Prevalence of Post-Traumatic Stress Disorder (PTSD) in Healthcare Workers following the First SARS-CoV Epidemic of 2003: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
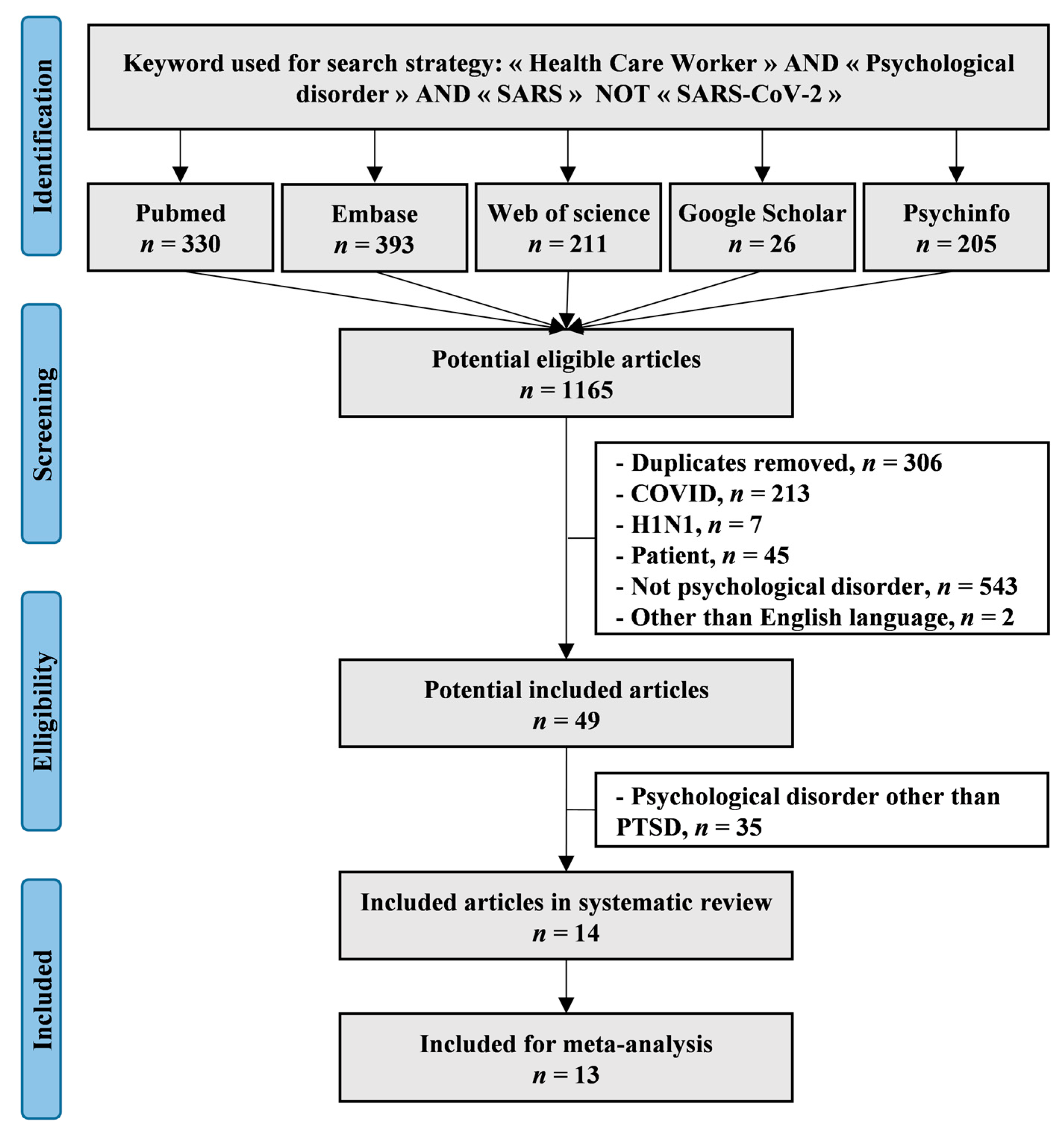
2. Materials and Methods
2.1. Literature Search
2.2. Data Extraction
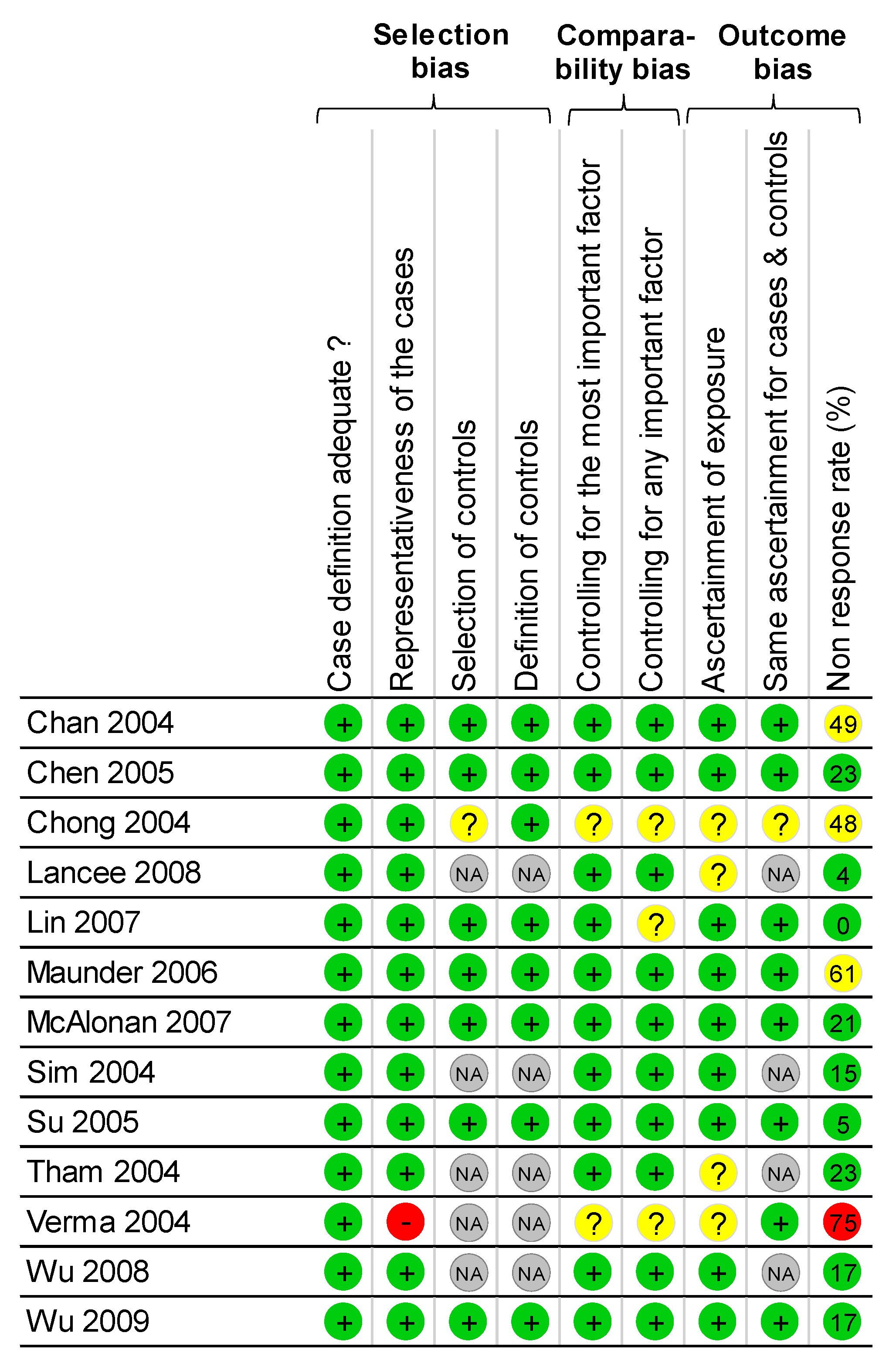
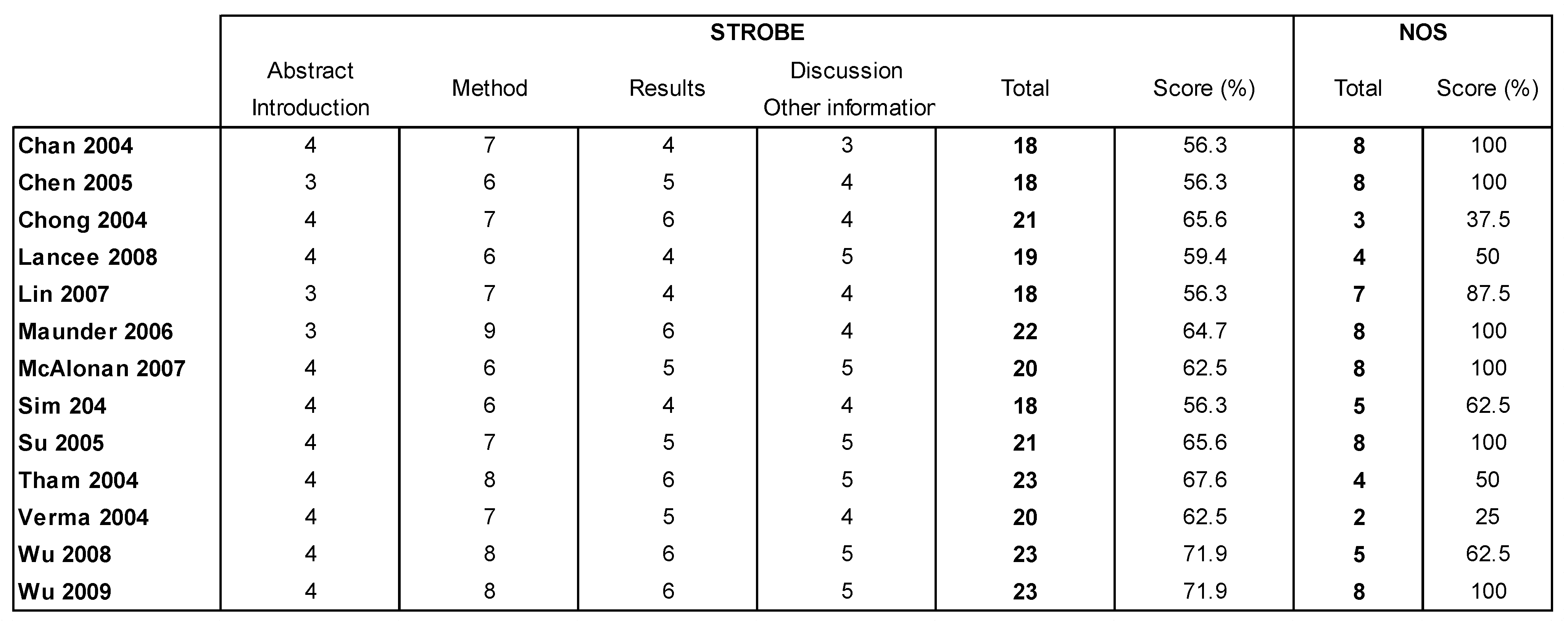
2.3. Quality of Assessment
2.4. Statistical Considerations
3. Results
3.1. Study Designs of Included Studies
3.2. Quality of Articles
3.3. Aims of Included Articles
3.4. Inclusion and Exclusion Criteria of Included Studies
3.5. Population
3.6. Assessment of PTSD
3.7. Characteristics of Exposure
3.8. Meta-Analysis of Prevalence of PTSD in HCWs Population
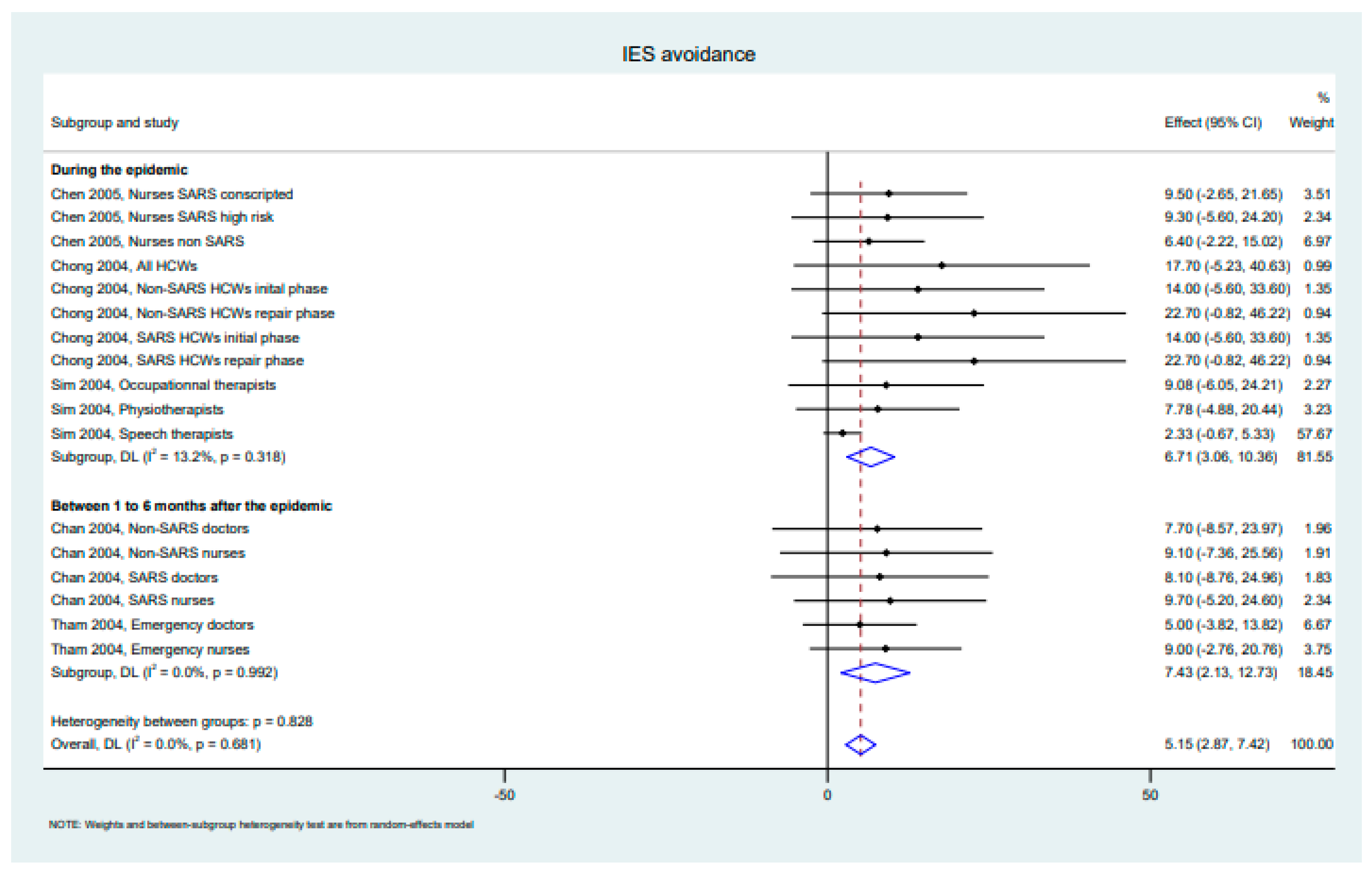
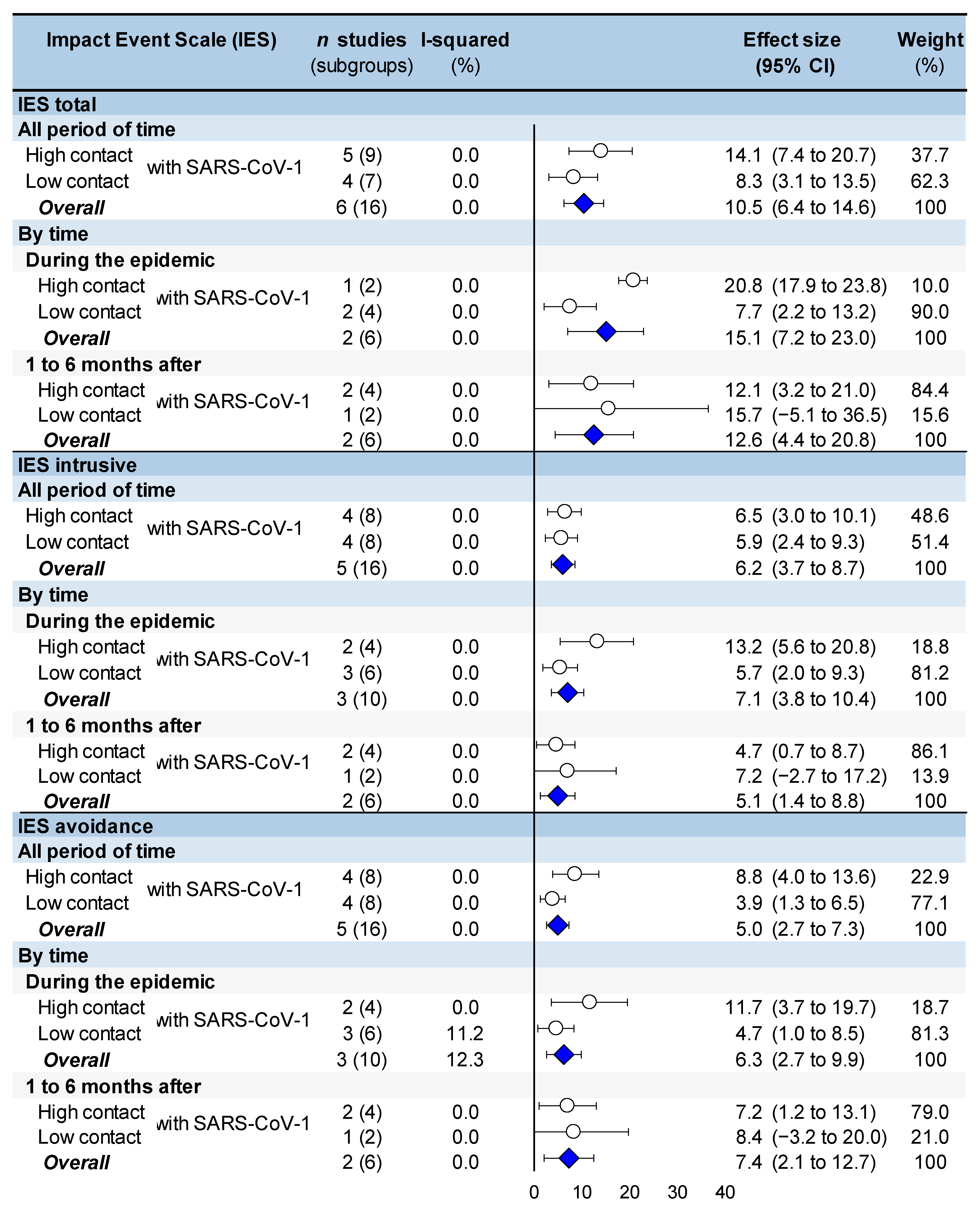
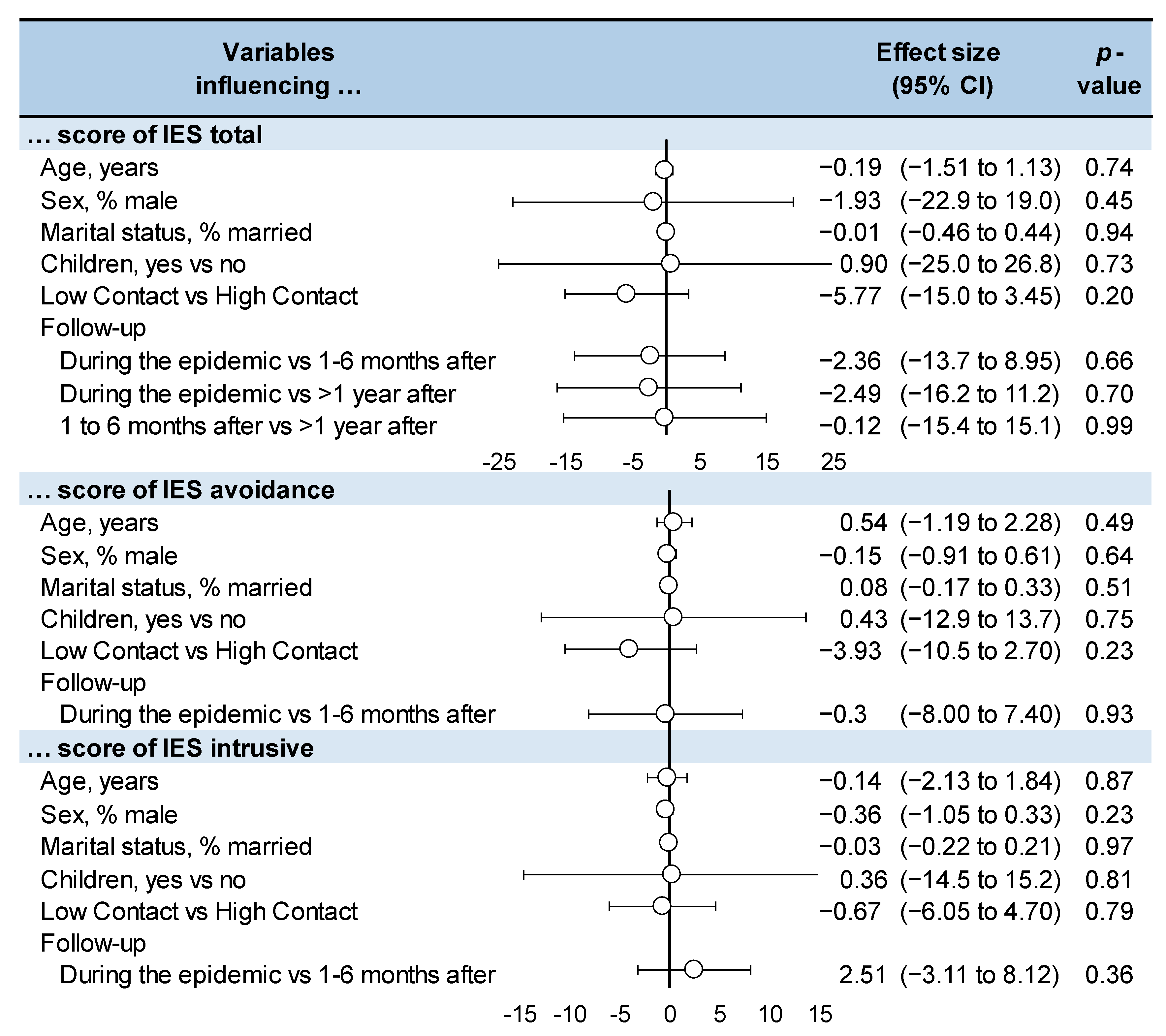
3.9. Meta-Analysis of IES Score in HCWs Population
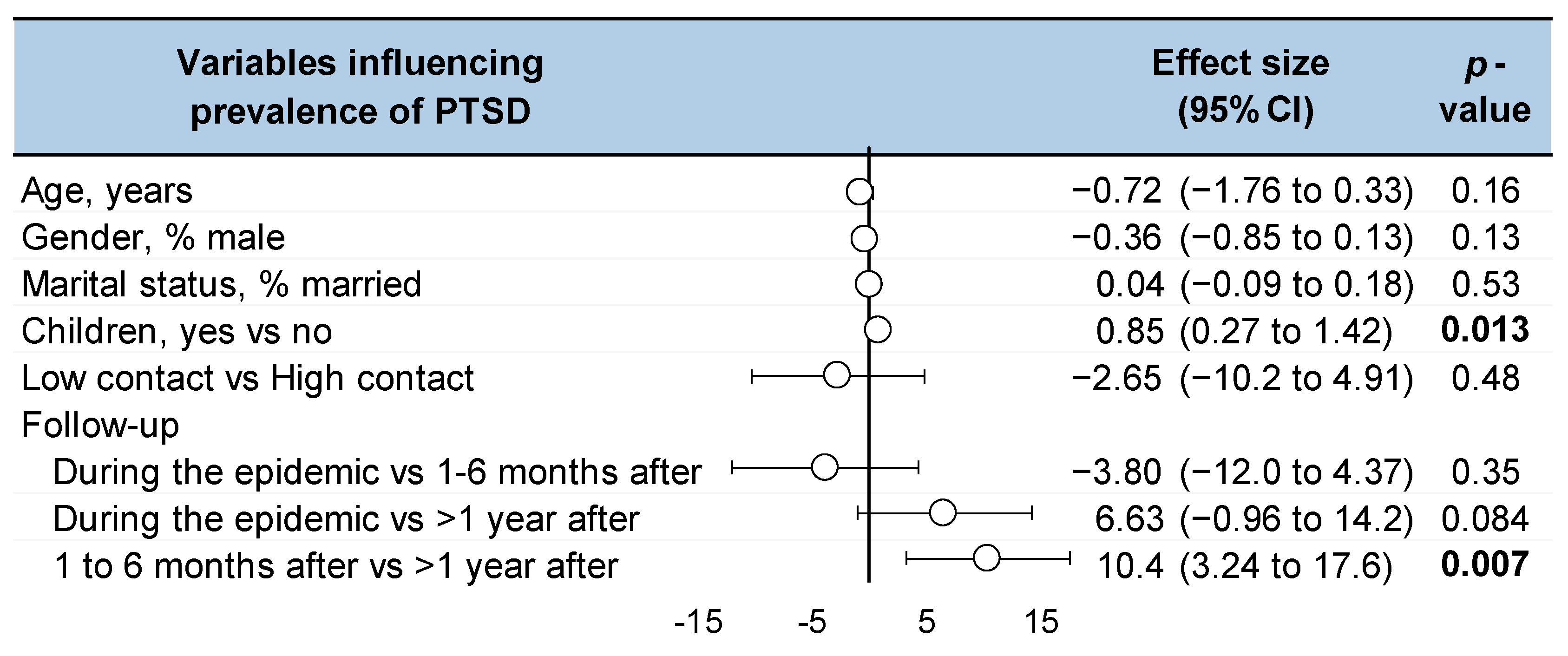
3.10. Meta-Regression and Influencing Factors
4. Discussion
4.1. PTSD in Healthcare Workers: A Public Health Issue
4.2. Long-Term PTSD
4.3. Contact with Patient with SARS: A Risk Factor for PTSD
4.4. Other Influencing Factors for PTSD
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- (“healthcare worker” OR “Health worker” OR “health care worker” OR “Health workers” OR “health care workers” OR “hospital workers” OR “hospital worker” OR “hospital employees” OR “hospital employee” OR “hospital staff” OR “hospital staffs” OR “personnel hospital” OR “hospital personnel” OR “healthcare provider” OR “health personnel” OR “health care providers” OR “nurses” OR “nurse” OR “nursing personnel” OR “nursing field” OR “discipline of nursing” OR “nursing profession” OR “personnel nursing” OR “paramedical practitioners” OR “assistant healthcare” OR “healthcare support worker” OR “professional allied health” OR “assistants healthcare” OR “healthcare assistant” OR “healthcare assistants” OR “professionals allied health” OR “paramedics” OR “health professionals allied” OR “healthcare support workers” OR “allied health professionals” OR “allied health professional” OR “population program specialists” OR “allied health personnel” OR “therapists physical” OR “therapist physical” OR “physical therapist” OR “physiotherapists” OR “physical therapists” OR “physiotherapist” OR “physicians” OR “doctor” OR “medical practitioner” OR “physician” OR “assistant nursing” OR “personal care assistant” OR “nursing assistant” OR “Nursing Assistants” OR “assistants nursing” OR “provider health care” OR “healthcare professional” OR “health professional” OR “personnel health” OR “provider healthcare” OR “healthcare providers” OR “care personnel” OR “field workers” OR “providers health care” OR “health profession” OR “worker field” OR “providers healthcare” OR “health care provider” OR “healthcare workers” OR “health care personnel” OR “fieldworker” OR “field worker” OR “primary care provider” OR “workers field” OR “nursing staff hospital” OR “hospital nursing staffs” OR “hospital nursing staff” OR “hospital registrars” OR “hospital registrar” OR “medical staffs hospital” OR “hospital medical staff” OR “medical staff hospital” OR “hospital medical staffs” OR”medical staff” OR “staffs medical” OR “staff medical” OR “medical staffs”)
- AND
- (Psychosocial OR psychological OR anxiety OR stress OR stressors OR stressful OR Stresses OR Anxieties OR “psychologic adaptation” OR “adaptation psychological” OR “behavior coping” OR “behaviors coping” OR “skill coping” OR “behavior adaptive” OR “adaptive behavior” OR “coping behavior” OR “skills coping” OR “coping behaviors” OR “adaptation psychologic” OR “coping skill” OR “coping skills” OR “adaptive behaviors” OR “behaviors adaptive” OR “psychological adaptation” OR “health mental” OR “mental hygiene” OR “hygiene mental” OR “emotional health” OR “mental health” OR “mental well-being” OR “caregiver burnout” OR “burn-out syndrome” OR “psychological burn-out” OR “burnout” OR “student burnout” OR “burnout psychological” OR “burnout school” OR “school burnout” OR “psychological burn-out” OR “caregiver exhaustion” OR “burnout syndrome” OR “burn-out syndrome” OR “psychological burnout” OR “burn-out” OR “burn-out” OR “stressor psychological” OR “stressed” OR “stressors psychological” OR “psychological stressors” OR “life stresses” OR “stress” OR “psychological stresses” OR “psychological stressor” OR “stresses job” OR “workplace stresses” OR “job-related stresses” OR “work place stresses” OR “work-related stresses” OR “job stresses” OR “occupational stresses” OR “stresses professional” OR “professional stresses” OR “posttraumatic neurosis” OR “posttraumatic psychosis” OR “complex ptsd” OR “neuroses post traumatic” OR “moral injury” OR “stress disorders posttraumatic” OR “moral injuries” OR “post-traumatic neuroses” OR “posttraumatic neuroses” OR “posttraumatic syndrome” OR “post-traumatic stress disorder” OR “post-traumatic neuroses” OR “ptsd” OR “chronic ptsd” OR “adjustment disorder diagnosis” OR “disorders adjustment” OR “culture shock” OR “adjustment disease” OR “depressions reactive” OR “grief reaction” OR “adjustment disorder diagnosis” OR “disorders adjustment” OR “reactive disorder” OR “adjustment disorder” OR “adjustment reaction” OR “adaptation reaction” OR “reactive depression” OR “depressions reactive” OR “performance anxieties”)
- AND
- (“SARS virus OR “coronavirus infections” OR “corona virus infection” “sars-cov1” OR “sars-cov-1” OR “sars-cov” OR “coronavirus sars” “sars-1” OR “severe acute respiratory syndrome sars cov” OR “severe acute respiratory syndrome sars” OR “sars-associated coronavirus” OR “severe acute respiratory syndrome sars cov” OR “sars-cov infection” OR “sars” OR “respiratory syndrome severe acute” OR “sars coronavirus infection” OR “coronavirus” OR “severe acute respiratory syndrome sars” OR “sars-cov infection” OR “respiratory syndrome severe acute” OR “sars severe acute respiratory syndrome” OR “severe acute respiratory syndrome” OR “sars severe acute respiratory syndrome” OR “sars-associated coronavirus” OR “severe acute respiratory syndrome sars diagnosis” OR “severe acute respiratory syndrome sars diagnosis” OR “sars-related coronavirus” OR “severe acute respiratory syndrome-related coronavirus” OR “severe acute respiratory syndrome virus” OR “sars” OR “severe acute respiratory syndrome-related coronavirus” OR “severe acute respiratory syndrome coronavirus” OR “sars associated coronavirus urbani” OR “sars-coronavirus” OR “severe acute respiratory syndrome sars coronavirus” OR “sars-related coronavirus” OR “severe acute respiratory syndrome associated coronavirus.
Appendix B
Appendix C

Appendix D
Appendix E
References
- Bisson, J.I.; Cosgrove, S.; Lewis, C.; Roberts, N.P. Post-traumatic Stress Disorder. BMJ—Brit. Med. J. 2015, 351, h6161. [Google Scholar] [CrossRef]
- Kessler, R.C.; Sonnega, A.; Bromet, E.; Hughes, M.; Nelson, C.B. Posttraumatic Stress Disorder in the National Comorbidity Survey. Arch. Gen. Psychiatry 1995, 52, 1048–1060. [Google Scholar] [CrossRef]
- Hsiao, Y.Y.; Chang, W.H.; Ma, I.C.; Wu, C.-L.; Chen, P.S.; Yang, Y.K.; Lin, C.-H. Long-Term PTSD Risks in Emergency Medical Technicians Who Responded to the 2016 Taiwan Earthquake: A Six-Month Observational Follow-Up Study. Int. J. Env. Res. Public Health 2019, 16, 4983. [Google Scholar] [CrossRef]
- Gregory, J.; de Lepinau, J.; de Buyer, A.; Delanoy, N.; Mir, O.; Gaillard, R. The Impact of the Paris Terrorist Attacks on the Mental Health of Resident Physicians. BMC Psychiatry 2019, 19, 79. [Google Scholar] [CrossRef] [PubMed]
- Serrano-Ripoll, M.J.; Meneses-Echavez, J.F.; Ricci-Cabello, I.; Fraile-Navarro, D.; Fiol-deRoque, M.A.; Pastor-Moreno, G.; Castro, A.; Ruiz-Pérez, I.; Zamanillo Campos, R.; Gonçalves-Bradley, D.C. Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta-analysis. J. Affect. Disord. 2020, 277, 347–357. [Google Scholar] [CrossRef]
- Ouyang, H.; Geng, S.; Zhou, Y.; Wang, J.; Zhan, J.; Shang, Z.; Jia, Y.; Yan, W.; Zhang, Y.; Li, X.; et al. The Increase of PTSD in Front-line Health Care Workers During the COVID-19 Pandemic and the Mediating Role of Risk Perception: A One-Year Follow-up Study. Transl. Psychiatry 2022, 12, 180. [Google Scholar] [CrossRef] [PubMed]
- Crabbe, J.; Bowley, D.; Boffard, K.; Alexander, D.; Klein, S. Are Health Professionals Getting Caught in the Crossfire? The Personal Implications of Caring for Trauma Victims. Emerg. Med. J. 2004, 21, 568–572. [Google Scholar] [CrossRef]
- Dutheil, F.; Mondillon, L.; Navel, V. PTSD as the second tsunami of the SARS-Cov-2 pandemic. Psychol. Med. 2021, 51, 1773–1774. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Chen, Y.; Li, X.; An, Y. Predicting Posttraumatic Stress and Depression Symptoms Among Frontline Firefighters in China. J. Nerv. Ment. Dis. 2021, 209, 23–27. [Google Scholar] [CrossRef]
- Ćosić, K.; Popović, S.; Šarlija, M.; Kesedžić, I.; Jovanovic, T. Artificial Intelligence in Prediction of Mental Health Disorders Induced by The COVID-19 Pandemic Among Health Care Workers. Croat. Med. J. 2020, 61, 279–288. [Google Scholar] [CrossRef]
- Antonaccio, C.M.; Pham, P.; Vinck, P.; Collet, K.; Brennan, R.T.; Betancourt, T.S. Fear, Distress, and Perceived Risk Shape Stigma Toward Ebola Survivors: A Prospective Longitudinal Study. BMC Public Health 2021, 21, 2066. [Google Scholar] [CrossRef] [PubMed]
- Chan-Yeung, M.; Xu, R. SARS: Epidemiology. Respirology 2003, 8, S9–S14. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Fang, Y.; Guan, Z.; Fan, B.; Kong, J.; Yao, Z.; Liu, X.; Fuller, C.J.; Susser, E.; Lu, J.; et al. The Psychological Impact of the SARS Epidemic on Hospital Employees in China: Exposure, Risk Perception, and Altruistic Acceptance of Risk. Can. J. Psychiatry 2009, 54, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-Y.; Peng, Y.-C.; Wu, Y.-H.; Chang, J.; Chan, C.-H.; Yang, D.-Y. The Psychological Effect of Severe Acute Respiratory Syndrome on Emergency Department Staff. Emerg. Med. J. 2007, 24, 12–17. [Google Scholar] [CrossRef]
- Maunder, R.G.; Lancee, W.J.; Balderson, K.E.; Bennett, J.P.; Borgundvaag, B.; Evans, S.; Fernandes, C.M.B.; Goldbloom, D.S.; Gupta, M.; Hunter, J.J.; et al. Long-term Psychological and Occupational Effects of Providing Hospital Healthcare during SARS Outbreak. Emerg. Infect. Dis. J. CDC 2006, 12, 1924. [Google Scholar] [CrossRef]
- Horowitz, M.; Wilner, N.; Alvarez, W. Impact of Event Scale: A Measure of Subjective Stress. Psychosom. Med. 1979, 41, 209–218. [Google Scholar] [CrossRef]
- Sundin, E.C.; Horowitz, M.J. Impact of Event Scale: Psychometric Properties. Br. J. Psychiatry 2002, 180, 205–209. [Google Scholar] [CrossRef]
- Creamer, M.; Bell, R.; Failla, S. Psychometric Properties of The Impact of Event Scale—Revised. Behav. Res. 2003, 41, 1489–1496. [Google Scholar] [CrossRef] [PubMed]
- Davidson, J.R.T.; Tharwani, H.M.; Connor, K.M. Davidson Trauma Scale (DTS): Normative Scores in The General Population and Effect Sizes in Placebo-Controlled SSRI Trials. Depress. Anxiety 2002, 15, 75–78. [Google Scholar] [CrossRef]
- Chen, C.H.; Lin, S.K.; Tang, H.S.; Shen, W.W.; Lu, M.L. The Chinese Version of The Davidson Trauma Scale: A Practice Test for Validation. Psychiatry Clin. Neurosci. 2001, 55, 493–499. [Google Scholar] [CrossRef]
- O’Donnell, M.L.; Elliott, P.; Lau, W.; Creamer, M. PTSD Symptom Trajectories: From Early to Chronic Response. Behav. Res. Ther. 2007, 45, 601–606. [Google Scholar] [CrossRef] [PubMed]
- Galli, F.; Pozzi, G.; Ruggiero, F.; Mameli, F.; Cavicchioli, M.; Barbieri, S.; Canevini, M.P.; Priori, A.; Pravettoni, G.; Sani, G.; et al. A Systematic Review and Provisional Metanalysis on Psychopathologic Burden on Health Care Workers of Coronavirus Outbreaks. Front. Psychiatry 2020, 11, 568664. [Google Scholar] [CrossRef] [PubMed]
- Kaysen, D.; Rosen, G.; Bowman, M.; Resick, P.A. Duration of Exposure and the Dose-Response Model of PTSD. J. Interpers. Violence 2010, 25, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Goenjian, A.K.; Walling, D.; Steinberg, A.M.; Karayan, I.; Najarian, L.M.; Pynoos, R. A Prospective Study of Posttraumatic Stress and Depressive Reactions Among Treated and Untreated Adolescents 5 Years After a Catastrophic Disaster. Am. J. Psychiatry 2005, 162, 2302–2308. [Google Scholar] [CrossRef]
- Stang, A. Critical Evaluation of the Newcastle-Ottawa Scale for the Assessment of the Quality of Nonrandomized Studies in Meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’Connell, D.; Robertson, J.; Peterson, J.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analysis. Available online: https://web.archive.org/web/20210716121605id_/http://www3.med.unipmn.it/dispense_ebm/2009-2010/Corso%20Perfezionamento%20EBM_Faggiano/NOS_oxford.pdf (accessed on 30 August 2022).
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. Ann. Intern. Med. 2007, 147, W-163–W-194. [Google Scholar] [CrossRef]
- Da Costa, B.R.; Cevallos, M.; Altman, D.G.; Rutjes, A.W.S.; Egger, M. Uses and Misuses of the STROBE Statement: Bibliographic Study. BMJ Open 2011, 1, e000048. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in Clinical Trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Chan, A.O.M.; Huak, C.Y. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup. Med. 2004, 54, 190–196. [Google Scholar] [CrossRef]
- Chen, C.-S.; Wu, H.-Y.; Yang, P.; Yen, C.-F. Psychological Distress of Nurses in Taiwan Who Worked During The Outbreak of SARS. Psychiatr. Serv. 2005, 56, 76–79. [Google Scholar] [CrossRef]
- Chong, M.-Y.; Wang, W.-C.; Hsieh, W.-C.; Lee, C.-Y.; Chiu, N.-M.; Yeh, W.-C.; Huang, O.-L.; Wen, J.-K.; Chen, C.-L. Psychological Impact of Severe Acute Respiratory Syndrome on Health Workers in A Tertiary Hospital. Br. J. Psychiatry 2004, 185, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Tham, K.Y.; Tan, Y.H.; Loh, O.H.; Tan, W.L.; Ong, M.K.; Tang, H.K. Psychiatric morbidity among emergency department doctors and nurses after the SARS outbreak. Ann. Acad. Med. Singap. 2004, 33, S78–S79. [Google Scholar] [PubMed]
- Lancee, W.J.; Maunder, R.G.; Goldbloom, D.S. Prevalence of Psychiatric Disorders Among Toronto Hospital Workers One to Two Years After the SARS Outbreak. Psychiatr. Serv. 2008, 59, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.-C.; Shu, B.-C.; Chang, Y.-Y.; Lung, F.-W. The Mental Health of Hospital Workers Dealing with Severe Acute Respiratory Syndrome. Psychother. Psychosom. 2006, 75, 370–375. [Google Scholar] [CrossRef] [PubMed]
- McAlonan, G.M.; Lee, A.M.; Cheung, V.; Cheung, C.; Tsang, K.W.T.; Sham, P.C.; Chua, S.E.; Wong, J.G.W.S. Immediate and Sustained Psychological Impact of an Emerging Infectious Disease Outbreak on Health Care Workers. Can. J. Psychiatry 2007, 52, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Sim, S.S.; Huak, C.Y. Psychological Impact of the SARS Outbreak on a Singaporean Rehabilitation Department. Int. J. Ther. Rehabil. 2004, 11, 417–423. [Google Scholar] [CrossRef]
- Su, T.-P.; Lien, T.-C.; Yang, C.-Y.; Su, Y.L.; Wang, J.-H.; Tsai, S.-L.; Yin, J.-C. Prevalence of Psychiatric Morbidity and Psychological Adaptation of the Nurses in a Structured SARS Caring Unit During Outbreak: A Prospective and Periodic Assessment Study in Taiwan. J. Psychiatr. Res. 2007, 41, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.; Mythily, S.; Chan, Y.H.; Deslypere, J.P.; Teo, E.K.; Chong, S.A. Post-SARS Psychological Morbidity and Stigma Among General Practitioners and Traditional Chinese Medicine Practitioners in Singapore. Ann. Acad. Med. Singap. 2004, 33, 743–748. [Google Scholar] [PubMed]
- Wu, P.; Liu, X.; Fang, Y.; Fan, B.; Fuller, C.J.; Guan, Z.; Yao, Z.; Kong, J.; Lu, J.; Litvak, I.J. Alcohol Abuse/Dependence Symptoms Among Hospital Employees Exposed to a SARS Outbreak. Alcohol Alcohol. 2008, 43, 706–712. [Google Scholar] [CrossRef]
- Dutheil, F.; Aubert, C.; Pereira, B.; Dambrun, M.; Moustafa, F.; Mermillod, M.; Baker, J.S.; Trousselard, M.; Lesage, F.-X.; Navel, V. Suicide Among Physicians and Health-Care Workers: A Systematic Review and Meta-analysis. PLoS ONE 2019, 14, e0226361. [Google Scholar] [CrossRef]
- Yates, S.W. Physician Stress and Burnout. Am. J. Med. 2020, 133, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Menon, N.K.; Shanafelt, T.D.; Sinsky, C.A.; Linzer, M.; Carlasare, L.; Brady, K.J.S.; Stillman, M.J.; Trockel, M.T. Association of Physician Burnout With Suicidal Ideation and Medical Errors. JAMA Netw. Open 2020, 3, e2028780. [Google Scholar] [CrossRef]
- Renner, A.; Kaiser, J.; Kersting, A. Traumatization in the Medical Profession: Initiating Events, Roles and Process Factors. Psychother. Psychosom. Med. Psychol. 2022. [Google Scholar] [CrossRef]
- Edmondson, D.; von Känel, R. Posttraumatic Stress Disorder and Cardiovascular Disease. Lancet Psychiatry 2017, 4, 320–329. [Google Scholar] [CrossRef]
- Miller, M.W.; Lin, A.P.; Wolf, E.J.; Miller, D.R. Oxidative Stress, Inflammation, and Neuroprogression in Chronic PTSD. Harv. Rev. Psychiatry 2018, 26, 57–69. [Google Scholar] [CrossRef] [PubMed]
- Perkins, J.D.; Wilkins, S.S.; Kamran, S.; Shuaib, A. Post-traumatic Stress Disorder and its Association with Stroke and Stroke Risk Factors: A Literature Review. Neurobiol. Stress 2021, 14, 100332. [Google Scholar] [CrossRef]
- Rosman, L.; Sico, J.J.; Lampert, R.; Gaffey, A.E.; Ramsey, C.M.; Dziura, J.; Chui, P.W.; Cavanagh, C.E.; Brandt, C.; Haskell, S.; et al. Posttraumatic Stress Disorder and Risk for Stroke in Young and Middle-Aged Adults. Stroke 2019, 50, 2996–3003. [Google Scholar] [CrossRef]
- Schug, C.; Geiser, F.; Hiebel, N.; Beschoner, P.; Jerg-Bretzke, L.; Albus, C.; Weidner, K.; Morawa, E.; Erim, Y. Sick Leave and Intention to Quit the Job among Nursing Staff in German Hospitals during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 1947. [Google Scholar] [CrossRef]
- Giannopoulou, I.; Tsobanoglou, G.O. COVID-19 Pandemic: Challenges and Opportunities For the Greek Health Care System. Ir. J. Psychol. Med. 2020, 37, 226–230. [Google Scholar] [CrossRef] [PubMed]
- Bashier, H.; Ikram, A.; Khan, M.A.; Baig, M.; Al Gunaid, M.; Al Nsour, M.; Khader, Y. The Anticipated Future of Public Health Services Post COVID-19: Viewpoint. JMIR Public Health Surveill. 2021, 7, e26267. [Google Scholar] [CrossRef]
- Hong, X.; Currier, G.W.; Zhao, X.; Jiang, Y.; Zhou, W.; Wei, J. Posttraumatic Stress Disorder in Convalescent Severe Acute Respiratory Syndrome Patients: A 4-Year Follow-up Study. Gen. Hosp. Psychiatry 2009, 31, 546–554. [Google Scholar] [CrossRef]
- Shlosberg, A.; Strous, R.D. Long-term Follow-up (32 Years) of PTSD in Israeli Yom Kippur War Veterans. J. Nerv. Ment. Dis. 2005, 193, 693–696. [Google Scholar] [CrossRef] [PubMed]
- Notman, M.T.; Nadelson, C.C. Medicine: A Career Conflict for Women. Am. J. Psychiatry 1973, 130, 1123–1127. [Google Scholar] [CrossRef]
- Mao, J.; Wang, C.; Teng, C.; Wang, M.; Zhou, S.; Zhao, K.; Ye, X.; Wang, Y. Prevalence and Associated Factors of PTSD Symptoms After the COVID-19 Epidemic Outbreak in an Online Survey in China: The Age and Gender Differences Matter. Neuropsychiatr. Dis. Treat. 2022, 18, 761–771. [Google Scholar] [CrossRef]
- Jakšić, N.; Brajković, L.; Ivezić, E.; Topić, R.; Jakovljević, M. The Role of Personality Traits in Posttraumatic Stress Disorder (PTSD). Psychiatr. Danub. 2012, 24, 256–266. [Google Scholar]
- Dutheil, F.; Danini, B.; Bagheri, R.; Fantini, M.L.; Pereira, B.; Moustafa, F.; Trousselard, M.; Navel, V. Effects of a Short Daytime Nap on the Cognitive Performance: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 10212. [Google Scholar] [CrossRef]
- Benichou, T.; Pereira, B.; Mermillod, M.; Tauveron, I.; Pfabigan, D.; Maqdasy, S.; Dutheil, F. Heart Rate Variability In Type 2 Diabetes Mellitus: A Systematic Review And Meta-analysis. PLoS ONE 2018, 13, e0195166. [Google Scholar] [CrossRef] [PubMed]
- Al Falasi, B.; Al Mazrouei, M.; Al Ali, M.; Al Dhamani, M.; Al Ali, A.; Al Kindi, M.; Dalkilinc, M.; Al Qubaisi, M.; Campos, L.A.; Al Tunaiji, H.; et al. Prevalence and Determinants of Immediate and Long-Term PTSD Consequences of Coronavirus-Related (CoV-1 and CoV-2) Pandemics among Healthcare Professionals: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 2182. [Google Scholar] [CrossRef] [PubMed]
- Dutheil, F.; Parreira, L.M.; Eismann, J.; Lesage, F.-X.; Balayssac, D.; Lambert, C.; Clinchamps, M.; Pezet, D.; Pereira, B.; Le Roy, B. Burnout in French General Practitioners: A Nationwide Prospective Study. Int. J. Environ. Res. Public Health 2021, 18, 12044. [Google Scholar] [CrossRef]
- Lopez, V.; Chamoux, A.; Tempier, M.; Thiel, H.; Ughetto, S.; Trousselard, M.; Naughton, G.; Dutheil, F. The Long-term Effects of Occupational Exposure to Vinyl Chloride Monomer on Microcirculation: A Cross-Sectional Study 15 years After Retirement. BMJ Open 2013, 3, e002785. [Google Scholar] [CrossRef]
- Hopwood, C.J.; Morey, L.C.; Edelen, M.O.; Shea, M.T.; Grilo, C.M.; Sanislow, C.A.; McGlashan, T.H.; Daversa, M.T.; Gunderson, J.G.; Zanarini, M.C.; et al. A Comparison of Interview And Self-Report Methods For the Assessment of Borderline Personality Disorder Criteria. Psychol. Assess. 2008, 20, 81–85. [Google Scholar] [CrossRef]
- Dutheil, F.; de Saint Vincent, S.; Pereira, B.; Schmidt, J.; Moustafa, F.; Charkhabi, M.; Bouillon-Minois, J.-B.; Clinchamps, M. DHEA as a Biomarker of Stress: A Systematic Review and Meta-Analysis. Front. Psychiatry 2021, 12, 688367. [Google Scholar] [CrossRef]
- Dutheil, F.; Bessonnat, B.; Pereira, B.; Baker, J.S.; Moustafa, F.; Fantini, M.L.; Mermillod, M.; Navel, V. Napping and Cognitive Performance During Night Shifts: A Systematic Review and Meta-analysis. Sleep 2020, 43, zsaa109. [Google Scholar] [CrossRef]



| Study | Country | Design | Category of | Contact | Hospital | n | Age | Gender | PTSD | Measurement | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| HCWs | High/Low | Department | Years | % Men | n | Scale | Time | ||||
| Chan 2004 | Singapour | Cross- sectionnal | Physicians/Nurses | High | SARS unit | 106 | n per age group | - | 20 | IES | 2 months after epidemic |
| Physicians/Nurses | Low | Non-SARS unit | 555 | 107 | |||||||
| Chen 2005 | Taiwan | Cross- sectionnal | Nurses | High | SARS unit | 86 | 26.5 ± 3.1 | 0 | - | IES | During the epidemic |
| Low | Non-SARS unit | 42 | |||||||||
| Chong 2004 | Taiwan | Cohort | All | High/Low | 1257 | 31.8 ± 6.43 | 18.9 | - | IES | ||
| Lancee 2008 | Canada | Cohort | All | High | ED, SARS unit, ICU | 448 | 41.3 ± 10.2 | 14 | 4 | IES | 1 year after epidemic |
| 139 | 45.0 ± 9.6 | 13 | 2 | 2 years after epidemic | |||||||
| Lin 2007 | Taiwan | Cross- sectionnal | All | High | ED | 66 | 33.5 | 7.6 | 13 | DTS-C | 1 month after epidemic |
| Low | Psychiatry | 26 | 34.5 | 11.5 | 5 | ||||||
| Lu 2006 * | Taiwan | Cross- sectionnal | Physicians | 24 | 36.5 ± 6.7 | 100 | |||||
| Nurses | High | SARS unit | 49 | 31.6 ± 5.5 | 6.1 | - | - | During the epidemic | |||
| Other HCWs | 54 | 31.1 ± 7.6 | 48.1 | ||||||||
| Maunder 2006 | Canada | Cross- sectionnal | All | High | SARS unit | 587 | n per age group | 14 | 81 | IES | 1 year after epidemic |
| Low | Non-SARS unit | 182 | 10.4 | 15 | |||||||
| McAlonan 2007 | Hong-Kong | Cohort | All | High | 106 | n per age group | 29.2 | - | - | During The epidemic | |
| Low | 70 | 24.3 | |||||||||
| High | 71 | 33.8 | IES-R | 1 year after epidemic | |||||||
| Low | 113 | 37.1 | |||||||||
| Sim 2004 | Singapour | Cross- sectionnal | Physiotherapist | Low | Rehabilitation unit | 18 | n per age group | - | 2 | IES | |
| Occupational therapist | 13 | 2 | During the epidemic | ||||||||
| Speech therapist | 3 | 1 | |||||||||
| Su 2007 | Taiwan | Cohort | Nurses | High | SARS ICU | 26 | 31.5 ± 6.2 | 0 | 10 | DTS-C | During the epidemic |
| Regular SARS unit | 44 | 29.8 ± 7.6 | 13 | ||||||||
| Low | ICU | 17 | 32.7 ± 4.3 | 2 | |||||||
| Neurology | 15 | 25.4 ± 3.7 | 4 | ||||||||
| Tham 2004 | Singapour | Cross- sectionnal | Physicians | High | Emergency | 38 | 31.6 ± 4.4 | 65.8 | 5 | IES | 6 months after epidemic |
| Nurses | 58 | 32.1 ± 9.2 | 8.6 | 12 | |||||||
| Verma 2004 | Singapour | Cross- sectionnal | General practitionner | High | 32 | 45.0 ± 11.2 | 60.6 | - | IES | During the epidemic | |
| Low | 682 | ||||||||||
| Traditionnal Chinese Medicine | High | 1 | 50.1 ± 9.0 | 59 | |||||||
| Low | 326 | ||||||||||
| Wu 2008 | China | Cross- sectionnal | All | High | 549 | n per age group | 23.5 | 55 | IES | 3 years after epidemic | |
| Wu 2009 | China | Cross- sectionnal | All | High | SARS unit | 135 | n per age group | 23.5 | 26 | IES-R | 3 years after epidemic |
| Low | Non-SARS unit | 414 | 29 | ||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alberque, B.; Laporte, C.; Mondillon, L.; Baker, J.S.; Mermillod, M.; Brousse, G.; Ugbolube, U.C.; Bagheri, R.; Bouillon-Minois, J.-B.; Dutheil, F. Prevalence of Post-Traumatic Stress Disorder (PTSD) in Healthcare Workers following the First SARS-CoV Epidemic of 2003: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 13069. https://doi.org/10.3390/ijerph192013069
Alberque B, Laporte C, Mondillon L, Baker JS, Mermillod M, Brousse G, Ugbolube UC, Bagheri R, Bouillon-Minois J-B, Dutheil F. Prevalence of Post-Traumatic Stress Disorder (PTSD) in Healthcare Workers following the First SARS-CoV Epidemic of 2003: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(20):13069. https://doi.org/10.3390/ijerph192013069
Chicago/Turabian StyleAlberque, Bastien, Catherine Laporte, Laurie Mondillon, Julien S. Baker, Martial Mermillod, George Brousse, Ukadike Chris Ugbolube, Reza Bagheri, Jean-Baptiste Bouillon-Minois, and Frédéric Dutheil. 2022. "Prevalence of Post-Traumatic Stress Disorder (PTSD) in Healthcare Workers following the First SARS-CoV Epidemic of 2003: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 20: 13069. https://doi.org/10.3390/ijerph192013069
APA StyleAlberque, B., Laporte, C., Mondillon, L., Baker, J. S., Mermillod, M., Brousse, G., Ugbolube, U. C., Bagheri, R., Bouillon-Minois, J.-B., & Dutheil, F. (2022). Prevalence of Post-Traumatic Stress Disorder (PTSD) in Healthcare Workers following the First SARS-CoV Epidemic of 2003: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(20), 13069. https://doi.org/10.3390/ijerph192013069












