Forecasting Hospital Visits Due to Influenza Based on Emergency Department Visits for Fever: A Feasibility Study on Emergency Department-Based Syndromic Surveillance
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Settings and Study Population
2.2. Statistical Analyses
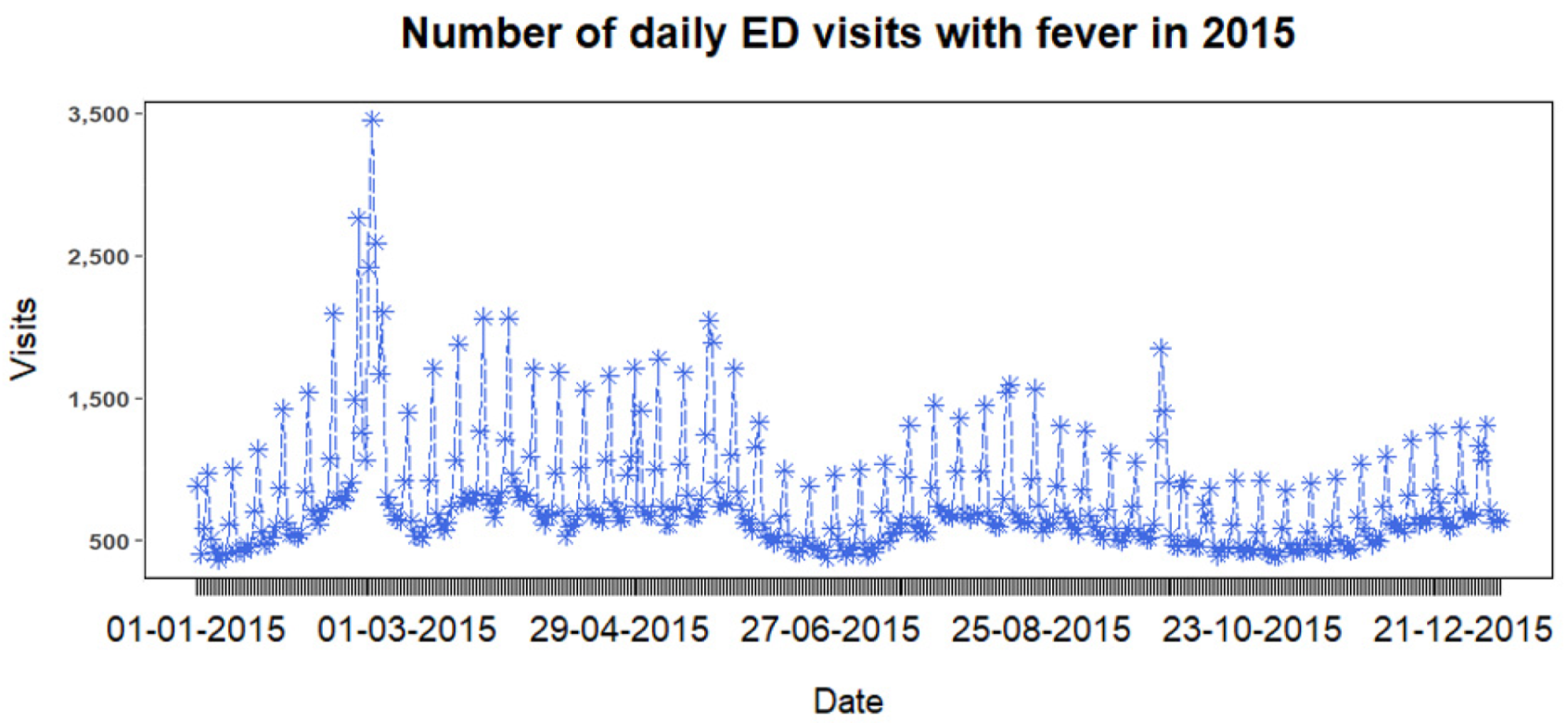
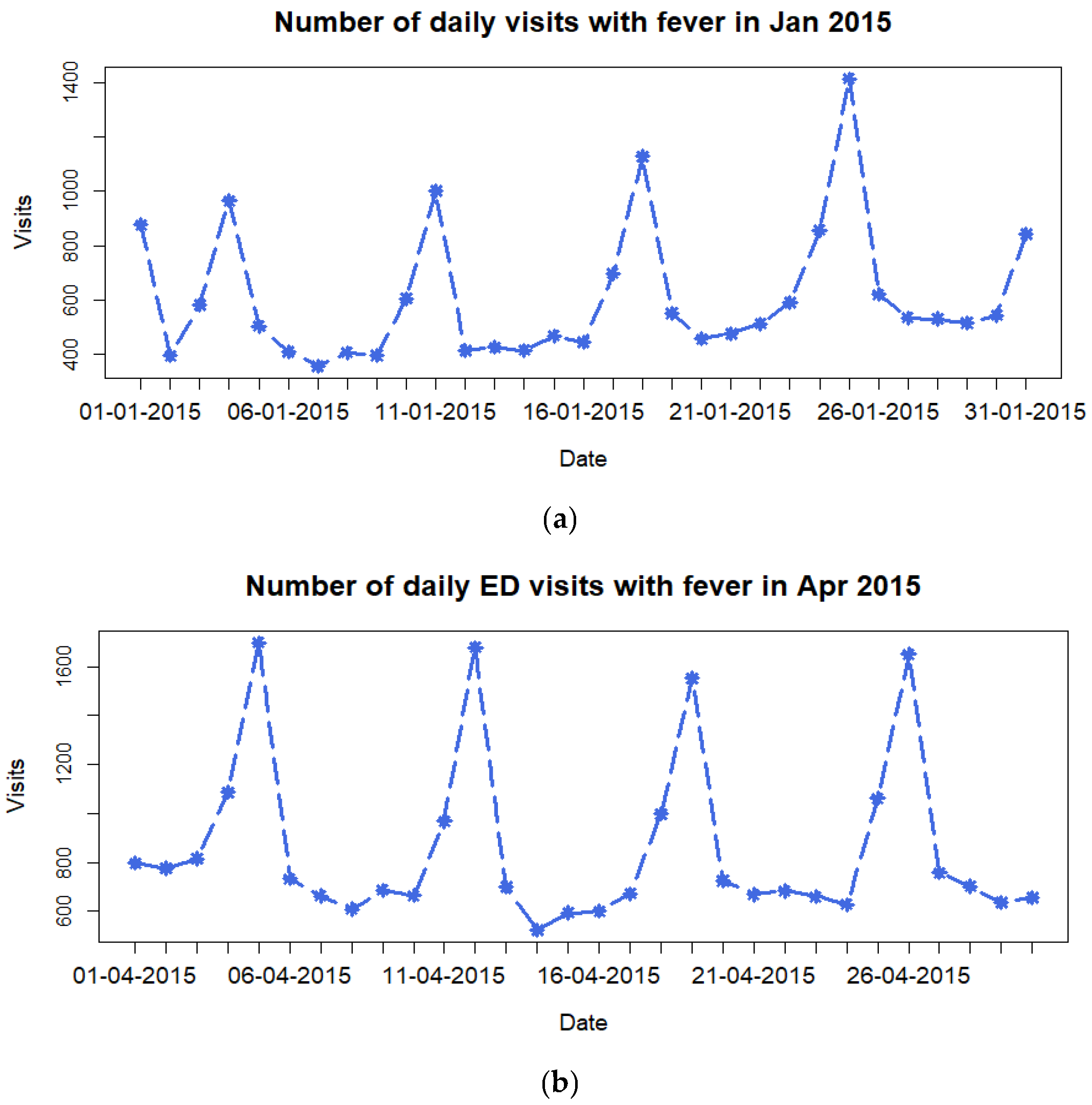
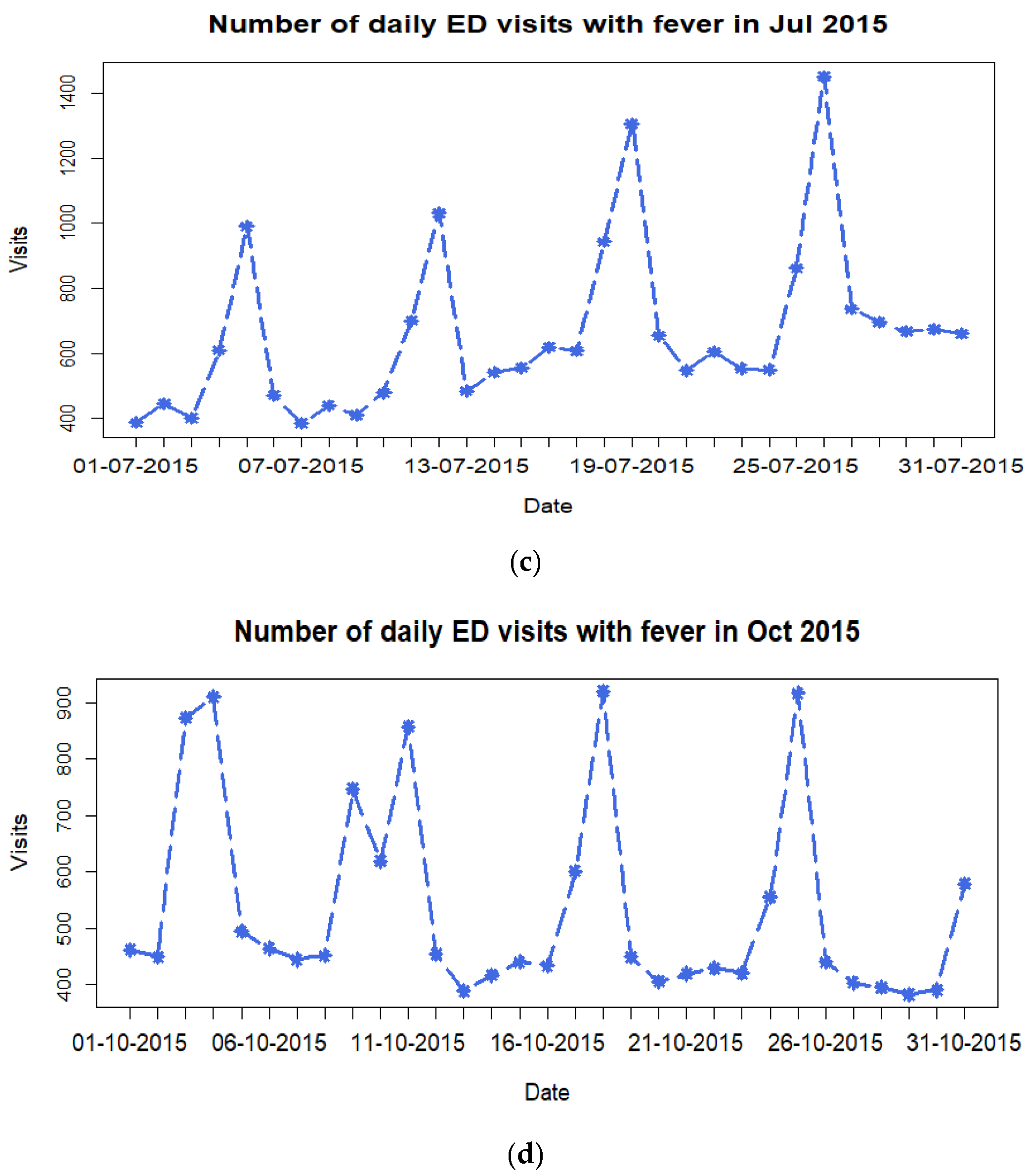
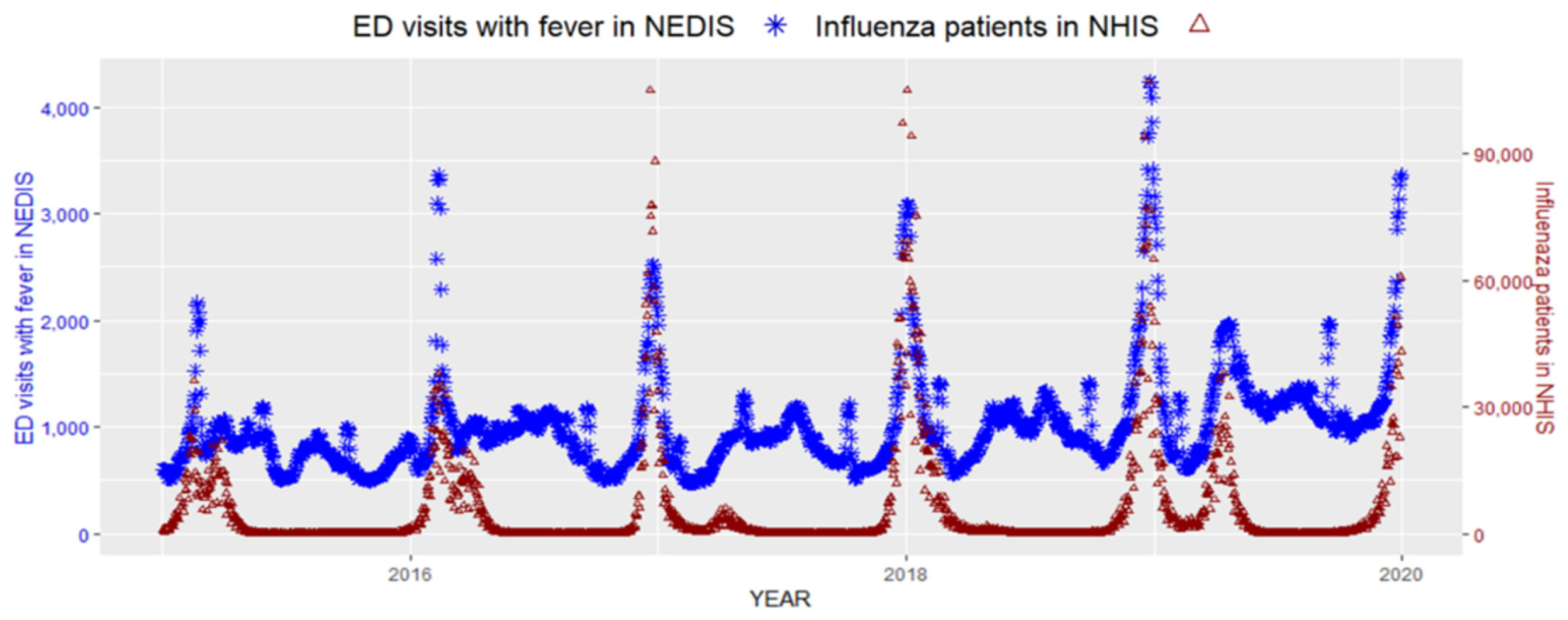
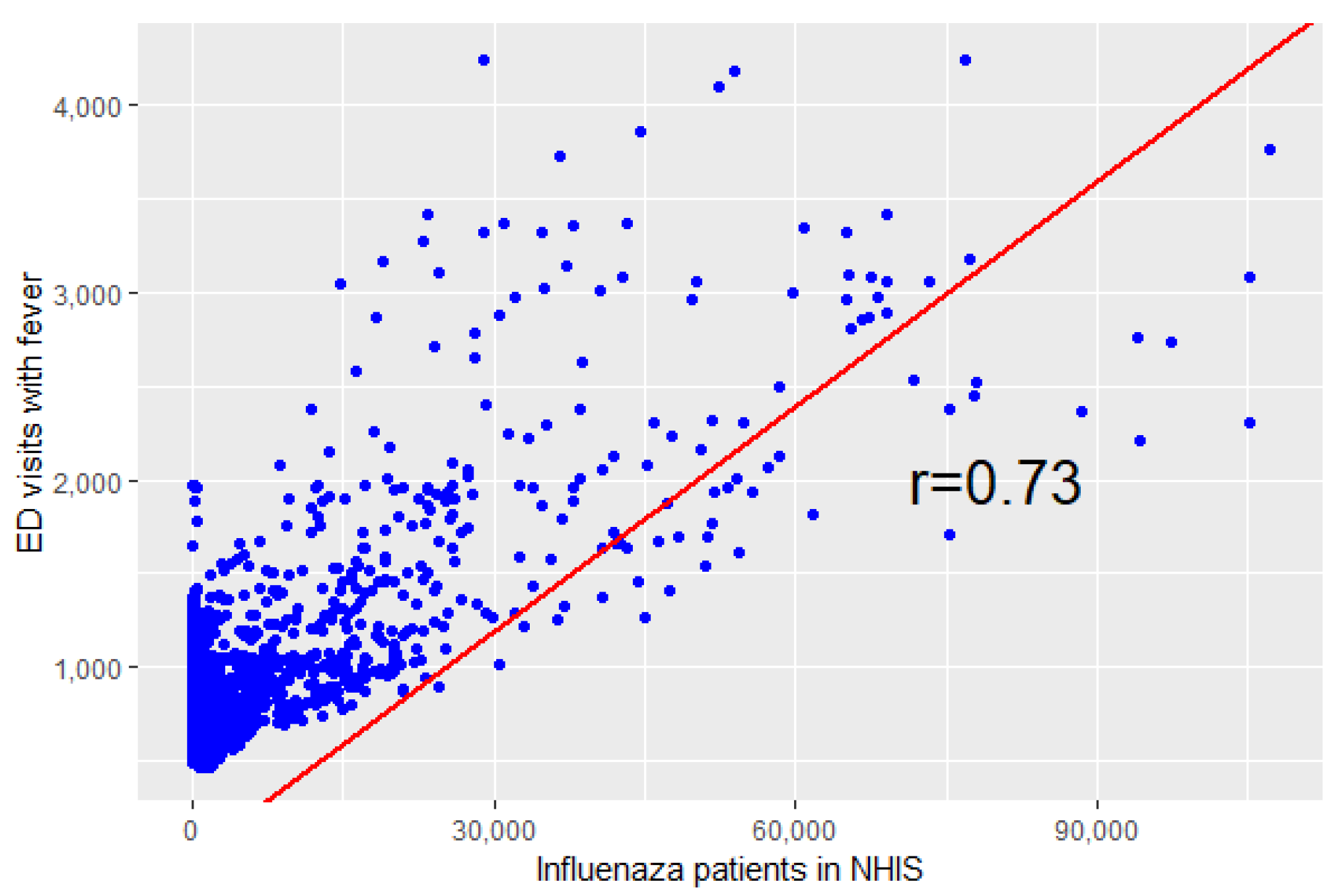
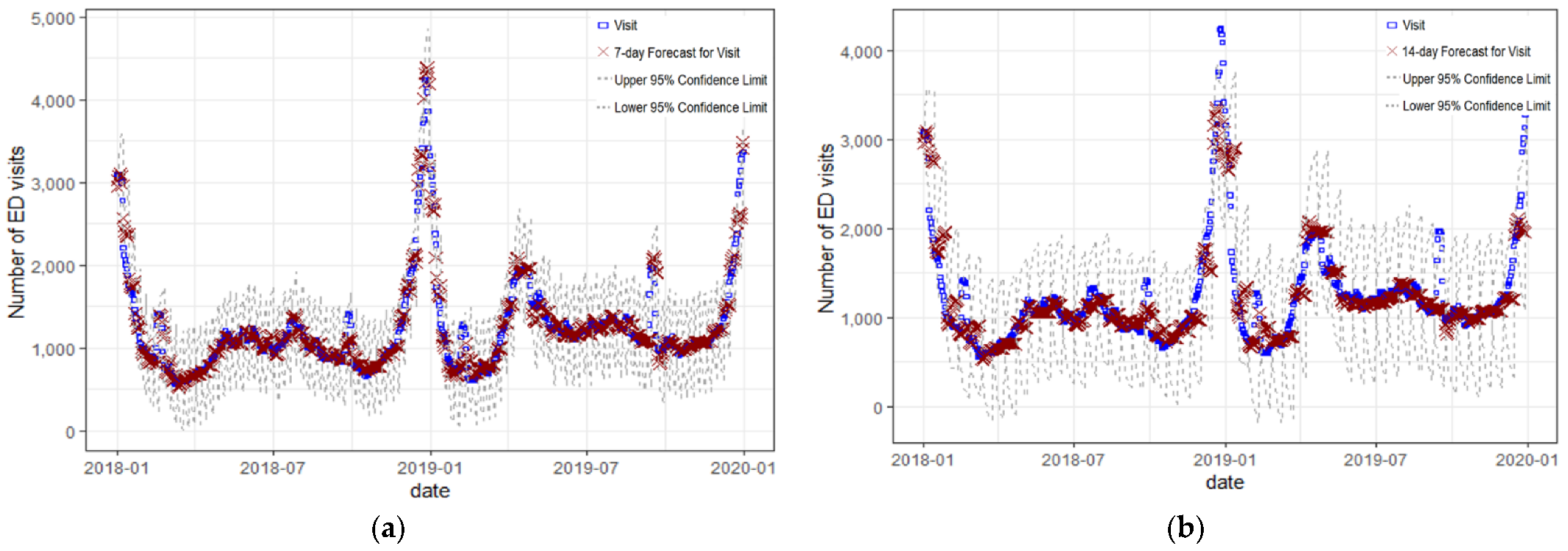
3. Results
| Parameter | Estimate | Standard Error | t Value | Approximate Pr > |t| | Lag |
|---|---|---|---|---|---|
| MA1,1 | 0.45215 | 0.02936 | 15.4 | <0.0001 | 7 |
| MA2,1 | −0.21127 | 0.03849 | −5.49 | <0.0001 | 1 |
| AR1,1 | 0.67686 | 0.02949 | 22.95 | <0.0001 | 1 |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix B
References
- Boktor, S.W.; Hafner, J.W. Influenza; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Macias, A.E.; McElhaney, J.E.; Chaves, S.S.; Nealon, J.; Nunes, M.C.; Samson, S.I.; Seet, B.T.; Weinke, T.; Yu, H. The disease burden of influenza beyond respiratory illness. Vaccine 2020, 39 (Suppl. 1), A6–A14. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Influenza Collaborators. Mortality, morbidity, and hospitalisations due to influenza lower respiratory tract infections, 2017: An analysis for the global burden of disease study 2017. Lancet Respir. Med. 2019, 7, 69–89. [Google Scholar] [CrossRef]
- Cozza, V.; Campbell, H.; Chang, H.H.; Iuliano, A.D.; Paget, J.; Patel, N.N.; Reiner, R.C.; Troeger, C.; Viboud, C.; Bresee, J.S.; et al. Global Seasonal Influenza Mortality Estimates: A Comparison of 3 Different Approaches. Am. J. Epidemiol. 2021, 190, 718–727. [Google Scholar] [CrossRef] [PubMed]
- Global Influenza Surveillance and Response System. 2022. Available online: https://www.who.int/news/item/03-02-2022-2022-celebrating-70-years-of-gisrs-(the-global-influenza-surveillance-and-response-system) (accessed on 18 September 2022).
- Charbonneau, D.H.; James, L.N. FluView and FluNet: Tools for Influenza Activity and Surveillance. Med. Ref. Serv. Q. 2019, 38, 358–368. [Google Scholar] [CrossRef]
- Simpson, R.B.; Gottlieb, J.; Zhou, B.; Hartwick, M.A.; Naumova, E.N. Completeness of open access FluNet influenza surveillance data for Pan-America in 2005–2019. Sci. Rep. 2021, 11, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Park Kwangsuk, P.S.; Donghyok, K.; Donghan, L. Influenza sentinel surveillance report in the republic of korea, 2018–2019. Public Health Wkly. Rep. 2019, 12, 2224–2232. [Google Scholar]
- Lee, C.-S. The diagnosis and treatment of influenza. J. Korean Med. Assoc. 2010, 43–51. [Google Scholar] [CrossRef][Green Version]
- Hiller, K.M.; Stoneking, L.; Min, A.; Rhodes, S.M. Syndromic Surveillance for Influenza in the Emergency Department–A Systematic Review. PLoS ONE 2013, 8, e73832. [Google Scholar] [CrossRef] [PubMed]
- National Emergency Medical Center, Korea. 2020 Emergency Medical Statistical Yearbook. 2021. Available online: https://www.e-gen.or.kr/nemc/statistics_annual_report.do (accessed on 3 October 2022).
- Heffernan, R.; Mostashari, F.; Das, D.; Karpati, A.; Kulldorff, M.; Weiss, D. Syndromic surveillance in public health practice, new york city. Emerg. Infect. Dis. 2004, 10, 858–864. [Google Scholar] [CrossRef]
- Olson, D.R.; Heffernan, R.T.; Paladini, M.; Konty, K.; Weiss, D.; Mostashari, F. Monitoring the Impact of Influenza by Age: Emergency Department Fever and Respiratory Complaint Surveillance in New York City. PLoS Med. 2007, 4, e247. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Choi, A.; Ryoo, H.W.; Pak, Y.-S.; Kim, H.C.; Kim, J.H. Changes in Clinical Characteristics among Febrile Patients Visiting the Emergency Department before and after the COVID-19 Outbreak. Yonsei Med. J. 2021, 62, 1136–1144. [Google Scholar] [CrossRef]
- DeWitt, S.; Chavez, S.A.; Perkins, J.; Long, B.; Koyfman, A. Evaluation of fever in the emergency department. Am. J. Emerg. Med. 2017, 35, 1755–1758. [Google Scholar] [CrossRef] [PubMed]
- Definitions of Symptoms for Reportable Illnesses. 2022. Available online: https://www.cdc.gov/quarantine/air/reporting-deaths-illness/definitions-symptoms-reportable-illnesses.html (accessed on 3 October 2022).
- Jeong, H.-S. Korea’s national health insurance—lessons from the past three decades. Health Aff. 2011, 30, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Byeon, K.H.; Kim, J.; Choi, B.Y.; Kim, J.Y.; Lee, N. Age-Period-Cohort Analysis of Influenza in Korean: The National Health Insurance Research Database, 2009–2018. J. Korean Med. Sci. 2020, 35, e121. [Google Scholar] [CrossRef]
- Hitzek, J.; Fischer-Rosinský, A.; Möckel, M.; Kuhlmann, S.L.; Slagman, A. Influence of Weekday and Seasonal Trends on Urgency and In-hospital Mortality of Emergency Department Patients. Front. Public Heal. 2022, 10, 711235. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.J.; Yoon, P.W.; Collins, J.M.; Davidson, A.J.; Mac Kenzie, W.R. Evaluation of Syndromic Surveillance Systems in 6 US State and Local Health Departments. J. Public Heal. Manag. Pr. 2018, 24, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Ginsberg, J.; Mohebbi, M.H.; Patel, R.S.; Brammer, L.; Smolinski, M.S.; Brilliant, L. Detecting influenza epidemics using search engine query data. Nature 2009, 457, 1012–1014. [Google Scholar] [CrossRef] [PubMed]
- Charles, L.; Reynolds, T.L.; Cameron, M.A.; Conway, M.; Lau, E.; Olsen, J.M.; Pavlin, J.A.; Shigematsu, M.; Streichert, L.; Suda, K.J.; et al. Using Social Media for Actionable Disease Surveillance and Outbreak Management: A Systematic Literature Review. PLoS ONE 2015, 10, e0139701. [Google Scholar] [CrossRef]
- Hughes, H.E.; Edeghere, O.; O’Brien, S.J.; Vivancos, R.; Elliot, A.J. Emergency department syndromic surveillance systems: A systematic review. BMC Public Health 2020, 20, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Yom-Tov, E. Active syndromic surveillance of COVID-19 in Israel. Sci. Rep. 2021, 11, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Güemes, A.; Ray, S.; Aboumerhi, K.; Desjardins, M.R.; Kvit, A.; Corrigan, A.E.; Fries, B.; Shields, T.; Stevens, R.D.; Curriero, F.C.; et al. A syndromic surveillance tool to detect anomalous clusters of COVID-19 symptoms in the United States. Sci. Rep. 2021, 11, 1–11. [Google Scholar] [CrossRef]
- Milyavsky, D.; Bachenheimer, E.; Eskin, B.; Allegra, J. 21 Monitoring the Incidence of COVID-19 Using Syndromic Surveillance of Emergency Department Visits. Ann. Emerg. Med. 2020, 76, S8–S9. [Google Scholar] [CrossRef]
- Beitel, A.J.; Olson, K.L.; Reis, B.Y.; Mandl, K.D. Use of Emergency Department Chief Complaint and Diagnostic Codes for Identifying Respiratory Illness in a Pediatric Population. Pediatr. Emerg. Care 2004, 20, 355–360. [Google Scholar] [CrossRef] [PubMed]
- May, L.S.; Griffin, B.A.; Bauers, N.M.; Jain, A.; Mitchum, M.; Sikka, N.; Carim, M.; Stoto, M.A. Emergency Department Chief Complaint and Diagnosis Data to Detect Influenza-Like Illness with an Electronic Medical Record. West. J. Emerg. Med. 2010, 11, 1–9. [Google Scholar] [PubMed]
- Kim, T.H.; Hong, K.J.; Shin, S.D.; Park, G.J.; Kim, S.; Hong, N. Forecasting respiratory infectious outbreaks using ED-based syndromic surveillance for febrile ED visits in a Metropolitan City. Am. J. Emerg. Med. 2019, 37, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Ahn, J.H.; Choi, S.C.; Kim, G.W.; Min, Y.G.; Park, R.W.; Jung, Y.S.; Cho, J.P. The applicability and usefulness of emergency department syndromic surveillance using a computed data source for epidemic keratoconjunctivitis and meningitis. J. Korean Soc. Emerg. Med. 2010, 21, 374–381. [Google Scholar]
- Ahn, S.; Lee, J.H.; Kim, W.; Lim, K.S. Analysis of the Korean Emergency Department Syndromic Surveillance System: Mass Type Acute Diarrheal Syndrome. Healthc. Inform. Res. 2010, 16, 177–184. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yoon, Y.-H.; Kim, J.-Y.; Choi, S.-H. Analysis of Patients with Acute Toxic Exposure between 2009 and 2013: Data from the Korea Health Insurance Review and Assessment Service and the National Emergency Department Information System. J. Korean Med. Sci. 2018, 33, e254. [Google Scholar] [CrossRef]
| Year | Total | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|---|---|---|---|---|---|
| Total ED visits | 29,142,229 | 5,359,831 | 5,823,780 | 5,813,188 | 5,998,742 | 6,146,688 |
| ED visits with chief complaint of fever | 2,447,446 (8.4%) | 398,237 (7.4%) | 505,334 (8.7%) | 419,465 (7.2%) | 544,454 (9.1%) | 579,956 (9.4%) |
| Body temperature ≥ 38.0°C at the ED | 7,298,957 (25.0%) | 1,346,799 (25.1%) | 1,609,449 (27.6%) | 1,458,243 (25.1%) | 1,545,582 (25.8%) | 1,338,884 (21.8%) |
| Both fever as a chief complaint and body temperature ≥ 38.0 °C at the ED | 1,880,308 (6.5%) | 285,230 (5.3%) | 374,006 (6.4%) | 322,237 (5.5%) | 429,432 (7.2%) | 469,403 (7.6%) |
| Patients with influenza in the NHIS | 11,182,104 | 1,141,514 | 2,772,409 | 1,489,343 | 3,505,807 | 2,273,031 |
| Number of Day in Forecast | 1-Day | 2-Day | 3-Day | 4-Day | 5-Day | 6-Day | 7-Day |
|---|---|---|---|---|---|---|---|
| MAPE(%) | 2.2813 | 3.4674 | 4.0205 | 4.6546 | 7.1822 | 8.5615 | 6.4605 |
| Number of Day in Forecast | Correlation Coefficient | p-Value |
|---|---|---|
| 1-day | 0.772 | <0.0001 |
| 2-day | 0.763 | <0.0001 |
| 3-day | 0.753 | <0.0001 |
| 4-day | 0.733 | <0.0001 |
| 5-day | 0.765 | <0.0001 |
| 6-day | 0.740 | <0.0001 |
| 7-day | 0.782 | <0.0001 |
| 8-day | 0.685 | <0.0001 |
| 9-day | 0.684 | <0.0001 |
| 10-day | 0.743 | <0.0001 |
| 11-day | 0.720 | <0.0001 |
| 12-day | 0.666 | <0.0001 |
| 13-day | 0.723 | <0.0001 |
| 14-day | 0.775 | <0.0001 |
| 15-day | 0.624 | <0.0001 |
| 16-day | 0.666 | <0.0001 |
| 17-day | 0.647 | <0.0001 |
| 18-day | 0.602 | <0.0001 |
| 19-day | 0.594 | <0.0001 |
| 20-day | 0.577 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, S.; Son, W.-S.; Park, B.; Choi, B.Y. Forecasting Hospital Visits Due to Influenza Based on Emergency Department Visits for Fever: A Feasibility Study on Emergency Department-Based Syndromic Surveillance. Int. J. Environ. Res. Public Health 2022, 19, 12954. https://doi.org/10.3390/ijerph191912954
Hong S, Son W-S, Park B, Choi BY. Forecasting Hospital Visits Due to Influenza Based on Emergency Department Visits for Fever: A Feasibility Study on Emergency Department-Based Syndromic Surveillance. International Journal of Environmental Research and Public Health. 2022; 19(19):12954. https://doi.org/10.3390/ijerph191912954
Chicago/Turabian StyleHong, Sunghee, Woo-Sik Son, Boyoung Park, and Bo Youl Choi. 2022. "Forecasting Hospital Visits Due to Influenza Based on Emergency Department Visits for Fever: A Feasibility Study on Emergency Department-Based Syndromic Surveillance" International Journal of Environmental Research and Public Health 19, no. 19: 12954. https://doi.org/10.3390/ijerph191912954
APA StyleHong, S., Son, W.-S., Park, B., & Choi, B. Y. (2022). Forecasting Hospital Visits Due to Influenza Based on Emergency Department Visits for Fever: A Feasibility Study on Emergency Department-Based Syndromic Surveillance. International Journal of Environmental Research and Public Health, 19(19), 12954. https://doi.org/10.3390/ijerph191912954






