A Review on Aging, Sarcopenia, Falls, and Resistance Training in Community-Dwelling Older Adults
Abstract
:1. Introduction
1.1. Aging and Sarcopenia
1.2. Correlates of Sarcopenia: Falls and Fall-Related Injuries
1.3. Resistance Training, Sarcopenia, and Falls
2. Resistance Training: Intensity and Volume
2.1. Strength Training Using Resistance Machines
2.2. Strength Training Using Bodyweight and Low-Cost Materials
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations. World Population Ageing 2019 (ST/ESA/SER. A/444); United Nations, Department of Economic and Social Affairs, Population Division: New York, NY, USA, 2020. [Google Scholar]
- World Health Organization. Ageing and Health Report. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 19 September 2021).
- European Comission. The 2018 Ageing Report: Economic and Budgetary Projections for the EU Member States (2016–2070); European Comission: Geneva, Switzerland, 2018. [Google Scholar]
- Landi, F.; Liperoti, R.; Russo, A.; Capoluongo, E.D.; Barillaro, C.; Pahor, M.; Bernabei, R.; Onder, G. Disability, more than multimorbidity, was predictive of mortality among older persons aged 80 years and older. J. Clin. Epidemiol. 2010, 63, 752–759. [Google Scholar] [CrossRef]
- Ruiz, J.R.; Sui, X.; Lobelo, F.; Morrow, J.R.; Jackson, A.W.; Sjöström, M.; Blair, S.N. Association between muscular strength and mortality in men: Prospective cohort study. BMJ 2008, 337, a439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merchant, R.A.; Morley, J.E.; Izquierdo, M. Exercise, Aging and Frailty: Guidelines for Increasing Function. J. Nutr. Health Aging 2021, 25, 405–409. [Google Scholar] [CrossRef] [PubMed]
- Benavent-Caballer, V.; Rosado-Calatayud, P.; Segura-Ortí, E.; Amer-Cuenca, J.; Lisón, J. Effects of three different low-intensity exercise interventions on physical performance, muscle CSA and activities of daily living: A randomized controlled trial. Exp. Gerontol. 2014, 58, 159–165. [Google Scholar] [CrossRef]
- Bishop, N.A.; Lu, T.; Yankner, B.A. Neural mechanisms of ageing and cognitive decline. Nature 2010, 464, 529–535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cadore, E.L.; Casas-Herrero, A.; Zambom-Ferraresi, F.; Idoate, F.; Millor, N.; Gómez, M.; Rodríguez-Mañas, L.; Izquierdo, M. Multicomponent exercises including muscle power training enhance muscle mass, power output, and functional outcomes in institutionalized frail nonagenarians. AGE 2014, 36, 773–785. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2017; pp. 1–24. [Google Scholar]
- Freiberger, E.; Menz, H.; Abu-Omar, K.; Rütten, A. Preventing Falls in Physically Active Community-Dwelling Older People: A Comparison of Two Intervention Techniques. Gerontology 2007, 53, 298–305. [Google Scholar] [CrossRef] [Green Version]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [Green Version]
- Doherty, T.J. Invited Review: Aging and sarcopenia. J. Appl. Physiol. 2003, 95, 1717–1727. [Google Scholar] [CrossRef] [Green Version]
- Phu, S.; Boersma, D.; Duque, G. Exercise and Sarcopenia. J. Clin. Densitom. 2015, 18, 488–492. [Google Scholar] [CrossRef]
- Beurskens, R.; Gollhofer, A.; Muehlbauer, T.; Cardinale, M.; Granacher, U. Effects of Heavy-Resistance Strength and Balance Training on Unilateral and Bilateral Leg Strength Performance in Old Adults. PLoS ONE 2015, 10, e0118535. [Google Scholar] [CrossRef]
- Liguori, G.; American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2020. [Google Scholar]
- Montero-Fernandez, N.; Serra-Rexach, J.A. Role of exercise on sarcopenia in the elderly. Eur. J. Phys. Rehabil. Med. 2013, 49, 131–143. [Google Scholar] [PubMed]
- Larsson, L.; Degens, H.; Li, M.; Salviati, L.; Lee, Y.I.; Thompson, W.; Kirkland, J.L.; Sandri, M. Sarcopenia: Aging-Related Loss of Muscle Mass and Function. Physiol. Rev. 2019, 99, 427–511. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.-P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [Green Version]
- Pahor, M.; Manini, T.; Cesari, M. Sarcopenia: Clinical evaluation, biological markers and other evaluation tools. J. Nutr. Health Aging 2009, 13, 724–728. [Google Scholar] [CrossRef] [PubMed] [Green Version]
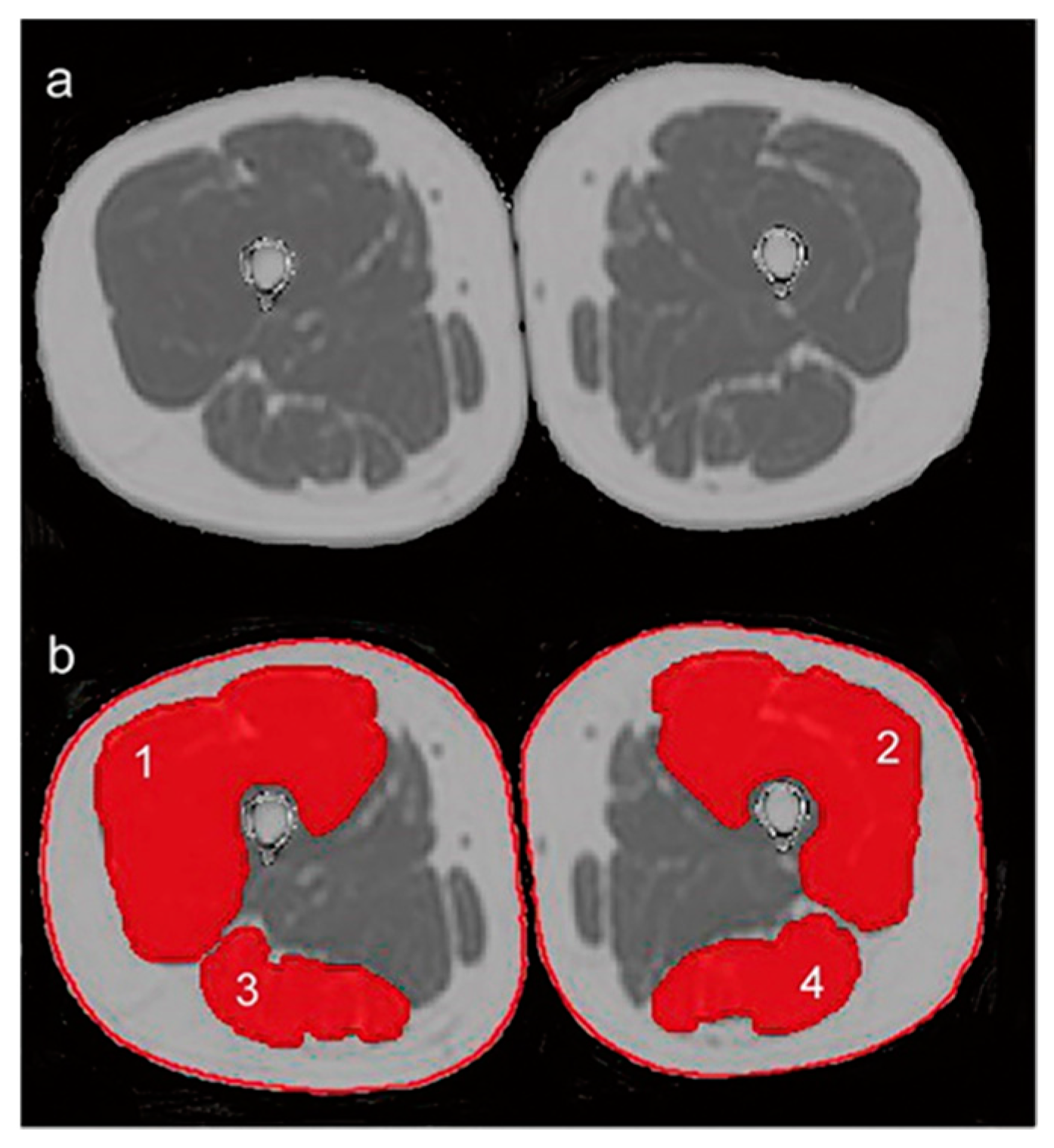
- Edmunds, K.; Gíslason, M.; Sigurðsson, S.; Guðnason, V.; Harris, T.; Carraro, U.; Gargiulo, P. Advanced quantitative methods in correlating sarcopenic muscle degeneration with lower extremity function biometrics and comorbidities. PLoS ONE 2018, 13, e0193241. [Google Scholar] [CrossRef] [PubMed]
- Inhuber, S.; Sollmann, N.; Schlaeger, S.; Dieckmeyer, M.; Burian, E.; Kohlmeyer, C.; Karampinos, D.C.; Kirschke, J.S.; Baum, T.; Kreuzpointner, F.; et al. Associations of thigh muscle fat infiltration with isometric strength measurements based on chemical shift encoding-based water-fat magnetic resonance imaging. Eur. Radiol. Exp. 2019, 3, 45. [Google Scholar] [CrossRef] [Green Version]
- Delbono, O.; Rodrigues, A.C.Z.; Bonilla, H.J.; Messi, M.L. The emerging role of the sympathetic nervous system in skeletal muscle motor innervation and sarcopenia. Ageing Res. Rev. 2021, 67, 101305. [Google Scholar] [CrossRef]
- Keller, K.; Engelhardt, M. Strength and muscle mass loss with aging process. Age and strength loss. Muscle Ligaments Tendons J. 2019, 3, 346–350. [Google Scholar] [CrossRef]
- Freiberger, E.; Haeberle, L.; Spirduso, W.W.; Zijlstra, G.A.R. Long-Term Effects of Three Multicomponent Exercise Interventions on Physical Performance and Fall-Related Psychological Outcomes in Community-Dwelling Older Adults: A Randomized Controlled Trial. J. Am. Geriatr. Soc. 2012, 60, 437–446. [Google Scholar] [CrossRef]
- Bruyere, O.; Wuidart, M.-A.; Di Palma, E.; Gourlay, M.; Ethgen, O.; Richy, F.; Reginster, J.-Y. Controlled whole body vibration to decrease fall risk and improve health-related quality of life of nursing home residents. Arch. Phys. Med. Rehabil. 2005, 86, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Álvarez-Barbosa, F.; del Pozo-Cruz, J.; del Pozo-Cruz, B.; Rosa, R.M.A.; Rogers, M.E.; Zhang, Y. Effects of supervised whole body vibration exercise on fall risk factors, functional dependence and health-related quality of life in nursing home residents aged 80+. Maturitas 2014, 79, 456–463. [Google Scholar] [CrossRef] [PubMed]
- Healee, D.J.; McCallin, A.; Jones, M. Older adult’s recovery from hip fracture: A literature review. Int. J. Orthop. Trauma Nurs. 2011, 15, 18–28. [Google Scholar] [CrossRef] [Green Version]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.M.; Lamb, S.E. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2012, 9, CD007146. [Google Scholar] [CrossRef]
- Zhuang, J.; Huang, L.; Wu, Y.; Zhang, Y. The effectiveness of a combined exercise intervention on physical fitness factors related to falls in community-dwelling older adults. Clin. Interv. Aging 2014, 9, 131–140. [Google Scholar] [CrossRef] [Green Version]
- Kannus, P.; Sievänen, H.; Palvanen, M.; Järvinen, T.; Parkkari, J. Prevention of falls and consequent injuries in elderly people. Lancet 2005, 366, 1885–1893. [Google Scholar] [CrossRef]
- Gillespie, L.D.; Gillespie, W.J.; Robertson, M.C.; Lamb, S.E.; Cumming, R.G.; Rowe, B.H. Interventions for preventing falls in elderly people. Cochrane Database Syst. Rev. 2003, 4, CD000340. [Google Scholar] [CrossRef]
- Duncan, P.W.; Weiner, D.K.; Chandler, J.; Studenski, S. Functional Reach: A New Clinical Measure of Balance. J. Gerontol. 1990, 45, M192–M197. [Google Scholar] [CrossRef]
- El-Sharif, S.I.; Al-Harbi, A.B.; Al-Shihabi, A.M.; Al-Daour, D.S.; Sharif, R.S. Falls in the elderly: Assessment of prevalence and risk factors. Pharm. Pract. 2018, 16, 1206. [Google Scholar] [CrossRef] [Green Version]
- Maidan, I.; Droby, A.; Jacob, Y.; Giladi, N.; Hausdorff, J.M.; Mirelman, A. The neural correlates of falls: Alterations in large-scale resting-state networks in elderly fallers. Gait Posture 2020, 80, 56–61. [Google Scholar] [CrossRef]
- Hughes, V.A.; Frontera, W.R.; Wood, M.; Evans, W.J.; Dallal, G.E.; Roubenoff, R.; Singh, M.A.F. Longitudinal Muscle Strength Changes in Older Adults: Influence of Muscle Mass, Physical Activity, and Health. J. Gerontol. Ser. A 2001, 56, B209–B217. [Google Scholar] [CrossRef] [PubMed]
- Spirduso, W.W. Physical Activity and Aging: Retrospections and Visions for the Future. J. Aging Phys. Act. 1994, 2, 233–242. [Google Scholar] [CrossRef]
- Beaudart, C.; Rizzoli, R.; Bruyère, O.; Reginster, J.-Y.; Biver, E. Sarcopenia: Burden and challenges for public health. Arch. Public Health 2014, 72, 45. [Google Scholar] [CrossRef] [Green Version]
- Santos, D.; Silva, A.; Baptista, F.; Santos, R.; Vale, S.; Mota, J.; Sardinha, L.B. Sedentary behavior and physical activity are independently related to functional fitness in older adults. Exp. Gerontol. 2012, 47, 908–912. [Google Scholar] [CrossRef] [PubMed]
- Lopez, P.; Pinto, R.S.; Radaelli, R.; Rech, A.; Grazioli, R.; Izquierdo, M.; Cadore, E. Benefits of resistance training in physically frail elderly: A systematic review. Aging Clin. Exp. Res. 2018, 30, 889–899. [Google Scholar] [CrossRef] [PubMed]
- Sousa, N.; Mendes, R.; Abrantes, C.; Sampaio, J. Differences in Maximum Upper and Lower Limb Strength in Older Adults after a 12 Week Intense Resistance Training Program. J. Hum. Kinet. 2011, 30, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Pirker, W.; Katzenschlager, R. Gait disorders in adults and the elderly: A clinical guide. Wien. Klin. Wochenschr. 2016, 129, 81–95. [Google Scholar] [CrossRef] [Green Version]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1094–1105. [Google Scholar] [CrossRef] [Green Version]
- Phillips, S.M.; Winett, R.A. Uncomplicated Resistance Training and Health-Related Outcomes: Evidence for a public health mandate. Curr. Sports Med. Rep. 2010, 9, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Kraemer, W.J.; Ratamess, N.A. Fundamentals of Resistance Training: Progression and Exercise Prescription. Med. Sci. Sports Exerc. 2004, 36, 674–688. [Google Scholar] [CrossRef]
- Fragala, M.S.; Cadore, E.L.; Dorgo, S.; Izquierdo, M.; Kraemer, W.J.; Peterson, M.D.; Ryan, E.D. Resistance Training for Older Adults: Position Statement From the National Strength and Conditioning Association. J. Strength Cond. Res. 2019, 33, 2019–2052. [Google Scholar] [CrossRef] [PubMed]
- Law, T.D.; Clark, L.A.; Clark, B.C. Resistance Exercise to Prevent and Manage Sarcopenia and Dynapenia. Annu. Rev. Gerontol. Geriatr. 2016, 36, 205–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kraemer, W.J.; Adams, K.; Cafarelli, E.; Dudley, G.A.; Dooly, C.; Feigenbaum, M.S.; Fleck, S.J.; Franklin, B.; Fry, A.C.; Hoffman, J.; et al. Progression Models in Resistance Training for Healthy Adults. Med. Sci. Sports Exerc. 2002, 34, 364–380. [Google Scholar] [CrossRef] [PubMed]
- Borde, R.; Hortobágyi, T.; Granacher, U. Dose–Response Relationships of Resistance Training in Healthy Old Adults: A Systematic Review and Meta-Analysis. Sports Med. 2015, 45, 1693–1720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hart, P.D.; Buck, D.J. The effect of resistance training on health-related quality of life in older adults: Systematic review and meta-analysis. Health Promot. Perspect. 2019, 9, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peterson, M.D.; Rhea, M.R.; Sen, A.; Gordon, P. Resistance exercise for muscular strength in older adults: A meta-analysis. Ageing Res. Rev. 2010, 9, 226–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Talar, K.; Hernández-Belmonte, A.; Vetrovsky, T.; Steffl, M.; Kałamacka, E.; Courel-Ibáñez, J. Benefits of Resistance Training in Early and Late Stages of Frailty and Sarcopenia: A Systematic Review and Meta-Analysis of Randomized Controlled Studies. J. Clin. Med. 2021, 10, 1630. [Google Scholar] [CrossRef]
- Mañas, A.; Gómez-Redondo, P.; Valenzuela, P.L.; Morales, J.S.; Lucía, A.; Ara, I. Unsupervised home-based resistance training for community-dwelling older adults: A systematic review and meta-analysis of randomized controlled trials. Ageing Res. Rev. 2021, 69, 101368. [Google Scholar] [CrossRef]
- Skelton, D.A.; Young, A.; Greig, C.A.; Malbut, K.E. Effects of Resistance Training on Strength, Power, and Selected Functional Abilities of Women Aged 75 and Older. J. Am. Geriatr. Soc. 1995, 43, 1081–1087. [Google Scholar] [CrossRef]
- Hruda, K.V.; Hicks, A.L.; McCartney, N. Training for Muscle Power in Older Adults: Effects on Functional Abilities. Can. J. Appl. Physiol. 2003, 28, 178–189. [Google Scholar] [CrossRef]
- Kim, H.K.; Suzuki, T.; Saito, K.; Yoshida, H.; Kobayashi, H.; Kato, H.; Katayama, M. Effects of Exercise and Amino Acid Supplementation on Body Composition and Physical Function in Community-Dwelling Elderly Japanese Sarcopenic Women: A Randomized Controlled Trial. J. Am. Geriatr. Soc. 2012, 60, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Suzuki, T.; Saito, K.; Yoshida, H.; Kojima, N.; Kim, M.; Sudo, M.; Yamashiro, Y.; Tokimitsu, I. Effects of exercise and tea catechins on muscle mass, strength and walking ability in community-dwelling elderly Japanese sarcopenic women: A randomized controlled trial. Geriatr. Gerontol. Int. 2013, 13, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Suzuki, T.; Kim, M.; Kojima, N.; Ota, N.; Shimotoyodome, A.; Hase, T.; Hosoi, E.; Yoshida, H. Effects of Exercise and Milk Fat Globule Membrane (MFGM) Supplementation on Body Composition, Physical Function, and Hematological Parameters in Community-Dwelling Frail Japanese Women: A Randomized Double Blind, Placebo-Controlled, Follow-Up Trial. PLoS ONE 2015, 10, e0116256. [Google Scholar] [CrossRef] [Green Version]
- Vasconcelos, K.S.S.; Dias, J.M.D.; Araújo, M.C.; Pinheiro, A.C.; Moreira, B.S.; Dias, R.C. Effects of a progressive resistance exercise program with high-speed component on the physical function of older women with sarcopenic obesity: A randomized controlled trial. Braz. J. Phys. Ther. 2016, 20, 432–440. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.-W.; Ku, J.-W.; Lin, L.-F.; Liao, C.-D.; Chou, L.-C.; Liou, T.-H. Body composition influenced by progressive elastic band resistance exercise of sarcopenic obesity elderly women: A pilot randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2017, 53, 556–563. [Google Scholar] [CrossRef]
- Liao, C.-D.; Tsauo, J.-Y.; Huang, S.-W.; Ku, J.-W.; Hsiao, D.-J.; Liou, T.-H. Effects of elastic band exercise on lean mass and physical capacity in older women with sarcopenic obesity: A randomized controlled trial. Sci. Rep. 2018, 8, 2317. [Google Scholar] [CrossRef] [Green Version]
- Piastra, G.; Perasso, L.; Lucarini, S.; Monacelli, F.; Bisio, A.; Ferrando, V.; Gallamini, M.; Faelli, E.; Ruggeri, P. Effects of Two Types of 9-Month Adapted Physical Activity Program on Muscle Mass, Muscle Strength, and Balance in Moderate Sarcopenic Older Women. BioMed Res. Int. 2018, 2018, 5095673. [Google Scholar] [CrossRef]
- Rodrigues, F.; Macedo, R. Exercise Promotion: Reviewing the Importance of Health Professionals’ Interpersonal Behaviors on Exercisers’ Basic Psychological Needs. Percept. Mot. Ski. 2021, 128, 800–812. [Google Scholar] [CrossRef]
- Rodrigues, F.; Teixeira, D.S.; Cid, L.; Monteiro, D. Promoting Physical Exercise Participation: The Role of Interpersonal Behaviors for Practical Implications. J. Funct. Morphol. Kinesiol. 2019, 4, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodrigues, F.; Domingos, C.; Monteiro, D.; Morouço, P. A Review on Aging, Sarcopenia, Falls, and Resistance Training in Community-Dwelling Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 874. https://doi.org/10.3390/ijerph19020874
Rodrigues F, Domingos C, Monteiro D, Morouço P. A Review on Aging, Sarcopenia, Falls, and Resistance Training in Community-Dwelling Older Adults. International Journal of Environmental Research and Public Health. 2022; 19(2):874. https://doi.org/10.3390/ijerph19020874
Chicago/Turabian StyleRodrigues, Filipe, Christophe Domingos, Diogo Monteiro, and Pedro Morouço. 2022. "A Review on Aging, Sarcopenia, Falls, and Resistance Training in Community-Dwelling Older Adults" International Journal of Environmental Research and Public Health 19, no. 2: 874. https://doi.org/10.3390/ijerph19020874
APA StyleRodrigues, F., Domingos, C., Monteiro, D., & Morouço, P. (2022). A Review on Aging, Sarcopenia, Falls, and Resistance Training in Community-Dwelling Older Adults. International Journal of Environmental Research and Public Health, 19(2), 874. https://doi.org/10.3390/ijerph19020874







