The Impact of Therapeutic Community Gardening on the Wellbeing, Loneliness, and Life Satisfaction of Individuals with Mental Illness
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Programme Details
2.2. Procedure
2.3. Measures
2.3.1. Demographic and Attendance Information
2.3.2. Wellbeing (Secondary Data Provided)
2.3.3. Loneliness
2.3.4. Life Satisfaction
2.4. Data Processing and Statistical Analysis
2.4.1. Wellbeing
2.4.2. Loneliness and Life Satisfaction
3. Results
3.1. Participants
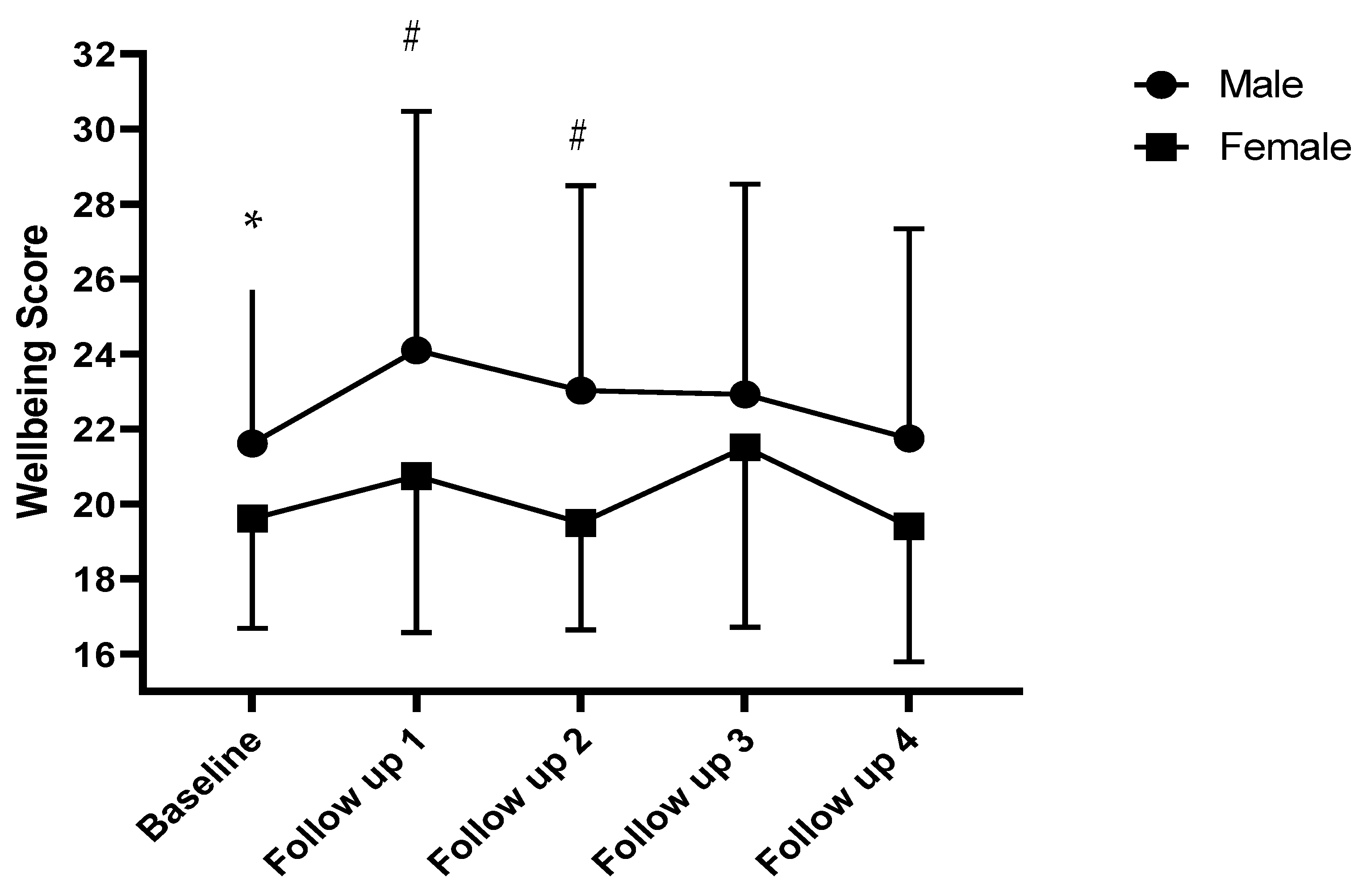
3.2. Wellbeing
3.3. Loneliness and Life Satisfaction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. Mental Health: Strengthening Our Response 2022 [Updated 17 June 2022]. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response (accessed on 18 July 2022).
- World Health Organisation. Mental Disorders 2022 [Updated 8 June 2022]. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed on 18 July 2022).
- McManus, S.; Bebbington, P.E.; Jenkins, R.; Brugha, T. Mental Health and Wellbeing in England: Adult Psychiatric Morbidity Survey 2014; NHS Digital: Leeds, UK, 2016. [Google Scholar]
- Vos, T.; Barber, R.M.; Bell, B.; Bertozzi-Villa, A.; Biryukov, S.; Bolliger, I.; Charlson, F.; Davis, A.; Degenhardt, L.; Dicker, D.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 743–800. [Google Scholar] [CrossRef]
- McDaid, D.; Park, A.L.; Davidson, G.; John, A.; Knifton, L.; McDaid, S.; Morton, A.; Thorpe, L.; Wilson, N. The Economic Case for Investing in the Prevention of Mental Health Conditions in the UK; The Mental Health Foundation: London, UK, 2022. [Google Scholar]
- Shankar, A.; Rafnsson, S.B.; Steptoe, A. Longitudinal associations between social connections and subjective wellbeing in the English Longitudinal Study of Ageing. Psychol. Health 2015, 30, 686–698. [Google Scholar] [CrossRef] [PubMed]
- Perlman, D.; Peplau, L.A. Personal Relationships: 3. Relationships in Disorder. In Toward a Social Psychology of Loneliness; Gilmour, R., Duck, S., Eds.; Academic Press: London, UK, 1981. [Google Scholar]
- Weiss, R.S. Loneliness: The Experience of Emotional and Social Isolation; The MIT Press: Cambridge, MA, USA, 1975. [Google Scholar]
- Steptoe, A.; Shankar, A.; Demakakos, P.; Wardle, J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc. Natl. Acad. Sci. USA 2013, 110, 5797–5801. [Google Scholar] [CrossRef] [PubMed]
- Hawkley, L.C.; Cacioppo, J.T. Aging and Loneliness: Downhill Quickly? Curr. Dir. Psychol. Sci. 2007, 16, 187–191. [Google Scholar] [CrossRef]
- Mushtaq, R.; Shoib, S.; Shah, T.; Mushtaq, S. Relationship between loneliness, psychiatric disorders, and physical health? A review on the psychological aspects of loneliness. J. Clin. Diagn. Res. 2014, 8, WE01–WE4. [Google Scholar] [CrossRef]
- Meltzer, H.; Bebbington, P.; Dennis, M.S.; Jenkins, R.; McManus, S.; Brugha, T.S. Feelings of loneliness among adults with mental disorder. Soc. Psychiatry Psychiatr. Epidemiol. 2013, 48, 5–13. [Google Scholar] [CrossRef]
- Lee, S.L.; Pearce, E.; Ajnakina, O.; Johnson, S.; Lewis, G.; Mann, F.; Pitman, A.; Solmi, F.; Sommerlad, A.; Steptoe, A.; et al. The association between loneliness and depressive symptoms among adults aged 50 years and older: A 12-year population-based cohort study. Lancet Psychiatry 2021, 8, 48–57. [Google Scholar] [CrossRef]
- Clair, R.; Gordon, M.; Kroon, M.; Reilly, C. The effects of social isolation on well-being and life satisfaction during pandemic. Humanit. Soc. Sci. Commun. 2021, 8, 28. [Google Scholar] [CrossRef]
- HM Government. A Connected Society. A Strategy for Tackling Loneliness—Laying the Foundations for Change; Crown: London, UK, 2018. Available online: https://www.gov.uk/government/news/pm-launches-governments-first-loneliness-strategy (accessed on 18 June 2022).
- Chatterjee, H.J.; Camic, P.M.; Lockyer, B.; Thomson, L.J.M. Non-clinical community interventions: A systematised review of social prescribing schemes. Arts Health 2018, 10, 97–123. [Google Scholar] [CrossRef]
- NHS England. The Long-Term Plan 2019. Available online: https://www.longtermplan.nhs.uk/ (accessed on 16 June 2022).
- Robinson, J.M.; Breed, M.F. Green Prescriptions and Their Co-Benefits: Integrative Strategies for Public and Environmental Health. Challenges 2019, 10, 9. [Google Scholar] [CrossRef]
- NHS England. Green Social Prescribing. Available online: https://www.england.nhs.uk/personalisedcare/social-prescribing/green-social-prescribing/ (accessed on 21 April 2022).
- Howarth, M.; Brettle, A.; Hardman, M.; Maden, M. What is the evidence for the impact of gardens and gardening on health and well-being: A scoping review and evidence-based logic model to guide healthcare strategy decision making on the use of gardening approaches as a social prescription? BMJ Open 2020, 10, e036923. [Google Scholar] [CrossRef] [PubMed]
- Genter, C.; Roberts, A.; Richardson, J.; Sheaff, M. The contribution of allotment gardening to health and wellbeing: A systematic review of the literature. Br. J. Occup. Ther. 2015, 78, 593–605. [Google Scholar] [CrossRef]
- Yang, Y.; Ro, E.; Lee, T.J.; An, B.C.; Hong, K.P.; Yun, H.J.; Park, E.Y.; Cho, H.R.; Yun, S.Y.; Park, M.; et al. The Multi-Sites Trial on the Effects of Therapeutic Gardening on Mental Health and Well-Being. Int. J. Environ. Res. Public Health 2022, 19, 8046. [Google Scholar] [CrossRef] [PubMed]
- Lampert, T.; Costa, J.; Santos, O.; Sousa, J.; Ribeiro, T.; Freire, E. Evidence on the contribution of community gardens to promote physical and mental health and well-being of non-institutionalized individuals: A systematic review. PLoS ONE 2021, 16, e0255621. [Google Scholar] [CrossRef]
- Bailey, A.; Kingsley, J. Connections in the garden: Opportunities for wellbeing. Local Environ. 2020, 25, 907–920. [Google Scholar] [CrossRef]
- Soga, M.; Gaston, K.J.; Yamaura, Y. Gardening is beneficial for health: A meta-analysis. Prev. Med. Rep. 2017, 5, 92–99. [Google Scholar] [CrossRef]
- Spano, G.; D’Este, M.; Giannico, V.; Carrus, G.; Elia, M.; Lafortezza, R.; Panno, A.; Sanesi, G. Are Community Gardening and Horticultural Interventions Beneficial for Psychosocial Well-Being? A Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 3584. [Google Scholar] [CrossRef]
- Wakefield, S.; Yeudall, F.; Taron, C.; Reynolds, J.; Skinner, A. Growing urban health: Community gardening in South-East Toronto. Health Promot. Int. 2007, 22, 92–101. [Google Scholar] [CrossRef]
- Wood, C.J.; Pretty, J.; Griffin, M. A case-control study of the health and well-being benefits of allotment gardening. J. Public Health 2016, 38, e336–e344. [Google Scholar] [CrossRef]
- Wood, C.J.; Polley, M.; Barton, J.L.; Wicks, C.L. Therapeutic community gardening as a green social prescription for mental ill-health: Impact, barriers, and facilitators from the perspective of multiple stakeholders. Int. J. Environ. Res. Pub. Health, 2022; in review. [Google Scholar]
- Suto, M.J.; Smith, S.; Damiano, N.; Channe, S. Participation in Community Gardening: Sowing the Seeds of Well-Being: Participation au jardinage communautaire: Pour semer les graines du bien-être. Can. J. Occup. Ther. 2021, 88, 142–152. [Google Scholar] [CrossRef]
- McGuire, L.; Morris, S.L.; Pollard, T.M. Community gardening and wellbeing: The understandings of organisers and their implications for gardening for health. Health Place 2022, 75, 102773. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.; Jacob, L.; Yakkundi, A.; McDermott, D.; Armstrong, N.C.; Barnett, Y.; Barnett, Y.; López-Sánchez, G.F.; Martin, S.; Butler, L.; et al. Correlates of symptoms of anxiety and depression and mental wellbeing associated with COVID-19: A cross-sectional study of UK-based respondents. Psychiatry Res. 2020, 291, 113138. [Google Scholar] [CrossRef] [PubMed]
- Wood, C.J.; Barton, J.; Smyth, N. A cross-sectional study of physical activity behaviour and associations with wellbeing during the UK coronavirus lockdown. J. Health Psychol. 2021, 27, 1432–1444. [Google Scholar] [CrossRef] [PubMed]
- Heron, P.N.; Spanakis, P.; Crosland, S.; Johnston, G.; Newbronner, E.; Wadman, R.; Walker, L.; Gilbody, S.; Peckham, E. Loneliness among people with severe mental ill health during the COVID-19 pandemic: Results from a linked UK population cohort study. medRxiv 2021, 17, e0262363. [Google Scholar] [CrossRef]
- Jaspal, R.; Breakwell, G.M. Socio-economic inequalities in social network, loneliness, and mental health during the COVID-19 pandemic. Int. J. Soc. Psychiatry 2020, 68, 002076402097669. [Google Scholar] [CrossRef]
- Kwong, A.S.F.; Pearson, R.M.; Adams, M.J.; Northstone, K.; Tilling, K.; Smith, D.; Fawns-Ritchie, C.; Bould, H.; Warne, N.; Zammit, S.; et al. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. Br. J. Psychiatry 2021, 218, 334–343. [Google Scholar] [CrossRef]
- Marmot, M.; Allen, J.; Goldblatt, P.; Herd, E.; Morrison, J. Build Back Fairer: The COVID-19 Marmot Review. The Pandemic, Socioeconomic and Health Inequalities in England; Institute of Health Equity: London, UK, 2020. [Google Scholar]
- World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact; World Health Organization: Geneva, Switzerland, 2022.
- Brunier, A.; Drysdale, C. COVID-19 Disrupting Mental Health Services in Most Countries, WHO Survey. World Health Organization: Geneva, Switzerland, 2020.
- Di Gessa, G.; Maddock, J.; Green, M.J.; Thompson, E.J.; McElroy, E.; Davies, H.L.; Mundy, J.; Stevenson, A.J.; Kwong, A.S.F.; Griffith, G.J.; et al. Pre-pandemic mental health and disruptions to healthcare, economic and housing outcomes during the COVID-19 pandemic: Evidence from 12 UK longitudinal studies. Br. J. Psychiatry 2022, 220, 21–30. [Google Scholar] [CrossRef]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): Development and UK validation. Health Qual. Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef]
- Stewart-Brown, S.; Tennant, A.; Tennant, R.; Platt, S.; Parkinson, J.; Weich, S. Internal construct validity of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS): A Rasch analysis using data from the Scottish Health Education Population Survey. Health Qual. Life Outcomes 2009, 7, 15. [Google Scholar] [CrossRef]
- Fat, L.; Scholes, S.; Boniface, S.; Mindell, J.; Stewart-Brown, S. Evaluating and establishing national norms for mental wellbeing using the short Warwick–Edinburgh Mental Well-being Scale (SWEMWBS): Findings from the Health Survey for England. Qual. Life Res. 2017, 26, 1129–1144. [Google Scholar] [CrossRef]
- Gierveld, J.D.J.; van Tilburg, T. A 6-Item Scale for Overall, Emotional, and Social Loneliness. Res. Aging 2006, 28, 582–598. [Google Scholar] [CrossRef]
- van Tilburg, T.G.; Gierveld, J.D.J. Cut-off points on the De Jong Gierveld Loneliness Scale. Tijdschr. Gerontol. Geriatr. 1999, 30, 158–163. [Google Scholar]
- Helliwell, J.F.; Layard, R.; Sachs, J.D. (Eds.) World Happiness Report 2019; Sustainable Development Solutions Network: New York, NY, USA, 2019. [Google Scholar]
- Helliwell, J.F.; Layard, R.; Sachs, J.D.; De Neve, J.E. (Eds.) World Happiness Report 2020; Sustainable Development Solutions Network: New York, NY, USA, 2020. [Google Scholar]
- Clark, A.E.; Georgellis, Y. Back to Baseline in Britain: Adaptation in the British Household Panel Survey. Economica 2013, 80, 496–512. [Google Scholar] [CrossRef]
- Clark, A.E.; Fleche, S.; Layard, R.; Powdthavee, N.; Ward, G. The Origins of Happiness; Princeton University Press: Princeton, NJ, USA, 2018. [Google Scholar]
- Pretty, J.; Barton, J. Nature-Based Interventions and Mind-Body Interventions: Saving Public Health Costs Whilst Increasing Life Satisfaction and Happiness. Int. J. Environ. Res. Public Health 2020, 17, 7769. [Google Scholar] [CrossRef] [PubMed]
- Office for National Statistics. Annual Personal Wellbeing Estimates; Office for National Statistics: Newport, UK, 2021.
- Milligan, C.; Payne, S.; Bingley, A.; Cockshott, Z. Place, and wellbeing: Shedding light on activity interventions for older men. Ageing Soc. 2015, 35, 124–149. [Google Scholar] [CrossRef]
- Hoglund, M.W.; Sadovsky, R.; Classie, J. Engagement in life activities promotes healthy aging in men. J. Men’s Health 2009, 6, 354–365. [Google Scholar] [CrossRef]
- Culph, J.S.; Wilson, N.J.; Cordier, R.; Stancliffe, R.J. Men’s Sheds and the experience of depression in older Australian men. Aust. Occup. Ther. J. 2015, 62, 306–315. [Google Scholar] [CrossRef]
- Kelly, D.; Steiner, A.; Mason, H.; Teasdale, S. Men’s sheds as an alternative healthcare route? A qualitative study of the impact of Men’s sheds on user’s health improvement behaviours. BMC Public Health 2021, 21, 553. [Google Scholar] [CrossRef]
- Moylan, M.M.; Carey, L.B.; Blackburn, R.; Hayes, R.; Robinson, P. The Men’s Shed: Providing Biopsychosocial and Spiritual Support. J. Relig. Health 2015, 54, 221–234. [Google Scholar] [CrossRef]
- Diener, E.; Oishi, S.; Lucas, R.E. Personality, culture, and subjective well-being: Emotional and cognitive evaluations of life. Annu. Rev. Psychol. 2003, 54, 403–425. [Google Scholar] [CrossRef]
- Smyth, N.; Thorn, L.; Wood, C.; Hall, D.; Lister, C. Increased Wellbeing following Engagement in a Group Nature-Based Programme: The Green Gym Programme Delivered by the Conservation Volunteers. Healthcare 2022, 10, 978. [Google Scholar] [CrossRef] [PubMed]
- Chief Medical Officer. Annual Report 2018: Better Health within Research; UK Government: London, UK, 2018.
- Collins, B. How do we value wellbeing? Combining data to put an economic value on the change in Short Warwick Edinburgh Wellbeing Scale (SWEMWBS) scores. SSRN Work. Pap. 2016. [Google Scholar] [CrossRef]
- National Academy for Social Prescribing. National Academy for Social Prescribing 2020–2023 Strategic Plan; NASP: London, UK, 2019. [Google Scholar]
- Bouchard, M.; Lecomte, T.; Cloutier, B.; Herrera-Roberge, J.; Potvin, S. Dropout Rates in Psychosocial Interventions for People with Both Severe Mental Illness and Substance Misuse: A Systematic Review and Meta-Analysis. Front. Psychiatry 2022, 13, 842329. [Google Scholar] [CrossRef] [PubMed]
| Percentage (n) | ||
|---|---|---|
| Duration of attendance | Just started | 8.2% (n = 4) |
| Up to one year | 2.0% (n = 1) | |
| 1–3 years | 36.7% (n = 18) | |
| 4–6 years | 22.4% (n = 11) | |
| 7–9 years | 20.4% (n = 10) | |
| 10+ years | 10.2% (n = 5) | |
| Frequency of attendance | Once a week | 63.8% (n = 30) |
| Twice a week | 29.8% (n = 14) | |
| 3–4 times a week+ | 6.4% (n = 3) | |
| Attended in the last year | Yes | 93.3% (n = 42) |
| No | 6.7% (n = 3) |
| Timepoint 1 | Timepoint 2 | Timepoint 3 | ||
|---|---|---|---|---|
| Wellbeing (7–35 scale) | Male | 23.69 ± 5.90 (n = 35) | 22.17 ± 4.66 (n = 33) | 23.22 ± 6.00 (n = 24) |
| Female | 18.76 ± 3.25 * (n = 15) | 20.72 ± 3.65 * (n = 15) | 21.94 ± 4.83 (n = 12) | |
| Total | 22.21 ± 5.69 (n = 50) | 21.72 ± 4.39 (n = 48) | 22.80 ± 5.60 (n = 36) | |
| Pooled (n = 53) | 21.98 | 21.46 | 22.74 | |
| Emotional Loneliness (0–3 scale) | Male | 1.40 ± 1.03 (n = 35) | 1.77 ± 0.96 (n = 34) | 1.70 ± 1.15 (n = 23) |
| Female | 2.09 ± 0.83 (n = 11) | 1.80 ± 1.01 (n = 15) | 1.36 ± 1.21 (n = 11) | |
| Total | 1.57 ± 1.03 (n = 46) | 1.78 ± 0.96 (n = 49) | 1.59 ± 1.16 (n = 34) | |
| Pooled (n = 53) | 1.55 | 1.79 | 1.58 | |
| Social Loneliness (0–3 scale) | Male | 0.83 ± 1.16 (n = 36) | 0.94 ± 1.08 (n = 35) | 0.57 ± 0.95 (n = 23) |
| Female | 1.46 ± 1.39 (n = 13) | 1.40 ± 1.30 (n = 15) | 1.46 ± 1.39 (n = 13) | |
| Total | 1.00 ± 1.24 (n = 49) | 1.08 ± 1.16 (n = 50) | 0.89 ± 1.19 (n = 36) | |
| Pooled (n = 53) | 1.02 | 1.12 | 0.86 | |
| Life satisfaction (0–10 scale) | Male | 6.89 ± 2.92 (n = 36) | 7.00 ± 2.60 (n = 35) | 7.04 ± 2.82 (n = 24) |
| Female | 4.97 ± 1.82 (n = 17) | 6.38 ± 2.36 (n = 16) | 5.43 ± 3.08 (n = 14) | |
| Total | 6.27 ± 2.75 * (n = 53) | 6.80 ± 2.52 (n = 51) | 6.45 ± 2.90 (n = 38) | |
| Pooled (n = 53) | 6.27 | 6.85 | 6.71 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wood, C.J.; Barton, J.L.; Wicks, C.L. The Impact of Therapeutic Community Gardening on the Wellbeing, Loneliness, and Life Satisfaction of Individuals with Mental Illness. Int. J. Environ. Res. Public Health 2022, 19, 13166. https://doi.org/10.3390/ijerph192013166
Wood CJ, Barton JL, Wicks CL. The Impact of Therapeutic Community Gardening on the Wellbeing, Loneliness, and Life Satisfaction of Individuals with Mental Illness. International Journal of Environmental Research and Public Health. 2022; 19(20):13166. https://doi.org/10.3390/ijerph192013166
Chicago/Turabian StyleWood, Carly J., Jo L. Barton, and Claire L. Wicks. 2022. "The Impact of Therapeutic Community Gardening on the Wellbeing, Loneliness, and Life Satisfaction of Individuals with Mental Illness" International Journal of Environmental Research and Public Health 19, no. 20: 13166. https://doi.org/10.3390/ijerph192013166
APA StyleWood, C. J., Barton, J. L., & Wicks, C. L. (2022). The Impact of Therapeutic Community Gardening on the Wellbeing, Loneliness, and Life Satisfaction of Individuals with Mental Illness. International Journal of Environmental Research and Public Health, 19(20), 13166. https://doi.org/10.3390/ijerph192013166








