Health-Risk Behaviors, COVID-19 Preventive Behaviors, and the Impact of the COVID-19 Pandemic on the Working-Age Population of Bangkok, Thailand
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Design and Sampling
2.1.1. Health-Risk Behaviors Related to COVID-19 Infection
2.1.2. Knowledge of COVID-19
2.1.3. COVID-19 Preventive Behaviors
2.1.4. Effects of COVID-19
2.1.5. Sociodemographic Information
2.2. Data Analyses
3. Results
3.1. Characteristics of Participants
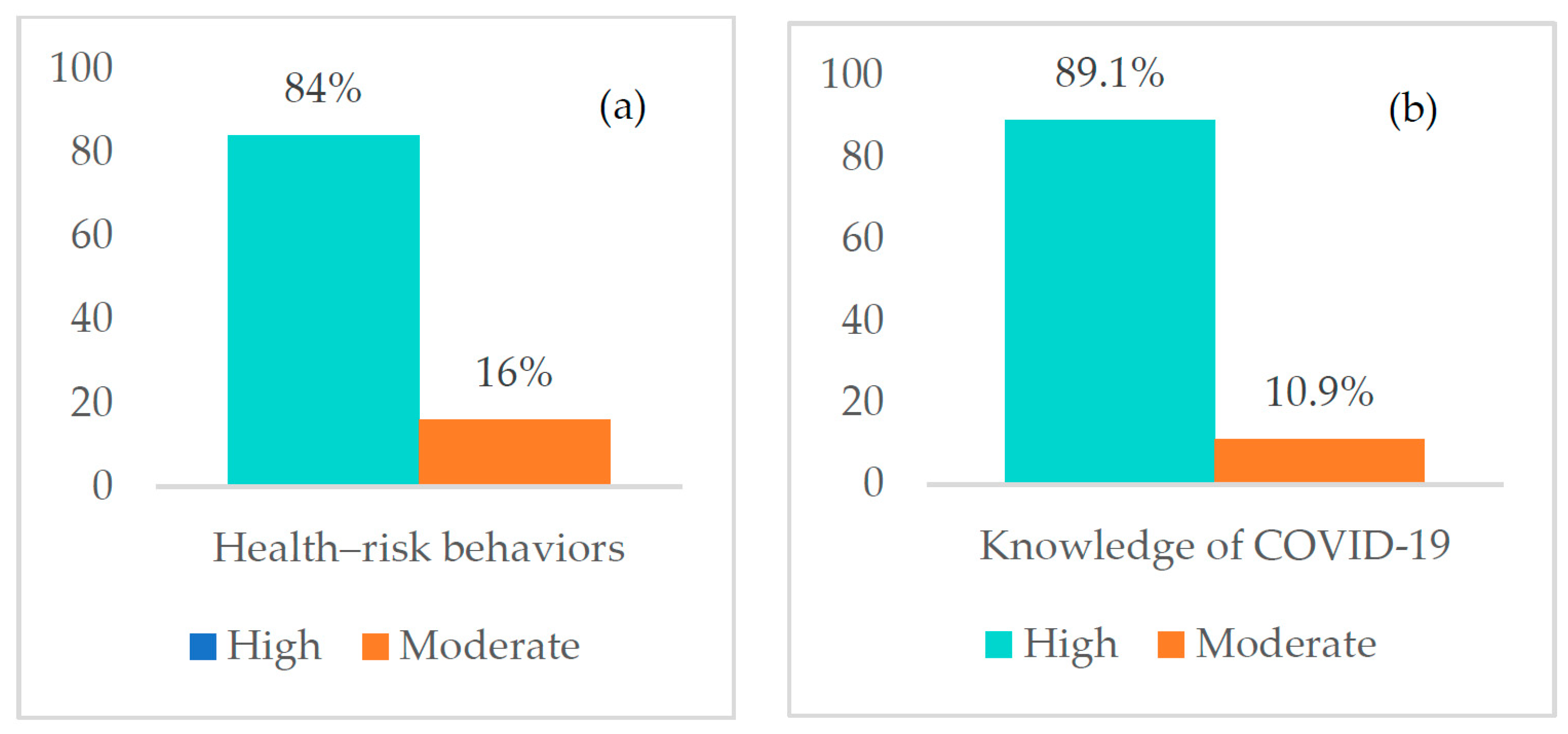
3.2. Participant Levels of Health-Risk Behaviors and Knowledge about COVID-19
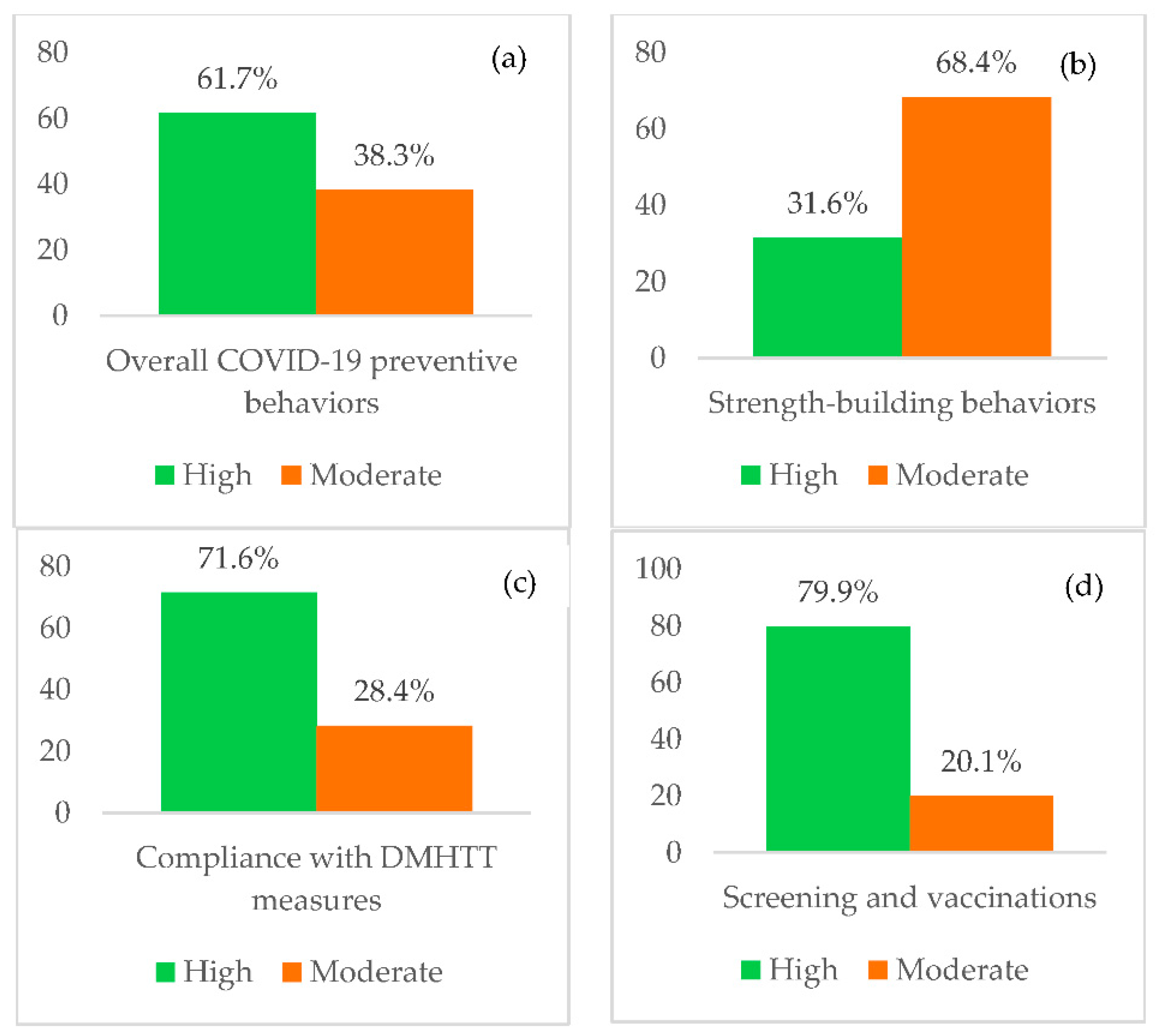
3.3. COVID-19 Preventive Behaviors Levels
3.4. Effects of COVID-19 among Study Participants
3.5. Factors Correlated with Level of COVID-19 Preventive Behaviors
3.6. Factors Influencing COVID-19 Preventive Behaviors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tran, B.X.; Dang, A.K.; Thai, P.K.; Le, H.T.; Le, X.T.T.; Do, T.T.T.; Nguyen, T.H.; Pham, H.Q.; Phan, H.T.; Vu, G.T. Coverage of health information by different sources in communities: Implication for COVID-19 epidemic response. Int. J. Environ. Res. Public Health 2020, 17, 3577. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. COVID Data Tracker. Available online: https://covid.cdc.gov/covid-data-tracker (accessed on 27 September 2022).
- Choompunuch, B.; Suksatan, W.; Sonsroem, J.; Kutawan, S.; In-udom, A. Stress, adversity quotient, and health behaviors of undergraduate students in a Thai university during COVID-19 outbreak. Belitung Nurs. J. 2021, 7, 1–7. [Google Scholar] [CrossRef]
- Waewwab, P.; Pan-Ngum, W.; Siri, S.; Bhopdhornangkul, B.; Mahikul, W. Knowledge, Attitudes, and Practices Regarding “New Normal” Guidelines and Quality of Life Among Thai People During the COVID-19 Outbreak: An Online Cross-Sectional Survey. Front. Public Health 2022, 10, 914417. [Google Scholar] [CrossRef]
- Okada, P.; Buathong, R.; Phuygun, S.; Thanadachakul, T.; Parnmen, S.; Wongboot, W.; Waicharoen, S.; Wacharapluesadee, S.; Uttayamakul, S.; Vachiraphan, A.; et al. Early transmission patterns of coronavirus disease 2019 (COVID-19) in travellers from Wuhan to Thailand, January 2020. Eurosurveillance 2020, 25, 2000097. [Google Scholar] [CrossRef] [PubMed]
- Both, L.M.; Zoratto, G.; Calegaro, V.C.; Ramos-Lima, L.F.; Negretto, B.L.; Hauck, S.; Freitas, L.H.M. COVID-19 pandemic and social distancing: Economic, psychological, family, and technological effects. Trends Psychiatry Psychother. 2021, 43, 85–91. [Google Scholar] [CrossRef]
- Chag, J.; Chaudhury, S.; Saldanha, D. Economic and psychological impact of COVID-19 lockdown: Strategies to combat the crisis. Ind. Psychiatry J. 2020, 29, 362–368. [Google Scholar] [CrossRef]
- Santana, C.L.A.; Manfrinato, C.V.; Souza, P.R.P.; Marino, A.; Condé, V.F.; Stedefeldt, E.; Tomita, L.Y.; do Carmo Franco, M. Psychological distress, low-income, and socio-economic vulnerability in the COVID-19 pandemic. Public Health 2021, 199, 42–45. [Google Scholar] [CrossRef]
- Suksatan, W.; Choompunuch, B.; Koontalay, A.; Posai, V.; Abusafia, A.H. Predictors of Health Behaviors Among Undergraduate Students During the COVID-19 Pandemic: A Cross-Sectional Predictive Study. J. Multidiscip. Heal. 2021, 14, 727–734. [Google Scholar] [CrossRef]
- Limkunakul, C.; Phuthomdee, S.; Srinithiwat, P.; Chanthanaroj, S.; Boonsawat, W.; Sawanyawisuth, K. Factors associated with preventive behaviors for COVID-19 infection among healthcare workers by a health behavior model. Trop. Med. Health 2022, 50, 65. [Google Scholar] [CrossRef]
- Upake, C.; Nanthamongkolchai, S.; Taechaboonsermsak, P.; Yodmai, K.; Suksatan, W. Factors Predicting the Coronavirus Disease 2019 Preventive Behaviors of Older Adults: A Cross-Sectional Study in Bangkok, Thailand. Int. J. Environ. Res. Public Health 2022, 19, 10361. [Google Scholar] [CrossRef]
- Khandia, R.; Singhal, S.; Alqahtani, T.; Kamal, M.A.; El-Shall, N.A.; Nainu, F.; Desingu, P.A.; Dhama, K. Emergence of SARS-CoV-2 Omicron (B.1.1.529) variant, salient features, high global health concerns and strategies to counter it amid ongoing COVID-19 pandemic. Environ. Res. 2022, 209, 112816. [Google Scholar] [CrossRef] [PubMed]
- Pothisa, T.; Ong-Artborirak, P.; Seangpraw, K.; Tonchoy, P.; Kantow, S.; Auttama, N.; Boonyathee, S.; Choowanthanapakorn, M.; Bootsikeaw, S.; Panta, P.; et al. Knowledge of COVID-19 and Its Relationship with Preventive Behaviors and Vaccination among Adults in Northern Thailand’s Community. Int. J. Environ. Res. Public Health 2022, 19, 1521. [Google Scholar] [CrossRef] [PubMed]
- Yodmai, K.; Pechrapa, K.; Kittipichai, W.; Charupoonpol, P.; Suksatan, W. Factors Associated with Good COVID-19 Preventive Behaviors Among Older Adults in Urban Communities in Thailand. J. Prim. Care Community Health 2021, 12, 21501327211036251. [Google Scholar] [CrossRef] [PubMed]
- Bloom, B.S. Learning for Mastery. Instruction and Curriculum; Evaluation Comment UCLA-CSIEP: Los Angeles, CA, USA, 1968. [Google Scholar]
- Kasatpibal, N.; Viseskul, N.; Thummathai, K.; Kumnon, K.; Sungkumpung, S.; Tokelea, R. Predicting Factors of Thai Population Practices Amid People Have Been Infected/Quarantined and Impacts of COVID-19 Outbreak (Phase I); National Research Council of Thailand: Bangkok, Thailand, 2020. [Google Scholar]
- Barrett, C.; Cheung, K.L. Knowledge, socio-cognitive perceptions and the practice of hand hygiene and social distancing during the COVID-19 pandemic: A cross-sectional study of UK university students. BMC Public Health 2021, 21, 426. [Google Scholar] [CrossRef] [PubMed]
- Marome, W.; Shaw, R. Covid-Response in Thailand Its Implications on Future, Preparedness. Int. J. Environ. Res. Public Health 2021, 18, 1089. [Google Scholar] [CrossRef]
- Liang, W.; Duan, Y.; Shang, B.; Hu, C.; Baker, J.S.; Lin, Z.; He, J.; Wang, Y. Precautionary Behavior and Depression in Older Adults during the COVID-19 Pandemic: An Online Cross-Sectional Study in Hubei, China. Int. J. Environ. Res. Public Health 2021, 18, 1853. [Google Scholar] [CrossRef]
- Kuo, Y.J.; Chen, Y.P.; Wang, H.W.; Liu, C.H.; Strong, C.; Saffari, M.; Ko, N.Y.; Lin, C.Y.; Griffiths, M.D. Community Outbreak Moderates the Association Between COVID-19-Related Behaviors and COVID-19 Fear Among Older People: A One-Year Longitudinal Study in Taiwan. Front. Med. (Lausanne) 2021, 8, 756985. [Google Scholar] [CrossRef]
- Takalay, S.; Ngo-Giang-Huong, N.; Kongnim, W.; Mongkolwat, P.; Phoseng, P.; Wangsaeng, N.; Hongjaisee, S.; Butr-Indr, B.; Tragoolpua, K.; Jourdain, G.; et al. Prevalences of SARS-CoV-2 RNA and anti-SARS-CoV-2 among at-risk populations in Chiang Mai and Lamphun provinces, Thailand, during November 2020–January 2021. PLoS ONE 2022, 17, e0263127. [Google Scholar] [CrossRef]
- Uppala, R.; Sitthikarnkha, P.; Niamsanit, S.; Sutra, S.; Thepsuthammarat, K.; Techasatian, L.; Anantasit, N.; Teeratakulpisarn, J. Effect of the COVID-19 Pandemic on Lower Respiratory Tract Infection Determinants in Thai Hospitalized Children: National Data Analysis 2015–2020. Trop. Med. Infect. Dis. 2022, 7, 151. [Google Scholar] [CrossRef]
- Posai, V.; Suksatan, W.; Choompunuch, B.; Koontalay, A.; Ounprasertsuk, J.; Sadang, J.M. Assessment of the Health-Promoting Behaviors of Hospitalized Patients with Non-Communicable Diseases During the Second Wave of COVID-19. J. Multidiscip. Heal. 2021, 14, 2185–2194. [Google Scholar] [CrossRef]
- Tiaprapong, K.; Sirikul, A.; Krajangmek, C.; Duangthongkul, N.; Pandam, N.; Piya-amornphan, N. Awareness of COVID-19 influences on the wellness of Thai health professional students: An ambulatory assessment during the early “new normal” informing policy. PLoS ONE 2021, 16, e0252681. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.P.L.; Pattanrsi, S. The Influence of Ethnic, Social, and Demographic Factors on Urban Slum Dwellers’ Threat Appraisal, Awareness, and Protective Practices against COVID-19 in Thailand. Am. J. Trop. Med. Hyg. 2022, 107, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Kollamparambil, U.; Oyenubi, A. Behavioural response to the Covid-19 pandemic in South Africa. PLoS ONE 2021, 16, e0250269. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.J.; Santos, P. The Impact of Health Literacy on Knowledge and Attitudes towards Preventive Strategies against COVID-19: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 5421. [Google Scholar] [CrossRef] [PubMed]
- Zhong, B.L.; Luo, W.; Li, H.M.; Zhang, Q.Q.; Liu, X.G.; Li, W.T.; Li, Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int. J. Biol. Sci. 2020, 16, 1745–1752. [Google Scholar] [CrossRef] [PubMed]
- Arslanca, T.; Fidan, C.; Daggez, M.; Dursun, P. Knowledge, preventive behaviors and risk perception of the COVID-19 pandemic: A cross-sectional study in Turkish health care workers. PLoS ONE 2021, 16, e0250017. [Google Scholar] [CrossRef]
- Sharma, G.; Volgman Annabelle, S.; Michos Erin, D. Sex Differences in Mortality From COVID-19 Pandemic. JACC Case Rep. 2020, 2, 1407–1410. [Google Scholar] [CrossRef]
- Bronfman, N.; Repetto, P.; Cordón, P.; Castañeda, J.; Cisternas, P. Gender Differences on Psychosocial Factors Affecting COVID-19 Preventive Behaviors. Sustainability 2021, 13, 6148. [Google Scholar] [CrossRef]
- Pender, N.J.; Murdaugh, C.L.; Parsons, M.A. Health Promotion in Nursing Practice, 7th ed.; Pearson: Boston, MA, USA, 2015. [Google Scholar]
- Ezati Rad, R.; Mohseni, S.; Kamalzadeh Takhti, H.; Hassani Azad, M.; Shahabi, N.; Aghamolaei, T.; Norozian, F. Application of the protection motivation theory for predicting COVID-19 preventive behaviors in Hormozgan, Iran: A cross-sectional study. BMC Public Health 2021, 21, 466. [Google Scholar] [CrossRef]
- Nudelman, G.; Peleg, S.; Shiloh, S. The Association Between Healthy Lifestyle Behaviours and Coronavirus Protective Behaviours. Int. J. Behav. Med. 2021, 28, 779–787. [Google Scholar] [CrossRef]
- Onder, G.; Rezza, G.; Brusaferro, S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA 2020, 323, 1775–1776. [Google Scholar] [CrossRef] [PubMed]
- Nanthamongkolchai, S.; Tojeen, A.; Munsawaengsub, C.; Yodmai, K.; Suksatan, W. Quality of Life of Older Adults with Physical and Mobility Disabilities during the COVID-19 Pandemic: A Cross-Sectional Study in Thailand. Sustainability 2022, 14, 8525. [Google Scholar] [CrossRef]
- Pasion, R.; Paiva, T.O.; Fernandes, C.; Barbosa, F. The AGE Effect on Protective Behaviors During the COVID-19 Outbreak: Sociodemographic, Perceptions and Psychological Accounts. Front. Psychol. 2020, 11, 561785. [Google Scholar] [CrossRef] [PubMed]
- Bechard, L.E.; Bergelt, M.; Neudorf, B.; DeSouza, T.C.; Middleton, L.E. Using the Health Belief Model to Understand Age Differences in Perceptions and Responses to the COVID-19 Pandemic. Front. Psychol. 2021, 12, 609893. [Google Scholar] [CrossRef]
| Factors | Number | Percentage |
|---|---|---|
| Sex | ||
| Female | 227 | 72.5 |
| Male | 86 | 27.5 |
| Age (years) | ||
| 18–30 | 136 | 43.5 |
| 31–40 | 87 | 27.8 |
| 41–50 | 63 | 20.1 |
| 51–59 | 27 | 8.6 |
| (mean = 34.6, SD ± 10.23) | ||
| Educational level | ||
| High school or lower | 48 | 15.3 |
| Bachelor’s degrees or higher | 265 | 84.7 |
| Marital status | ||
| Single | 230 | 73.5 |
| Married | 83 | 26.5 |
| Income (USD) | ||
| 57–429 | 94 | 30.0 |
| 430–714 | 83 | 26.5 |
| 715–1000 | 57 | 18.2 |
| >1000 | 79 | 24.8 |
| (mean = 734.08, SD ± 172.42) | ||
| Family size (person) | ||
| 1–2 | 118 | 37.70 |
| 3–4 | 130 | 41.53 |
| >5 | 65 | 20.77 |
| (mean = 3.2, SD ± 1.24) |
| Number | Percentage | |
|---|---|---|
| Overall effects from COVID-19 | ||
| Low | 58 | 18.5 |
| Moderate | 153 | 48.9 |
| High | 102 | 32.6 |
| Health and disease prevention | ||
| Low | 50 | 16.0 |
| Moderate | 148 | 47.3 |
| High | 115 | 36.7 |
| Family | ||
| Low | 81 | 25.9 |
| Moderate | 103 | 32.9 |
| High | 129 | 41.2 |
| Economic | ||
| Low | 85 | 27.2 |
| Moderate | 89 | 28.4 |
| High | 139 | 44.4 |
| Psychological | ||
| Low | 52 | 16.6 |
| Moderate | 98 | 31.3 |
| High | 163 | 52.1 |
| Variables | COVID-19 Preventive Behaviors | |
|---|---|---|
| Coefficient Correlation (r) | p-Value | |
| Age | 0.226 | <0.001 |
| Income | −0.034 | 0.55 |
| Number of family member | 0.102 | 0.07 |
| Health-risk behaviors | 0.475 | <0.001 |
| Knowledge of COVID-19 | 0.116 | 0.040 |
| Factors | B | Beta | T | p-Value |
|---|---|---|---|---|
| Health-risk behaviors | 0.798 | 0.445 | 8.929 | <0.001 |
| Knowledge of COVID-19 | 0.660 | 0.148 | 3.050 | 0.002 |
| Gender (female vs. male *) | 2.130 | 0.145 | 3.005 | 0.003 |
| Age | 0.086 | 0.133 | 2.663 | 0.008 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nanthamongkolchai, S.; Taechaboonsermsak, P.; Tawatting, K.; Suksatan, W. Health-Risk Behaviors, COVID-19 Preventive Behaviors, and the Impact of the COVID-19 Pandemic on the Working-Age Population of Bangkok, Thailand. Int. J. Environ. Res. Public Health 2022, 19, 13394. https://doi.org/10.3390/ijerph192013394
Nanthamongkolchai S, Taechaboonsermsak P, Tawatting K, Suksatan W. Health-Risk Behaviors, COVID-19 Preventive Behaviors, and the Impact of the COVID-19 Pandemic on the Working-Age Population of Bangkok, Thailand. International Journal of Environmental Research and Public Health. 2022; 19(20):13394. https://doi.org/10.3390/ijerph192013394
Chicago/Turabian StyleNanthamongkolchai, Sutham, Pimsurang Taechaboonsermsak, Kanasap Tawatting, and Wanich Suksatan. 2022. "Health-Risk Behaviors, COVID-19 Preventive Behaviors, and the Impact of the COVID-19 Pandemic on the Working-Age Population of Bangkok, Thailand" International Journal of Environmental Research and Public Health 19, no. 20: 13394. https://doi.org/10.3390/ijerph192013394
APA StyleNanthamongkolchai, S., Taechaboonsermsak, P., Tawatting, K., & Suksatan, W. (2022). Health-Risk Behaviors, COVID-19 Preventive Behaviors, and the Impact of the COVID-19 Pandemic on the Working-Age Population of Bangkok, Thailand. International Journal of Environmental Research and Public Health, 19(20), 13394. https://doi.org/10.3390/ijerph192013394









