Abstract
The Feldenkrais Method (FM) is based on the learning of alternative movement patterns, carried out in an active and conscious way, which may have therapeutic effects. The objective of this systematic review is to identify the populations and conditions for which the FM can be used in physiotherapy and to determine the intervention modalities. Research in PubMed, Cochrane and PEDro databases was performed. The PEDro scale was employed to assess the methodological quality. Meta-analyses (MA) were performed whenever populations and outcome measures were comparable in at least two studies. Sixteen studies were included. In elderly people, in three of the four selected trials, the FM group significantly improved gait, balance, mobility and quality of life. The MA showed significant differences between interventions in the Timed-Up-and-Go test [Cohen’s d = −1.14, 95% CI (−1.78, −0.49), p = 0.0006]. FM significantly improved pain, functional balance, and perceived exertion in three trials performed on subjects with cervical, dorsal, or shoulder pain. FM demonstrated improvements in pain, disability, quality of life and interoceptive awareness in the three trials performed in subjects with chronic low back pain. In multiple sclerosis, an improvement in functional capacity was observed in the two selected studies. The MA showed no significant differences between groups in the Function (p = 0.97) and Control (p = 0.82) dimensions of the Multiple Sclerosis Self-Efficacy Scale. In Parkinson’s disease, two studies showed significant effects on quality of life and functional tests. In conclusion, evidence shows that FM has therapeutic effects comparable to other physiotherapy techniques in patients with spine pain. In addition, improvements in mobility and balance were seen in the elderly and people with neurodegenerative diseases.
1. Introduction
The Feldenkrais Method (FM) is a technique aiming at increasing personal self-knowledge through conscious movements, developed by the physicist Moshe Feldenkrais [1,2]. This method is based on the discovery and learning of varied, alternative patterns of movement and aims to improve the human ability to learn movement [3,4]. The method has been applied to different educational areas in different countries to improve sports and theatre performance [5]. Furthermore, FM has been employed in movement lessons by using two modalities. One modality, named “Awareness through movement” (ATM), is applied in group sessions. In this modality, the Feldenkrais therapist guides the subjects verbally into postures and movements and asks them about bodily sensations. The other modality, named “Functional Integration” (FI), consists of individual sessions of passive and soft mobilizations directed to movement re-education and to improve proprioception [5,6].
The main objective of FM seems to be more educational than therapeutic [7]. However, the FM is recognized by the German health system and is widely employed in the United States, Australia and Germany. In Germany, FM is generally used to treat postural deformities, musculoskeletal limitations, dorsal pain, neurological pathologies, chronic pain, development disorders in children and adolescents, psychosomatic and stress-related disorders [1]. Thus, the indications of the FM seem to be compatible with the physical therapy practice.
Previous systematic reviews have studied the effects of FM. The first of them was published in 2005 by Ernst and Canter [2], and it concluded that although there were some trials that supported the FM, the evidence published was not sufficient in quantity and quality to support the method robustly. The second systematic review was published in 2015 by Hillier and Worley [5], where the authors updated the first review and included a meta-analysis (MA), concluding that the trials about FM were very heterogeneous in terms of population, variables and results. They suggested that although there was promising evidence of the efficacy of the FM in improving balance in elderly people, more research was needed to support these findings. Another systematic review focused on patients with cervical or lumbar pain [8] included four trials and concluded that there was some evidence about the efficacy of FM to improve pain, although they determined that the intervention modalities seemed to be inconsistent and the measurement variables heterogeneous.
Accordingly, the hypothesis of this systematic review and MA is that the actual evidence would be sufficient to support the inclusion of FM among physical therapy tools, and the FM could have similar effects when compared to other techniques already employed in physical therapy.
To test this hypothesis, it is necessary to update the evidence about FM, focusing on its therapeutic potential within the scope of physical therapy. Therefore, the objectives of this systematic review and MA were (1) to identify the recent scientific evidence about FM and determine the populations and pathologies where FM could be employed as a physical therapy tool; (2) to analyze which of the two modalities of FM is more effective in physical therapy; (3) and to analyze the therapeutic effects obtained with the FM.
2. Materials and Methods
This review was planned and conducted based on the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) [9]. The protocol of this review has been previously registered in the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42021282249).
2.1. Eligibility Criteria
This systematic review included all the randomized clinical trials (RCT) that met the following eligibility criteria: (1) RCT with a population of interest in the field of physical therapy; (2) group, individual or mixed-modality sessions of FM as the primary intervention; (3) a control group (CG) classified as no intervention, placebo, simulation, educational intervention or conventional physical therapy intervention; (4) at least one primary outcome measure to assess patient’s physical condition such as mobility, cardiovascular condition, muscle strength, balance, pain, gait performance, functionality or quality of life; (5) articles written in English or in Spanish.
As an exclusion criterion, studies carried out on healthy subjects were excluded from this review.
2.2. Search Strategy and Selection Process
The following electronic databases were searched: PubMed, Cochrane and PEDro, from inception to August 2022. Reference lists of selected trials, previous publications and cited reviews were manually examined.
The following keywords were employed to carry out the search: “Feldenkrais”, “Awareness through Movement” and “Functional Integration”. Terms were related using the Boolean index “OR”. No publication data restrictions were applied. Results were restricted only to human subjects.
The searching process, the text screening and the application of the eligibility criteria were performed by two independent reviewers (RB, TSM). First, the results were screened by title and abstract, and second, remaining references were assessed for eligibility by in-depth reading of the full texts. Inconsistences between reviewers were solved by consensus.
2.3. Data Collection and Risk of Bias Assessment
Two independent reviewers (RB, TSM) performed the study identification, data extraction and assessed risk of bias using PEDro scale. When different results were obtained by the reviewers, it was discussed among them, and an agreement was reached.
All the included articles underwent a protocolized, systematic and standardized analysis. The following data were extracted into a spreadsheet: title, authors, year of publication, country, study design, population, sample size, sample mean age, sample gender, characteristics of FM and CG interventions, follow-up, outcome measures and results.
Regarding PEDro scale, it is considered that scores ≤3 points indicate poor methodological quality, between 4 and 5 points indicate fair methodological quality, between 6 and 8 points mean good methodological quality and scores >8 points indicate excellent methodological quality [10].
2.4. Statistical Analysis
When RCTs investigated the same type of population and extracted the same outcome measure, a random-effects MA was performed, with standardized mean differences for continuous outcomes. The Review Manager software (RevMan) version 5.4, The Cochrane Collaboration, London, United Kingdom, was employed [11].
Moreover, 95% confidence intervals (CI) and heterogeneity values (I2) were calculated. I² values of 25%, 50% and 75% were considered as low, moderate and high heterogeneity, respectively [12]. In addition, mean effects sizes and the resulting forest plots to visualize MA results were obtained.
3. Results
3.1. Study Selection
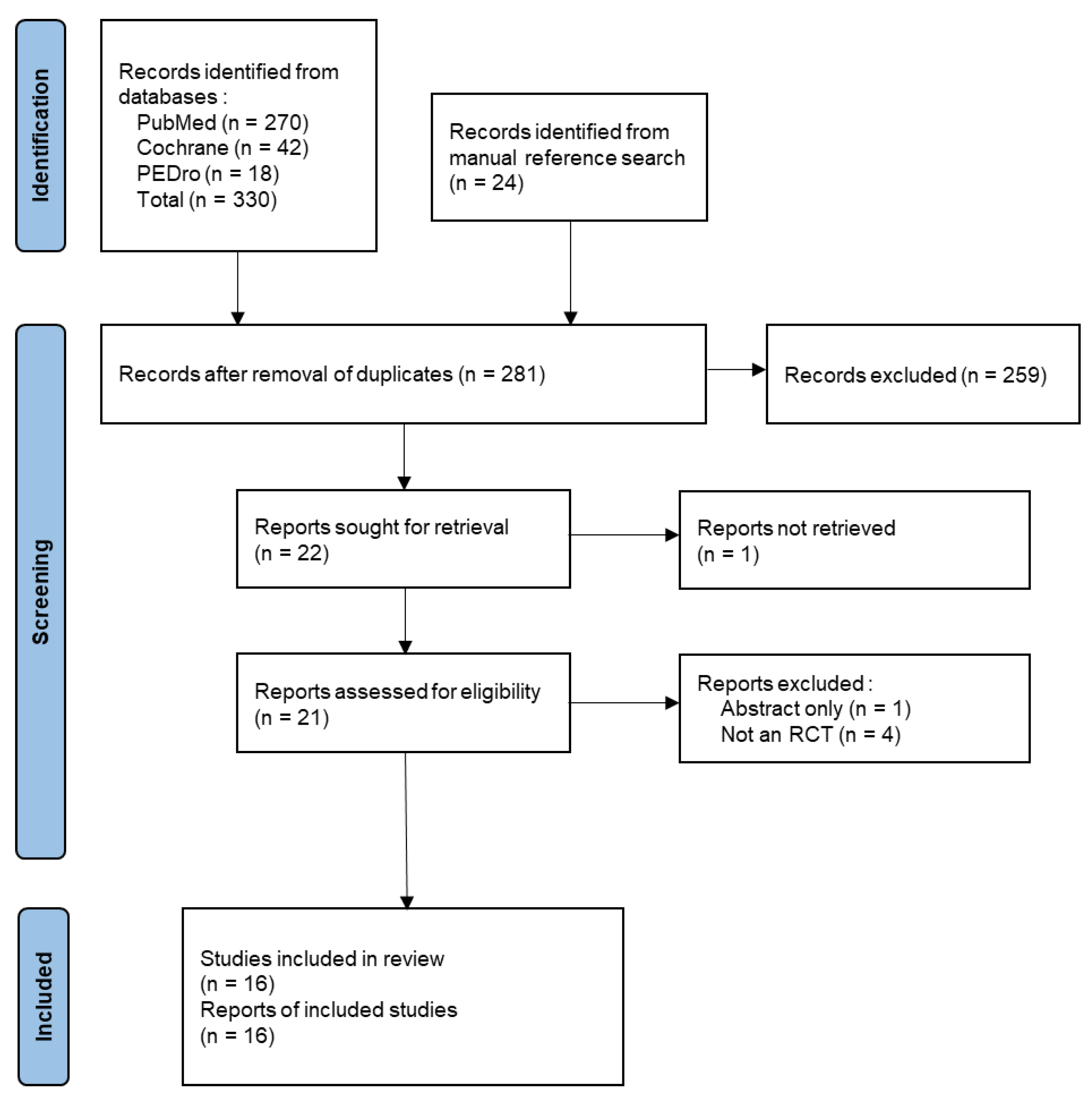
A total of 330 publications were identified in databases using the search strategy (Figure 1), among which 270 were found in PubMed, 42 in Cochrane and 18 in PEDro. A further 24 trials were found by manual search. After applying the eligibility criteria and discarding duplicates, 16 studies were finally included.
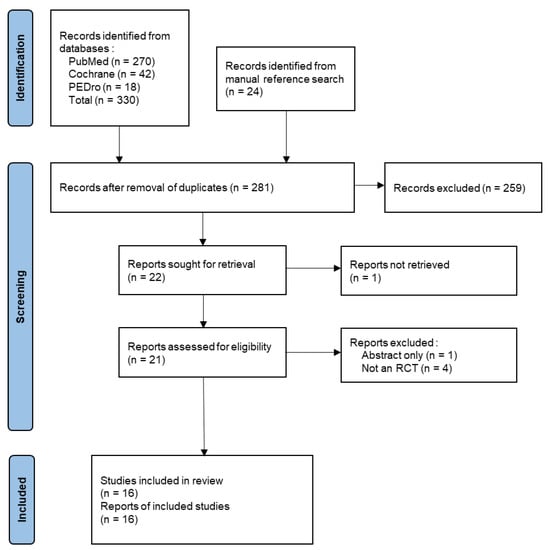
Figure 1.
PRISMA Flowchart of the search and selection of the articles.
3.2. Methodological Quality Assessment
The methodological quality of the included studies is presented in Table 1. Five articles [13,14,15,16,17] presented a good methodological quality, one of them [18] presented a poor methodological quality, and the others presented a fair methodological quality. Neither the subjects nor the therapists were blinded in any of the studies. Intention-to-treat analysis was performed in four studies [13,14,19,20] and allocation concealment in five studies [13,15,16,17,21]. In most studies, assessors were not blinded, nor was the follow-up adequate.

Table 1.
Methodological quality of the included articles assessed by using the PEDro scale.
3.3. Characteristics of the Studies
Table 2 shows the characteristics and results of the included studies. The articles were published between 1994 [19] and 2020 [13]. Most studies were RCTs with two parallel groups. The populations found were heterogeneous. Three of the studies investigated subjects with cervical, dorsal or shoulder pain [14,19,23], three of them subjects with chronic low back pain [13,15,16], two of them subjects with multiple sclerosis [22,26], two of them subjects with Parkinson’s disease [27,28], four of them elderly subjects [17,18,20,24], one trial investigated children with nocturnal bruxism [25] and one investigated middle-aged subjects with intellectual disability [21].

Table 2.
Description of the included studies.
The most frequent intervention in the Feldenkrais group (FG) was ATM. Two trials employed a combination of ATM and FI [14,23]. The CG performed no intervention in six trials [14,17,18,20,21,23], educational sessions in four trials [13,26,27,27], simulation in two trials [19,22], physical activity in two trials [13,24] and conventional physical therapy in one trial [15]. In the three-arms clinical trials, the other intervention group performed physical therapy sessions [23] or Pilates [24].
Regarding outcome measures, the most frequently employed were pain, balance, functional capacity and quality of life.
The characteristics of the studies for each type of population investigated are detailed below.
3.3.1. Elderly Subjects
The effects of FM in elderly subjects were studied in four trials (total number of participants n = 286) [17,18,20,24]. The mean age was between 69 and 76 years, and the predominant gender was female. The intervention protocol of the FG was one to three ATM group sessions per week, totaling between eight sessions [17] and eighteen sessions [24]. The CG performed either no intervention or a 12-min walking program at a comfortable speed with a previous warm-up [24]. Nambi et al. [24] included a second intervention group that performed 18 sessions of Pilates.
Regarding outcome measures, all trials evaluated mobility and balance. Except for Ullmann et al. [20], all trials evaluated the quality of life.
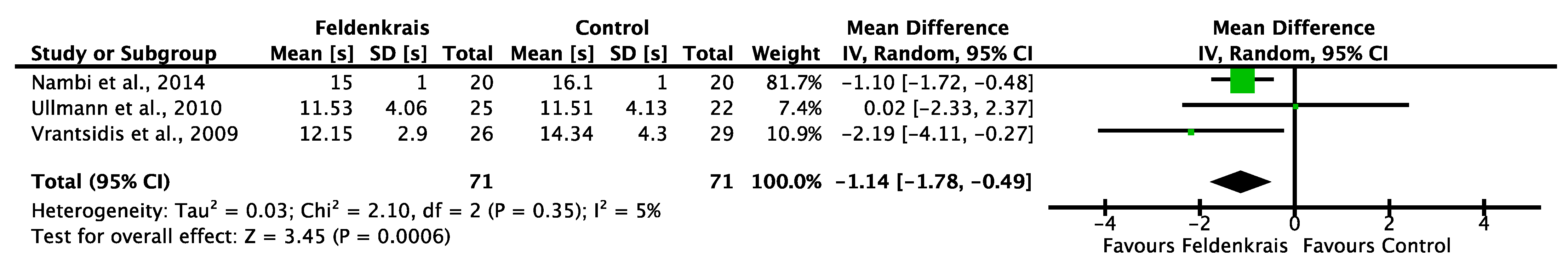
Regarding trial results, three of the four trials [17,20,24] obtained significant improvements in favor of FM with respect to mobility (Timed-Up-and-Go test, gait speed), balance (tandem posture, functional reach and fear of falling) [17,18,20,24] and quality of life [18,24]. The Timed-Up-and-Go test, analyzed in all studies, showed significant improvements in all trials except for Palmer [18]. The MA showed significant differences between interventions (FG and CG) in The Timed-Up-and-Go test [Cohen’s d = −1.14, 95% CI (−1.78, −0.49), p = 0.0006]. Complete MA information with forest plot is presented in Figure 2.
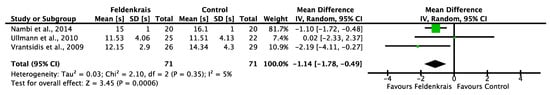
Figure 2.
Meta-analysis of TUG in elderly subjects measured in seconds. (Nambi et al. [24], Ullmann et al. [20], Vrantsidis et al. [17]).
Heterogeneity (I2) was low, with a value of 5%. As far as quality of life is concerned, significant improvements were found in favor of the FM intervention, except in the study of Vrantsidis et al. [17]. It was not possible to perform a MA because of the heterogeneity of employed outcome measures.
3.3.2. Subjects with Cervical, Dorsal or Shoulder Pain
Three trials investigated the effects of FM in patients with cervical, dorsal or shoulder pain (total number of participants n = 181) [14,19,23]. The mean age was between 18 and 59 years, and most of the participants were female. The FG intervention protocol consisted of: (1) a program of 12–16 sessions of ATM combined with FI [14,23] or (2) a single pre-recorded ATM session [19]. Moreover, Lundblad et al. [23] included a second intervention group that performed a physical therapy protocol for 16 weeks. The CG performed either no intervention [14,23] or a pre-recorded simulated session of ATM [19].
The outcome measures related to pain [14,23], functional balance [19] and perceived exertion [19] were heterogeneous; thus, the MA was not performed. Significant changes were found in favor of the FG [14,19,23]. Regarding pain and muscle complaints, significant differences were found between FG and CG [14,23]. Lundqvist et al. [14] observed a significant increase in palpation pain in the occipital muscles and left and right upper trapezius in the CG at post-intervention and at one-year follow-up, while the FG did not show significant changes. Lundqvist et al. [14] showed a significant reduction of muscle complaints in the FG. Furthermore, Lundblad et al. [23] showed a significant reduction of muscle complaints and disability in FG, while the muscle complaints increased in the CG and remained stable in the physical therapy group. Regarding pain intensity, Lundblad et al. [23] showed a significant reduction in CG and FG, but the reduction was more pronounced in FG compared to CG. The physical therapy group did not show significant reductions in pain intensity. Lastly, Chinn et al. [19] showed a significant reduction in the perceived exertion during the forward reach test in the FG.
3.3.3. Subjects with Chronic Low Back Pain
Three trials investigated the effects of FM in subjects with chronic low back pain (total number of participants n = 139) [13,15,16]. The mean age was between 39 and 61 years, and most of the sample was female. The FG performed either 10 ATM group sessions [13,15], or a unique, pre-recorded ATM session [16]. Regarding the CG, Paolucci et al. [15] provided back school lessons imparted by a physical therapist and Ahmadi et al. [13] educational sessions and core stability exercises.
Regarding outcome measures, Paolucci et al. [15] and Ahmadi et al. [13] assessed pain, disability, quality of life and interoceptive awareness. Both trials evaluated pain through the McGill questionnaire and interoceptive awareness through the Multidimensional Assessment of Interoceptive Awareness questionnaire [29]. Smith et al. [16] assessed pain and anxiety. All the studies showed significant changes in the FG [13,15,16]. Regarding pain, changes were found in the FG, but no differences with the CG were found. The FG obtained better scores than the back school lessons with respect to the McGill Present Pain Intensity subscale [15] and obtained better McGill scores than the core stability training program [13]. Smith et al. [16] measured pain through the Short Form- McGill questionnaire and observed a significant reduction in pain in the CG. Moreover, the FM showed significant improvements in quality of life, disability and interoceptive awareness compared to core stability training [13]. On the other hand, Paolucci et al. [15] showed better scores in the back school group than the FG with respect to the Vitality and Social Functioning dimensions of the Short Form-36 (measuring quality of life), while the Multidimensional Assessment of Interoceptive Awareness questionnaire score was not different between groups.
3.3.4. Subjects with Multiple Sclerosis
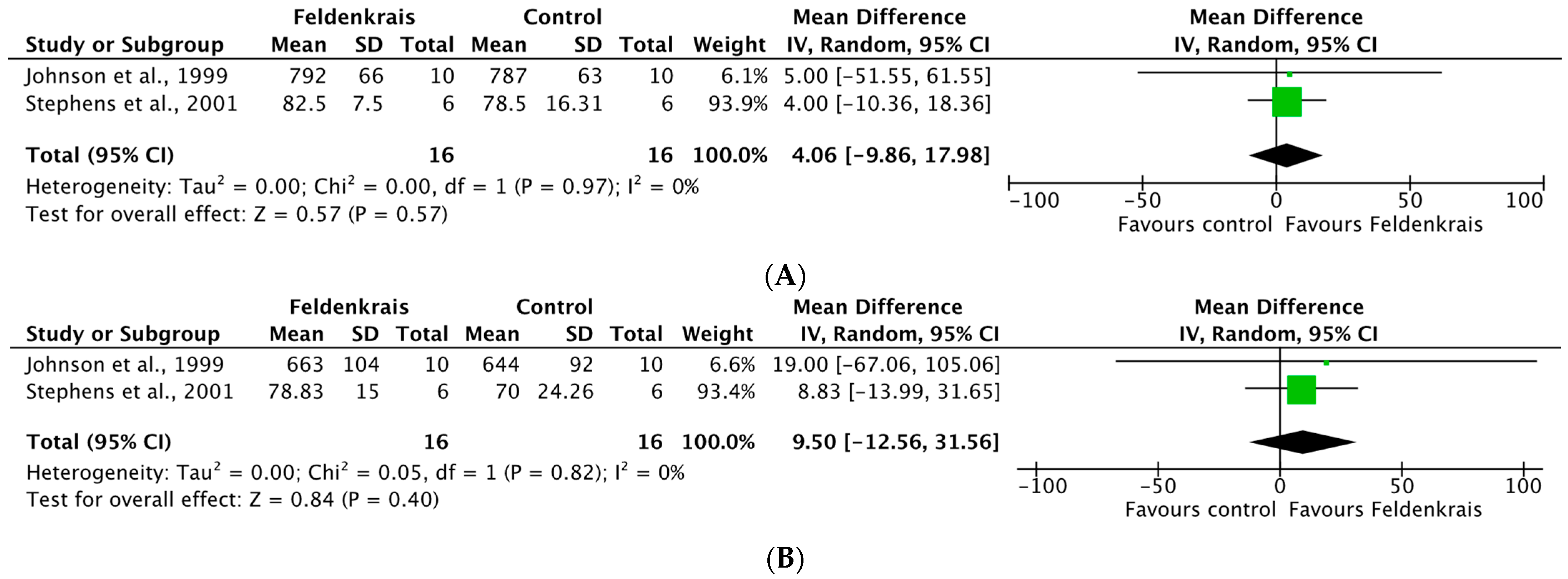
Two studies investigated the effects of FM in subjects with multiple sclerosis (total number of participants n = 32) [22,26]. The mean age was between 45 and 56 years, and the predominant gender was female. The intervention protocol consisted of ATM group sessions. Johnson et al. [22] performed a total of 6 h of ATM, while Stephens et al. [26] imparted a total of 20 h. The CG received a manual treatment simulation [22] or educative sessions [26]. Stephens et al. [26] assessed balance and functional capacity, while Johnson et al. [22] evaluated functional capacity, anxiety, depression and symptoms. Both trials evaluated confidence in functional capacity through the Multiple Sclerosis Self-Efficacy scale.
Regarding the results, both trials showed significant changes in the FG [22,26]. Johnson et al. [22] showed a significant reduction in the perceived stress in the FG. Stephens et al. [26] showed a significant improvement in balance and balance confidence in the FG. Regarding confidence in functional capacity, both trials showed a trend toward improvement in the FG.
The MA showed no significant differences between FG and CG with respect to the dimensions of Function [Cohen’s d = 4.06, 95% CI (−9.86, 17.98), p = 0.97] and Control [Cohen’s d = 9.50, 95% CI (−12.56, 31.56), p = 0.82] of the Multiple Sclerosis Self-Efficacy scale. Complete MA information with forest plot is presented in Figure 3A,B.
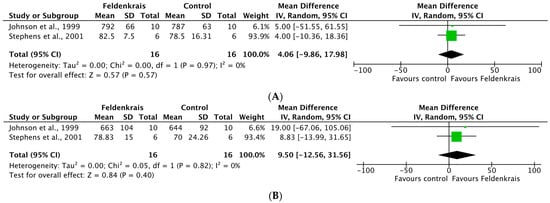
Figure 3.
(A) Meta-analysis for the Function dimension of the MSSE scale in subjects with multiple sclerosis. (B) Meta-analysis for the Control dimension of the MSSE scale in subjects with multiple sclerosis. (Johnson et al. [22], Stephens et al. [26]).
3.3.5. Subjects with Parkinson’s Disease
The effects of FM in subjects with Parkinson’s disease were analyzed in two studies with identical samples and protocol (total number of participants n = 30) [27,28]. The mean age was 61 years. The FG received a total of 50 h of ATM sessions, while the CG received educative sessions.
Regarding outcome measures, one of them evaluated the quality of life, depression and cognitive status [27], while the other analyzed balance, mobility, gait speed and strength through functional tests [28]. Both studies showed significant effects on the FG [27,28]. One of them showed significant improvements in quality of life, depression and cognitive status in the FG compared to the CG [27]. The other trial showed that the FG improved significantly in all the variables compared to the CG, whereas in the CG all the values worsened [28]. The Timed-Up-and-Go test showed a reduction in the FG, decreasing from 22.27 ± 2.93 to 12.46 ± 0.92 s (p = 0.003).
3.3.6. Other Populations
Quintero et al. [25] investigated the effects of a 30 h ATM sessions protocol on the head posture of 26 children with nocturnal bruxism with a mean age of three to four years. Torres-Unda et al. [21] investigated the effects of a 30 h ATM sessions protocol on the physical function and balance (measured with a stability platform) of middle-aged persons with intellectual disabilities, for whom difficulties due to aging appear earlier than in people without intellectual disabilities [21].
Regarding the effects, Quintero et al. [25] showed the efficacy of FM in treating children with nocturn bruxism, for whom the FM increased the craniovertebral angle and corrected the head posture. In middle-aged persons with intellectual disabilities, Torres-Unda et al. [21] showed a significant improvement in physical function in FG compared to CG and a reduction of the sway area.
4. Discussion
This systematic review presents the evidence available to date on the effects of FM in the population eligible for physical therapy treatment. Population groups included elderly people, people with musculoskeletal pain in the spine or shoulder, and people with neurodegenerative diseases such as MS or PD.
In relation to the obtained results, most of the trials showed significant changes in the FG. In elderly subjects, the mean differences obtained in favor of FM in the Timed-Up-and-Go test MA (mean difference of 1.14 s) could be considered clinically significant based on the study of Wright et al. [30] where the minimum clinically significant difference in Timed-Up-and-Go test was calculated in patients with hip osteoarthritis and showed that a reductions ≥0.8–1.4 s could be considered clinically significant. Moreover, a reduction in the Timed-Up-and-Go test is related to the decrease in fall risk [31]. This outcome measure is also related to sarcopenia [32], frailty [33] and osteoporosis [34], which are highly prevalent in the elderly population. Future studies should assess whether this treatment method influences this situation of great interest in the elderly population. It shall be noted that the Timed-Up-and-Go test MA results obtained in this review are identical to those obtained by an earlier review [5]. Older adults also improved through the FM in terms of balance, fear of falling and quality of life. Nambi et al. [24] showed that both studied interventions (FM and Pilates method) led to improvements, but the results with the Pilates method were better than with the FM. The authors discuss that the popularity of Pilates and social interactions could partly explain the results obtained.
Regarding musculoskeletal pain, the subjects with cervical, dorsal or shoulder pain improved through the FM in terms of pain intensity, muscle complaints, leisure disability and perceived exertion during the reach test. Lundblad et al. [23] trial showed that FM was better than conventional therapy. These findings are in line with the results of the Mohan et al. [8] systematic review regarding subjects with chronic low back pain, where FM was equal to or better than physical therapy interventions based on back school [15] or core stability exercises [13]. Significant improvements were found in pain, quality of life, disability, interoceptive awareness and abdominal musculature. According to Mehling et al. [35], interoceptive awareness may play important roles in health, particularly in pain perception. The Multidimensional Assessment of Interoceptive Awareness questionnaire could be useful when the therapeutic intervention directly targets the mind-body interface, as is the case with the FM [35]. Paolucci et al. [15] observed that the effects of FM in reducing pain and improving interoceptive awareness were still effective three months after the start of the intervention. Moreover, they indicated that the FM could reduce the intensity of pain and modify the pain perception faster than back school lessons. Ahmadi et al. [13] concluded that FM has the advantage, compared to an educational program and core exercises, of improving abdominal musculature, interoceptive awareness and disability.
In subjects with multiple sclerosis, the FM improved the perceived stress, balance and balance confidence. However, the samples were small, and future studies with larger samples are needed to confirm these results. In subjects with Parkinson’s disease, improvements in balance, mobility, speed and quality of life were found. The changes in the Timed-Up-and-Go test (the time spent in the test decreased by 9.8 s to reach a mean value of 12.46 s) indicate that the FM has clinical effects in subjects with Parkinson’s disease. According to Barry et al. [31], values below 13.5 s may indicate a decreased risk of falling. However, since only two studies were published in this area and the sample was the same, new studies are needed to confirm these improvements.
With regard to methodological quality, which has been criticized in previous reviews [2,5,8], it should be noted that, in the included articles, it was either good or fair, except in one article where the methodological quality was poor. The difficulty of blinding subjects and therapists is common in rehabilitation trials [36]. The trials scores are consistent with the analysis of a study about the construction validity of the PEDro scale, in which Albanese et al. [37] showed that subjects and therapists blinding was almost never implemented, while criteria related to random assignment, comparisons between groups, point measures and variability measures were almost always met. However, only five articles obtained a good methodological quality, and other criteria of the PEDro scale were frequently not met, such as concealed allocation, blinding assessors, adequate follow-up and intention-to-treat analysis.
In relation to the intervention modality, the most employed protocol for the FG included 10 to 30 sessions, applied once or twice per week, with a duration of 45 min to 2 h. The findings of this review contradict the idea that sessions should be short (between 30–45 min) to prevent mental fatigue [38]. ATM group sessions constituted the most used practice. The improvements obtained through this modality are interesting, considering aspects such as costs and time of the professional’s work. Future cost-effectiveness studies are needed to clarify this issue. Furthermore, the ATM modality enhances participation, which is one of the pillars to consider in a rehabilitation process within the framework of the International Classification of Functioning, Disability and Health [39].
The greatest strength of this review is that this is the first work that analyzes the effects of FM on the population that needs physical therapy. In addition, despite the different types of FM and the different control group interventions, the most frequently used exercises and protocols have been described and shortlisted. We also highlight the statistical rigor performed in the study. Moreover, the results of the analyzed variables show a low heterogeneity. Finally, the differentiation by type of illness facilitates the understanding of the results and could be used as a guide for the development of new studies in each field.
This systematic review and meta-analysis have some limitations that should be mentioned. Firstly, the search was performed in a limited number of databases. Secondly, language was also a restriction that could have reduced the number of studies reviewed. Thirdly, the risk of bias remains high due to the insufficient methodological quality of certain studies. Finally, in some populations, trials with larger samples are needed to be able to extract solid conclusions.
5. Conclusions
This systematic review and MA concluded that FM applied in ATM group sessions is effective in the treatment and prevention of some pathologies or clinical conditions. Regarding elderly people, FM improves mobility, balance and quality of life. Regarding pain, in people with chronic low back pain, FM has similar benefits such as back school lessons or core stability exercises; in people with cervical pain, the FM may be more adequate than conventional physical therapy. Regarding people with neurodegenerative diseases, the FM is effective in improving balance.
These findings should be taken with caution due to the low number of RCTs in the different specific populations. Future research would be useful to give more solidity to these findings and to consider the role of this treatment method in the prevention of falls and other age-related problems, such as sarcopenia, frailty and falls, due to its implication in improving the Timed-Up-and-Go test in different populations.
Author Contributions
Conceptualization, R.B., T.S.-M. and J.L.M.-M.; methodology, R.B., T.S.-M. and J.L.M.-M.; software, R.B. and T.S.-M.; validation, A.L.-R., N.M.-S. and E.M.-S.; formal analysis, R.B., T.S.-M. and J.L.M.-M.; investigation, A.L.-R., N.M.-S. and E.M.-S.; data curation, A.L.-R., N.M.-S. and E.M.-S.; writing—original draft preparation, R.B., T.S.-M., A.L.-R. and J.L.M.-M.; writing—review and editing, A.L.-R., N.M.-S. and E.M.-S.; visualization, A.L.-R. and N.M.-S.; supervision, E.M.-S. and T.S.-M.; project administration, E.M.-S. and T.S.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Brummer, M.; Walach, H.; Schmidt, S. Feldenkrais ‘Functional Integration’ Increases Body Contact Surface in the Supine Position: A Randomized-Controlled Experimental Study. Front. Psychol. 2018, 9, 2023. [Google Scholar] [CrossRef] [PubMed]
- Ernst, E.; Canter, P.H. The Feldenkrais Method—A Systematic Review of Randomised Clinical Trials. Phys. Med. Rehabil. Kurortmed. 2005, 15, 151–156. [Google Scholar] [CrossRef][Green Version]
- Buchanan, P.A. The Feldenkrais Method® of Somatic Education; IntechOpen: London, UK, 2012; ISBN 978-953-307-863-2. [Google Scholar]
- Mattes, J. Attentional Focus in Motor Learning, the Feldenkrais Method, and Mindful Movement. Percept. Mot. Skills 2016, 123, 258–276. [Google Scholar] [CrossRef]
- Hillier, S.; Worley, A. The Effectiveness of the Feldenkrais Method: A Systematic Review of the Evidence. Evid.-Based Complement. Altern. Med. 2015, 2015, 752160. [Google Scholar] [CrossRef] [PubMed]
- Verrel, J.; Almagor, E.; Schumann, F.; Lindenberger, U.; Kühn, S. Changes in Neural Resting State Activity in Primary and Higher-Order Motor Areas Induced by a Short Sensorimotor Intervention Based on the Feldenkrais Method. Front. Hum. Neurosci. 2015, 9, 232. [Google Scholar] [CrossRef]
- Federación de enseñanza de CC.OO.; de Andalucía. El Método Feldenkrais Como Sistema de Educación Postural Del Músico. Temas Para Educ. 2011. Available online: https://www.feandalucia.ccoo.es/docu/p5sd8761.pdf (accessed on 27 September 2022).
- Mohan, V.; Paungmali, A.; Sitilertpisan, P.; Henry, L.J.; Mohamad, N.B.; Kharami, N.N.B. Feldenkrais Method on Neck and Low Back Pain to the Type of Exercises and Outcome Measurement Tools: A Systematic Review. Pol. Ann. Med. 2017, 24, 77–83. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Cashin, A.G.; McAuley, J.H. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J. Physiother. 2020, 66, 59. [Google Scholar] [CrossRef]
- Review Manager (RevMan) [Computer Program], Version 5.4. The Cochrane Collaboration: London, UK, 2020.
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring Inconsistency in Meta-Analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Ahmadi, H.; Adib, H.; Selk-Ghaffari, M.; Shafizad, M.; Moradi, S.; Madani, Z.; Partovi, G.; Mahmoodi, A. Comparison of the Effects of the Feldenkrais Method versus Core Stability Exercise in the Management of Chronic Low Back Pain: A Randomised Control Trial. Clin. Rehabil. 2020, 34, 1449–1457. [Google Scholar] [CrossRef] [PubMed]
- Lundqvist, L.-O.; Zetterlund, C.; Richter, H.O. Effects of Feldenkrais Method on Chronic Neck/Scapular Pain in People with Visual Impairment: A Randomized Controlled Trial with One-Year Follow-Up. Arch. Phys. Med. Rehabil. 2014, 95, 1656–1661. [Google Scholar] [CrossRef] [PubMed]
- Paolucci, T.; Zangrando, F.; Iosa, M.; De Angelis, S.; Marzoli, C.; Piccinini, G.; Saraceni, V.M. Improved Interoceptive Awareness in Chronic Low Back Pain: A Comparison of Back School versus Feldenkrais Method. Disabil. Rehabil. 2017, 39, 994–1001. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.L.; Kolt, G.S.; McConville, J.C. The Effect of the Feldenkrais Method on Pain and Anxiety in People Experiencing Chronic Low Back Pain. N. Z. J. Physiother. 2001, 29, 6–14. [Google Scholar]
- Vrantsidis, F.; Hill, K.D.; Moore, K.; Webb, R.; Hunt, S.; Dowson, L. Getting Grounded Gracefully: Effectiveness and Acceptability of Feldenkrais in Improving Balance. J. Aging Phys. Act. 2009, 17, 57–76. [Google Scholar] [CrossRef] [PubMed]
- Palmer, C.F. Feldenkrais Movement Lessons Improve Older Adults’ Awareness, Comfort, and Function. Gerontol. Geriatr. Med. 2017, 3, 2333721417724014. [Google Scholar] [CrossRef]
- Chinn, J.; Trujillo, D.; Kegerreis, S.; Worrell, T. Effect of a Feldenkrais Intervention on Symptomatic Subjects Performing a Functional Reach. Isokinet. Exerc. Sci. 1994, 4, 131–136. [Google Scholar] [CrossRef]
- Ullmann, G.; Williams, H.G.; Hussey, J.; Durstine, J.L.; McClenaghan, B.A. Effects of Feldenkrais Exercises on Balance, Mobility, Balance Confidence, and Gait Performance in Community-Dwelling Adults Age 65 and Older. J. Altern. Complement. Med. 2010, 16, 97–105. [Google Scholar] [CrossRef]
- Torres-Unda, J.; Polo, V.; Dunabeitia, I.; Bidaurrazaga-Letona, I.; García-Gil, M.; Rodriguez-Larrad, A.; Irazusta, J. The Feldenkrais Method Improves Functioning and Body Balance in People with Intellectual Disability in Supported Employment: A Randomized Clinical Trial. Res. Dev. Disabil. 2017, 70, 104–112. [Google Scholar] [CrossRef]
- Johnson, S.K.; Frederick, J.; Kaufman, M.; Mountjoy, B. A Controlled Investigation of Bodywork in Multiple Sclerosis. J. Altern. Complement. Med. 1999, 5, 237–243. [Google Scholar] [CrossRef]
- Lundblad, I.; Elert, J.; Gerdle, B. Randomized Controlled Trial of Physiotherapy and Feldenkrais Interventions in Female Workers with Neck-Shoulder Complaints. J. Occup. Rehabil. 1999, 9, 179–194. [Google Scholar] [CrossRef]
- Nambi, G.; Trivedi, P.; Momin, S.; Patel, S.; Pancholi, D. Comparative Effect of Pilates and Feldenkrais Intervention on Functional Balance and Quality of Life in Ambulatory Geriatric Population: A Randomized Controlled Study. Int. J. Health Sci. Res. 2014, 4, 71–79. [Google Scholar]
- Quintero, Y.; Restrepo, C.C.; Tamayo, V.; Tamayo, M.; Vélez, A.L.; Gallego, G.; Peláez-Vargas, A. Effect of Awareness through Movement on the Head Posture of Bruxist Children. J. Oral Rehabil. 2009, 36, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Stephens, J.; DuShuttle, D.; Hatcher, C.; Shmunes, J.; Slaninka, C. Use of Awareness Through Movement Improves Balance and Balance Confidence in People with Multiple Sclerosis: A Randomized Controlled Study. J. Neurol. Phys. Ther. 2001, 25, 39–49. [Google Scholar] [CrossRef]
- Teixeira-Machado, L.; Araújo, F.M.; Cunha, F.A.; Menezes, M.; Menezes, T.; Melo DeSantana, J. Feldenkrais Method-Based Exercise Improves Quality of Life in Individuals with Parkinson’s Disease: A Controlled, Randomized Clinical Trial. Altern. Ther. Health Med. 2015, 21, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Teixeira-Machado, L.; de Araújo, F.M.; Menezes, M.A.; Cunha, F.A.; Menezes, T.; da Ferreira, C.S.; DeSantana, J.M. Feldenkrais Method and Functionality in Parkinson’s Disease: A Randomized Controlled Clinical Trial. Int. J. Disabil. Hum. Dev. 2017, 16, 59–66. [Google Scholar] [CrossRef]
- Mehling, W.E.; Price, C.; Daubenmier, J.J.; Acree, M.; Bartmess, E.; Stewart, A. The Multidimensional Assessment of Interoceptive Awareness (MAIA). PLoS ONE 2012, 7, e48230. [Google Scholar] [CrossRef]
- Wright, A.A.; Cook, C.E.; Baxter, G.D.; Dockerty, J.D.; Abbott, J.H. A Comparison of 3 Methodological Approaches to Defining Major Clinically Important Improvement of 4 Performance Measures in Patients with Hip Osteoarthritis. J. Orthop. Sports Phys. Ther. 2011, 41, 319–327. [Google Scholar] [CrossRef]
- Barry, E.; Galvin, R.; Keogh, C.; Horgan, F.; Fahey, T. Is the Timed Up and Go Test a Useful Predictor of Risk of Falls in Community Dwelling Older Adults: A Systematic Review and Meta- Analysis. BMC Geriatr. 2014, 14, 14. [Google Scholar] [CrossRef]
- Martinez, B.P.; Gomes, I.B.; de Oliveira, C.S.; Ramos, I.R.; Rocha, M.D.M.; Júnior, L.A.F.; Camelier, F.W.R.; Camelier, A.A. Accuracy of the Timed Up and Go Test for Predicting Sarcopenia in Elderly Hospitalized Patients. Clinics 2015, 70, 369–372. [Google Scholar] [CrossRef]
- Larsson, B.A.M.; Johansson, L.; Johansson, H.; Axelsson, K.F.; Harvey, N.; Vandenput, L.; Magnusson, P.; McCloskey, E.; Liu, E.; Kanis, J.A.; et al. The Timed up and Go Test Predicts Fracture Risk in Older Women Independently of Clinical Risk Factors and Bone Mineral Density. Osteoporos. Int. 2021, 32, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Mousa, S.M.; Rasheedy, D.; El-Sorady, K.E.; Mortagy, A.K. Beyond Mobility Assessment: Timed up and Go Test and Its Relationship to Osteoporosis and Fracture Risk. J. Clin. Gerontol. Geriatr. 2016, 7, 48–52. [Google Scholar] [CrossRef][Green Version]
- Mehling, W.E.; Daubenmier, J.; Price, C.J.; Acree, M.; Bartmess, E.; Stewart, A.L. Self-Reported Interoceptive Awareness in Primary Care Patients with Past or Current Low Back Pain. J. Pain Res. 2013, 6, 403–418. [Google Scholar] [CrossRef] [PubMed]
- Rassafiani, M.; Copley, J.; Kuipers, K.; Sahaf, R. Are Explanatory Randomized Controlled Trials Feasible in Rehabilitation? Int. J. Ther. Rehabil. 2008, 15, 478–479. [Google Scholar] [CrossRef]
- Albanese, E.; Bütikofer, L.; Armijo-Olivo, S.; Ha, C.; Egger, M. Construct Validity of the Physiotherapy Evidence Database (PEDro) Quality Scale for Randomized Trials: Item Response Theory and Factor Analyses. Res. Synth. Methods 2020, 11, 227–236. [Google Scholar] [CrossRef]
- Lyttle, T.S.K. The Feldenkrais Method: Application, Practice and Principles. J. Od Bodyw. Mov. Ther. 1997, 1, 262–269. [Google Scholar] [CrossRef]
- Hemmingsson, H.; Jonsson, H. An Occupational Perspective on the Concept of Participation in the International Classification of Functioning, Disability and Health--Some Critical Remarks. Am. J. Occup. Ther. Off. Publ. Am. Occup. Ther. Assoc. 2005, 59, 569–576. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).