Abstract
Farmers in Canada faced higher levels of mental distress than the general public prior to the Coronavirus Disease 2019 (COVID-19) pandemic and are generally less likely than the public to seek help. However, the mental health impacts of COVID-19 on farmers in Canada remain unexplored. Our objective was to investigate mental health outcomes among farmers in Canada by gender and within the context of COVID-19. We conducted a national, online, cross-sectional survey of farmers in Canada (February–May 2021). The survey included validated scales of anxiety, depression, perceived stress, burnout (emotional exhaustion, cynicism, professional efficacy), alcohol use, resilience, and questions regarding participants’ perceived changes in these outcomes during the pandemic. Data were also collected on the impact of COVID-19 specific social and economic factors on mental health, help-seeking, and sense of community belonging through the pandemic. Descriptive statistics were summarized, and Chi-square analyses and t-tests were conducted to compare survey results between genders and to data collected in our similar 2016 survey and normative population data. A total of 1167 farmers participated in the survey. Participants scored more severely across scales than scale norms and the general Canadian population during COVID-19. Scale means were consistent between the 2016 and 2021 samples. Most participants with moderate to severe scores for any outcome reported worsening symptoms since the pandemic began. Women fared significantly worse than men across measures. Over twice as many women reported seeking mental health or substance use support during the pandemic than men. Participants rated the mental health impacts of all social and economic factors related to COVID-19 examined significantly (p < 0.05) differently than the Canadian public. The pandemic has negatively impacted the mental health of farmers in Canada and in ways that differ from the general population. National level and gender-specific mental health supports are needed to help improve the mental health of farmers in Canada.
1. Introduction
Ongoing assessment of the mental health impacts of the Coronavirus Disease 2019 (COVID-19) pandemic is important, as the impact of factors affecting the public (i.e., public health restrictions, grocery shortages due to panic buying, personal protective equipment shortages, school closures, fear of contracting COVID-19, and uncertainty) may be cumulative [1]. Indeed, Lowe et al. (2022) found the mental health of Ontarians and Albertans deteriorated over the beginning of the pandemic (Spring 2020), improved through Summer 2020, and declined again in the Fall/Winter of 2020/2021 [2]. Mental Health Research Canada’s national polling found levels of anxiety and depression were higher in late 2020/early 2021 than during the first wave of the pandemic in Spring 2020 [3].
In addition to the COVID-19 factors impacting Canadians in the Winter/Spring of 2021, such as continuing to experience public health restrictions, school closures, mask mandates, and the start of vaccine rollout, Canadian farmers faced unique COVID-19 impacts. In early 2021, workplace outbreaks of COVID-19 in meat processing facilities left some farmers with nowhere to send their livestock [4]. Fruit and vegetable farmers relying on essential temporary international agricultural workers were concerned about coordinating travel restrictions, COVID testing, and housing requirements for the 2021 season after facing labour shortages in 2020 [5,6,7]. Uncertainty surrounding the global pandemic added to stress when forecasting markets [8], as COVID-19 outbreaks around the world impacted the global economy [9]. These pandemic-related stressors were in addition to farming stressors at the time, such as potential for African Swine Fever [10] and forecasted weather concerns (e.g., drought in prairies) [11,12]. The impacts of these pandemic-associated stressors on the mental health of farmers in Canada are unknown; however, there is evidence that the mental health of farmers around the world has been negatively impacted by the pandemic. For example, in a study of mental health in rural residents of China during COVID-19 lockdowns, Jia et al. [13] found rural women and those whose primary income came from agricultural production had higher risk of mental illness.
The first national survey of farmer mental health in Canada was conducted in 2015/2016 and found that prior to the COVID-19 pandemic, farmers in Canada faced increased levels of stress, anxiety, depression, burnout, and lower resilience and help-seeking than population norms [14,15]. Since the 2016 survey, mental health awareness campaigns and mental health literacy programs in the agricultural community have been launched [16]. For example, “In the Know”, a mental health literacy training program tailored to Canadian agriculture and delivered by mental health professionals with agricultural backgrounds, has been introduced in 5 provinces (Ontario, Alberta, Nova Scotia, British Columbia, Manitoba) and delivered to approximately 900 members of the Canadian agricultural community thus far [17,18]. Given the increase in mental health awareness programs since 2016 and the start of the COVID-19 pandemic, we anticipate the mental health landscape of farmers in Canada has changed since 2016. The primary goal of the present study was to determine the prevalence of anxiety, depression, stress, burnout, alcohol use, and resilience among farmers in Canada in the context of COVID-19, and the perceived impact of the pandemic on the mental health of farmers in Canada.
A secondary goal of this study was to explore gender differences in farmers’ mental health during COVID-19. Results from international studies have found that the mental health impacts of the pandemic are gendered [19]; compared to men, women have scored more severely on mental health measures in China [20], Italy [21], United Kingdom [22], and Canada [23] during COVID-19. Globally, more women than men are affected by deleterious domestic violence and financial disadvantage, which have been exacerbated during the pandemic [24]. Women have also been affected by particular social and economic aspects of life during the pandemic such as childcare and household duties, which increased during the pandemic due to school closures and stay-at-home orders [25]. Farming women have historically taken on a disproportionate amount of unpaid labour, such as childcare and household maintenance [26], in addition to on-farm and potentially off-farm labour. As school closures during COVID-19 in Canada meant higher caregiving responsibilities, farming women may have had a greater inter-role conflict (e.g., between farmer and caregiver) than men [27]. Therefore, we aimed to investigate whether Canadian farming women faced more negative mental health impacts of the pandemic than farming men.
Finally, there has been some investigation of factors which mitigate negative mental health impacts during the pandemic and associated lockdowns. Notably, community characteristics (e.g., available services, cohesion, green space) have been documented in many countries [13,28,29] to affect mental health during pandemic lockdowns, particularly in rural communities [13,29]. We sought to learn how pandemic related factors were perceived by farmers to impact their mental health, and specifically whether the pandemic impacted farmers’ sense of community belonging.
2. Materials and Methods
2.1. Study Design
We conducted a cross-sectional study from 1 February to 31 May 2021. Farmers were invited to complete an online questionnaire via Qualtrics (Provo, UT, USA). We used convenience sampling to recruit participants through use of national and provincial agricultural organizations who promoted the questionnaire in their newsletters, social media, and member listervs. The researchers also posted the questionnaire on social media using hashtags (e.g., #CdnAg, #AgTwitter).
To participate, participants were required to be over 18 years of age, able to read and write English or French, and self-identify as a farmer in any commodity in Canada. As an incentive, participants could enter their email address on a separate Qualtrics survey to enter a draw to win one of five $200 prizes. Email addresses were not connected to responses to the main survey, and no identifying information was asked in the study questionnaire. Informed written consent was obtained before participants began the questionnaire. This study protocol was approved by the Research Ethics Board at the University of Guelph (21-01-001).
2.2. Questionnaire
We used validated scales to investigate six outcomes: anxiety, depression, perceived stress, burnout (emotional exhaustion, cynicism, & professional efficacy), alcohol use, and resilience. Following each measure, participants were asked a question adapted from Statistics Canada’s Canadian Survey on COVID-19 and Mental Health, “Taking them together, did the above statements relating to [outcome] apply to you more over the past month than before the pandemic, less than before the pandemic, or about the same as before the pandemic?” with a 7-point Likert-type response option (1 = a lot more; 7= a lot less). To measure the mental health impacts of COVID-19 related variables (e.g., social isolation, daily COVID-19 news), we used questions from Mental Health Research Canada’s Mental Health During COVID-19 Outbreak polls and Statistics Canada’s Canadian Survey on COVID-19 and Mental Health. The questionnaire also collected data on demographics and farming taken from the 2016 cycle version. In all, the questionnaire was estimated to take 20–25 min to complete.
2.2.1. Anxiety and Depression
The Generalized Anxiety Disorder-7 (GAD-7) and Patient Health Questionaire-9 (PHQ-9) were used to measure anxiety symptom severity [30] and depressive symptom severity [31], respectively. The seven items on the GAD-7 and nine on the PHQ-9 are based on the DSM-IV diagnostic criteria for anxiety disorders and depressive disorders, respectively [31,32]. Neither scale has demonstrated differential item functioning across language (including English and French), age, or sex of participants [33]. These scales have established validity and reliability as measures of depression and anxiety [34]. Additionally, the PHQ-9 has been endorsed by the National Institute for Health and Clinical Excellence “for use in primary care in measuring baseline depression severity and responsiveness to treatment” [31]. Both scales require participants to self-report their anxiety or depressive symptoms over the past two weeks on a 4-point Likert-type scale, from 0 (not at all) to 3 (nearly every day) [35,36]. The GAD-7 is scored within a range of 0–21, where scores indicate how likely the participant is to have no (0–5), mild (6–10), moderate (11–15), or severe (16–21) anxiety disorder symptoms [32]. The PHQ-9 is scored within a range of 0–27, where scores indicate how likely the participant is to have no (0–4), mild (5–9), moderate (10–14), moderate to severe (15–19) or severe (20–27) depressive disorder symptoms [37]. Using cut points of >10, the GAD-7 and PHQ-9 scales are used to screen for Generalized Anxiety Disorder (GAD) and Major Depressive Disorder (MDD), respectively [33].
2.2.2. Perceived Stress
The Perceived Stress Scale (PSS) 10-item version was used to measure perceived stress in this sample. The PSS was developed with the aim to measure “the degree to which situations in one’s life are appraised as stressful” [38]. It has established reliability and validity in English [39] and French [40], and has been previously used with Canadian farmers [15]. The 10-item scale asks participants to rate their thoughts and feelings relating to perceived stress within the last month on a 5-point Likert type scale from 0 (never) to 4 (very often) [38]. Higher mean scores indicate higher perceived stress [38].
2.2.3. Burnout
We used the Maslach Burnout Inventory-General Survey (MBI) to measure the three components of burnout: emotional exhaustion, “wearing out, loss of energy, depletion, debilitation, and fatigue”; cynicism, “negative or inappropriate attitudes towards clients, irritability, loss of idealism, and withdrawal”; and professional efficacy, “productivity or capability, morale, and an ability to cope” [41]. The MBI is considered the gold standard to measure the construct of burnout and its components [42]. The scale has established validity and reliability in English [41] and French [43] and has been used previously with Canadian farmers [14]. The 16-item scale asks participants to rate their thoughts and feelings relating to burnout on a 7-point Likert-type scale from 0 (never) to 6 (every day) [41]. Responses for each of the three subscales (emotional exhaustion, cynicism, and professional efficacy) were scored separately. Higher mean scores for each subscale indicate higher emotional exhaustion, cynicism, or professional efficacy.
2.2.4. Alcohol Use
We used the Alcohol Use Disorders Identification Test (AUDIT) to screen for unhealthy alcohol use. The AUDIT was developed by the World Health Organization (WHO) to measure “alcohol consumption, drinking behaviour, and alcohol-related problems” [44]. It has been validated in English [45] and French [46]. The 10-item scale is scored from 0 to 40, where a score of 0 indicates the respondent has never drank alcohol, 1–7 indicates low risk consumption, 8–14 indicates hazardous/harmful alcohol consumption, and 15–40 indicates likely moderate-severe alcohol use disorder (AUD) [44,47].
2.2.5. Resilience
The Connor Davidson Resilience Scale (CD-RISC) 10-item version was used to investigate resilience. The CD-RISC was developed to measure resilience as “persistence and hardiness” [48]. Though there is no gold standard measure of resilience [49], the CD-RISC is one of the most widely used resilience measures [50] and has been validated in the general population in both English and French [51]. The CD-RISC 25-item version has previously been used with farmers in Canada [15], but the 10-item version has since been recommended for use in research due to superior psychometrics [50]. The measure asks participants to rate their agreement with 10 statements in the past month on a 5-point Likert-type scale from 0 (not true at all) to 4 (true nearly all the time). Higher mean scores indicate greater resilience [51].
2.2.6. Mental Health Impacts of COVID-19 Factors
To measure the perceived impact of various COVID-19-specific factors on participants’ mental health (e.g., social isolation, difficulties getting groceries), we used 15 items from Mental Health Research Canada’s Mental Health During COVID-19 Outbreak polls [3,52] (Table 1). Participants were asked to rate the impact of the 15 factors on their mental health using a 5-point Likert-type scale from 1 (very negative) to 5 (very positive). Each item was individually reported.

Table 1.
Complete list of individual items measuring COVID-19 specific factors, from Mental Health Research Canada’s Mental Health During COVID-19 Outbreak polls [3,52].
2.2.7. Self-Rated Mental Health & Perceived Stability/Change in Mental Health
To assess general self-rated mental health, we used one item from Statistics Canada’s Canadian Survey on COVID-19 and Mental Health. Participants were asked, “In general, how is your mental health?” with response options “Excellent”, “Very good”, “Good”, “Fair”, and “Poor” [53]. Participants who answered either “Excellent” or “Very Good” options were said to have high self-rated mental health [54]. To measure perceived stability/change in mental health, participants answered one item from Statistics Canada’s Canadian Survey on COVID-19 and Mental Health; “Compared to before the COVID-19 pandemic, how would you say your mental health is now?” with response options: “Much better now”, “Somewhat better now”, “About the same”, “Somewhat worse now” and “Much worse now” [53]. Participants who answered “Much better now”, “Somewhat better now”, or “About the same” were said to have stable/improved mental health [54].
2.2.8. Community Belonging & Perceived Stability/Change in Community Belonging
To investigate community belonging, we used one item from Statistics Canada’s Canadian Survey on COVID-19 and Mental Health. Participants were asked, “How would you describe your sense of belonging to your local community?” with response options “Very strong”, “Somewhat strong”, “Somewhat weak”, and “Very weak” [53]. Participants with high community belonging included those who answered “Very strong” or “Somewhat strong” [54]. To measure perceived stability/change in community belonging, participants answered one item developed by the researchers to match the item measuring stable/improved mental health from Statistics Canada’s Canadian Survey on COVID-19 and Mental Health; “Compared to before the COVID-19 pandemic, how would you say your sense of belonging to your local community is now?” with response options: “Much better now”, “Somewhat better now”, “About the same”, “Somewhat worse now” and “Much worse now”.
2.2.9. Help Seeking during COVID-19
To investigate help seeking during COVID-19, participants answered one item from Statistics Canada’s Canadian Survey on COVID-19 and Mental Health; “Have you accessed any resources (on the internet, via phone, or in-person) to help you manage your emotions, mental health, or use of alcohol or drugs during the COVID-19 pandemic?” with response options of “Yes” or “No” [53].
2.3. Sample Size
A minimum required sample size of 385 was calculated using a conservative a priori prevalence estimate of 50%, an allowable error of 5%, and a confidence level of 95%.
2.4. Statistical Analyses
We used descriptive statistics (means, standard deviations (SD), percentages, tertiles) of participant demographics to examine the data. To increase statistical power, person-mean imputation was used to account for missing data in validated scales (GAD-7, PHQ-9, CD-RISC, PSS, MBI, AUDIT) if only one response was missing [55]; if a participant was missing two or more responses to a scale/subscale, they were omitted from analysis of that scale/subscale. For the validated scales used (GAD-7, PHQ-9, CD-RISC, PSS, MBI, AUDIT), participants’ total scores were calculated, and scores were categorized according to each scale’s manual. As the data were normally distributed, Chi-square tests were used to compare proportions and t-tests were used to compare means between genders and to test comparisons of the 2021 survey data to population norms and 2016 survey data, where available. Results were also compared to Mental Health Research Canada’s Mental Health During COVID-19 Outbreak poll 6 (collected April 20 to 28, 2021), and Statistics Canada’s Canadian Survey on COVID-19 and Mental Health cycle 2 (collected February to May 2021), where noted. Statistical significance was set to p < 0.05. All statistical analyses were conducted using R version 4.1.1.
3. Results
3.1. Study Population
A total of 1167 farmers participated in the study. As participants were not required to answer any questions beyond consent, the sample size differed throughout the survey as noted (range n = 948–1167). The average age of participants (n = 968) was 49.3 years (SD 13.7; IQR 38–60; range 20–93). The majority (70.6%, n = 824) of participants chose to complete the survey in English, and 60.7% of participants were men (n = 565). Additional details of the sample population are presented in Table 2.

Table 2.
Demographics of study participants (February–May 2021) (n = 1167), and Canadian farmers from the 2021 Census of Agriculture (n = 262,642) [56].
3.2. Prevalence of Mental Health Outcomes
Mean scale scores, comparisons by gender, and comparisons to each scale’s normative population data are presented in Table 3.

Table 3.
Descriptive statistics (n, mean, standard deviations) for each validated scale used for the overall 2021 sample and by gender, and with comparisons to scale population norms and 2015/2016 survey data, where available.
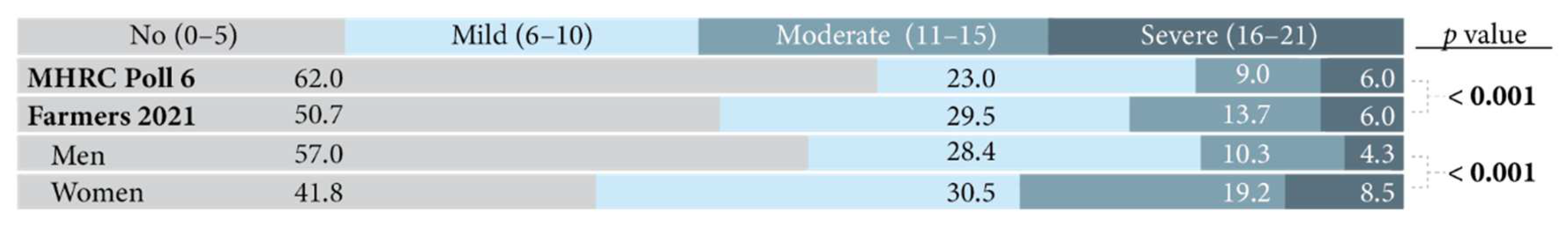
3.2.1. Anxiety
The average GAD-7 score for 2021 farmers was 6.12 (SD 4.88) and was significantly higher than the GAD-7 normative population mean (2.97 (3.35); p < 0.001) [32]. A positive screen for GAD, indicated by a score >10 on the GAD-7, was significantly higher in 2021 farmers (26.8%) compared to scores reported for Canadians in Spring 2021 (15.0%, p < 0.001) and Fall 2020 (13.0%, p < 0.001) (Table 4) [57]. Among the 2021 study population, 6% reported scores indicative of symptoms of severe anxiety disorder, consistent with Canadians in Spring 2021 (6%) (Figure 1) [3]. However, significantly more 2021 farmers demonstrated symptoms of moderate and mild anxiety disorder (13.7% and 29.5%, respectively) compared to Canadians in Spring 2021 (9.0% and 23.0%, respectively) [3]. Out of the 2021 participants, women had higher mean GAD-7 scores than men (7.16 vs. 5.45, respectively, p < 0.001), more positive screens for GAD (34.9% vs. 21.0%, p < 0.001), and more women demonstrated symptoms of mild (30.5%), moderate (19.2%), and severe GAD (8.5%) than men (28.4%, 10.3%, and 4.3% respectively; p < 0.001).

Table 4.
Prevalence of positive GAD screen (GAD-7 score >10) for the overall 2021 sample and by gender, and in comparison to Canadian general population from Statistics Canada’s Survey of COVID-19 and Mental Health (SCMH) cycles 1 (Spring 2020) and 2 (Fall 2021) [57].
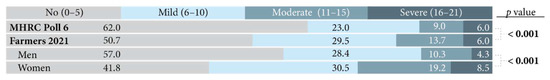
Figure 1.
Classification of no, mild, moderate, and severe anxiety disorder symptoms for overall 2021 sample and by gender, in comparison to the Canadian general population during COVID-19 from Mental Health Research Canada’s (MHRC) Mental Health During COVID-19 Outbreak poll 6.
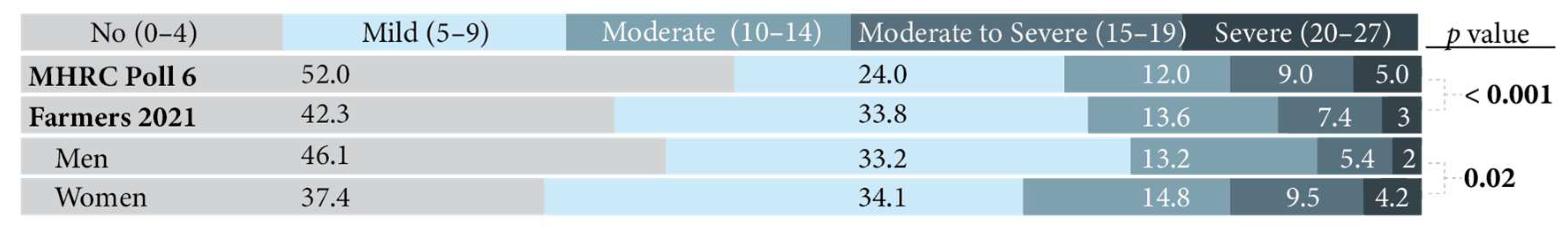
3.2.2. Depression
The mean PHQ-9 score for 2021 farmers was 5.89 (SD 5.27), which was significantly higher than the PHQ-9 general population scale norm (2.91, p < 0.001) [37]. The prevalence of a positive MDD screen (i.e., PHQ-9 score >10) was significantly higher in 2021 farmers (23.6%) than Canadians in the Spring of 2021 (19.0%, p < 0.001), Canadians in the Fall of 2020 (15.2%, p < 0.001), and Canadians prior to the pandemic (6.7%, p < 0.001) (Table 5) [58]. Fewer 2021 farmers demonstrated symptoms of severe (2.8% vs. 5.0%) and moderate to severe depressive disorder (7.4% vs. 9.0%) than Canadians in Spring 2021, but more 2021 farmers demonstrated symptoms of moderate (13.6% vs. 12.0%) and mild depressive disorder (33.8% vs. 24.0%) than Canadians in Spring 2021 (Figure 2) [3]. The mean PHQ-9 score in 2021 farmers was significantly higher for women (6.87) than for men (5.25, p < 0.001). Of the 2021 participants, women also had a higher prevalence of positive MDD screens than men (28.1% vs. 20.5%), and more women demonstrated symptoms of mild, moderate, moderate to severe, and severe depressive disorder than men (p = 0.02).

Table 5.
Prevalence of positive MDD screen (PHQ-9 score >10) for the overall 2021 sample and by gender, and in comparison to Canadian general population from Statistics Canada’s Survey of COVID-19 and Mental Health (SCMH) cycles 1 (Spring 2020) and 2 (Fall 2021) and prior to the pandemic from Canadian Community Health Survey (CCHS) data (2015–2019) [57].
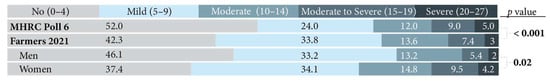
Figure 2.
Classification of no, mild, moderate, moderate to severe, and severe depressive disorder symptoms for overall 2021 sample and by gender, in comparison to the Canadian general population during COVID-19 from Mental Health Research Canada’s (MHRC) Mental Health During COVID-19 Outbreak poll 6.
3.2.3. Perceived Stress
The average PSS score of the 2021 farmers was 18.72 (SD 7.03), which is significantly higher than the normative population mean (13.0, (SD 6.34); p < 0.001) [59], but not significantly different from the 2016 sample mean (18.9 (4.9); p = 0.48) [15]. Of the 2021 participants, the mean PSS score for women (20.46, SD 6.98) was significantly higher than that for men (17.46, SD 7.15). The mean PSS scores for man and woman genders in the 2021 sample (17.46 and 20.46) were significantly higher than the normative population means (13.7, SD 6.60 and 12.1, SD 5.90; p < 0.001) [59]. The mean PSS scores of women were not significantly different between the 2021 and 2016 farming samples (p = 0.44), but the mean PSS scores of men were significantly lower in the 2021 sample (17.46, SD 7.15) compared to the 2016 sample (18.3, SD 4.9; p = 0.02), although this difference is small (0.84 points) [15].
3.2.4. Burnout
The average emotional exhaustion, cynicism, and professional efficacy subscale scores of the 2021 participants were 2.64 (1.62), 2.20 (1.45), and 4.70 (1.11), respectively. The emotional exhaustion and cynicism subscale means were significantly higher in the 2021 participants than normative population means (2.26 (1.47) and 1.74 (1.36); p < 0.001) [41]. The professional efficacy subscale mean was significantly higher in the 2021 sample than the normative population mean (4.34 (1.17); p < 0.001) [41], but significantly lower than the 2016 sample mean (4.85 (1.01); p = 0.001) [14]. Emotional exhaustion and cynicism subscale means did not significantly differ between the 2021 and 2016 farming samples. Within the 2021 participants, the mean emotional exhaustion subscale score of women (2.92, SD 1.62) was significantly higher than that of men (2.46, SD 1.60; p = 0.02), although this difference was small (0.9 points).
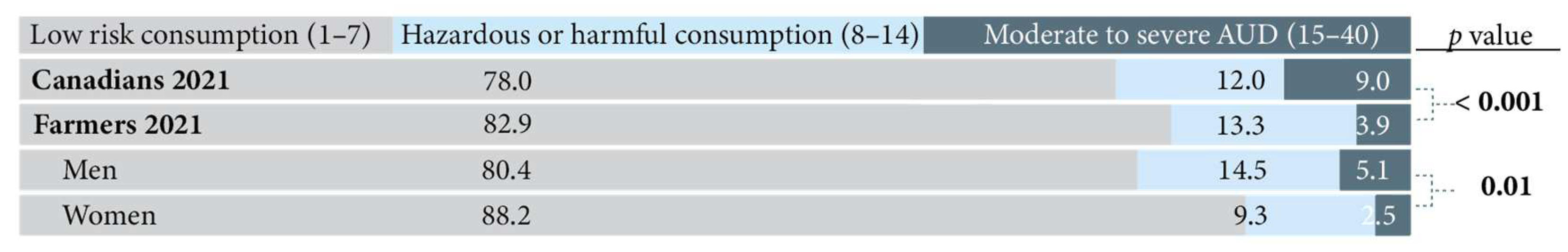
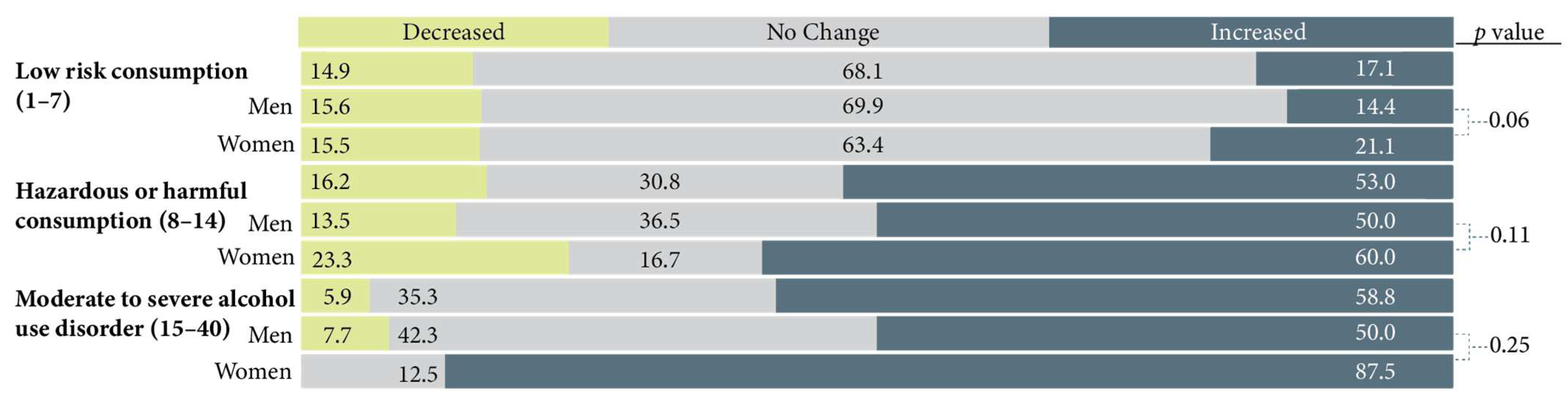
3.2.5. Alcohol Use
Participants in 2021 had significantly higher mean AUDIT scores (4.46) than the general population (3.61, p < 0.001) [60], reflecting higher alcohol consumption and related problems. Fewer farmers in 2021 were classified as having moderate to severe Alcohol Use Disorder (AUD) (3.9%) than Canadians in Fall 2020 (9.0%) [61], but more farmers in 2021 were classified as exhibiting hazardous or harmful alcohol consumption (13.3%) than Canadians (12.0%) in Fall 2020 (Figure 3) [61]. Within the 2021 sample, men had higher mean AUDIT scores than women (4.86 vs. 3.73, p < 0.001), and significantly more farming men were classified as having hazardous or harmful consumption or moderate to severe alcohol use disorder than farming women (p = 0.01). However, the 2021 farming men’s mean AUDIT scores did not significantly differ from the general population (p = 0.06), whereas the 2021 farming women’s mean AUDIT scores were significantly higher than women in the general population (3.73 vs. 2.71, p < 0.001) [60].
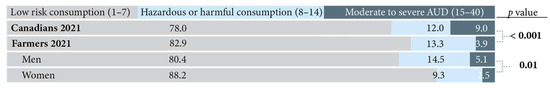
Figure 3.
Classification of low risk consumption, hazardous or harmful consumption, and moderate to severe alcohol use disorder (AUD) for the overall 2021 sample and by gender, in comparison to the Canadian general population during COVID-19 from the Canadian Centre on Substance Use and Addiction and Mental Health Commission of Canada’s Mental Health and Substance Use During COVID-19 survey.
3.2.6. Resilience
The mean CD-RISC score of the 2021 sample was 24.7 (SD 6.2), which was significantly lower than the mean CD-RISC score in the general population (31.8, SD 5.4, p < 0.001) [62]. Within the 2021 sample, the mean CD-RISC score of women (24.1) was significantly lower than that of men (25.0, p = 0.02), although this difference was small (0.9 points). Approximately 83.4% of participants in 2021 had CD-RISC scores lower than the reference population norm (<31.8); 92.5% of men and 86.5% of women in the 2021 sample had lower mean CD-RISC scores than the normative population (means of 33.53 and 31.08 versus 25.04 and 24.10, respectively) [62].
3.3. Perceived COVID-19 Impacts on Mental Health Outcomes
3.3.1. Anxiety
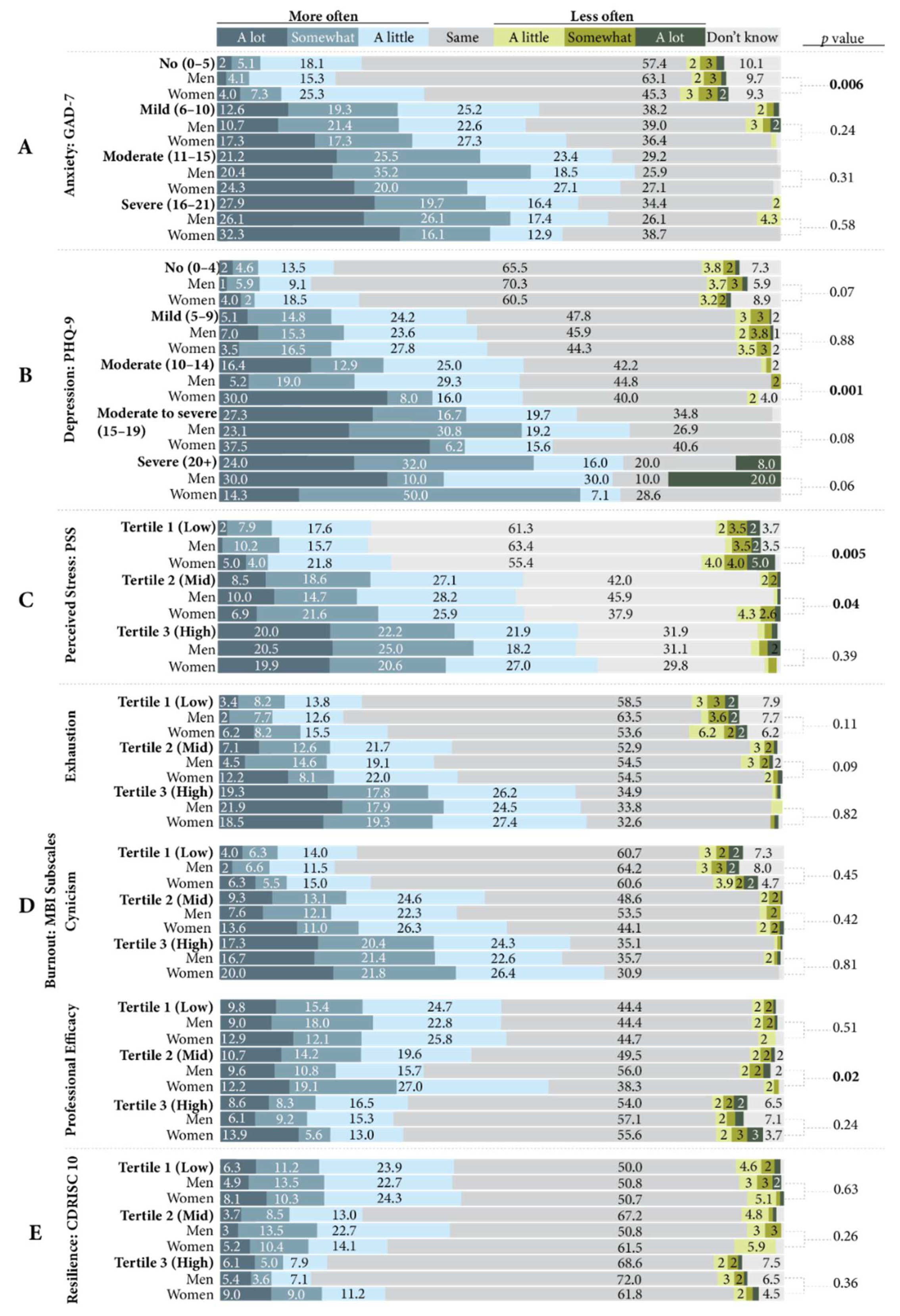
Over half of participants who screened positive for GAD reported experiencing symptoms of anxiety more often since the pandemic began (Figure 4, Block A). Of those who were categorized as likely to have a severe anxiety disorder, 27.9% reported experiencing anxiety symptoms “a lot” more often since the pandemic began. More women than men who were classified as having no likely anxiety disorder reported increased anxiety symptoms since the pandemic began (p = 0.006).
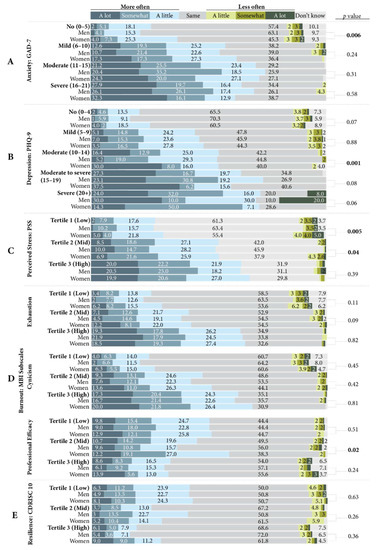
Figure 4.
Perceived change in scale symptoms since the pandemic began by scale classification (Generalized Anxiety Disorder-7 (GAD-7) and Patient Health Questionnaire-9 (PHQ-9) or tertile-Perceived Stress Scale (PSS), Maslach Burnout Inventory–General Survey (MBI), Connor Davidson Resilience Scale-10 (CD-RISC 10)), and comparisons by gender.
3.3.2. Depression
Approximately 54.3% of participants who demonstrated symptoms of moderate depressive disorder, and 63.7% and 72% of participants who demonstrated symptoms of moderate to severe and severe depressive disorder, respectively, reported experiencing more depression symptoms since the pandemic began (Figure 4, Block B). Women who demonstrated symptoms of moderate depressive disorder reported experiencing depression symptoms since the pandemic began significantly more often than men (p = 0.001).
3.3.3. Perceived Stress
Most of the participants who had PSS scores in the mid- and high-tertiles reported feeling increased perceived stress since the pandemic began (54.2% and 64.1%, respectively) (Figure 4, Block C). More women in the low- and mid-tertiles reported feeling perceived stress less frequently since the pandemic began than men (p = 0.005 and p = 0.04, respectively).
3.3.4. Burnout
In all three MBI subscales, most participants reported no change in their symptoms of burnout since the pandemic began (Figure 4, Block D). However, most participants with high emotional exhaustion (63.3%), cynicism (62.0%), and low professional efficacy (49.9%) reported experiencing symptoms of burnout more often since the pandemic began. Women with mid professional efficacy scores reported experiencing symptoms of burnout more often since the pandemic began significantly more than men (58.2% vs. 36.1%, p = 0.02).
3.3.5. Resilience
Most of the participants in all three tertiles of CD-RISC scores reported no change in their levels of resilience since the pandemic began, and no significant gender differences were found (Figure 4, Block E).
3.3.6. Alcohol Use
Perceived change in alcohol consumption since the pandemic began by AUDIT score category are presented in Figure 5. Approximately 3 out of 5 farmers (58.8%) who were classified as having moderate to severe AUD and 1 in 2 farmers (53%) who were classified as exhibiting hazardous or harmful alcohol consumption reported increased alcohol consumption since the pandemic began. No significant gender differences were found regarding the change in alcohol consumption since the pandemic began.
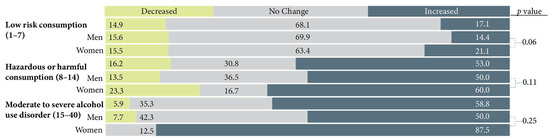
Figure 5.
Perceived change in alcohol consumption since the pandemic began by Alcohol Use Disorder Identification Test (AUDIT) classification and by gender.
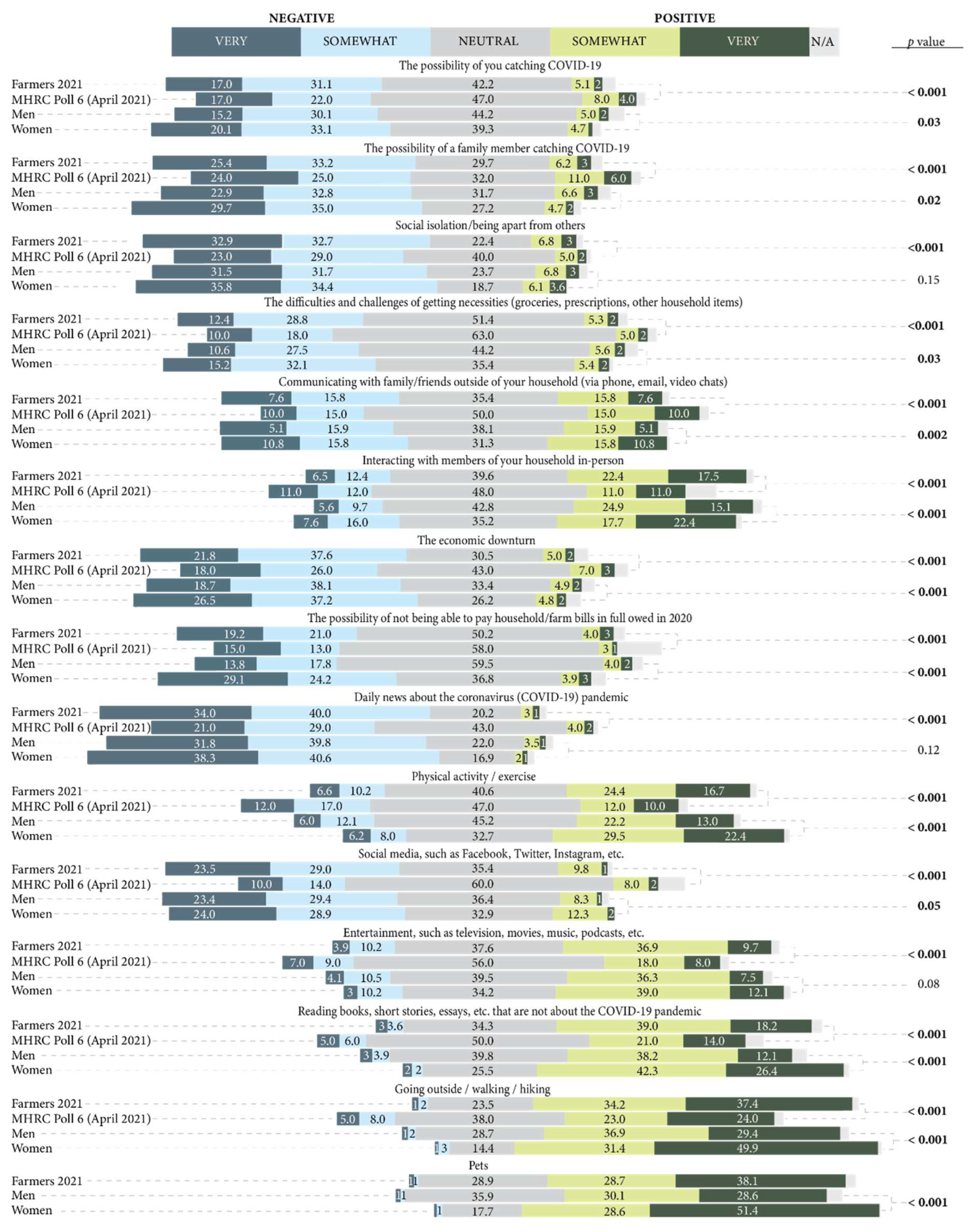
3.4. Impact of COVID-19 Specific Factors on Mental Health
Figure 6 shows the perceived impact of COVID-19 specific factors on participants’ mental health, with comparisons to the Canadian general population in Spring 2021 [3]. The COVID-19 specific factors which most farmers reported to have had a negative impact on their mental health included the possibility of a family member contracting COVID-19, the economic downturn, social media, and social isolation. Social isolation was the leading stressor on the mental health of Canadians, whereas daily news about the COVID-19 pandemic was the leading stressor on the mental health of farmers, where 74% of participants reported a negative impact. Conversely, over 50% of farmers reported many factors as having a positive impact on their mental health, including reading materials that are not related to COVID-19 and pets. Going outside had the most positive impact on both farmers and Canadians’ mental health in Spring 2021 [3].
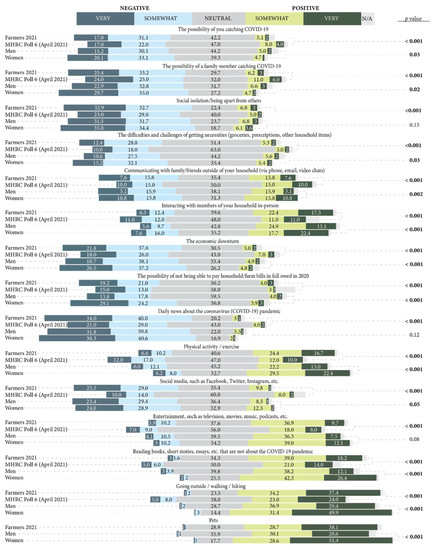
Figure 6.
Perceived impact of COVID-19 specific factors on participants’ mental health in comparison to the general Canadian population during COVID-19 and comparison of the 2021 sample by gender (men and women lines).
More women than men reported difficulties with getting necessities (such as groceries) during the pandemic (p = 0.04) and the possibility of not being able to pay household/farm bills in 2020 (p < 0.001) as having a negative impact on their mental health during the pandemic. Further, more women than men reported physical activity (p < 0.001), reading material not about the COVID-19 pandemic (p < 0.001), going outside (p < 0.001), and pets (p < 0.001) as having a positive impact on their mental health during the pandemic.
3.5. Mental Health and COVID-19
Prevalence of high self-rated mental health and perceived stability/improvement of mental health since the pandemic began are presented in Table 6. Overall, 46.3% of farmers reported high self-rated mental health, which is significantly lower than Canadians in Spring 2021 (51.5%, p = 0.001) and Fall 2020 (59.9%, p < 0.001) [54]. Significantly more men (52.8%) reported high self-rated mental health than women (36.4%, p < 0.001), as well as stable/improved mental health since the pandemic began than women (69.4% vs. 60.3%, p < 0.001). One-third (66%) of farmers reported stable or improved mental health since the pandemic began, which is significantly higher than Canadians in Spring 2021 (58.1%, p < 0.001), but not significantly different from Canadians in Fall 2020 (66.5%, p = 0.72) [54].

Table 6.
Prevalence of high self-rated mental health and perceived stability/improvement in mental health since the pandemic began for the overall 2021 sample and by gender in comparison to the Canadian general population from Statistics Canada’s Survey of COVID-19 and Mental Health (SCMH) cycles 1 (Spring 2020) and 2 (Fall 2021).
3.6. Community Belonging during COVID-19
Table 7 presents the prevalence of perceived high community belonging and perceived stability/improvement in community belonging since the pandemic began. Overall, 66% of farmers reported high community belonging, which is significantly higher than Canadians in Spring 2021 (57.3%, p < 0.001), but not significantly different from Canadians in Fall 2020 (63.7%, p = 0.13) [54]. There were no significant gender differences within the farming sample, or between farming women and Canadian women in Spring 2021 or Fall 2020 [54]. However, 69.6% of farmers who identified as men reported high community belonging, which is significantly higher than Canadian men in Spring 2021 (58.2%, p < 0.001) and Fall 2020 (63.8%, p = 0.004) [54]. Seven in 10 (71.3%) farmers reported stable or improved community belonging since the pandemic began, and there were no significant gender differences.

Table 7.
Prevalence of high self-rated community belonging and perceived stability/improvement in community belonging since the pandemic began for the overall 2021 sample and by gender in comparison to the Canadian general population from Statistics Canada’s Survey of COVID-19 and Mental Health (SCMH) cycles 1 (Spring 2020) and 2 (Fall 2021).
3.7. Help Seeking during COVID-19
Approximately 1 in 5 (20.9%, n = 967) participants accessed any resources to help them manage their emotions, mental health, or use of alcohol or drugs during the COVID-19 pandemic. Notably, a significant gender difference was observed, as 32.3% of women sought help during the pandemic compared to 13.7% of men (p < 0.001).
4. Discussion
We conducted a national, online, cross-sectional survey of Canadian farmers (February–May 2021) using validated scales of generalized anxiety disorder (GAD-7), major depressive disorder (PHQ-9), perceived stress (PSS), burnout (MBI), alcohol use disorder (AUDIT), and resilience (CD-RISC), and perceived changes in these outcomes during the pandemic. Data were also collected on the impact of COVID-19 specific social and economic factors on mental health, help-seeking, and sense of community belonging through the pandemic.
4.1. Comparisons to 2016 Sample
The second National Survey of Farmer Mental Health in Canada builds upon the first national survey in 2015/16 [14,15], expands our knowledge through the addition of psychometric scales (e.g., coping, alcohol use), and adds important insights on the differential experiences of mental health by gender and the impacts of the COVID-19 pandemic on farmers’ mental health. The results from the 2015/16 national survey were generally agreed upon by farmers, agricultural organizations, industry, government, and mental health professionals as concerning and sparked considerable attention and discussion in Canadian agriculture. Regrettably, the 2021 survey data continue to document significant concerns with farmer mental health in Canada. Consistent with the 2016 survey results, farmers scored more severely on all mental health outcome measures than the general population. Farmers had higher mean scores for anxiety (GAD-7), depression (PHQ-9), perceived stress (PSS), and emotional exhaustion and cynicism MBI subscales, and lower resilience (CD-RISC) scale scores than scale norms. Because we used different scales in the 2021 survey than the 2016 survey to measure anxiety (GAD-7 vs. Hospital Anxiety and Depression Scale; HADS), depression (PHQ-9 vs. HADS), and resilience (CD-RISC 10-item vs. 25-item version), we cannot reliably compare results between the 2016 and 2021 samples. Notably, in 2016, farmers’ mean anxiety and depression subscale scores from the HADS were also significantly higher than scale norms, and farmers’ mean resilience (CD-RISC) scores on the CD-RISC 25-item version were also significantly lower than scale norms. Identical measures were used in both administrations of the survey for perceived stress (PSS) and burnout (MBI), and in both scales, no significant differences were observed between the overall 2021 and 2016 samples, other than the mean professional efficacy subscale score of the MBI was significantly lower in the 2021 sample than the 2016 sample (0.15 points difference). Therefore, although mental health awareness campaigns and mental health literacy programs within the agricultural sector have increased since the 2016 survey, we cannot report any improvement in population-level mental health outcomes in farmers since the first survey administration. However, it is possible that the mental health awareness campaigns have led farmers to become more self-aware of their mental health concerns to report them in this survey more accurately than in the 2016 survey. Regardless, greater efforts are needed to improve the mental health of Canadian farmers. National efforts must move beyond the awareness level to implement mental health (e.g., positive psychology training) and mental illness interventions that are developed for the agricultural context and are delivered by mental health professionals with experience or understanding in agriculture to meet farmers’ specific needs [18].
4.2. Comparisons to Canadians during COVID-19
Because national mental health polling was prioritized by Statistics Canada and Mental Health Research Canada throughout COVID-19, we could compare our results to nationally representative samples collected around the same time as our survey was active. Interestingly, more Canadians scored in the most severe categories, but more farmers scored in the moderate/harmful categories of anxiety (GAD-7), depression (PHQ-9), and alcohol use (AUDIT). A similar observation in the burnout data was made. Burnout is a syndrome characterized by high emotional exhaustion, high cynicism, and low professional efficacy. Interestingly, while farmers scored higher in emotional exhaustion and cynicism, they also scored higher in professional efficacy than the reference population. Hence, despite feelings of emotional exhaustion and the feeling of “indifference or a distant attitude towards work” that is associated with cynicism, participants nevertheless reported feelings of effectiveness at work and confidence in being “effective in getting things done” [41]. This observation of high emotional exhaustion and cynicism without low professional efficacy is likely indicative of participants being in a transitional state towards burnout (e.g., overextended profile) [63]. The findings of high/moderate classifications but not severe ones for anxiety (GAD-7, depression (PHQ-9), and alcohol use (AUDIT) may be explained by our participation requirements. Because we sampled those who currently identify as a farmer, our sample likely includes a higher proportion of people whose mental health or substance use concerns do not compromise their ability to remain in farming. Further in-depth qualitative research would be useful to investigate whether severe anxiety, depression, substance use, or burnout contribute to farmers leaving the profession–a notable decision for farmers who often view farming as a lifestyle rather than an occupation and are therefore less likely to consider changing occupations [64].
4.3. COVID-19 Impacts
Unsurprisingly, the pandemic was perceived to exacerbate issues with high stress, anxiety, depression, emotional exhaustion, cynicism, and alcohol use. Participants with high anxiety, depression, perceived stress, emotional exhaustion, and cynicism scores, and low resilience and professional efficacy scores, reported an increase in these symptoms since the beginning of the pandemic. This is consistent with national mental health polling, which reports worsening symptoms of anxiety and depression over the course of the pandemic [3,57], likely due to cumulative pandemic stressors [1] and in relation to severity of public health safety measures [65]. Further analyses are required to determine how the pandemic might have influenced the comorbidity of mental health outcomes in this sample. Brotto et al. (2021) found a relationship between increased alcohol consumption and symptoms of anxiety and depression during the pandemic, with the highest association between November 2020–March 2021 than any prior phase of the pandemic or prior to the pandemic [65]. Notably, many participants reported increased alcohol consumption since the pandemic began, which reflects a global trend of increased substance use during the pandemic, particularly during or following periods of high public health restrictions [66].
Because this is a cross-sectional study, we cannot determine whether the negative mental health outcomes we observed during the pandemic are more attributable to farming stressors and/or pandemic stressors, and/or their interactions. Although farmers perceived the pandemic to worsen mental health outcomes, farmers had significantly poorer self-rated mental health than Canadians in Spring 2021, and more farmers than Canadians reported stable or improved mental health since the pandemic began. We also know farmers scored more severely than the general population across mental health outcomes prior to the pandemic [15]. Additionally, community belonging may have been a protective factor for farmers’ mental health during the pandemic. Most farmers reported stable or increased community belonging since the pandemic began, and farmers, specifically farming men, reported higher community belonging than Canadians in Spring 2021. Strong community ties and high sense of belonging has been characteristic of rural communities in Canada prior to the pandemic [67], and community belonging is associated with strong mental health [67], feeling supported in times of change [68], and has been found to be a protective factor for Major Depressive Disorder during the pandemic [58]. Finally, our results suggest several occupational factors protected farmers’ mental health during the pandemic. For example, going outside was the COVID-19 related factor with the most positive impact on farmers’ mental health. The decline in mental health in the general population during the pandemic has been partly attributed to the decrease in opportunities for physical activity due to public health restrictions such as stay-at-home orders [69], and exposure to nature has been found to prevent the negative mental health implications of public health restrictions, including stay-at-home orders [70]. Fortunately, farmers often live on their farms and many farming activities are done outdoors, therefore, farmers may not have been as impacted by public health restrictions, and farmers’ mental health likely benefitted from being in nature during the pandemic. On the other hand, the COVID-19 related factor with the most negative impact on farmers’ mental health was daily COVID-19 news. Indeed, following the COVID-19 news closely has been associated with greater psychological distress [71]; however, during Spring 2021, social isolation was the leading COVID-19 stressor on Canadians’ mental health [3]. Therefore, although many farmers reported a negative impact of social isolation on their mental health, the socially isolated and outdoor nature of farming may have had a protective effect on farmers’ mental health during the pandemic [72].
4.4. Gender
Our findings raise important gender-based concerns and call for additional research and action to support the implementation of gender-based mental health programming in agriculture. In our sample, women scored more severely on measures of anxiety, depression, stress, and emotional exhaustion than men. This finding has been observed internationally and within Canada-women, regardless of sociodemographic characteristics (e.g., age, ethnicity) have consistently scored higher on measures of anxiety, depression, stress, loneliness throughout the pandemic [65]. Unsurprisingly, farming women also scored more severely on these measures compared to Canadian women during the pandemic. In addition to the occupational factors which might explain this finding, the poorer mental health of farming women compared to farming men may be due to women taking on disproportionate childcare duties during school closures, as the pandemic has led to more traditional gender roles in the agricultural industry [73].
Notably, no participants identified as nonbinary/gender-diverse in response to our open-ended gender question. Unfortunately, the gender distribution of farmers in Canada is unknown, because the Canadian Census of Agriculture collects data on sex instead of gender [74]. However, we know that mental health concerns are greater in gender-diverse and transgender individuals in the general population during the pandemic [65]. Future research which focuses on the mental health research of farmers who identify as gender-diverse, in addition to other equity-deserving groups like LGBTQIA+, would be helpful.
Over twice as many women reported seeking help for their mental health or substance use than men, highlighting an opportunity to help men decrease perceived barriers to help-seeking. Given our previous finding that farming women score more severely than men across all mental health outcomes, as previously recommended [75], it is important to not interpret higher help-seeking in women as an opportunity to reach farming men for mental health support. To reiterate, farming women are inundated with household and childcare responsibilities on top of their farm work, and women often work off the farm to subsidize farm bills [72]. To add the responsibility of organizing mental health support for men may present an additional burden on their own mental health. Previous qualitative work regarding mental health help-seeking of Canadian farmers [75] and farming men [76] has stressed the importance of mental health resource accessibility. Our findings echo their recommendations for gender-specific strategies to provide mental health supports to farmers.
The objective of this paper was to report prevalence estimates of mental health outcomes amongst farmers in Canada. Given the existing literature reporting gender as a risk factor for mental health concerns during the pandemic and the common gender differences in labour division in farmers in Canada, we also compared outcomes by gender. Comparisons of outcomes by other demographic variables are outside the scope of this article but will be investigated elsewhere.
4.5. Limitations
This is a cross-sectional, retrospective study with a convenience sample. Therefore, we have a snapshot of participants’ mental health and cannot infer causality. There is potential for recall bias because participants were asked to reflect on their mental health over the course of the pandemic. Although randomized sampling would have been ideal, we could not gain access to lists of farmers in Canada for research purposes. Our study sample was also limited to those who had access to internet, were members of an agricultural organization or were connected to agricultural social media. Hence, sampling bias may limit the generalizability of this sample to the total Canadian farming population. While this is the second national survey of farmer mental health in Canada, it is not a longitudinal study. Because responses were collected anonymously, we are unable to determine how many farmers participated in both the 2016 and 2021 surveys or to make intra-individual comparisons. We observed gendered differences in mental health outcomes, with women faring worse overall than men in our sample, however, it is possible that men underreported or did not experience the specific symptoms included in the scales despite having mental health concerns [77,78]. We strongly encourage future investigations of farmers’ mental health and gender. Finally, the survey was conducted strategically to be at a time of year with low farming stress (prior to planting season) to increase likelihood of participation. However, it is likely that farming stressors would increase over the planting and harvesting seasons for crop farmers, and during the extreme hot and cold seasons for livestock farmers; hence, our estimates may be underestimated for the yearly average.
4.6. Implications
We emphasize the importance of implementing national mental health interventions for Canadian farmers beyond awareness campaigns. Accessible and affordable mental health services delivered by mental health professionals with experience in agriculture, such as the Farmer Wellness Initiative in Ontario [79], address many of the barriers to help-seeking farmers in Canada have previously identified [75]. Mental illness interventions, such as the Farmer Wellness Initiative in Ontario, and mental health promotion programs, like the Ripple Effect intervention for suicide stigma reduction [80], and the Campfire platform delivered by the National Centre for Farmer Health in Australia [81] are needed at the national scale.
Given the low scores for resilience observed in this study, implementing positive psychology interventions in farming populations as a companion to tailored mental health services may be useful for universal mental health promotion. There is evidence that online positive psychology interventions have been effective during the pandemic to strengthen the resilience during stay-at-home orders or social distance requirements [82,83] and with frontline workers [84]. Additionally, positive psychology interventions are recommended for use in the public health context as the first step in a stepped care approach and are also effective when delivered in a self-directed, online format [85,86] and through phone apps [87]. Given the recent prioritization of high speed internet access for people living in rural and remote areas of Canada [88], online delivery of interventions may become preferable for farmers in the future due to their convenience and anonymity [75].
Although this survey was conducted in the context of COVID-19 and pandemic stressors were measured, we caution against solely attributing our findings to the pandemic, as it is likely that the pandemic exacerbated existing mental health concerns related to farming stressors. Indeed, we did not observe any improvement in mental health outcomes between 2016 and 2021 despite knowledge of mental health awareness and literacy efforts within the agricultural sector. Finally, further research investigating how farming affects mental health differently by gender will be helpful to improve existing farmer mental health resources and develop necessary gender-specific resources.
5. Conclusions
Overall, the findings from the second National Survey of Farmer Mental Health reflect significant concerns with the mental health and well-being of farmers in Canada. Farmers scored higher on measures of anxiety and depression than the Canadian general population during COVID-19, and scored higher on measures of perceived stress, emotional exhaustion and cynicism (two components of burnout) and alcohol use, and lower on resilience, than population norms prior to COVID-19. Participants perceived the COVID-19 pandemic as detrimental to their mental health, as participants identified specific COVID-19 variables which negatively impacted their mental health, and reported experiencing symptoms of anxiety, depression, perceived stress, emotional exhaustion, and cynicism more often since the pandemic began. Notably, participants who identified as women scored more severely on measures of anxiety, depression, perceived stress, and emotional exhaustion than farming men and Canadian women. While great strides have been made in terms of awareness and programming since the first cycle of this survey was conducted in 2016, the data suggest that we must further expand our efforts to include accessible, gender-specific mental health resources tailored for farmers and available nationally. Additionally, future research is encouraged to develop positive psychology interventions for protection against daily farming stressors and prevent negative mental health impacts of future pandemics or farming catastrophes.
Author Contributions
Conceptualization, A.J.-B., B.N.M.H. and R.T.; methodology, A.J.-B., B.N.M.H., and R.T.; formal analysis, R.T., B.N.M.H., and A.J.-B.; investigation, A.J.-B., B.N.M.H., and R.T.; resources, A.J.-B., B.N.M.H., and R.T.; writing—original draft preparation, R.T.; writing—review and editing, R.T., A.J.-B., B.N.M.H., C.B.W., M.N.L., and B.G.; supervision, A.J.-B., B.N.M.H., C.B.W., M.N.L., and B.G.; project administration, A.J.-B.; funding acquisition, A.J.-B. and B.N.M.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Agriculture and Agri-Food Canada. Rochelle Thompson was funded by an Ontario Veterinary College graduate scholarship.
Institutional Review Board Statement
The study methodologies were approved by the University of Guelph Research Ethics Board (REB#21-01-001).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data sharing is not applicable to this article because the research participants did not consent to data sharing.
Acknowledgments
We would like to thank participating farmers for sharing their thoughts, feelings, and information with us for this study. We are deeply grateful for what we have learned from all the farmers in our lives, including the knowledge shared by our stakeholder working group in the years leading up to this study.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Goldmann, E.; Galea, S. Mental health consequences of disasters. Annu. Rev. Public Health 2014, 35, 169–183. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 pandemic mental health trajectories: Patterns from a sample of Canadians primarily recruited from Alberta and Ontario. Available online: https://psycnet.apa.org/record/2022-26090-001 (accessed on 3 September 2022).
- Mental Health Research Canada. National Polling: COVID-19—Mental Health Research Canada. 2021. Available online: https://www.mhrc.ca/national-polling-covid (accessed on 1 December 2020).
- Ijaz, M.; Yar, M.K.; Badar, I.H.; Ali, S.; Islam, M.; Jaspal, M.H.; Hayat, Z.; Sardar, A.; Ullah, S.; Guevara-Ruiz, D. Meat production and supply chain under COVID-19 scenario: Current trends and future prospects. Front. Vet. Sci. 2021, 432, 660736. [Google Scholar] [CrossRef]
- Canadian Agricultural Human Resource Council. Understanding the Effects of COVID-19 on Canada’s Agricultural Workforce; Canadian Agricultural Human Resource Council: Gloucester, ON, Canada, 2021. [Google Scholar]
- Chenarides, L.; Richards, T.J.; Rickard, B. COVID-19 impact on fruit and vegetable markets: One year later. Can. J. Agric. Econ. Rev. Can. D’agroeconomie 2021, 69, 203–214. [Google Scholar] [CrossRef]
- Fraser, D.C. Bibeau Vows Clarity Soon on Temporary Worker Rules. The Western Producer. 2021. Available online: https://www.producer.com/digital-edition/the-western-producer_2021-12-23/ (accessed on 13 September 2022).
- Rude, J. COVID-19 and the Canadian cattle/beef sector: A second look. Can. J. Agric. Econ. Rev. Can. D’agroeconomie 2021, 69, 233–241. [Google Scholar] [CrossRef]
- White, E.; Producers Face Increased Uncertainty as Seeding Begins. The Western Producer. 2021. Available online: https://www.producer.com/markets/producers-face-increased-uncertainty-as-seeding-begins/ (accessed on 30 March 2022).
- Canadian Food Inspection Agency. Canada, United States Agree on Protocil to Guide Bilateral Trade if African Swine Fever is Detected in Wild Pigs. 16 March 2021. Available online: https://www.canada.ca/en/food-inspection-agency/news/2021/03/canada-united-states-agree-on-protocol-to-guide-bilateral-trade-if-african-swine-fever-is-detected-in-wild-pigs.html (accessed on 30 March 2021).
- Arnason, R.; Climatologists Ring Drought Alarm. The Western Producer. 2021. Available online: https://www.producer.com/news/climatologists-ring-drought-alarm/ (accessed on 30 March 2022).
- Peleshaty, A. ‘Extreme Drought’ Expands in Prairies. The Western Producer. 2021. Available online: https://www.producer.com/news/extreme-drought-expands-in-prairies/ (accessed on 30 March 2022).
- Jia, Z.; Xu, S.; Zhang, Z.; Cheng, Z.; Han, H.; Xu, H.; Wang, M.; Zhang, H.; Zhou, Y.; Zhou, Z. Association between mental health and community support in lockdown communities during the COVID-19 pandemic: Evidence from rural China. J. Rural Stud. 2021, 82, 87–97. [Google Scholar] [CrossRef]
- Jones-Bitton, A.; Hagen, B.; Fleming, S.J.; Hoy, S. Farmer burnout in Canada. Int. J. Environ. Res. Public Health 2019, 16, 5074. [Google Scholar] [CrossRef]
- Jones-Bitton, A.; Best, C.; MacTavish, J.; Fleming, S.; Hoy, S. Stress, anxiety, depression, and resilience in Canadian farmers. Soc. Psychiatry Psychiatr. Epidemiol. 2020, 55, 229–236. [Google Scholar] [CrossRef]
- Agriculture and Agrifood Canada. Mental Health in Agriculture. 2022. Available online: https://agriculture.canada.ca/en/mental_health (accessed on 30 March 2022).
- Hagen, B. In the Know. 2022. Available online: https://www.ajbresearch.com/in-the-know (accessed on 1 January 2022).
- Hagen, B.N.; Harper, S.L.; O’Sullivan, T.L.; Jones-Bitton, A. Tailored mental health literacy training improves mental health knowledge and confidence among Canadian farmers. Int. J. Environ. Res. Public Health 2020, 17, 3807. [Google Scholar] [CrossRef]
- Santomauro, D.F.; Mantilla Herrera, A.M.; Shadid, J.; Zheng, P.; Ashbaugh, C.; Pigott, D.M.; Abbafati, C.; Adolph, C.; Amlag, J.O.; Aravkin, A.Y.; et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Env. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef] [PubMed]
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020, 7, 883–892. [Google Scholar] [CrossRef]
- Jenkins, E.K.; McAuliffe, C.; Hirani, S.; Richardson, C.; Thomson, K.C.; McGuinness, L.; Morris, J.; Kousoulis, A.; Gadermann, A. A portrait of the early and differential mental health impacts of the COVID-19 pandemic in Canada: Findings from the first wave of a nationally representative cross-sectional survey. Prev. Med. 2021, 145, 106333. [Google Scholar] [CrossRef] [PubMed]
- United Nations. Policy Brief: The Impact of COVID-19 on Women; United Nations: New York, NY, USA, 2020. [Google Scholar]
- Power, K. The COVID-19 pandemic has increased the care burden of women and families. Sustain. Sci. Pract. Policy 2020, 16, 67–73. [Google Scholar] [CrossRef]
- Contzen, S.; Forney, J. Family farming and gendered division of labour on the move: A typology of farming-family configurations. Agric. Hum. Values 2017, 34, 27–40. [Google Scholar] [CrossRef]
- Harth, N.S.; Mitte, K. Managing multiple roles during the COVID-19 lockdown: Not men or women, but parents as the emotional “loser in the crisis”. Soc. Psychol. Bull. 2020, 15, 4347. [Google Scholar] [CrossRef]
- Xiao, J.; Zhao, J.; Luo, Z.; Liu, F.; Greenwood, D. The impact of built environment on mental health: A COVID-19 lockdown perspective. Health Place 2022, 77, 102889. [Google Scholar] [CrossRef]
- Herron, R.V.; Lawrence, B.C.; Newall, N.E.; Ramsey, D.; Waddell-Henowitch, C.M.; Dauphinais, J. Rural older adults’ resilience in the context of COVID-19. Soc. Sci. Med. 2022, 306, 115153. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Löwe, B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. Gen. Hosp. Psychiatry 2010, 32, 345–359. [Google Scholar] [CrossRef]
- Smarr, K.L.; Keefer, A.L. Measures of depression and depressive symptoms: Beck depression Inventory-II (BDI-II), center for epidemiologic studies depression scale (CES-D), geriatric depression scale (GDS), hospital anxiety and depression scale (HADS), and patient health Questionnaire-9 (PHQ-9). Arthritis Care Res. 2011, 63 (Suppl. S11), S454–S466. [Google Scholar]
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Teymoori, A.; Real, R.; Gorbunova, A.; Haghish, E.; Andelic, N.; Wilson, L.; Asendorf, T.; Menon, D.; von Steinbüchel, N. Measurement invariance of assessments of depression (PHQ-9) and anxiety (GAD-7) across sex, strata and linguistic backgrounds in a European-wide sample of patients after Traumatic Brain Injury. J. Affect. Disord. 2020, 262, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Wu, J.; Yu, Z.; Bair, M.J.; Kean, J.; Stump, T.; Monahan, P.O. The patient health questionnaire anxiety and depression scale (PHQ-ADS): Initial validation in three clinical trials. Psychosom. Med. 2016, 78, 716. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Kocalevent, R.-D.; Hinz, A.; Brähler, E. Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry 2013, 35, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. Perceived stress scale. Meas. Stress Guide Health Soc. Sci. 1994, 10, 1–2. [Google Scholar]
- Lee, E.-H. Review of the psychometric evidence of the perceived stress scale. Asian Nurs. Res. 2012, 6, 121–127. [Google Scholar] [CrossRef]
- Lesage, F.-X.; Berjot, S.; Deschamps, F. Psychometric properties of the French versions of the Perceived Stress Scale. Int. J. Occup. Med. Environ. Health 2012, 25, 178–184. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. Maslach Burnout Inventory Manual, 4th ed.; Mind Garden, Inc.: Menlo Park, CA, USA, 2016. [Google Scholar]
- Schutte, N.; Toppinen, S.; Kalimo, R.; Schaufeli, W. The factorial validity of the Maslach Burnout Inventory-General Survey (MBI-GS) across occupational groups and nations. J. Occup. Organ. Psychol. 2000, 73, 53–66. [Google Scholar] [CrossRef]
- Bocéréan, C.; Dupret, E.; Feltrin, M. Maslach Burnout Inventory-General Survey: French validation in a representative sample of employees. SCIREA 2019, 3, 24–41. [Google Scholar]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; De la Fuente, J.R.; Grant, M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef] [PubMed]
- Meneses-Gaya, C.D.; Zuardi, A.W.; Loureiro, S.R.; Crippa, J.A.S. Alcohol Use Disorders Identification Test (AUDIT): An updated systematic review of psychometric properties. Psychol. Neurosci. 2009, 2, 83–97. [Google Scholar] [CrossRef]
- Gache, P.; Michaud, P.; Landry, U.; Accietto, C.; Arfaoui, S.; Wenger, O.; Daeppen, J.B. The Alcohol Use Disorders Identification Test (AUDIT) as a screening tool for excessive drinking in primary care: Reliability and validity of a French version. Alcohol. Clin. Exp. Res. 2005, 29, 2001–2007. [Google Scholar] [CrossRef] [PubMed]
- Saunders, J.B. Scoring the AUDIT. Available online: https://auditscreen.org/about/scoring-audit (accessed on 1 December 2020).
- Campbell-Sills, L.; Stein, M.B. Psychometric analysis and refinement of the connor–davidson resilience scale (CD-RISC): Validation of a 10-item measure of resilience. J. Trauma. Stress Off. Publ. Int. Soc. Trauma. Stress Stud. 2007, 20, 1019–1028. [Google Scholar] [CrossRef]
- Windle, G.; Bennett, K.M.; Noyes, J. A methodological review of resilience measurement scales. Health Qual. Life Outcomes 2011, 9, 8. [Google Scholar] [CrossRef]
- Salisu, I.; Hashim, N. A critical review of scales used in resilience research. IOSR J. Bus. Manag. 2017, 19, 23–33. [Google Scholar] [CrossRef]
- Connor-Davidson Resilience Scale (CD-RISC) Manual. Available online: http://www.connordavidson-resiliencescale.com/CD-RISC%20Manual%2008-19-18.pdf (accessed on 1 December 2020).
- Canada, M.H.R. Mental Health during COVID-19 Outbreak. 2021. Available online: https://www.mhrc.ca/national-polling-covid (accessed on 3 September 2022).
- Statistics Canada. Survey on COVID-19 and Mental Health—Cycle 2. 2021. Available online: https://www23.statcan.gc.ca/imdb/p3Instr.pl?Function=assembleInstr&lang=en&Item_Id=1294613 (accessed on 3 September 2022).
- Capaldi, C.A.; Liu, L.; Ooi, L.L.; Roberts, K.C. Self-rated mental health, community belonging, life satisfaction and perceived change in mental health among adults during the second and third waves of the COVID-19 pandemic in Canada. Health Promot. Chronic Dis. Prev. Can. Res. Policy Pract. 2022, 42, 218–225. [Google Scholar] [CrossRef]
- Van der Heijden, G.J.; Donders, A.R.T.; Stijnen, T.; Moons, K.G. Imputation of missing values is superior to complete case analysis and the missing-indicator method in multivariable diagnostic research: A clinical example. J. Clin. Epidemiol. 2006, 59, 1102–1109. [Google Scholar] [CrossRef]
- Statistics Canada. Canada’s 2021 Census of Agriculture: A Story about the Transformation of the Agriculture Industry and Adaptiveness of Canadian Farmers. 2022. Available online: https://www150.statcan.gc.ca/n1/daily-quotidien/220511/dq220511a-eng.htm (accessed on 11 April 2022).
- Statistics Canada. The Daily: Survey on COVID-19 and Mental Health, February to May 2021. 2021. Available online: https://www150.statcan.gc.ca/n1/daily-quotidien/210927/dq210927a-eng.htm (accessed on 30 March 2022).
- Shields, M.; Tonmyr, L.; Gonzalez, A.; Weeks, M.; Park, S.-B.; Robert, A.-M.; Blair, D.-L.; Macmillan, H.L. Symptoms of major depressive disorder during the COVID-19 pandemic: Results from a representative sample of the Canadian population. Health Promot. Chronic Dis. Prev. Can. 2021, 41, 340–358. [Google Scholar] [CrossRef]
- Cohen, S. Perceived stress in a probability sample of the United States. In The Social Psychology of Health; SAGE: Thousand Oaks, CA, USA, 1988. [Google Scholar]
- Moehring, A.; Rumpf, H.-J.; Hapke, U.; Bischof, G.; John, U.; Meyer, C. Diagnostic performance of the alcohol use disorders identification test (AUDIT) in detecting DSM-5 alcohol use disorders in the general population. Drug Alcohol Depend. 2019, 204, 107530. [Google Scholar] [CrossRef] [PubMed]
- Canadian Centre on Substance Use and Addiction & Mental Health Commission of Canada. Mental Health and Substance Use During COVID-19. 2020. Available online: https://www.ccsa.ca/mental-health-and-substance-use-during-covid-19 (accessed on 3 September 2021).
- Campbell-Sills, L.; Forde, D.R.; Stein, M.B. Demographic and childhood environmental predictors of resilience in a community sample. J. Psychiatr. Res. 2009, 43, 1007–1012. [Google Scholar] [CrossRef] [PubMed]
- Leiter, M.P.; Maslach, C. Latent burnout profiles: A new approach to understanding the burnout experience. Burn. Res. 2016, 3, 89–100. [Google Scholar] [CrossRef]
- Vayro, C.; Brownlow, C.; Ireland, M.; March, S. ‘Farming is not Just an Occupation [but] a Whole Lifestyle’: A qualitative examination of lifestyle and cultural factors affecting mental health help-seeking in Australian farmers. Sociol. Rural. 2020, 60, 151–173. [Google Scholar] [CrossRef]
- Brotto, L.A.; Chankasingh, K.; Baaske, A.; Albert, A.; Booth, A.; Kaida, A.; Smith, L.W.; Racey, S.; Gottschlich, A.; Murray, M.C. The influence of sex, gender, age, and ethnicity on psychosocial factors and substance use throughout phases of the COVID-19 pandemic. PLoS ONE 2021, 16, e0259676. [Google Scholar] [CrossRef]
- Mallet, J.; Dubertret, C.; Le Strat, Y. Addictions in the COVID-19 era: Current evidence, future perspectives a comprehensive review. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 106, 110070. [Google Scholar] [CrossRef]
- Kitchen, P.; Williams, A.; Chowhan, J. Sense of community belonging and health in Canada: A regional analysis. Soc. Indic. Res. 2012, 107, 103–126. [Google Scholar] [CrossRef]
- Looker, E.D. Supportive communities and a sense of belonging in rural and non-rural communities in Canada. J. Rural Community Dev. 2014, 9, 163–180. [Google Scholar]
- Wilke, J.; Hollander, K.; Mohr, L.; Edouard, P.; Fossati, C.; González-Gross, M.; Sánchez Ramírez, C.; Laiño, F.; Tan, B.; Pillay, J.D. Drastic reductions in mental well-being observed globally during the COVID-19 pandemic: Results from the ASAP survey. Front. Med. 2021, 8, 246. [Google Scholar] [CrossRef]
- Ribeiro, A.I.; Triguero-Mas, M.; Santos, C.J.; Gómez-Nieto, A.; Cole, H.; Anguelovski, I.; Silva, F.M.; Baró, F. Exposure to nature and mental health outcomes during COVID-19 lockdown. A comparison between Portugal and Spain. Environ. Int. 2021, 154, 106664. [Google Scholar] [CrossRef]
- Stainback, K.; Hearne, B.N.; Trieu, M.M. COVID-19 and the 24/7 news cycle: Does COVID-19 news exposure affect mental health? Socius 2020, 6, 2378023120969339. [Google Scholar] [CrossRef]
- Pappas, S. COVID-19 Fallout Hits Farmers. American Psychological Association. 2020. Available online: https://www.apa.org/topics/covid-19/farming-communities-stress (accessed on 30 March 2022).
- McKee, A.; Sutherland, L.-A. The Changing Role of Women in Farming, Crofting, and the Agricultural Industry: 2016–2021; The James Hutton Institute & the Rural and Environment Science and Analytical Services Division of the Scottish Government: Aberdeen, Scotland, 2021. [Google Scholar]
- Statistics Canada. Census of Agriculture: Farm and Farm Operator Data Visualization Tool. 2022. Available online: https://www150.statcan.gc.ca/n1/pub/71-607-x/71-607-x2022006-eng.htm (accessed on 1 June 2022).
- Hagen, B.N.; Sawatzky, A.; Harper, S.L.; O’Sullivan, T.L.; Jones-Bitton, A. “Farmers Aren’t into the Emotions and Things, Right?”: A Qualitative Exploration of Motivations and Barriers for Mental Health Help-Seeking among Canadian Farmers. J. Agromedicine 2022, 27, 113–123. [Google Scholar] [CrossRef] [PubMed]
- Roy, P.; Tremblay, G.; Robertson, S. Help-seeking among male farmers: Connecting masculinities and mental health. Sociol. Rural. 2014, 54, 460–476. [Google Scholar] [CrossRef]
- Martin, L.A.; Neighbors, H.W.; Griffith, D.M. The experience of symptoms of depression in men vs women: Analysis of the National Comorbidity Survey Replication. JAMA Psychiatry 2013, 70, 1100–1106. [Google Scholar] [CrossRef]
- Smith, D.T.; Mouzon, D.M.; Elliott, M. Reviewing the assumptions about men’s mental health: An exploration of the gender binary. Am. J. Men’s Health 2018, 12, 78–89. [Google Scholar] [CrossRef]
- Canadian Agricultural Partnership, Canadian Mental Health Association. Ontario Federation of Agriculture. Farmer Wellness Initiative. Available online: https://farmerwellnessinitiative.ca/ (accessed on 20 July 2022).
- Kennedy, A.J.; Brumby, S.A.; Versace, V.L.; Brumby-Rendell, T. The ripple effect: A digital intervention to reduce suicide stigma among farming men. BMC Public Health 2020, 20, 813. [Google Scholar] [CrossRef]
- National Centre for Farmer Health. 2022. Available online: https://farmerhealth.org.au/ (accessed on 15 September 2022).
- “Staying Home–Feeling Positive”: Effectiveness of an on-line positive psychology group intervention during the COVID-19 pandemic. Available online: https://link.springer.com/article/10.1007/s12144-021-01613-x (accessed on 15 September 2022).
- Chilver, M.R.; Gatt, J.M. Six-week online multi-component positive psychology intervention improves subjective wellbeing in young adults. J. Happiness Stud. 2022, 23, 1267–1288. [Google Scholar] [CrossRef]
- ‘Stay Safe-Feel Positive’on the frontline: An online positive psychology intervention for police officers during the COVID-19 pandemic. Available online: https://www.tandfonline.com/doi/full/10.1080/17439760.2021.1975161 (accessed on 15 September 2022).
- Bolier, L.; Haverman, M.; Westerhof, G.J.; Riper, H.; Smit, F.; Bohlmeijer, E. Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health 2013, 13, 119. [Google Scholar] [CrossRef]
- Datu, J.A.D.; Valdez, J.P.M.; McInerney, D.M.; Cayubit, R.F. The effects of gratitude and kindness on life satisfaction, positive emotions, negative emotions, and COVID-19 anxiety: An online pilot experimental study. Appl. Psychol. Health Well-Being 2022, 14, 347–361. [Google Scholar] [CrossRef]
- Howells, A.; Ivtzan, I.; Eiroa-Orosa, F.J. Putting the ‘app’in happiness: A randomised controlled trial of a smartphone-based mindfulness intervention to enhance wellbeing. J. Happiness Stud. 2016, 17, 163–185. [Google Scholar] [CrossRef]
- Innovation Science and Economic Development Canada. High-Speed Internet for all of Canada. 2022. Available online: https://ised-isde.canada.ca/site/high-speed-internet-canada/en (accessed on 5 June 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).