Does Seasonal Influenza Related Hospital Occupancy Surge Impact Hospital Staff Sickness Presenteeism and Productivity Costs?
Abstract
1. Introduction
1.1. Seasonal Influenza Flu Surge and Staff Presenteeism in Metropolitan Hospitals
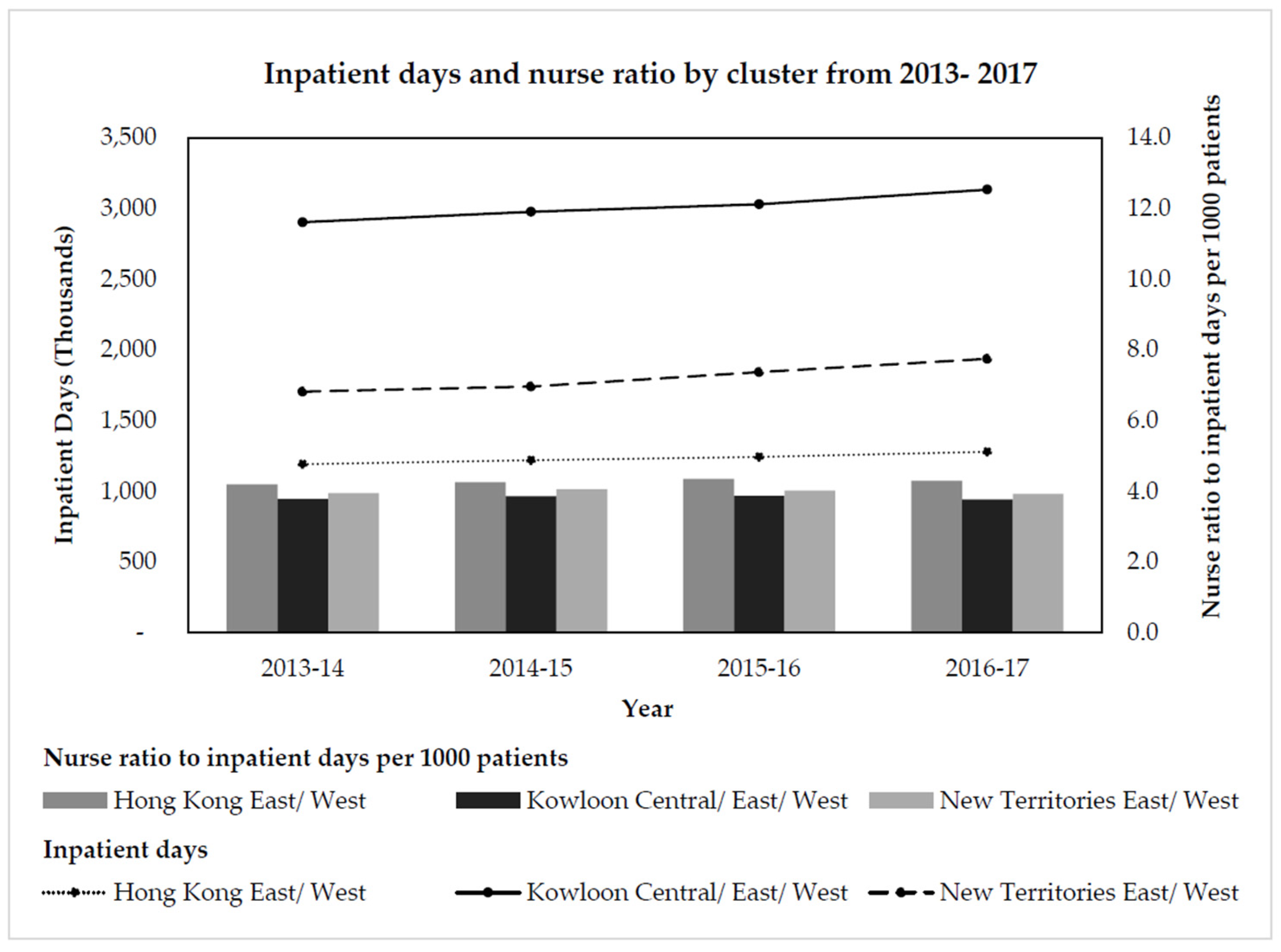
1.2. Hong Kong Hospital Cluster Division and Nurse Workforce
1.3. Productivity Loss Costs, Influenza and Staff Presenteeism
2. Materials and Methods
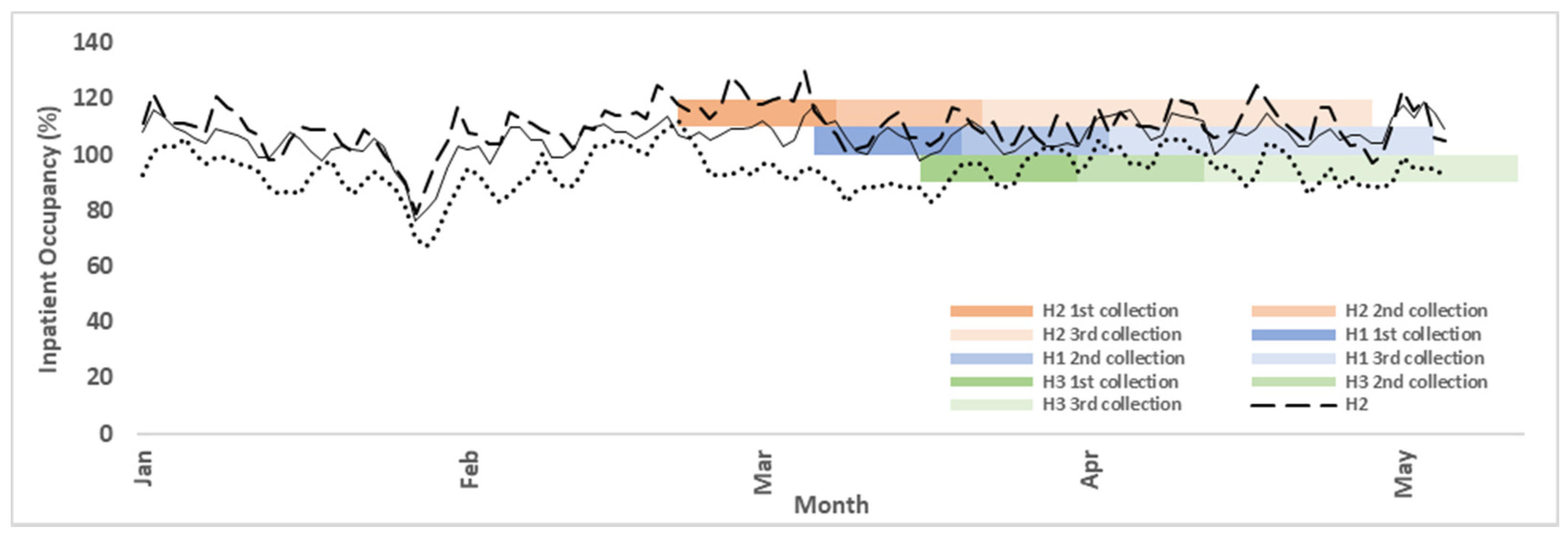
2.1. Sample Frame
2.2. Survey Administration and Collection Procedure
2.3. Measures
2.4. Data Analyses
2.4.1. Presenteeism Prevalence
2.4.2. Association between Presenteeism and Workload
2.4.3. Productivity Costing
3. Results
3.1. Nurse Presenteeism Prevalence
3.2. Association between Workload and Nurse Presenteeism
3.3. Productivity Lost Costs of Nurses in Different Health States
4. Discussion
4.1. Workload and Presenteeism
4.2. Hong Kong Nurse Presenteeism Productivity Costs Highest Worldwide
4.3. Low Productivity Levels across Different Health States
4.4. Implications for Hospital Management and Human Resources Managers
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rainbow, J.G.; Steege, L. Presenteeism in nursing: An evolutionary concept analysis. Nurs. Outlook 2017, 65, 615–623. [Google Scholar] [CrossRef]
- Hemp, P. Presenteeism: At work—But out of it. Harv. Bus. Rev. 2004, 82, 49–58. [Google Scholar] [PubMed]
- Aronsson, G.; Gustafsson, K.; Dallner, M. Sick but yet at work. An empirical study of sickness presenteeism. J. Epidemiol. Community Health 2000, 54, 502–509. [Google Scholar] [CrossRef]
- Bergström, G.; Bodin, L.; Hagberg, J.; Aronsson, G.; Josephson, M. Sickness Presenteeism Today, Sickness Absenteeism Tomorrow? A Prospective Study on Sickness Presenteeism and Future Sickness Absenteeism. J. Occup. Environ. Med. 2009, 51, 629–638. [Google Scholar] [CrossRef] [PubMed]
- Widera, E.; Chang, A.; Chen, H.L. Presenteeism: A Public Health Hazard. J. Gen. Intern. Med. 2010, 25, 1244–1247. [Google Scholar] [CrossRef]
- Chiu, S.; Black, C.L.; Yue, X.; Greby, S.M.; Laney, A.S.; Campbell, A.P.; de Perio, M.A. Working with influenza-like illness: Presenteeism among US health care personnel during the 2014–2015 influenza season. Am. J. Infect. Control 2017, 45, 1254–1258. [Google Scholar] [CrossRef]
- Poon, C.M.; Wong, E.L.Y.; Chau, P.Y.K.; Yau, S.Y.; Yeoh, E.K. Management decision of hospital surge: Assessing seasonal upsurge in inpatient medical bed occupancy rate among public acute hospitals in Hong Kong. Qjm Int. J. Med. 2018, 112, 11–16. [Google Scholar] [CrossRef]
- Webster, R.K.; Liu, R.; Karimullina, K.; Hall, I.; Amlôt, R.; Rubin, G.J. A systematic review of infectious illness Presenteeism: Prevalence, reasons and risk factors. BMC Public Health 2019, 19, 799. [Google Scholar] [CrossRef]
- Resources Allocation among Hospital Clusters by the Hospital Authority; Updated Background Brief Prepared by the Legislative Council Secretariat for the Meeting on 20 January 2014; Legislative Council: Hong Kong, China, 2014.
- Hospital Authority. Hospital Authority Data Sharing Portal Hong Kong. 2019. Available online: http://www3.ha.org.hk/data/HAStatistics/MajorReport (accessed on 10 July 2019).
- LCQ19: Healthcare Manpower; The Government of the Hong Kong Special Administrative Region: Hong Kong, China, 2018.
- Health Services Statistical Highlights; Research Office, Legislative Council Secretariat: Hong Kong, China, 2018.
- Report of the Strategic Review on Healthcare Manpower Planning and Professional Development; Food and Health Bureau: Hong Kong, China, 2019.
- Strategic Review on Healthcare Manpower Planning and Professional Development; Legislative Council Panel on Health Services: Hong Kong, China, 2017.
- Schultz, A.B.; Chen, C.-Y.; Edington, D.W.; Edington, D.W. The Cost and Impact of Health Conditions on Presenteeism to Employers. PharmacoEconomics 2009, 27, 365–378. [Google Scholar] [CrossRef]
- Burton, W.N.; Conti, D.J.; Chen, C.-Y.; Schultz, A.B.; Edington, D.W. The Economic Burden of Lost Productivity Due to Migraine Headache: A Specific Worksite Analysis. J. Occup. Environ. Med. 2002, 44, 523–529. [Google Scholar] [CrossRef]
- Goetzel, R.Z.; Long, S.R.; Ozminkowski, R.J.; Hawkins, K.; Shaohung, W.; Lynch, W. Health, Absence, Disability, and Presenteeism Cost Estimates of Certain Physical and Mental Health Conditions Affectig U.S. Employers. J. Occup. Environ. Med. 2004, 46, 398–412. [Google Scholar] [CrossRef]
- Collins, J.J.; Baase, C.M.; Sharda, C.E.; Ozminkowski, R.J.; Nicholson, S.; Billotti, G.M.; Turpin, R.S.; Olson, M.; Berger, M.L. The Assessment of Chronic Health Conditions on Work Performance, Absence, and Total Economic Impact for Employers. J. Occup. Environ. Med. 2005, 47, 547–557. [Google Scholar] [CrossRef]
- Van Wormer, J.J.; King, J.P.; Gajewski, A.; McLean, H.Q.; Belongia, E.A. Influenza and workplace productivity loss in working adults. J. Occup. Environ. Med. 2017, 59, 1135–1139. [Google Scholar] [CrossRef]
- Hubble, M.W.; Renkiewicz, G.K. Estimated Cost Effectiveness of Influenza Vaccination for Emergency Medical Services Professionals. West. J. Emerg. Med. 2021, 22, 1317–1325. [Google Scholar] [CrossRef]
- Freeling, M.; Rainbow, J.G.; Chamberlain, D. Painting a picture of nurse presenteeism: A multi-country integrative review. Int. J. Nurs. Stud. 2020, 109, 103659. [Google Scholar] [CrossRef]
- Leal, C.C.; Ferreira, A.I. In Sickness and in Health: The Role of Housework Engagement in Work Productivity despite Presenteeism. Span. J. Psychol. 2021, 24, e39. [Google Scholar] [CrossRef]
- Li, Y.; Zhang, J.; Wang, S.; Guo, S. The Effect of Presenteeism on Productivity Loss in Nurses: The Mediation of Health and the Moderation of General Self-Efficacy. Front. Psychology 2019, 10, 1745. [Google Scholar] [CrossRef]
- Tomonaga, Y.; Zens, K.D.; Lang, P.; Born, R.; Schwenkglenks, M. Productivity losses due to influenza and influenza-like illness in Switzerland: Results of the Swiss Sentinel Surveillance Network in a non-pandemic era. Swiss Med. Weekly. 2021, 33, 1–11. [Google Scholar]
- Kockaya, G.; Oğuzhan, G.; Şen, S.; Kurnaz, M.; Ökçün, S.; Caliskan, Z.; Kahveci, B.; Saylan, M. PIN53 Cost of Productivity Loss of Common Cold and FLU in Turkey. Value Health 2020, 23, S553. [Google Scholar] [CrossRef]
- Haque, A. Strategic human resource management and presenteeism: A conceptual framework to predict human resource outcomes. New Zealand J. Hum. Resour. Manag. 2018, 18, 3–18. [Google Scholar]
- Hospital Authority. Service Guides -Clusters, Hospitals & Institutions Hong Kong. 2019. Available online: https://www.ha.org.hk/visitor/ha_visitor_index.asp?Content_ID=10084&Lang=ENG&Dimension=100 (accessed on 20 June 2019).
- Hong Kong Hospital Authority. Hospital Authority Annual Report 2017–2018; Hong Kong Hospital Authority: Hong Kong, China, 2017. [Google Scholar]
- Needham, J. Accuracy in workload measurement: A fact or fallacy? J. Nurs. Manag. 1997, 5, 83–87. [Google Scholar] [CrossRef]
- Lau, E.H.Y.; Cowling, B.J.; Ho, L.-M.; Leung, G.M. Optimizing Use of Multistream Influenza Sentinel Surveillance Data. Emerg. Infect. Dis. 2008, 14, 1154–1157. [Google Scholar] [CrossRef]
- Demerouti, E.; Le Blanc, P.M.; Bakker, A.B.; Schaufeli, W.B.; Hox, J. Present but sick: A three-wave study on job demands, presenteeism and burnout. Career Dev. Int. 2009, 14, 50–68. [Google Scholar] [CrossRef]
- Hansen, C.D.; Andersen, J.H. Going ill to work-what personal circumstances, attitudes and work-related factors are associated with sickness presenteeism? Soc. Sci. Med. 2008, 67, 956–964. [Google Scholar] [CrossRef]
- Dellve, L.; Hadzibajramovic, E.; Ahlborg, G., Jr. Work attendance among healthcare workers: Prevalence, incentives, and long-term consequences for health and performance. J. Adv. Nurs. 2011, 67, 1918–1929. [Google Scholar] [CrossRef]
- Lui, N.M.J.; Andres, E.B.; Johnston, J.M. Presenteeism exposures and outcomes amongst hospital doctors and nurses: A systematic review. BMC Health Serv. Res. 2018, 18, 1–15. [Google Scholar] [CrossRef]
- Mitchell, K.J.; Vayalumkal, J.V. Sickness presenteeism: The prevalence of coming to work while ill among paediatric resident physicians in Canada. Paediatr. Child Health 2017, 22, 84–88. [Google Scholar] [CrossRef][Green Version]
- Kessler, R.C.; Barber, C.; Beck, A.; Berglund, P.; Cleary, P.D.; McKenas, D.; Pronk, N.; Simon, G.; Stang, P.; Ustun, T.B.; et al. The World Health Organization Health and Work Performance Questionnaire (HPQ). J. Occup. Environ. Med. 2003, 45, 156–174. [Google Scholar] [CrossRef]
- Stewart, W.F.; Ricci, J.A.; Leotta, C. Health-Related Lost Productive Time (LPT): Recall Interval and Bias in LPT Estimates. J. Occup. Environ. Med. 2004, 46, S12–S22. [Google Scholar] [CrossRef]
- Lunardon, N.; Scharfstein, D. Comment on ‘Small sample GEE estimation of regression parameters for longitudinal data’. Stat. Med. 2017, 36, 3596–3600. [Google Scholar] [CrossRef]
- McNeish, D.; Stapleton, L.M. Modeling clustered data with very few clusters. Multivar. Behav. Res. 2016, 51, 495–518. [Google Scholar] [CrossRef]
- Aronsson, G.; Gustafsson, K. Sickness presenteeism: Prevalence, attendance-pressure factors, and an outline of a model for research. J. Occup. Environ. Med. 2005, 47, 958–966. [Google Scholar] [CrossRef]
- Hong Kong Hospital Authority. Press Releases. 2017. Available online: http://www.ha.org.hk/visitor/ha_visitor_index.asp?Content_ID=643&Lang=ENG&Dimension=100&Parent_ID=10000 (accessed on 5 October 2018).
- Van Buuren, S.; Groothuis-Oudshoorn, K. Mice: Multivariate imputation by chained equations in R. J. Stat. Software. 2011, 45, 1–68. [Google Scholar] [CrossRef]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; John Wiley & Sons: New York, NY, USA, 1987. [Google Scholar]
- Berger, M.L.; Murray, J.F.; Xu, J.; Pauly, M. Alternative Valuations of Work Loss and Productivity. J. Occup. Environ. Med. 2001, 43, 18–24. [Google Scholar] [CrossRef]
- Ricci, J.A.; Chee, E. Lost Productive Time Associated with Excess Weight in the U.S. Workforce. J. Occup. Environ. Med. 2005, 47, 1227–1234. [Google Scholar] [CrossRef][Green Version]
- Braakman-Jansen, L.M.A.; Taal, E.; Kuper, I.H.; Van De Laar, M.A.F.J. Productivity loss due to absenteeism and presenteeism by different instruments in patients with RA and subjects without RA. Rheumatology 2011, 51, 354–361. [Google Scholar] [CrossRef]
- Warren, C.L.; White-Means, S.I.; Wicks, M.N.; Chang, C.F.; Gourley, D.; Rice, M. Cost burden of the presenteeism health outcome: Diverse workforce of nurses and pharmacists. J. Occup. Environ. Medicine. 2011, 53, 90–99. [Google Scholar] [CrossRef]
- Letvak, S.A.; Ruhm, C.J.; Gupta, S.N. Nurses’ presenteeism and its effects on self-reported quality of care and costs. AJN Am. J. Nursing. 2012, 112, 30–38. [Google Scholar] [CrossRef]
- d’Errico, A.; Viotti, S.; Baratti, A.; Mottura, B.; Barocelli, A.P.; Tagna, M.; Sgambelluri, B.; Battaglino, P.; Converso, D. Low back pain and associated presenteeism among hospital nursing staff. J. Occup. Health. 2013, 55, 276–283. [Google Scholar] [CrossRef]
- Duffield, C.; Diers, D.; O’Brien-Pallas, L.; Aisbett, C.; Roche, M.; King, M.; Aisbett, K. Nursing staffing, nursing workload, the work environment and patient outcomes. Appl. Nurs. Res. 2011, 24, 244–255. [Google Scholar] [CrossRef]
- Diwas, S.K.; Terwiesch, C. Impact of workload on service time and patient safety: An econometric analysis of hospital operations. Manag. Sci. 2009, 55, 1486–1498. [Google Scholar]
- Aiken, L.H.; Clarke, S.; Sloane, D.M.; Sochalski, J.; Silber, J.H. Hospital Nurse Staffing and Patient Mortality, Nurse Burnout, and Job Dissatisfaction. JAMA 2002, 288, 1987–1993. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, M.; Batty, G.D.; Pentti, J.; Vahtera, J.; Oksanen, T.; Tuisku, K.; Salo, P.; Terho, K.; Ahola, K.; Elovainio, M.; et al. Patient overcrowding in hospital wards as a predictor of diagnosis-specific mental disorders among staff: A 2-year prospective cohort study. J. Clin. Psychiatry 2010, 71, 1308–1312. [Google Scholar] [CrossRef] [PubMed]
- Elstad, J.I.; Vabø, M. Job stress, sickness absence and sickness presenteeism in Nordic elderly care. Scand. J. Public Health 2008, 36, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Rantanen, I.; Tuominen, R. Relative magnitude of presenteeism and absenteeism and work-related factors affecting them among health care professionals. Int. Arch. Occup. Environ. Health 2010, 84, 225–230. [Google Scholar] [CrossRef]
- Shan, G.; Wang, S.; Wang, W.; Guo, S.; Li, Y. Presenteeism in Nurses: Prevalence, Consequences, and Causes from the Perspectives of Nurses and Chief Nurses. Front. Psychiatry 2021, 11, 1–10. [Google Scholar] [CrossRef]
- Siu, O.L.; Cooper, C.L.; Roll, L.C.; Lo, C. Occupational Stress and Its Economic Cost in Hong Kong: The Role of Positive Emotions. Int. J. Environ. Res. Public Health 2020, 17, 8601. [Google Scholar] [CrossRef]
- Andres, E.B.; Lui, J.N.M.; Song, W.; Johnston, J.M. Exploring Hong Kong nurses’ decision-making processes around presenteeism. Occup. Med. 2021, 71, 189–195. [Google Scholar] [CrossRef]
- Karoly, P.; Ruehlman, L.S.; Okun, M.A. Psychosocial and demographic correlates of employment vs. disability status in a national community sample of adults with chronic pain: Toward a psychology of pain presenteeism. Pain Med. 2013, 14, 1698–1707. [Google Scholar] [CrossRef]
| Questions/Health States | How Many Times during the Last Year Have You Gone to Work When You Should Have Been on Sick Leave Due to Your Health Condition? (1—Never, 2—Once, 3—2 to 5 Times, 4—>5 Times) | Miss an Entire/Part of Work Day Because of Problems with Your Physical or Mental Health? |
|---|---|---|
| Healthy | 1 | 0 |
| Sickness Presenteeism | >1 | 0 |
| Sick Leave | 1,2,3,4 (anything) | >0 |
| Healthy and Sickness Presenteeism Measure self-rated productivity (a) by item “How would you rate your overall job performance on the days you worked during the past 4 weeks (28 days)? (0—worst performance, 10—best performance)” Convert the above item to percentage productivity loss: (10 − a) × 10 = x% Discount monthly median salary by percentage productivity loss: monthly salary × x% Sick Leave—USD productivity loss remaining days worked Measure self-rated productivity (a) by item “How would you rate your overall job performance on the days you worked during the past 4 weeks (28 days)? (0—worst performance, 10—best performance)” Convert the above item to % productivity loss: (10 − a) × 10 = x% Measure number of days sick leave by 2 items “ Miss an entire work day because of problems with your physical or mental health?” and “Miss part of a work day because of problems with your physical or mental health?” Discount monthly median salary by % productivity loss: monthly salary / 30 days × days not on leave × x% | ||
| Characteristics | H1 n = 824 (rr: 71.9%) n (%) | H2 n = 835 (rr: 61.1%) n (%) | H3 n = 1379 (rr: 64.3%) n (%) | P Value between Hospital Differences |
|---|---|---|---|---|
| Gender | ||||
| Male | 95 (11.5) | 133 (15.9) | 192 (13.9) | 0.034 * |
| Female | 729 (88.5) | 702 (84.1) | 1187 (86.1) | |
| Age Group | ||||
| ≤30 | 226 (28.4) | 285 (35.1) | 507 (38.3) | <0.001 ** |
| 31–40 | 196 (24.6) | 235 (28.9) | 265 (20.0) | |
| 41–50 | 263 (33.0) | 189 (23.3) | 357 (26.9) | |
| ≥51 | 111 (13.9) | 103 (12.7) | 196 (14.8) | |
| Educational Qualifications | ||||
| Certificate/diploma | 72 (9.1) | 65 (8.2) | 111 (8.6) | <0.001 ** |
| Associate diploma/higher diploma | 47 (6.0) | 40 (5.1) | 176 (13.6) | |
| Bachelor’s degree | 432 (54.8) | 436 (55.1) | 582 (45.1) | |
| Postgraduate degree | 237 (30.1) | 251 (31.7) | 422 (32.7) | |
| Rank | ||||
| Junior staff (EN) | 51 (6.2) | 63 (7.5) | 96 (7.0) | 0.393 |
| Junior staff (RN) | 566 (68.7) | 579 (69.3) | 959 (69.5) | |
| Middle management (APN/NC) | 172 (20.9) | 146 (17.5) | 248 (18.0) | |
| Senior management (WM/DOM) | 35 (4.2) | 47 (5.6) | 76 (5.5) | |
| Working Schedule | ||||
| Shift schedule | 664 (82.8) | 652 (79.5) | 1044 (77.6) | 0.015 * |
| Regular schedule (9 am–6 pm) | 138 (17.2) | 168 (20.5) | 302 (22.4) | |
| Main Working Location | ||||
| A&E | 46 (5.9) | 68 (8.3) | 46 (3.4) | <0.001 ** |
| GOPC/SOPC | 48 (6.1) | 49 (6.0) | 125 (9.3) | |
| Medicine a | 309 (39.6) | 384 (46.8) | 536 (39.8) | |
| Surgery b | 303 (38.8) | 208 (25.4) | 481 (35.7) | |
| Others c | 75 (9.6) | 111 (13.5) | 159 (11.8) | |
| Self-Rated Health (n (%)) | ||||
| Poor (score: 1,2) | 334 (40.5) | 338 (40.5) | 541 (39.2) | 0.011 * |
| Normal (score: 3) | 232 (28.2) | 212 (25.4) | 428 (31.0) | |
| Good (score: 4,5) | 244 (29.6) | 281 (33.7) | 397 (28.8) | |
| Missing | 14 (1.7) | 4 (0.5) | 13 (0.9) | |
| Number of Sick Leave Days (mean(sd)) | 0.64 (2.13) | 0.65 (3.02) | 0.54 (2.01) | 0.593 |
| Nurse Self-Reported Presenteeism and Productivity | n = 3038 (rr: 71.9%) n (%) |
|---|---|
| Presenteeism Frequency | |
| “How many times during the last year have you gone to work when you should have been on sick leave due to your health condition?” | |
| Never | 352 (11.8) |
| Once | 508 (17.0) |
| 2–5times | 1440 (48.2) |
| >5 times | 689 (23.1) |
| n (sd) | |
| Self-rated Productivity a | 6.61 (1.57) |
| Hospital-Level Risk Factor | Generalized Estimating Equation (GEE) Regression Adjusted OR (95% CI) a,b,c | Conventional Logistic Regression Adjusted OR (95% CI) b |
|---|---|---|
| Occupancy z-score | 1.19 * (1.05–1.35) | 1.18 (0.98–1.42) |
| Health States of Nurses | On-the-Job Productivity Loss (%) a | Mean Sick Leave (days) | Sick Leave Costs (USD) b | Productivity Loss (USD) b |
|---|---|---|---|---|
| Healthy | 32.6 | - | - | 1983 |
| Presenteeism | 33.0 | - | - | 2008 |
| Took Sick leave | 37.4 | 2.56 | 622 | 2081 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lui, J.N.M.; Andres, E.B.; Johnston, J.M. Does Seasonal Influenza Related Hospital Occupancy Surge Impact Hospital Staff Sickness Presenteeism and Productivity Costs? Int. J. Environ. Res. Public Health 2022, 19, 769. https://doi.org/10.3390/ijerph19020769
Lui JNM, Andres EB, Johnston JM. Does Seasonal Influenza Related Hospital Occupancy Surge Impact Hospital Staff Sickness Presenteeism and Productivity Costs? International Journal of Environmental Research and Public Health. 2022; 19(2):769. https://doi.org/10.3390/ijerph19020769
Chicago/Turabian StyleLui, Juliana Nga Man, Ellie Bostwick Andres, and Janice Mary Johnston. 2022. "Does Seasonal Influenza Related Hospital Occupancy Surge Impact Hospital Staff Sickness Presenteeism and Productivity Costs?" International Journal of Environmental Research and Public Health 19, no. 2: 769. https://doi.org/10.3390/ijerph19020769
APA StyleLui, J. N. M., Andres, E. B., & Johnston, J. M. (2022). Does Seasonal Influenza Related Hospital Occupancy Surge Impact Hospital Staff Sickness Presenteeism and Productivity Costs? International Journal of Environmental Research and Public Health, 19(2), 769. https://doi.org/10.3390/ijerph19020769






