The Efficacy of a New AMCOP® Elastodontic Protocol for Orthodontic Interceptive Treatment: A Case Series and Literature Overview
Abstract
:1. Introduction
2. Materials and Methods
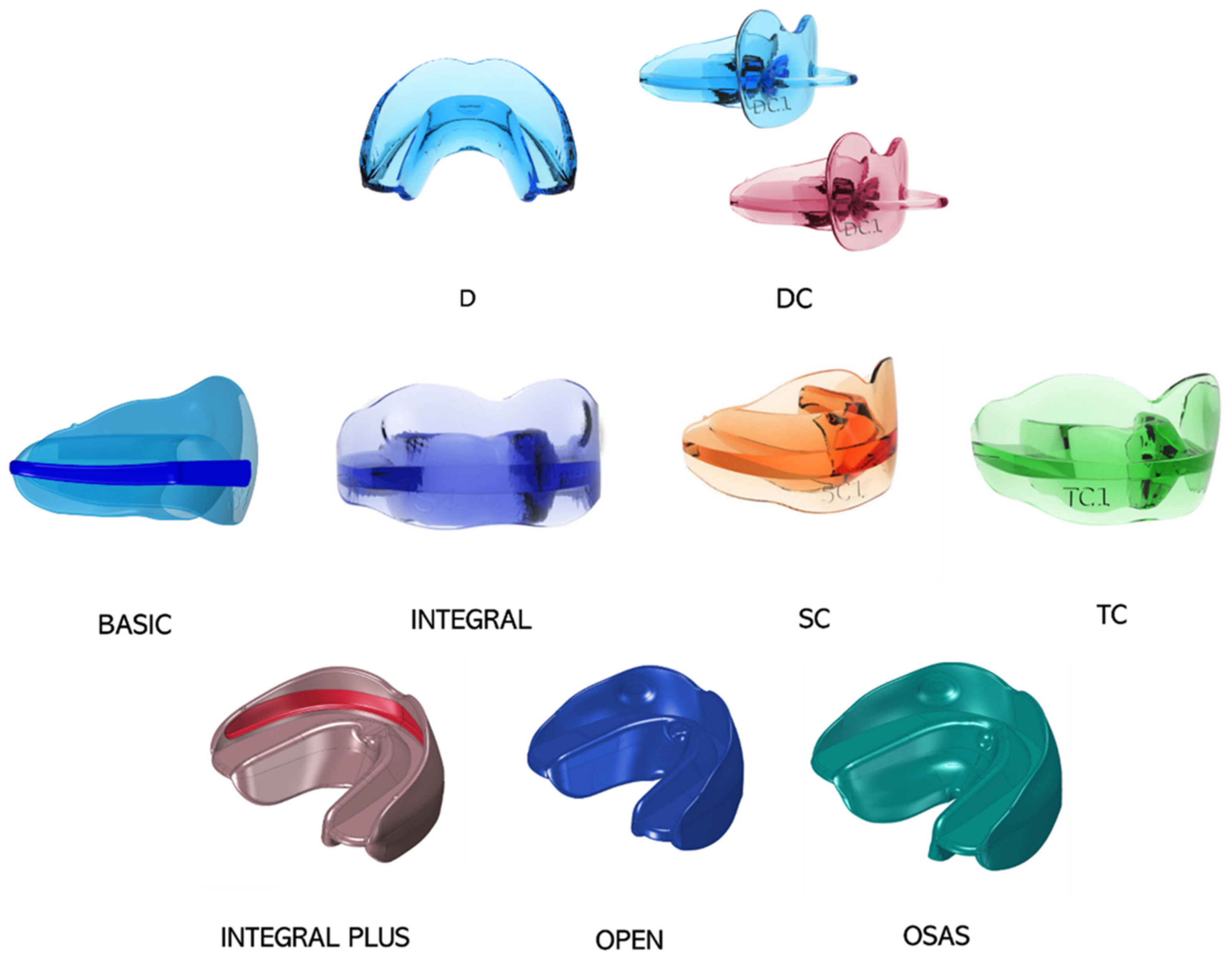
2.1. AMCOP Bio-Activator Devices
2.1.1. Bio-Activator for young children
2.1.2. First Class Bio-Activator
- − S: For mesocephalic cranial index and oval dental arches
- − OS: for mesocephalic cranial index and squared dental arches
- − F: For dolichocephalic cranial index
- − C: For mesocephalic cranial index and squared dental arches
2.1.3. Second Class (SC) Bio-Activator
2.1.4. Third Class (TC) Bio-Activator
2.1.5. Novel Bio-Activators
3. Case Series Presentation
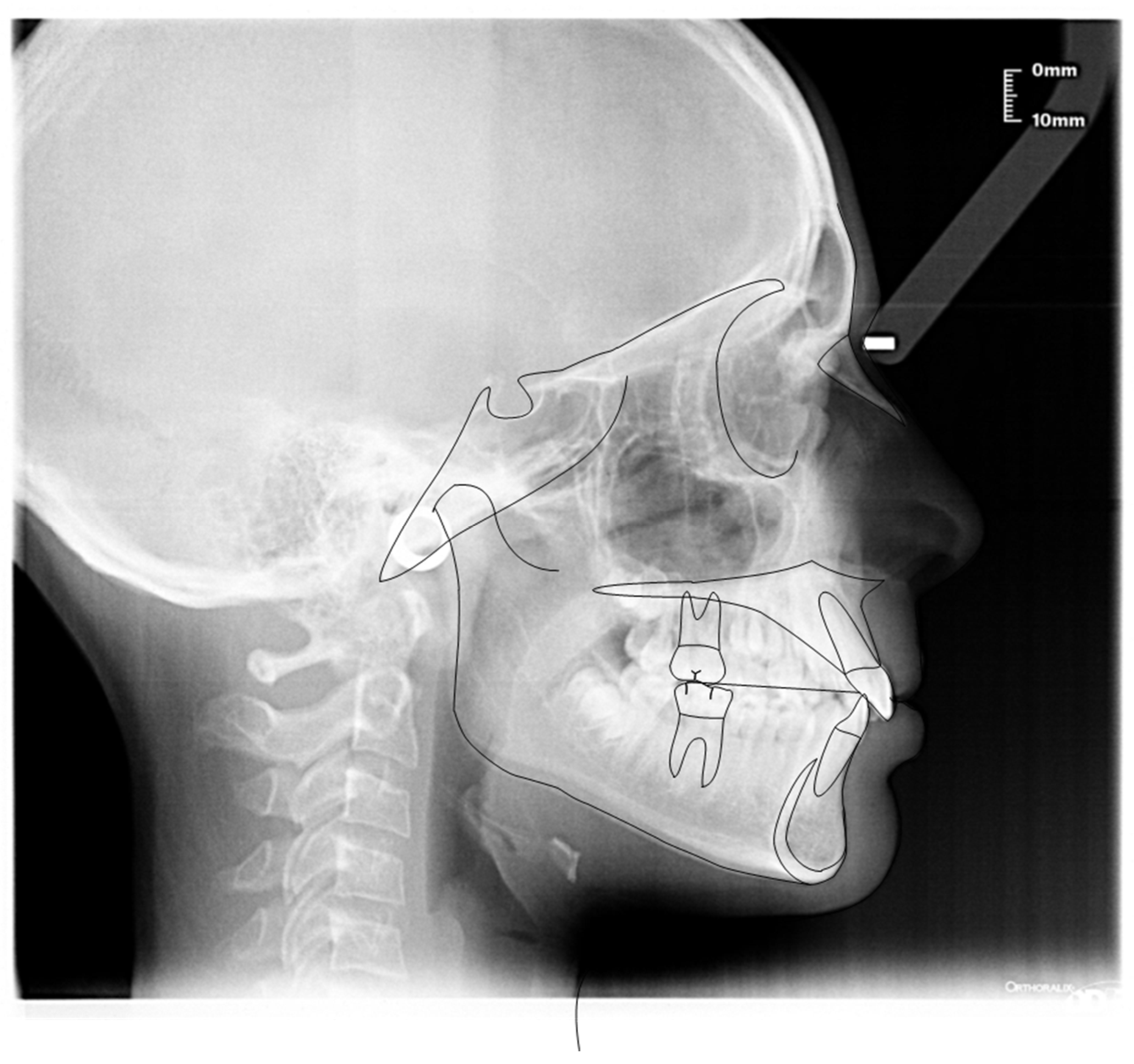
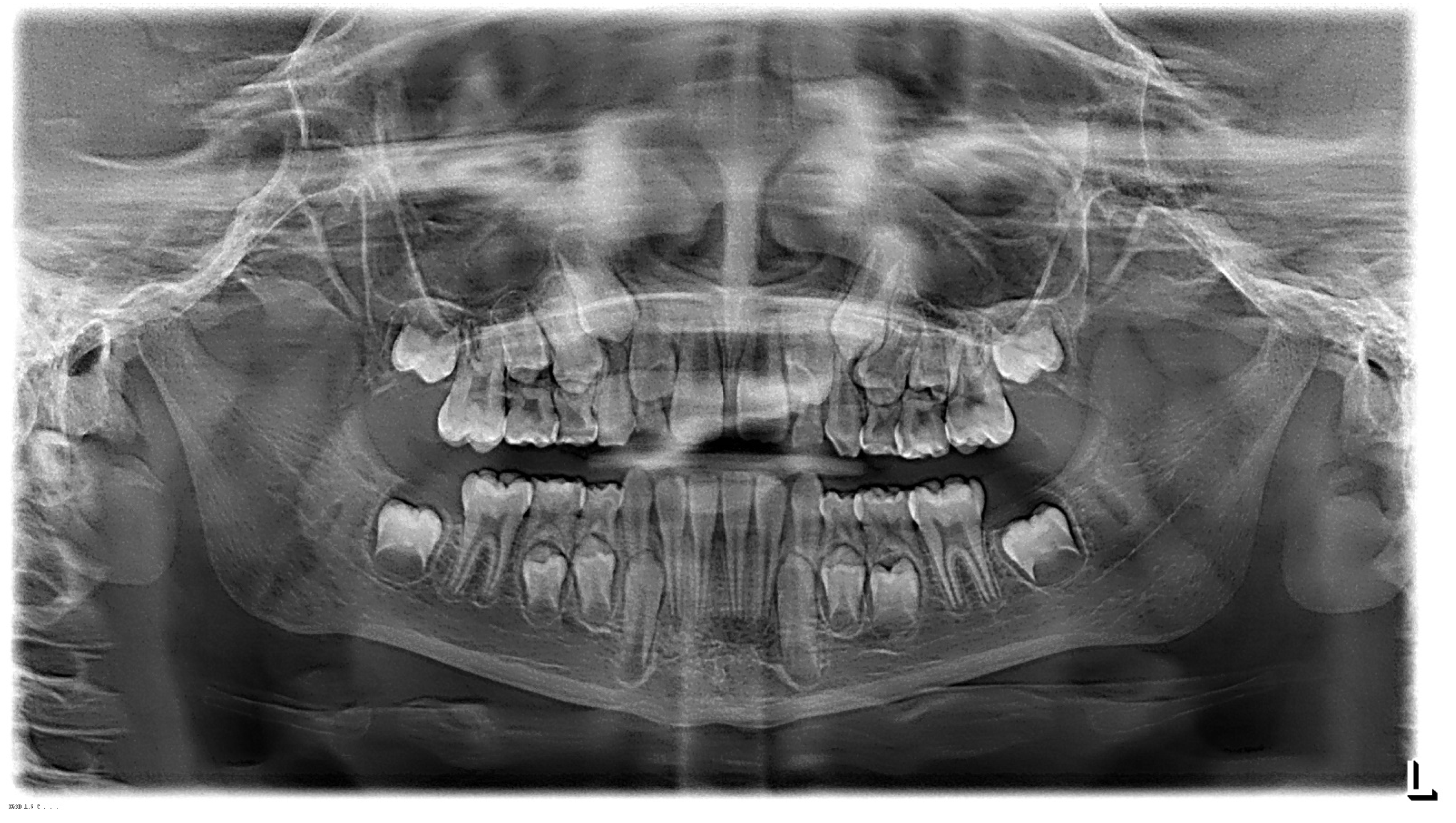
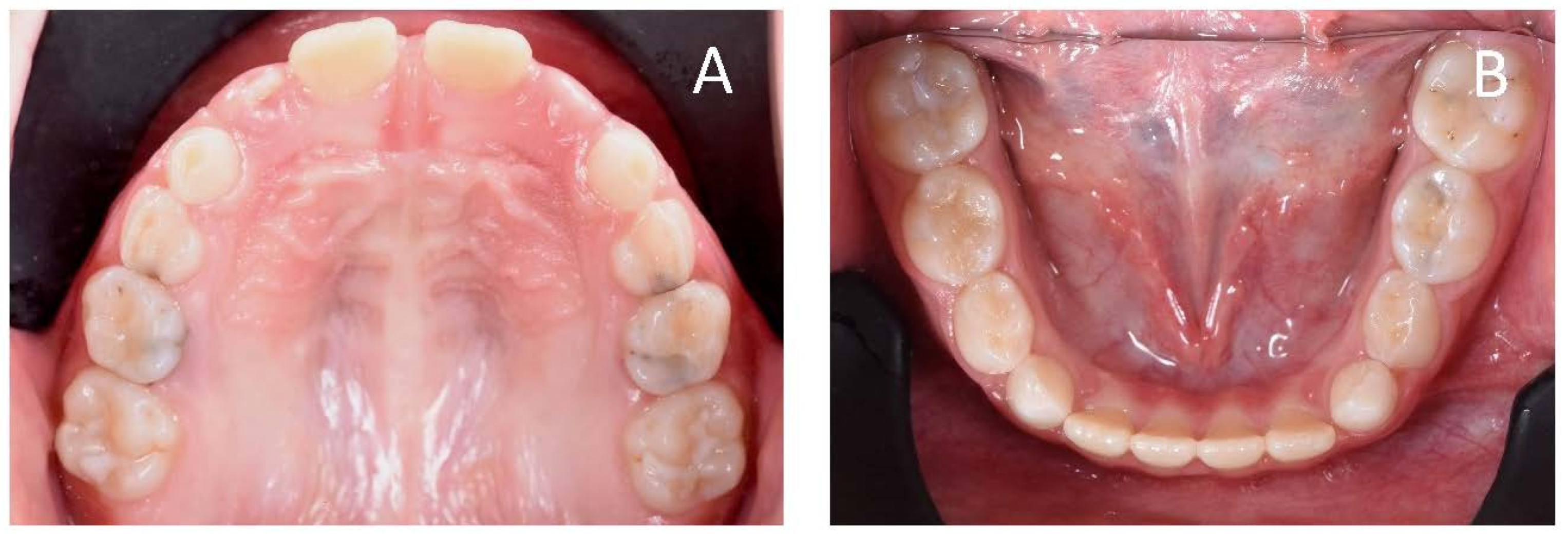
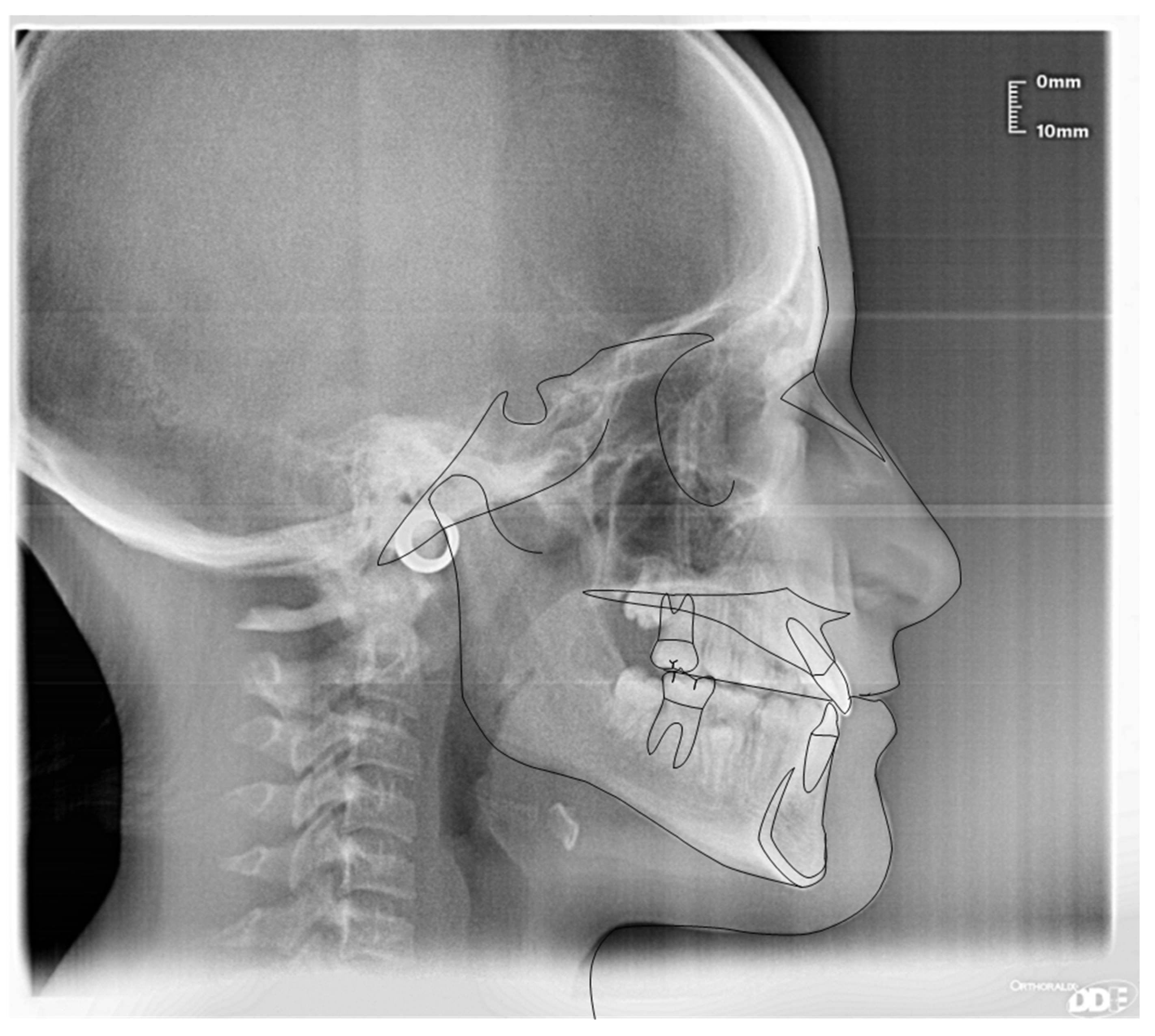
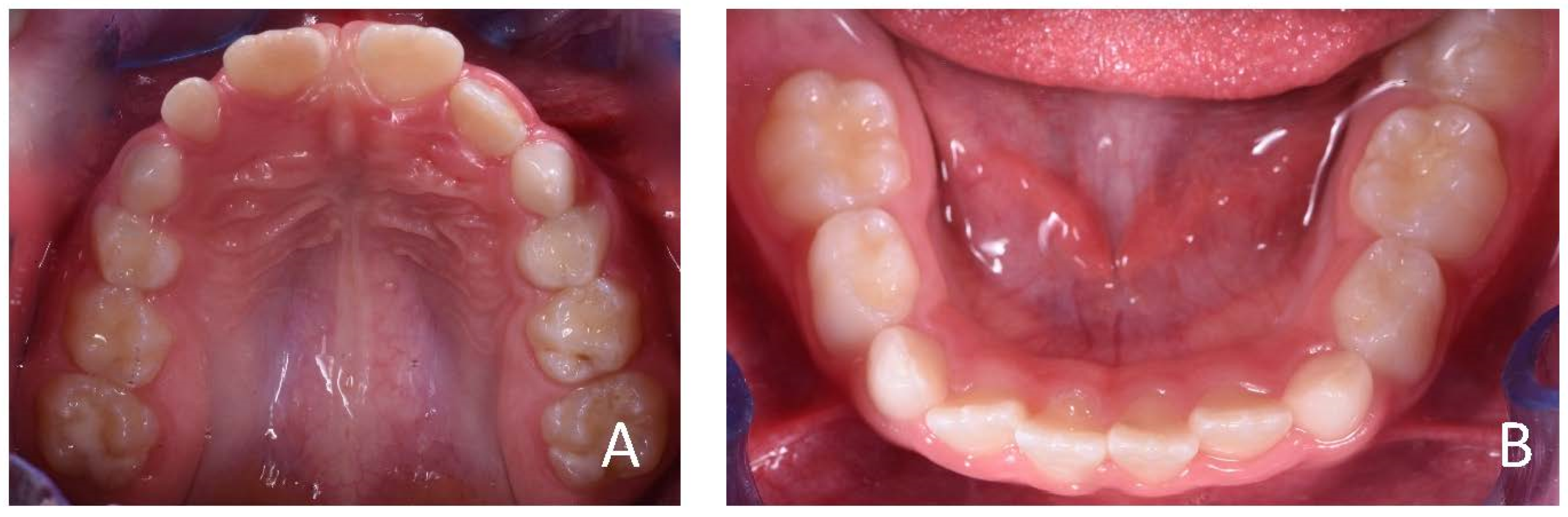
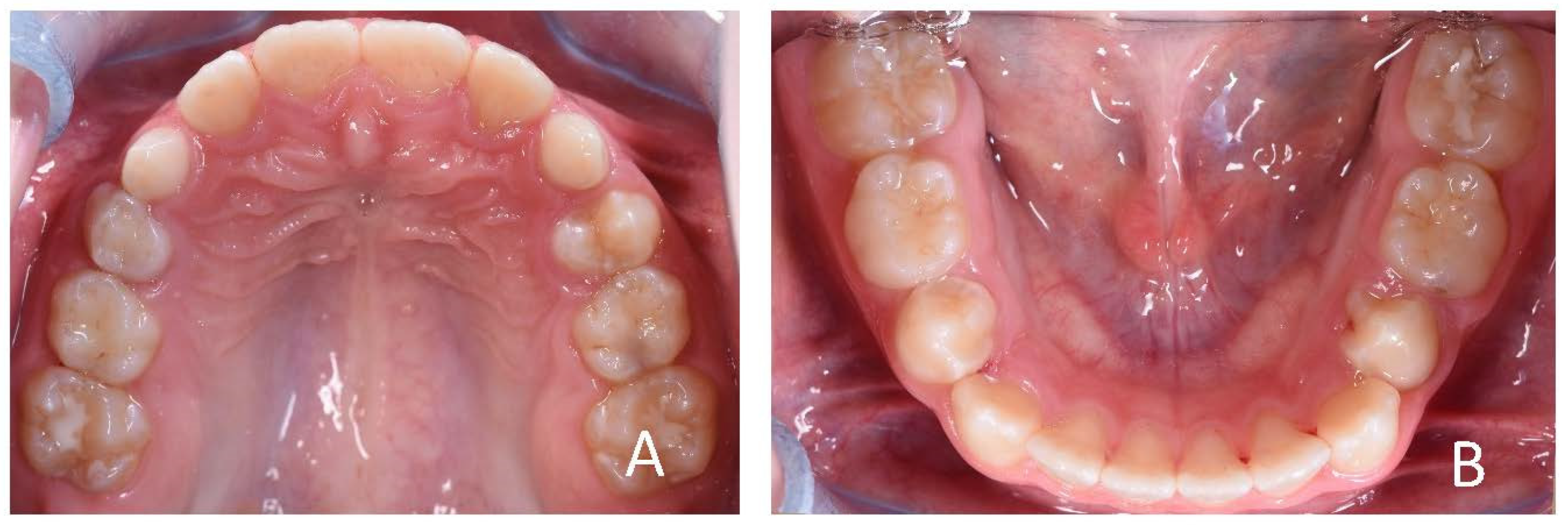
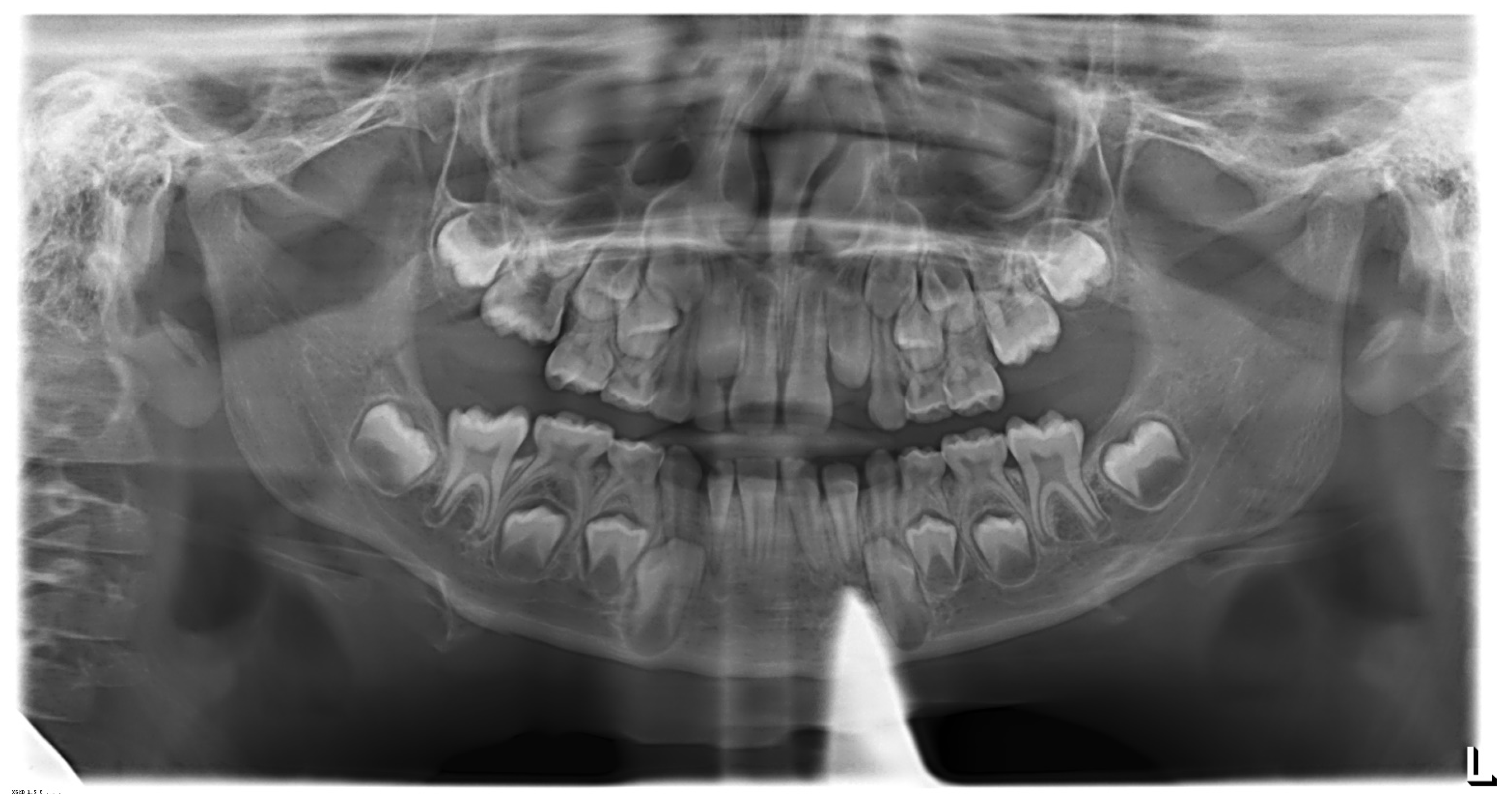
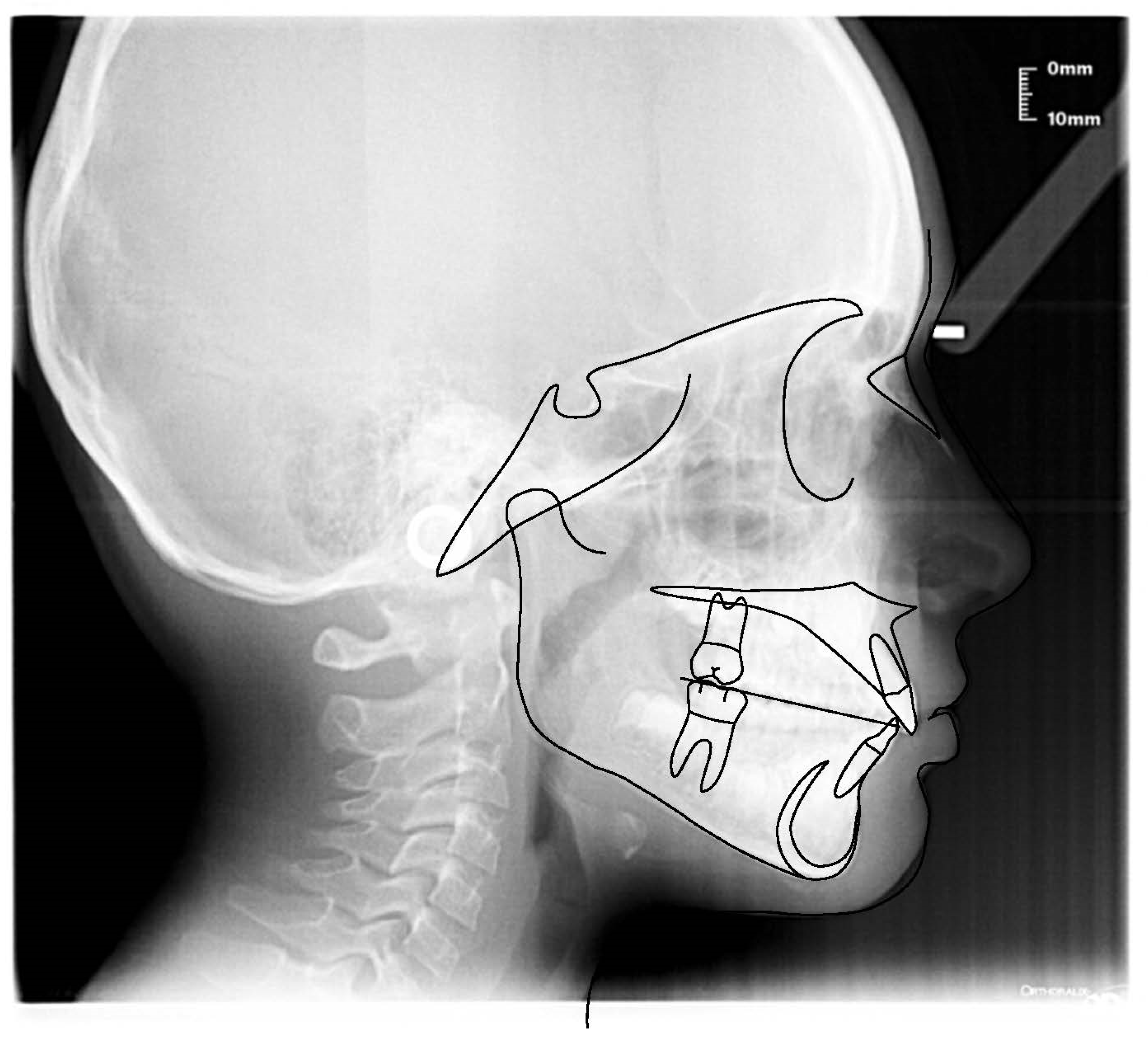
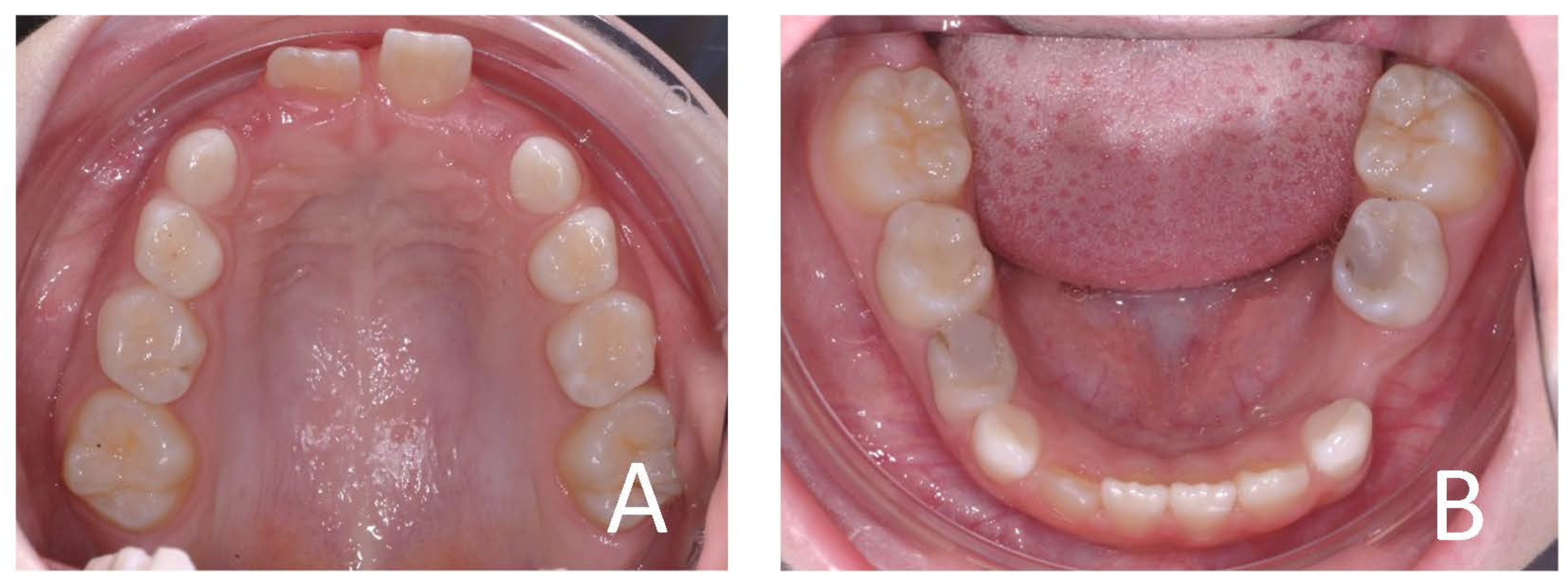
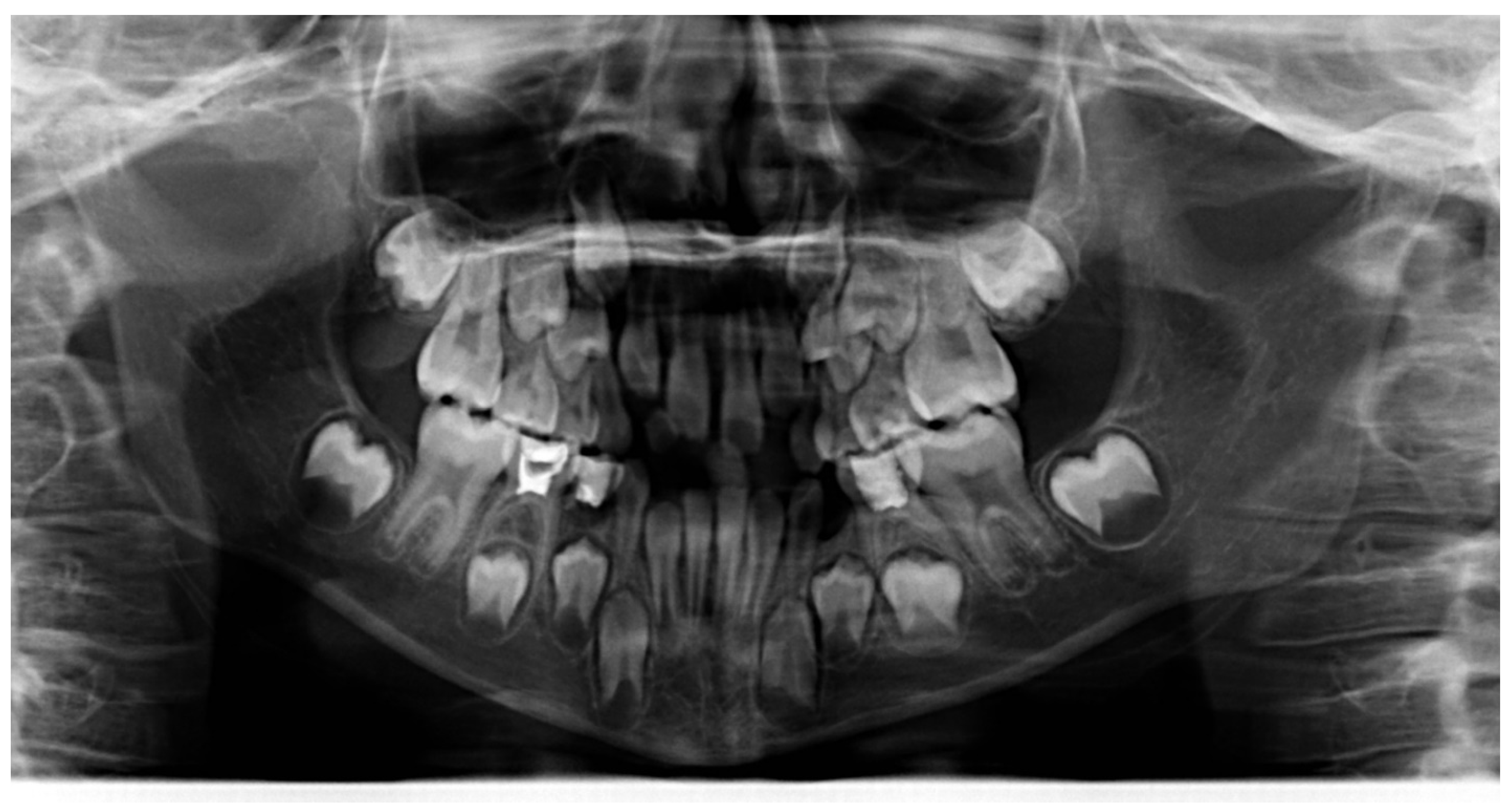
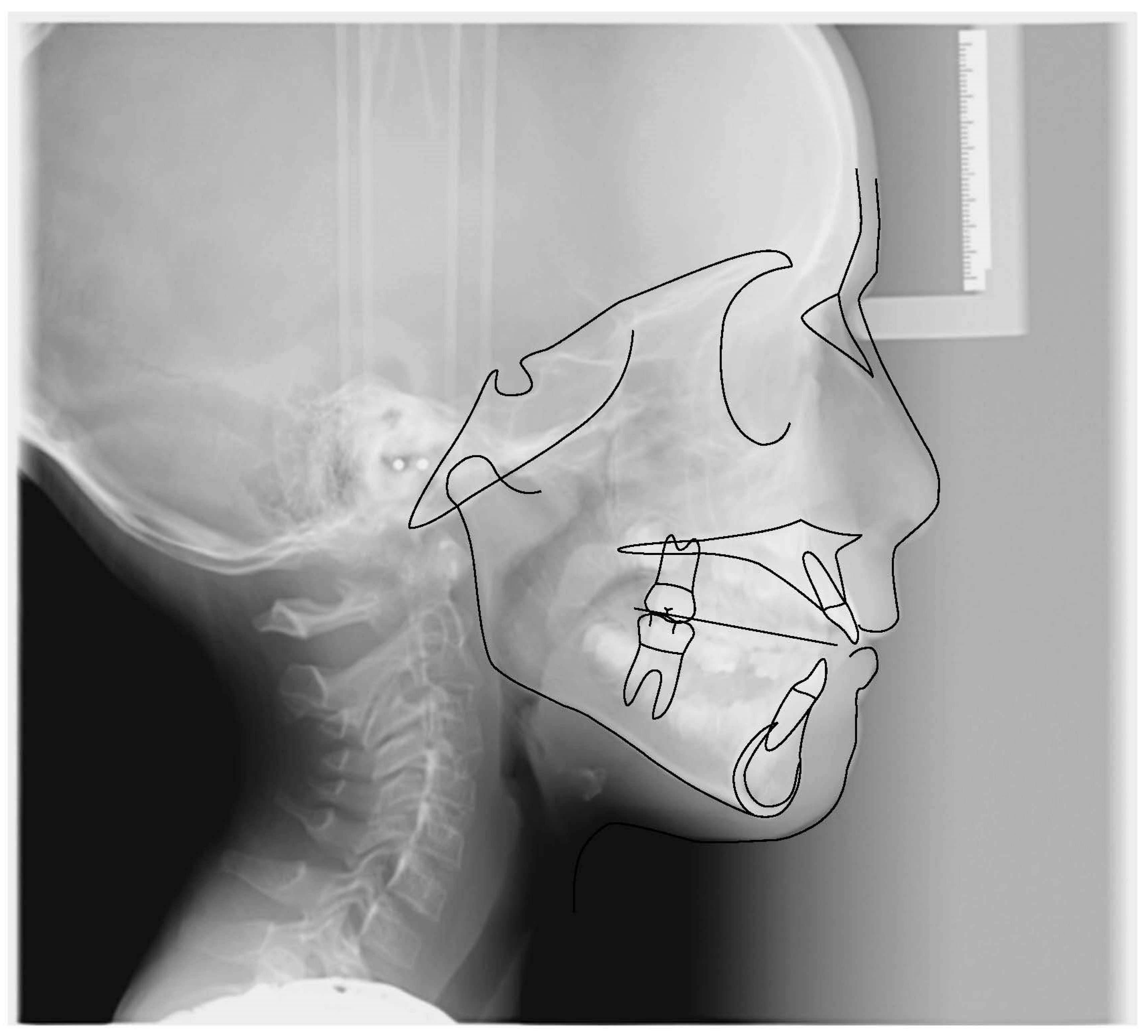
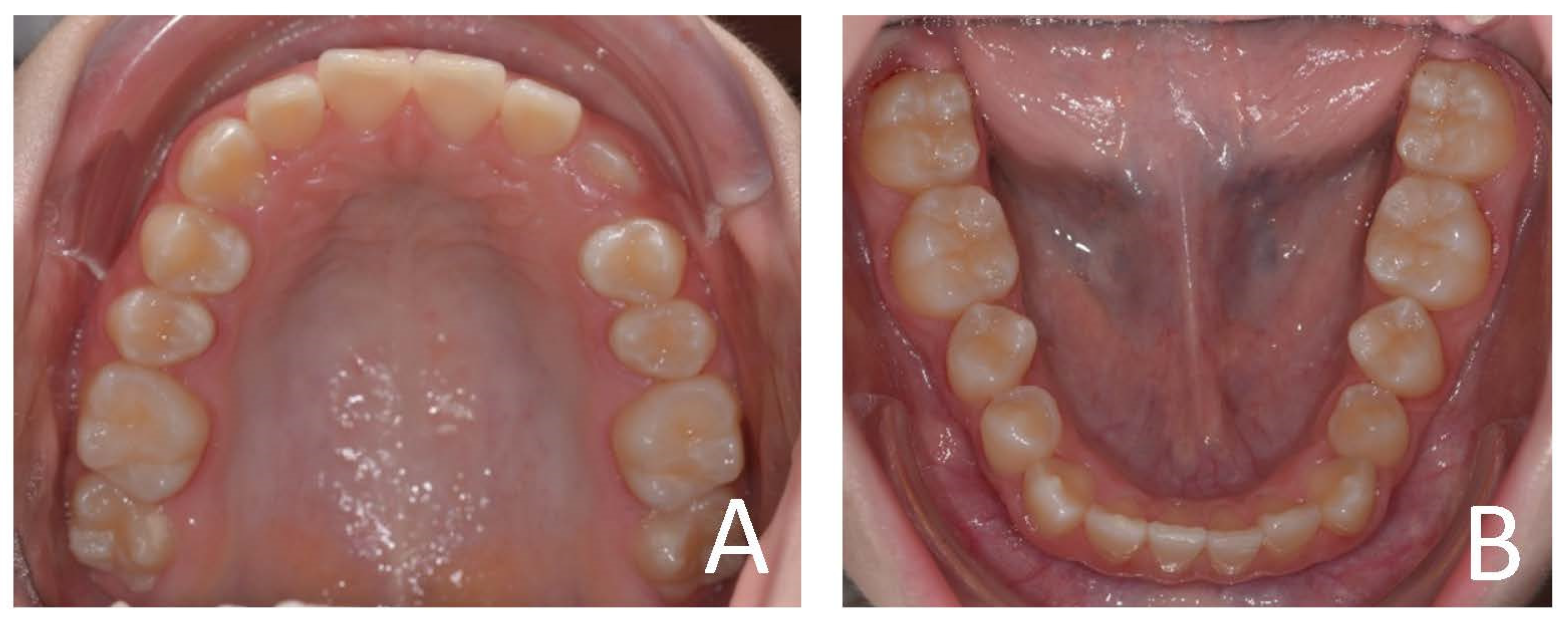
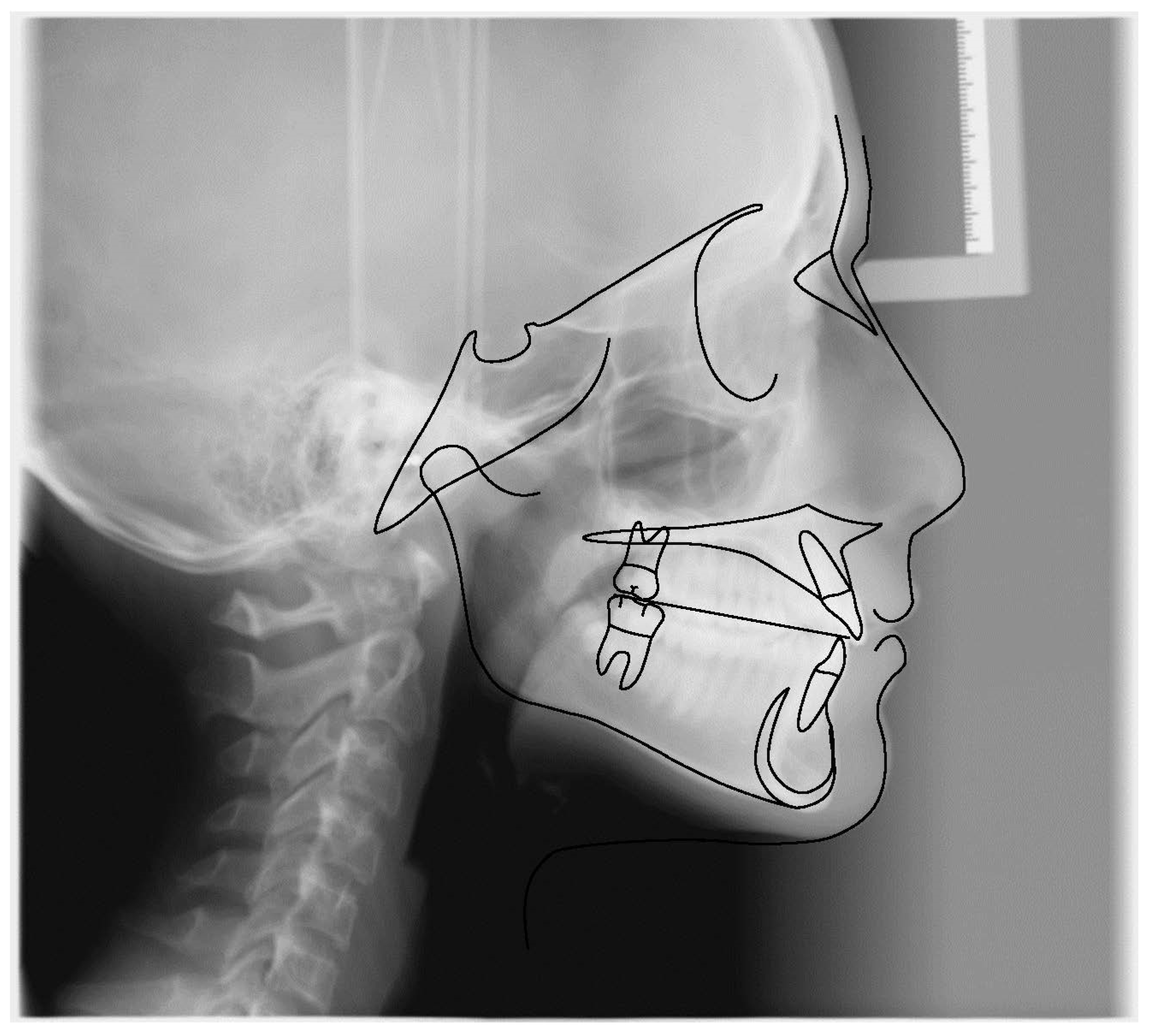
3.1. Clinical Case #1
3.2. Clinical Case #2
3.3. Clinical Case #3
3.4. Clinical Case #4
4. Discussion
4.1. Evolution of Functional Appliances: From Monobloc to Elastodontic Devices
- EF devices designed by Daniel Rollet (Éducation Fonctionnelle, Orthoplus®, Igny, France);
- T4K and POT (Trainer For Kids e Pre-Orthodontic Trainer), actually called Myobrace® (MRC Myofunctional Research, Helensvale, Australia);
- LM-Activator (LM, Parainen, Finland);
- MFS (Multi-Function System) by Duran von Arx (Orthodontic World, Barcelona Spain);
- Muppy® Oral Screen developed by Hintz (DHD, Herne, Germany)
- Occlus-o-Guide®, Nite-Guide®, Class III® and Healthy Start™ (Sweden and Martina)
- AMCOP® (Armonizzatori Multifunzionali Cranio-Occluso-Posturali, Cranio-Occlusion-Postural Multifunctional Harmonizers) by Micerium [37].
4.2. Structural Features of Elastodontic Devices
4.3. Indication of Elastodontic Devices
4.4. Orthopedic-Functional Orthodontic Therapy with Elastomeric Devices
4.5. Preventive Phase
- − Anterior and posterior crossbites;
- − Ankylosis of teeth;
- − Augmented protrusions and diastemas (linked to injury or traumatic avulsions);
- − Anterior and lateral open bites (often in association with bad tongue or digit habits);
- − Ectopic molars;
- − Serious arch length differences;
- − Cleft palate;
- − Pseudo Class III;
- − Class III malocclusion due to maxillary retrusions.
4.6. Interceptive Phase
4.7. Retention Phase
4.8. Comparison between Elastodontic Appliances and Traditional Functional Devices
- Simple patient compliance as they need to be worn fewer hours during the day;
- Less invasiveness;
- Lower costs because it is often unnecessary to adopt more devices during therapy;
- Three-dimensionality;
- No construction bite is needed, so it allows you to avoid the imprint maneuver that is not very tolerated.
- These devices have some limitations regarding:
- Severe skeletal dysmorphisms;
- Rotation of the canines, premolars and molars;
- Impacted elements;
- Severe periodontal disease;
- Mobility of teeth.
4.9. Comparison between Bio-Activators and Other Elastodontic Devices
5. Conclusions
6. Patents
- − Title: dispositivo ortodontico-elastico-armonizzatore dento cranio-facciale, scope: Italian, granted under n° 102015000057082
- − Title: dispositivo ortodontico-elastico-armonizzatore dento cranio-facciale, scope: International, n° WO 2017/056010
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AMCOP | Cranium-Occluded-Postural Multifunctional Harmonizers |
| EGA | Eruption Guidance Appliance |
| EF | Éducation Fonctionnelle |
| T4K | Trainer For Kids |
| POT | Pre-Orthodontic Trainer |
| MRC | Myofunctional Research |
| MFS | Multi-Function System |
| TMJ | Temporo-Mandibular-Joint |
| OSAS | Obstruction Sleep Apnea Syndrome |
| CVM | Cervical Vertebral Maturation |
| CVMS | Cervical Vertebral Maturational Stages |
| EOT | Early Orthodontic Treatment |
| EA | Elastodontic Appliance |
| Co | Condylion |
| Gn | Gnathion |
| Me | Menton |
References
- DiBiase, A.T.; Cobourne, M.T.; Lee, R.T. The Use of Functional Appliances in Contemporary Orthodontic Practice. Br. Dent. J. 2015, 218, 123–128. [Google Scholar] [CrossRef]
- Marinelli, G.; Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Limongelli, L.; Montenegro, V.; Coloccia, G.; Laudadio, C.; Patano, A.; Inchingolo, F.; et al. White Spot Lesions in Orthodontics: Prevention and Treatment. A Descriptive Review. J. Biol. Regul. Homeost. Agents 2021, 35, 227–240. [Google Scholar] [CrossRef]
- Ballini, A.; Cantore, S.; Fotopoulou, E.A.; Georgakopoulos, I.P.; Athanasiou, E.; Bellos, D.; Paduanelli, G.; Saini, R.; Dipalma, G.; Inchingolo, F. Combined Sea Salt-Based Oral Rinse with Xylitol in Orthodontic Patients: Clinical and Microbiological Study. J. Biol. Regul. Homeost. Agents 2019, 33, 263–268. [Google Scholar]
- Adina, S.; Dipalma, G.; Bordea, I.R.; Lucaciu, O.; Feurdean, C.; Inchingolo, A.D.; Septimiu, R.; Malcangi, G.; Cantore, S.; Martin, D.; et al. Orthopedic Joint Stability Influences Growth and Maxillary Development: Clinical Aspects. J. Biol. Regul. Homeost. Agents 2020, 34, 747–756. [Google Scholar] [CrossRef]
- Patianna, A.G.; Ballini, A.; Meneghello, M.; Cantore, S.; Inchingolo, A.M.; Dipalma, G.; Inchingolo, A.D.; Inchingolo, F.; Malcangi, G.; Lucchese, A.; et al. Comparison of Conventional Orthognathic Surgery and “Surgery-First” Protocol: A New Weapon against Time. J. Biol. Regul. Homeost. Agents 2019, 33, 59–67. [Google Scholar] [PubMed]
- Coloccia, G.; Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Montenegro, V.; Patano, A.; Marinelli, G.; Laudadio, C.; Limongelli, L.; Di Venere, D.; et al. Effectiveness of Dental and Maxillary Transverse Changes in Tooth-Borne, Bone-Borne, and Hybrid Palatal Expansion through Cone-Beam Tomography: A Systematic Review of the Literature. Medicina 2021, 57, 288. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Martelli, F.S.; Gargiulo Isacco, C.; Borsani, E.; Cantore, S.; Corcioli, F.; Boddi, A.; Nguyễn, K.C.D.; De Vito, D.; Aityan, S.K.; et al. Chronic Periodontitis and Immunity, Towards the Implementation of a Personalized Medicine: A Translational Research on Gene Single Nucleotide Polymorphisms (SNPs) Linked to Chronic Oral Dysbiosis in 96 Caucasian Patients. Biomedicines 2020, 8, 115. [Google Scholar] [CrossRef] [PubMed]
- Charitos, I.A.; Ballini, A.; Bottalico, L.; Cantore, S.; Passarelli, P.C.; Inchingolo, F.; D’Addona, A.; Santacroce, L. Special Features of SARS-CoV-2 in Daily Practice. WJCC 2020, 8, 3920–3933. [Google Scholar] [CrossRef] [PubMed]
- Alouini, O.; Rollet, D. Modifications Péri-Orales Fonctionnelles et Morphologiques Lors Du Traitement Précoce Des Malocclusions de Classe II Division 1 Avec Des Appareils d’éducation Fonctionnelle de La Gamme EF Line ®. L’Orthod. Française 2018, 89, 289–306. [Google Scholar] [CrossRef] [PubMed]
- Kluemper, G.T.; Beeman, C.S.; Hicks, E.P. Early orthodontic treatment: What are the imperatives? J. Am. Dent. Assoc. 2000, 131, 613–620. [Google Scholar] [CrossRef]
- Fleming, P. Timing Orthodontic Treatment: Early or Late? Aust. Dent. J. 2017, 62, 11–19. [Google Scholar] [CrossRef] [Green Version]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Laudadio, C.; Palmieri, G.; et al. Genetic Pattern, Orthodontic and Surgical Management of Multiple Supplementary Impacted Teeth in a Rare, Cleidocranial Dysplasia Patient: A Case Report. Medicina 2021, 57, 1350. [Google Scholar] [CrossRef]
- Ierardo, G.; Luzzi, V.; Nardacci, G.; Vozza, I.; Polimeni, A. Minimally Invasive Orthodontics: Elastodontic Therapy in a Growing Patient Affected by Dentinogenesis Imperfecta. Ann. Stomatol. 2017, 8, 34. [Google Scholar]
- Fichera, G.; Martina, S.; Palazzo, G.; Musumeci, R.; Leonardi, R.; Isola, G.; Lo Giudice, A. New Materials for Orthodontic Interceptive Treatment in Primary to Late Mixed Dentition. A Retrospective Study Using Elastodontic Devices. Materials 2021, 14, 1695. [Google Scholar] [CrossRef]
- Elastodontic Therapy Un Nuovo Approccio Alla Terapia Ortodontica Funzionale. Available online: https://www.ildentistamoderno.com/elastodontic-therapy-un-nuovo-approccio-alla-terapia-ortodontica-funzionale/ (accessed on 15 October 2021).
- Bishara, S.E.; Ziaja, R.R. Functional Appliances: A Review. Am. J. Orthod. Dentofac. Orthop. 1989, 95, 250–258. [Google Scholar] [CrossRef]
- Proffit, W.R.; Fields, H.W., Jr.; Sarver, D.M. Contemporary Orthodontics; Elsevier Health Sciences: Amsterdam, The Netherlands, 2006. [Google Scholar]
- Vargervik, K.; Harvold, E.P. Response to Activator Treatment in Class II Malocclusions. Am. J. Orthod. 1985, 88, 242–251. [Google Scholar] [CrossRef]
- Wahl, N. Orthodontics in 3 Millennia. Chapter 9: Functional Appliances to Midcentury. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 829–833. [Google Scholar] [CrossRef]
- Ingelsson, M.; Forsberg, C.M. Viggo Andresen–the Originator of Orthodontic Therapy Involving the Use of Oral Activators. Tandlakartidningen 1988, 80, 820–827. [Google Scholar]
- Bimler, H.P. The Bimler Cephalometric Analysis; YASUNAGA Publishing Co.: Wiesbaden, Germany, 1973. [Google Scholar]
- Clark, W.J. The Twin Block Technique A Functional Orthopedic Appliance System. Am. J. Orthod. Dentofac. Orthop. 1988, 93, 1–18. [Google Scholar] [CrossRef]
- Fränkel, R. A Functional Approach to Orofacial Orthopaedics. Br. J. Orthod. 1980, 7, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Bass, N.M. Simplified Bass Appliance. J. Clin. Orthod. 1989, 23, 756–762. [Google Scholar] [PubMed]
- Graber, T.M. The Bionator: Hans L. Eirew Br. J. Orthod. 8: 33–36, 1981. Am. J. Orthod. 1982, 81, 434–435. [Google Scholar]
- Simoes, W.A.; Petrovic, A.; Stutzmann, J. Modus Operandi of Planas’ Appliance. J. Clin. Pediatric Dent. 1992, 16, 79–85. [Google Scholar]
- Albanese, S.; Minervini, G.; Semeraro, G.; Veneziano, R.; Troiano, A.; Rossi, C. Use of functional bite plate (the J.A. Cervera PFB) in the treatment of skeletal and dental open bite. Arch. Stomatol. 1982, 23, 165–180. [Google Scholar]
- Polimeni, A. Pediatric Dentistry; John Wiley & Sons: New York, NY, USA, 2017; ISBN 88-214-5153-4. [Google Scholar]
- Janson, G.R.P.; da Silva, C.C.A.; Bergersen, E.O.; Henriques, J.F.C.; Pinzan, A. Eruption Guidance Appliance Effects in the Treatment of Class II, Division 1 Malocclusions. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 119–129. [Google Scholar] [CrossRef]
- Kesling, C.K. History of Functional Appliances. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 127. [Google Scholar] [CrossRef]
- Besombes, A.; Soulet, R. A New Instrument in Simplified Functional Orthopedic Treatment. Rev. Fr. D’odonto-Stomatol. 1955, 2, 483–490. [Google Scholar]
- Heideborn, M. Clinical and electromyographic results of treatment with the splint-activator of Soulet-Besombes. Fortschr. Kieferorthopadie 1965, 26, 293–299. [Google Scholar] [CrossRef]
- Bergersen, E.O. Preventive Eruption Guidance in the 5-to 7-Year-Old. J. Clin. Orthod. 1995, 29, 382–395. [Google Scholar]
- Bergersen, E.O. Preventive Orthodontics for the 5-to 7-Year-Old with the Nite-Guide Technique. Int. J. Orthod. Milwaukee 2009, 20, 31–35. [Google Scholar]
- Bergersen, E.O. The Eruption Guidance Myofunctional Appliances: How It Works, How to Use It. Funct. Orthod. 1984, 1, 31–35. [Google Scholar]
- Ramirez-Yañez, G.O.; Faria, P. Early Treatment of a Class II, Division 2 Malocclusion with the Trainer for Kids (T4K): A Case Report. J. Clin. Pediatr. Dent. 2008, 32, 325–329. [Google Scholar] [CrossRef]
- Ricciardi, C.; Cagetti, M.G.; Cattaneo, S.; Qing Hu, Y.; Strohmenger, L. Trattamento Ortodontico Intercettivo Con Dispositivi Elastomerici Preformati: Revisione Della Letteratura e Casi Clinici. Dent. Cadmos 2017, 85, 146–155. [Google Scholar] [CrossRef]
- Galluccio, G.; Guarnieri, R.; Jamshir, D.; Impellizzeri, A.; Ierardo, G.; Barbato, E. Comparative Evaluation of Esthetic and Structural Aspects in Class II Functional Therapy. A Case–Control Retrospective Study. IJERPH 2021, 18, 6978. [Google Scholar] [CrossRef]
- Janson, G.; Nakamura, A.; Chiqueto, K.; Castro, R.; de Freitas, M.R.; Henriques, J.F.C. Treatment Stability with the Eruption Guidance Appliance. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 717–728. [Google Scholar] [CrossRef]
- Farronato, G.; Giannini, L.; Galbiati, G.; Grillo, E.; Maspero, C. Occlus-o-Guide®versus Andresen Activator Appliance: Neuromuscular Evaluation. Prog. Orthod. 2013, 14, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grillo, E.; Currò, F.; Salvadori, S.; Viganò, V.M.; Giannini, L.; Farronato, G. Utilizzo di apparecchiature elastodontiche: Caso clinico. Mondo Ortod. 2012, 37, 135–140. [Google Scholar] [CrossRef]
- Ortu, E.; Pietropaoli, D.; Cova, S.; Marci, M.C.; Monaco, A. Efficacy of Elastodontic Devices in Overjet and Overbite Reduction Assessed by Computer-Aid Evaluation. BMC Oral Health 2021, 21, 269. [Google Scholar] [CrossRef]
- Ciavarella, D.; Campobasso, A.; Campa, R.; Suriano, C.; Illuzzi, G.; Cazzolla, A.; Tepedino, M. Cephalometric Effects of the Elastodontic Appliance in Managing Skeletal Class II Di-Vision 1 Cases. Australas. Orthod. J. 2021, 37, 251–258. [Google Scholar] [CrossRef]
- Chen, Y.; Hagg, U.; McGrath, C. Elastodontic Appliance Assisted Fixed Appliance Treatment: A New Two-Phase Protocol for Extraction Cases. J. Orthod. 2019, 46, 251–258. [Google Scholar] [CrossRef]
- Deroze, D.; Lacout, J. Occlusal Finishing, Functional Occlusion, and Elastodontic Concept: How? And Why? A Look at One Case. J. Dentofacial Anom. Orthod. 2011, 14, 208. [Google Scholar] [CrossRef] [Green Version]
- Schmitz, D. Adult Orthodontic and TMJ Retreatment with Elastodontic Appliance. An Early Progress Report. Funct. Orthod. 1990, 7, 35–40. [Google Scholar]
- Balian, A.; Malerba, A.; Strohmenger, L. Obstructive Sleep Apnea Syndrome (OSAS) Treated with Orthodontic Appliances in Children: A New Feasible Approach. Ann Dent. Oral Disord 2018, 1, 105. [Google Scholar]
- Aprile, G.; Ortu, E.; Cattaneo, R.; Pietropaoli, D.; Giannoni, M.; Monaco, A. Orthodontic Management by Functional Activator Treatment: A Case Report. J. Med. Case Rep. 2017, 11, 336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franchi, L.; Nieri, M.; Lomonaco, I.; McNamara, J.A.; Giuntini, V. Predicting the Mandibular Growth Spurt: The roles of chronological age, sex, and the cervical vertebral maturation method. Angle Orthod. 2021, 91, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Mellion, Z.J.; Behrents, R.G.; Johnston, L.E. The Pattern of Facial Skeletal Growth and Its Relationship to Various Common Indexes of Maturation. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 845–854. [Google Scholar] [CrossRef] [PubMed]
- O’Reilly, M.T.; Yanniello, G.J. Mandibular Growth Changes and Maturation of Cervical Vertebrae--a Longitudinal Cephalometric Study. Angle Orthod. 1988, 58, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Baccetti, T.; Franchi, L.; McNamara, J.A. An Improved Version of the Cervical Vertebral Maturation (CVM) Method for the Assessment of Mandibular Growth. Angle Orthod. 2002, 72, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Galui, S.; Pal, S. Early Orthodontic Treatment Need among 6-9-Year-Old Children of West Bengal. J. Oral Res. Rev. 2021, 13, 12. [Google Scholar] [CrossRef]
- Ackerman, J.L.; Proffit, W.R. Preventive and Interceptive Orthodontics: A Strong Theory Proves Weak in Practice. Angle Orthod. 1980, 50, 75–87. [Google Scholar] [CrossRef]
- Moss, M.L.; Salentijn, L. The Primary Role of Functional Matrices in Facial Growth. Am. J. Orthod. 1969, 55, 566–577. [Google Scholar] [CrossRef]
- White, L. Early Orthodontic Intervention. Am. J. Orthod. Dentofac. Orthop. 1998, 113, 24–28. [Google Scholar] [CrossRef]
- Keski-Nisula, K.; Keski-Nisula, L.; Salo, H.; Voipio, K.; Varrela, J. Dentofacial Changes after Orthodontic Intervention with Eruption Guidance Appliance in the Early Mixed Dentition. Angle Orthod. 2008, 78, 324–331. [Google Scholar] [CrossRef]
- O’Brien, K.; Wright, J.; Conboy, F.; Sanjie, Y.; Mandall, N.; Chadwick, S.; Connolly, I.; Cook, P.; Birnie, D.; Hammond, M.; et al. Effectiveness of Early Orthodontic Treatment with the Twin-Block Appliance: A Multicenter, Randomized, Controlled Trial. Part 1: Dental and Skeletal Effects. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 234–243. [Google Scholar] [CrossRef]
- Anastasi, G.; Putrino, A. Cephalometric Evaluation of Mandibular Changes Following Orthodontic Treatment with Preformed Appliances on Class II Patients: A Meta-Analysis. Open Access Biomed. Publ. Using Post Publ. Peer Rev. 2014, 5, WMC004491. [Google Scholar]
- Condò, R.; Perugia, C.; Bartolino, M.; Docimo, R. Analysis of Clinical Efficacy of Interceptive Treatment of Class II Division 2 Malocclusion in a Pair of Twins through the Use of Two Modified Removable Appliances. Oral Implantol. 2010, 3, 11. [Google Scholar]
- Baccetti, T.; Franchi, L.; Toth, L.R.; McNamara, J.A. Treatment Timing for Twin-Block Therapy. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 159–170. [Google Scholar] [CrossRef] [Green Version]
- Ramirez-Yañez, G.; Sidlauskas, A.; Junior, E.; Fluter, J. Dimensional Changes in Dental Arches After Treatment with a Prefabricated Functional Appliance. J. Clin. Pediatric Dent. 2007, 31, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Denotti, M.L.P. L’ Ortodonzia e i Suoi Dispositivi–Apparecchi Mobili e Fissi Rimovibili Nella Pratica Clinica; Elsevier: Amsterdam, The Netherlands, 2007; ISBN 8821429628. [Google Scholar]
- Arreghini, A.; Trigila, S.; Lombardo, L.; Siciliani, G. Objective Assessment of Compliance with Intra- and Extraoral Removable Appliances. Angle Orthod. 2017, 87, 88–95. [Google Scholar] [CrossRef]
- O’Brien, K.; Wright, J.; Conboy, F.; Sanjie, Y.; Mandall, N.; Chadwick, S.; Connolly, I.; Cook, P.; Birnie, D.; Hammond, M.; et al. Effectiveness of Treatment for Class II Malocclusion with the Herbst or Twin-Block Appliances: A Randomized, Controlled Trial. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 128–137. [Google Scholar] [CrossRef]
- Yassir, Y.A.; McIntyre, G.T.; Bearn, D.R. The Impact of Labial Fixed Appliance Orthodontic Treatment on Patient Expectation, Experience, and Satisfaction: An Overview of Systematic Reviews. Eur. J. Orthod. 2020, 42, 223–230. [Google Scholar] [CrossRef]
- Bordea, I.; Sîrbu, A.; Lucaciu, O.; Ilea, A.; Câmpian, R.; Todea, D.; Alexescu, T.; Aluaș, M.; Budin, C.; Pop, A. Microleakage—The Main Culprit in Bracket Bond Failure? JMMS 2019, 6, 86–94. [Google Scholar] [CrossRef] [Green Version]
- Sirbu, A.; Bordea, R.; Lucaciu, O.; Braitoru, C.; Szuhanek, C.; Campian, R.S. 3D Printed Splints an Innovative Method to Treat Temporomandibular Joint Pathology. Rev. Chim. 2018, 69, 3087–3090. [Google Scholar] [CrossRef]
- Patano, A.; Cirulli, N.; Beretta, M.; Plantamura, P.; Inchingolo, A.D.; Inchingolo, A.M.; Bordea, I.R.; Malcangi, G.; Marinelli, G.; Scarano, A.; et al. Education Technology in Orthodontics and Paediatric Dentistry during the Covid-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6056. [Google Scholar] [CrossRef]
- Stavridi, R.; Ahlgren, J. Muscle Response to the Oral-Screen Activator. An EMG Study of the Masseter, Buccinator, and Mentalis Muscles. Eur. J. Orthod. 1992, 14, 339–349. [Google Scholar] [CrossRef]
- Yagci, A.; Uysal, T.; Kara, S.; Okkesim, S. The Effects of Myofunctional Appliance Treatment on the Perioral and Masticatory Muscles in Class II, Division 1 Patients. World J. Orthod. 2010, 11, 117–122. [Google Scholar]
- Tallgren, A.; Christiansen, R.L.; Ash, M.M., Jr.; Miller, R.L. Effects of a Myofunctional Appliance on Orofacial Muscle Activity and Structures. Angle Orthod. 1998, 68, 249–258. [Google Scholar] [PubMed]
- McNamara, J.A.; Howe, R.P.; Dischinger, T.G. A Comparison of the Herbst and Fränkel Appliances in the Treatment of Class II Malocclusion. Am. J. Orthod. Dentofac. Orthop. 1990, 98, 134–144. [Google Scholar] [CrossRef]
- Toth, L.R.; McNamara, J.A. Treatment Effects Produced by the Twin-Block Appliance and the FR-2 Appliance of Fränkel Compared with an Untreated Class II Sample. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 597–609. [Google Scholar] [CrossRef]
- Janson, G.; de Souza, J.E.P.; de Freitas, M.R.; Henriques, J.F.C.; Cavalcanti, C.T. Occlusal Changes of Class II Malocclusion Treatment between Fränkel and the Eruption Guidance Appliances. Angle Orthod. 2004, 74, 521–525. [Google Scholar] [CrossRef] [PubMed]
- Janson, G.R.; Pereira, A.C.; Bergersen, E.O.; Henriques, J.F.; Pinzan, A.; de Almeida, R.R. Cephalometric Evaluation of the Eruption Guidance Appliance in Class II, Division 1 Treatment. J. Clin. Orthod. 1997, 31, 299–306. [Google Scholar] [PubMed]
- Staderini, E.; Patini, R.; Camodeca, A.; Guglielmi, F.; Gallenzi, P. Three-Dimensional Assessment of Morphological Changes Following Nasoalveolar Molding Therapy in Cleft Lip and Palate Patients: A Case Report. Dent. J. 2019, 7, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janson, G.; Nakamura, A.; de Freitas, M.R.; Henriques, J.F.C.; Pinzan, A. Apical Root Resorption Comparison between Fränkel and Eruption Guidance Appliances. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 729–735. [Google Scholar] [CrossRef] [PubMed]
- Migliaccio, S.; Aprile, V.; Zicari, S.; Grenci, A. Eruption Guidance Appliance: A Review. Eur. J. Paediatr. Dent. 2014, 15, 163–166. [Google Scholar]
- Cardarelli, D.F. Il Trattamento Funzionale Elastodontico Con Apparecchi AMCOP: Funzione, Estetica e Postura. Dent. Trib. Ital. Ed. 2019, 23–25. [Google Scholar]
- Vanini, L.; Cardarelli, F.; D’arcangelo, C. Elastodonzia: La Bioortodonzia Con Funzione Posturale. Teamwork Clin. 2021, 60–76. [Google Scholar]
- Patini, R.; Staderini, E.; Camodeca, A.; Guglielmi, F.; Gallenzi, P. Case Reports in Pediatric Dentistry Journals: A Systematic Review about Their Effect on Impact Factor and Future Investigations. Dent. J. 2019, 7, 103. [Google Scholar] [CrossRef] [Green Version]
- Cardarelli, F.; Cardarelli, A. Il Laser in Elastodonzia. Doctor OS 2021, 20–23. [Google Scholar]























| Cephalometric Analysis before Treatment | Val | Dev | Min | Med | Max | Diff |
|---|---|---|---|---|---|---|
| SNA | 82° | N | 80° | 82° | 84° | 0° |
| SNB | 78.6° | N | 78° | 80° | 82° | 0° |
| ANB | 3.4° | N | 0° | 2° | 4° | 0° |
| sna-snp^Go-Gn | 22.3° | N | 15° | 20° | 25° | 0° |
| S-N^sna-snp | 8.9° | N | 7° | 10° | 13° | 0° |
| S-N^PO | 14.2° | N | 11° | 14° | 17° | 0° |
| S-N^Go-Gn | 31.2° | N | 27° | 32° | 37° | 0° |
| SNBa | 136.6° | x | 124° | 129° | 134° | 2.6° |
| SND | 75.1° | N | 74° | 76° | 78° | 0° |
| IS^II | 128.9° | N | 125° | 130° | 135° | 0° |
| IS:N-A | 3.5 | N | 3 | 4 | 5 | 0 |
| II:N-B | 3.7 | N | 3 | 4 | 5 | 0 |
| II:A-Pog | 1.7 | N | −1 | 1 | 3 | 0 |
| Ls:Line S | −2.1 | −xx | −1 | 0 | 1 | 1.1 |
| Li: Line S | 0.4 | N | −1 | 0 | 1 | 0 |
| Cvm:S-Gn | −3.4 | −xxx | −1 | 0 | 1 | 2.4 |
| Mol Sup^P. Occl | 99.5° | xxxx | 88° | 90° | 92° | 7.5° |
| N-S-Cop | 135.2° | xx | 117° | 122° | 127° | 8.2° |
| S-Cop-Go | 137.3° | N | 137° | 143° | 149° | 0° |
| Cop-Go-Gn | 118.7° | N | 115° | 120° | 125° | 0° |
| Cop-Go-N | 51.2° | N | 48° | 50° | 52° | 0° |
| N-Go-Gn | 67.6° | −x | 68° | 70° | 72° | 0.4° |
| II^Go-Gn | 94.1° | x | 92° | 93° | 94° | 0.1° |
| SOr:sna | 62.9 | 0 | 0 | 0 | 62.9 | |
| sna:Me | 63.7 | 0 | 0 | 0 | 63.7 | |
| S:N | 69.6 | −xx | 75 | 78 | 81 | 5.4 |
| snp:A | 54.7 | 0 | 0 | 0 | 54.7 | |
| Go:Me | 75.4 | N | 73.7 | 78.7 | 83.7 | 0 |
| Wits | 1.5 | N | −2 | 0 | 2 | 0 |
| IS^N-S | 105.9° | x | 101° | 103° | 105° | 0.9° |
| Pog:N-B | 0.9 | 0 | 0 | 0 | 0.9 | |
| Pog:N-B—II:N-B | −2.8 | - | 0 | 0 | 0 | 2.8 |
| Cephalometric Analysis after Treatment | Val | Dev | Min | Med | Max | Diff |
|---|---|---|---|---|---|---|
| SNA | 81.8° | N | 80° | 82° | 84° | 0° |
| SNB | 78.9° | N | 78° | 80° | 82° | 0° |
| ANB | 2.9° | N | 0° | 2° | 4° | 0° |
| sna-snp^Go-Gn | 22.4° | N | 15° | 20° | 25° | 0° |
| S-N^sna-snp | 9.1° | N | 7° | 10° | 13° | 0° |
| S-N^PO | 12.4° | N | 11° | 14° | 17° | 0° |
| S-N^Go-Gn | 31.5° | N | 27° | 32° | 37° | 0° |
| SNBa | 139.7° | xx | 124° | 129° | 134° | 5.7° |
| SND | 76.1° | N | 74° | 76° | 78° | 0° |
| IS^II | 125.1° | N | 125° | 130° | 135° | 0° |
| IS:N-A | 3.8 | N | 3 | 4 | 5 | 0 |
| II:N-B | 4.4 | N | 3 | 4 | 5 | 0 |
| II:A-Pog | 2.2 | N | −1 | 1 | 3 | 0 |
| Ls:Line S | −3 | −xxx | −1 | 0 | 1 | 2 |
| Li: Line S | 1.2 | x | −1 | 0 | 1 | 0.2 |
| Cvm:S-Gn | −4.7 | −xxxx | −1 | 0 | 1 | 3.7 |
| Mol Sup^P. Occl | 95.2° | xx | 88° | 90° | 92° | 3.2° |
| N-S-Cop | 132.3° | xx | 117° | 122° | 127° | 5.3° |
| S-Cop-Go | 143.9° | N | 137° | 143° | 149° | 0° |
| Cop-Go-Gn | 115.3° | N | 115° | 120° | 125° | 0° |
| Cop-Go-N | 49.4° | N | 48° | 50° | 52° | 0° |
| N-Go-Gn | 66° | −xx | 68° | 70° | 72° | 2° |
| II^Go-Gn | 93.4° | N | 92° | 93° | 94° | 0° |
| SOr:sna | 72.3 | 0 | 0 | 0 | 72.3 | |
| sna:Me | 67.3 | 0 | 0 | 0 | 67.3 | |
| S:N | 72.9 | −x | 75 | 78 | 81 | 2.1 |
| snp:A | 56.1 | 0 | 0 | 0 | 56.1 | |
| Go:Me | 86.4 | x | 73.7 | 78.7 | 83.7 | 2.7 |
| Wits | 2 | N | −2 | 0 | 2 | 0 |
| IS^N-S | 109.9° | xxx | 101° | 103° | 105° | 4.9° |
| Pog:N-B | 1.5 | 0 | 0 | 0 | 1.5 | |
| Pog:N-B—II:N-B | −2.9 | - | 0 | 0 | 0 | 2.9 |
| Cephalometric Analysis before Treatment | Val | Dev | Min | Med | Max | Diff |
|---|---|---|---|---|---|---|
| SNA | 82.4° | N | 80° | 82° | 84° | 0° |
| SNB | 83.2° | x | 78° | 80° | 82° | 1.2° |
| ANB | −0.8° | −x | 0° | 2° | 4° | 0.8° |
| sna-snp^Go-Gn | 22.4° | N | 15° | 20° | 25° | 0° |
| S-N^sna-snp | 7.6° | N | 7° | 10° | 13° | 0° |
| S-N^PO | 20.4° | xx | 11° | 14° | 17° | 3.4° |
| S-N^Go-Gn | 30° | N | 27° | 32° | 37° | 0° |
| SNBa | 134.5° | x | 124° | 129° | 134° | 0.5° |
| SND | 78.8° | x | 74° | 76° | 78° | 0.8° |
| IS^II | 142.5° | xx | 125° | 130° | 135° | 7.5° |
| IS:N-A | 2.2 | −x | 3 | 4 | 5 | 0.8 |
| II:N-B | 3.2 | N | 3 | 4 | 5 | 0 |
| II:A-Pog | 2.9 | N | −1 | 1 | 3 | 0 |
| Ls:Line S | −1.6 | −x | −1 | 0 | 1 | 0.6 |
| Li: Line S | −1.4 | −x | −1 | 0 | 1 | 0.4 |
| Cvm:S-Gn | 1 | N | −1 | 0 | 1 | 0 |
| Mol Sup^P. Occl | 106° | xxx | 88° | 90° | 92° | 14° |
| N-S-Cop | 134.1° | xx | 117° | 122° | 127° | 7.1° |
| S-Cop-Go | 132.8° | −x | 137° | 143° | 149° | 4.2° |
| Cop-Go-Gn | 123.1° | N | 115° | 120° | 125° | 0° |
| Cop-Go-N | 53.7° | x | 48° | 50° | 52° | 1.7° |
| N-Go-Gn | 69.3° | N | 68° | 70° | 72° | 0° |
| II^Go-Gn | 84.1° | −xxx | 92° | 93° | 94° | 7.9° |
| SOr:sna | 45 | 0 | 0 | 0 | 45 | |
| sna:Me | 51.2 | 0 | 0 | 0 | 51.2 | |
| S:N | 53.7 | −xxxxxx | 68.7 | 71.7 | 74.7 | 15 |
| snp:A | 40 | 0 | 0 | 0 | 40 | |
| Go:Me | 63.4 | −x | 66.7 | 71.7 | 76.7 | 3.3 |
| Wits | −8.5 | −xxxx | −2 | 0 | 2 | 6.5 |
| IS^N-S | 103.4° | x | 101° | 103° | 105° | 0° |
| Pog:N-B | 1.1 | 0 | 0 | 0 | 1.1 | |
| Pog:N-B—II:N-B | −2.1 | - | 0 | 0 | 0 | 2.1 |
| Cephalometric Analysis after Treatment | Val | Dev | Min | Med | Max | Diff |
|---|---|---|---|---|---|---|
| SNA | 84.6° | x | 80° | 82° | 84° | 0.6° |
| SNB | 84.2° | xx | 78° | 80° | 82° | 2.2° |
| ANB | 0.4° | N | 0° | 2° | 4° | 0° |
| sna-snp^Go-Gn | 20.1° | N | 15° | 20° | 25° | 0° |
| S-N^sna-snp | 11.6° | N | 7° | 10° | 13° | 0° |
| S-N^PO | 17.3° | x | 11° | 14° | 17° | 0.3° |
| S-N^Go-Gn | 31.7° | N | 27° | 32° | 37° | 0° |
| SNBa | 140.3° | xx | 124° | 129° | 134° | 6.3° |
| SND | 80.9° | xx | 74° | 76° | 78° | 2.9° |
| IS^II | 135.3° | x | 125° | 130° | 135° | 0.3° |
| IS:N-A | 2.7 | −x | 3 | 4 | 5 | 0.3 |
| II:N-B | 3.5 | N | 3 | 4 | 5 | 0 |
| II:A-Pog | 3.2 | x | −1 | 1 | 3 | 0.2 |
| Ls:Line S | −3.9 | −xxx | −1 | 0 | 1 | 2.9 |
| Li: Line S | −4.4 | −xxxx | −1 | 0 | 1 | 3.4 |
| Cvm:S-Gn | −3.6 | −xxx | −1 | 0 | 1 | 2.6 |
| Mol Sup^P. Occl | 108° | xxx | 88° | 90° | 92° | 16° |
| N-S-Cop | 137° | xxx | 117° | 122° | 127° | 10° |
| S-Cop-Go | 128.7° | −xx | 137° | 143° | 149° | 8.3° |
| Cop-Go-Gn | 126.1° | x | 115° | 120° | 125° | 1.1° |
| Cop-Go-N | 54.4° | xx | 48° | 50° | 52° | 2.4° |
| N-Go-Gn | 71.6° | N | 68° | 70° | 72° | 0° |
| II^Go-Gn | 79° | −xxx | 92° | 93° | 94° | 13° |
| SOr:sna | 63.3 | 0 | 0 | 0 | 63.3 | |
| sna:Me | 57.5 | 0 | 0 | 0 | 57.5 | |
| S:N | 59.4 | −xxxx | 68.7 | 71.7 | 74.7 | 9.3 |
| snp:A | 49.7 | 0 | 0 | 0 | 49.7 | |
| Go:Me | 74.6 | N | 66.7 | 71.7 | 76.7 | 0 |
| Wits | −7.8 | −xxx | −2 | 0 | 2 | 5.8 |
| IS^N-S | 113.9° | xxxxx | 101° | 103° | 105° | 8.9° |
| Pog:N-B | 0.3 | 0 | 0 | 0 | 0.3 | |
| Pog:N-B—II:N-B | −3.2 | - | 0 | 0 | 0 | 3.2 |
| Cephalometric Analysis before Treatment | Val | Dev | Min | Med | Max | Diff |
|---|---|---|---|---|---|---|
| SNA | 82.4° | N | 80° | 82° | 84° | 0° |
| SNB | 74.7° | −xx | 78° | 80° | 82° | 3.3° |
| ANB | 7.7° | xx | 0° | 2° | 4° | 3.7° |
| sna-snp^Go-Gn | 23.2° | N | 15° | 20° | 25° | 0° |
| S-N^sna-snp | 10.6° | N | 7° | 10° | 13° | 0° |
| S-N^PO | 20.6° | xx | 11° | 14° | 17° | 3.6° |
| S-N^Go-Gn | 33.7° | N | 27° | 32° | 37° | 0° |
| SNBa | 127.1° | N | 124° | 129° | 134° | 0° |
| SND | 71.1° | −xx | 74° | 76° | 78° | 2.9° |
| IS^II | 103° | −xxxxx | 125° | 130° | 135° | 22° |
| IS:N-A | 2.9 | −x | 3 | 4 | 5 | 0.1 |
| II:N-B | 4.8 | N | 3 | 4 | 5 | 0 |
| II:A-Pog | 0.8 | N | −1 | 1 | 3 | 0 |
| Ls:Line S | 2.6 | xx | −1 | 0 | 1 | 1.6 |
| Li:Line S | 0.6 | N | −1 | 0 | 1 | 0 |
| Cvm:S-Gn | −3.3 | −xxx | −1 | 0 | 1 | 2.3 |
| Mol Sup^P. Occl | 109° | xxx | 88° | 90° | 92° | 17° |
| N-S-Cop | 118.3° | N | 117° | 122° | 127° | 0° |
| S-Cop-Go | 156.4° | xx | 137° | 143° | 149° | 7.4° |
| Cop-Go-Gn | 119° | N | 115° | 120° | 125° | 0° |
| Cop-Go-N | 48.5° | N | 48° | 50° | 52° | 0° |
| N-Go-Gn | 70.5° | N | 68° | 70° | 72° | 0° |
| II^Go-Gn | 104.1° | xxx | 92° | 93° | 94° | 10.1° |
| SOr:sna | 57.5 | 0 | 0 | 0 | 57.5 | |
| sna:Me | 54.1 | 0 | 0 | 0 | 54.1 | |
| S:N | 63.2 | −xxx | 71 | 74 | 77 | 7.8 |
| snp:A | 44.4 | 0 | 0 | 0 | 44.4 | |
| Go:Me | 59 | −xxx | 69.3 | 74.3 | 79.3 | 10.3 |
| Wits | 4.2 | xx | −2 | 0 | 2 | 2.2 |
| IS^N-S | 119.1° | xxx | 101° | 103° | 105° | 14.1° |
| Pog:N-B | 1.6 | 0 | 0 | 0 | 1.6 | |
| Pog:N-B—II:N-B | −3.2 | - | 0 | 0 | 0 | 3.2 |
| Cephalometric Analysis after Treatment | Val | Dev | Min | Med | Max | Diff |
|---|---|---|---|---|---|---|
| SNA | 79.5° | −x | 80° | 82° | 84° | 0.5° |
| SNB | 76.4° | −x | 78° | 80° | 82° | 1.6° |
| ANB | 3.2° | N | 0° | 2° | 4° | 0° |
| sna-snp^Go-Gn | 23.3° | N | 15° | 20° | 25° | 0° |
| S-N^sna-snp | 11.4° | N | 7° | 10° | 13° | 0° |
| S-N^PO | 20.1° | xx | 11° | 14° | 17° | 3.1° |
| S-N^Go-Gn | 34.7° | N | 27° | 32° | 37° | 0° |
| SNBa | 136.4° | x | 124° | 129° | 134° | 2.4° |
| SND | 72.1° | −x | 74° | 76° | 78° | 1.9° |
| IS^II | 122° | −x | 125° | 130° | 135° | 3° |
| IS:N-A | 4 | N | 3 | 4 | 5 | 0 |
| II:N-B | 3.5 | N | 3 | 4 | 5 | 0 |
| II:A-Pog | 2.1 | N | −1 | 1 | 3 | 0 |
| Ls:Line S | −2 | −xx | −1 | 0 | 1 | 1 |
| Li:Line S | 0 | N | −1 | 0 | 1 | 0 |
| Cvm:S-Gn | −0.1 | N | −1 | 0 | 1 | 0 |
| Mol Sup^P. Occl | 95.8° | xx | 88° | 90° | 92° | 3.8° |
| N-S-Cop | 129.4° | x | 117° | 122° | 127° | 2.4° |
| S-Cop-Go | 141.5° | N | 137° | 143° | 149° | 0° |
| Cop-Go-Gn | 123.8° | N | 115° | 120° | 125° | 0° |
| Cop-Go-N | 52.5° | x | 48° | 50° | 52° | 0.5° |
| N-Go-Gn | 71.3° | N | 68° | 70° | 72° | 0° |
| II^Go-Gn | 99.9° | xxxxxx | 92° | 93° | 94° | 5.9° |
| SOr:sna | 57.1 | 0 | 0 | 0 | 57.1 | |
| sna:Me | 56.3 | 0 | 0 | 0 | 56.3 | |
| S:N | 62.9 | −xxx | 71 | 74 | 77 | 8.1 |
| snp:A | 46.7 | 0 | 0 | 0 | 46.7 | |
| Go:Me | 61 | −xx | 69.3 | 74.3 | 79.3 | 8.3 |
| Wits | −0.8 | N | −2 | 0 | 2 | 0 |
| IS^N-S | 103.4° | N | 101° | 103° | 105° | 0° |
| Pog:N-B | 0.4 | 0 | 0 | 0 | 0.4 | |
| Pog:N-B—II:N-B | −3.1 | - | 0 | 0 | 0 | 3.1 |
| Cephalometric Analysis before Treatment | Val | Dev | Min | Med | Max | Diff |
|---|---|---|---|---|---|---|
| SNA | 74.5° | −xxx | 80° | 82° | 84° | 5.5° |
| SNB | 70.3° | −xxxx | 78° | 80° | 82° | 7.7° |
| ANB | 4.2° | x | 0° | 2° | 4° | 0.2° |
| sna-snp^Go-Gn | 30.7° | xx | 15° | 20° | 25° | 5.7° |
| S-N^sna-snp | 11.4° | N | 7° | 10° | 13° | 0° |
| S-N^PO | 25.2° | xxx | 11° | 14° | 17° | 8.2° |
| S-N^Go-Gn | 42.1° | xx | 27° | 32° | 37° | 5.1° |
| SNBa | 140.5° | xx | 124° | 129° | 134° | 6.5° |
| SND | 66.4° | −xxxx | 74° | 76° | 78° | 7.6° |
| IS^II | 120.3° | −x | 125° | 130° | 135° | 4.7° |
| IS:N-A | 1.9 | −xx | 3 | 4 | 5 | 1.1 |
| II:N-B | 2.2 | −x | 3 | 4 | 5 | 0.8 |
| II:A-Pog | 0.8 | N | −1 | 1 | 3 | 0 |
| Ls:Line S | 0.9 | N | −1 | 0 | 1 | 0 |
| Li:Line S | −0.8 | N | −1 | 0 | 1 | 0 |
| Cvm:S-Gn | −3.3 | −xxx | −1 | 0 | 1 | 2.3 |
| Mol Sup^P. Occl | 89.4° | N | 88° | 90° | 92° | 0° |
| N-S-Cop | 135.2° | xx | 117° | 122° | 127° | 8.2° |
| S-Cop-Go | 135° | −x | 137° | 143° | 149° | 2° |
| Cop-Go-Gn | 131.9° | xx | 115° | 120° | 125° | 6.9° |
| Cop-Go-N | 57.7° | xxx | 48° | 50° | 52° | 5.7° |
| N-Go-Gn | 74.2° | xx | 68° | 70° | 72° | 2.2° |
| II^Go-Gn | 94.3° | x | 92° | 93° | 94° | 0.3° |
| SOr:sna | 52.9 | 0 | 0 | 0 | 52.9 | |
| sna:Me | 57.3 | 0 | 0 | 0 | 57.3 | |
| S:N | 63.7 | −x | 66.6 | 69.6 | 72.6 | 2.9 |
| snp:A | 41.6 | 0 | 0 | 0 | 41.6 | |
| Go:Me | 57.7 | −xx | 66 | 71 | 76 | 8.3 |
| Wits | 0.1 | N | −2 | 0 | 2 | 0 |
| IS^N-S | 103.4° | N | 101° | 103° | 105° | 0° |
| Pog:N-B | 0.2 | 0 | 0 | 0 | 0.2 | |
| Pog:N-B—II:N-B | −2 | - | 0 | 0 | 0 | 2 |
| Cephalometric Analysis after Treatment | Val | Dev | Min | Med | Max | Diff |
|---|---|---|---|---|---|---|
| SNA | 76.6° | −xx | 80° | 82° | 84° | 3.4° |
| SNB | 74.1° | −xx | 78° | 80° | 82° | 3.9° |
| ANB | 2.5° | N | 0° | 2° | 4° | 0° |
| sna-snp^Go-Gn | 23.3° | N | 15° | 20° | 25° | 0° |
| S-N^sna-snp | 12.7° | N | 7° | 10° | 13° | 0° |
| S-N^PO | 25.7° | xxx | 11° | 14° | 17° | 8.7° |
| S-N^Go-Gn | 36.1° | N | 27° | 32° | 37° | 0° |
| SNBa | 138.2° | x | 124° | 129° | 134° | 4.2° |
| SND | 71.2° | −xx | 74° | 76° | 78° | 2.8° |
| IS^II | 130.3° | N | 125° | 130° | 135° | 0° |
| IS:N-A | 1.6 | −xx | 3 | 4 | 5 | 1.4 |
| II:N-B | 2.3 | −x | 3 | 4 | 5 | 0.7 |
| II:A-Pog | 0.4 | N | −1 | 1 | 3 | 0 |
| Ls:Line S | −2 | −xx | −1 | 0 | 1 | 1 |
| Li:Line S | −1.8 | −x | −1 | 0 | 1 | 0.8 |
| Cvm:S-Gn | 4.4 | xxxx | −1 | 0 | 1 | 3.4 |
| Mol Sup^P. Occl | 92.1° | x | 88° | 90° | 92° | 0.1° |
| N-S-Cop | 133.1° | xx | 117° | 122° | 127° | 6.1° |
| S-Cop-Go | 133.6° | −x | 137° | 143° | 149° | 3.4° |
| Cop-Go-Gn | 129.4° | x | 115° | 120° | 125° | 4.4° |
| Cop-Go-N | 57.4° | xxx | 48° | 50° | 52° | 5.4° |
| N-Go-Gn | 71.9° | N | 68° | 70° | 72° | 0° |
| II^Go-Gn | 92.1° | N | 92° | 93° | 94° | 0° |
| SOr:sna | 64.3 | 0 | 0 | 0 | 64.3 | |
| sna:Me | 56.5 | 0 | 0 | 0 | 56.5 | |
| S:N | 65.6 | −x | 67.3 | 70.3 | 73.3 | 1.7 |
| snp:A | 49.3 | 0 | 0 | 0 | 49.3 | |
| Go:Me | 63.6 | −x | 66 | 71 | 76 | 2.4 |
| Wits | −2.7 | −x | −2 | 0 | 2 | 0.7 |
| IS^N-S | 101.6° | N | 101° | 103° | 105° | 0° |
| Pog:N-B | 1.5 | 0 | 0 | 0 | 1.5 | |
| Pog:N-B—II:N-B | −0.8 | - | 0 | 0 | 0 | 0.8 |
| Passive Activators Myofunctional Activators Biodynamic Activators | Active Activators Biodynamic Activators | |
|---|---|---|
| Rigid: | Bimaxillary: | - Bass |
| - Bionator | - Bassani appliance | - Lehman |
| - Andresen-Haulp | - Ducovator | - Teuscher |
| Elastic: | Double plates: | |
| - Bimler | -Twin Block | |
| - Frankel | - Planas | |
| - Cervera | - Kinetor | |
| - Elastodontic appliances | - Sanders | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Laudadio, C.; Pede, C.D.; et al. The Efficacy of a New AMCOP® Elastodontic Protocol for Orthodontic Interceptive Treatment: A Case Series and Literature Overview. Int. J. Environ. Res. Public Health 2022, 19, 988. https://doi.org/10.3390/ijerph19020988
Inchingolo AD, Patano A, Coloccia G, Ceci S, Inchingolo AM, Marinelli G, Malcangi G, Montenegro V, Laudadio C, Pede CD, et al. The Efficacy of a New AMCOP® Elastodontic Protocol for Orthodontic Interceptive Treatment: A Case Series and Literature Overview. International Journal of Environmental Research and Public Health. 2022; 19(2):988. https://doi.org/10.3390/ijerph19020988
Chicago/Turabian StyleInchingolo, Alessio Danilo, Assunta Patano, Giovanni Coloccia, Sabino Ceci, Angelo Michele Inchingolo, Grazia Marinelli, Giuseppina Malcangi, Valentina Montenegro, Claudia Laudadio, Chiara Di Pede, and et al. 2022. "The Efficacy of a New AMCOP® Elastodontic Protocol for Orthodontic Interceptive Treatment: A Case Series and Literature Overview" International Journal of Environmental Research and Public Health 19, no. 2: 988. https://doi.org/10.3390/ijerph19020988













