Development of the Children and Adolescents Physical Activity and Sedentary Questionnaire (CAPAS-Q): Psychometric Validity and Clinical Interpretation
Abstract
1. Introduction
2. Methods
2.1. Development of the Children and Adolescents Physical Activity and Sedentary Questionnaire (CAPAS-Q)
2.2. Description of the Children and Adolescents Physical Activity and Sedentary Questionnaire (CAPAS-Q)
2.3. Data Collection and Validation process
2.3.1. Participants and Methods
2.3.2. Anthropometric Measurements
2.3.3. Accelerometry Physical Activity and Sedentary Times
2.4. Statistical Analysis
3. Results
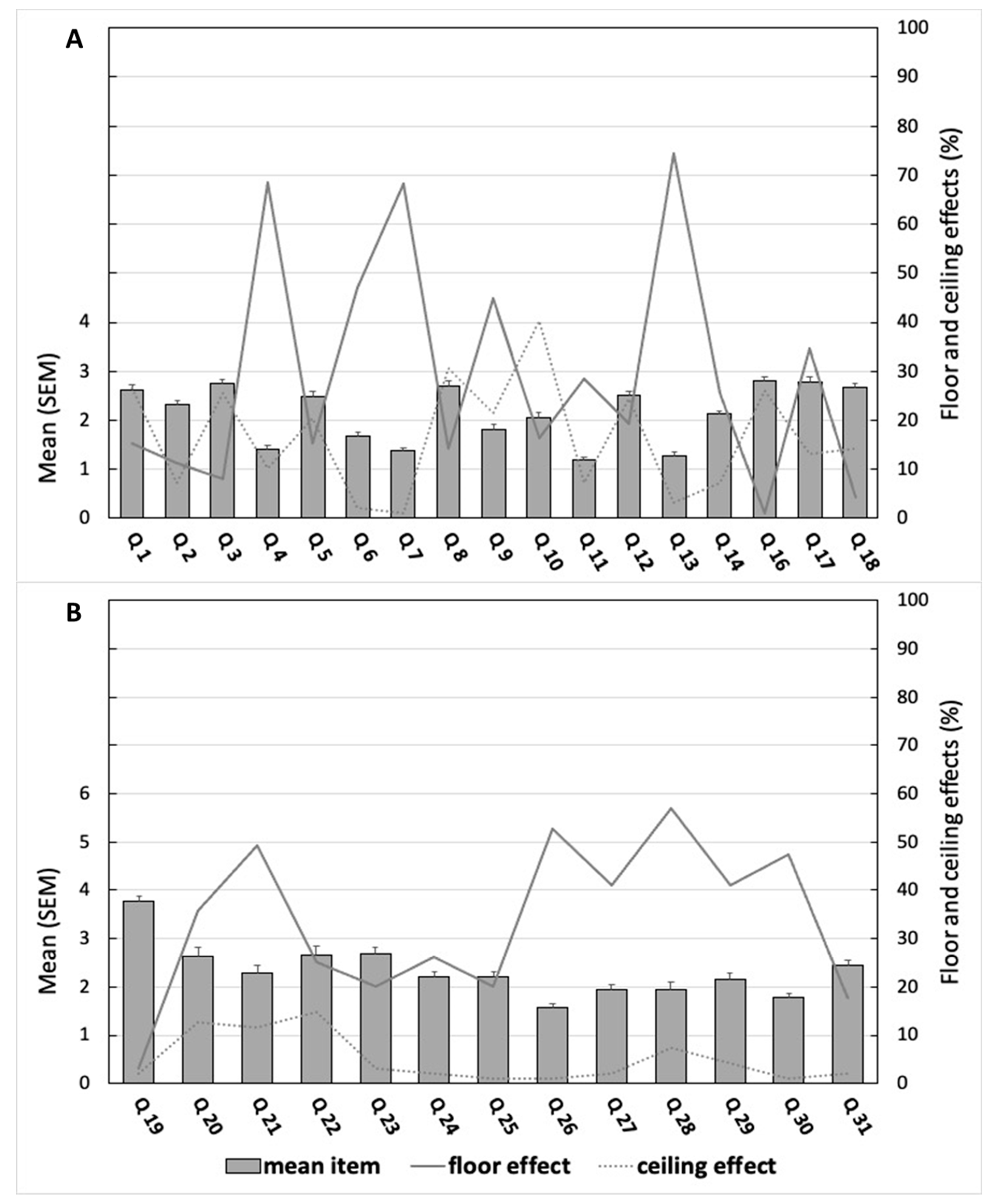
3.1. Internal Consistency
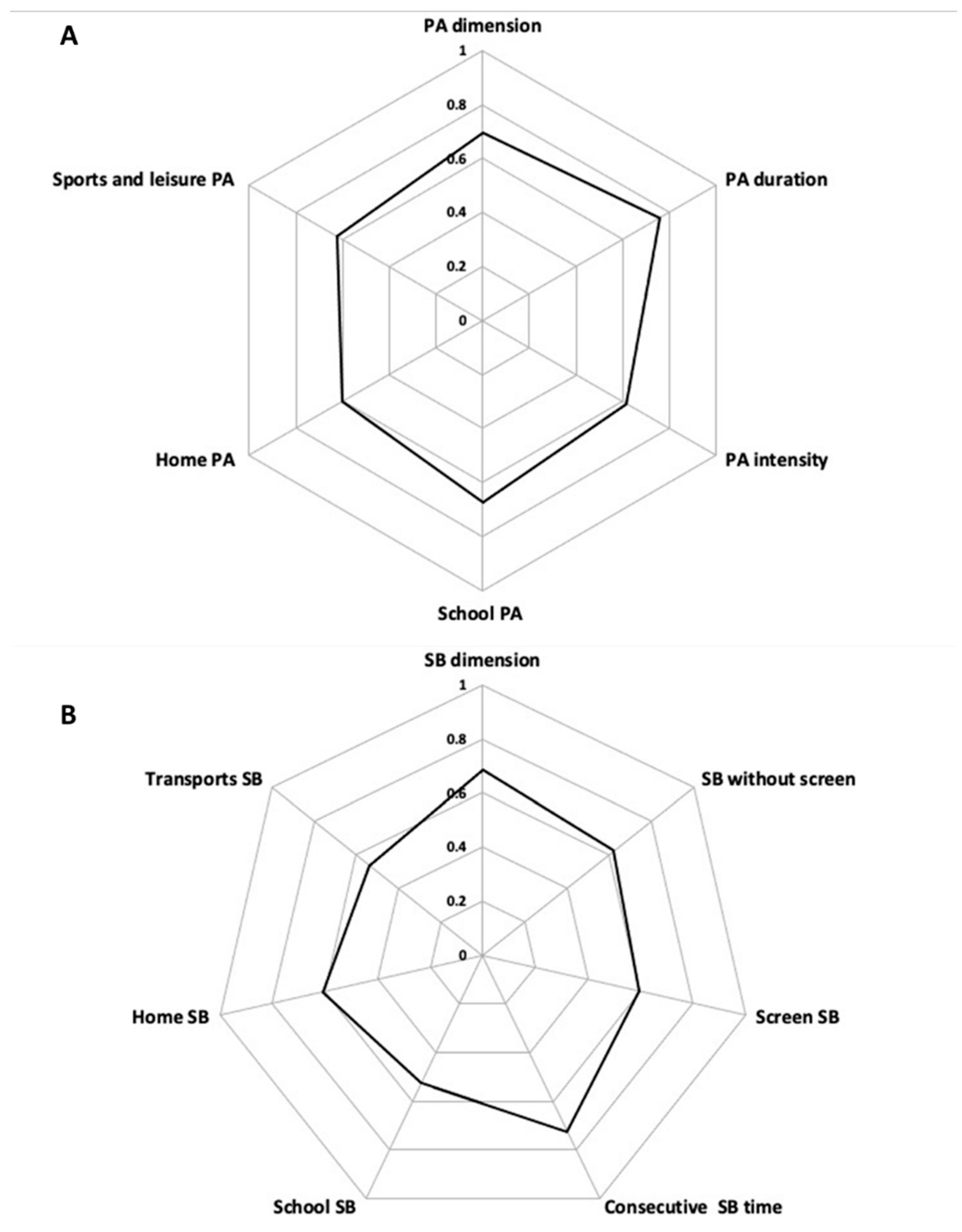
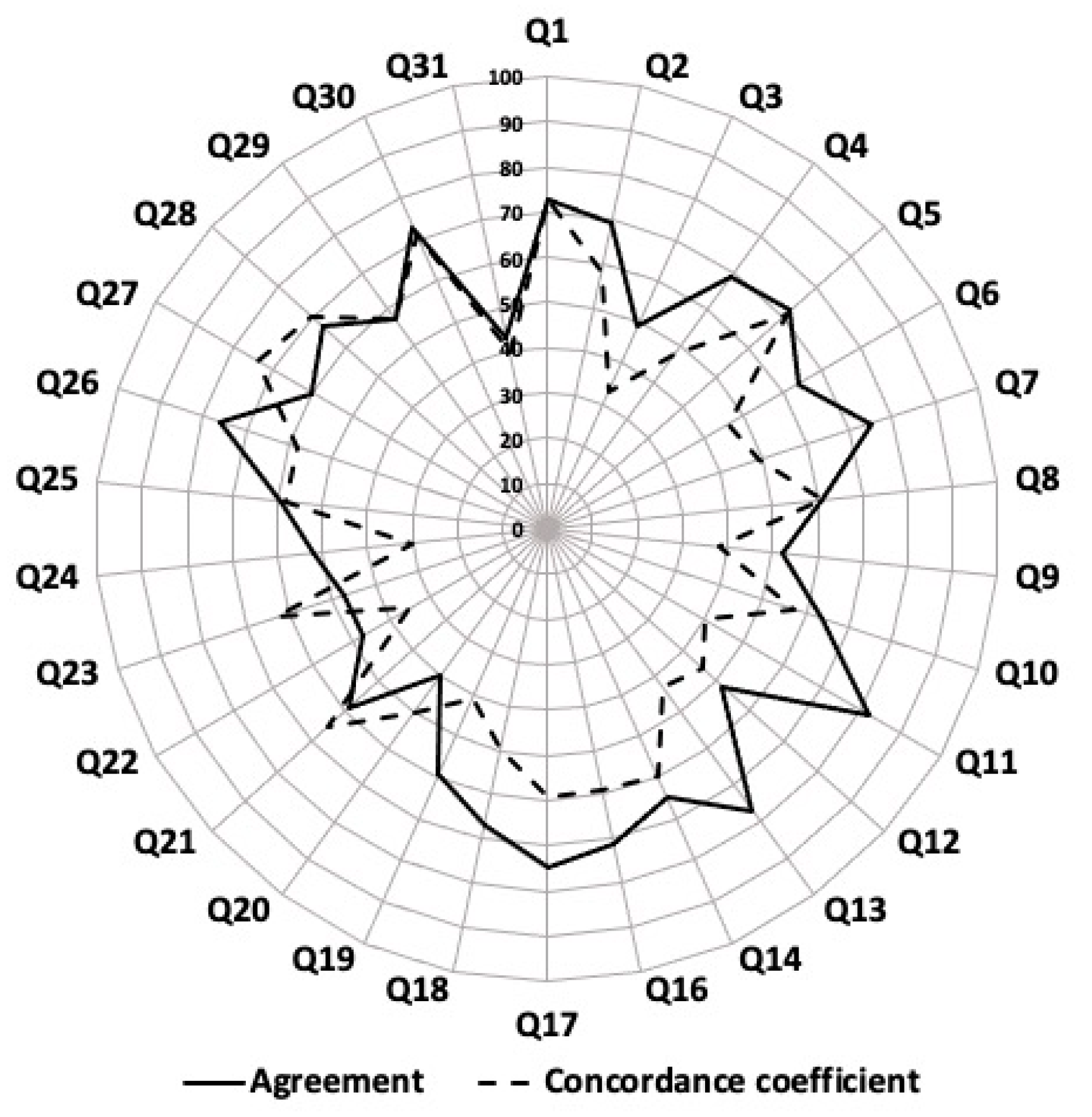
3.2. Test-Retest Repeatability
3.3. Concurrent Validity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Poitras, V.J.; Gray, C.E.; Borghese, M.M.; Carson, V.; Chaput, J.-P.; Janssen, I.; Katzmarzyk, P.T.; Pate, R.R.; Connor Gorber, S.; Kho, M.E.; et al. Systematic Review of the Relationships between Objectively Measured Physical Activity and Health Indicators in School-Aged Children and Youth. Appl. Physiol. Nutr. Metab. 2016, 41, S197–S239. [Google Scholar] [CrossRef]
- Cesa, C.C.; Sbruzzi, G.; Ribeiro, R.A.; Barbiero, S.M.; de Oliveira Petkowicz, R.; Eibel, B.; Machado, N.B.; Marques, R.D.V.; Tortato, G.; dos Santos, T.J.; et al. Physical Activity and Cardiovascular Risk Factors in Children: Meta-Analysis of Randomized Clinical Trials. Prev. Med. 2014, 69, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Marker, A.M.; Steele, R.G.; Noser, A.E. Physical Activity and Health-Related Quality of Life in Children and Adolescents: A Systematic Review and Meta-Analysis. Health Psychol. 2018, 37, 893–903. [Google Scholar] [CrossRef]
- Andermo, S.; Hallgren, M.; Nguyen, T.-T.-D.; Jonsson, S.; Petersen, S.; Friberg, M.; Romqvist, A.; Stubbs, B.; Elinder, L.S. School-Related Physical Activity Interventions and Mental Health among Children: A Systematic Review and Meta-Analysis. Sports Med. Open 2020, 6, 25. [Google Scholar] [CrossRef] [PubMed]
- Sember, V.; Jurak, G.; Kovač, M.; Morrison, S.A.; Starc, G. Children’s Physical Activity, Academic Performance, and Cognitive Functioning: A Systematic Review and Meta-Analysis. Front. Public Health 2020, 8, 307. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; LeBlanc, A.G.; Kho, M.E.; Saunders, T.J.; Larouche, R.; Colley, R.C.; Goldfield, G.; Connor Gorber, S. Systematic Review of Sedentary Behaviour and Health Indicators in School-Aged Children and Youth. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 98. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Tarp, J.; Steene-Johannessen, J.; Hansen, B.H.; Jefferis, B.; Fagerland, M.W.; Whincup, P.; Diaz, K.M.; Hooker, S.P.; Chernofsky, A.; et al. Dose-Response Associations between Accelerometry Measured Physical Activity and Sedentary Time and All Cause Mortality: Systematic Review and Harmonised Meta-Analysis. BMJ 2019, 366, l4570. [Google Scholar] [CrossRef]
- Carson, V.; Tremblay, M.S.; Chaput, J.-P.; Chastin, S.F.M. Associations between Sleep Duration, Sedentary Time, Physical Activity, and Health Indicators among Canadian Children and Youth Using Compositional Analyses. Appl. Physiol. Nutr. Metab. 2016, 41, S294–S302. [Google Scholar] [CrossRef]
- Carson, V.; Hunter, S.; Kuzik, N.; Gray, C.E.; Poitras, V.J.; Chaput, J.-P.; Saunders, T.J.; Katzmarzyk, P.T.; Okely, A.D.; Connor Gorber, S.; et al. Systematic Review of Sedentary Behaviour and Health Indicators in School-Aged Children and Youth: An Update. Appl. Physiol. Nutr. Metab. 2016, 41, S240–S265. [Google Scholar] [CrossRef]
- Chaput, J.-P.; Lambert, M.; Mathieu, M.-E.; Tremblay, M.S.; Loughlin, J.O.; Tremblay, A. Physical Activity vs. Sedentary Time: Independent Associations with Adiposity in Children. Pediatric. Obes. 2012, 7, 251–258. [Google Scholar] [CrossRef]
- Renninger, M.; Hansen, B.H.; Steene-Johannessen, J.; Kriemler, S.; Froberg, K.; Northstone, K.; Sardinha, L.; Anderssen, S.A.; Andersen, L.B.; Ekelund, U.; et al. Associations between Accelerometry Measured Physical Activity and Sedentary Time and the Metabolic Syndrome: A Meta-Analysis of More than 6000 Children and Adolescents. Pediatr. Obes. 2020, 15, e12578. [Google Scholar] [CrossRef]
- Katzmarzyk, P.T.; Barreira, T.V.; Broyles, S.T.; Champagne, C.M.; Chaput, J.-P.; Fogelholm, M.; Hu, G.; Johnson, W.D.; Kuriyan, R.; Kurpad, A.; et al. Physical Activity, Sedentary Time, and Obesity in an International Sample of Children. Med. Sci. Sports Exerc. 2015, 47, 2062–2069. [Google Scholar] [CrossRef] [PubMed]
- Julian, V.; Bergsten, P.; Forslund, A.; Ahlström, H.; Ciba, I.; Dahlbom, M.; Furthner, D.; Gomahr, J.; Kullberg, J.; Maruszczak, K.; et al. Sedentary Time Has a Stronger Impact on Metabolic Health than Moderate to Vigorous Physical Activity in Adolescents with Obesity: A Cross-Sectional Analysis of the Beta-JUDO Study. Pediatr. Obes. 2022, 2022, e12897. [Google Scholar] [CrossRef] [PubMed]
- Jakubec, L.; Gába, A.; Dygrýn, J.; Rubín, L.; Šimůnek, A.; Sigmund, E. Is Adherence to the 24-Hour Movement Guidelines Associated with a Reduced Risk of Adiposity among Children and Adolescents? BMC Public Health 2020, 20, 1119. [Google Scholar] [CrossRef] [PubMed]
- Mann, K.D.; Howe, L.D.; Basterfield, L.; Parkinson, K.N.; Pearce, M.S.; Reilly, J.K.; Adamson, A.J.; Reilly, J.J.; Janssen, X. Longitudinal Study of the Associations between Change in Sedentary Behavior and Change in Adiposity during Childhood and Adolescence: Gateshead Millennium Study. Int. J. Obes. 2017, 41, 1042–1047. [Google Scholar] [CrossRef] [PubMed]
- Schwarzfischer, P.; Gruszfeld, D.; Socha, P.; Luque, V.; Closa-Monasterolo, R.; Rousseaux, D.; Moretti, M.; Mariani, B.; Verduci, E.; Koletzko, B.; et al. Longitudinal Analysis of Physical Activity, Sedentary Behaviour and Anthropometric Measures from Ages 6 to 11 Years. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 126. [Google Scholar] [CrossRef]
- Saunders, T.J.; Gray, C.E.; Poitras, V.J.; Chaput, J.-P.; Janssen, I.; Katzmarzyk, P.T.; Olds, T.; Connor Gorber, S.; Kho, M.E.; Sampson, M.; et al. Combinations of Physical Activity, Sedentary Behaviour and Sleep: Relationships with Health Indicators in School-Aged Children and Youth. Appl. Physiol. Nutr. Metab. 2016, 41, S283–S293. [Google Scholar] [CrossRef]
- Sampasa-Kanyinga, H.; Standage, M.; Tremblay, M.S.; Katzmarzyk, P.T.; Hu, G.; Kuriyan, R.; Maher, C.; Maia, J.; Olds, T.; Sarmiento, O.L.; et al. Associations between Meeting Combinations of 24-h Movement Guidelines and Health-Related Quality of Life in Children from 12 Countries. Public Health 2017, 153, 16–24. [Google Scholar] [CrossRef]
- Lien, A.; Sampasa-Kanyinga, H.; Colman, I.; Hamilton, H.A.; Chaput, J.-P. Adherence to 24-Hour Movement Guidelines and Academic Performance in Adolescents. Public Health 2020, 183, 8–14. [Google Scholar] [CrossRef]
- Chaput, J.-P.; Willumsen, J.; Bull, F.; Chou, R.; Ekelund, U.; Firth, J.; Jago, R.; Ortega, F.B.; Katzmarzyk, P.T. 2020 WHO Guidelines on Physical Activity and Sedentary Behaviour for Children and Adolescents Aged 5-17 Years: Summary of the Evidence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 141. [Google Scholar] [CrossRef]
- Fillon, A.; Genin, P.; Larras, B.; Vanhelst, J.; Luiggi, M.; Aubert, S.; Verdot, C.; Rey, O.; Lhuisset, L.; Bois, J.; et al. France’s 2020 Report Card on Physical Activity and Sedentary Behaviors in Children and Youth: Results and Progression. J. Phys. Act. Health 2021, 18, 811–817. [Google Scholar] [CrossRef] [PubMed]
- Lobelo, F.; Rohm Young, D.; Sallis, R.; Garber, M.D.; Billinger, S.A.; Duperly, J.; Hutber, A.; Pate, R.R.; Thomas, R.J.; Widlansky, M.E.; et al. Routine Assessment and Promotion of Physical Activity in Healthcare Settings: A Scientific Statement From the American Heart Association. Circulation 2018, 137, e495–e522. [Google Scholar] [CrossRef] [PubMed]
- Warren, J.M.; Ekelund, U.; Besson, H.; Mezzani, A.; Geladas, N.; Vanhees, L. Assessment of Physical Activity—A Review of Methodologies with Reference to Epidemiological Research: A Report of the Exercise Physiology Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur. J. Cardiovasc. Prev. Rehabil. 2010, 17, 127–139. [Google Scholar] [CrossRef] [PubMed]
- Lubans, D.R.; Hesketh, K.; Cliff, D.P.; Barnett, L.M.; Salmon, J.; Dollman, J.; Morgan, P.J.; Hills, A.P.; Hardy, L.L. A Systematic Review of the Validity and Reliability of Sedentary Behaviour Measures Used with Children and Adolescents. Obes. Rev. 2011, 12, 781–799. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.J.; Sallis, J.F.; Long, B. A Physical Activity Screening Measure for Use With Adolescents in Primary Care. Arch. Pediatr. Adolesc. Med. 2001, 155, 554. [Google Scholar] [CrossRef] [PubMed]
- Saint-Maurice, P.F.; Welk, G.J. Validity and Calibration of the Youth Activity Profile. PLoS ONE 2015, 10, e0143949. [Google Scholar] [CrossRef] [PubMed]
- Rääsk, T.; Mäestu, J.; Lätt, E.; Jürimäe, J.; Jürimäe, T.; Vainik, U.; Konstabel, K. Comparison of IPAQ-SF and Two Other Physical Activity Questionnaires with Accelerometer in Adolescent Boys. PLoS ONE 2017, 12, e0169527. [Google Scholar] [CrossRef]
- Camargo, D.M.; Santisteban, S.; Paredes, E.; Flórez, M.A.; Bueno, D. Reliability of a questionnaire for measuring physical activity and sedentary behavior in children from preschool to fourth grade. Biomedica 2015, 35, 347–356. [Google Scholar] [CrossRef]
- Hidding, L.M.; Altenburg, T.M.; Mokkink, L.B.; Terwee, C.B.; Chinapaw, M.J.M. Systematic Review of Childhood Sedentary Behavior Questionnaires: What Do We Know and What Is Next? Sports Med. 2017, 47, 677–699. [Google Scholar] [CrossRef] [PubMed]
- Bacquaert, P.; Bacquaert, M. Evaluer L’activité Physique. Available online: https://www.irbms.com/questionnaire-dauto-evaluation-du-niveau-de-sedentarite-revue-de-litterature/ (accessed on 4 July 2022).
- Chinapaw, M.J.M.; Mokkink, L.B.; van Poppel, M.N.M.; van Mechelen, W.; Terwee, C.B. Physical Activity Questionnaires for Youth: A Systematic Review of Measurement Properties. Sports Med. 2010, 40, 539–563. [Google Scholar] [CrossRef]
- Schröder, H.; Subirana, I.; Wärnberg, J.; Medrano, M.; González-Gross, M.; Gusi, N.; Aznar, S.; Alcaraz, P.E.; González-Valeiro, M.A.; Serra-Majem, L.; et al. Validity, Reliability, and Calibration of the Physical Activity Unit 7 Item Screener (PAU-7S) at Population Scale. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 98. [Google Scholar] [CrossRef] [PubMed]
- Verney, J.; Metz, L.; Chaplais, E.; Cardenoux, C.; Pereira, B.; Thivel, D. Bioelectrical Impedance Is an Accurate Method to Assess Body Composition in Obese but Not Severely Obese Adolescents. Nutr. Res. 2016, 36, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Verney, J.; Schwartz, C.; Amiche, S.; Pereira, B.; Thivel, D. Comparisons of a Multi-Frequency Bioelectrical Impedance Analysis to the Dual-Energy X-Ray Absorptiometry Scan in Healthy Young Adults Depending on Their Physical Activity Level. J. Hum. Kinet. 2015, 47, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Mâsse, L.C.; Tilert, T.; McDowell, M. Physical Activity in the United States Measured by Accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Romanzini, M.; Petroski, E.L.; Ohara, D.; Dourado, A.C.; Reichert, F.F. Calibration of ActiGraph GT3X, Actical and RT3 Accelerometers in Adolescents. Eur. J. Sport Sci. 2014, 14, 91–99. [Google Scholar] [CrossRef]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C.W. The COSMIN Study Reached International Consensus on Taxonomy, Terminology, and Definitions of Measurement Properties for Health-Related Patient-Reported Outcomes. J. Clin. Epidemiol. 2010, 63, 737–745. [Google Scholar] [CrossRef]
- Terwee, C.B.; Bot, S.D.M.; de Boer, M.R.; van der Windt, D.A.W.M.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C.W. Quality Criteria Were Proposed for Measurement Properties of Health Status Questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef]
- Altman, D.G. Practical Statistics for Medical Research, 1st ed.; Chapman and Hall/CRC: Boca Raton, FL, USA, 1991. [Google Scholar]
- Berry, K.J.; Mielke, P.W. A Monte Carlo Investigation of the Fisher Z Transformation for Normal and Nonnormal Distributions. Psychol. Rep. 2000, 87, 1101–1114. [Google Scholar] [CrossRef] [PubMed]
- Diedenhofen, B.; Musch, J. Cocron: A Web Interface and R Package for the Statistical Comparison of Cronbach’s Alpha Coefficients. Int. J. Internet Sci. 2016, 11, 51–60. [Google Scholar]
- Helmerhorst, H.J.F.; Brage, S.; Warren, J.; Besson, H.; Ekelund, U. A Systematic Review of Reliability and Objective Criterion-Related Validity of Physical Activity Questionnaires. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 103. [Google Scholar] [CrossRef]
- Rangul, V.; Holmen, T.L.; Kurtze, N.; Cuypers, K.; Midthjell, K. Reliability and Validity of Two Frequently Used Self-Administered Physical Activity Questionnaires in Adolescents. BMC Med. Res. Methodol. 2008, 8, 47. [Google Scholar] [CrossRef] [PubMed]
- Charles, M.; Thivel, D.; Verney, J.; Isacco, L.; Husu, P.; Vähä-Ypyä, H.; Vasankari, T.; Tardieu, M.; Fillon, A.; Genin, P.; et al. Reliability and Validity of the ONAPS Physical Activity Questionnaire in Assessing Physical Activity and Sedentary Behavior in French Adults. Int. J. Environ. Res. Public Health 2021, 18, 5643. [Google Scholar] [CrossRef] [PubMed]


| Overall (n = 103) | Males (n = 52) | Females (n = 51) | (8–11) Years Old (n = 39) | (12–18) Years Old (n = 64) | |
|---|---|---|---|---|---|
| Anthropometry | |||||
| Age (year) | 12.2 ± 2.3 | 11.8 ± 1.9 | 12.5 ± 2.5 | 9.5 ± 1.1 | 13.4 ± 1.4 ### |
| Height (cm) | 155.5 ± 13.9 | 155.7 ± 14.6 | 155.2 ± 13.4 | 140.2 ± 9.5 | 161.4 ± 10.5 ### |
| Weight (kg) | 46.3 ± 10.5 | 46.1 ± 14.8 | 46.5 ± 12.2 | 32.6 ± 5.4 | 51.4 ± 12.0 ### |
| BMI (kg·m−2) | 18.7 ± 2.9 | 18.5 ± 3.1 | 18.9 ± 2.8 | 16.5 ± 1.8 | 19.6 ± 3.1 ### |
| Z-BMI (z-score) | −0.063 ± 0.94 | −0.129 ± 1.13 | 0.002 ± 0.73 | −0.10 ± 0.9 | −0.04 ± 0.9 |
| BMI (percentile) | 48.5 ± 27.7 | 47.2 ± 30.8 | 49.8 ± 24.5 | 46.5 ± 26.8 | 49.5 ± 28.2 |
| Fat-free mass (kg) | 34.7 ± 9.7 | 35.7 ± 11.4 | 33.5 ± 7.6 | 24.9 ± 8.2 | 37.5 ± 10.2 |
| Fat mass (%) | 20.5 ± 4.7 | 17.9 ± 4.9 | 23.16 ± 4.4 *** | 19.4 ± 3.2 | 21.6 ± 5.9 # |
| Accelerometry First Questionnaire | |||||
| Total PA (min/day) | 275 ± 56 | 298 ± 61 | 240 ± 51 *** | 346 ± 57 | 268 ± 57 ### |
| LPA (min/day) | 183 ± 37 | 196 ± 40 | 163 ± 33 | 227 ± 30 | 169 ± 40 ## |
| MPA (min/day) | 46.6 ± 14.5 | 50.0 ± 14 | 41.7 ± 13.6 | 60 ± 15 | 45 ± 13 ## |
| VPA (min/day) | 45 ± 21 | 51 ± 23 | 35 ± 19 ** | 59 ± 21 | 44 ± 23 |
| MVPA (min/day) | 92 ± 34 | 101 ± 34 | 76 ± 28 * | 119 ± 35 | 89 ± 33 # |
| Sedentary time (min/day) | 532 ± 96 | 519 ± 80 | 551 ± 115 | 472 ± 62 | 541 ± 103 # |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fillon, A.; Pereira, B.; Vanhelst, J.; Baran, J.; Masurier, J.; Guirado, T.; Boirie, Y.; Duclos, M.; Julian, V.; Thivel, D. Development of the Children and Adolescents Physical Activity and Sedentary Questionnaire (CAPAS-Q): Psychometric Validity and Clinical Interpretation. Int. J. Environ. Res. Public Health 2022, 19, 13782. https://doi.org/10.3390/ijerph192113782
Fillon A, Pereira B, Vanhelst J, Baran J, Masurier J, Guirado T, Boirie Y, Duclos M, Julian V, Thivel D. Development of the Children and Adolescents Physical Activity and Sedentary Questionnaire (CAPAS-Q): Psychometric Validity and Clinical Interpretation. International Journal of Environmental Research and Public Health. 2022; 19(21):13782. https://doi.org/10.3390/ijerph192113782
Chicago/Turabian StyleFillon, Alicia, Bruno Pereira, Jérémy Vanhelst, Joanna Baran, Julie Masurier, Terry Guirado, Yves Boirie, Martine Duclos, Valérie Julian, and David Thivel. 2022. "Development of the Children and Adolescents Physical Activity and Sedentary Questionnaire (CAPAS-Q): Psychometric Validity and Clinical Interpretation" International Journal of Environmental Research and Public Health 19, no. 21: 13782. https://doi.org/10.3390/ijerph192113782
APA StyleFillon, A., Pereira, B., Vanhelst, J., Baran, J., Masurier, J., Guirado, T., Boirie, Y., Duclos, M., Julian, V., & Thivel, D. (2022). Development of the Children and Adolescents Physical Activity and Sedentary Questionnaire (CAPAS-Q): Psychometric Validity and Clinical Interpretation. International Journal of Environmental Research and Public Health, 19(21), 13782. https://doi.org/10.3390/ijerph192113782








