What’s behind the Dashboard? Intervention Mapping of a Mobility Outcomes Monitoring System for Rehabilitation
Abstract
1. Introduction
2. Materials and Methods
2.1. Step 1—Logic Model of the Problem
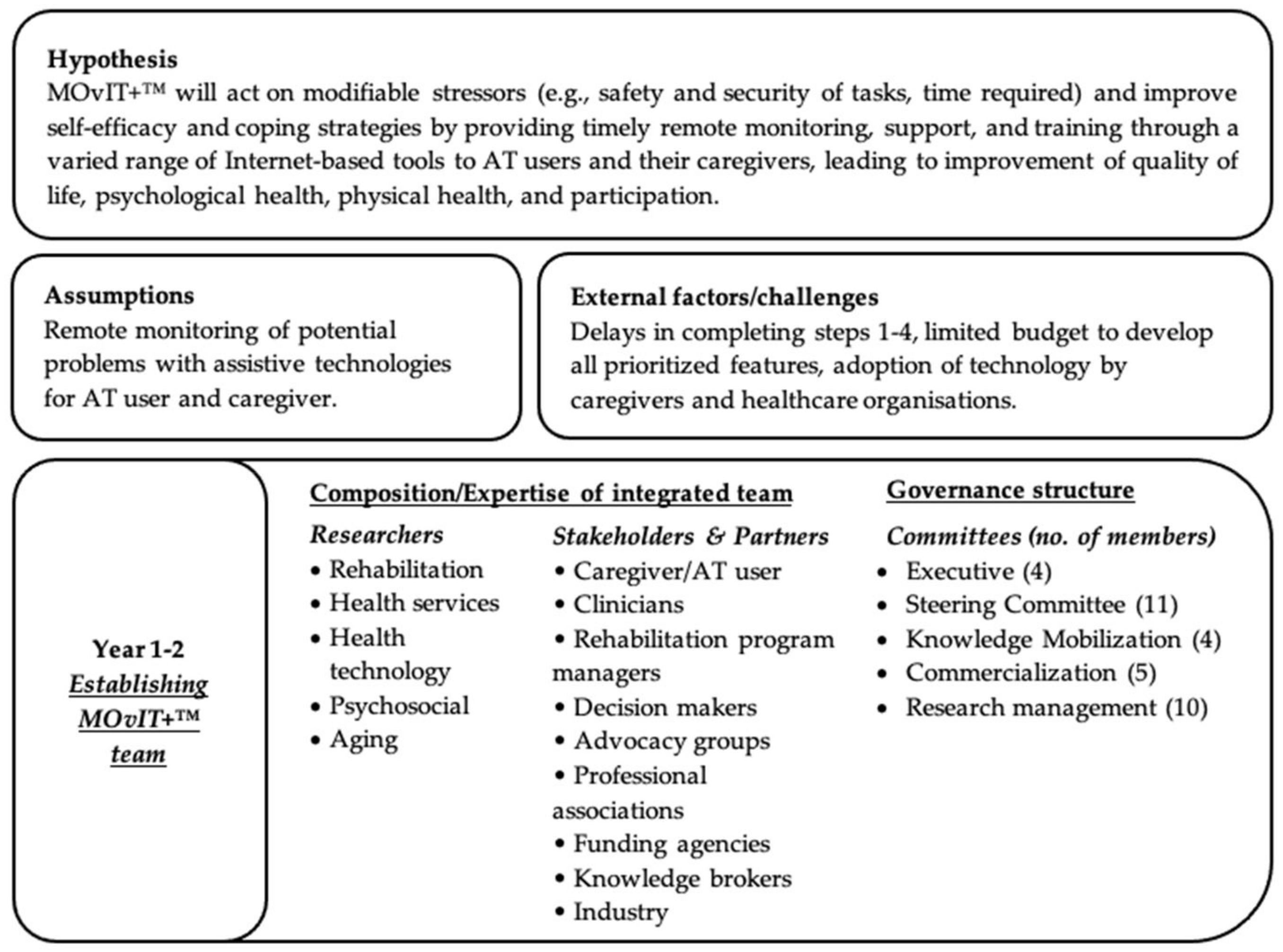
2.1.1. Governance Structure
2.1.2. Needs Assessment
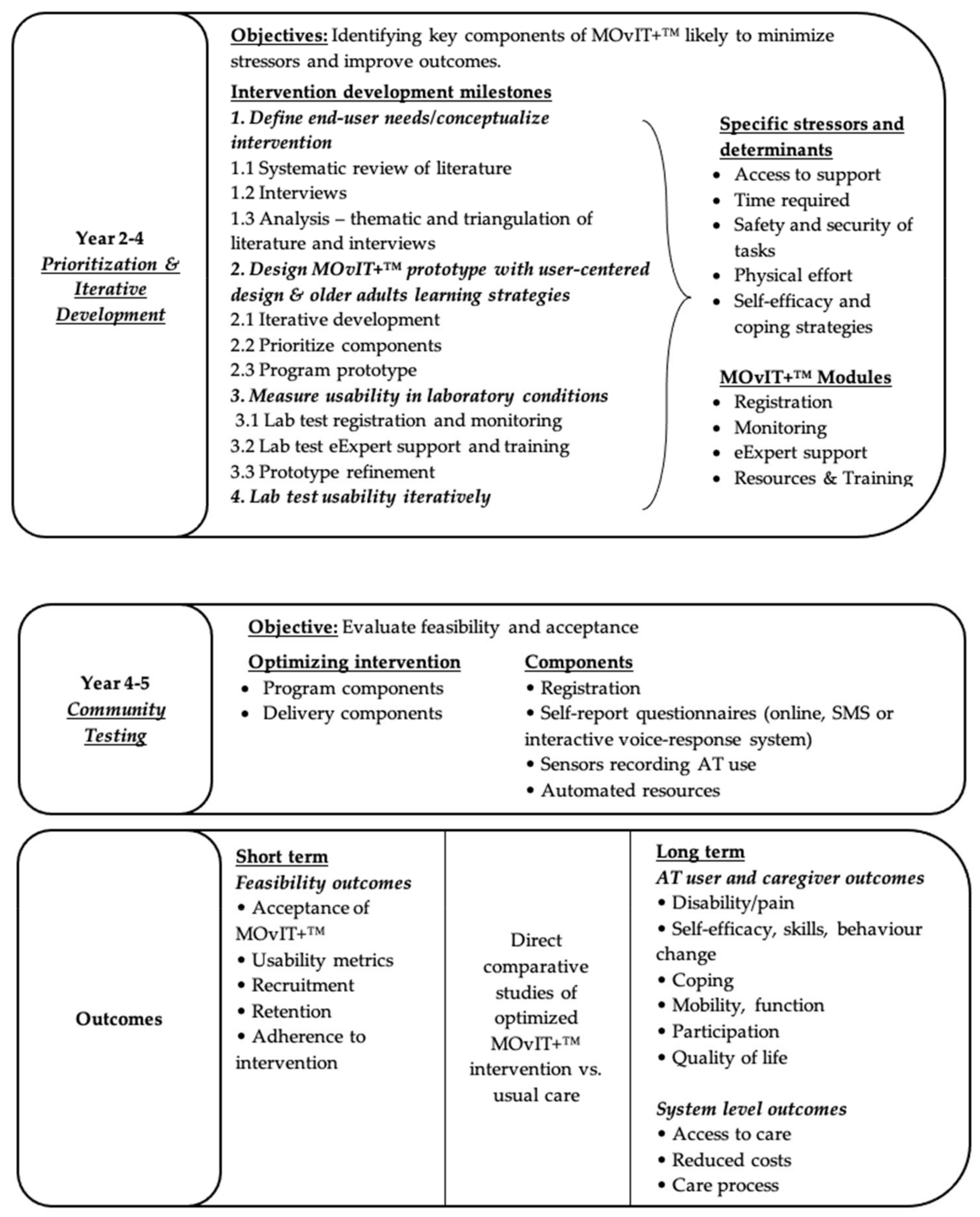
2.2. Step 2—Program Outcomes and Objectives; Logic Model of Change
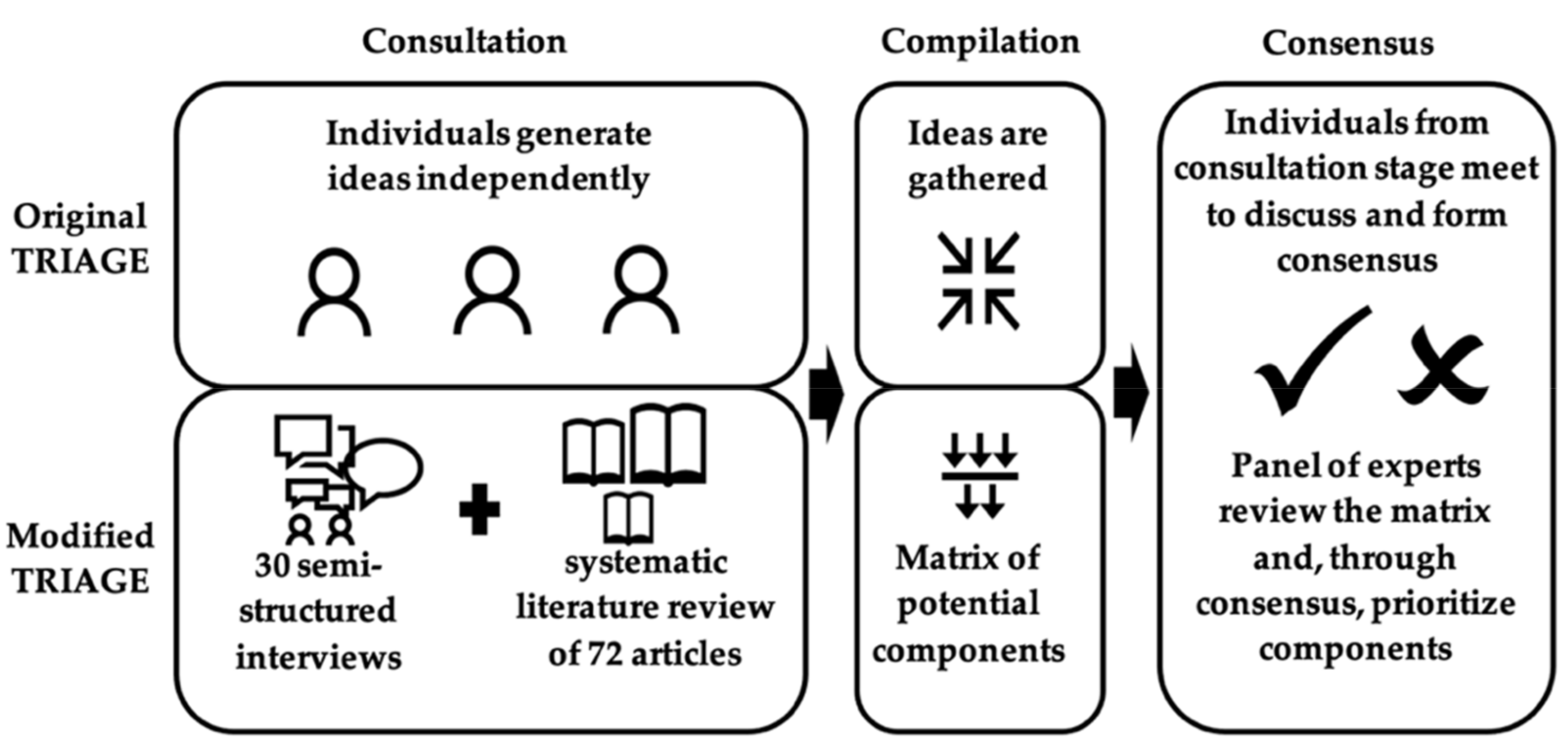
2.3. Step 3—Program Design
2.3.1. Program Themes, Components, and Scope
2.3.2. Program Sequence
2.4. Step 4—Program Production
2.4.1. Monitoring Components
2.4.2. Library of Resources
2.4.3. Lab Tests
2.5. Step 5—Program Implementation Plan
2.6. Step 6—Evaluation Plan
3. Results
3.1. Step 1—Logic Model of the Problem
3.1.1. Governance Structure
3.1.2. Needs Assessment
3.2. Step 2—Program Outcomes and Objectives; Logic Model of Change
3.3. Step 3—Program Design
3.3.1. Program Themes, Components, and Scope
3.3.2. Program Sequence
3.4. Step 4—Program Production
3.4.1. Monitoring Components
3.4.2. Library of Resources
3.4.3. Lab Tests
3.5. Step 5—Program Implementation Plan
3.6. Step 6—Evaluation Plan
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Han, L.M.D.P.; Allore, H.P.; Murphy, T.P.; Gill, T.M.D.; Peduzzi, P.P.; Lin, H.P. Dynamics of functional aging based on latent-class trajectories of activities of daily living. Ann. Epidemiol. 2013, 23, 87–92. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Assistive Devices and Technologies. Available online: https://www.who.int/disabilities/technology/en/ (accessed on 1 November 2020).
- Mortenson, W.B.; Pysklywec, A.; Fuhrer, M.J.; Jutai, J.W.; Plante, M.; Demers, L. Caregivers’ experiences with the selection and use of assistive technology. Disabil. Rehabil. Assist. Technol. 2018, 13, 562–567. [Google Scholar] [CrossRef] [PubMed]
- Madara Marasinghe, K. Assistive technologies in reducing caregiver burden among informal caregivers of older adults: A systematic review. Disabil. Rehabil. Assist. Technol. 2016, 11, 353–360. [Google Scholar] [CrossRef]
- Hammel, J.; Southall, K.; Jutai, J.; Finlayson, M.; Kashindi, G.; Fok, D. Evaluating use and outcomes of mobility technology: A multiple stakeholder analysis. Disabil. Rehabil. Assist. Technol. 2013, 8, 294–304. [Google Scholar] [CrossRef] [PubMed]
- Wittich, W.; Granberg, S.; Wahlqvist, M.; Pichora-Fuller, M.K.; Mäki-Torkko, E. Device abandonment in deafblindness: A scoping review of the intersection of functionality and usability through the International Classification of Functioning, Disability and Health lens. BMJ Open 2021, 11, e044873. [Google Scholar] [CrossRef]
- Petrie, H.; Carmien, S.; Lewis, A. Assistive Technology Abandonment: Research Realities and Potentials. In Proceedings of the Computers Helping People with Special Needs: 16th International Conference, ICCHP 2018, Part II Lecture Notes in Computer Science: Information Systems and Applications, incl. Internet/Web, and HCI 1611-3349, Linz, Austria, 11–13 July 2018; Springer: Cham, Switzerland, 2018; pp. 532–540. [Google Scholar]
- Arthanat, S.; Vroman, K.G.; Lysack, C. A home-based individualized information communication technology training program for older adults: A demonstration of effectiveness and value. Disabil. Rehabil. Assist. Technol. 2016, 11, 316–324. [Google Scholar] [CrossRef]
- Kirby, R.L.; Dupuis, D.J.; MacPhee, A.H.; Coolen, A.L.; Smith, C.; Best, K.L.; Newton, A.M.; Mountain, A.D.; MacLeod, D.A.; Bonaparte, J.P. The wheelchair skills test (version 2.4): Measurement properties. Arch. Phys. Med. Rehabil. 2004, 85, 794–804. [Google Scholar] [CrossRef]
- Best, K.L.; Miller, W.C.; Eng, J.J.; Huston, G.; Routhier, F. Pilot study of a peer-led wheelchair training program to improve self-efficacy using a manual wheelchair: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2016, 97, 37–44. [Google Scholar] [CrossRef]
- Song, Y.; van der Cammen, T.J.M. Electronic assistive technology for community-dwelling solo-living older adults: A systematic review. Maturitas 2019, 125, 50–56. [Google Scholar] [CrossRef]
- Kintsch, A.; DePaula, R. A framework for the adoption of assistive technology. SWAAAC 2002 Support. Learn. Through Assist. Technol. 2002, 3, 1–10. [Google Scholar]
- Gitlin, L.N. Assistive technology in the home and community for older people: Psychological and social considerations. In Assistive Technology: Matching Device and Consumer for Successful Rehabilitation; American Psychological Association: Washington, DC, USA, 2002; pp. 109–122. [Google Scholar]
- Lenker, J.A.; Paquet, V.L. A New Conceptual Model for Assistive Technology Outcomes Research and Practice. Assist. Technol. 2004, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Auger, C.; Miller, W.C.; Jutai, J.; Tamblyn, R. Development and feasibility of an automated call monitoring intervention for older wheelchair users: The MOvIT project. BMC Health Serv. Res. 2015, 15, 386. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Auger, C.; Readman, J.; Dominique, A.; Thibault, F.; Jobin, É.; Beauregard, S. Impact d’un suivi systématique par appels automatisés sur l’adhésion aux recommandations ergothérapiques suite à l’attribution d’un fauteuil roulant chez des utilisateurs de plus de 50 ans. Rev. Francoph. Rech. En Ergothér. 2015, 1, 5–21. [Google Scholar] [CrossRef]
- Auger, C.; Demers, L.; Mortenson, W.B.; Guay, M.; Bier, N.; Michaud, F.o.; Ahmed, S. MOvIT-PLUS Portal for monitoring and training user-caregiver dyads after provision of assistive technology. In Proceedings of the 45th Annual Scientific and Educational Meeting, Montreal, QC, Canada, 20–22 October 2016; Canadian Association on Gerontology: Toronto, ON, Canada, 2016. [Google Scholar]
- Demers, L.; Fast, J.; Mortenson, W.B.; Routhier, F.; Auger, C.; Polgar, J. Advancing research on evaluating needs and developing technological solutions for family caregivers. In Proceedings of the 10th World Conference of Gerontechnology, Nice, France, 28–30 September 2016. [Google Scholar]
- Gélinas-Bronsard, D.; Mortenson, W.B.; Ahmed, S.; Guay, C.; Auger, C. Co-construction of an Internet-based intervention for older assistive technology users and their family caregivers: Stakeholders’ perceptions. Disabil. Rehabil. Assist. Technol. 2019, 14, 602–611. [Google Scholar] [CrossRef]
- Campeau-Vallerand, C.; Michaud, F.o.; Routhier, F.o.; Archambault, P.S.; Létourneau, D.; Gélinas-Bronsard, D.; Auger, C. Development of a Web-Based Monitoring System for Power Tilt-in-Space Wheelchairs: Formative Evaluation. JMIR Rehabil. Assist. Technol. 2019, 6, e13560. [Google Scholar] [CrossRef]
- Guay, C.; Auger, C.; Demers, L.; Mortenson, W.B.; Miller, W.C.; Gélinas-Bronsard, D.; Ahmed, S. Components and Outcomes of Internet-Based Interventions for Caregivers of Older Adults: Systematic Review. J. Med. Internet Res. 2017, 19, e313. [Google Scholar] [CrossRef]
- Bartholomew, L.K.; Markham, C.M.; Ruiter, R.A.C.; Fernández, M.E.; Kok, G.; Parcel, G.S. Planning Health Promotion Programs: An Intervention Mapping Approach, 4th ed.; Jossey-Bass: San Francisco, CA, USA, 2016. [Google Scholar]
- Mohr, D.C.; Schueller, S.M.; Montague, E.; Burns, M.N.; Rashidi, P. The Behavioral Intervention Technology Model: An Integrated Conceptual and Technological Framework for eHealth and mHealth Interventions. J. Med. Internet Res. 2014, 16, e146. [Google Scholar] [CrossRef]
- Poupart, J.; Deslauriers, J.-P.; Groulz, L.H.; Laperrière, A.; Mayer, R.; Pires, A. La Recherche Qualitative: Enjeux Épistémologiques et Méthodologiques; Gaëtan Morin: Boucherville, QC, Canada, 1997. [Google Scholar]
- Paillé, P.; Mucchielli, A. L’analyse Qualitative en Sciences Humaines et Sociales, 4th ed.; Armand Colin: Paris, France, 2016. [Google Scholar]
- Paré, G.; Sicotte, C. Les Technologies de l’Information et la Transformation de l’Offre de Soins. Cah. Groupe Rech. Système D’Information 2004, 4, 1–25. [Google Scholar]
- Sicotte, C.; Paré, G.; Paccioni, A.; Lehoux, P. Analyse du Risque Associé au Déploiement d’un Dossier Patient Partageable; Université de Montréal: Montreal, QC, Canada, 2004. [Google Scholar]
- Sicotte, C.; Paré, G.; Moreault, M.-P.; Paccioni, A. A risk assessment of two interorganizational clinical information systems. J. Am. Med. Inform. Assoc. 2006, 13, 557–566. [Google Scholar] [CrossRef]
- Albert, V.; Durand, M.; Pepin, G. TRIAGE: Une technique structurée sollicitant l’opinion d’experts en vue d’atteindre un consensus. In Méthodes Qualitatives, Quantitatives et Mixtes: Dans la Recherche en Sciences Humaines, Sociales et de la Santé; Corbière, A., Larivière, N., Eds.; Presse de l’Université du Québec: Québec City, QC, Canada, 2014; pp. 305–326. [Google Scholar]
- Gervais, M.; Pepin, G. Triage: A new group technique gaining recognition in evaluation. Eval. J. Australas. 2002, 2, 45–49. [Google Scholar] [CrossRef]
- Lamontagne, M.-E.; Routhier, F.; Auger, C. Team consensus concerning important outcomes for augmentative and alternative communication assistive technologies: A pilot study. Augment. Altern. Commun. 2013, 29, 182–189. [Google Scholar] [CrossRef]
- Pysklywec, A.; Auger, C.; Gélinas-Bronsard, D.; Bier, N.; Boutin, S.; Demers, L.; Miller, W.C.; Talbot, V.; Ahmed, S. Prioritizing features for an Internet-based intervention for assistive technology users and their caregivers. In Proceedings of the La Journée scientifique et assemblée annuelle REPAR-INTER, Québec City, QC, Canada, 11 May 2018. [Google Scholar]
- Akl, E.; Mustafa, R.; Santesso, N.; Wiercioch, W. Handbook for Grading the Quality of Evidence and the Strength of Recommendations Using the GRADE Approach; Schünemann, H., Brożek, J., Guyatt, G., Oxman, A., Eds.; 2013; Available online: https://gdt.gradepro.org/app/handbook/handbook.html (accessed on 1 November 2020).
- Baumel, A.; Faber, K.; Mathur, N.; Kane, J.M.; Muench, F. Enlight: A Comprehensive Quality and Therapeutic Potential Evaluation Tool for Mobile and Web-Based eHealth Interventions. J. Med. Internet Res. 2017, 19, e82. [Google Scholar] [CrossRef] [PubMed]
- Health on the Net. Health Website Evaluation Tool. Available online: https://www.hon.ch/HONcode/Patients/HealthEvaluationTool.html (accessed on 1 June 2017).
- Silberg, W.M.; Lundberg, G.D.; Musacchio, R.A. Assessing, controlling, and assuring the quality of medical information on the Internet: Caveant lector et viewor—Let the reader and viewer beware. JAMA 1997, 277, 1244–1245. [Google Scholar] [CrossRef] [PubMed]
- Wolfson, N.E.; Cavanagh, T.M.; Kraiger, K. Older adults and technology-based instruction: Optimizing learning outcomes and transfer. Acad. Manag. Learn. Educ. 2014, 13, 26–44. [Google Scholar] [CrossRef]
- Ferreira, B.; Silva, W.; Oliveira, E.A.J.; Conte, T. Designing Personas with Empathy Map. In Proceedings of the SEKE, Pittsburgh, PA, USA, 6–8 July 2015. [Google Scholar]
- Miller, F.; Wallis, J. Social Interaction and the Role of Empathy in Information and Knowledge Management: A Literature Review. J. Educ. Libr. Inf. Sci. 2011, 52, 122–132. [Google Scholar]
- Donetto, S.; Pierri, P.; Tsianakas, V.; Robert, G. Experience-based Co-design and Healthcare Improvement: Realizing Participatory Design in the Public Sector. Des. J. 2015, 18, 227–248. [Google Scholar] [CrossRef]
- Proctor, E.; Raghavan, R.; Hovmand, P.; Bunger, A.; Hensley, M.; Silmere, H.; Aarons, G.; Griffey, R. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Adm. Policy Ment. Health Ment. Health Serv. Res. 2011, 38, 65–76. [Google Scholar] [CrossRef]
- Beauchamp, N.; Irvine, A.B.; Seeley, J.; Johnson, B. Worksite-Based Internet Multimedia Program for Family Caregivers of Persons With Dementia. Gerontologist 2005, 45, 793–801. [Google Scholar] [CrossRef]
- Berk, L.; Berk, M.; Dodd, S.; Kelly, C.; Cvetkovski, S.; Jorm, A.F. Evaluation of the acceptability and usefulness of an information website for caregivers of people with bipolar disorder. BMC Med. 2013, 11, 162. [Google Scholar] [CrossRef]
- Blom, M.M.; Zarit, S.H.; Groot Zwaaftink, R.B.M.; Cuijpers, P.; Pot, A.M. Effectiveness of an Internet intervention for family caregivers of people with dementia: Results of a randomized controlled trial. PLoS ONE 2015, 10, e0116622. [Google Scholar] [CrossRef] [PubMed]
- Bryant, J.; Sanson-Fisher, R.; Stevenson, W.; Smits, R.; Henskens, F.; Wei, A.; Tzelepis, F.; D’Este, C.; Paul, C.; Carey, M. Protocol of a multi-centre randomised controlled trial of a web-based information intervention with nurse-delivered telephone support for haematological cancer patients and their support persons. BMC Cancer 2015, 15, 295. [Google Scholar] [CrossRef] [PubMed]
- Chiang, L.-C.; Chen, W.-C.; Dai, Y.-T.; Ho, Y.-L. The effectiveness of telehealth care on caregiver burden, mastery of stress, and family function among family caregivers of heart failure patients: A quasi-experimental study. Int. J. Nurs. Stud. 2012, 49, 1230–1242. [Google Scholar] [CrossRef]
- Chih, M.-Y.; DuBenske, L.L.; Hawkins, R.P.; Brown, R.L.; Dinauer, S.K.; Cleary, J.F.; Gustafson, D.H. Communicating advanced cancer patients’ symptoms via the Internet: A pooled analysis of two randomized trials examining caregiver preparedness, physical burden, and negative mood. Palliat. Med. 2013, 27, 533–543. [Google Scholar] [CrossRef] [PubMed]
- Chiu, T.; Marziali, E.; Colantonio, A.; Carswell, A.; Gruneir, M.; Tang, M.; Eysenbach, G. Internet-Based Caregiver Support for Chinese Canadians Taking Care of a Family Member with Alzheimer Disease and Related Dementia. Can. J. Aging 2009, 28, 323–336. [Google Scholar] [CrossRef]
- Cox, C.E.; Wysham, N.G.; Walton, B.; Jones, D.; Cass, B.; Tobin, M.; Jonsson, M.; Kahn, J.M.; White, D.B.; Hough, C.L.; et al. Development and usability testing of a Web-based decision aid for families of patients receiving prolonged mechanical ventilation. Ann. Intensive Care 2015, 5, 6. [Google Scholar] [CrossRef]
- Cristancho-Lacroix, V.; Wrobel, J.; Cantegreil-Kallen, I.; Dub, T.; Rouquette, A.; Rigaud, A.-S. A web-based psychoeducational program for informal caregivers of patients with Alzheimer’s disease: A pilot randomized controlled trial. J. Med. Internet Res. 2015, 17, e117. [Google Scholar] [CrossRef]
- Czaja, S.J.; Rubert, M.P. Telecommunications Technology as an Aid to Family Caregivers of Persons With Dementia. Psychosom. Med. 2002, 64, 469–476. [Google Scholar] [CrossRef]
- Dew, M.A.; Goycoolea, J.M.; Harris, R.C.; Lee, A.; Zomak, R.; Dunbar-Jacob, J.; Rotondi, A.; Griffith, B.P.; Kormos, R.L. An internet-based intervention to improve psychosocial outcomes in heart transplant recipients and family caregivers: Development and evaluation. J. Heart Lung Transplant. 2004, 23, 745–758. [Google Scholar] [CrossRef]
- Diefenbach, M.A.; Butz, B.P. A Multimedia Interactive Education System for Prostate Cancer Patients: Development and Preliminary Evaluation. J. Med. Internet Res. 2004, 6, e3. [Google Scholar] [CrossRef]
- DuBenske, L.L.; Gustafson, D.H.; Namkoong, K.; Hawkins, R.P.; Atwood, A.K.; Brown, R.L.; Chih, M.-Y.; McTavish, F.; Carmack, C.L.; Buss, M.K.; et al. CHESS improves cancer caregivers’ burden and mood: Results of an eHealth RCT. Health Psychol. 2014, 33, 1261–1272. [Google Scholar] [CrossRef] [PubMed]
- Ducharme, F.; Dubé, V.; Lévesque, L.; Saulnier, D.; Giroux, F. An Online Stress Management Training Program as a Supportive Nursing Intervention for Family Caregivers of an Elderly Person. Can. J. Nurs. Inform. 2011, 6. [Google Scholar]
- Eames, S.; Hoffmann, T.; Worrall, L.; Read, S.; Wong, A. Randomised controlled trial of an education and support package for stroke patients and their carers. BMJ Open 2013, 3. [Google Scholar] [CrossRef] [PubMed]
- Glueckauf, R.L.; Ketterson, T.U.; Loomis, J.S.; Dages, P. Online Support and Education for Dementia Caregivers: Overview, Utilization, and Initial Program Evaluation. Telemed. J. e-Health 2004, 10, 223–232. [Google Scholar] [CrossRef]
- Glueckauf, R.L.; Loomis, J.S. Alzheimer’s Caregiver Support Online: Lessons learned, initial findings and future directions. NeuroRehabilitation 2003, 18, 135–146. [Google Scholar] [CrossRef] [PubMed]
- Glynn, S.M.; Randolph, E.T.; Garrick, T.; Lui, A. A proof of concept trial of an online psychoeducational program for relatives of both veterans and civilians living with schizophrenia. Psychiatr. Rehabil. J. 2010, 33, 278–287. [Google Scholar] [CrossRef]
- Griffiths, P.C.; Parmelee, P.; Johnson Ii, T.M. Using telehealth technology to support family caregivers: Description of a pilot intervention and preliminary results. Gerontechnology 2010, 9, 213. [Google Scholar] [CrossRef]
- Haigh, K.Z.; Kiff, L.M.; Ho, G. The Independent LifeStyle Assistant: Lessons Learned. Assist. Technol. 2006, 18, 87–106. [Google Scholar] [CrossRef]
- Hanson, E.J.; Tetlely, J.; Shewan, J. Supporting family carers using interative multimedia. Br. J. Nurs. 2000, 9, 713–719. [Google Scholar] [CrossRef]
- Huang, Y.-C.; Hsu, Y.-L. Social networking-based personal home telehealth system: A pilot study. J. Clin. Gerontol. Geriatr. 2014, 5, 132–139. [Google Scholar] [CrossRef]
- Kajiyama, B.; Thompson, L.W.; Eto-Iwase, T.; Yamashita, M.; Di Mario, J.; Marian Tzuang, Y.; Gallagher-Thompson, D. Exploring the effectiveness of an Internet-based program for reducing caregiver distress using the iCare Stress Management e-Training Program. Aging Ment. Health 2013, 17, 544–554. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.I.; Lee, S.; Kim, J.H. Effects of a web-based stroke education program on recurrence prevention behaviors among stroke patients: A pilot study. Health Educ. Res. 2013, 28, 488–501. [Google Scholar] [CrossRef] [PubMed]
- Kwok, T.; Au, A.; Wong, B.; Ip, I.; Mak, V.; Ho, F. Effectiveness of online cognitive behavioral therapy on family caregivers of people with dementia. Clin. Interv. Aging 2014, 2014, 631–636. [Google Scholar] [CrossRef] [PubMed]
- Lewis, M.L.; Hobday, J.V.; Hepburn, K.W. Internet-Based Program for Dementia Caregivers. Am. J. Alzheimer’s Dis. Other Dement. 2010, 25, 674–679. [Google Scholar] [CrossRef] [PubMed]
- Lexis, M.; Everink, I.; van der Heide, L.; Spreeuwenberg, M.; Willems, C.; de Witte, L. Activity monitoring technology to support homecare delivery to frail and psychogeriatric elderly persons living at home alone. Technol. Disabil. 2013, 25, 189–198. [Google Scholar] [CrossRef]
- Lorig, K.; Thompson-Gallagher, D.; Ritter, P.L.; Laurent, D.D.; Plant, K.; Thompson, L.W.; Traylor, L.; Hahn, T.J. Building better caregivers: A pilot online support workshop for family caregivers of cognitively impaired adults. J. Appl. Gerontol. 2012, 31, 423–437. [Google Scholar] [CrossRef]
- Lundberg, S. The results from a two-year case study of an information and communication technology support system for family caregivers. Disabil. Rehabil. Assist. Technol. 2014, 9, 353–358. [Google Scholar] [CrossRef]
- Magnusson, L.; Hanson, E.; Brito, L.; Berthold, H.; Chambers, M.; Daly, T. Supporting family carers through the use of information and communication technology-the EU project ACTION. Int. J. Nurs. Stud. 2002, 39, 369–381. [Google Scholar] [CrossRef]
- Mahoney, D.M.F.; Mutschler, P.H.; Tarlow, B.; Liss, E. Real world implementation lessons and outcomes from the Worker Interactive Networking (WIN) project: Workplace-based online caregiver support and remote monitoring of elders at home. Telemed. J. e-Health Off. J. Am. Telemed. Assoc. 2008, 14, 224–234. [Google Scholar] [CrossRef]
- Marziali, E.; Donahue, P. Caring for Others: Internet Video-Conferencing Group Intervention for Family Caregivers of Older Adults with Neurodegenerative Disease. Gerontologist 2006, 46, 398–403. [Google Scholar] [CrossRef]
- Marziali, E.; Garcia, L. Dementia Caregivers’ Responses to 2 Internet-Based Intervention Programs. Am. J. Alzheimer’s Dis. Other Dement. 2011, 26, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, K.; Antoku, Y.; Inoue, R.; Kobayashi, M.; Hanada, E.; Iwasaki, Y.; Kumagai, Y.; Iwamoto, H.; Tsuchihashi, S.; Iwaki, M.; et al. A Network System of Medical and Welfare Information Service for the Patients, Their Families, Hospitals, Local Governments, and Commercial Companies in a Medical Service Area. J. Med. Syst. 2002, 26, 249–254. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, K.A.; Glang, A.; Beaver, S.V.; Gau, J.M.; Keen, S. Web-based training in family advocacy. J. Head Trauma Rehabil. 2013, 28, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Moen, A.; Smørdal, O. Informatics-based learning resources for patients and their relatives in recovery. Stud. Health Technol. Inform. 2006, 122, 44–48. [Google Scholar]
- Nahm, E.-S.; Resnick, B.; Orwig, D.; Magaziner, J.; Bellantoni, M.; Sterling, R.; Brennan, P.F. A theory-based online hip fracture resource center for caregivers: Effects on dyads. Nurs. Res. 2012, 61, 413–422. [Google Scholar] [CrossRef]
- Namkoong, K.; DuBenske, L.L.; Shaw, B.R.; Gustafson, D.H.; Hawkins, R.P.; Shah, D.V.; McTavish, F.M.; Cleary, J.F. Creating a Bond Between Caregivers Online: Effect on Caregivers’ Coping Strategies. J. Health Commun. 2012, 17, 125–140. [Google Scholar] [CrossRef]
- Ossebaard, H.C.; van Gemert-Pijnen, L.; Seydel, E.R. Online usability and patients with long-term conditions: A mixed-methods approach. Int. J. Med. Inform. 2012, 81, 374–387. [Google Scholar] [CrossRef]
- Pagán-Ortiz, M.E.; Cortés, D.E.; Rudloff, N.; Weitzman, P.; Levkoff, S. Use of an Online Community to Provide Support to Caregivers of People With Dementia. J. Gerontol. Soc. Work. 2014, 57, 694–709. [Google Scholar] [CrossRef]
- Pierce, L.L.; Steiner, V. Usage and design evaluation by family caregivers of a stroke intervention web site. J. Neurosci. Nurs. 2013, 45, 254–261. [Google Scholar] [CrossRef]
- Pierce, L.L.; Steiner, V.; Govoni, A.L. In-home online support for caregivers of survivors of stroke: A feasibility study. Comput. Inform. Nurs. 2002, 20, 157–164. [Google Scholar] [CrossRef]
- Pierce, L.L.; Steiner, V.; Govoni, A.L.; Hicks, B.; Thompson, T.L.C.; Friedemann, M.-L. Internet-based Support for Rural Caregivers of Persons with Stroke Shows Promise. Rehabil. Nurs. 2004, 29, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Pierce, L.L.; Steiner, V.L.; Khuder, S.A.; Govoni, A.L.; Horn, L.J. The effect of a Web-based stroke intervention on carers’ well-being and survivors’ use of healthcare services. Disabil. Rehabil. 2009, 31, 1676–1684. [Google Scholar] [CrossRef] [PubMed]
- Rentz, M.; Von Hoene, A. Online Coaching for Caregivers: Using Technology to Provide Support and Information. Alzheimer’s Care Today 2010, 11, 206–209. [Google Scholar]
- Rochette, A.; Korner-Bitensky, N.; Tremblay, V.; Kloda, L. Stroke rehabilitation information for clients and families: Assessing the quality of the StrokEngine-Family website. Disabil. Rehabil. 2008, 30, 1506–1512. [Google Scholar] [CrossRef]
- Rotondi, A.J.; Sinkule, J.; Spring, M. An interactive Web-based intervention for persons with TBI and their families: Use and evaluation by female significant others. J. Head Trauma Rehabil. 2005, 20, 173–185. [Google Scholar] [CrossRef]
- Sabat, S.R. Flourishing of the self while caregiving for a person with Dementia: A case study of education, counseling, and psychosocial support via email. Dementia 2011, 10, 81–97. [Google Scholar] [CrossRef]
- Sander, A.M.; Clark, A.N.; Atchison, T.B.; Rueda, M. A Web-Based Videoconferencing Approach to Training Caregivers in Rural Areas to Compensate for Problems Related to Traumatic Brain Injury. J. Head Trauma Rehabil. 2009, 24, 248–261. [Google Scholar] [CrossRef]
- Sin, J.; Henderson, C.; Norman, I. Usability of online psychoeducation for siblings of people with psychosis. Int. J. Technol. Assess. Health Care 2015, 30, 374–380. [Google Scholar] [CrossRef]
- Smith, G.C.; Dellman-Jenkins, M.; Egbert, N.; Nanna, K.; Palmieri, P.A. Reducing depression in stroke survivors and their informal caregivers: A randomized clinical trial of a web-based intervention. Rehabil. Psychol. 2012, 57, 196–206. [Google Scholar] [CrossRef]
- Steiner, V.; Pierce, L.L. Building a web of support for caregivers of persons with stroke. Top. Stroke Rehabil. 2002, 9, 102–111. [Google Scholar] [CrossRef]
- Torkamani, M.; McDonald, L.; Saez Aguayo, I.; Kanios, C.; Katsanou, M.-N.; Madeley, L.; Limousin, P.D.; Lees, A.J.; Haritou, M.; Jahanshahi, M.; et al. A randomized controlled pilot study to evaluate a technology platform for the assisted living of people with dementia and their carers. J. Alzheimer’s Dis. 2014, 41, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Torp, S.; Bing-Jonsson, P.C.; Hanson, E. Experiences with using information and communication technology to build a multi-municipal support network for informal carers. Inform. Health Soc. Care 2013, 38, 265–279. [Google Scholar] [CrossRef] [PubMed]
- Torp, S.; Hanson, E.; Hauge, S.; Ulstein, I.; Magnusson, L. A pilot study of how information and communication technology may contribute to health promotion among elderly spousal carers in Norway. Health Soc. Care Community 2008, 16, 75–85. [Google Scholar] [CrossRef]
- Van der Roest, H.G.; Meiland, F.J.M.; Jonker, C.; Dröes, R.M. User evaluation of the DEMentia-specific Digital Interactive Social Chart (DEM-DISC). A pilot study among informal carers on its impact, user friendliness and, usefulness. Aging Ment. Health 2010, 14, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Zulman, D.M.; Schafenacker, A.; Barr, K.L.; Moore, I.T.; Fisher, J.; McCurdy, K.; Derry, H.A.; Saunders, E.W.; An, L.C.; Northouse, L. Adapting an in-person patient-caregiver communication intervention to a tailored web-based format. Psycho-Oncology 2012, 21, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.; Gélinas-Bronsard, D.; Alliche, Z.; Pysklywec, A.; Ahmed, S.; Auger, C. Co-construire des outils efficaces de transfert des connaissances pour une utilisation appropriée des aides à la mobilité. In Proceedings of the 17e Carrefour des Connaissances en Déficience Motrice, Sensorielle, et du Langage, Montréal, QC, Canada, 6 June 2019. [Google Scholar]
- Wang, R.H.; Kenyon, L.K.; McGilton, K.S.; Miller, W.C.; Hovanec, N.; Boger, J.; Viswanathan, P.; Robillard, J.M.; Czarnuch, S.M. The Time Is Now: A FASTER Approach to Generate Research Evidence for Technology-Based Interventions in the Field of Disability and Rehabilitation. Arch. Phys. Med. Rehabil. 2021, 102, 1848–1859. [Google Scholar] [CrossRef]
- Bergström, A.L.; Hanson, E. An integrative review of information and communication technology based support interventions for carers of home dwelling older people. Technol. Disabil. 2017, 29, 1–14. [Google Scholar] [CrossRef]
- Luo, X.; Gao, L.; Li, J.; Lin, Y.; Zhao, J.; Li, Q. A critical literature review of dyadic web-based interventions to support cancer patients and their caregivers, and directions for future research. Psycho-Oncology 2020, 29, 38–48. [Google Scholar] [CrossRef]
- Murray, E.; Treweek, S.; Pope, C.; MacFarlane, A.; Ballini, L.; Dowrick, C.; Finch, T.; Kennedy, A.; Mair, F.; O’Donnell, C.; et al. Normalisation process theory: A framework for developing, evaluating and implementing complex interventions. BMC Med. 2010, 8, 63. [Google Scholar] [CrossRef]
- Moller, A.C.; Merchant, G.; Conroy, D.E.; West, R.; Hekler, E.; Kugler, K.C.; Michie, S. Applying and advancing behavior change theories and techniques in the context of a digital health revolution: Proposals for more effectively realizing untapped potential. J. Behav. Med. 2017, 40, 85–98. [Google Scholar] [CrossRef]
- Heesen, R.; Bright, L.K.; Zucker, A. Vindicating methodological triangulation. Synthese 2019, 196, 3067–3081. [Google Scholar] [CrossRef]

| Step | Description | |
|---|---|---|
 | STEP 1: Logic Model of the Problem |
|
| STEP 2: Program Outcomes and Objectives; Logic Model of Change |
| |
| STEP 3: Project Design |
| |
| STEP 4: Program Production |
| |
| STEP 5: Program Implementation Plan |
| |
| STEP 6: Evaluation Plan |
|
| Component | Rank | Supporting Literature |
|---|---|---|
| Monitoring components | ||
| Self-report questionnaires—Online | 2 | [43,48,54,55,80,87,89,95,99] |
| Self-report questionnaires—Interactive voice-response system | 4 | [16] |
| Self-report questionnaires—SMS | 6 | None |
| Sensors recording AT use | 7 | None |
| eExpert components | ||
| Clinician support by telephone (synchronous) | 3 | [47,61,72,87,89] |
| Clinician support by video conferencing (synchronous) | 8 | [72,73,90,95] |
| Clinical alerts | 12 | [69,95] |
| Clinician report | 14 | [48,54,55,80] |
| Clinician support by email (asynchronous) | 16 | [46,49,66,73,74,83,84,85,86,87,90,93,94] |
| Ask an expert section (asynchronous) | 26 | [48,53,55,79,80,82,89,92,94,95] |
| Technical support by phone | 28 | [48,55,73,77,83,84,85,86,90] |
| Technical support by email | 35 | [73,77,81,89] |
| Technical support button | None | [92] |
| Resources & Training components | ||
| Skill-based videos | 1 | [65,77] |
| Decision aids | 5 | [50,54] |
| Data base of accessible public places | 9 | None |
| Written educational material | 11 | [43,45,46,48,51,53,55,56,57,63,68,70,71,74,75,77,78,79,80,81,83,84,85,86,88,89,90,91,92,94,96,97,98] |
| Educational videos | 15 | [45,54,60,63,68,71,75,78,79,82] |
| Interactive and thematic classes | 17 | [51,58,59,66,67,91] |
| Written caregiver tips | 19 | [48,55,80,82] |
| Resource directory | 21 | [44,48,52,53,55,63,80,82,87,89] |
| List of relevant web links | 29 | [47,48,53,55,58,59,60,66,70,73,76,77,80,82,83,84,85,86,92,93,94,96] |
| Frequently asked questions (FAQ) section | 31 | [48,53,55,59,80,92] |
| Videos with testimonials | 33 | [43,54] |
| Instant library | 35 | [48,53,54,55,58,59,77,79,80,87] |
| Facebook and Twitter links | 35 | [64,81,82] |
| Reminders | 36 | [50,52,62,90] |
| References library | None | [53,58,59,89] |
| Search bar | None | [81,93] |
| Online quizzes/homework | None | [45,56,63,66,70,79,93] |
| Variables | Sub-Variables | Measurement Tool/Source | AT user | Caregiver | Coordinator | Management | Administration Time (min) | |||
|---|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | T2 | T3 | |||||||
| Clinical variables | ||||||||||
| Problems | No. detected problems No. resolved issues | Automated questionnaires | X | X | 8 | 8 | ||||
| Satisfaction with AT | General satisfaction Satisfaction with AT characteristics Satisfaction with online AT services | QUEST | X | 10 | 10 | |||||
| Satisfaction with participation with AT | Importance of mobility assistance and satisfaction with activities carried out inside and outside. Satisfaction with the positioning. State of the skin. | WhOM | X | 10 | 10 | |||||
| Impacts AT on caregiver | Field and type of assistance Stressors and burden of AT use Impacts on physical health Impacts on quality of life | CATOM | X | 15 | 15 | |||||
| Knowledge | What knowledge did you learn with the follow-up intervention? | End of intervention interview | X | X | 15 | |||||
| Behaviors | Tell me about your new ways of doing things or new activities that you have done after seeing the resources provided by MOvIT+™? | |||||||||
| Implementation variables | ||||||||||
| Relevance | Compatibility Perceived utility/added value of the intervention Sample questions: What are your expectations of the MOvIT+™ project in the short and long term (earnings)? What are the difficulties you expect to encounter with MOvIT+™ (Brake/Loss) | Meeting of managers | X | 30 | ||||||
| Values map | X | 30 | 30 | |||||||
| Acceptability | Perceived usability Intent to use Satisfaction with the intervention Sample questions: How do you describe the utility of MOvIT+™? What other problems could be improved by MOvIT+™ (earnings)? | End of intervention interview | X | X | 15 | |||||
| Feedback at 6 weeks between T1 and T4 | X | 15 | ||||||||
| Feasibility | Rate of intervention adoption by sites and reasons for refusal | Recruitment tracking diagram | N/A | Extracting data from the interface | ||||||
| Rate of refusal/exclusion of users and caregivers and characteristics (age, site, AT) | ||||||||||
| Attrition rate and reasons for abandonment | Follow-up chart of abandonments | |||||||||
| Rate of participation in the intervention | Navigation data on the site MOvIT+™ | |||||||||
| Fidelity | Adherence to the intervention protocol | MOvIT+™ navigation data | N/A | Extracting data from the interface | ||||||
| Dosage | ||||||||||
| Costs | Consultations related to the detected problems | Statistics extracted from the purchase orders and clinical notes found in patients’ records | N/A | N/A | ||||||
| AT Repairs | ||||||||||
| Use of health services | Patients’ records summary; convert service time into economic value | |||||||||
| Technology | Reports of web hosting costs, hardware, technical support resources and TelASK Inc. automated service. | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Auger, C.; Guay, C.; Pysklywec, A.; Bier, N.; Demers, L.; Miller, W.C.; Gélinas-Bronsard, D.; Ahmed, S. What’s behind the Dashboard? Intervention Mapping of a Mobility Outcomes Monitoring System for Rehabilitation. Int. J. Environ. Res. Public Health 2022, 19, 13303. https://doi.org/10.3390/ijerph192013303
Auger C, Guay C, Pysklywec A, Bier N, Demers L, Miller WC, Gélinas-Bronsard D, Ahmed S. What’s behind the Dashboard? Intervention Mapping of a Mobility Outcomes Monitoring System for Rehabilitation. International Journal of Environmental Research and Public Health. 2022; 19(20):13303. https://doi.org/10.3390/ijerph192013303
Chicago/Turabian StyleAuger, Claudine, Cassioppée Guay, Alex Pysklywec, Nathalie Bier, Louise Demers, William C. Miller, Dominique Gélinas-Bronsard, and Sara Ahmed. 2022. "What’s behind the Dashboard? Intervention Mapping of a Mobility Outcomes Monitoring System for Rehabilitation" International Journal of Environmental Research and Public Health 19, no. 20: 13303. https://doi.org/10.3390/ijerph192013303
APA StyleAuger, C., Guay, C., Pysklywec, A., Bier, N., Demers, L., Miller, W. C., Gélinas-Bronsard, D., & Ahmed, S. (2022). What’s behind the Dashboard? Intervention Mapping of a Mobility Outcomes Monitoring System for Rehabilitation. International Journal of Environmental Research and Public Health, 19(20), 13303. https://doi.org/10.3390/ijerph192013303







