Impact of Depsychopathologization of Transgender and Gender Diverse Individuals in ICD-11 on Care Delivery: Looking at Trans Expertise through a Trans Lens
Abstract
1. Introduction
2. Materials and Methods
2.1. Epistemic Challenges
2.2. Ethical Conformity
2.3. Materials
2.4. Analyses
- -
- Each word’s form in the corpus is recognized and, after an initial part-of-speech tagging, lemmatized, replacing them with the associated lemma.
- -
- The corpus is segmented in elementary context units (ecu) following a pre-established set of rules [30], allowing for lemmas to be analyzed in semantic context.
- -
- The ecu are segmented to build a grid for analysis.
3. Results
3.1. Description of Participants
3.2. Lexical Analysis of Participants’ Recommendations
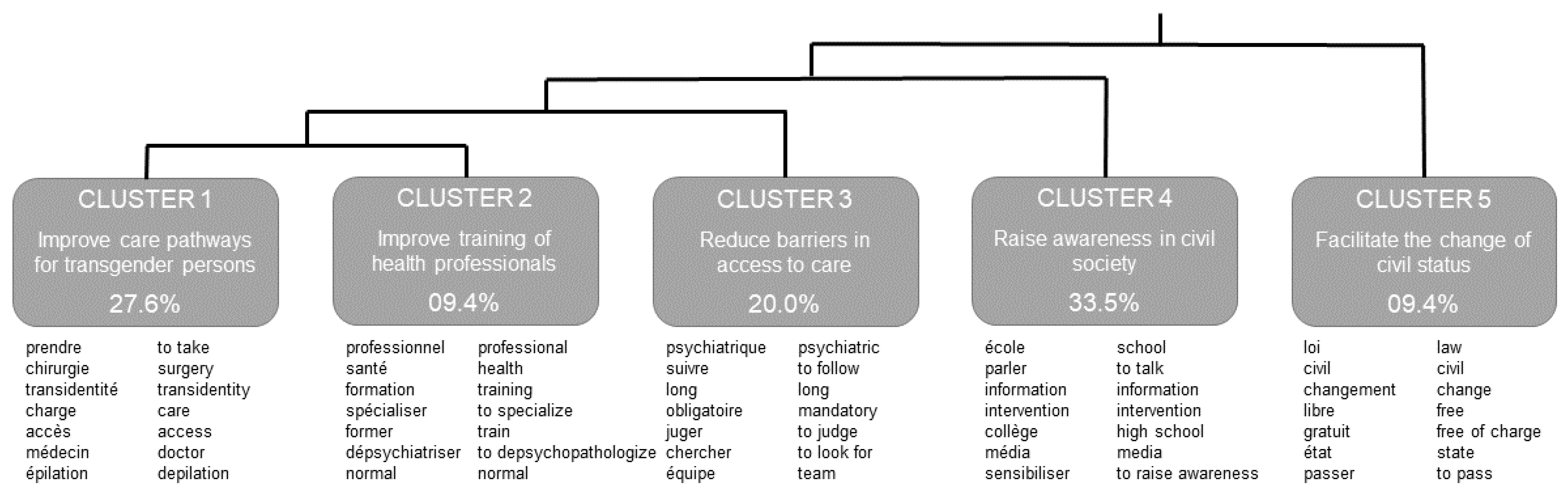
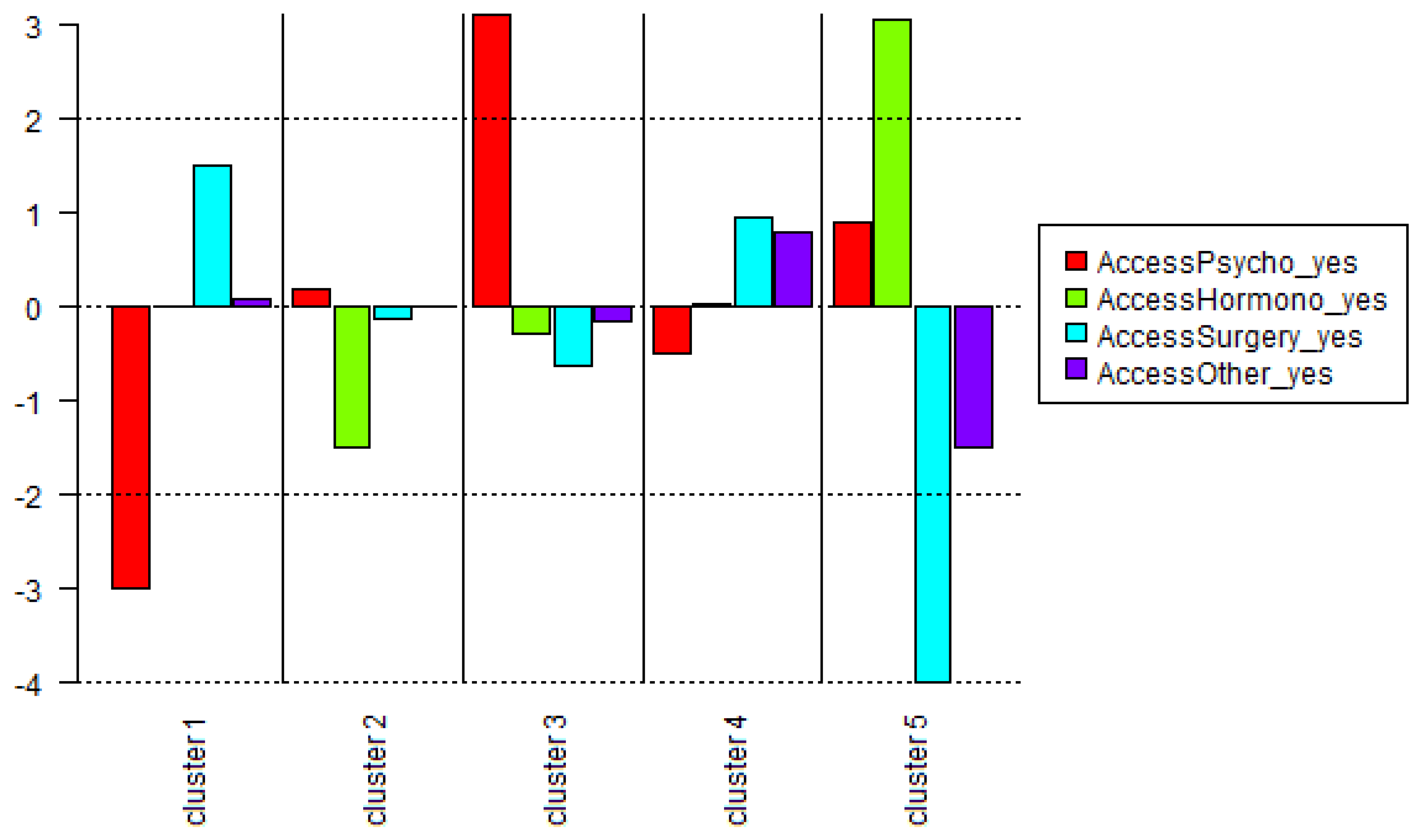
3.3. First Descending Hierarchical Classification
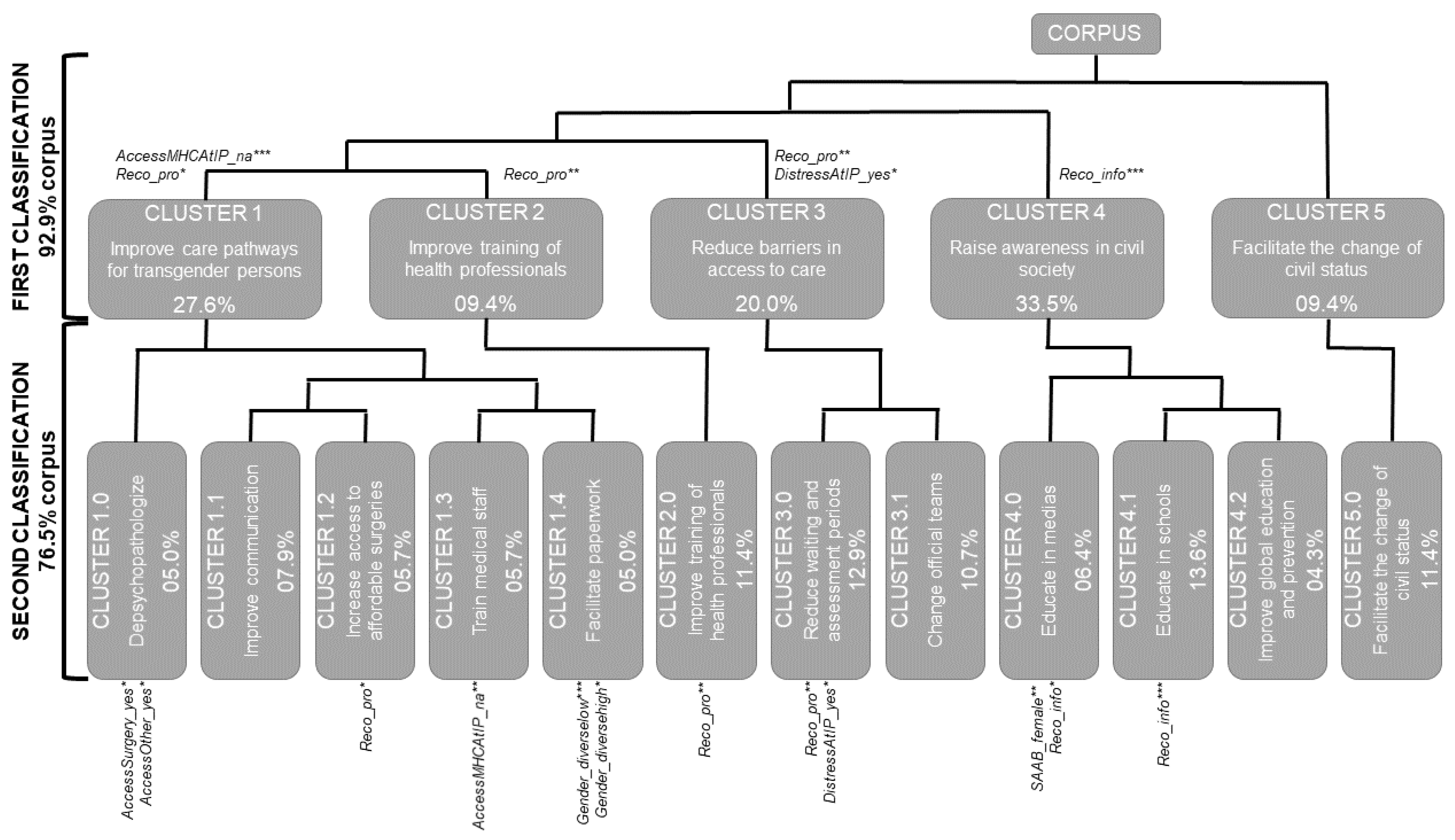
3.4. Second Descending Hierarchical Classification
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thorne, N.; Yip, A.K.T.; Bouman, W.P.; Marshall, E.; Arcelus, J. The terminology of identities between, outside and beyond the gender binary–A systematic review. Int. J. Transgenderism 2019, 20, 138–154. [Google Scholar] [CrossRef] [PubMed]
- Cruz, T.M. Assessing access to care for transgender and gender nonconforming people: A consideration of diversity in combating discrimination. Soc. Sci. Med. 2014, 110, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Reisner, S.L.; Poteat, T.; Keatley, J.; Cabral, M.; Mothopeng, T.; Dunham, E.; E Holland, C.; Max, R.; Baral, S.D. Global health burden and needs of transgender populations: A review. Lancet 2016, 388, 412–436. [Google Scholar] [CrossRef]
- Wylie, K.; Knudson, G.; Khan, S.I.; Bonierbale, M.; Watanyusakul, S.; Baral, S. Serving transgender people: Clinical care considerations and service delivery models in transgender health. Lancet 2016, 388, 401–411. [Google Scholar] [CrossRef]
- Baleige, A.; de la Chenelière, M.; Dassonneville, C.; Martin, M.-J. Following ICD-11, Rebuilding Mental Health Care for Transgender Persons: Leads from Field Experimentations in Lille, France. Transgender Health 2021, 1, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Davy, Z.; Sørlie, A.; Schwend, A.S. Democratising diagnoses? The role of the depathologisation perspective in constructing corporeal trans citizenship. Crit. Soc. Policy 2018, 38, 13–34. [Google Scholar] [CrossRef]
- Castro-Peraza, M.E.; García-Acosta, J.M.; Delgado, N.; Perdomo-Hernández, A.M.; Sosa-Alvarez, M.I.; Llabrés-Solé, R.; Lorenzo-Rocha, N.D. Gender Identity: The Human Right of Depathologization. Int. J. Environ. Res. Public Health 2019, 16, 978. [Google Scholar] [CrossRef]
- Baleige, A.; Guernut, M. Constructing a new epistemology of transgender persons: Impact of gender studies on mental health ideologies. Implic. Philos. 2021. Available online: http://www.implications-philosophiques.org/constructing-a-new-epistemology-of-transgender-persons-impact-of-gender-studies-on-mental-health-ideologies (accessed on 1 August 2022).
- Robles, R.; Keeley, J.W.; Vega-Ramírez, H.; Cruz-Islas, J.; Rodríguez-Pérez, V.; Sharan, P.; Purnima, S.; Rao, R.; Rodrigues-Lobato, M.I.; Soll, B.; et al. Validity of Categories Related to Gender Identity in ICD-11 and DSM-5 Among Transgender Individuals who Seek Gender-Affirming Medical Procedures. Int. J. Clin. Health Psychol. 2022, 22, 100281. [Google Scholar] [CrossRef] [PubMed]
- Askevis-Leherpeux, F.; De La Chenelière, M.; Baleige, A.; Chouchane, S.; Martin, M.-J.; Robles-García, R.; Fresán, A.; Quach, A.; Stona, A.-C.; Reed, G.; et al. Why and how to support depsychiatrisation of adult transidentity in ICD-11: A French study. Eur. Psychiatry 2019, 59, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Robles, R.; Fresán, A.; Vega-Ramirez, E.H.; Cruz-Islas, J.; Rodriguez, V.; Domínguez, T.; Reed, G.M. Removing transgender identity from the classification of mental disorders: A Mexican field study for ICD-11. Lancet Psychiatry 2016, 3, 850–859. [Google Scholar] [CrossRef]
- Rood, B.A.; Reisner, S.L.; Surace, F.I.; Puckett, J.A.; Maroney, M.R.; Pantalone, D.W. Expecting Rejection: Understanding the Minority Stress Experiences of Transgender and Gender-Nonconforming Individuals. Transgender Health 2016, 1, 151–164. [Google Scholar] [CrossRef]
- Reed, G.M. Vers la CIM-11: Créer un espace pour une diversité de perspectives. Inf. Psychiatr. 2011, 87, 169. [Google Scholar] [CrossRef]
- De la Chenelière, M. From patient to researcher: Personal empowerment journey related to transidentity. Inf. Psychiatr. 2018, 94, 817–823. [Google Scholar] [CrossRef]
- Rose, D. Participatory research: Real or imagined. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 765–771. [Google Scholar] [CrossRef]
- Rose, D. Survivor-produced knowledge; This is survivor research. In Ross-on-Wye; Sweeney, A., Beresford, P., Faulkner, A., Nettle, M., Rose, D., Eds.; PCCS Books: Monmouth, UK, 2009; pp. 38–43. [Google Scholar]
- Giami, A.; Nayak, L. Controverses dans les prises en charge des situations trans: Une ethnographie des conférences médico-scientifiques. Sci. Soc. Sante 2019, 37, 39–64. [Google Scholar] [CrossRef]
- Stroumsa, D.; Shires, D.A.; Richardson, C.R.; Jaffee, K.D.; Woodford, M.R. Transphobia rather than education predicts provider knowledge of transgender health care. Med. Educ. 2019, 53, 398–407. [Google Scholar] [CrossRef]
- Friedrich, C.; Filippelli, A. The transgender lens is underrepresented and overlooked in transgender health research to the detriment of the population it seeks to serve. J. Women’s Health 2019, 28, 111. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Patients for Patient Safety [Internet]; World Health Organization: Geneva, Switzerland, 2006.
- Borkman, T. Experiential Knowledge: A New Concept for the Analysis of Self-Help Groups. Soc. Serv. Rev. 1976, 3, 445–456. [Google Scholar] [CrossRef]
- Fairclough, N. Language and Power, 3rd ed.; Routledge: London, UK, 2015; pp. 1–264. [Google Scholar]
- Fricker, M.; Jenkins, K. Epistemic Injustice, Ignorance, and Trans Experiences. In The Routledge Companion to Feminist Philosophy; Garry, A., Khader, S.J., Stone, A., Eds.; Routledge Companion to Feminist Philosophy: London, UK, 2017. [Google Scholar]
- Sweeney, A.; Beresford, P.; Faulkner, A.; Nettle, M.; Rose, D. This is survivor research. In Ross-on-Wye; PCCS Books: Monmouth, UK, 2009; pp. 1–200. [Google Scholar]
- Ozolins, U.; Hale, S.; Cheng, X.; Hyatt, A.; Schofield, P. Translation and back-translation methodology in health research–a critique. Expert Rev. Pharm. Outcomes Res. 2020, 20, 69–77. [Google Scholar] [CrossRef]
- World Health Organization. Translation and Linguistic Evaluation Protocol and Supporting Material. Man WHO Disabil Assess Sched WHODAS 20; World Health Organization: Geneva, Switzerland, 2010; pp. 1–8.
- Winter, S.; Diamond, M.; Green, J.; Karasic, D.; Reed, T.; Whittle, S.; Wylie, K. Transgender people: Health at the margins of society. Lancet 2016, 388, 390–400. [Google Scholar] [CrossRef]
- Callander, D.; Newman, C.E.; Holt, M.; Rosenberg, S.; Duncan, D.T.; Pony, M.; Timmins, L.; Cornelisse, V.; Duck-Chong, L.; Wang, B.; et al. The Complexities of Categorizing Gender: A Hierarchical Clustering Analysis of Data from the First Australian Trans and Gender Diverse Sexual Health Survey. Transgender Health 2021, 6, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Camargo, B.V.; Justo, A.M.; Forte, T. Iramuteq: R Interface for Multidimensional Analysis of Texts and Questionnaires [Internet]. 2016. Available online: http://www.iramuteq.org/documentation/fichiers/IRaMuTeQ%20Tutorial%20translated%20to%20English_17.03.2016.pdf (accessed on 1 August 2022).
- Reinert, M. Alceste une méthodologie d’analyse des données textuelles et une application: Aurelia De Gerard De Nerval. Bull. De Méthodologie Sociol. 1990, 26, 24–54. [Google Scholar] [CrossRef]
- Preciado, P.B. Je Suis un Monstre qui Vous Parle; Grasset: Paris, France, 2020; pp. 67–88. [Google Scholar]
- Kuhn, T. The Structure of Scientific Revolutions, 4 ed.; University of Chicago Press: Chicago, IL, USA, 2015. [Google Scholar]
- Baleige, A.; Guernut, M.; Denis, F. Trans Expertise and the Revision and Translation of ICD-11: An Analysis of Available French Data from a Trans Perspective. Int. J. Environ. Res. Public Health 2022, 19, 1983. [Google Scholar] [CrossRef]
- Fallery, B.; Rodhain, F. Quatre approches pour l’analyse de données textuelles: Lexicale, linguistique, cognitive, thématique. In XVIème Conférence Internationale de Management Stratégique; AIMS: Montreal, QC, Canada, 2007; p. 16. [Google Scholar]
- Khelifi, H. La lexicométrie: Un outil efficient pour l’analyse du discours. In Colloque International Médias Numériques, Langues, Discours, Pratiques et Interculturalité; Open Science: Agadir, Morocco, 2016; p. 161. [Google Scholar]
- Van Heesewijk, J.; Kent, A.; van de Grift, T.C.; Harleman, A.; Muntinga, M. Transgender health content in medical education: A theory-guided systematic review of current training practices and implementation barriers & facilitators. Adv. Health Sci. Educ. Theory Pr. 2022, 27, 817–846. [Google Scholar] [CrossRef]
- Bret, L. Sexe et genre: Réflexions sur la place de la volonté individuelle dans l’état civil. In Les Mutations Contemporaines du Droit de la Famille; Bernard, S., Farge, M., Eds.; Presses Universitaires de Grenoble: Grenoble, France, 2020; pp. 11–18. [Google Scholar]
- Lupton, D. Discourse analysis: A new methodology for understanding the ideologies of health and illness. Aust. J. Public Health 1992, 16, 145–150. [Google Scholar] [CrossRef] [PubMed]
| Total Sample (n = 72) | Women (n = 34) | Men (n = 22) | Gender Diverse (n = 16) | |
|---|---|---|---|---|
| Mean (SD; Range) | ||||
| Age (years) | 27.7 (9.7; 18–50) | 31.6 (11.6; 18–50) | 22.6 (4.5; 18–34) | 26.2 (6.8; 18–47) |
| Education (years) | 13.7 (2.5; 9–20) | 13.6 (2.6; 9–20) | 13.4 (2.5; 9–18) | 14.7 (2.3; 10–17) |
| Life-long care linked to gender identity | ||||
| n (%); Mean (SD; Range) | ||||
| Any healthcare | 65 (90.3%) | 31 (91.2%) | 20 (90.9%) | 14 (87.5%) |
| Delay before study (years) a | 1.5 (2.9; 0–15) | 1.8 (3.6; 0–15) | 1.3 (2.5; 0–10) | 1.1 (1.0; 0–3) |
| Psychological Support | 34 (47.2%) | 18 (52.9%) | 9 (40.9%) | 7 (43.8%) |
| Delay before study (years) a | 3.7 (4.1; 0–19) | 4.6 (5.1; 0–19) | 2.7 (2.6; 0–6) | 2.7 (2.4; 0–6) |
| Hormonal treatment | 60 (83.3%) | 28 (82.4%) | 19 (86.4%) | 13 (81.3%) |
| Delay before study (years) a | 2.8 (5.4; 0–27) | 4.1 (7.3; 0–27) | 1.8 (3.0; 0–11) | 1.5 (1.3; 0–4) |
| Surgery | 23 (31.9%) | 11 (32.4%) | 8 (36.4%) | 4 (25%) |
| Delay before study (years) a | 3 (4.7; 0–17) | 4.0 (6.1; 0–17) | 2.5 (3.6; 0–10) | 1.3 (1.0; 0–2) |
| Other | 25 (34.7%) | 20 (58.8%) | 1 (4.5%) | 4 (25%) |
| Delay before study (years) a | 2.4 (4.4; 0–16) | 2.9 (4.9; 0–16) | 0.0 | 0.8 (1.0; 0–2) |
| Psychological distress linked to gender identity at Index Period | ||||
| n (%); Mean (SD; Range) | ||||
| Age at Index Period (years) | 10.7 (7.1; 3–40) | 11.8 (7.7; 3–40) | 9.3 (4.8; 3–22) | 10.4 (8.5; 4–40) |
| Experience of psychological distress | 61 (84.7%) | 27 (79.4%) | 21 (95.5%) | 13 (81.3%) |
| Sought mental health care b | 21 (34.4%) | 7 (25.9%) | 10 (47.6%) | 4 (30.8%) |
| Received mental health care c | 21 (100.0%) | 7 (100.0%) | 10 (100.0%) | 4 (100.0%) |
| Delay before study (years) | 14.0 (8.1; 5–45) | 16.4 (13.0; 5–45) | 11.5 (3.6; 7–17) | 15.8 (4.6; 10–20) |
| Cluster | Representative Quotes (Gender; Set) |
|---|---|
| 1. Improve care pathways for transgender persons | Changer la classification dans la CIM ** pour ne plus être obligé de passer par les psychiatres. Change the classification in the ICD ** so that you don’t have to go through the psychiatrists anymore. (man; how health professionals can better respond) |
| Développer les soins ** et structures pour les trans (chirurgie ***, épilation **, etc…). Develop care *** and structures for trans people (surgery ***, hair removal **, etc...). (woman; improving information, support, or care provided) | |
| Ne pas forcer les personnes à la prise *** d’hormones. Do not force people to take *** hormones. (man; how health professionals can better respond) | |
| Faciliter *l’accès *** à l’ALD avec l’instauration d’un vrai ** protocole. Facilitating * access *** to long-term healthcare coverage with the establishment of a real ** protocol. (man; how health professionals can better respond) | |
| 2. Improve training of health professionals | Plus de formation *** pour les professionnels ***, peut-être plus de moyens, mais le manque de formation *** est le principal. More training *** for professionals ***, maybe more resources, but the lack of training *** is the main one. (gender diverse; how health professionals can better respond) |
| Avoir une formation *** des professionnels *** sur le comportement à avoir quand on reçoit une personne trans. Train *** professionals *** on how to behave when dealing with a trans person. (man; how health professionals can better respond) | |
| Former *les professionnels *** de santé *** à la question pour pouvoir repérer les personnes plus tôt pendant l’enfance ou l’adolescence. Train * health care professionals *** on the issue so that they can identify individuals earlier in childhood or adolescence. (man; how health professionals can better respond) | |
| Former *les professionnels *** de santé *** uniquement par des personnes trans. Train * health care professionals *** only by trans people. (gender diverse; how health professionals can better respond) | |
| 3. Reduce barriers in access to care | Éviter de trop creuser en consultation (ex: chercher *** une raison dans l’enfance) car quand on va voir * un psychiatre * le questionnement est là depuis longtemps donc il faut *** éviter de nous remettre en question car ce n’est pas une maladie. Avoid digging too deep in consultation (e.g., looking for *** a reason in childhood) because when we go to see* a psychiatrist * the questioning has been there for a long time so it is necessary *** to avoid questioning ourselves as it is not an illness. (man; how health professionals can better respond) |
| Informer les personnes trans’ sur le fait que l’équipe *** officielle *** n’est pas un passage obligatoire ***. Inform trans people that the official *** team *** is not a requirement ***. (woman; improving information, support, or care provided) | |
| Deux ans ** de psychiatrie c’est trop long *** car pour nous, c’est dur à vivre. Two years ** of psychiatry is too long *** because for us, it’s hard to live. (gender diverse; how health professionals can better respond) | |
| La file d’attente * pour les opérations * est trop longue *** et la prise de médicaments avec autorisation des parents n’est pas juste * pour les mineurs. The waiting * list for surgery * is too long *** and requiring parental permission to take medication is not fair * to minors. (woman; improving information, support, or care provided) | |
| 4. Raise awareness in civil society | Informer ***dans les écoles *** dès la primaire ** puis en évoluant avec l’âge. Provide information *** in schools *** starting in primary school ** and progressing with age. (woman; improving information, support, or care provided) |
| Les trans doivent être plus représenté dans les médias *** et les dessins animés pour montrer aux enfants afin qu’ils soient plus ouverts. Trans people need to be more represented in the media *** and in cartoons to teach children to be more open. (gender diverse; improving information, support, or care provided) | |
| Sensibiliser ***les parents pendant la grossesse. Raise parents’ awareness *** during pregnancy. (man; improving information, support, or care provided) | |
| Sensibiliser ***à la transphobie dans les écoles *** (mise en situation via des vidéos comme les spots contre le racisme). Raise awareness *** of transphobia in schools *** (using videos such as anti-racism spots). (man; improving information, support, or care provided) | |
| 5. Facilitate the change of civil status | Changer *la loi *** pour rendre *** le changement *** d’état civil *** libre *** et gratuit *** en mairie ***. Change * the law *** to make *** civil *** status change *** free *** and unrestricted *** at the town hall ***. (woman; improving information, support, or care provided) |
| Simplifier ***la nouvelle loi *** pour la rendre *** plus précise pour éviter l’appréciation du juge. Simplify *** the new law *** to make *** it more precise to avoid the judge’s appreciation. (gender diverse; improving information, support, or care provided) | |
| Arrêter de demander ** des attestations ***. C’est inutile car on n’est pas malade. Stop asking ** for attestations ***. It’s useless because we’re not sick. (gender diverse; improving information, support, or care provided) | |
| Faciliter les changements *** administratifs. Les rendre *** libres *** et gratuits ***. Simplify administrative changes ***. Make them free *** and unrestricted ***. (woman; improving information, support, or care provided) |
| Clusters | In First Classification (92.9% of Corpus) | In Second Classification (76.5% of Corpus) | Proportion of Corpus | Corpus Lost between Classifications |
|---|---|---|---|---|
| Cluster 1 | 27.6% | 25.6% | 3.2% | |
| Cluster 1.0 | 4.1% | 5.0% | 3.8% | |
| Cluster 1.1 | 6.5% | 7.9% | 6.0% | |
| Cluster 1.2 | 4.7% | 5.7% | 4.4% | |
| Cluster 1.3 | 4.7% | 5.7% | 4.4% | |
| Cluster 1.4 | 4.1% | 5.0% | 3.8% | |
| Total | 24.1% | 29.3% | 22.4% | |
| Cluster 2 | 9.4% | 8.7% | 0.0% | |
| Cluster 2.0 | 9.4% | 11.4% | 8.7% | |
| Cluster 3 | 20.0% | 18.6% | 0.5% | |
| Cluster 3.0 | 10.6% | 12.9% | 9.9% | |
| Cluster 3.1 | 8.8% | 10.7% | 8.2% | |
| Total | 19.4% | 23.6% | 18.1% | |
| Cluster 4 | 33.5% | 31.1% | 12.5% | |
| Cluster 4.0 | 5.3% | 6.4% | 4.9% | |
| Cluster 4.1 | 11.2% | 13.6% | 10.4% | |
| Cluster 4.2 | 3.5% | 4.3% | 3.3% | |
| Total | 20.0% | 24.3% | 18.6% | |
| Cluster 5 | 9.4% | 8.7% | 0.0% | |
| Cluster 5.0 | 9.4% | 11.4% | 8.7% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baleige, A.; Guernut, M.; Denis, F. Impact of Depsychopathologization of Transgender and Gender Diverse Individuals in ICD-11 on Care Delivery: Looking at Trans Expertise through a Trans Lens. Int. J. Environ. Res. Public Health 2022, 19, 13257. https://doi.org/10.3390/ijerph192013257
Baleige A, Guernut M, Denis F. Impact of Depsychopathologization of Transgender and Gender Diverse Individuals in ICD-11 on Care Delivery: Looking at Trans Expertise through a Trans Lens. International Journal of Environmental Research and Public Health. 2022; 19(20):13257. https://doi.org/10.3390/ijerph192013257
Chicago/Turabian StyleBaleige, Anna, Mathilde Guernut, and Frédéric Denis. 2022. "Impact of Depsychopathologization of Transgender and Gender Diverse Individuals in ICD-11 on Care Delivery: Looking at Trans Expertise through a Trans Lens" International Journal of Environmental Research and Public Health 19, no. 20: 13257. https://doi.org/10.3390/ijerph192013257
APA StyleBaleige, A., Guernut, M., & Denis, F. (2022). Impact of Depsychopathologization of Transgender and Gender Diverse Individuals in ICD-11 on Care Delivery: Looking at Trans Expertise through a Trans Lens. International Journal of Environmental Research and Public Health, 19(20), 13257. https://doi.org/10.3390/ijerph192013257






