Quality of Life and Stress Management in Healthcare Professionals of a Dental Care Setting at a Teaching Hospital in Rome: Results of a Randomized Controlled Clinical Trial
Abstract
1. Introduction
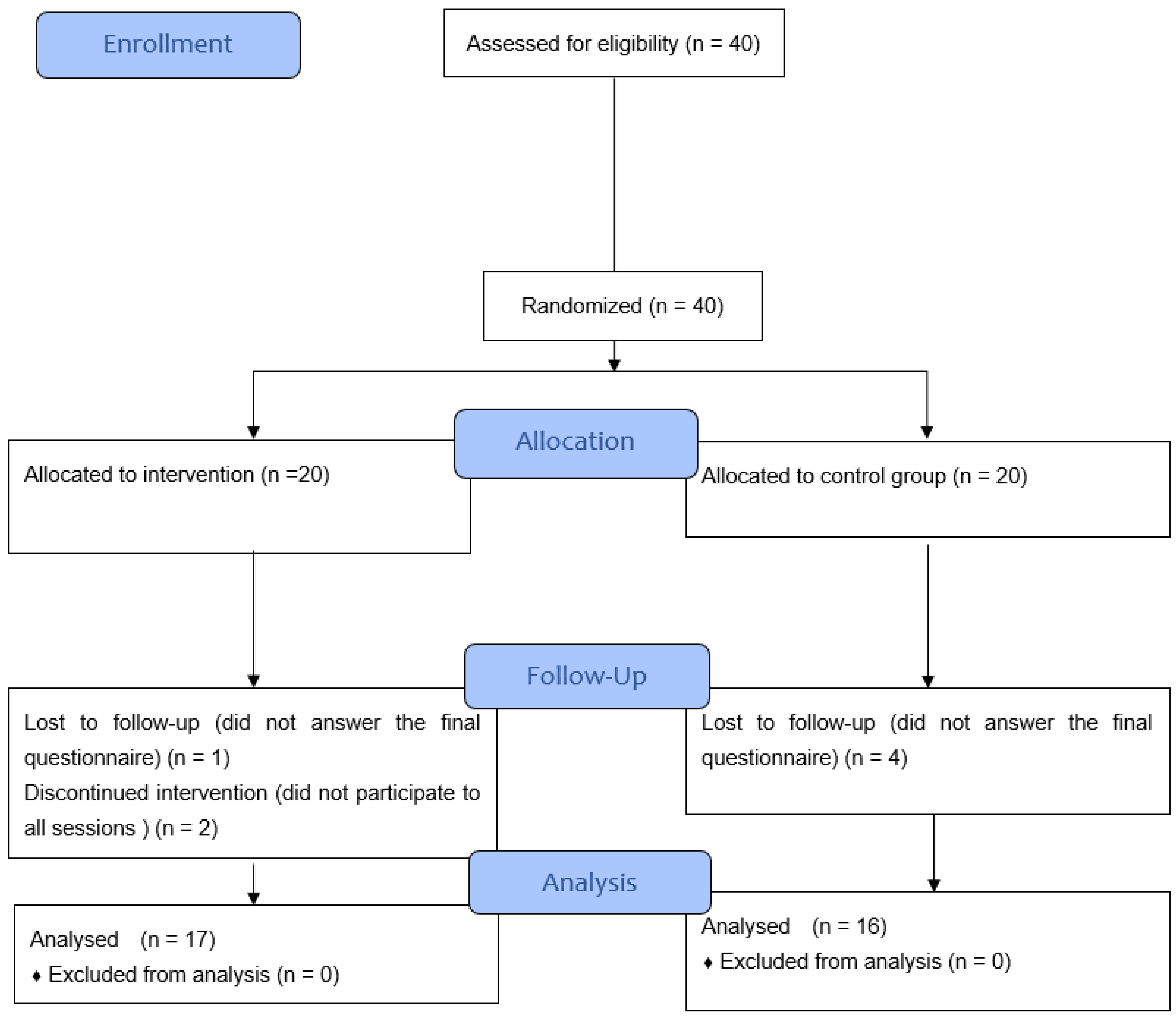
2. Materials and Methods
2.1. Setting
2.2. Sample Sizing
- Alpha level = 5%.
- Study Power = 80%.
- A 10% increase in MCS in the intervention group.
2.3. Inclusion and Exclusion Criteria
2.4. The Intervention
- Before the shift to encourage motivation and support for professionals involved in department activities to boost strength, determination, tolerance, good mood, efficiency, and balanced compassion.
- At the end of the shift, with the provision of another 15 min to allow quick decompression, facilitate relaxation, and its beneficial effect in favor of rebalancing, and releasing anxiety and stress caused by the emotional conditions in which they have been immersed during work to facilitate physiological rest and optimal conditions of the psychological/physical and emotional systems.
- (a)
- Brief verbal portion aimed at motivation.
- (b)
- Performance of various exercises, stretching and relaxation exercises of various parts of the body; muscular, visceral, and connective tissue. Work focused mainly on the shoulders, neck, chest, back, pelvis, and hamstrings (areas that are more likely to maintain tension).
- (c)
- Breathing techniques (Pranayama) performed simultaneously with physical exercises, slowing down and consciously channeling the breath to counteract a series of physiological components of stress while reducing feelings of anxiety.
- ○
- Increase in the length of exhalation compared to inhalation
- ○
- Fractional breathing
- ○
- Relaxed diaphragmatic breathing training. Main techniques carried out:
- Accelerated thoracic and diaphragmatic rhythmic breathing (Bhastrika),
- Alternating nostril breaths (Nadishodana),
- Fast breathing technique that involves the stomach and belly (Kapalabhati)
- (d)
- Specific meditations, movements, focalizations, and positions to free oneself from the tension that remains trapped in the body, help balancing emotions, recovering from fatigue, and reaching a state of mental neutrality.
- (e)
- Use of sound repeated to aid concentration and calm the restless mind (mantra).
- (f)
- Music mixed with the performance of exercises and meditations and for relaxation to inhibit thought production and facilitate inner calm and promote a physiological breathing rhythm.
- (g)
- Relaxation sessions.
2.5. The Questionnaires
- -
- The Italian version of SF12 for the assessment of quality of life, which allowed for the calculation of the mental composite score (MCS) and physical composite score (PCS) indicators [30].
- -
- Positivity scale for the assessment of positivity [31].
- -
- The Italian version of the 15-item Karasek questionnaire for the assessment of the two dimensions of work-related stress; job demand and decision latitude [32].
2.5.1. SF-12
2.5.2. Positivity Scale
2.5.3. Robert Karasek Questionnaire
2.6. Statistical Analyses
3. Results
- -
- SF-12: 0.837
- -
- Positivity: 0.891
- -
- Karasek: 0.815
4. Discussion
4.1. Limitations of Study
4.2. Strengths and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cocchiara, R.; Peruzzo, M.; Mannocci, A.; Ottolenghi, L.; Villari, P.; Polimeni, A.; Guerra, F.; La Torre, G. The Use of Yoga to Manage Stress and Burnout in Healthcare Workers: A Systematic Review. J. Clin. Med. 2019, 8, 284. [Google Scholar] [CrossRef] [PubMed]
- Li, A.W.; Goldsmith, C.A.W. The effects of yoga on anxiety and stress. Altern. Med. Rev. J. Clin. Ther. 2012, 17, 21–35. [Google Scholar]
- La Torre, G.; Raffone, A.; Peruzzo, M.; Calabrese, L.; Cocchiara, R.A.; D’Egidio, V.; Leggieri, P.F.; Dorelli, B.; Zaffina, S.; Mannocci, A.; et al. Yoga and Mindfulness as a Tool for Influencing Affectivity, Anxiety, Mental Health, and Stress among Healthcare Workers: Results of a Single-Arm Clinical Trial. J. Clin. Med. 2020, 9, 1037. [Google Scholar] [CrossRef]
- Kemper, K.; Bulla, S.; Krueger, D.; Ott, M.J.; McCool, J.A.; Gardiner, P. Nurses’ experiences, expectations, and preferences for mind-body practices to reduce stress. BMC Complement. Altern. Med. 2011, 11, 26. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Jackson, S.; Leiter, M. The Maslach Burnout Inventory Manual. In Evaluating Stress: A Book of Resources; Palo Alto Networks: Santa Clara, CA, USA, 1997; Volume 3, pp. 191–218. [Google Scholar]
- Humphris, G.; Blinkhorn, A.; Freeman, R.; Gorter, R.; Hoad-Reddick, G.; Murtomaa, H.; O’Sullivan, R.; Splieth, C. Psychological stress in undergraduate dental students: Baseline results from seven European dental schools. Eur. J. Dent. Educ. 2002, 6, 22–29. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Dyrbye, L.N.; Sloan, J.A.; Shanafelt, T.D. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J. Gen. Intern. Med. 2009, 24, 1318–1321. [Google Scholar] [CrossRef] [PubMed]
- Büssing, A.; Michalsen, A.; Khalsa, S.B.S.; Telles, S.; Sherman, K.J. Effects of yoga on mental and physical health: A short summary of reviews. Evid. Based Complement Altern. Med. ECAM 2012, 2012, 165410. [Google Scholar] [CrossRef]
- Riley, K.E.; Park, C.L.; Wilson, A.; Sabo, A.N.; Antoni, M.H.; Braun, T.D.; Harrington, J.; Reiss, J.; Pasalis, E.; Harris, A.D.; et al. Improving physical and mental health in frontline mental health care providers: Yoga-based stress management versus cognitive behavioral stress management. J. Workplace Behav. Health 2017, 32, 26–48. [Google Scholar] [CrossRef]
- Alexander, G.K.; Rollins, K.; Walker, D.; Wong, L.; Pennings, J. Yoga for Self-Care and Burnout Prevention Among Nurses. Workplace Health Saf. 2015, 63, 462–470. [Google Scholar] [CrossRef]
- Chismark, A.; Asher, G.; Stein, M.; Tavoc, T.; Curran, A. Use of complementary and alternative medicine for work-related pain correlates with career satisfaction among dental hygienists. J. Dent. Hyg. 2011, 85, 273–284. [Google Scholar]
- Koneru, S.; Tanikonda, R. Role of yoga and physical activity in work-related musculoskeletal disorders among dentists. J. Int. Soc. Prev. Community Dent. 2015, 5, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Alzahem, A.M.; van der Molen, H.T.; Alaujan, A.H.; Schmidt, H.G.; Zamakhshary, M.H. Stress amongst dental students: A systematic review. Eur. J. Dent. Educ. 2011, 15, 8–18. [Google Scholar] [CrossRef] [PubMed]
- Gorter, R.C.; Albrecht, G.; Hoogstraten, J.; Eijkman, M.A. Professional burnout among Dutch dentists. Community Dent. Oral Epidemiol. 1999, 27, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Kheiraoui, F.; Gualano, M.R.; Mannocci, A.; Boccia, A.; La Torre, G. Quality of life among healthcare workers: A multicentre cross-sectional study in Italy. Public Health 2012, 126, 624–629. [Google Scholar] [CrossRef]
- Shirey, M.R. An evidence-based solution for minimizing stress and anger in nursing students. J. Nurs. Educ. 2007, 46, 568–571. [Google Scholar] [CrossRef]
- Sulenes, K.; Freitas, J.; Justice, L.; Colgan, D.D.; Shean, M.; Brems, C. Underuse of yoga as a referral resource by health professions students. J. Altern. Complement. Med. NYN 2015, 21, 53–59. [Google Scholar] [CrossRef]
- Cordioli, D.F.C.; Cordioli, J.R.; Gazetta, C.E.; Silva, A.G.D.; Lourenção, L.G. Occupational stress and engagement in primary health care workers. Rev. Bras. Enferm. 2019, 72, 1580–1587. [Google Scholar] [CrossRef]
- Plessas, A.; Delgado, M.B.; Nasser, M.; Hanoch, Y.; Moles, D.R. Impact of stress on dentists’ clinical performance. A systematic review. Community Dent. Health 2018, 35, 9–15. [Google Scholar]
- Miyamoto, J.J.; Honda, M.; Saito, D.N.; Okada, T.; Ono, T.; Ohyama, K.; Sadato, N. The representation of the human oral area in the somatosensory cortex: A functional MRI study. Cereb. Cortex. 2006, 16, 669–675. [Google Scholar] [CrossRef]
- Chipchase, S.Y.; Chapman, H.R.; Bretherton, R. A study to explore if dentists’ anxiety affects their clinical decision-making. Br. Dent. J. 2017, 222, 277–290. [Google Scholar] [CrossRef]
- De Sio, S.; Traversini, V.; Rinaldo, F.; Colasanti, V.; Buomprisco, G.; Perri, R.; Mormone, F.; La Torre, G.; Guerra, F. Ergonomic risk and preventive measures of musculoskeletal disorders in the dentistry environment: An umbrella review. Peer J. 2018, 6, e4154. [Google Scholar] [CrossRef]
- Zhang, M.; Murphy, B.; Cabanilla, A.; Yidi, C. Physical relaxation for occupational stress in healthcare workers: A systematic review and network meta-analysis of randomized controlled trials. J. Occup. Health. 2021, 63, e12243. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.L.; Huang, C.Y.; Shiu, S.P.; Yeh, S.H. Effects of Yoga on Stress, Stress Adaption, and Heart Rate Variability Among Mental Health Professionals—A Randomized Controlled Trial. Worldviews Evid. Based Nurs. 2015, 12, 236–245. [Google Scholar] [CrossRef]
- Hartfiel, N.; Burton, C.; Rycroft-Malone, J.; Clarke, G.; Havenhand, J.; Khalsa, S.B.; Edwards, R.T. Yoga for reducing perceived stress and back pain at work. Occup. Med. Oxf. Engl. 2012, 62, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Jeter, P.E.; Slutsky, J.; Singh, N.; Khalsa, S.B.S. Yoga as a Therapeutic Intervention: A Bibliometric Analysis of Published Research Studies from 1967 to 2013. J. Altern. Complement. Med. NYN 2015, 21, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Ebnezar, J.; Nagarathna, R.; Yogitha, B.; Nagendra, H.R. Effect of integrated yoga therapy on pain, morning stiffness and anxiety in osteoarthritis of the knee joint: A randomized control study. Int. J. Yoga 2012, 5, 28–36. [Google Scholar] [CrossRef] [PubMed]
- García-Sesnich, J.N.; Flores, M.G.; Ríos, M.H.; Aravena, J.G. Longitudinal and Immediate Effect of Kundalini Yoga on Salivary Levels of Cortisol and Activity of Alpha-Amylase and Its Effect on Perceived Stress. Int. J. Yoga 2017, 10, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Fang, R.; Li, X. A regular yoga intervention for staff nurse sleep quality and work stress: A randomised controlled trial. J. Clin. Nurs. 2015, 24, 3374–3379. [Google Scholar] [CrossRef]
- Kodraliu, G.; Mosconi, P.; Groth, N.; Carmosino, G.; Perilli, A.; Gianicolo, E.A.; Rossi, C.; Apolone, G. Subjective health status assessment: Evaluation of the Italian version of the SF-12 Health Survey. Results from the MiOS Project. J. Epidemiol. Biostat. 2001, 6, 305–316. [Google Scholar] [CrossRef]
- Caprara, G.V.; Alessandri, G.; Eisenberg, N.; Kupfer, A.; Steca, P.; Caprara, M.G.; Yamaguchi, S.; Fukuzawa, A.; Abela, J. The Positivity Scale. Psychol. Assess. 2012, 24, 701–712. [Google Scholar] [CrossRef]
- Ferrario, M.; Cecchino, C.; Chiodini, P.; Ragno, G.; Merluzzi, F.; Borchini, R.; Taborelli, S.; Cesana, G. Affidabilità della scala di Karasek per la valutazione dello stress lavorativo percepito e differenze dei punteggi tra sessi. Lo studio SEMM [Reliability of the Karasek scale in the assessment of perceived occupational stress and gender-related differences in scores. The SEMM study]. G. Ital. Med. Lav. Ergon. 2003, 25 (Suppl. S3), 204–205. [Google Scholar]
- Ware, J.E.J.; Sherbourne, C.D. The MOS 36-ltem Short-Form Health Survey (SF-36): I. Conceptual Framework and Item Selection. Med. Care 1992, 30, 473–483. Available online: https://journals.lww.com/lww-medicalcare/Abstract/1992/06000/The_MOS_36_ltem_Short_Form_Health_Survey__SF_36__.2.asp (accessed on 22 April 2022). [CrossRef] [PubMed]
- Bischoff, L.L.; Otto, A.K.; Hold, C.; Wollesen, B. The effect of physical activity interventions on occupational stress for health personnel: A systematic review. Int. J. Nurs. Stud. 2019, 97, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Slabšinskienė, E.; Gorelik, A.; Kavaliauskienė, A.; Zaborskis, A. Burnout and Its Relationship with Demographic and Job-Related Variables among Dentists in Lithuania: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 3968. [Google Scholar] [CrossRef] [PubMed]
- Mijakoski, D.; Karadzinska-Bislimovska, J.; Basarovska, V.; Stoleski, S.; Minov, J. Burnout and Work Demands Predict Reduced Job Satisfaction in Health Professionals Working in a Surgery Clinic. Open Access Maced. J. Med. Sci. 2015, 3, 166–173. [Google Scholar] [CrossRef]
- Molina-Hernández, J.; Fernández-Estevan, L.; Montero, J.; González-García, L. Work environment, job satisfaction and burnout among Spanish dentists: A cross-sectional study. BMC Oral Health 2021, 21, 156. [Google Scholar] [CrossRef] [PubMed]
| Variables | Intervention Group N (%) or Mean (SD) | Control Group N (%) or Mean (SD) | p |
|---|---|---|---|
| Gender | 0.611 | ||
| Females | 7 (41.2) | 8 (50) | |
| Males | 10 (58.8) | 8 (50) | |
| Age | 36.8 (9.2) | 36.1 (8.7) | 0.830 |
| Civil status | 0.169 | ||
| Married/cohabitant | 7 (41.2) | 11 (68.8) | |
| Divorced | 2 (11.8) | 0 (0) | |
| Single | 8 (47.1) | 5 (31.3) | |
| Having children | 0.829 | ||
| No | 10 (58.8) | 10 (62.5) | |
| Yes | 7 (41.2) | 6 (37.5) | |
| Educational level | 0.909 | ||
| PhD or Specialization | 12 (70.6) | 11 (68.8) | |
| University Degree | 5 (29.4) | 5 (31.3) |
| Variables | Intervention Group Median (SD) | Control Group Median (SD) | p |
|---|---|---|---|
| MCS—pre | 45.9 (33.2–55.7) | 42.6 (25.1–54.7) | 0.367 |
| MCS—post | 52.8 (42.5–57.6) | 42.9 (29.2–56.6) | 0.006 |
| p | 0.002 | 0.733 | |
| PCS—pre | 54.7 (42.4–58.8) | 55.6 (44.8–62.6) | 0.262 |
| PCS—post | 55.0 (43.7- 59.2) | 56.7 (46.6–61.3) | 0.203 |
| p | 0.653 | 0.397 | |
| Positivity—pre | 3.5 (3.0–4.5) | 3.7 (2.7–4.7) | 0.591 |
| Positivity—post | 3.4 (2.7–4.9) | 3.5 (2.7–5.0) | 0.986 |
| p | 0.373 | 0.627 | |
| Job demand—pre | 28.0 (20.0–37.0) | 29 (24–35) | 0.414 |
| Job demand—post | 28 (22–37) | 29 (21–37) | 0.790 |
| p | 0.231 | 0.555 | |
| Decision latitude—pre | 40.0 (38.0–48.0) | 40.0 (32.0–44.0) | 0.166 |
| Decision latitude—post | 42.0 (36.0–46.0) | 40.0 (36.0–46.0) | 0.260 |
| p | 0.340 | 0.135 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guerra, F.; Corridore, D.; Peruzzo, M.; Dorelli, B.; Raimondi, L.; Ndokaj, A.; Mazur, M.; Ottolenghi, L.; Torre, G.L.; Polimeni, A. Quality of Life and Stress Management in Healthcare Professionals of a Dental Care Setting at a Teaching Hospital in Rome: Results of a Randomized Controlled Clinical Trial. Int. J. Environ. Res. Public Health 2022, 19, 13788. https://doi.org/10.3390/ijerph192113788
Guerra F, Corridore D, Peruzzo M, Dorelli B, Raimondi L, Ndokaj A, Mazur M, Ottolenghi L, Torre GL, Polimeni A. Quality of Life and Stress Management in Healthcare Professionals of a Dental Care Setting at a Teaching Hospital in Rome: Results of a Randomized Controlled Clinical Trial. International Journal of Environmental Research and Public Health. 2022; 19(21):13788. https://doi.org/10.3390/ijerph192113788
Chicago/Turabian StyleGuerra, Fabrizio, Denise Corridore, Margherita Peruzzo, Barbara Dorelli, Lucrezia Raimondi, Artnora Ndokaj, Marta Mazur, Livia Ottolenghi, Giuseppe La Torre, and Antonella Polimeni. 2022. "Quality of Life and Stress Management in Healthcare Professionals of a Dental Care Setting at a Teaching Hospital in Rome: Results of a Randomized Controlled Clinical Trial" International Journal of Environmental Research and Public Health 19, no. 21: 13788. https://doi.org/10.3390/ijerph192113788
APA StyleGuerra, F., Corridore, D., Peruzzo, M., Dorelli, B., Raimondi, L., Ndokaj, A., Mazur, M., Ottolenghi, L., Torre, G. L., & Polimeni, A. (2022). Quality of Life and Stress Management in Healthcare Professionals of a Dental Care Setting at a Teaching Hospital in Rome: Results of a Randomized Controlled Clinical Trial. International Journal of Environmental Research and Public Health, 19(21), 13788. https://doi.org/10.3390/ijerph192113788











