Abstract
This study aimed to investigate the change in the incidence and variance of otorhinolaryngologic diseases during the coronavirus disease 19 (COVID-19) pandemic. The entire Korean population (~50 million) was evaluated for the monthly incidence of 11 common otorhinolaryngologic diseases of upper respiratory infection (URI), influenza, acute tonsillitis, peritonsillar abscess, retropharyngeal and parapharyngeal abscess, acute laryngitis and bronchitis, stomatitis and related lesions, acute sinusitis, rhinitis, otitis media, and dizziness from January 2018 through March 2021 using the International Classification of Disease (ICD)-10 codes with the data of the Korea National Health Insurance Service. The differences in the mean incidence of 11 common otorhinolaryngologic diseases before and during COVID-19 were compared using the Mann—Whitney U test. The differences in the variance of incidence before and during COVID-19 were compared using Levene’s test. The incidence of all 11 otorhinolaryngologic diseases was lower during COVID-19 than before COVID-19 (all p < 0.05). The variations in disease incidence by season were lower during COVID-19 than before COVID-19 for infectious diseases, including URI, influenza, acute tonsillitis, peritonsillar abscess, retropharyngeal and parapharyngeal abscess, acute laryngitis and bronchitis, acute sinusitis, and otitis media (all p < 0.05), while it was not in noninfectious diseases, including stomatitis, rhinitis, and dizziness. As expected, the incidences of all otorhinolalryngolgic diseases were decreased. Additionally, we found that seasonal variations in infectious diseases disappeared during the COVID-19 pandemic, while noninfectious diseases did not.
1. Introduction
Coronavirus disease 19 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2. COVID-19 has changed our daily lives. Due to the limitations of accessibility of clinics, the clinical procedures were preferentially provided to those with emergency or acute phases of the disease [1,2]. Medical resources have been redistributed to triage emergent diseases. For instance, in neurosurgery departments, the proportion of elective surgery decreased from 57.7% in the pre-COVID-19 era to 11.3% in the COVID-19 era (p < 0.001) [2]. Both research and clinical practice have been focused on COVID-19. Thus, there has been concern about the inequality of medical care [3]. In addition to changes in medical resources, the epidemiologic features of diseases have changed during the COVID-19 pandemic period. Changes in health-seeking behavior and improved hygiene have an impact on the incidence of disease [4]. A healthy diet and lifestyle habits were suggested to decrease the incidence of metabolic diseases as well as infectious diseases [5]. In Korea, nationwide surveillance strategies have been acted for the early detection and diagnosis of patients with COVID-19 [6]. In addition, social distancing strategies have been continued to prevent the spread of COVID-19 [7].
Multiple factors determine the epidemic of infectious diseases, including circulating viruses, the immunity of the population, and the transmissibility of viruses [8,9]. Among these determinants, the transmissibility of viruses can be diminished during the COVID-19 pandemic period by strategies of quarantine. Due to changes in health-seeking behavior and improved hygiene, the distribution of disease incidence as well as the overall incidence of diseases can change during the COVID-19 pandemic period. A number of recent studies have suggested alleviating the burden of respiratory infectious diseases during COVID-19. Influenza contraction declined by approximately 44% (95% confidence intervals = 34%–53%) during social distancing measures against the COVID-19 pandemic in Hong Kong [4]. As otorhinolaryngologic diseases include many upper respiratory infectious diseases, their incidence and epidemics could be influenced by the COVID-19 pandemic. A retrospective study reported a decrease in overall otorhinolaryngological diseases (80.4% vs. 19.5%, p < 0.001) and otitis media (92.8% vs. 8.0%, p < 0.001) during the lockdown period (21 February–3 May 2020) in Italy [10]. However, the study population was limited to children, and the study population was small (4538) [10]. In addition, there has been no previous research on the variance or seasonality of infectious diseases during COVID-19.
We hypothesized that the incidence and variance of a wide range of otorhinolaryngologic diseases, in addition to influenza and upper respiratory infection (URI), may be changed during the COVID-19 era. To test this hypothesis, this study compared the number and variations of incidence of numerous otorhinolaryngologic diseases between the pre-COVID-19 pandemic and during the COVID-19 pandemic period. To estimate the seasonality of diseases, the incidences of diseases were collected monthly and compared between the pre-COVID-19 pandemic and the COVID-19 pandemic period. Few previous studies have extensively investigated the impact of the COVID-19 pandemic on the epidemiology of otorhinolaryngological diseases in a large, nationwide population.
2. Methods
2.1. Ethics
The Ethics Committee of Hallym University (code number: 2021-11-004) approved the use of these data. The study was exempted from the need for written informed consent by the Institutional Review Board.
2.2. Study Population
This study includes the entire Korean population (~50 million) without an exception, as a single, mandatory health insurance system covers the whole country. Thus, we could gather data on the entire Korean population from the primary clinic to the tertiary hospital. In this study, we evaluated the incidence of diseases from January 2018 through March 2021. As the first COVID-19 cases in Korea were discovered on 20 January 2020, and disease prevention and control were started on March 2020, we defined the periods of “before COVID-19” until February 2020 and “during COVID-19” from March 2020 to March 2021.
2.3. Otorhinolarynologic Diseases
We evaluated the monthly incidence of 11 otorhinolaryngologic diseases that are common in the primary clinic. The patients were diagnosed with each disease and recorded using the International Classification of Disease (ICD)-10 codes: URI (J00, J02, and J03), influenza (J09, J10, and J11), acute tonsillitis (J03), peritonsillar abscess (J36), retropharyngeal and parapharyngeal abscess (J39.0), acute laryngitis and bronchitis (J04), stomatitis and related diseases (K12), acute sinusitis (J01), rhinitis (J30), otitis media (H65, H66, and HJ67), and dizziness (R42 and H81). The incidence of these diseases was calculated without duplication, as we had the medical records of the entire hospital or clinics, and patients were identified with unique resident registration numbers.
2.4. Statistical Analysis
The difference in the mean incidence of diseases before and during COVID-19 was compared using the Mann—Whitney U test for nonparametric values. The difference in the variance of diseases before and during COVID-19 was compared using Levene’s test for nonparametric values [11]. For the subgroup analyses, we divided the participants by age (0–19 years old, 20–59 years old, and 60+ years old) and sex. The subgroup analyses were conducted due to the potential age and sex differences in terms of the impact of COVID-19. For instance, the knowledge of COVID-19 and quarantine maneuvers can have different impacts on daily life according to age and sex.
Two-tailed analyses were conducted, and p values < 0.05 were considered to indicate significance. The results were statistically analyzed using SPSS version 22.0 (IBM, Armonk, NY, USA).
3. Results
3.1. Incidences of Infectious Diseases
The incidence of URI, influenza, acute tonsillitis, peritonsillar abscess, retropharyngeal and parapharyngeal abscess, acute laryngitis and bronchitis, acute sinusitis, and otitis media was lower during COVID-19 than before COVID-19 (all p < 0.001, Table 1).

Table 1.
Mean and standard deviation of the incidence of diseases before and during COVID-19 and their difference.
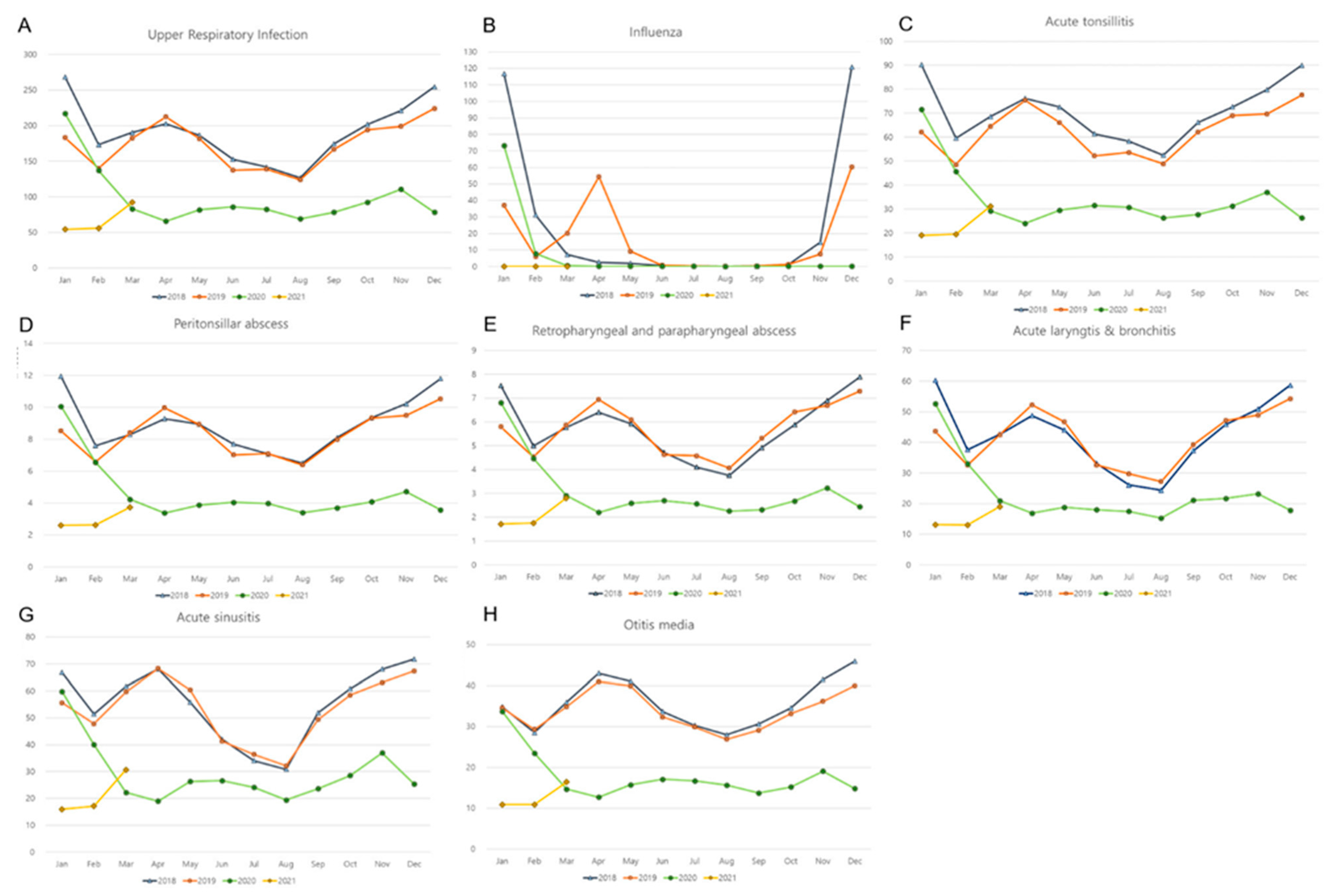
The variations in disease incidence were significantly lower during COVID-19 than before COVID-19 for all of these infectious diseases (all p < 0.05). All of these diseases demonstrated seasonality before COVID-19 (Figure 1). The incidences of URI and influenza were high during autumn and winter (October, November, December, January, and February) before COVID-19 (Figure 1). The incidences of acute tonsillitis, peritonsillar abscess, retropharyngeal and parapharyngeal abscess, acute laryngitis and bronchitis, acute sinusitis, rhinitis, and otitis media showed small peaks during spring (March, April, and May), in addition to the peak incidence during autumn and winter. During COVID-19, the seasonal variations in the incidence of all of these diseases were attenuated.
Figure 1.
Monthly incidences of (A) upper respiratory infection, (B) influenza, (C) acute tonsillitis, (D) peritonsillar abscess, (E) retropharyngeal and parapharyngeal abscess, (F) acute laryngitis and bronchitis, (G) acute sinusitis, and (H) otitis media. (y-axis: ×10,000 person).
In terms of sex, both men and women showed a lower incidence of URI, influenza, acute tonsillitis, peritonsillar abscess, retropharyngeal and parapharyngeal abscess, acute laryngitis and bronchitis, acute sinusitis, and otitis media during COVID-19 than before COVID-19 (all p < 0.05, Table 2).

Table 2.
Mean and standard deviation of the incidence of diseases before and during COVID-19 and their differences in the subgroups relative to sex.
The variations in disease incidence were different before and during COVID-19 for URI, acute tonsillitis, peritonsillar abscess, retropharyngeal and parapharyngeal abscess, acute laryngitis and bronchitis, acute sinusitis, and otitis media in the male group (all p < 0.05). In the female group, the variations in the incidence of URI, influenza, acute tonsillitis, peritonsillar abscess, retropharyngeal and parapharyngeal abscess, acute laryngitis and bronchitis, acute sinusitis, and otitis media were low during COVID-19 compared with before COVID-19 (all p < 0.05).
In terms of age, all age groups showed a lower incidence of URI, influenza, acute tonsillitis, peritonsillar abscess, retropharyngeal and parapharyngeal abscess, acute laryngitis and bronchitis, acute sinusitis, and otitis media during COVID-19 than before COVID-19 (all p < 0.05, Table 3). The variances in disease incidence were lower for URIs and acute tonsillitis, peritonsillar abscess, retropharyngeal and parapharyngeal abscess, acute laryngitis and bronchitis, and otitis media during the COVID-19 pandemic in all age groups (all p < 0.05). The variance in acute sinusitis was lower during the COVID-19 pandemic in the age groups of 20-to-59 years and 60 years or above (all p < 0.05).

Table 3.
Mean and standard deviation of the incidence of diseases before and during COVID-19 and their differences in the subgroups relative to age.
3.2. Incidences of Noninfectious Diseases
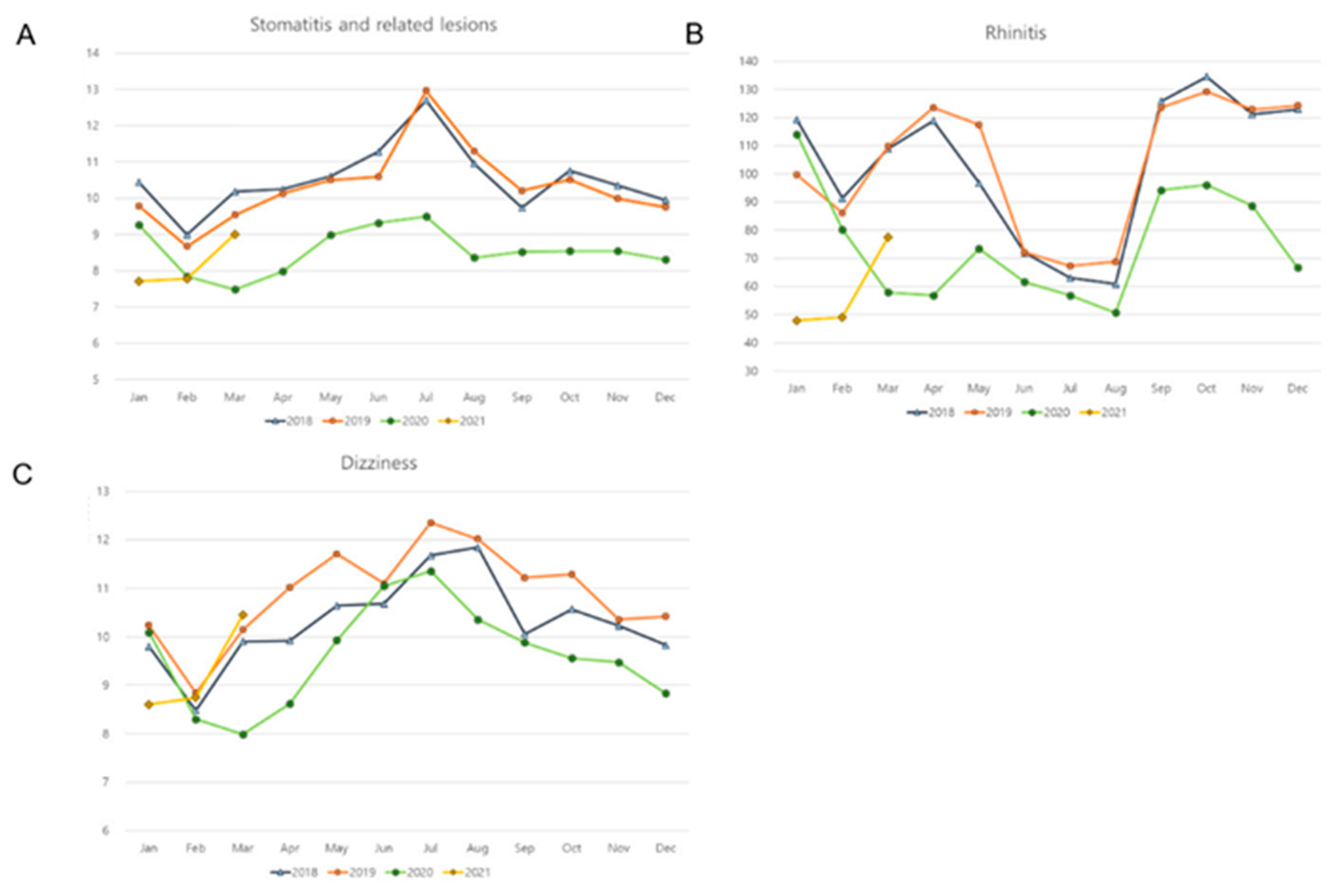
Stomatitis and related lesions, rhinitis, and dizziness showed a lower incidence during COVID-19 than before COVID-19 (all p < 0.001, Table 1). These noninfectious diseases demonstrated no difference in variations in disease incidence before and during COVID-19. Dizziness showed a similar incidence of diseases throughout the year (Figure 2). The incidence of stomatitis and related lesions was high during the summer season (July and August) before COVID-19 (Figure 2). The incidences of rhinitis showed a small peak during spring (March, April, and May), in addition to the peak incidence during autumn and winter before COVID-19.
Figure 2.
Monthly incidences of (A) stomatitis and related lesions, (B) rhinitis, and (C) dizziness. (y-axis: ×10,000 person).
The subgroup analyses also demonstrated a lower incidence of stomatitis and related lesions, rhinitis, and dizziness during COVID-19 than before COVID-19 in both the male and female groups (all p < 0.05, Table 2). The variations in the incidence of stomatitis and related lesions, rhinitis, and dizziness were not significant before COVID-19 or during COVID-19 in the male and female subgroups, except for stomatitis and related lesions in the female subgroup. The female group showed a lower variance in the incidence of stomatitis and related lesions during COVID-19 than before COVID-19 (all p = 0.035).
In all the age subgroups, stomatitis and related lesions and rhinitis showed lower incidence during the COVID-19 pandemic (all p < 0.05, Table 3). The incidence of dizziness was lower during the COVID-19 pandemic in the 20-to-59-year-old group (p = 0.001). The variation in the incidence of stomatitis and related lesions, rhinitis, and dizziness was not different during the COVID-19 pandemic compared with before the COVID-19 pandemic in all age groups, except for the decreased variance in rhinitis in those 60 years old or older (p = 0.013).
4. Discussion
During the COVID-19 pandemic period, the incidences of otorhinolaryngologic diseases were lower than before the COVID-19 pandemic period. In addition, the seasonality of infectious diseases was attenuated during the COVID-19 pandemic period. On the other hand, noninfectious diseases, such as stomatitis, rhinitis, and dizziness, did not show differences in the variance in disease incidence during COVID-19. The decreased incidence of otorhinolaryngologic diseases and the variance in infectious diseases during COVID-19 were consistent in sex and age subgroups. This study is novel in demonstrating the decreased variance in the incidence of various otorhinolaryngologic infectious diseases during the COVID-19 pandemic period compared with before the COVID-19 pandemic period in the general population. An extensive number of upper respiratory infectious diseases of URI, influenza, acute tonsillitis, peritonsillar abscess, retropharyngeal and parapharyngeal abscess, acute laryngitis and bronchitis, acute sinusitis, and otitis media were evaluated. In addition, noninfectious diseases of stomatitis, rhinitis, and dizziness were investigated, which did not show a difference in the variance of incidence before COVID-19 and during COVID-19.
Similar to the present results, a number of prior studies described the low incidence of infectious diseases during the COVID-19 pandemic. Among these studies, many reported a decreased incidence of influenza during the COVID-19 pandemic [4,12,13,14,15]. A retrospective study demonstrated the short and low epidemic peak of influenza during the 2019–2020 season, compared with the 2018–2019 season, in Korea (5.9 vs. 6.3 influenza-like illnesses per 1000 outpatients and 19-week 1-day vs. 31-week 1-day duration) [16]. In addition to influenza, other infectious diseases have been suggested to have declined during the COVID-19 pandemic [12]. In China, notifiable infectious diseases were reduced by approximately 41.38% in 2020 compared with 2019 [12]. Among infectious diseases, influenza was the most decreased infectious disease in 2020, followed by hand–foot–mouth disease and other infectious diseases such as diarrhea [12]. Other lower respiratory tract infections, such as community-acquired pneumonia and hospital-acquired pneumonia, were also reported to be declined during the COVID-19 pandemic [17,18]. Respiratory coronavirus infections other than SARS-CoV-2 were suppressed during the lockdown period in Chinese children (0–24 months) [13]. During the COVID-19 lockdown period, otitis media was reported to have declined in children [19]. As many as 82.3% of the cases of children with otitis media were resolved during the lockdown period and monitored using telemedicine [19]. Thus, it can be presumed that the COVID-19 pandemic status may have a role in the low incidence of various infectious diseases in both upper and lower respiratory tracts.
Nonpharmaceutical interventions (NPIs) may have preventive effects for upper respiratory infectious diseases in addition to mitigating the spread of SARS-CoV-2 transmission [20]. NPIs can be defined as preventive strategies in addition to pharmacologic management to cope with infectious diseases [21]. For instance, the wearing of facemasks, hand hygiene, and social distancing strategies can be considered as NPIs. In personal aspects, self-protective practices include wearing facial masks, hand hygiene, cough etiquette, and voluntarily staying home during the COVID-19 pandemic period [20]. In social aspects, social distancing acts encompass school closures, work at home, telecommuting, and avoidance of mass public gatherings [22]. These NPIs could suppress the contraction of many upper respiratory viruses in addition to severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2) during asymptomatic periods, which can harbor considerably high viral loads [23]. In Hong Kong, the daily effective reproduction number for influenza decreased to 0.72 (95% CI = 0.70–0.74) after school closure from 1.28 (95% CI = 1.26–1.30) during school closure [4]. A systemic review estimated an approximately 23% decline in cumulative influenza attacks associated with workplace social distancing measures in the general population [22].
In addition to the decrease in incidence, infectious diseases showed a lower variance in disease incidence during the COVID-19 pandemic in the present study. In line with the present study, a retrospective observational study described the extraordinarily low incidence of respiratory syncytial virus infection during the winter season, while a high incidence of respiratory syncytial virus infection during the summer season in England during the COVID-19 pandemic [24]. They suggested that the lack of immunity to the respiratory syncytial virus during winter may induce an increase in the incidence of respiratory syncytial virus infection during the summer season [24]. As a result, the seasonality of respiratory infection was diluted. In addition to respiratory infections, acute otitis media in children has been reported to have seasonality due to variations in the viral transmissibility of respiratory syncytial virus, human metapneumovirus, and influenza, and its seasonal variation was diminished in the current study [25]. The high prevalence of upper respiratory tract infectious diseases during the winter season is attributed to a number of viral and host factors, including increased crowding and indoor activities and the cooling of the nasal epithelium [8,9]. Increased viral stability and transmissibility and weakened host immune responses could accelerate the high incidence of infectious diseases during winter [26]. In host factors, the low temperature of the nasal epithelium could decrease the immunities and defense mechanisms to fight against viral infections, such as mucociliary clearance and the phagocytic activity of leukocytes [8]. In addition, due to cold weather, indoor activities and opportunities for physical contact with viral carriers can be increased during the winter season [8,9]. Although some viral and host factors, such as viral stability and host immune systems, cannot be overcome by NPIs, strict NPIs to cope with SARS-CoV-2 contraction can dissolve the seasonal epidemics of other infectious diseases.
As there are variations in the severity of the COVID-19 pandemic among countries, the current data should be interpreted with caution [27,28]. This study analyzed the entire Korean population (~50 million). The meteorological characteristics of Korea show four distinctive spring, summer, autumn, and winter seasons because Korea resides in the Northern Hemisphere. Thus, it is susceptible to seasonal infectious diseases. In Korea, the first patient with COVID-19 was reported on 20 January 2020 [29], and therefore, we defined before February 2020 as before the COVID-19 period. From February 2020, COVID-19 was persistently outbroken in Korea [29]. To cope with the COVID-19 pandemic, the Korean government enacted stratified social distancing policies [29]. Thus, the effects of quarantine could be high in Korea.
This study was based on the health claim data that classified the diseases according to diagnostic codes. Therefore, undiagnosed or subclinical diseases could be missed in the present study. However, in Korea, a national influenza surveillance system exists, and consequently, there may be few undiagnosed cases [30]. In addition, the accuracy of diagnosis was limited due to the inaccessibility of the results of laboratory tests. There may be heterogeneity in the severity and subtypes of diseases. For instance, the transmissibility and severity of influenza vary depending on the subtypes of influenza virus (H1N1, H2N2, H3N3, H5N1, and H7N9 for influenza A) [31]. To attenuate the bias from any possible misclassification of diseases, we analyzed two years (2018 and 2019) before the COVID-19 pandemic period. The distributions of disease incidence were similar between 2018 and 2019 (Figure 1). As this study analyzed 11 diseases, the bias from multiple comparisons could not be excluded. This study counted the cumulative cases of otorhinolaryngologic diseases without the trends of the daily cumulative numbers of patients treated for otorhinolaryngologic diseases before and during COVID-19. Segmented regression analysis can improve the current limitation. Further follow-up studies might be warranted to delineate the effect of the COVID-19 pandemic on the incidence and seasonality of upper respiratory infectious diseases.
5. Conclusions
The incidence of otorhinolaryngologic infectious diseases decreased during the COVID-19 pandemic period in the Korean population. In addition, the seasonality of otorhinolaryngologic infectious disease was diminished during the COVID-19 pandemic. NPIs may control the infection rate and epidemics of infectious diseases during the COVID-19 era.
Author Contributions
H.G.C. designed the study; D.M.Y. and H.G.C. analyzed the data; S.Y.K., J.H.K., M.J.K., J.-H.K., J.C. and H.G.C. drafted and revised the paper; and H.G.C. drew the figures. All authors have read and agreed to the published version of the manuscript.
Funding
This paper was supported by Wonkwang University in 2020.
Institutional Review Board Statement
The Ethics Committee of Hallym University (2021-11-004) permitted this study following the guidelines and regulations.
Informed Consent Statement
Written informed consent was waived by the Institutional Review Board.
Data Availability Statement
Releasing of the data by the researcher is not legally permitted. All the data are available from the database of the Korea Centers for Disease Control and Prevention. The Korea Centers for Disease Control and Prevention allows data access, at a particular cost, for any researcher who promises to follow research ethics. The data of this article can be downloaded from the website after agreeing to follow the research ethics.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sahoo, S.K.; Dhandapani, S.; Singh, A.; Gendle, C.; Karthigeyan, M.; Salunke, P.; Aggarwal, A.; Singla, N.; Singla, R.; Tripathi, M.; et al. COVID-19: Changing patterns among neurosurgical patients from North India, efficacy of repeat testing, and inpatient prevalence. Neurosurg. Focus 2020, 49, E7. [Google Scholar] [CrossRef]
- Goyal, N.; Venkataram, T.; Singh, V.; Chaturvedi, J. Collateral damage caused by COVID-19: Change in volume and spectrum of neurosurgery patients. J. Clin. Neurosci. 2020, 80, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Bambra, C.; Riordan, R.; Ford, J.; Matthews, F. The COVID-19 pandemic and health inequalities. J. Epidemiol. Commun. Health 2020, 74, 964–968. [Google Scholar] [CrossRef] [PubMed]
- Cowling, B.J.; Ali, S.T.; Ng, T.W.Y.; Tsang, T.K.; Li, J.C.M.; Fong, M.W.; Liao, Q.; Kwan, M.Y.; Lee, S.L.; Chiu, S.S.; et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Health 2020, 5, e279–e288. [Google Scholar] [CrossRef]
- Yu, X. COVID-19 changes the lifestyle of the population and subtly reduces the incidence of metabolic disease. Med. Hypotheses 2021, 146, 110416. [Google Scholar] [CrossRef]
- Hong, K.H.; Lee, S.W.; Kim, T.S.; Huh, H.J.; Lee, J.; Kim, S.Y.; Park, J.-S.; Kim, G.J.; Sung, H.; Roh, K.H.; et al. Guidelines for Laboratory Diagnosis of Coronavirus Disease 2019 (COVID-19) in Korea. Ann. Lab. Med. 2020, 40, 351–360. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.; Kim, J.S.; Choi, H.; Lee, H.; Lee, C.H. Assessment of Social Distancing for Controlling COVID-19 in Korea: An Age-Structured Modeling Approach. Int. J. Environ. Res. Public Health 2020, 17, 7474. [Google Scholar] [CrossRef] [PubMed]
- Eccles, R. An Explanation for the Seasonality of Acute Upper Respiratory Tract Viral Infections. Acta Oto-Laryngol. 2002, 122, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Price, R.H.M.; Graham, C.; Ramalingam, S. Association between viral seasonality and meteorological factors. Sci. Rep. 2019, 9, 929. [Google Scholar] [CrossRef]
- Torretta, S.; Cantoni, B.; Bertolozzi, G.; Capaccio, P.; Milani, G.; Pignataro, L.; Aleo, S.; Marchisio, P. Has Otitis Media Disappeared during COVID-19 Pandemic? A Fortuitus Effect of Domestic Confinement. J. Clin. Med. 2021, 10, 2851. [Google Scholar] [CrossRef] [PubMed]
- Nordstokke, D.W.; Zumbo, B.D. A New Nonparametric Levene Test for Equal Variances. Psicológica 2010, 31, 401–430. [Google Scholar]
- Chen, B.; Wang, M.; Huang, X.; Xie, M.; Pan, L.; Liu, H.; Liu, Z.; Zhou, P. Changes in Incidence of Notifiable Infectious Diseases in China Under the Prevention and Control Measures of COVID-19. Front. Public Health 2021, 9, 1548. [Google Scholar] [CrossRef] [PubMed]
- Diesner-Treiber, S.C.; Voitl, P.; Voitl, J.J.M.; Langer, K.; Kuzio, U.; Riepl, A.; Patel, P.; Mühl-Riegler, A.; Mühl, B. Respiratory Infections in Children During a Covid-19 Pandemic Winter. Front. Pediatr. 2021, 9, 740785. [Google Scholar] [CrossRef]
- Soo, R.J.J.; Chiew, C.J.; Ma, S.; Pung, R.; Lee, V. Decreased Influenza Incidence under COVID-19 Control Measures, Singapore. Emerg. Infect. Dis. 2020, 26, 1933–1935. [Google Scholar] [CrossRef] [PubMed]
- Wong, N.-S.; Leung, C.-C.; Lee, S.-S. Abrupt Subsidence of Seasonal Influenza after COVID-19 Outbreak, Hong Kong, China. Emerg. Infect. Dis. 2020, 26, 2752–2754. [Google Scholar] [CrossRef]
- Noh, J.Y.; Seong, H.; Yoon, J.G.; Song, J.Y.; Cheong, H.J.; Kim, W.J. Social Distancing against COVID-19: Implication for the Control of Influenza. J. Korean Med. Sci. 2020, 35, e182. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Komiya, K.; Fujita, N.; Okabe, E.; Hiramatsu, K.; Kadota, J.-I. COVID-19 pandemic and the incidence of community-acquired pneumonia in elderly people. Respir. Investig. 2020, 58, 435–436. [Google Scholar] [CrossRef]
- Huang, C. The COVID-19 Pandemic and the Incidence of the Non-COVID-19 Pneumonia in Adults. Front. Med. 2021, 8, 737999. [Google Scholar] [CrossRef]
- Torretta, S.; Capaccio, P.; Coro, I.; Bosis, S.; Pace, M.E.; Bosi, P.; Pignataro, L.; Marchisio, P. Incidental lowering of otitis-media complaints in otitis-prone children during COVID-19 pandemic: Not all evil comes to hurt. Eur. J. Pediatrics 2021, 180, 649–652. [Google Scholar] [CrossRef]
- Qualls, N.; Levitt, A.; Kanade, N.; Wright-Jegede, N.; Dopson, S.; Biggerstaff, M.; Reed, C.; Uzicanin, A.; Frank, M.; Holloway, R.; et al. Community Mitigation Guidelines to Prevent Pandemic Influenza—United States, 2017. MMWR. Recomm. Rep. 2017, 66, 1–34. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.E.; Park, S.W.; Yang, W.; Vecchi, G.A.; Metcalf, C.J.E.; Grenfell, B.T. The impact of COVID-19 nonpharmaceutical interventions on the future dynamics of endemic infections. Proc. Natl. Acad. Sci. USA 2020, 117, 30547–30553. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.; Zviedrite, N.; Uzicanin, A. Effectiveness of workplace social distancing measures in reducing influenza transmission: A systematic review. BMC Public Health 2018, 18, 518. [Google Scholar] [CrossRef] [PubMed]
- Song, J.-Y.; Yun, J.-G.; Noh, J.-Y.; Cheong, H.-J.; Kim, W.-J. Covid-19 in South Korea—Challenges of Subclinical Manifestations. New Engl. J. Med. 2020, 382, 1858–1859. [Google Scholar] [CrossRef] [PubMed]
- Bardsley, M.; Morbey, R.A.; Hughes, H.E.; Beck, C.R.; Watson, C.H.; Zhao, H.; Ellis, J.; Smith, G.E.; Elliot, A.J. Epidemiology of respiratory syncytial virus in children younger than 5 years in England during the COVID-19 pandemic, measured by laboratory, clinical, and syndromic surveillance: A retrospective observational study. Lancet Infect. Dis. 2022, (in press). [CrossRef]
- Stockmann, C.; Ampofo, K.; Hersh, A.L.; Carleton, S.T.; Korgenski, K.; Sheng, X.; Pavia, A.T.; Byington, C.L. Seasonality of Acute Otitis Media and the Role of Respiratory Viral Activity in Children. Pediatr. Infect. Dis. J. 2013, 32, 314–319. [Google Scholar] [CrossRef]
- Audi, A.; Al Ibrahim, M.; Kaddoura, M.; Hijazi, G.; Yassine, H.M.; Zaraket, H. Seasonality of Respiratory Viral Infections: Will COVID-19 Follow Suit? Front. Public Health 2020, 8, 567184. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kim, D.W. Does the Clinical Spectrum of Coronavirus Disease 2019 (COVID-19) Show Regional Differences? Clin. Exp. Otorhinolaryngol. 2020, 13, 83–84. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Jang, W.; Kim, S.-W.; Lee, J.; Lim, Y.-S.; Cho, C.-G.; Park, S.-W.; Kim, B.H. The Clinical Manifestations and Chest Computed Tomography Findings of Coronavirus Disease 2019 (COVID-19) Patients in China: A Proportion Meta-Analysis. Clin. Exp. Otorhinolaryngol. 2020, 13, 95–105. [Google Scholar] [CrossRef]
- Prevention KCfDCa. Coronavirus Disease. 2019–2020. Available online: http://ncov.mohw.go.kr (accessed on 5 October 2020).
- Choi, W.S. The National Influenza Surveillance System of Korea. Infect. Chemother. 2019, 51, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-E.; Ryu, Y. Transmissibility and severity of influenza virus by subtype. Infect. Genet. Evol. 2018, 65, 288–292. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).