Development and Validation of a Knowledge, Attitude and Practice Questionnaire on Antibiotic Use in Arabic and French Languages in Lebanon
Abstract
:1. Introduction
2. Methods
2.1. Study Setting and Population
2.2. Validation Procedure
2.3. Content Validity
2.4. Face Validity
2.5. Pilot Testing
2.6. Reliability
2.7. Construct Validity
2.8. Questionnaire Overall Reliability, Acceptability and Item Response Rate
3. Results
3.1. Content Validity
3.2. Face Validity and Pilot Testing
3.3. Reliability
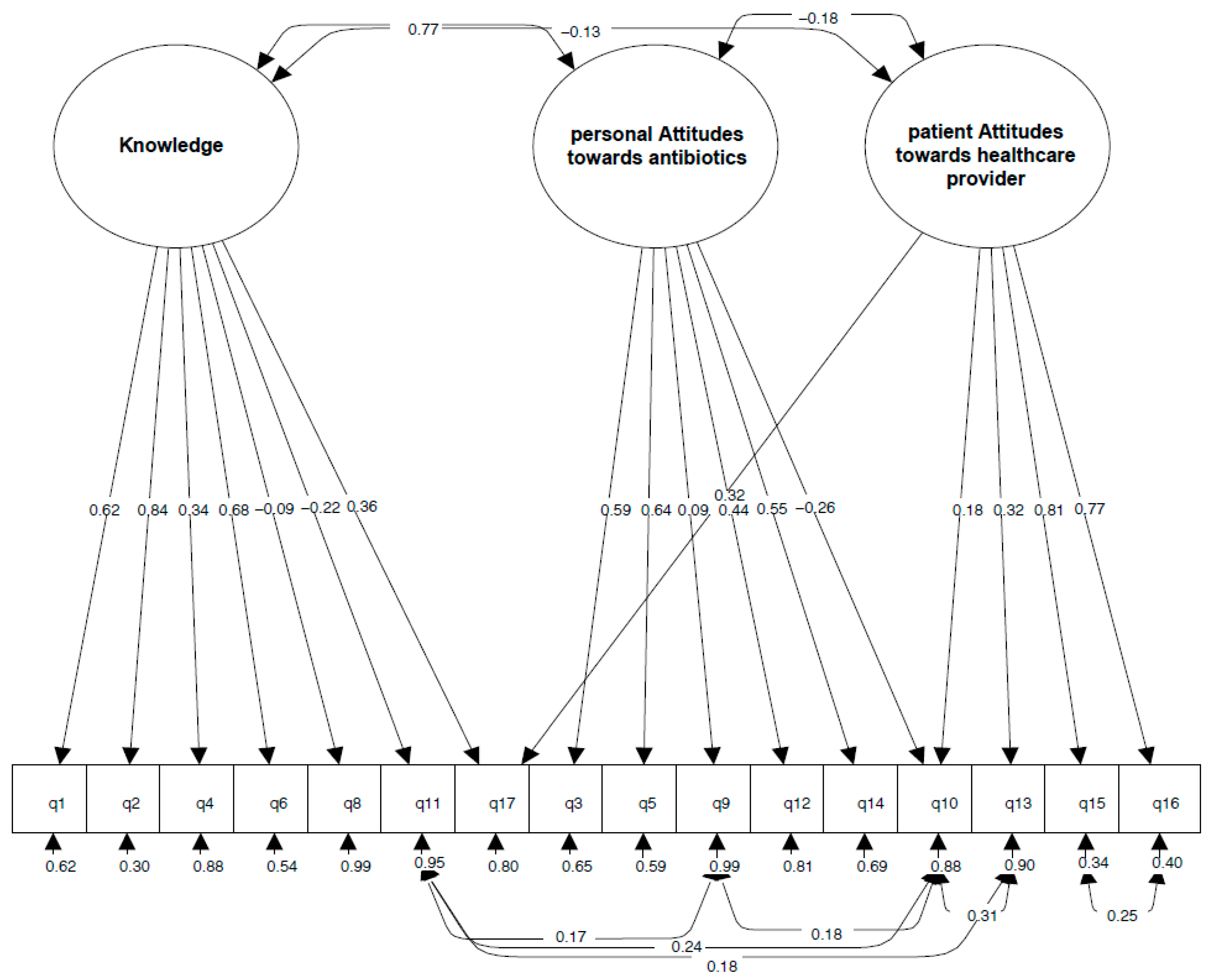
3.4. Construct Validity
3.5. Questionnaire Internal Reliability
3.6. Questionnaire Acceptability
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kosiyaporn, H.; Chanvatik, S.; Issaramalai, T.; Kaewkhankhaeng, W.; Kulthanmanusorn, A.; Saengruang, N.; Witthayapipopsakul, W.; Viriyathorn, S.; Kirivan, S.; Kunpeuk, W.; et al. Surveys of knowledge and awareness of antibiotic use and antimicrobial resistance in general population: A systematic review. PLoS ONE 2020, 15, e0227973. [Google Scholar] [CrossRef] [PubMed]
- Gualano, M.R.; Gili, R.; Scaioli, G.; Bert, F.; Siliquini, R. General population’s knowledge and attitudes about antibiotics: A systematic review and meta-analysis. Pharmacoepidemiol. Drug Saf. 2015, 24, 2–10. [Google Scholar] [CrossRef] [PubMed]
- McCullough, A.R.; Parekh, S.; Rathbone, J.; Del Mar, C.B.; Hoffmann, T.C. A systematic review of the public’s knowledge and beliefs about antibiotic resistance. J. Antimicrob. Chemother. 2016, 71, 27–33. [Google Scholar] [CrossRef]
- Médcins du Monde. The KAP Survey Model (Knowledge, Attitudes, & Practices). Available online: https://www.medecinsdumonde.org/en/actualites/publications/2012/02/20/kap-survey-model-knowledge-attitude-and-practices (accessed on 15 February 2021).
- Centers for Disease Control and Prevention. Antibiotic Use Questions and Answers. Available online: https://www.cdc.gov/antibiotic-use/community/about/should-know.html#anchor_1572453021219 (accessed on 21 April 2021).
- United Nations Office on Drugs and Crime. The Non-Medical Use of Prescription Drugs: Poliy Direction Issues. Available online: https://www.unodc.org/documents/drug-prevention-and-treatment/nonmedical-use-prescription-drugs.pdf (accessed on 21 April 2021).
- World Bank. Drug-Resistant Infections: A Threat to Our Economic Future. Available online: https://documents.worldbank.org/en/publication/documents-reports/documentdetail/323311493396993758/final-report (accessed on 21 April 2021).
- Wellcome Trust. Review on Antimicrobial Resistance. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. Available online: https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf (accessed on 21 April 2021).
- World Health Organization (WHO)—Working Group on Monitoring & Evaluation. Knowledge, Attitudes, and Practices (KAP) Surveys During Cholera Vaccination Campaigns: Guidance for Oral Cholera Vaccine Stockpile Campaigns. Available online: https://www.who.int/cholera/vaccines/kap_protocol.pdf (accessed on 21 April 2021).
- Mallah, N.; Rodriguez-Cano, R.; Figueiras, A.; Takkouche, B. Design, reliability and construct validity of a knowledge, attitude and practice questionnaire on personal use of antibiotics in Spain. Sci. Rep. 2020, 10, 20668. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef] [Green Version]
- Guillemin, F.; Bombardier, C.; Beaton, D. Cross-cultural adaptation of health-related quality of life measures: Literature review and proposed guidelines. J. Clin. Epidemiol. 1993, 46, 1417–1432. [Google Scholar] [CrossRef]
- World Atlas. Arab Speaking Countries. Available online: https://www.worldatlas.com/articles/arabic-speaking-countries.html (accessed on 26 May 2021).
- Lingualinx. French—The Most Global Language? Available online: https://www.lingualinx.com/blog/french-the-most-global-language (accessed on 26 May 2021).
- Ballais, J.L.; Al Amrawy, M.; Al Dbiyat, M.; Charbel, L.; Geyer, B.; Mezedjri, L.; Brunn, S.; Kehrein, R. (Eds.) Handbook of the Changing World Language Map; Springer: Cham, Switzerland, 2018. [Google Scholar]
- Lynn, M.R. Determination and quantification of content validity. Nurs. Res. 1986, 35, 382–385. [Google Scholar] [CrossRef]
- McDowell, I. (Ed.) Measuring Health. A Guide to Rating Scales and Questionnaires, 3rd ed.; University Press: Oxford, UK, 2006. [Google Scholar]
- Polit, D.F.; Beck, C.T. The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Res. Nurs. Health 2006, 29, 489–497. [Google Scholar] [CrossRef] [Green Version]
- Polit, D.F.; Beck, C.T.; Owen, S.V. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res. Nurs. Health 2007, 30, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Cicchetti, D.V.; Sparrow, S.A. Developing criteria for establishing interrater reliability of specific items: Applications to assessment of adaptive behavior. Am. J. Ment. Defic. 1981, 86, 127–137. [Google Scholar]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research; The Guilford Press: New York, NY, USA, 2006. [Google Scholar]
- Little, T.D. Mean and Covariance Structures (MACS) Analyses of Cross-Cultural Data: Practical and Theoretical Issues. Multivar. Behav. Res. 1997, 32, 53–76. [Google Scholar] [CrossRef]
- Little, T.D. Longitudinal Structural Equation Modeling; The Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Vrieze, S.I. Model selection and psychological theory: A discussion of the differences between the Akaike information criterion (AIC) and the Bayesian information criterion (BIC). Psychol. Methods 2012, 17, 228–243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taber, K.S. The use of Cronbach’s alpha when developing and reporting research instruments in science education. Res. Sci. Educ. 2018, 48, 1273–1296. [Google Scholar] [CrossRef]
- Ursachi, G.; Horodnic, I.A.; Zait, A. How reliable are measurement scales? External factors with indirect influence on reliability estimators. Procedia Econ. Financ. 2015, 20, 679–686. [Google Scholar] [CrossRef] [Green Version]
- Egleston, B.L.; Miller, S.M.; Meropol, N.J. The impact of misclassification due to survey response fatigue on estimation and identifiability of treatment effects. Stat. Med. 2011, 30, 3560–3572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galesic, M.; Bosnjak, M. Effects of questionnaire length on participation and indicators of response quality in a web survey. Public Opin. Q. 2009, 73, 349–360. [Google Scholar] [CrossRef]
- Rosenberg, A.R.; Dussel, V.; Orellana, L.; Kang, T.; Geyer, J.R.; Feudtner, C.; Wolfe, J. What’s missing in missing data? Omissions in survey responses among parents of children with advanced cancer. J. Palliat. Med. 2014, 17, 953–956. [Google Scholar] [CrossRef] [Green Version]
- Statistical Policy Working Paper 31. Measuring and Reporting Sources of Error in Surveys. Executive Office of the President of the United States. Available online: https://www.oecd.org/sdd/measuringandreportingsourcesoferrorinsurveysintheunitedstates.htm (accessed on 21 April 2021).
- Zahreddine, L.; Hallit, S.; Shakaroun, S.; Al-Hajje, A.; Awada, S.; Lahoud, N. Knowledge of pharmacists and parents towards antibiotic use in pediatrics: A cross-sectional study in Lebanon. Pharm. Pract. 2018, 16, 1194. [Google Scholar] [CrossRef] [Green Version]
- Salti, N.; Chaaban, J.; Raad, F. Health equity in Lebanon: A microeconomic analysis. Int. J. Equity Health 2010, 9, 11. [Google Scholar] [CrossRef] [Green Version]
- Tawil, S.; Sacre, H.; Sili, G.; Salameh, P. Patients’ perceptions regarding pharmacists’ healthcare services: The case of Lebanon. J. Pharm. Pract. Res. 2020, 50, 137–143. [Google Scholar] [CrossRef]
- Mallah, N.; Badro, D.A.; Figueiras, A.; Takkouche, B. Association of knowledge and beliefs with the misuse of antibiotics in parents: A study in Beirut (Lebanon). PLoS ONE 2020, 15, e0232464. [Google Scholar] [CrossRef] [PubMed]
- El Bizri, L.; Dimassi, A. Lebanese community pharmacy: The role of the pharmacist in the health care. EJPMR 2019, 6, 149–158. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; The Guilford Press: New York, NY, USA, 2015. [Google Scholar]
| Knowledge or Attitude Statement | ICC (95%CI) | |
|---|---|---|
| Q1 | Antibiotics are effective against viruses | 0.80 (0.69, 0.87) |
| Q2 | When I get a cold, I take antibiotics to help me feel better faster | 0.77 (0.66, 0.85) |
| Q3 | If I feel better after a few days, I sometimes stop taking my antibiotics before completing the course of treatment | 0.82 (0.73, 0.88) |
| Q4 | I expect my doctor to prescribe antibiotics if I suffer from common cold or flu symptoms | 0.71 (0.56, 0.81) |
| Q5 | It is good to be able to get antibiotics from relatives or friends without having to see a medical doctor | 0.82 (0.73, 0.88) |
| Q6 | When I have a sore throat, I prefer to use an antibiotic | 0.87 (0.81, 0.92) |
| Q7 | Each infection needs a different antibiotic | 0.76 (0.64, 0.84) |
| Q8 | Antibiotics can kill the bacteria that normally live on the skin and in the gut | 0.72 (0.57, 0.82) |
| Q9 | If I feel side effects during a course of treatment of antibiotics, I should stop taking them as soon as possible | 0.85 (0.77, 0.90) |
| Q10 | I take the antibiotics according to the doctor’s instructions | 0.71 (0.55, 0.81) |
| Q11 | If antibiotics are consumed in excess, they will not work when they are really needed | 0.70 (0.55, 0.80) |
| Q12 | I prefer to keep antibiotics at home in case there is a need for them later | 0.79 (0.69, 0.86) |
| Q13 | I trust the doctor’s decision if s/he decides to prescribe or not prescribe antibiotics | 0.59 (0.38, 0.73) |
| Q14 | If I believe that I need an antibiotic and the doctor did not prescribe it, I will get it at the pharmacy without a prescription | 0.71 (0.56, 0.81) |
| Q15 | Doctors often explain clearly to the patient the reasons for prescribing or not prescribing antibiotics | 0.78 (0.66, 0.85) |
| Q16 | Doctors often explain clearly to the patient the instructions for the use of antibiotics | 0.80 (0.70, 0.87) |
| Q17 | When you buy antibiotics, the pharmacist tells you about the importance of correct therapeutic compliance/adherence | 0.87 (0.80, 0.91) |
| Indicator | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| χ2 | 1185.56 | 852.603 | 629.856 | 459.392 |
| df | 116 | 100 | 97 | 93 |
| p | <0.001 | <0.001 | <0.001 | <0.001 |
| RSMEA (90% CI) | 0.081 (0.077, 0.085) | 0.073 (0.069, 0.078) | 0.063 (0.058, 0.067) | 0.053 (0.048, 0.058) |
| CFI | 0.77 | 0.83 | 0.88 | 0.92 |
| TLI | 0.73 | 0.80 | 0.85 | 0.90 |
| AIC | 112,294.425 | 105,927.216 | 105,710.469 | 105,548.005 |
| BIC | 112,577.613 | 106,199.916 | 105,998.901 | 105,857.414 |
| aBIC | 112,406.075 | 106,034.731 | 105,824.187 | 105,669.993 |
| SRMR | 0.085 | 0.068 | 0.055 | 0.045 |
| Item | Loading Estimate | Standard Error | p-Value | Standard Loading Estimate |
|---|---|---|---|---|
| Knowledge | ||||
| Q1. Antibiotics are effective against viruses | 1.078 | 0.036 | <0.001 | 0.618 |
| Q2. When I get a cold, I take antibiotics to help me feel better faster | 1.212 | 0.032 | <0.001 | 0.839 |
| Q4. I expect my doctor to prescribe antibiotics if I suffer from common cold or flu symptoms | 0.666 | 0.047 | <0.001 | 0.342 |
| Q6. When I have a sore throat, I prefer to use an antibiotic | 1.044 | 0.034 | <0.001 | 0.682 |
| Q8. Antibiotics can kill the bacteria that normally live on the skin and in the gut | −0.121 | 0.042 | 0.004 | −0.086 |
| Q11. If antibiotics are consumed in excess, they will not work when they are really needed | −0.257 | 0.034 | <0.001 | −0.222 |
| Q17. When you buy antibiotics, the pharmacist tells you about the importance of correct therapeutic compliance/adherence | 0.545 | 0.046 | <0.001 | 0.363 |
| Personal attitudes towards antibiotics | ||||
| Q3. If I feel better after a few days, I sometimes stop taking my antibiotics before completing the course of treatment | 1.453 | 0.063 | <0.001 | 0.590 |
| Q5. It is good to be able to get antibiotics from relatives or friends without having to see a medical doctor | 1.037 | 0.045 | <0.001 | 0.640 |
| Q9. If I feel side effects during a course of treatment of antibiotics, I should stop taking them as soon as possible | 0.208 | 0.073 | 0.004 | 0.087 |
| Q10. I take the antibiotics according to the doctor’s instructions | −0.315 | 0.037 | <0.001 | −0.263 |
| Q12. I prefer to keep antibiotics at home in case there is a need for them later | 1.186 | 0.067 | <0.001 | 0.438 |
| Q14. If I believe that I need an antibiotic and the doctor did not prescribe it, I will get it at the pharmacy without a prescription | 1.116 | 0.052 | <0.001 | 0.553 |
| Patient attitudes towards healthcare provider | ||||
| Q10. I take the antibiotics according to the doctor’s instructions | 0.207 | 0.046 | <0.001 | 0.175 |
| Q13. I trust the doctor’s decision if s/he decides to prescribe or not prescribe antibiotics | 0.566 | 0.091 | <0.001 | 0.318 |
| Q15. Doctors often explain clearly to the patient the reasons for prescribing or not prescribing antibiotics | 1.791 | 0.124 | <0.001 | 0.813 |
| Q16. Doctors often explain clearly to the patient the instructions for the use of antibiotics | 1.686 | 0.120 | <0.001 | 0.772 |
| Q17. When you buy antibiotics, the pharmacist tells you about the importance of correct therapeutic compliance/adherence | 0.751 | 0.117 | <0.001 | 0.319 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mallah, N.; Rodríguez-Cano, R.; Badro, D.A.; Figueiras, A.; Gonzalez-Barcala, F.-J.; Takkouche, B. Development and Validation of a Knowledge, Attitude and Practice Questionnaire on Antibiotic Use in Arabic and French Languages in Lebanon. Int. J. Environ. Res. Public Health 2022, 19, 687. https://doi.org/10.3390/ijerph19020687
Mallah N, Rodríguez-Cano R, Badro DA, Figueiras A, Gonzalez-Barcala F-J, Takkouche B. Development and Validation of a Knowledge, Attitude and Practice Questionnaire on Antibiotic Use in Arabic and French Languages in Lebanon. International Journal of Environmental Research and Public Health. 2022; 19(2):687. https://doi.org/10.3390/ijerph19020687
Chicago/Turabian StyleMallah, Narmeen, Rubén Rodríguez-Cano, Danielle A. Badro, Adolfo Figueiras, Francisco-Javier Gonzalez-Barcala, and Bahi Takkouche. 2022. "Development and Validation of a Knowledge, Attitude and Practice Questionnaire on Antibiotic Use in Arabic and French Languages in Lebanon" International Journal of Environmental Research and Public Health 19, no. 2: 687. https://doi.org/10.3390/ijerph19020687
APA StyleMallah, N., Rodríguez-Cano, R., Badro, D. A., Figueiras, A., Gonzalez-Barcala, F.-J., & Takkouche, B. (2022). Development and Validation of a Knowledge, Attitude and Practice Questionnaire on Antibiotic Use in Arabic and French Languages in Lebanon. International Journal of Environmental Research and Public Health, 19(2), 687. https://doi.org/10.3390/ijerph19020687







