H.; Paganini, S.; Sander, L.; Lin, J.; Schlicker, S.; Terhorst, Y.; Moshagen, M.; Bengel, J.; Lehr, D.; Ebert, D.D. Effectiveness of a guided internet- and mobile-based intervention for patients with chronic back pain and depression (WARD-BP): A multicenter, pragmatic randomized controlled trial. Psychother. Psychosom. 2021, 90, 255–268. [Google Scholar] [CrossRef]
- Street, L.L.; Louma, J.B. Control Groups in Psychosocial Intervention Research: Ethical and Methodological Issues. Ethics Behav. 2002, 12, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Braun, L.; Freund, J.; Thielecke, J.; Baumeister, H.; Ebert, D.D.; Titzler, I. Barriers to and Facilitators of Engaging With and Adhering to Guided Internet-based Interventions for Depression Prevention and Reduction of Pain-Related Disability in Green Professions: Mixed Methods Study. JMIR Ment. Health. 2022, 9(10), e39122. [Google Scholar] [CrossRef]
- Donkin, L.; Christensen, H.; Naismith, S.L.; Neal, B.; Hickie, I.B.; Glozier, N. A systematic review of the impact of adherence on the effectiveness of e-therapies. J. Med. Internet Res. 2011, 13, e1772. [Google Scholar] [CrossRef] [PubMed]
- DasMahapatra, P.; Chiauzzi, E.; Pujol, L.M.; Los, C.; Trudeau, K.J. Mediators and moderators of chronic pain outcomes in an online self-management program. Clin. J. Pain 2015, 31, 404–413. [Google Scholar] [CrossRef] [PubMed]
- Trompetter, H.R.; Bohlmeijer, E.T.; Lamers, S.M.A.; Schreurs, K.M.G. Positive psychological wellbeing is required for online self-help acceptance and commitment therapy for chronic pain to be effective. Front. Psychol. 2016, 7, 353. [Google Scholar] [CrossRef]
- McCracken, L.M.; Turk, D.C. Behavioral and cognitive-behavioral treatment for chronic pain: Outcome, predictors of outcome, and treatment process. Spine 2002, 27, 2564–2573. [Google Scholar] [CrossRef]
- Maxwell, A.; Özmen, M.; Iezzi, A.; Richardson, J. Deriving population norms for the AQoL-6D and AQoL-8D multi-attribute utility instruments from web-based data. Qual. Life Res. 2016, 25, 3209–3219. [Google Scholar] [CrossRef]
- Palit, S.; Fillingim, R.B.; Bartley, E.J. Pain resilience moderates the influence of negative pain beliefs on movement-evoked pain in older adults. J. Behav. Med. 2020, 43, 754–763. [Google Scholar] [CrossRef]
- Wetherell, J.L.; Petkus, A.J.; Alonso-Fernandez, M.; Bower, E.S.; Steiner, A.R.W.; Afari, N. Age moderates response to acceptance and commitment therapy vs. cognitive behavioral therapy for chronic pain. Int. J. Geriatr. Psychiatry 2016, 31, 302–308. [Google Scholar] [CrossRef]
- Xie, L.; Zhang, S.; Xin, M.; Zhu, M.; Lu, W.; Mo, P.K.H. Electronic health literacy and health-related outcomes among older adults: A systematic review. Prev. Med. 2022, 157, 106997. [Google Scholar] [CrossRef]
- Wuyou, S.; Facca, D. Digital health in a broadband land: The role of digital health literacy within rural environments. Health Sci. Inq. 2020, 11, 140–143. [Google Scholar] [CrossRef]
- Goossens, M.E.J.B.; Vlaeyen, J.W.S.; Hidding, A.; Kole-Snijders, A.; Evers, S.M.A.A. Treatment expectancy affects the outcome of cognitive-behavioral interventions in chronic pain. Clin. J. Pain 2005, 21, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Smeets, R.J.E.M.; Beelen, S.; Goossens, M.E.J.B.; Schouten, E.G.W.; Knottnerus, J.A.; Vlaeyen, J.W.S. Treatment expectancy and credibility are associated with the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. Clin. J. Pain 2008, 24, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Stewart, H.; Jameson, J.P.; Curtin, L. The relationship between stigma and self-reported willingness to use mental health services among rural and urban older adults. Psychol. Serv. 2015, 12, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Hagen, B.N.M.; Sawatzky, A.; Harper, S.L.; O’Sullivan, T.L.; Jones-Bitton, A. “Farmers aren’t into the emotions and things, right?”: A qualitative exploration of motivations and barriers for mental health help-seeking among Canadian farmers. J. Agromedicine 2021, 27, 113–123. [Google Scholar] [CrossRef]
- Bendig, E.; Bauereiß, N.; Buntrock, C.; Habibović, M.; Ebert, D.D.; Baumeister, H. Lessons learned from an attempted randomized-controlled feasibility trial on “WIDeCAD”—An internet-based depression treatment for people living with coronary artery disease (CAD). Internet Interv. 2021, 24, 100375. [Google Scholar] [CrossRef]
- Ebert, D.D.; Van Daele, T.; Nordgreen, T.; Karekla, M.; Compare, T.A.; Zarbo, C.; Brugnera, A.; Oeverland, S.; Trebbi, G.; Jensen, K.L.; et al. Internet and mobile-based psychological interventions: Applications, efficacy and potential for improving mental health. Eur. Psychol. 2018, 23, 167–187. [Google Scholar] [CrossRef]
- Lin, J.; Faust, B.; Ebert, D.D.; Krämer, L.; Baumeister, H. A web-based acceptance-facilitating intervention for identifying patients’ acceptance, uptake, and adherence of internet- and mobile-based pain interventions: Randomized controlled trial. J. Med. Internet Res. 2018, 20, e244. [Google Scholar] [CrossRef]
- Thew, G.R. IAPT and the internet: The current and future role of therapist-guided internet interventions within routine care settings. Cogn. Behav. Ther. 2020, 13, e4. [Google Scholar] [CrossRef]
- Hagen, B.N.M.; Harper, S.L.; O’Sullivan, T.L.; Jones-Bitton, A. Tailored mental health literacy training improves mental health knowledge and confidence among canadian farmers. Int. J. Environ. Res. Public Health 2020, 17, 3807. [Google Scholar] [CrossRef]
- Hart, C.R.; Berry, H.L.; Tonna, A.M. Improving the mental health of rural New South Wales communities facing drought and other adversities. Aust. J. Rural Health 2011, 19, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Neter, E.; Brainin, E. eHealth literacy: Extending the digital divide to the realm of health information. J. Med. Internet Res. 2012, 14, e19. [Google Scholar] [CrossRef] [PubMed]
- van de Graaf, D.L.; Trompetter, H.R.; Smeets, T.; Mols, F. Online Acceptance and Commitment Therapy (ACT) interventions for chronic pain: A systematic literature review. Internet Interv. 2021, 26, 100465. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Scott, W.; Carpenter, L.; Norton, S.; Domhardt, M.; Baumeister, H.; McCracken, L.M. Acceptance and commitment therapy for chronic pain: Protocol of a systematic review and individual participant data meta-Analysis. Syst. Rev. 2019, 8, 140. [Google Scholar] [CrossRef]
| Characteristic | Total Sample (N = 81) | Intervention Group (n = 43) | Control Group (n = 38) | |
|---|---|---|---|---|
| Age, mean (SD) | 56.98 ± 8.65 | 57.23 ± 9.50 | 56.68 ± 7.70 | |
| Gender | Male, n (%) | 24 (29.6) | 13 (30.2) | 11 (28.9) |
| Female, n (%) | 57 (70.4) | 30 (69.8) | 27 (71.1) | |
| Relationship | Single, n (%) | 2 (2.5) | 1 (2.3) | 1 (2.6) |
| In partnership, n (%) | 4 (4.9) | 0 (0.0) | 4 (10.5) | |
| Married, n (%) | 74 (91.4) | 41 (95.3) | 33 (86.8) | |
| Divorced or separated, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Widowed, n (%) | 1 (1.2) | 1 (2.3) | 0 (0.0) | |
| Ethnicity | Caucasian, n (%) | 79 (97.5) | 41 (95.3) | 38 (100.0) |
| Other, n (%) | 2 (2.5) | 2 (4.7) | 0 (0.0) | |
| Country of birth | Germany, n (%) | 80 (98.8) | 43 (100.0) | 37 (97.4) |
| Other, n (%) | 1 (1.2) | 0 (0.0) | 1 (2.6) | |
| Level of education a | Low, n (%) | 53 (65.4) | 28 (65.1) | 25 (65.8) |
| Middle, n (%) | 15 (18.5) | 9 (20.9) | 6 (15.8) | |
| High, n (%) | 13 (16.0) | 6 (14.0) | 7 (18.4) | |
| Employment status | Entrepreneur, n (%) | 32 (39.5) | 15 (34.9) | 17 (44.7) |
| Contributing spouse, n (%) | 22 (27.2) | 12 (27.9) | 10 (26.3) | |
| Contributing family member, n (%) | 9 (11.1) | 7 (16.3) | 2 (5.3) | |
| Pensioner or spouse of pensioner, n (%) | 14 (17.3) | 9 (20.9) | 5 (13.2) | |
| Incapacitated for work, n (%) | 4 (4.9) | 0 (0.0) | 4 (10.5) | |
| Company size (number of contributing persons) b | 1–4, n (%) | 51 (76.1) | 28 (77.8) | 23 (74.2) |
| 5–9, n (%) | 9 (13.4) | 6 (16.7) | 3 (9.7) | |
| 10–24, n (%) | 6 (9.0) | 1 (2.8) | 5 (16.1) | |
| 25–49, n (%) | 1 (1.5) | 1 (2.8) | 0 (0.0) | |
| ≥50, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Main area of production b | Dairy farming, n (%) | 24 (35.8) | 13 (36.1) | 11 (35.5) |
| Arable farming, n (%) | 16 (23.9) | 6 (16.7) | 10 (32.3) | |
| Livestock farming, n (%) | 10 (14.9) | 7 (19.4) | 3 (9.7) | |
| Fruit farming, n (%) | 1 (1.5) | 1 (2.8) | 0 (0.0) | |
| Viniculture, n (%) | 5 (7.5) | 2 (5.6) | 3 (9.7) | |
| Forestry, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Horticulture, n (%) | 5 (7.5) | 2 (5.6) | 3 (9.7) | |
| Biogas plant, n (%) | 1 (1.5) | 1 (2.8) | 0 (0.0) | |
| Other, n (%) | 5 (7.5) | 4 (11.1) | 1 (3.2) | |
| Personal income per month (in Euros) c | <1000, n (%) | 8 (23.5) | 3 (17.6) | 5 (29.4) |
| 1000–2000, n (%) | 12 (35.3) | 8 (47.1) | 4 (23.5) | |
| 2000–3000, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| 3000–4000, n (%) | 4 (11.8) | 0 (0.0) | 4 (23.5) | |
| 4000–5000, n (%) | 1 (2.9) | 1 (5.9) | 0 (0.0) | |
| >5000, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Not disclosed, n (%) | 9 (26.5) | 5 (29.4) | 4 (23.5) | |
| Minor second job d | Yes, n (%) | 6 (19.4) | 4 (21.1) | 2 (16.7) |
| No, n (%) | 25 (80.6) | 15 (78.9) | 10 (83.3) | |
| Chronic pain region e,f | Headaches, n (%) | 14 (17.3) | 9 (20.9) | 5 (13.2) |
| Back pain, n (%) | 37 (45.7) | 20 (46.5) | 17 (44.7) | |
| Tumor pain, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Shoulder/arm pain, n (%) | 29 (35.8) | 15 (34.9) | 14 (36.8) | |
| Muscle/joint pain, n (%) | 39 (48.1) | 22 (51.2) | 17 (44.7) | |
| Other, n (%) | 17 (21.0) | 8 (18.6) | 9 (23.7) | |
| Disability degree f | Yes, n (%) | 16 (30.8) | 8 (29.6) | 8 (32.0) |
| No, n (%) | 35 (67.3) | 18 (66.7) | 17 (68.0) | |
| Not disclosed, n (%) | 1 (1.9) | 1 (3.7) | 0 (0.0) | |
| Previous pain treatment f | Yes, n (%) | 32 (61.5) | 15 (55.6) | 17 (68.0) |
| No, n (%) | 20 (38.5) | 12 (44.4) | 8 (32.0) |
| IG (n = 43) | CG (n = 38) | ITT a (95% CI) | p b | Cohen’s d (95% CI) | ||
|---|---|---|---|---|---|---|
| Primary outcome | ||||||
| Pain interference (MPI) | Baseline | 33.28 ± 12.11 | 35.79 ± 10.85 | |||
| 9 weeks | 29.75 ± 14.94 | 31.81 ± 10.56 | −0.16 [−0.64; 0.32] | 0.256 | −0.16 [−0.59; 0.28] | |
| Secondary outcomes | ||||||
| Pain-related outcomes | ||||||
| Pain interference (MPI) | 6 months | 27.02 ± 14.22 | 28.36 ± 12.50 | 0.02 [−0.47; 0.50] | 0.947 | 0.10 [−0.34; 0.54] |
| 12 months | 26.10 ± 14.38 | 28.32 ± 12.01 | −0.04 [−0.49; 0.42] | 0.872 | −0.17 [−0.60; 0.27] | |
| Pain-related interference with function (BPI) | Baseline | 30.70 ± 15.95 | 30.03 ± 14.02 | |||
| 9 weeks | 26.30 ± 16.94 | 27.27 ± 15.29 | −0.09 [−0.52; 0.33] | 0.670 | −0.06 [−0.50; 0.38] | |
| 6 months | 21.83 ± 14.56 | 23.85 ± 13.84 | −0.17 [−0.71; 0.36] | 0.520 | −0.14 [−0.58; 0.30] | |
| 12 months | 21.59 ± 16.74 | 26.78 ± 15.78 | −0.34 [−0.84; 0.16] | 0.175 | −0.32 [−0.76; 0.12] | |
| Reliable change (MPI) | 9 weeks | 13 (30.2) | 14 (36.8) | 0.58 [0.22; 1.54] | 0.281 | - |
| 6 months | 20 (46.5) | 22 (57.9) | 0.54 [0.22; 1.31] | 0.175 | - | |
| 12 months | 22 (51.2) | 15 (39.5) | 1.66 [0.64; 4.29] | 0.300 | - | |
| Reliable deterioration (MPI) | 9 weeks | 8 (18.6) | 3 (7.9) | 0.88 [0.17; 4.62] | 0.875 | - |
| 6 months | 5 (11.6) | 5 (13.2) | 0.57 [0.09; 3.60] | 0.551 | - | |
| 12 months | 4 (9.3) | 2 (5.3) | 0.88 [0.12; 6.56] | 0.899 | - | |
| Pain intensity (NRS) | Baseline | 17.47 ± 7.31 | 17.37 ± 6.49 | |||
| 9 weeks | 15.48 ± 7.88 | 15.00 ± 6.75 | 0.05 [−0.39; 0.49] | 0.809 | 0.06 [−0.37; 0.50] | |
| 6 months | 13.38 ± 7.31 | 14.32 ± 6.56 | −0.14 [−0.69; 0.40] | 0.594 | −0.13 [−0.57; 0.30] | |
| 12 months | 13.66 ± 8.00 | 14.95 ± 7.37 | −0.18 [−0.63; 0.28] | 0.438 | −0.17 [−0.60; 0.27] | |
| Subjective rating of perceived improvement | 9 weeks | 3.63 ± 1.21 | 3.76 ± 1.46 | −0.10 [−0.65; 0.45] | 0.709 | −0.10 [−0.53; 0.34] |
| 6 months | 3.20 ± 1.48 | 3.71 ± 1.48 | −0.34 [−0.86; 0.18] | 0.193 | −0.35 [−0.78; 0.09] | |
| 12 months | 3.13 ± 1.49 | 3.39 ± 1.38 | −0.18 [−0.75; 0.38] | 0.520 | −0.18 [−0.62; 0.26] | |
| ACT-based measures | ||||||
| Activity engagement (CPAQ subscale) | Baseline | 36.33 ± 10.22 | 37.37 ± 11.23 | |||
| 9 weeks | 38.40 ± 13.27 | 37.21 ± 11.30 | 0.17 [−0.19; 0.53] | 0.356 | 0.10 [−0.34; 0.53] | |
| 6 months | 40.36 ± 13.64 | 36.37 ± 12.79 | 0.37 [−0.08; 0.82] | 0.102 | 0.30 [−0.14; 0.74] | |
| 12 months | 42.39 ± 12.44 | 38.93 ± 9.77 | 0.36 [−0.09; 0.82] | 0.116 | 0.31 [−0.13; 0.74] | |
| Pain willingness (CPAQ subscale) | Baseline | 26.14 ± 10.01 | 26.24 ± 10.32 | |||
| 9 weeks | 30.01 ± 10.82 | 29.98 ± 8.82 | 0.01 [−0.33; 0.35] | 0.948 | 0.003 [−0.43; 0.44] | |
| 6 months | 31.49 ± 11.06 | 29.48 ± 9.36 | 0.20 [−0.21; 0.61] | 0.320 | 0.20 [−0.24; 0.63] | |
| 12 months | 32.86 ± 11.17 | 28.49 ± 9.83 | 0.41 [−0.04; 0.86] | 0.070 | 0.41 [−0.03; 0.85] | |
| Chronic pain Acceptance (CPAQ total score) | Baseline | 62.47 ± 17.77 | 63.61 ± 18.71 | |||
| 9 weeks | 68.41 ± 21.43 | 67.18 ± 17.84 | 0.11 [−0.20; 0.43] | 0.474 | 0.06 [−0.37; 0.50] | |
| 6 months | 71.85 ± 22.43 | 65.85 ± 18.85 | 0.33 [−0.05; 0.71] | 0.085 | 0.29 [−0.15; 0.73] | |
| 12 months | 75.26 ± 20.70 | 67.43 ± 17.61 | 0.44 [0.04; 0.84] | 0.034 | 0.41 [−0.04; 0.84] | |
| Cognitive fusion (CFQ) | Baseline | 23.35 ± 8.33 | 19.58 ± 9.47 | |||
| 9 weeks | 19.13 ± 8.59 | 16.94 ± 8.16 | 0.02 [−0.42; 0.46] | 0.926 | 0.26 [−0.18; 0.70] | |
| 6 months | 18.07 ± 9.13 | 19.05 ± 9.39 | −0.34 [−0.80; 0.12] | 0.145 | −0.11 [−0.54; 0.33] | |
| 12 months | 17.95 ± 8.80 | 20.02 ± 8.80 | −0.46 [−0.92; −0.001] | 0.050 | −0.23 [−0.67; 0.20] | |
| Committed action (CAQ) | Baseline | 68.74 ± 14.98 | 68.84 ± 16.87 | |||
| 9 weeks | 71.78 ± 15.10 | 72.85 ± 14.56 | −0.07 [−0.46; 0.32] | 0.727 | −0.07 [−0.51; 0.36] | |
| 6 months | 71.84 ± 16.59 | 70.58 ± 17.38 | 0.08 [−0.29; 0.45] | 0.665 | 0.07 [−0.36; 0.51] | |
| 12 months | 74.27 ± 17.64 | 70.76 ± 17.48 | 0.20 [−0.27; 0.68] | 0.387 | 0.20 [−0.24; 0.64] | |
| Mental health–related outcomes | ||||||
| Depressive symptom severity (QIDS-SR16) | Baseline | 7.63 ± 3.80 | 7.89 ± 4.43 | |||
| 9 weeks | 5.28 ± 3.40 | 6.41 ± 4.02 | −0.26 [−0.65; 0.13] | 0.187 | −0.31 [−0.74; 0.13] | |
| 6 months | 5.26 ± 4.16 | 6.89 ± 4.60 | −0.33 [−0.74; 0.09] | 0.121 | −0.37 [−0.81; 0.07] | |
| 12 months | 5.77 ± 4.14 | 6.36 ± 4.28 | −0.10 [−0.54; 0.34] | 0.650 | −0.14 [−0.58; 0.30] | |
| Onset of MDD (QIDS-SR16) | 9 weeks | 0 of 38 (0.0) | 0 of 31 (0.0) | 1.00 [1.00; 1.00] | NA | - |
| 6 months | 1 of 38 (2.6) | 3 of 31 (9.7) | 0.95 [0.89; 1.02] | 0.131 | - | |
| 12 months | 1 of 38 (2.6) | 1 of 31 (3.2) | 0.97 [0.93; 1.02] | 0.290 | - | |
| Onset of MDD (CIDI-SC) | 9 weeks | 1 of 35 (2.8) | 0 of 26 (0.0) | 1.02 [0.98; 1.07] | 0.350 | - |
| 6 months | 1 of 35 (2.8) | 2 of 26 (7.7) | 0.97 [0.89; 1.06] | 0.491 | - | |
| 12 months | 2 of 35 (5.7) | 2 of 26 (7.7) | 0.99 [0.90; 1.09] | 0.901 | - | |
| Remission of MDD (QIDS-SR16) | 9 weeks | 3 of 5 (60.0) | 3 of 7 (42.9) | 0.97 [0.89; 1.06] | 0.491 | - |
| 6 months | 1 of 5 (20.0) | 4 of 7 (57.1) | 0.92 [0.85; 1.00] | 0.062 | - | |
| 12 months | 2 of 5 (40.0) | 5 of 7 (71.4) | 0.95 [0.86; 1.04] | 0.254 | - | |
| Remission of MDD (CIDI-SC) | 9 weeks | 5 of 8 (62.5) | 8 of 12 (66.7) | 0.91 [0.77; 1.07] | 0.254 | - |
| 6 months | 5 of 8 (62.5) | 5 of 12 (41.7) | 0.98 [0.85; 1.14] | 0.837 | - | |
| 12 months | 5 of 8 (62.5) | 8 of 12 (66.7) | 0.91 [0.77; 1.07] | 0.254 | - | |
| Anxiety (GAD-7) | Baseline | 7.16 ± 4.08 | 5.87 ± 4.08 | |||
| 9 weeks | 4.38 ± 3.60 | 4.36 ± 3.41 | −0.19 [−0.62; 0.24] | 0.374 | −0.01 [−0.44; 0.43] | |
| 6 months | 4.45 ± 3.75 | 4.77 ± 3.89 | −0.26 [−0.77; 0.26] | 0.318 | −0.08 [−0.52; 0.35] | |
| 12 months | 3.93 ± 3.94 | 5.20 ± 4.06 | −0.50 [−0.95; −0.04] | 0.033 | −0.32 [−0.76; 0.12] | |
| Perceived stress (PSS) | Baseline | 18.26 ± 6.60 | 17.76 ± 6.94 | |||
| 9 weeks | 15.15 ± 8.33 | 14.03 ± 7.45 | 0.09 [−0.31; 0.50] | 0.652 | 0.14 [−0.30; 0.58] | |
| 6 months | 14.77 ± 7.77 | 15.51 ± 9.05 | −0.13 [−0.58; 0.33] | 0.578 | −0.09 [−0.52; 0.35] | |
| 12 months | 13.50 ± 7.31 | 16.99 ± 7.85 | −0.49 [−0.95; −0.03] | 0.037 | −0.46 [−0.90; −0.02] | |
| Insomnia (ISI) | Baseline | 8.63 ± 4.91 | 9.08 ± 6.16 | |||
| 9 weeks | 7.75 ± 5.23 | 7.00 ± 5.08 | 0.20 [−0.22; 0.62] | 0.340 | 0.15 [−0.29; 0.58] | |
| 6 months | 7.24 ± 5.44 | 7.83 ± 5.69 | −0.06 [−0.52; 0.41] | 0.809 | −0.11 [−0.54; 0.33] | |
| 12 months | 7.33 ± 6.35 | 7.32 ± 5.71 | 0.06 [−0.34; 0.46] | 0.771 | 0.002 [−0.43; 0.44] | |
| Alcohol consumption (AUDIT-10) | Baseline | 2.58 ± 2.00 | 2.13 ± 1.79 | |||
| 9 weeks | 2.09 ± 1.87 | 1.98 ± 1.74 | −0.14 [−0.41; 0.13] | 0.303 | −0.06 [−0.50; 0.38] | |
| 6 months | 2.33 ± 1.54 | 1.74 ± 1.50 | 0.22 [−0.20; 0.63] | 0.294 | 0.39 [−0.05; 0.83] | |
| 12 months | 1.59 ± 1.03 | 1.87 ± 1.39 | −0.36 [−0.86; 0.13] | 0.148 | −0.22 [−0.66; 0.22] | |
| Quality of life (AQoL-8D) | Baseline | 69.44 ± 11.01 | 68.53 ± 10.26 | |||
| 9 weeks | 71.09 ± 13.15 | 71.11 ± 11.85 | −0.07 [−0.36; 0.21] | 0.603 | −0.002 [−0.44; 0.43] | |
| 6 months | 73.29 ± 12.83 | 70.12 ± 13.50 | 0.17 [−0.16; 0.50] | 0.300 | 0.24 [−0.20; 0.68] | |
| 12 months | 77.14 ± 11.52 | 70.11 ± 10.74 | 0.54 [0.19; 0.89] | 0.003 | 0.63 [0.18; 1.08] | |
| Subjective prognosis of employment (SPE) | Baseline | 1.51 ± 1.08 | 1.47 ± 0.98 | |||
| 9 weeks | 1.35 ± 1.16 | 1.17 ± 1.05 | 0.14 [−0.20; 0.47] | 0.425 | 0.16 [−0.27; 0.60] | |
| 6 months | 1.18 ± 1.01 | 1.19 ± 1.09 | −0.04 [−0.48; 0.41] | 0.874 | −0.01 [−0.45; 0.42] | |
| 12 months | 1.34 ± 1.17 | 1.24 ± 1.11 | 0.07 [−0.40; 0.54] | 0.780 | 0.09 [−0.35; 0.52] |
| IG, No. (%) | CG, No. (%) | Difference between Groups, % (95% CI) a | ||||||
|---|---|---|---|---|---|---|---|---|
| Health Care Service | Baseline b (n = 43) | 6-Month FU c (n = 27) | 12-Month FU d (n = 25) | Baseline b (n = 38) | 6-Month FU c (n = 30) | 12-Month FU d (n = 28) | 6-Month FU c | 12-Month FU d |
| Primary care clinician | 39 (90.7) | 19 (70.4) | 19 (76.0) | 34 (89.5) | 27 (90.0) | 23 (82.1) | −0.20 [−0.40; 0.01] | −0.06 [−0.28; 0.16] |
| Psychotherapist | 1 (2.3) | 1 (3.7) | 0 (0) | 1 (2.6) | 1 (3.3) | 1 (3.6) | 0.004 [−0.13; 0.15] | −0.04 [−0.18; 0.10] |
| Psychiatrist, Neurologist, Psychosomatic medicine specialist | 2 (4.7) | 1 (3.7) | 2 (8.0) | 1 (2.6) | 2 (6.7) | 2 (7.1) | −0.03 [−0.18; 0.12] | 0.01 [−0.16; 0.19] |
| Pain treatment e | 9 (20.9) | 3 (11.1) | 3 (12.0) | 8 (21.1) | 8 (26.7) | 2 (7.1) | −0.16 [−0.35; 0.05] | 0.05 [−0.13; 0.24] |
| Psychological pain treatment e | 1 (2.3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (3.6) | 0.0 [−0.11; 0.12] | −0.04 [−0.18; 0.10] |
| Pain medication prescription | 30 (69.8) | 9 (33.3) | 9 (36.0) | 25 (65.8) | 17 (56.7) | 13 (46.4) | −0.23 [−0.45; 0.02] | −0.10 [−0.34; 0.15] |
| Antidepressant prescription | 3 (7.0) | 3 (11.1) | 2 (8.0) | 0 (0) | 0 (0) | 0 (0) | 0.11 [−0.02; 0.28] | 0.08 [−0.05; 0.25] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Braun, L.; Terhorst, Y.; Titzler, I.; Freund, J.; Thielecke, J.; Ebert, D.D.; Baumeister, H. Lessons Learned from an Attempted Pragmatic Randomized Controlled Trial for Improvement of Chronic Pain-Associated Disability in Green Professions: Long-Term Effectiveness of a Guided Online-Based Acceptance and Commitment Therapy (PACT-A). Int. J. Environ. Res. Public Health 2022, 19, 13858. https://doi.org/10.3390/ijerph192113858
Braun L, Terhorst Y, Titzler I, Freund J, Thielecke J, Ebert DD, Baumeister H. Lessons Learned from an Attempted Pragmatic Randomized Controlled Trial for Improvement of Chronic Pain-Associated Disability in Green Professions: Long-Term Effectiveness of a Guided Online-Based Acceptance and Commitment Therapy (PACT-A). International Journal of Environmental Research and Public Health. 2022; 19(21):13858. https://doi.org/10.3390/ijerph192113858
Chicago/Turabian StyleBraun, Lina, Yannik Terhorst, Ingrid Titzler, Johanna Freund, Janika Thielecke, David Daniel Ebert, and Harald Baumeister. 2022. "Lessons Learned from an Attempted Pragmatic Randomized Controlled Trial for Improvement of Chronic Pain-Associated Disability in Green Professions: Long-Term Effectiveness of a Guided Online-Based Acceptance and Commitment Therapy (PACT-A)" International Journal of Environmental Research and Public Health 19, no. 21: 13858. https://doi.org/10.3390/ijerph192113858
APA StyleBraun, L., Terhorst, Y., Titzler, I., Freund, J., Thielecke, J., Ebert, D. D., & Baumeister, H. (2022). Lessons Learned from an Attempted Pragmatic Randomized Controlled Trial for Improvement of Chronic Pain-Associated Disability in Green Professions: Long-Term Effectiveness of a Guided Online-Based Acceptance and Commitment Therapy (PACT-A). International Journal of Environmental Research and Public Health, 19(21), 13858. https://doi.org/10.3390/ijerph192113858






