Equity Analysis of Repeated Cross-Sectional Survey Data on Mental Health Outcomes in Saskatchewan, Canada during COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Outcome Variables
2.3. Independent Variables and Covariates
2.4. Data Analysis
2.5. Implications Identified through a World Café Policy Dialogue
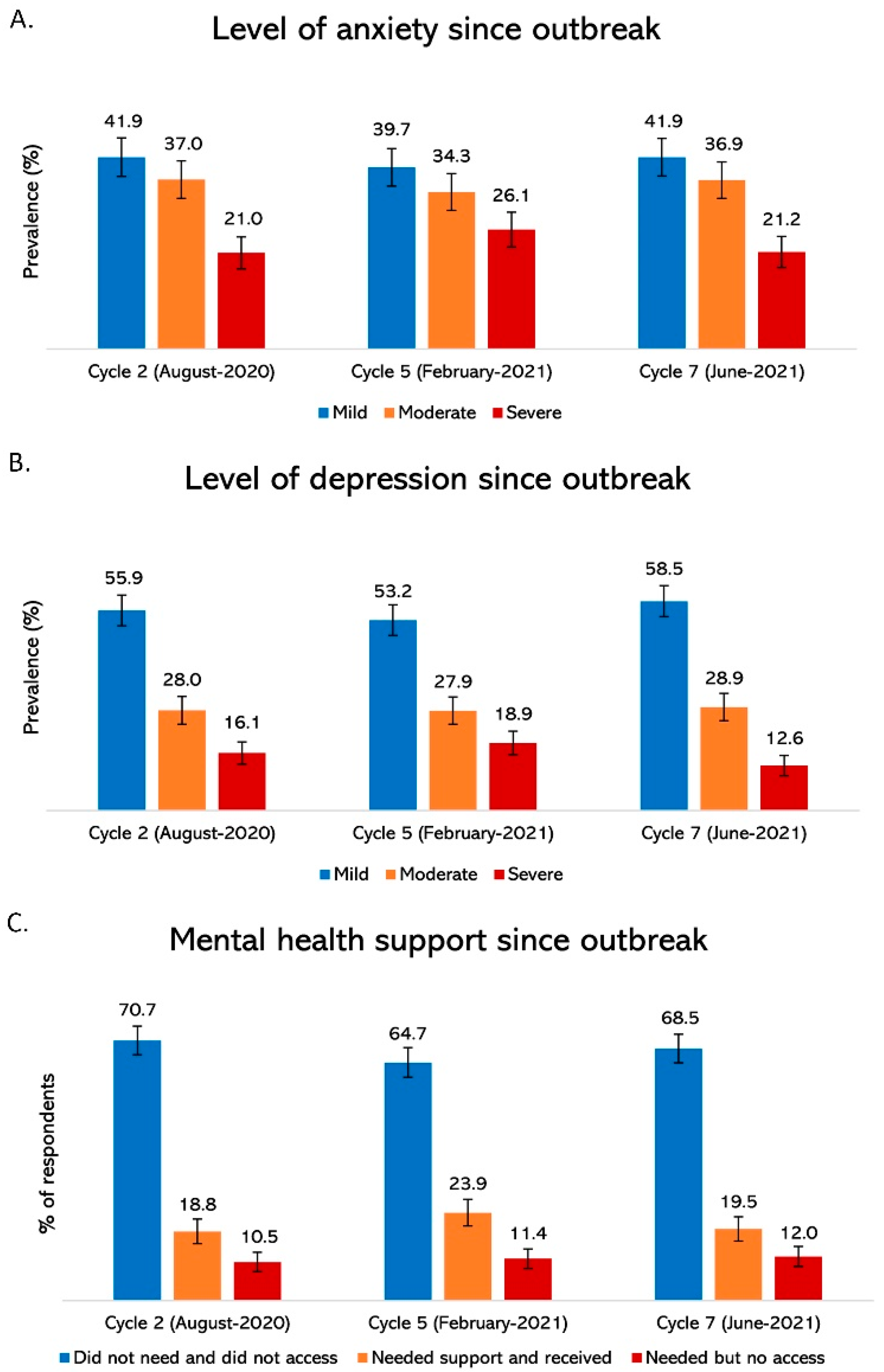
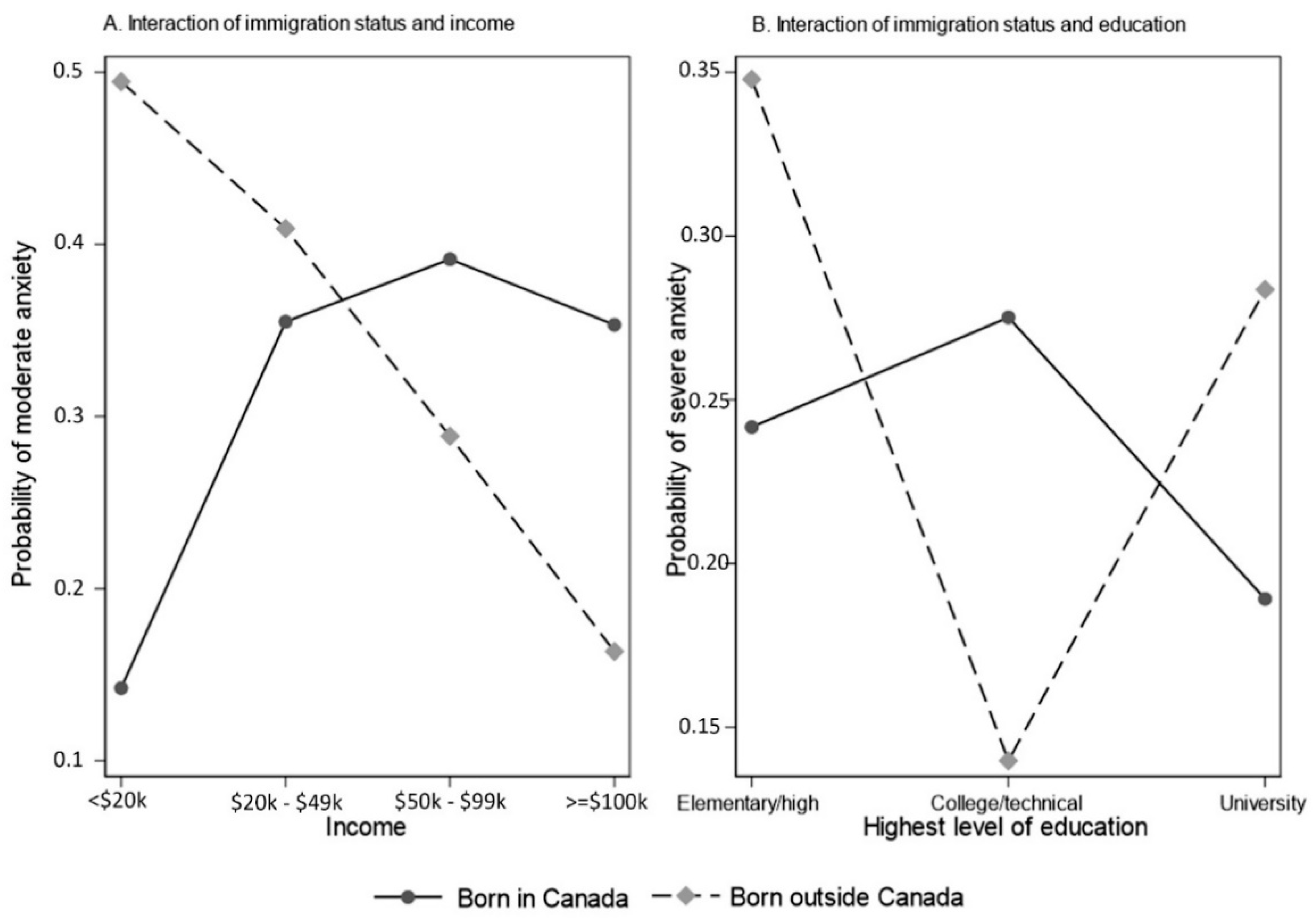
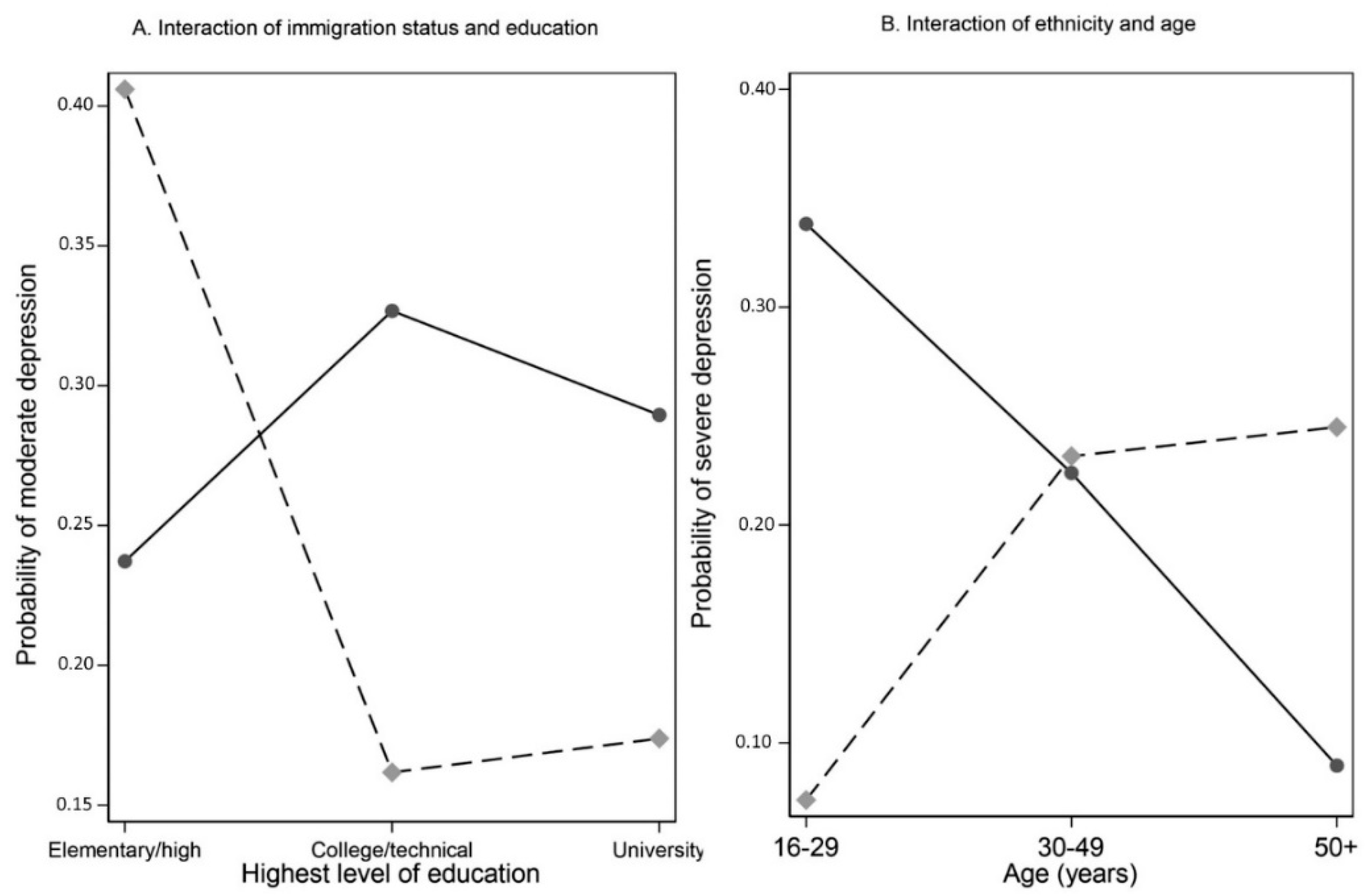
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zakaria, F. A Pandemic Should Be the Great Equalizer. This One Had the Opposite Effect. Available online: https://www.washingtonpost.com/opinions/a-pandemic-should-be-the-great-equalizer-this-one-had-the-opposite-effect/2020/10/15/ca5af870-0f20-11eb-8074-0e943a91bf08_story.html (accessed on 15 October 2022).
- Galasso, V. COVID: Not a Great Equalizer. Cesifo Econ. Stud. 2020, 66, 376–393. [Google Scholar] [CrossRef]
- Mein, S.A. COVID-19 and health disparities: The reality of “the great equalizer”. J. Gen. Intern. Med. 2020, 35, 2439–2440. [Google Scholar] [CrossRef] [PubMed]
- Timothy, R. Coronavirus Is Not the Great Equalizer—Race Matters. Available online: https://theconversation.com/coronavirus-is-not-the-great-equalizer-race-matters-133867 (accessed on 15 October 2022).
- Abedi, V.; Olulana, O.; Avula, V.; Chaudhary, D.; Khan, A.; Shahjouei, S.; Li, J.; Zand, R. Racial, economic, and health inequality and COVID-19 infection in the United States. J. Racial Ethn. Health Disparities 2021, 8, 732–742. [Google Scholar] [CrossRef] [PubMed]
- Boserup, B.; McKenney, M.; Elkbuli, A. Disproportionate impact of COVID-19 pandemic on Racial and Ethnic Minorities. Am. Surg. 2020, 86, 1615–1622. [Google Scholar] [CrossRef] [PubMed]
- Jacques-Aviñó, C.; López-Jiménez, T.; Medina-Perucha, L.; de Bont, J.; Gonçalves, A.Q.; Duarte-Salles, T.; Berenguera, A. Gender-based approach on the social impact and mental health in Spain during COVID-19 lockdown: A cross-sectional study. BMJ Open 2020, 10, e044617. [Google Scholar] [CrossRef] [PubMed]
- Mojtahedi, D.; Dagnall, N.; Denovan, A.; Clough, P.; Hull, S.; Canning, D.; Lilley, C.; Papageorgiou, K.A. The relationship between mental toughness, job loss, and mental health issues during the COVID-19 pandemic. Front. Psychiatry 2021, 11, 607246. [Google Scholar] [CrossRef] [PubMed]
- Amerio, A.; Brambilla, A.; Morganti, A.; Aguglia, A.; Bianchi, D.; Santi, F.; Costantini, L.; Odone, A.; Costanza, A.; Signorelli, C.; et al. COVID-19 Lockdown: Housing built environment’s effects on mental health. Int. J. Environ. Res. Public Health 2020, 17, 5973. [Google Scholar] [CrossRef]
- Bowler, R.M.; Harris, M.; Li, J.; Gocheva, V.; Stellman, S.D.; Wilson, K.; Alper, H.; Schwarzer, R.; Cone, J.E. Longitudinal mental health impact among police responders to the 9/11 terrorist attack. Am. J. Ind. Med. 2012, 55, 297–312. [Google Scholar] [CrossRef]
- Galea, S.; Brewin, C.R.; Gruber, M.; Jones, R.T.; King, D.W.; King, L.A.; McNally, R.J.; Ursano, R.J.; Petukhova, M.; Kessler, R.C. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Arch. Gen. Psychiatry 2007, 64, 1427–1434. [Google Scholar] [CrossRef]
- Kar, N.; Krishnaraaj, R.; Rameshraj, K. Long-term mental health outcomes following the 2004 Asian tsunami disaster: A comparative study on direct and indirect exposure. Disaster Health 2013, 2, 35–45. [Google Scholar] [CrossRef]
- Findlay, L.; Arim, R. Canadians Report Lower Self-Perceived Mental Health during the COVID-19 Pandemic. StatCan COVID-19: Data to Insights for a Better Canada. Stat. Can. 2020. Available online: https://www150.statcan.gc.ca/n1/en/catalogue/45280001202000100003 (accessed on 15 October 2022).
- Statistics Canada. Survey on COVID-19 and Mental Health, February to May 2021. 2021. Available online: https://www150.statcan.gc.ca/n1/daily-quotidien/210927/dq210927a-eng.htm (accessed on 15 October 2022).
- Arriagada, P.; Hahmann, T.; O’Donnell, V. Indigenous People and Mental Health during the COVID-19 Pandemic. StatCan COVID-19: Data to Insights for a Better Canada. Stat. Can. 2020. Available online: https://www150.statcan.gc.ca/n1/en/pub/45-28-0001/2020001/article/00035-eng.pdf?st=EBR4vCbO (accessed on 15 October 2022).
- Jenkins, E.K.; McAuliffe, C.; Hirani, S.; Richardson, C.; Thomson, K.C.; McGuinness, L.; Morris, J.; Kousoulis, A.; Gadermann, A. A portrait of the early and differential mental health impacts of the COVID-19 pandemic in Canada: Findings from the first wave of a nationally representative cross-sectional survey. Prev. Med. 2021, 145, 106333. [Google Scholar] [CrossRef] [PubMed]
- Miconi, D.; Li, Z.Y.; Frounfelker, R.L.; Santavicca, T.; Cénat, J.M.; Venkatesh, V.; Rousseau, C. Ethno-cultural disparities in mental health during the COVID-19 pandemic: A cross-sectional study on the impact of exposure to the virus and COVID-19-related discrimination and stigma on mental health across ethno-cultural groups in Quebec (Canada). BJPsych Open 2020, 7, e14. [Google Scholar] [CrossRef] [PubMed]
- Dahlgren, G.; Whitehead, M. Policies and Strategies to Promote Social Equity in Health. 1991. Available online: https://econpapers.repec.org/paper/hhsifswps/2007_5f014.htm (accessed on 15 October 2022).
- Dahlgren, G.; Whitehead, M. European Strategies for Tackling Social Inequities in Health: Levelling up Part 2. WHO Regional Office for Europe, Copenhagen. 2007. Available online: http://www.euro.who.int/__data/assets/pdf_file/0018/103824/E89384.pdf (accessed on 15 October 2022).
- Fuhrman, S.; Kalyanpur, A.; Friedman, S.; Tran, N.T. Gendered implications of the COVID-19 pandemic for policies and programmes in humanitarian settings. BMJ Glob. Health 2020, 5, e002624. [Google Scholar] [CrossRef] [PubMed]
- Moyser, M. Gender Differences in Mental Health during the COVID-19 Pandemic. StatCan COVID-19: Data to Insights for a Better Canada. Stat. Can. 2020. Available online: https://www150.statcan.gc.ca/n1/en/pub/45-28-0001/2020001/article/00047-eng.pdf?st=3R0pqnzH (accessed on 15 October 2022).
- Kozloff, N.; Mulsant, B.H.; Stergiopoulos, V.; Voineskos, A.N. The COVID-19 global pandemic: Implications for people with schizophrenia and related disorders. Schizophr. Bull. 2020, 46, 752–757. [Google Scholar] [CrossRef]
- Mental Health Research Canada. Mental Health during COVID-19 Outbreak: Poll #7, 1–12. 2021. Available online: https://static1.squarespace.com/static/5f31a311d93d0f2e28aaf04a/t/60eca8f005183b3b57a10652/1626122483072/FINAL+-+Abridged+-+MHRC+Mental+Health+During+COVID+Poll+7+Report.pdf (accessed on 15 October 2022).
- Statistics Canada. Impacts on Indigenous Peoples. 2020. Available online: https://www150.statcan.gc.ca/n1/pub/11-631-x/2020004/pdf/s7-eng.pdf (accessed on 15 October 2022).
- Vigo, D.; Patten, S.; Pajer, K.; Krausz, M.; Taylor, S.; Rush, B.; Raviola, G.; Saxena, S.; Thornicroft, G.; Yatham, L.N. Mental Health of communities during the COVID-19 Pandemic. Can. J. Psychiatry. Rev. Can. De Psychiatr. 2020, 65, 681–687. [Google Scholar] [CrossRef]
- Griffiths, D.; Sheehan, L.; van Vreden, C.; Petrie, D.; Grant, G.; Whiteford, P.; Sim, M.R.; Collie, A. The Impact of work loss on mental and physical health during the COVID-19 pandemic: Baseline findings from a prospective cohort study. J. Occup. Rehabil. 2021, 31, 455–462. [Google Scholar] [CrossRef]
- Moyser, M. The Mental Health of Population Groups Designated as Visible Minorities in Canada during the COVID-19 Pandemic. StatCan COVID-19: Data to Insights for a Better Canada. Stat. Can. 2020. Available online: https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00077-eng.pdf (accessed on 15 October 2022).
- Benjamen, J.; Girard, V.; Jamani, S.; Magwood, O.; Holland, T.; Sharfuddin, N.; Pottie, K. Access to refugee and migrant mental health care services during the first six months of the COVID-19 pandemic: A Canadian Refugee Clinician Survey. Int. J. Environ. Res. Public Health 2021, 18, 5266. [Google Scholar] [CrossRef]
- Dozois, D.J.A. Anxiety and depression in Canada during the COVID-19 pandemic: A national survey. Can. Psychol./Psychol. Can. 2020, 62, 139–142. [Google Scholar] [CrossRef]
- Ritch, E.L.; Brennan, C. Using world café and drama to explore older people’s experience of financial products and services. Int. J. Consum. Stud. 2010, 34, 405–441. [Google Scholar] [CrossRef]
- Emlet, C.A.; Moceri, J.T. The importance of social connectedness in building age-friendly communities. J. Aging Res. 2012, 1–9. [Google Scholar] [CrossRef]
- Hamilton Wright, E.; Woodhall-Melnik, J.; Hamilton-Wright, S.; Guilcher, S.J.; Wendaferew, A.; Schuler, A.; Matheson, F.I. Reflections on poverty, homelessness, and problem gambling: Discoveries from a world café. J. Gambl. Issues 2019, 42, 62–84. [Google Scholar]
- McIntosh, T.; Novik, N.; DeCorby, A.; Muhajarine, N.; Jeffery, B.; Kallio, N. Mental Health and COVID-19 in Saskatchewan Adults: Report from a World Café Event. Regina/Saskatoon: Saskatchewan Population Health and Evaluation Research Unit. 2021. Available online: https://spheru.ca/images/covid19-images/worldcafementalhealthcovidsk14072021v11.pdf (accessed on 20 October 2022).
- Torres González, C.; Galindo-Aldana, G.; García León, I.A.; Alfredo Padilla-López, L.; Alvarez Núñez, D.N.; Espinoza Gutiérrez, Y.I. COVID-19 voluntary social isolation and its effects in sociofamily and children’s behavior. Salud Ment. 2020, 43, 263–271. [Google Scholar] [CrossRef]
- Peterson, J. Sask. Anxiety, Depression Rates Higher during COVID-19: Researchers. 2020. Available online: https://www.cbc.ca/news/canada/saskatchewan/sask-COVID-mental-health-1.5848388 (accessed on 19 November 2021).
- Samji, H.; Dove, N.; Ames, M.; Barbic, S.; Sones, M.; Leadbeater, B. Impacts of the COVID-19 Pandemic on the Health and Well-Being of Young Adults in British Columbia. Br. Columbia Cent. Dis. Control. 2021. Available online: http://www.bccdc.ca/Health-Professionals-Site/Documents/COVID-Impacts/BCCDC_COVID-19_Young_Adult_Health_Well-being_Report.pdf (accessed on 15 October 2022).
- Benning, K. Saskatchewan Cannabis Businesses Seeing Increased Demand during Coronavirus Pandemic. 2020. Available online: https://globalnews.ca/news/6845123/saskatchewan-cannabis-businesses-demand-coronavirus/ (accessed on 20 November 2021).
- Wellness Together Canada. Mental Health and Substance Use Support. 2021. Available online: https://wellnesstogether.ca/en-CA (accessed on 21 November 2021).
- Xu, J.; Sun, R.; Li, Y.; Chen, X.; Yiu WY, V.; Zhou, N.; Liu, L. Subtypes of social withdrawal and mental health trajectories during COVID-19 pandemic. J. Res. Personal. 2022, 97, 104203. [Google Scholar] [CrossRef] [PubMed]
- Mental Health Research Canada. Mental Health during COVID-19 Outbreak: Poll 8. 2021. Available online: https://static1.squarespace.com/static/5f31a311d93d0f2e28aaf04a/t/6148f058802c3076621f5edc/1632170074064/Final+-+Poll+8+Public+Release.pdf (accessed on 15 October 2022).
- Pathways to Prosperity. Social and Cultural Integration of Immigrants in Canada. 2021. Available online: http://p2pcanada.ca/research/social-and-cultural-integration-of-immigrants-in-canada/ (accessed on 20 November 2021).
- Poros, M. Migrant Social Networks: Vehicles for Migration, Integration and Development. 2021. Available online: https://www.migrationpolicy.org/article/migrant-social-networks-vehicles-migration-integration-and-development (accessed on 20 November 2021).
- Ng, E.; Zhang, H. Access to mental health consultations by immigrants and refugees in Canada. Health Rep. 2021, 32, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Saunders, N.R.; Gill, P.J.; Holder, L.; Vigod, S.; Kurdyak, P.; Gandhi, S.; Guttmann, A. Use of the emergency department as a first point of contact for mental health care by immigrant youth in Canada: A population-based study. CMAJ 2018, 190, E1183–E1191. [Google Scholar] [CrossRef] [PubMed]
- Organisation for Economic Co-Operation and Development. What is the Impact of the COVID-19 Pandemic on Immigrants and Their Children? 2020. Available online: https://www.oecd.org/coronavirus/policy-responses/what-is-the-impact-of-the-COVID-19-pandemic-on-immigrants-and-their-children-e7cbb7de/ (accessed on 21 November 2021).
- Czeisler, M.É.; Lane, R.I.; Petrosky, E.; Wiley, J.F.; Christensen, A.; Njai, R.; Rajaratnam, S.M.W. Mental health, substance use, and suicidal ideation during the COVID-19 Pandemic—United States, 24–30 June 2020. Morb. Mortal. Wkly. Rep. 2022, 69, 1049–1057. [Google Scholar] [CrossRef] [PubMed]
- González-Sanguino, C.; Ausín, B.; Castellanos, M.Á.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020, 87, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Vahia, I.V.; Jeste, D.V.; Reynolds, C.F. Older adults and the mental health effects of COVID-19. JAMA 2020, 324, 2253–2254. [Google Scholar] [CrossRef]
- Dunlop, D.D.; Song, J.; Lyons, J.S.; Manheim, L.M.; Chang, R.W. Racial/ethnic differences in rates of depression among preretirement adults. Am. J. Public Health 2003, 93, 1945–1952. [Google Scholar] [CrossRef]
- Nelson, S.E.; Wilson, K. The mental health of Indigenous peoples in Canada: A critical review of research. Soc. Sci. Med. 2017, 176, 93–112. [Google Scholar] [CrossRef]
- Asher, M.; Asnaani, A.; Aderka, I.M. Gender differences in social anxiety disorder: A review. Clin. Psychol. Rev. 2017, 56, 1–12. [Google Scholar] [CrossRef] [PubMed]
- McLean, C.P.; Asnaani, A.; Litz, B.T.; Hofmann, S.G. Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. J. Psychiatr. Res. 2011, 45, 1027–1035. [Google Scholar] [CrossRef] [PubMed]
| Variables | Weighted Frequency 1 (%) | ||
|---|---|---|---|
| Study Cycle 2, August 2020 (N = 576) | Study Cycle 5, February 2021 (N = 577) | Study Cycle 7, June 2021 (N = 590) | |
| Current age (years) | |||
| 16 to 29 | 103 (17.9) | 104 (18.0) | 118 (20.0) |
| 30 to 49 | 202 (35.1) | 212 (36.8) | 217 (36.8) |
| 50 and above | 271 (47.0) | 261 (45.3) | 255 (43.2) |
| Gender | |||
| Women | 292 (50.8) | 293 (50.8) | 299 (50.7) |
| Men | 281 (48.8) | 277 (48.0) | 288 (48.8) |
| Not disclosed | 2 (0.4) | 7 (1.3) | 3 (0.5) |
| Location of residence | |||
| Mid-size city/town | 80 (13.9) | 90 (15.6) | 77 (13.0) |
| Rural | 144 (25.0) | 145 (25.1) | 174 (29.5) |
| Regina | 189 (32.9) | 167 (28.9) | 175 (29.7) |
| Saskatoon | 162 (28.2) | 175 (30.4) | 164 (27.7) |
| Household composition | |||
| Live alone | 136 (23.6) | 121 (21.0) | 122 (20.7) |
| Live with others | 440 (76.4) | 456 (79.0) | 468 (79.3) |
| Parental status | |||
| Not a parent | 354 (61.4) | 357 (61.8) | 346 (58.7) |
| Has children ≤ 17 years | 133 (23.1) | 134 (23.3) | 143 (24.3) |
| Has children ≥ 18 years | 71 (12.3) | 72 (12.5) | 88 (14.9) |
| Has children in both age groups | 18 (3.2) | 14 (2.4) | 12 (2.1) |
| Employment status | |||
| Unemployed | 65 (11.3) | 62 (10.7) | 51 (8.6) |
| Retired/Student | 153 (26.5) | 165 (28.7) | 171 (29.0) |
| Employed | 341 (59.2) | 347 (60.1) | 358 (60.8) |
| Not disclosed | 17 (2.9) | 3 (0.5) | 9 (1.6) |
| Highest level of education | |||
| Elementary/high | 169 (29.3) | 166 (28.8) | 182 (30.9) |
| College/technical | 187 (32.5) | 179 (31.1) | 171 (28.9) |
| University | 209 (36.3) | 225 (38.9) | 227 (38.6) |
| Not disclosed | 11 (1.9) | 7 (1.1) | 10 (1.6) |
| Income | |||
| <$20K | 38 (6.6) | 40 (6.9) | 22 (3.7) |
| $20K to $49K | 121 (21.0) | 142 (24.6) | 116 (19.6) |
| $50K to $99K | 225 (39.0) | 190 (32.9) | 250 (42.4) |
| ≥$100K | 135 (23.4) | 160 (27.8) | 155 (26.3) |
| Not disclosed | 58 (10.0) | 45 (7.8) | 47 (8.0) |
| Immigration status | |||
| Born outside Canada 2 | 145 (25.1) | 137 (23.7) | 136 (23.0) |
| Born in Canada 3 | 419 (72.8) | 417 (72.3) | 443 (75.1) |
| Not disclosed | 12 (2.1) | 23 (4.0) | |
| Ethnicity | |||
| Indigenous/Ethnocultural minority 4 (African, Asian, Hispanic/Latino/Others) | Not available | 65 (11.3) | 101 (17.2) |
| White | 512 (88.7) | 489 (82.8) | |
| Physical disability | |||
| Yes | Not available | 33 (5.7) | 37 (6.3) |
| No | 544 (94.3) | 553 (93.7) | |
| Moderate Anxiety | Severe Anxiety | |||
|---|---|---|---|---|
| RRR 1 (95% CI) | p-value | RRR 1 (95% CI) | p-value | |
| Age (years) | ||||
| 16–29 | 1.47 (0.60–3.57) | 0.388 | 1.97 (0.69–5.61) | 0.200 |
| 30–49 | 2.67 (1.41–5.05) | 0.002 | 3.47 (1.62–7.44) | 0.001 |
| 50 and above | Reference | reference | ||
| Gender | ||||
| Women | 1.73 (1.01–2.94) | 0.043 | 2.31 (1.21–4.39) | 0.010 |
| Men | Reference | reference | ||
| Income | ||||
| <$20K | 0.40 (0.11–1.46) | 0.168 | 2.44 (0.78–7.63) | 0.122 |
| $20K to $49K | 1.73 (0.83–3.62) | 0.142 | 3.81 (1.52–9.50) | 0.004 |
| $50K to $99K | 1.26 (0.68–2.35) | 0.451 | 1.24 (0.53–2.85) | 0.611 |
| ≥$100K | Reference | reference | ||
| Educational status | ||||
| Elementary/high | 0.47 (0.24–0.93) | 0.032 | 1.01 (0.45–2.25) | 0.977 |
| College/technical | 1.10 (0.61–1.99) | 0.729 | 1.83 (0.85–3.93) | 0.116 |
| University | Reference | reference | ||
| Income × immigration status | ||||
| <$20K × born outside Canada | 29.24 (1.42–601.41) | 0.029 | 2.34 (0.09–56.48) | 0.600 |
| $20K to $49K × born outside Canada | 3.17 (0.55–18.03) | 0.192 | 0.73 (0.10–5.04) | 0.753 |
| $50K to $99K × born outside Canada | 1.78 (0.37–8.45) | 0.467 | 0.97 (0.18–5.16) | 0.979 |
| ≥$100K × born in Canada | Reference | reference | ||
| Education × immigration status | ||||
| Elementary/high × born outside Canada | 2.06 (0.47–9.04) | 0.337 | 1.36 (0.29–6.21) | 0.687 |
| College/technical × born outside Canada | 0.78 (0.22–2.81) | 0.712 | 0.19 (0.03–0.95) | 0.044 |
| University x born in Canada | Reference | reference | ||
| Moderate Depression | Severe Depression | |||
|---|---|---|---|---|
| RRR 1 (95% CI) | p-value | RRR 1 (95% CI) | p-value | |
| Age (years) | ||||
| 16–29 | 3.69 (1.48–9.20) | 0.005 | 4.38 (1.31–14.66) | 0.016 |
| 30–49 | 3.79 (1.78–8.09) | 0.001 | 6.79 (2.72–16.89) | <0.001 |
| 50 and above | Reference | reference | ||
| Employment status | ||||
| Unemployed | 0.76 (0.34–1.70) | 0.516 | 1.07 (0.46–2.50) | 0.860 |
| Retired/Student | 0.67 (0.34–1.31) | 0.247 | 0.38 (0.15–0.96) | 0.041 |
| Employed | Reference | reference | ||
| Income | ||||
| <$20K | 1.51 (0.40–5.60) | 0.538 | 7.09 (1.75–28.72) | 0.006 |
| $20K to $49K | 3.20 (1.47–6.97) | 0.003 | 9.82 (3.24–29.71) | <0.001 |
| $50K to $99K | 1.68 (0.87–3.24) | 0.121 | 3.31 (1.28–8.54) | 0.013 |
| ≥$100K | Reference | reference | ||
| Education × immigration status | ||||
| Elementary/high × born outside Canada | 8.38 (1.60–43.91) | 0.012 | 4.04 (0.63–25.72) | 0.138 |
| College/technical × born outside Canada | 0.69 (0.15–3.16) | 0.637 | 0.78 (0.12–4.86) | 0.795 |
| University × born in Canada | Reference | reference | ||
| Age × ethnocultural | ||||
| 16–29 × indigenous/ethnocultural minority | 0.23 (0.00–7.63) | 0.414 | 0.00 (0.00–0.38) | 0.015 |
| 30–49 × indigenous/ethnocultural minority | 1.88 (0.25–13.65) | 0.532 | 0.35 (0.06–1.98) | 0.238 |
| 50 and above × White | Reference | reference | ||
| Needed Support and Received | Needed but No Access | |||
|---|---|---|---|---|
| RRR 1 (95% CI) | p-value | RRR1 (95% CI) | p-value | |
| Age (years) | ||||
| 16–29 | 6.02 (2.40–15.13) | <0.001 | 2.07 (0.80–5.32) | 0.129 |
| 30–49 | 4.21 (2.05–8.67) | <0.001 | 1.35 (0.61–2.99) | 0.499 |
| 50 and above | Reference | reference | ||
| Household composition | ||||
| Live alone | 2.25 (1.14–4.44) | 0.018 | 0.85 (0.34–2.12) | 0.741 |
| Live with others | Reference | reference | ||
| Income | ||||
| <$20K | 3.57 (1.22–10.43) | 0.020 | 1.05 (0.23–4.69) | 0.947 |
| $20K to $49K | 2.75 (1.19–6.34) | 0.018 | 2.48 (1.07–5.74) | 0.034 |
| $50K to $99K | 1.45 (0.71–2.96) | 0.304 | 1.15 (0.53–2.47) | 0.719 |
| ≥$100K | Reference | reference | ||
| Immigration status | ||||
| Born outside Canada | 0.61 (0.32–1.14) | 0.127 | 0.14 (0.05–0.43) | 0.001 |
| Born in Canada | Reference | reference | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muhajarine, N.; Adeyinka, D.A.; Pisolkar, V.; Ahmed, M.S.; Kallio, N.; Coomaran, V.; McIntosh, T.; Novik, N.; Jeffery, B. Equity Analysis of Repeated Cross-Sectional Survey Data on Mental Health Outcomes in Saskatchewan, Canada during COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 13808. https://doi.org/10.3390/ijerph192113808
Muhajarine N, Adeyinka DA, Pisolkar V, Ahmed MS, Kallio N, Coomaran V, McIntosh T, Novik N, Jeffery B. Equity Analysis of Repeated Cross-Sectional Survey Data on Mental Health Outcomes in Saskatchewan, Canada during COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2022; 19(21):13808. https://doi.org/10.3390/ijerph192113808
Chicago/Turabian StyleMuhajarine, Nazeem, Daniel A. Adeyinka, Vaidehi Pisolkar, Md Sabbir Ahmed, Natalie Kallio, Vithusha Coomaran, Tom McIntosh, Nuelle Novik, and Bonnie Jeffery. 2022. "Equity Analysis of Repeated Cross-Sectional Survey Data on Mental Health Outcomes in Saskatchewan, Canada during COVID-19 Pandemic" International Journal of Environmental Research and Public Health 19, no. 21: 13808. https://doi.org/10.3390/ijerph192113808
APA StyleMuhajarine, N., Adeyinka, D. A., Pisolkar, V., Ahmed, M. S., Kallio, N., Coomaran, V., McIntosh, T., Novik, N., & Jeffery, B. (2022). Equity Analysis of Repeated Cross-Sectional Survey Data on Mental Health Outcomes in Saskatchewan, Canada during COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 19(21), 13808. https://doi.org/10.3390/ijerph192113808








