Simulation-Based Education in Trauma Management: A Scoping Review
Abstract
1. Introduction
Goals of This Investigation
2. Materials and Methods
2.1. Data Sources
2.2. Study Selection
2.3. Data Analysis
3. Results
3.1. Characteristics of the Study
3.2. Main Results
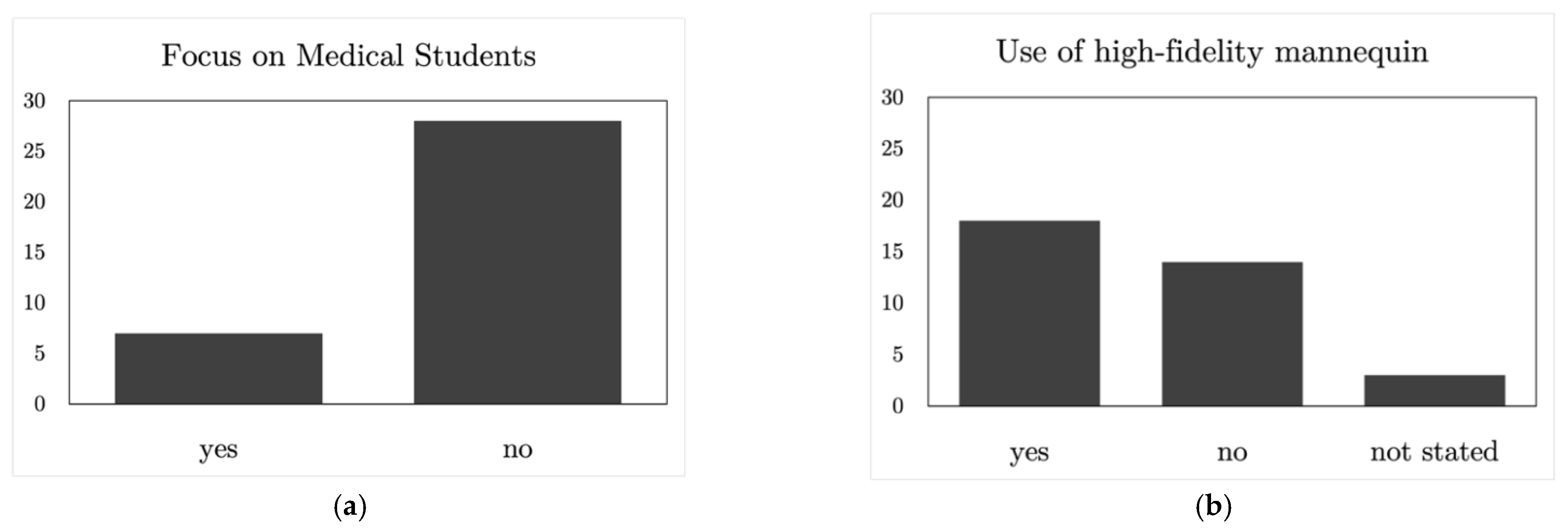
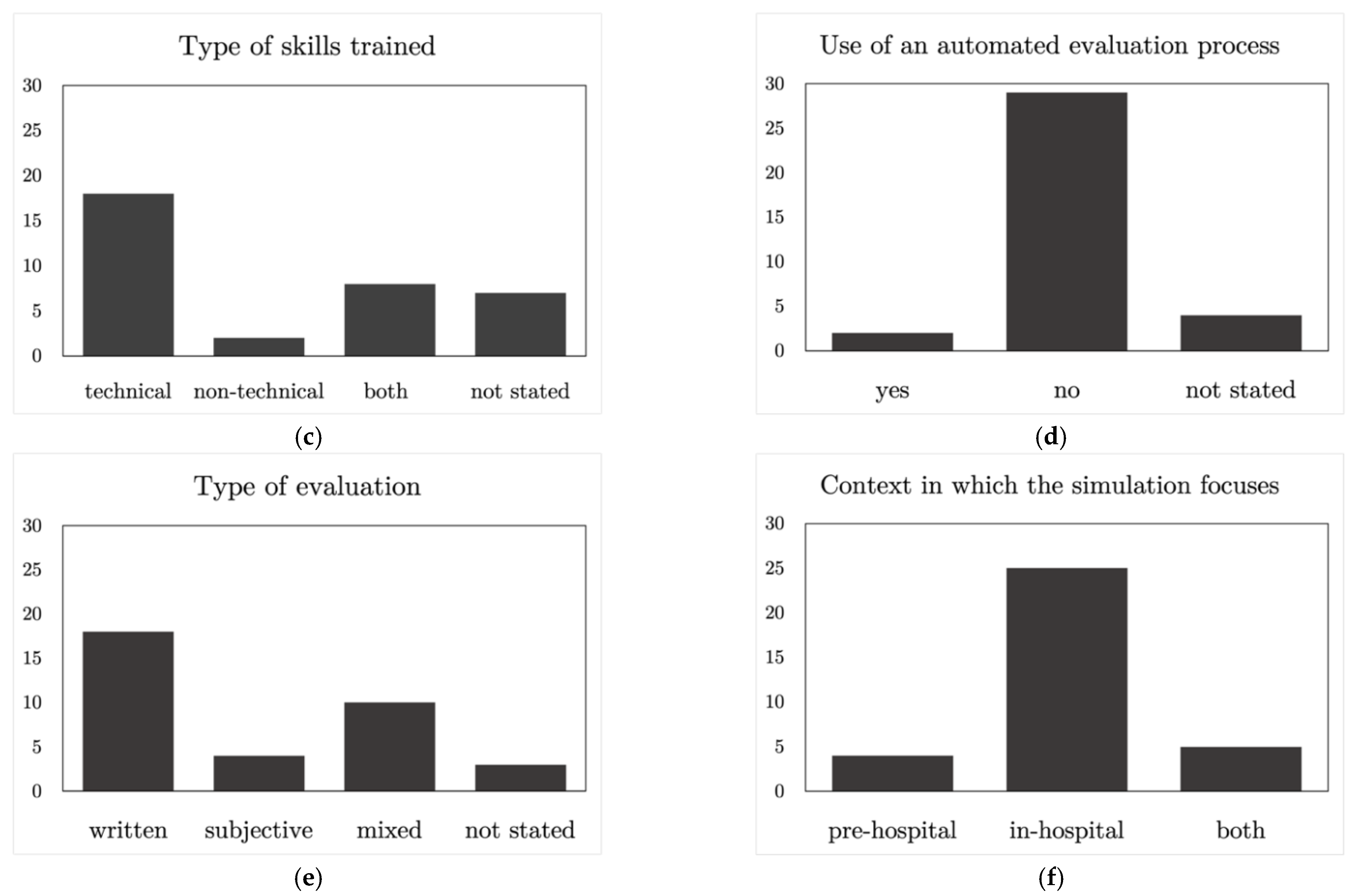
3.2.1. Target Audience of the Training Courses
3.2.2. Simulation Methods Used
3.2.3. Types of Skills Acquired after the Training Courses
3.2.4. Evaluation Methods Used
3.2.5. Context of the Simulations
3.2.6. Limitations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Injuries. 2021. Available online: https://platform.who.int/mortality/themes/theme-details/mdb/injuries (accessed on 2 June 2021).
- Quick, J.A. Simulation Training in Trauma. Mo. Med. 2018, 115, 447–450. [Google Scholar]
- Carmont, M.R. The Advanced Trauma Life Support course: A history of its development and review of related literature. Postgrad. Med. J. 2005, 81, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Gambhir, R.; Agrawal, A. Training in Trauma Management. Med. J. Armed Forces India 2010, 66, 354–356. [Google Scholar] [CrossRef]
- Lin, H.-L.; Chen, C.-W.; Lee, W.-C.; Kuo, L.-C.; Cheng, Y.-C.; Lin, Y.-K.; Lin, J.-N.; Chan, H.-M. Effects of the Emergency Trauma Training Course on the Confidence of Final-Year Medical Students Dealing with Trauma Patients. Kaohsiung J. Med. Sci. 2009, 25, 10–15. [Google Scholar] [CrossRef]
- Shukla, A.; Kline, D.; Cherian, A.; Lescanec, A.; Rochman, A.; Plautz, C.; Kirk, M.; Littlewood, K.E.; Custalow, C.; Srinivasan, R.; et al. A Simulation Course on Lifesaving Techniques for Third-Year Medical Students. Simul. Healthc. J. Soc. Simul. Healthc. 2007, 2, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Ashcroft, J.; Wilkinson, A.; Khan, M. A Systematic Review of Trauma Crew Resource Management Training: What Can the United States and the United Kingdom Learn From Each Other? J. Surg. Educ. 2021, 78, 245–264. [Google Scholar] [CrossRef] [PubMed]
- Mobrad, A.; Al Najjar, A.; Abu Zeid, R.; Atta Aldayes, A. Evaluating the effect of the prehospital trauma life support (PHTLS) course on emergency medical services students’ knowledge. Biomed. Res. 2020, 31, 31–36. [Google Scholar] [CrossRef]
- Häske, D.; Beckers, S.K.; Hofmann, M.; Lefering, R.; Gliwitzky, B.; Wölfl, C.C.; Grützner, P.; Stöckle, U.; Dieroff, M.; Münzberg, M. Quality of Documentation as a Surrogate Marker for Awareness and Training Effectiveness of PHTLS-Courses. Part of the Prospective Longitudinal Mixed-Methods EPPTC-Trial. PLoS ONE 2017, 12, e0170004. [Google Scholar] [CrossRef]
- Ali, J.; Adam, R.; Josa, D.; Pierre, I.; Bedsaysie, H.; West, U.; Winn, J.; Ali, E.; Haynes, B. Effect of basic prehospital trauma life support program on cognitive and trauma management skills. World J. Surg. 1998, 22, 1192–1196. [Google Scholar] [CrossRef] [PubMed]
- Requena, A.; Jimnez, L.; Gmez, R.; del Arco, C. International Trauma Life Support (ITLS) training through the Spanish Society of Emergency Medicine (SEMES): 10 years’ experience with the SEMES-ITLS program. Emergencias 2015, 27, 62–65. [Google Scholar]
- International Trauma Life Support (ITLS); Campbell, J. International Trauma Life Support for Emergency Care Providers; Pearson Education: Harlow, UK, 2013. [Google Scholar]
- Hammond, J. Simulation in critical care and trauma education and training. Curr. Opin. Crit. Care 2004, 10, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, R.; Mytton, O.; Derbrew, M.; Hananel, D.; Heydenburg, M.; Issenberg, B.; Macaulay, C.; Mancini, M.E.; Morimoto, T.; Soper, N.; et al. Training and simulation for patient safety. Qual. Saf. Health Care 2010, 19 (Suppl. 2), i34–i43. [Google Scholar] [CrossRef] [PubMed]
- Datta, R.; Upadhyay, K.; Jaideep, C. Simulation and its role in medical education. Med. J. Armed Forces India 2012, 68, 167–172. [Google Scholar] [CrossRef]
- Borggreve, A.S.; Meijer, J.M.R.; Schreuder, H.W.R.; ten Cate, O. Simulation-based trauma education for medical students: A review of literature. Med. Teach. 2017, 39, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Abelsson, A.; Rystedt, I.; Suserud, B.-O.; Lindwall, L. Mapping the use of simulation in prehospital care—A literature review. Scand. J. Trauma Resusc. Emerg. Med. 2014, 22, 22. [Google Scholar] [CrossRef] [PubMed]
- Murray, D.J.; Freeman, B.D.; Boulet, J.R.; Woodhouse, J.; Fehr, J.J.; Klingensmith, M.E. Decision Making in Trauma Settings. Simul. Healthc. J. Soc. Simul. Healthc. 2015, 10, 139–145. [Google Scholar] [CrossRef]
- Van Dillen, C.M.; Tice, M.R.; Patel, A.D.; Meurer, D.A.; Tyndall, J.A.; Elie, M.C.; Shuster, J.J. Trauma Simulation Training Increases Confidence Levels in Prehospital Personnel Performing Life-Saving Interventions in Trauma Patients. Emerg. Med. Int. 2016, 2016, 5437490. [Google Scholar] [CrossRef]
- Cuisinier, A.; Schilte, C.; Declety, P.; Picard, J.; Berger, K.; Bouzat, P.; Falcon, D.; Bosson, J.L.; Payen, J.-F.; Albaladejo, P. A major trauma course based on posters, audio-guides and simulation improves the management skills of medical students: Evaluation via medical simulator. Anaesth. Crit. Care Pain Med. 2015, 34, 339–344. [Google Scholar] [CrossRef]
- Lewis, C.; Veal, B. Patient Simulation as an Active Learning Tool in Medical Education. J. Med. Imaging Radiat. Sci. 2010, 41, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.; Lockey, A.; Bhanji, F.; Lin, Y.; Hunt, E.A.; Lang, E. The use of high-fidelity manikins for advanced life support training—A systematic review and meta-analysis. Resuscitation 2015, 93, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Finan, E.; Bismilla, Z.; Whyte, H.E.; Leblanc, V.; McNamara, P. High-fidelity simulator technology may not be superior to traditional low-fidelity equipment for neonatal resuscitation training. J. Perinatol. 2012, 32, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Nimbalkar, A.; Patel, D.; Kungwani, A.; Phatak, A.; Vasa, R.; Nimbalkar, S. Randomized control trial of high fidelity vs low fidelity simulation for training undergraduate students in neonatal resuscitation. BMC Res. Notes 2015, 8, 636. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.; Hawkins, J.; Chehab, L.Z.; Martin-Tuite, P.; Feler, J.; Tan, A.; Alpers, B.S.; Pink, S.; Wang, J.; Freise, J.; et al. Developing Virtual Reality Trauma Training Experiences Using 360-Degree Video: Tutorial. J. Med. Internet Res. 2020, 22, e22420. [Google Scholar] [CrossRef] [PubMed]
- Knudson, M.M.; Khaw, L.; Bullard, M.K.; Dicker, R.; Cohen, M.J.; Staudenmayer, K.; Sadjadi, J.; Howard, S.; Gaba, D.; Krummel, T. Trauma Training in Simulation: Translating Skills From SIM Time to Real Time. J. Trauma Inj. Infect. Crit. Care 2008, 64, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, G.L.; Page, D.W.; Coe, N.P.; Lee, P.C.; Patterson, L.A.; Skylizard, L.; Louis, M.S.; Amaral, M.H.; Wait, R.B.; Seymour, N.E. Boot Camp: Educational Outcomes After 4 Successive Years of Preparatory Simulation-Based Training at Onset of Internship. J. Surg. Educ. 2012, 69, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Alsaad, A.A.; Davuluri, S.; Bhide, V.Y.; Lannen, A.M.; Maniaci, M.J. Assessing the performance and satisfaction of medical residents utilizing standardized patient versus mannequin-simulated training. Adv. Med. Educ. Pract. 2017, 8, 481–486. [Google Scholar] [CrossRef]
- Cecilio-Fernandes, D.; Brando, C.; de Oliveira, D.; Fernandes, G.; Tio, R. Additional simulation training: Does it affect students’ knowledge acquisition and retention? BMJ Simul. Technol. Enhanc. Learn. 2018, 5, 140–143. [Google Scholar] [CrossRef] [PubMed]
- Harrington, C.M.; Kavanagh, D.O.; Quinlan, J.F.; Ryan, D.; Dicker, P.; O’Keeffe, D.; Traynor, O.; Tierney, S. Development and evaluation of a trauma decision-making simulator in Oculus virtual reality. Am. J. Surg. 2018, 215, 42–47. [Google Scholar] [CrossRef]
- Cohen, D.C.; Sevdalis, N.; Patel, V.; Taylor, D.; Batrick, N.; Darzi, A.W. Major Incident Preparation for Acute Hospitals: Current State-of-the-Art, Training Needs Analysis, and the Role of Novel Virtual Worlds Simulation Technologies. J. Emerg. Med. 2012, 43, 1029–1037. [Google Scholar] [CrossRef]
- Amiel, I.; Simon, D.; Merin, O.; Ziv, A. Mobile in Situ Simulation as a Tool for Evaluation and Improvement of Trauma Treatment in the Emergency Department. J. Surg. Educ. 2016, 73, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Pringle, K.; Mackey, J.; Ruskis, J.; Modi, P.; Foggle, J.; Levine, A. A Short Trauma Course for Physicians in a Resource-Limited Setting: Is Low-Cost Simulation Effective? Ann. Emerg. Med. 2013, 62, S100. [Google Scholar] [CrossRef]
- Jacobs, L.; Burns, K.; Luk, S.; Hull, S. Advanced Trauma Operative Management Course: Participant Survey. World J. Surg. 2009, 34, 164–168. [Google Scholar] [CrossRef]
- Bredmose, P.P.; Habig, K.; Davies, G.; Grier, G.; Lockey, D.J. Scenario based outdoor simulation in pre-hospital trauma care using a simple mannequin model. Scand. J. Trauma Resusc. Emerg. Med. 2010, 18, 13–16. [Google Scholar] [CrossRef]
- Springer, R.; Mah, J.; Shusdock, I.; Bräutigam, R.; Donahue, S.; Butler, K. Simulation Training in Critical Care: Does Practice Make Perfect? J. Surg. Res. 2013, 179, 229. [Google Scholar] [CrossRef]
- Montán, K.L.; Hreckovski, B.; Dobson, B.; Örtenwall, P.; Montán, C.; Khorram-Manesh, A.; Lennquist, S. Development and evaluation of a new simulation model for interactive training of the medical response to major incidents and disasters. Eur. J. Trauma Emerg. Surg. 2013, 40, 429–443. [Google Scholar] [CrossRef] [PubMed]
- Jawaid, M.; Memon, A.A.; Masood, Z.; Alam, S.N. Effectiveness of the Primary Trauma Care Course: Is the outcome satisfactory? Pak. J. Med. Sci. 2013, 29, 1265–1268. [Google Scholar] [CrossRef]
- Ali, J.; Dunn, J.; Eason, M.; Drumm, J. Comparing the Standardized Live Trauma Patient and the Mechanical Simulator Models in the ATLS Initial Assessment Station. J. Surg. Res. 2010, 162, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Courteille, O.; Fahlstedt, M.; Ho, J.; Hedman, L.; Fors, U.; Von Holst, H.; Felländer-Tsai, L.; Möller, H. Learning through a virtual patient vs. recorded lecture: A comparison of knowledge retention in a trauma case. Int. J. Med. Educ. 2018, 9, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Aekka, A.; Abraham, R.; Hollis, M.; Boudiab, E.; Laput, G.; Purohit, H.; Kumar, R.; Vyas, A.; Basson, M.; Vyas, D. Prehospital trauma care education for first responders in India. J. Surg. Res. 2015, 197, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Doumouras, A.G.; Engels, P.T. Early crisis nontechnical skill teaching in residency leads to long-term skill retention and improved performance during crises: A prospective, nonrandomized controlled study. Surgery 2017, 162, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, F.O.; Moftakhar, Y.; Iv, A.L.D.; Khan, R.; Dasgupta, R.; Blanda, R.; Marchand, T.; Ahmed, R. Trauma Boot Camp: A Simulation-Based Pilot Study. Cureus 2016, 8, e463. [Google Scholar] [CrossRef]
- Sullivan, S.; Campbell, K.; Ross, J.C.; Thompson, R.; Underwood, A.; LeGare, A.; Osman, I.; Agarwal, S.K.; Jung, H.S. Identifying Nontechnical Skill Deficits in Trainees Through Interdisciplinary Trauma Simulation. J. Surg. Educ. 2018, 75, 978–983. [Google Scholar] [CrossRef] [PubMed]
- Kaban, J.M.; Stone, M.E.; Safadjou, S.; Reddy, S.H.; Simon, R.; Teperman, S.H. Does resident depth of clinical trauma exposure affect Advanced Trauma Operative Management (ATOM) course experience? J. Am. Coll. Surg. 2014, 219, e164–e165. [Google Scholar] [CrossRef]
- Taylor, D.; Patel, V.; Cohen, D.; Aggarwal, R.; Kerr, K.; Sevdalis, N.; Batrick, N.; Darzi, A. Single and Multi-User Virtual Patient Design in the Virtual World. Med. Meets Virtual Real. 18 2011, 163, 650–652. [Google Scholar] [CrossRef]
- Fleiszer, D.; Hoover, M.L.; Posel, N.; Razek, T.; Bergman, S. Development and Validation of a Tool to Evaluate the Evolution of Clinical Reasoning in Trauma Using Virtual Patients. J. Surg. Educ. 2018, 75, 779–786. [Google Scholar] [CrossRef]
- Farahmand, S.; Jalili, E.; Arbab, M.; Sedaghat, M.; Shirazi, M.; Keshmiri, F.; Azizpour, A.; Valadkhani, S.; Bagheri-Hariri, S. Distance Learning Can Be as Effective as Traditional Learning for Medical Students in the Initial Assessment of Trauma Patients. Acta Med. Iran. 2016, 54, 600–604. [Google Scholar]
- Park, C.; Grant, J.; Dumas, R.P.; Dultz, L.; Shoultz, T.H.; Scott, D.J.; Luk, S.; Abdelfattah, K.R.; Cripps, M. Does simulation work? Monthly trauma simulation and procedural training are associated with decreased time to intervention. J. Trauma Acute Care Surg. 2019, 88, 242–248. [Google Scholar] [CrossRef]
- Walker, R.; Phieffer, L.S.; Bishop, J.Y. Four Successive Years of Trauma-Based Objective Structured Clinical Evaluations: What Have We Learned? J. Surg. Educ. 2016, 73, 648–654. [Google Scholar] [CrossRef]
- Hayden, E.M.; Khatri, A.; Kelly, H.; Yager, P.H.; Salazar, G.M. Mannequin-based Telesimulation: Increasing Access to Simulation-based Education. Acad. Emerg. Med. 2017, 25, 144–147. [Google Scholar] [CrossRef] [PubMed]
- Kuhlenschmidt, K.M.; Houshmand, N.; Bisgaard, E.; Grant, J.; Dumas, R.; Park, C.; Cripps, M.W. Simulation-Based Skill Training in Trauma: A Much Needed Confidence Boost. J. Am. Coll. Surg. 2020, 231, S256. [Google Scholar] [CrossRef]
- Gräff, I.; Ghamari, S.; Schacher, S.; Glien, P.; Fimmers, R.; Baehner, T.; Kim, S. Improvement of polytrauma management-quality inspection of a newly introduced course concept. J. Eval. Clin. Pract. 2017, 23, 1381–1386. [Google Scholar] [CrossRef] [PubMed]
- Mills, B.W.; Miles, A.; Phan, T.; Dykstra, P.M.; Hansen, S.S.; Walsh, A.S.; Reid, D.; Langdon, C. Investigating the Extent Realistic Moulage Impacts on Immersion and Performance Among Undergraduate Paramedicine Students in a Simulation-based Trauma Scenario. Simul. Healthc. J. Soc. Simul. Healthc. 2018, 13, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Campbell, R.G.; Labuschagne, M.; Bezuidenhout, J. Perspectives of advanced life support paramedics on clinical simulation for summative assessment in South Africa: Is it time for change? Afr. J. Health Prof. Educ. 2018, 10, 183–188. [Google Scholar] [CrossRef]
- Jouda, M.; Finn, Y. Training in polytrauma management in medical curricula: A scoping review. Med. Teach. 2020, 42, 1385–1393. [Google Scholar] [CrossRef]
- Ruesseler, M.; Weinlich, M.; Müller, M.P.; Byhahn, C.; Marzi, I.; Walcher, F. Simulation training improves ability to manage medical emergencies. Emerg. Med. J. 2010, 27, 734–738. [Google Scholar] [CrossRef]
- Barleycorn, D.; Lee, G.A. How effective is trauma simulation as an educational process for healthcare providers within the trauma networks? A systematic review. Int. Emerg. Nurs. 2018, 40, 37–45. [Google Scholar] [CrossRef]
- Abelsson, A.; Rystedt, I.; Suserud, B.-O.; Lindwall, L. Learning by simulation in prehospital emergency care—An integrative literature review. Scand. J. Caring Sci. 2015, 30, 234–240. [Google Scholar] [CrossRef]
- Cohen, D.; Sevdalis, N.; Taylor, D.; Kerr, K.; Heys, M.; Willett, K.; Batrick, N.; Darzi, A. Emergency preparedness in the 21st century: Training and preparation modules in virtual environments. Resuscitation 2013, 84, 78–84. [Google Scholar] [CrossRef]
- Ziesmann, M.T.; Widder, S.; Park, J.; Kortbeek, J.B.; Brindley, P.; Hameed, M.; Paton-Gay, J.D.; Engels, P.T.; Hicks, C.; Fata, P.; et al. S.T.A.R.T.T.: Development of a national, multidisciplinary trauma crisis resource management curriculum-results from the pilot course. J. Trauma Acute Care Surg. 2013, 75, 753–758. [Google Scholar] [CrossRef]
- Gillman, L.M.; Brindley, P.; Paton-Gay, J.D.; Engels, P.T.; Park, J.; Vergis, A.; Widder, S. Simulated Trauma and Resuscitation Team Training course—Evolution of a multidisciplinary trauma crisis resource management simulation course. Am. J. Surg. 2016, 212, 188–193.e3. [Google Scholar] [CrossRef] [PubMed]
- Wallenstein, J.; Heron, S.; Santen, S.; Shayne, P.; Ander, D. A Core Competency-based Objective Structured Clinical Examination (OSCE) Can Predict Future Resident Performance. Acad. Emerg. Med. 2010, 17, S67–S71. [Google Scholar] [CrossRef] [PubMed]
- Dausey, D.J.; Buehler, J.W.; Lurie, N. Designing and conducting tabletop exercises to assess public health preparedness for manmade and naturally occurring biological threats. BMC Public Health 2007, 7, 92. [Google Scholar] [CrossRef] [PubMed]
- Issenberg, S.B.; McGaghie, W.; Petrusa, E.R.; Gordon, D.L.; Scalese, R.J. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med. Teach. 2005, 27, 10–28. [Google Scholar] [CrossRef]

| Study | Population of the Training | Simulation Method Used | Skills Trained | Evaluation Type | Context | Publication Year | Number Citations |
|---|---|---|---|---|---|---|---|
| Patel et al. [26] | Residents | CineVR | NS | SB | IH | 2020 | 1 |
| Knudson et al. [27] | Residents | L and HF | T and NT | WE | IH | 2010 | 146 |
| Fernandez et al. [28] | Residents | LF and HF | T | WE | IH | 2012 | 133 |
| Cohen et al. [29] | Prehospital clinicians and emergency medicine consultants | VR | T | WE | PH and IH | 2013 | 90 |
| Ruesseler et al. [30] | Final year medical students | HF | T | SB and WE | PH and IH | 2010 | 128 |
| Harrington et al. [31] | ATLS trainees | VR | T | WE | IH | 2018 | 76 |
| Murray et al. [31] | Emergency medicine, surgery and anesthesia residents | HF | T | WE | IH | 2015 | 36 |
| Cohen et al. [32] | Ambulance HART practitioners, surgical residents and emergency consultants | VR | T and NT | SB and WE | PH and IH | 2013 | 43 |
| Amiel et al. [33] | Physicians and nurses | SS and HF | T and NT | WE | IH | 2016 | 28 |
| Pringle et al. [34] | Attending and senior resident physicians | SP | T and NT | WE | IH | 2015 | 26 |
| Jacobs et al. [35] | Surgeons | PS | T and NT | WE | IH | 2010 | 25 |
| Bredmose et al. [36] | Helicopter emergency medical service doctors and paramedics | HF | NS | SB | PH | 2010 | 50 |
| Springer et al. [37] | Residents | HF | NS | WE | IH | 2013 | 18 |
| Lennquist et al. [38] | Physicians, nurses, paramedics, military doctors and administrators | CC | T and NT | SB | PH and IH | 2014 | 25 |
| Jawaid et al. [39] | Final year medical students, interns and consultants | L, SS and CS | T | WE | IH | 2013 | 19 |
| Ali et al. [40] | Surgical residents | HF | T | SB and WE | IH | 2010 | 14 |
| Courteille et al. [41] | Medical students and residents | L and VR | T | WE | IH | 2018 | 28 |
| Aekka et al. [42] | Non-doctor first responders | HF | T | SB and WE | PH | 2015 | 20 |
| Nurses, radiology technicians and attending and trainee physicians | HF | T | NS | IH | 2018 | 26 | |
| Doumouras et al. [43] | Residents | HF | NT | WE | IH | 2017 | 11 |
| Figueroa et al. [44] | Interns | L, SS and HF | NS | WE | IH | 2016 | 22 |
| Sullivan et al. [45] | Residents and emergency nurses | HF | NT | WE | IH | 2018 | 13 |
| Kaban et al. [46] | Residents | NS | T | WE | IH | 2016 | 9 |
| Alsaad et al. [29] | Residents | HF and SP | T | WE | IH | 2017 | 21 |
| Taylor et al. [47] | Paramedics and different roles involved in emergency medicine | VR | NS | NS | PH and IH | 2011 | 11 |
| Fleiszer et al. [48] | Undergraduate medical students | VR | T | SB | NS | 2018 | 15 |
| Cuisinier et al. [20] | Medical students | HF | T | WE | IH | 2015 | 4 |
| Farahmand et al. [49] | Interns | L, CS and SS | T | SN and WE | IH | 2016 | 11 |
| Park et al. [50] | Residents | NS | T | NS | IH | 2020 | 6 |
| Walker et al. [51] | Residents | SP | T and NT | SB and WE | IH | 2016 | 3 |
| Hayden et al. [52] | Nurses, radiology technicians, attending and trainee physicians | HF | T | NS | IH | 2018 | 49 |
| Kuhlenschmidt et al. [53] | Residents | SS | T | WE | IH | 2020 | 0 |
| Cecilio-Fernandes et al. [30] | Medical students | HF and SS | T | SB and WE | IH | 2019 | 3 |
| Gräff et al. [54] | Doctors | HF | T and NT | SB and WE | IH | 2017 | 4 |
| Mills et al. [55] | Paramedic students | SP | NS | SB and WE | PH | 2018 | 11 |
| Campbell et al. [56] | Paramedics | HF | NS | SB and WE | PH | 2018 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Larraga-García, B.; Quintana-Díaz, M.; Gutiérrez, Á. Simulation-Based Education in Trauma Management: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 13546. https://doi.org/10.3390/ijerph192013546
Larraga-García B, Quintana-Díaz M, Gutiérrez Á. Simulation-Based Education in Trauma Management: A Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(20):13546. https://doi.org/10.3390/ijerph192013546
Chicago/Turabian StyleLarraga-García, Blanca, Manuel Quintana-Díaz, and Álvaro Gutiérrez. 2022. "Simulation-Based Education in Trauma Management: A Scoping Review" International Journal of Environmental Research and Public Health 19, no. 20: 13546. https://doi.org/10.3390/ijerph192013546
APA StyleLarraga-García, B., Quintana-Díaz, M., & Gutiérrez, Á. (2022). Simulation-Based Education in Trauma Management: A Scoping Review. International Journal of Environmental Research and Public Health, 19(20), 13546. https://doi.org/10.3390/ijerph192013546







