Social Support Mediates the Association between Health Anxiety and Quality of Life: Findings from a Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. The Quality of Life Scale (QOLS)
2.2.2. The Short Health Anxiety Inventory (SHAI)
2.2.3. Cyberchondria Severity Scale (CSS)
2.2.4. The Multidimensional Scale of Perceived Social Support (MSPSS)
2.3. Statistics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Revicki, D.; Osoba, D.; Fairclough, D.; Barofsky, I.; Berzon, R.; Leidy, N.; Rothman, M. Recommendations on health-related quality of life research to support labeling and promotional claims in the United States. Qual. Life Res. 2000, 9, 887–900. [Google Scholar] [CrossRef]
- Dantas, R.A.S.; Ciol, M.A. Flanagan Quality of Life Scale. In Encyclopedia of Quality of Life and Well-Being Research; Michalos, A.C., Ed.; Springer: Dordrecht, The Netherlands, 2014. [Google Scholar] [CrossRef]
- WHOQOL: Measuring Quality of Life; World Health Organization: Geneva, Switzerland, 2020.
- Phyo, A.Z.Z.; Freak-Poli, R.; Craig, H.; Gasevic, D.; Stocks, N.P.; Gonzalez-Chica, D.A.; Ryan, J. Quality of life and mortality in the general population: A systematic review and meta-analysis. BMC Public Health 2020, 20, 1596. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Measuring Healthy Days: Population Assessment of Health-Related Quality of Life; CDC: Atlanta, GA, USA, 2000. [Google Scholar]
- Centers for Disease Control and Prevention. Healthy People 2020. 2019. Available online: https://www.cdc.gov/nchs/healthy_people/hp2020.htm (accessed on 14 August 2019).
- World Health Organization. International Classification of Functioning, Disability, and Health: Children and Youth Version: ICF-CY; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Abdelghani, M.; Mahdy, R.; El-Gohari, H. Health anxiety to COVID-19 virus infection and its relationship to quality of life in a sample of health care workers in Egypt: A cross-sectional study. Arch. Psychiatry Psychother. 2021, 23, 19–28. [Google Scholar] [CrossRef]
- Taylor, S.; McKay, D.; Abramowitz, J.S. Hypochondriasis and health-related anxiety. In Handbook of Evidence-Based Practice in Clinical Psychology; Sturney, P., Hereson, M., Eds.; Wiley: New York, NY, USA, 2012; Volume 2, pp. 603–619. [Google Scholar]
- Olatunji, B.O.; Etzel, E.N.; Tomarken, A.J.; Ciesielski, B.G.; Deacon, B. The effects of safety behaviors on health anxiety: An experimental investigation. Behav. Res. Ther. 2011, 49, 719–728. [Google Scholar] [CrossRef]
- Özmete, E.; Pak, M. The Relationship between Anxiety Levels and Perceived Social Support during the Pandemic of COVID-19 in Turkey. Soc. Work Public Health 2020, 35, 603–616. [Google Scholar] [CrossRef]
- Sarason, B.R.; Sarason, I.G.; Pierce, G.R. (Eds.) Traditional views of social support and their impact on assessment. In Social Support: An interactional view; Wiley-Interscience: New York, NY, USA, 1990; pp. 9–25. [Google Scholar]
- Haber, M.G.; Cohen, J.L.; Lucas, T.; Baltes, B. The relationship between self-reported received and perceived social support: A meta-analytic review. Am. J. Community Psychol. 2007, 39, 133–144. [Google Scholar] [CrossRef]
- Lakey, B.; Orehek, E.; Hain, K.L.; Vanvleet, M. Enacted support’s links to negative affect isolated from trait influences. Personal. Soc. Psychol. Bull. 2010, 36, 132–142. [Google Scholar]
- Barrera, M. Distinctions between social support concepts, measures, and models. Am. J. Community Psychol. 1986, 14, 413–445. [Google Scholar]
- Lakey, B.; Lutz, C.J. Social support and preventive and therapeutic interventions. In Handbook of Social Support and the Family; Pierce, G.R., Sarason, B.R., Sarason, I.G., Eds.; Plenum: New York, NY, USA, 1996; pp. 435–465. [Google Scholar]
- Gupta, R.; Dhamija, R.K. Covid-19: Social distancing or social isolation? BMJ 2020, 369, m2399. [Google Scholar] [CrossRef]
- Douglas, M.; Katikireddi, S.V.; Taulbut, M.; McKee, M.; McCartney, G. Mitigating the wider health effects of covid-19 pandemic response. BMJ 2020, 369, m1557. [Google Scholar] [CrossRef]
- Razai, M.S.; Oakeshott, P.; Kankam, H.; Galea, S.; Stokes-Lampard, H. Mitigating the psychological effects of social isolation during the covid-19 pandemic. BMJ 2020, 369, m1904. [Google Scholar] [CrossRef]
- Dour, H.J.; Wiley, J.F.; Roy-Byrne, P.; Stein, M.B.; Sullivan, G.; Sherbourne, C.D.; Bystritsky, A.; Rose, R.D.; Craske, M.G. Perceived Social Support Mediates Anxiety and Depressive Symptom Changes following Primary Care Intervention. Depress. Anxiety 2014, 31, 436–442. [Google Scholar] [CrossRef]
- Warwick, H.M.; Salkovskis, P.M. Hypochondriasis. Behav. Res. Ther. 1990, 28, 105–117. [Google Scholar] [CrossRef]
- Chung, M.L.; Moser, D.K.; Lennie, T.A.; Frazier, S.K. Perceived social support predicted quality of life in patients with heart failure, but the effect is mediated by depressive symptoms. Qual. Life Res. 2013, 22, 1555–1563. [Google Scholar] [CrossRef]
- Al-Dmour, H.; Masa’Deh, R.; Salman, A.; Abuhashesh, M.; Al-Dmour, R. Influence of Social Media Platforms on Public Health Protection Against the COVID-19 Pandemic via the Mediating Effects of Public Health Awareness and Behavioral Changes: Integrated Model. J. Med. Internet Res. 2020, 22, e19996. [Google Scholar] [CrossRef]
- Stuart, J.; O’Donnell, K.; O’Donnell, A.; Scott, R.; Barber, B. Online Social Connection as a Buffer of Health Anxiety and Isolation During COVID-19. Cyberpsychol. Behav. Soc. Netw. 2021, 24, 521–525. [Google Scholar] [CrossRef]
- Xu, J.; Ou, J.; Luo, S.; Wang, Z.; Chang, E.; Novak, C.; Shen, J.; Zheng, S.; Wang, Y. Perceived Social Support Protects Lonely People Against COVID-19 Anxiety: A Three-Wave Longitudinal Study in China. Front. Psychol. 2020, 11, 566965. [Google Scholar] [CrossRef]
- Vismara, M.; Vitella, D.; Biolcati, R.; Ambrosini, F.; Pirola, V.; Dell’Osso, B.; Truzoli, R. The Impact of COVID-19 Pandemic on Searching for Health-Related Information and Cyberchondria on the General Population in Italy. Front. Psychiatry 2021, 12, 754870. [Google Scholar] [CrossRef]
- Starcevic, V.; Berle, D. Cyberchondria: Towards a better understanding of excessive health-related Internet use. Expert Rev. Neurother. 2013, 13, 205–213. [Google Scholar] [CrossRef]
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 2020, 15, e0231924. [Google Scholar] [CrossRef]
- Su, Z.; McDonnell, D.; Wen, J.; Kozak, M.; Abbas, J.; Šegalo, S.; Li, X.; Ahmad, J.; Cheshmehzangi, A.; Cai, Y.; et al. Mental health consequences of COVID-19 media coverage: The need for effective crisis communication practices. Glob. Health 2021, 17, 4. [Google Scholar] [CrossRef]
- Brown, R.J.; Skelly, N.; Chew-Graham, C.A. Online health research and health anxiety: A systematic review and conceptual integration. Clin. Psychol. Sci. Pr. 2020, 27, e12299. [Google Scholar] [CrossRef]
- Vismara, M.; Caricasole, V.; Starcevic, V.; Cinosi, E.; Dell’Osso, B.; Martinotti, G.; Fineberg, N.A. Is cyberchondria a new transdiagnostic digital compulsive syndrome? A systematic review of the evidence. Compr. Psychiatry 2020, 99, 152167. [Google Scholar] [CrossRef]
- McMullan, R.D.; Berle, D.; Arnáez, S.; Starcevic, V. The relationships between health anxiety, online health information seeking, and cyberchondria: Systematic review and meta-analysis. J. Affect. Disord. 2019, 245, 270–278. [Google Scholar] [CrossRef]
- Menon, V.; Kar, S.K.; Tripathi, A.; Nebhinani, N.; Varadharajan, N. Cyberchondria: Conceptual relation with health anxiety, assessment, management and prevention. Asian J. Psychiatry 2020, 53, 102225. [Google Scholar] [CrossRef]
- Nadeem, F.; Malik, N.I.; Atta, M.; Ullah, I.; Martinotti, G.; Pettorruso, M.; Vellante, F.; Di Giannantonio, M.; De Berardis, D. Relationship between Health-Anxiety and Cyberchondria: Role of Metacognitive Beliefs. J. Clin. Med. 2022, 11, 2590. [Google Scholar] [CrossRef]
- Eastin, M.S.; Guinsler, N.M. Worried and Wired: Effects of Health Anxiety on Information-Seeking and Health Care Utilization Behaviors. Cyberpsychol. Behav. 2006, 9, 494–498. [Google Scholar] [CrossRef]
- Starcevic, V.; Berle, D. Cyberchondria: An old phenomenon in a new guise? In Mental Health in the Digital Age: Grave Dangers, Great Promise; Aboujaoude, E., Starcevic, V., Eds.; Oxford University Press: New York, NY, USA, 2015; pp. 106–117. [Google Scholar]
- Andreassen, H.K.; Bujnowska-Fedak, M.M.; Chronaki, C.E.; Dumitru, R.C.; Pudule, I.; Santana, S.; Voss, H.; Wynn, R. European citizens’ use of E-health services: A study of seven countries. BMC Public Health 2007, 7, 53. [Google Scholar] [CrossRef]
- Doherty-Torstrick, E.R.; Walton, K.E.; Fallon, B.A. Cyberchondria: Parsing Health Anxiety from Online Behavior. J. Psychosom. Res. 2016, 57, 390–400. [Google Scholar] [CrossRef]
- Bajcar, B.; Babiak, J.; Olchowska-Kotala, A. Cyberchondria and its measurement. The Polish adaptation and psychometric properties of Cyberchondria Severity Scale CSS-PL. Psychiatr. Pol. 2019, 53, 49–60. [Google Scholar] [CrossRef]
- El-Gabalawy, R.; Mackenzie, C.; Thibodeau, M.; Asmundson, G.; Sareen, J. Health anxiety disorders in older adults: Conceptualizing complex conditions in late life. Clin. Psychol. Rev. 2013, 33, 1096–1105. [Google Scholar] [CrossRef]
- Cao, S.; Zhu, Y.; Li, P.; Zhang, W.; Ding, C.; Yang, D. Age Difference in Roles of Perceived Social Support and Psychological Capital on Mental Health During COVID-19. Front. Psychol. 2022, 13, 801241. [Google Scholar] [CrossRef]
- Zhang, X.B.; Xiao, W.; Lei, J.; Li, M.X.; Wang, X.; Hong, Y.J.; Xu, P.; Sun, J. Prevalence and influencing factors of anxiety and depression symptoms among the first-line medical staff in Wuhan mobile cabin hospital during the COVID-19 epidemic: A cross-sectional survey. Medicine 2021, 100, 4450. [Google Scholar]
- Özdin, S.; Bayrak, Ö.Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int. J. Soc. Psychiatry 2020, 66, 504–511. [Google Scholar]
- Atkinson, N.L.; Saperstein, S.L.; Pleis, J. Using the Internet for Health-Related Activities: Findings from a National Probability Sample. J. Med. Internet Res. 2009, 11, e4. [Google Scholar] [CrossRef]
- Barke, A.; Bleichhardt, G.; Rief, W.; Doering, B.K. The Cyberchondria Severity Scale (CSS): German Validation and Development of a Short Form. Int. J. Behav. Med. 2016, 23, 595–605. [Google Scholar] [CrossRef]
- Mathes, B.; Norr, A.; Allan, N.P.; Albanese, B.J.; Schmidt, N.B. Cyberchondria: Overlap with health anxiety and unique relations with impairment, quality of life, and service utilization. Psychiatry Res. 2018, 261, 204–211. [Google Scholar] [CrossRef]
- Shailaja, B.; Shetty, V.; Chaudhury, S.; Thyloth, M. Exploring cyberchondria and its associations in dental students amid COVID-19 infodemic. Ind. Psychiatry J. 2020, 29, 257–267. [Google Scholar] [CrossRef]
- Rahme, C.; Akel, M.; Obeid, S.; Hallit, S. Cyberchondria severity and quality of life among Lebanese adults: The mediating role of fear of COVID-19, depression, anxiety, stress and obsessive–compulsive behavior—A structural equation model approach. BMC Psychol. 2021, 9, 169. [Google Scholar] [CrossRef]
- Ambrosini, F.; Truzoli, R.; Vismara, M.; Vitella, D.; Biolcati, R. The effect of cyberchondria on anxiety, depression and quality of life during COVID-19: The mediational role of obsessive-compulsive symptoms and Internet addiction. Heliyon 2022, 8, e09437. [Google Scholar] [CrossRef]
- Computer-Assisted and Online Data Collection in General Population Surveys. Available online: https://www.emcdda.europa.eu/system/files/publications/808/Technical_report_Computer_assisted_and_online_data_collection_in_GPS_480810.pdf (accessed on 29 December 2021).
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Prev. Med. 2007, 45, 247–251. [Google Scholar]
- Burckhardt, C.S.; Anderson, K.L. The Quality of Life Scale (QOLS): Reliability, Validity, and Utilization. Health Qual. Life Outcomes 2003, 1, 60. [Google Scholar] [CrossRef]
- Quality of Life Scale. Available online: https://eprovide.mapi-trust.org/instruments/quality-of-life-scale2 (accessed on 29 December 2021).
- Kocjan, J. Evaluation of psychometric properties and factor structure of the Polish version of Short Health Anxiety Inventory (SHAI). Arch. Psychiatry Psychother. 2016, 18, 68–78. [Google Scholar] [CrossRef]
- Salkovskis, P.M.; Rimes, K.A.; Warwick, H.M.C.; Clark, D.M. The Health Anxiety Inventory: Development and validation of scales for the measurement of health anxiety and hypochon- driasis. Psychol Med. 2002, 32, 843–853. [Google Scholar]
- McElroy, E.; Shevlin, M. The development and initial validation of the cyberchondria severity scale (CSS). J. Anxiety Disord. 2014, 28, 259–265. [Google Scholar] [CrossRef]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Persinal. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Krystyna, B.; Hanna, P.-B. Polska adaptacja wielowymiarowej skali spostrzeganego wsparcia społecznego. Pol. Forum Psychol. 2017, 4, 581–599. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; The Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Field, A. Discovering Statistics Using SPSS, 3rd ed.; Sage Publications: Thousand Oaks, CA, USA, 2009. [Google Scholar]
- Hair, J.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson Education International: Upper Saddle River, NJ, USA, 2010. [Google Scholar]
- Nie, N.H.; Bent, D.H.; Hull, C.H. SPSS: Statistical Package for the Social Sciences; McGraw-Hill: New York, NY, USA, 1970. [Google Scholar]
- Arsenakis, S.; Chatton, A.; Penzenstadler, L.; Billieux, J.; Berle, D.; Starcevic, V.; Viswasam, K.; Khazaal, Y. Unveiling the relationships between cyberchondria and psychopathological symptoms. J. Psychiatr. Res. 2021, 143, 254–261. [Google Scholar] [CrossRef]
- Heinen, A.; Varghese, S.; Krayem, A.; Molodynski, A. Understanding health anxiety in the COVID-19 pandemic. Int. J. Soc. Psychiatry 2021, 25, 207640211057794. [Google Scholar] [CrossRef]
- Manu, P.; Affleck, G.; Tennen, H.; Morse, P.A.; Escobar, J.I. Hypochondriasis Influences Quality-of-Life Outcomes in Patients with Chronic Fatigue. Psychother. Psychosom. 1996, 65, 76–81. [Google Scholar] [CrossRef]
- Macy, A.S.; Theo, J.N.; Kaufmann, S.C.V.; Ghazzaoui, R.B.; Pawlowski, P.A.; Fakhry, H.I.; Cassmassi, B.J.; IsHak, W. Quality of life in obsessive compulsive disorder. CNS Spectr. 2013, 18, 21–33. [Google Scholar] [CrossRef]
- Barrera, T.L.; Norton, P.J. Quality of life impairment in generalized anxiety disorder, social phobia, and panic disorder. J. Anxiety Disord. 2009, 23, 1086–1090. [Google Scholar] [CrossRef]
- Noroozi, F.; Hassanipour, S.; Eftekharian, F.; Eisapareh, K.; Kaveh, M.H. Internet Addiction Effect on Quality of Life: A Systematic Review and Meta-Analysis. Sci. World J. 2021, 2021, 2556679. [Google Scholar] [CrossRef]
- Salkovskis, P.M.; Warwick, H.M. Morbid preoccupations, health anxiety and reassurance: A cognitive-behavioural approach to hypochondriasis. Behav. Res. Ther. 1986, 24, 597–602. [Google Scholar] [CrossRef]
- White, R.W.; Horvitz, E. Experiences with Web search on medical concerns and self-diagnosis. In Proceedings from the American Medical Informatics Association Annual Symposium 2009 (AMIA 2009); Curran Associates: Red Hook, NY, USA, 2009; pp. 696–700. [Google Scholar]
- Taylor, S.E.; Klein, L.C.; Lewis, B.P.; Gruenewald, T.L.; Gurung, R.A.R.; Updegraff, J.A. Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychol. Rev. 2000, 107, 411–429. [Google Scholar] [CrossRef]
- Miller, G.E.; Blackwell, E. Turning Up the Heat. Curr. Dir. Psychol. Sci. 2006, 15, 269–272. [Google Scholar] [CrossRef]
- Cohen, S. Social relationships and health. Am. Psychol. 2004, 59, 676–684. [Google Scholar]
- Terzi, Ş. The relationship between the psychological endurance of university students and the social support they perceive. Turk. Psychol. Couns. Guid. J. 2008, 3, 1–11. [Google Scholar]
- Janowski, K.; Tatala, M.; Jedynak, T.; Księżopolska, A.; Głowacka, B. Wsparcie społeczne a ocena własnej choroby, nasilenie objawów depresyjnych i akceptacja życia z chorobą u kobiet po mastektomii. Pol. Forum Psychol. 2016, 21, 188–205. [Google Scholar]
- Matud, M.P.; Ibáñez, I.; Bethencourt, J.M.; Marrero, R.; Carballeira, M. Structural gender differences in perceived social support. Pers. Individ. Differ. 2003, 35, 1919–1929. [Google Scholar] [CrossRef]
- Harding, K.J.; Skritskaya, N.; Doherty, E.; Fallon, B.A. Advances in understanding illness anxiety. Curr. Psychiatry Rep. 2008, 10, 311–317. [Google Scholar] [CrossRef]
- Singh, K.; Fox, J.R.E.; Brown, R.J. Health anxiety and Internet use: A thematic analysis. Cyberpsychol. J. Psychosoc. Res. Cyberspace 2016, 10, 4. [Google Scholar] [CrossRef]
- Poel, F.T.; Baumgartner, S.E.; Hartmann, T.; Tanis, M. The curious case of cyberchondria: A longitudinal study on the reciprocal relationship between health anxiety and online health information seeking. J. Anxiety Disord. 2016, 43, 32–40. [Google Scholar] [CrossRef]
- De la Cuesta, J.; Catedrilla, J.; Ebardo, R.; Limpin, L.; Leaño, C.; Trapero, H. Personality traits of future nurses and cyberchondria: Findings from an emerging economy. In Proceedings of the ICCE 2019—27th International Conference on Computers in Education, Kenting, Taiwan, 19 November 2019; Volume 2, pp. 274–279. Available online: https://animorepository.dlsu.edu.ph/faculty_research/712 (accessed on 5 January 2022).
- Bajcar, B.; Babiak, J. Neuroticism and cyberchondria: The mediating role of intolerance of uncertainty and defensive pessimism. Pers. Individ. Differ. 2020, 162, 110006. [Google Scholar] [CrossRef]
| Variable | n (%) | Mean ± SD | Median (Range) | Skewness | Kurtosis | Kolmogorov–Smirnov Test |
|---|---|---|---|---|---|---|
| Age, years | 36.65 ± 12.55 | 34.0 (59.0) | 0.768 | −0.006 | p < 0.001 | |
| Gender, males | 100 (18.6) | |||||
| Education, higher | 422 (78.4) | |||||
| CSS-PL total score | 60.90 ± 17.58 | 57.5 (99.0) | 0.817 | 0.643 | p = 0.191 | |
| SHAI total score | 15.53 ± 8.80 | 14.0 (51.0) | 1.104 | 1.693 | p = 0.103 | |
| MSPSS total score | 70.23 ± 15.75 | 76.0 (72.0) | −1.408 | 1.709 | p = 0.058 | |
| QOLS total score | 79.67 ± 15.13 | 80.5 (91.0) | −0.660 | 0.991 | p = 0.088 |
| General (n = 538) | Females (n = 438) | Males (n = 100) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | 2. | 3. | 4. | 5. | 1. | 2. | 3. | 4. | 5. | 1. | 2. | 3. | 4. | 5. | |
| 1.Age | 1 | 1 | 1 | ||||||||||||
| 2.SHAI | −0.048 | 1 | −0.061 | 1 | −0.072 | 1 | |||||||||
| 3.MSPSS | −0.015 | −0.333 ** | 1 | −0.029 | −0.331 ** | 1 | 0.156 | −0.190 | 1 | ||||||
| 4.CSS | 0.066 | 0.574 ** | −0.141 ** | 1 | 0.031 | 0.627 ** | −0.113 * | 1 | 0.010 | 0.662 ** | −0.024 | 1 | |||
| 5.QOLS | 0.161 ** | −0.439 ** | 0.501 ** | −0.199 ** | 1 | 0.154 ** | −0.453 ** | 0.523 ** | −0.170 ** | 1 | 0.254 * | −0.331 ** | 0.480 ** | −0.282 ** | 1 |
| Higher Education (n = 422) | Other Education (n = 422) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | 2. | 3. | 4. | 5. | 1. | 2. | 3. | 4. | 5. | |
| 1.Age | 1 | 1 | ||||||||
| 2.SHAI | −0.053 | 1 | −0.041 | 1 | ||||||
| 3.MSPSS | 0.038 | −0.263 ** | 1 | −0.142 | −0.363 ** | 1 | ||||
| 4.CSS | 0.041 | 0.612 ** | −0.084 | 1 | 0.003 | 0.743 ** | −0.191 * | 1 | ||
| 5.QOLS | 0.163 ** | −0.382 ** | 0.465 ** | −0.153 ** | 1 | 0.128 | 0.560 ** | 0.542 ** | −0.415 ** | 1 |
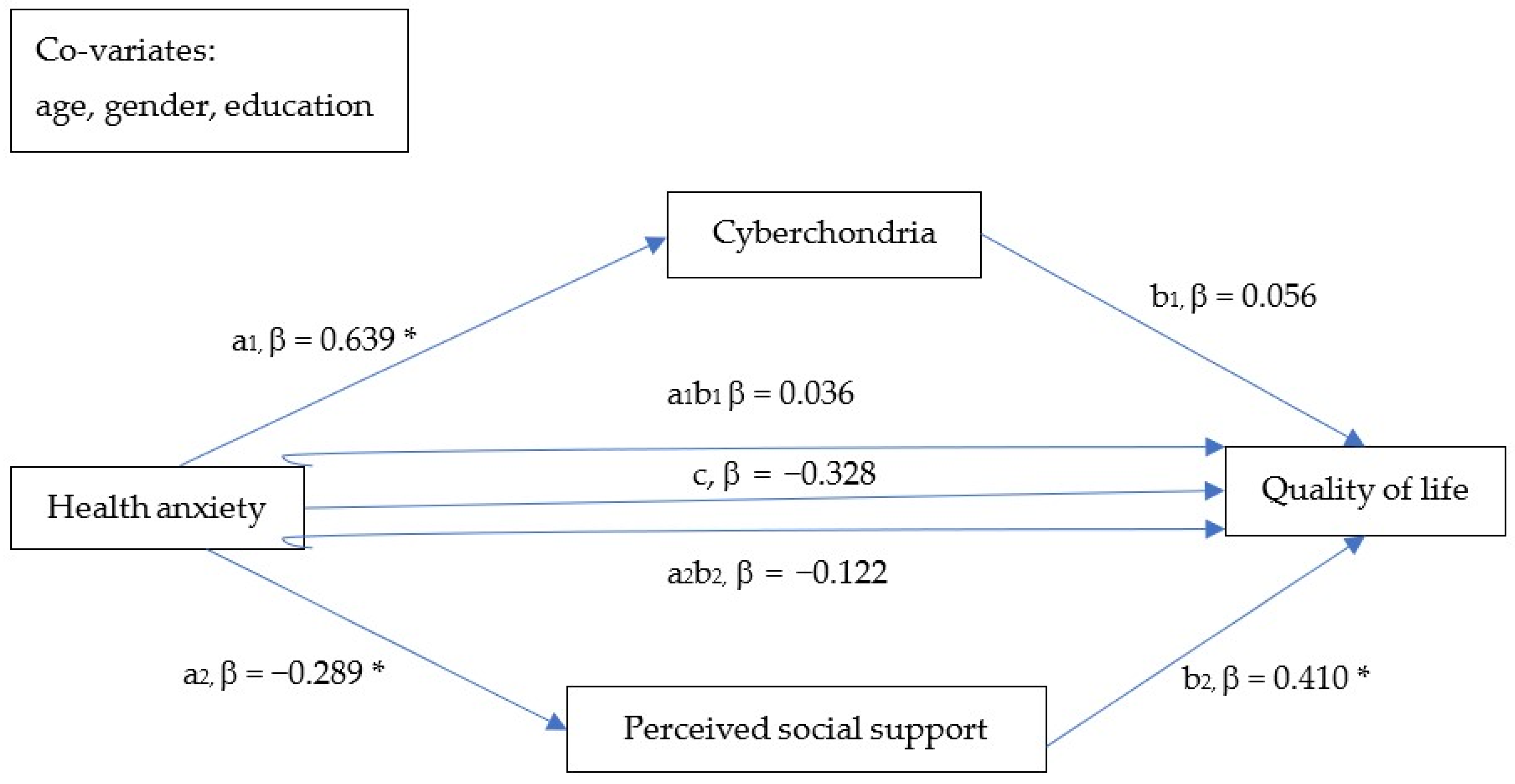
| β | SE | 95% CI | ||
|---|---|---|---|---|
| LLCI | ULCI | |||
| Direct effect of SHAI on CSS (a1) | 0.639 * | 0.034 | 0.573 | 0.705 |
| Direct effect of SHAI on MSPSS (a2) | −0.298 * | 0.042 | −0.380 | −0.217 |
| Direct effect of CSS on QoL (b1) | 0.056 | 0.045 | −0.032 | 0.144 |
| Direct effect of MSPSS on QoL (b2) | 0.410 * | 0.036 | 0.338 | 0.481 |
| Direct effect of SHAI on QoL (c) | −0.328 * | 0.047 | −0.421 | −0.236 |
| Indirect effect (through CSS) of SHAI on QoL (a1b1) | 0.036 | 0.030 | −0.025 | 0.095 |
| Indirect effect (through MSPSS) of SHAI on QoL (a2b2) | −0.122 * | 0.025 | −0.175 | −0.078 |
| Total indirect effect of SHAI on QoL (a1b1 + a2b2) | 0.086 * | 0.041 | −0.167 | −0.009 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciułkowicz, M.; Misiak, B.; Szcześniak, D.; Grzebieluch, J.; Maciaszek, J.; Rymaszewska, J. Social Support Mediates the Association between Health Anxiety and Quality of Life: Findings from a Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 12962. https://doi.org/10.3390/ijerph191912962
Ciułkowicz M, Misiak B, Szcześniak D, Grzebieluch J, Maciaszek J, Rymaszewska J. Social Support Mediates the Association between Health Anxiety and Quality of Life: Findings from a Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(19):12962. https://doi.org/10.3390/ijerph191912962
Chicago/Turabian StyleCiułkowicz, Marta, Błażej Misiak, Dorota Szcześniak, Jolanta Grzebieluch, Julian Maciaszek, and Joanna Rymaszewska. 2022. "Social Support Mediates the Association between Health Anxiety and Quality of Life: Findings from a Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 19: 12962. https://doi.org/10.3390/ijerph191912962
APA StyleCiułkowicz, M., Misiak, B., Szcześniak, D., Grzebieluch, J., Maciaszek, J., & Rymaszewska, J. (2022). Social Support Mediates the Association between Health Anxiety and Quality of Life: Findings from a Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(19), 12962. https://doi.org/10.3390/ijerph191912962







