Diet Composition, Anthropometrics, and Mortality Risk
Abstract
1. Introduction
2. Methods
2.1. Data
2.2. Anthropometric and Diet Measures
2.3. Statistical Analysis of Associations
3. Results
3.1. Cohort Characteristics
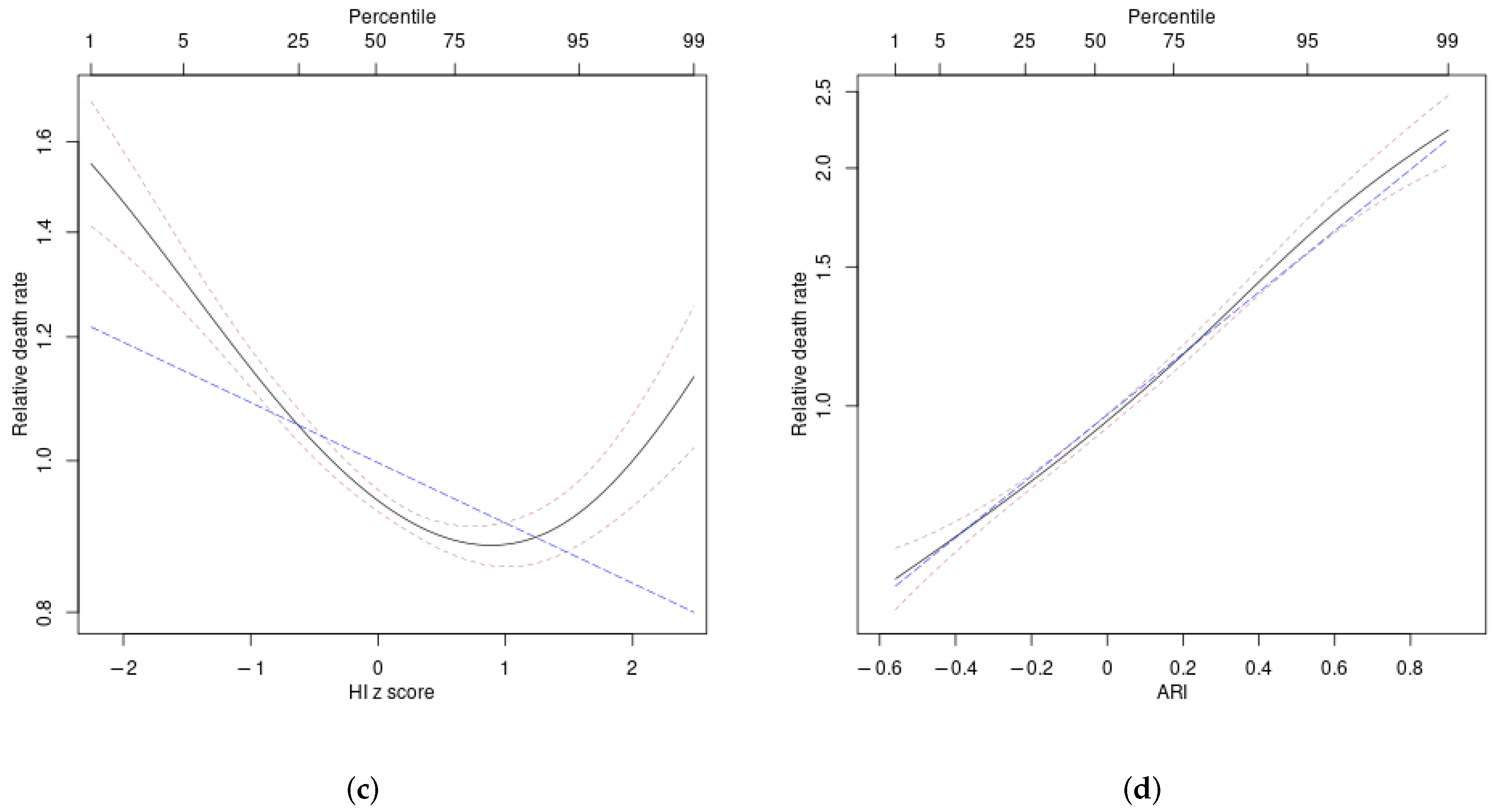
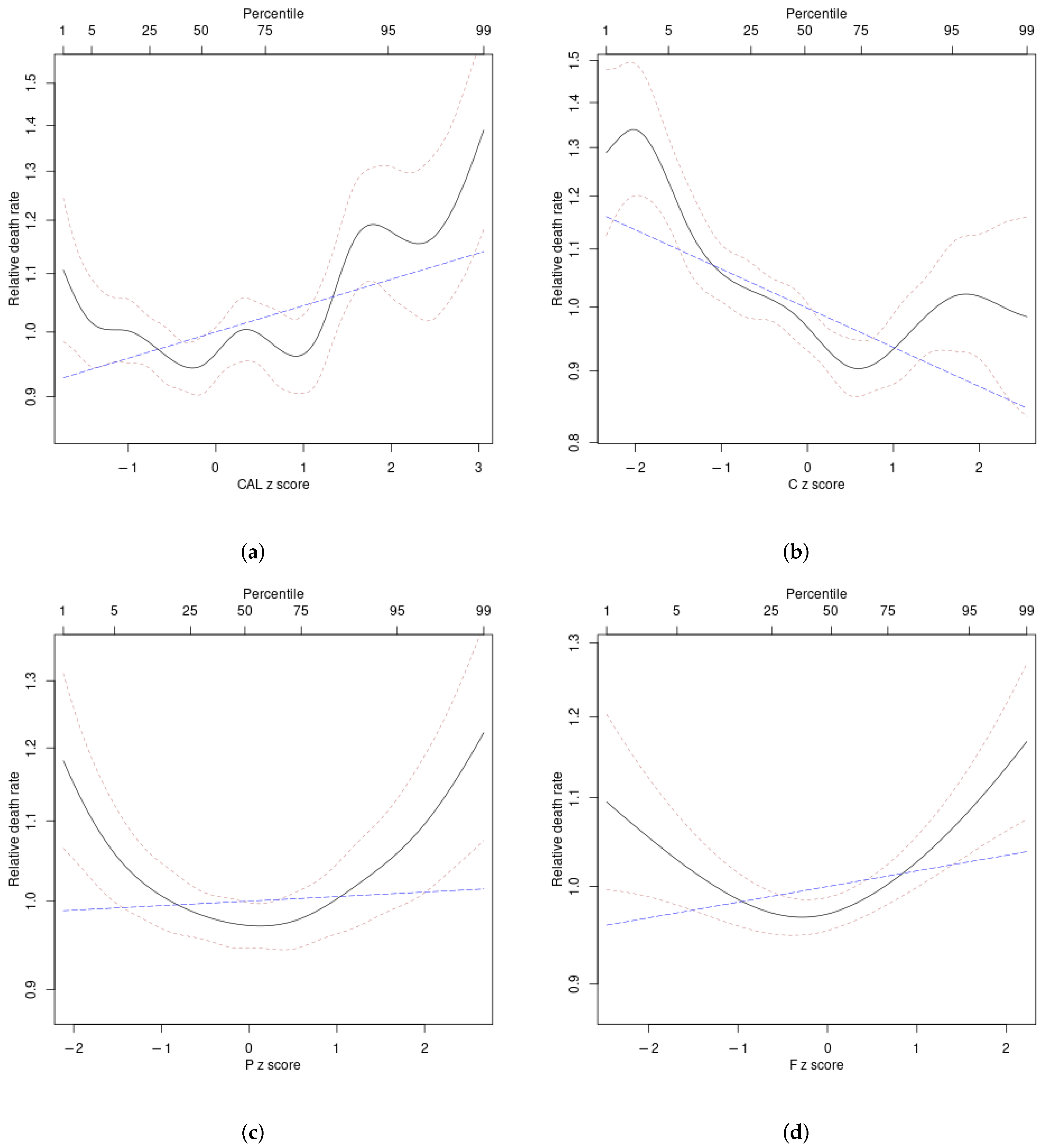
3.2. Anthropometrics Associations with Mortality
3.3. Diet Associations with Anthropometrics
3.4. Diet Associations with Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mazzini, I. Diet and medicine in the ancient world. In Food: A Culinary History from Antiquity to the Present; Columbia University Press: New York, NY, USA, 1999; pp. 141–152. [Google Scholar]
- Manuel, D.G.; Perez, R.; Sanmartin, C.; Taljaard, M.; Hennessy, D.; Wilson, K.; Tanuseputro, P.; Manson, H.; Bennett, C.; Tuna, M.; et al. Measuring Burden of Unhealthy Behaviours Using a Multivariable Predictive Approach: Life Expectancy Lost in Canada Attributable to Smoking, Alcohol, Physical Inactivity, and Diet. PLoS Med. 2016, 13, e1002082. [Google Scholar] [CrossRef] [PubMed]
- Pifferi, F.; Aujard, F. Caloric restriction, longevity and aging: Recent contributions from human and non-human primate studies. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2019, 95, 109702. [Google Scholar] [CrossRef] [PubMed]
- Le Couteur, D.G.; Solon-Biet, S.; Cogger, V.C.; Mitchell, S.J.; Senior, A.; de Cabo, R.; Raubenheimer, D.; Simpson, S.J. The impact of low-protein high-carbohydrate diets on aging and lifespan. Cell. Mol. Life Sci. 2016, 73, 1237–1252. [Google Scholar] [CrossRef]
- Le Couteur, D.G.; Solon-Biet, S.; Wahl, D.; Cogger, V.C.; Willcox, B.J.; Willcox, D.C.; Raubenheimer, D.; Simpson, S.J. New Horizons: Dietary protein, ageing and the Okinawan ratio. Age Ageing 2016, 45, 443. [Google Scholar] [CrossRef]
- Moatt, J.P.; Fyfe, M.A.; Heap, E.; Mitchell, L.J.M.; Moon, F.; Walling, C.A. Reconciling nutritional geometry with classical dietary restriction: Effects of nutrient intake, not calories, on survival and reproduction. Aging Cell 2018, 18, e12868. [Google Scholar] [CrossRef] [PubMed]
- Levine, M.E.; Suarez, J.A.; Brandhorst, S.; Balasubramanian, P.; Cheng, C.W.; Madia, F.; Fontana, L.; Mirisola, M.G.; Guevara-Aguirre, J.; Wan, J.; et al. Low protein intake is associated with a major reduction in IGF-1, cancer, and overall mortality in the 65 and younger but not older population. Cell Metab. 2014, 19, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Alkerwi, A.; Sauvageot, N.; Buckley, J.D.; Donneau, A.F.; Albert, A.; Guillaume, M.; Crichton, G.E. The potential impact of animal protein intake on global and abdominal obesity: Evidence from the Observation of Cardiovascular Risk Factors in Luxembourg (ORISCAV-LUX) study. Public Health Nutr. 2015, 18, 1831–1838. [Google Scholar] [CrossRef] [PubMed]
- Song, M.; Fung, T.T.; Hu, F.B.; Willett, W.C.; Longo, V.D.; Chan, A.T.; Giovannucci, E.L. Association of Animal and Plant Protein Intake With All-Cause and Cause-Specific Mortality. JAMA Intern. Med. 2016, 176, 1453. [Google Scholar] [CrossRef]
- Huang, J.; Liao, L.M.; Weinstein, S.J.; Sinha, R.; Graubard, B.I.; Albanes, D. Association Between Plant and Animal Protein Intake and Overall and Cause-Specific Mortality. JAMA Intern. Med. 2020, 180, 1173. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.D.; Sacks, G.; Chandramohan, D.; Chow, C.C.; Wang, Y.C.; Gortmaker, S.L.; Swinburn, B.A. Quantification of the effect of energy imbalance on bodyweight. Lancet 2011, 378, 826–837. [Google Scholar] [CrossRef]
- Hall, K.D.; Heymsfield, S.B.; Kemnitz, J.W.; Klein, S.; Schoeller, D.A.; Speakman, J.R. Energy balance and its components: Implications for body weight regulation. Am. J. Clin. Nutr. 2012, 95, 989–994. [Google Scholar] [CrossRef] [PubMed]
- Howell, S.; Kones, R. “Calories in, calories out” and macronutrient intake: The hope, hype, and science of calories. Am. J. Physiol.-Endocrinol. Metab. 2017, 313, E608–E612. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE 2012, 7, e39504. [Google Scholar] [CrossRef] [PubMed]
- Krakauer, N.Y.; Krakauer, J.C. An Anthropometric Risk Index based on combining height, weight, waist, and hip measurements. J. Obes. 2016, 2016, 8094275. [Google Scholar] [CrossRef] [PubMed]
- Krakauer, N.Y.; Krakauer, J.C. The new anthropometrics and abdominal obesity: A body shape index, hip index, and anthropometric risk index. In Nutrition in the Prevention and Treatment of Abdominal Obesity, 2nd ed.; Watson, R.R., Ed.; Academic Press: Cambridge, MA, USA, 2019; Chapter 2; pp. 19–27. [Google Scholar] [CrossRef]
- Ji, M.; Zhang, S.; An, R. Effectiveness of A Body Shape Index (ABSI) in predicting chronic diseases and mortality: A systematic review and meta-analysis. Obes. Rev. 2018, 19, 737–759. [Google Scholar] [CrossRef] [PubMed]
- Christakoudi, S.; Evangelou, E.; Riboli, E.; Tsilidis, K.K. GWAS of allometric body-shape indices in UK Biobank identifies loci suggesting associations with morphogenesis, organogenesis, adrenal cell renewal and cancer. Sci. Rep. 2021, 11, 10688. [Google Scholar] [CrossRef]
- Christakoudi, S.; Tsilidis, K.K.; Evangelou, E.; Riboli, E. A Body Shape Index (ABSI), hip index, and risk of cancer in the UK Biobank cohort. Cancer Med. 2021, 10, 5614–5628. [Google Scholar] [CrossRef]
- Christakoudi, S.; Riboli, E.; Evangelou, E.; Tsilidis, K.K. Associations of body shape index (ABSI) and hip index with liver, metabolic, and inflammatory biomarkers in the UK Biobank cohort. Sci. Rep. 2022, 12, 8812. [Google Scholar] [CrossRef] [PubMed]
- Christakoudi, S.; Riboli, E.; Evangelou, E.; Tsilidis, K.K. Associations of body shape phenotypes with sex steroids and their binding proteins in the UK Biobank cohort. Sci. Rep. 2022, 12, 10774. [Google Scholar] [CrossRef]
- Nagayama, D.; Sugiura, T.; Choi, S.Y.; Shirai, K. Various Obesity Indices and Arterial Function Evaluated with CAVI – Is Waist Circumference Adequate to Define Metabolic Syndrome? Vasc. Health Risk Manag. 2022, 18, 721–733. [Google Scholar] [CrossRef]
- Isaura, E.R.; Chen, Y.C.; Yang, S.H. The Association of Food Consumption Scores, Body Shape Index, and Hypertension in a Seven-Year Follow-Up among Indonesian Adults: A Longitudinal Study. Int. J. Environ. Res. Public Health 2018, 15, 175. [Google Scholar] [CrossRef]
- Glover, M.; Nolte, M.; Wagemakers, A.; McRobbie, H.; Kruger, R.; Breier, B.H.; Stephen, J.; Funaki-Tahifote, M.; Shanthakumar, M. Adherence to daily dietary and activity goals set within a Māori and Pacific weight loss competition. BMC Obes. 2019, 6, 6. [Google Scholar] [CrossRef] [PubMed]
- The ARIC Investigators. The Atherosclerosis Risk in Communities (ARIC) study: Design and objectives. Am. J. Epidemiol. 1989, 129, 687–702. [Google Scholar] [CrossRef]
- Seidelmann, S.B.; Claggett, B.; Cheng, S.; Henglin, M.; Shah, A.; Steffen, L.M.; Folsom, A.R.; Rimm, E.B.; Willett, W.C.; Solomon, S.D. Dietary carbohydrate intake and mortality: A prospective cohort study and meta-analysis. Lancet Public Health 2018, 3, e419–e428. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. Expansion of waist circumference in medical literature: Potential clinical application of a body shape index. J. Obes. Weight Loss Ther. 2014, 4, 216. [Google Scholar] [CrossRef]
- Akaike, H. A new look at the statistical model identification. IEEE Trans. Autom. Control 1974, 19, 716–723. [Google Scholar] [CrossRef]
- Burnham, K.P.; Anderson, D.R. Multimodel inference: Understanding AIC and BIC in model selection. Sociol. Methods Res. 2004, 33, 261–304. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Therneau, T.M.; Grambsch, P.M. Modeling Survival Data: Extending the Cox Model; Springer: New York, NY, USA, 2000. [Google Scholar]
- Therneau, T.M. A Package for Survival Analysis in R, R Package version 3.2-7; R Project, Free Software Foundation: Boston, MA, USA, 2020. [Google Scholar]
- Rizza, W.; Veronese, N.; Fontana, L. What are the roles of calorie restriction and diet quality in promoting healthy longevity? Ageing Res. Rev. 2014, 13, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Arganda, S.; Bouchebti, S.; Bazazi, S.; Le Hesran, S.; Puga, C.; Latil, G.; Simpson, S.J.; Dussutour, A. Parsing the life-shortening effects of dietary protein: Effects of individual amino acids. Proc. R. Soc. Lond. B Biol. Sci. 2017, 284, 20162052. [Google Scholar] [CrossRef] [PubMed]
- Almendáriz-Palacios, C.; Mousseau, D.D.; Eskiw, C.H.; Gillespie, Z.E. Still Living Better through Chemistry: An Update on Caloric Restriction and Caloric Restriction Mimetics as Tools to Promote Health and Lifespan. Int. J. Mol. Sci. 2020, 21, 9220. [Google Scholar] [CrossRef]
- Kim, H.; Lee, K.; Rebholz, C.M.; Kim, J. Plant-based diets and incident metabolic syndrome: Results from a South Korean prospective cohort study. PLoS Med. 2020, 17, e1003371. [Google Scholar] [CrossRef] [PubMed]
- Suksatan, W.; Moradi, S.; Naeini, F.; Bagheri, R.; Mohammadi, H.; Talebi, S.; Mehrabani, S.; Hojjati Kermani, M.A.; Suzuki, K. Ultra-Processed Food Consumption and Adult Mortality Risk: A Systematic Review and Dose–Response Meta-Analysis of 207,291 Participants. Nutrients 2021, 14, 174. [Google Scholar] [CrossRef] [PubMed]
- Senior, A.M.; Solon-Biet, S.M.; Cogger, V.C.; Couteur, D.G.L.; Nakagawa, S.; Raubenheimer, D.; Simpson, S.J. Dietary macronutrient content, age-specific mortality and lifespan. Proc. R. Soc. B Biol. Sci. 2019, 286, 20190393. [Google Scholar] [CrossRef] [PubMed]
- Kantor, L.S. A Dietary Assessment of the U.S. Food Supply: Comparing Per Capita Food Consumption with Food Guide Pyramid Serving Recommendations; Technical Report; Economic Research Service, U.S. Department of Agriculture: Washington, DC, USA, 1998.
- Tom, M.S.; Fischbeck, P.S.; Hendrickson, C.T. Energy use, blue water footprint, and greenhouse gas emissions for current food consumption patterns and dietary recommendations in the US. Environ. Syst. Decis. 2015, 36, 92–103. [Google Scholar] [CrossRef]
- Heymsfield, S.B.; Childers, D.; Beetsch, J.; Allison, D.B.; Pietrobelli, A. Body size and human energy requirements: Reduced mass-specific resting energy expenditure in tall adults. J. Appl. Physiol. 2007, 103, 1543–1550. [Google Scholar] [CrossRef]
- Freedman, L.S.; Commins, J.M.; Moler, J.E.; Arab, L.; Baer, D.J.; Kipnis, V.; Midthune, D.; Moshfegh, A.J.; Neuhouser, M.L.; Prentice, R.L.; et al. Pooled Results From 5 Validation Studies of Dietary Self-Report Instruments Using Recovery Biomarkers for Energy and Protein Intake. Am. J. Epidemiol. 2014, 180, 172–188. [Google Scholar] [CrossRef]
- Liese, A.D.; Krebs-Smith, S.M.; Subar, A.F.; George, S.M.; Harmon, B.E.; Neuhouser, M.L.; Boushey, C.J.; Schap, T.E.; Reedy, J. The Dietary Patterns Methods Project: Synthesis of Findings across Cohorts and Relevance to Dietary Guidance. J. Nutr. 2015, 145, 393–402. [Google Scholar] [CrossRef]
- Subar, A.F.; Freedman, L.S.; Tooze, J.A.; Kirkpatrick, S.I.; Boushey, C.; Neuhouser, M.L.; Thompson, F.E.; Potischman, N.; Guenther, P.M.; Tarasuk, V.; et al. Addressing Current Criticism Regarding the Value of Self-Report Dietary Data. J. Nutr. 2015, 145, 2639–2645. [Google Scholar] [CrossRef]
- Hooper, L.; Abdelhamid, A.; Bunn, D.; Brown, T.; Summerbell, C.D.; Skeaff, C.M. Effects of total fat intake on body weight. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef]
- Wennberg, M.; Tornevi, A.; Johansson, I.; Hörnell, A.; Norberg, M.; Bergdahl, I.A. Diet and lifestyle factors associated with fish consumption in men and women: A study of whether gender differences can result in gender-specific confounding. Nutr. J. 2012, 11, 101. [Google Scholar] [CrossRef]
- Ocké, M.C. Evaluation of methodologies for assessing the overall diet: Dietary quality scores and dietary pattern analysis. Proc. Nutr. Soc. 2013, 72, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Thorpe, M.G.; Milte, C.M.; Crawford, D.; McNaughton, S.A. A comparison of the dietary patterns derived by principal component analysis and cluster analysis in older Australians. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 30. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Hu, E.A.; E Wong, K.; Yu, B.; Steffen, L.M.; Seidelmann, S.B.; Boerwinkle, E.; Coresh, J.; Rebholz, C.M. Serum Metabolites Associated with Healthy Diets in African Americans and European Americans. J. Nutr. 2021, 151, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Yi, S.Y.; Steffen, L.M.; Lutsey, P.L.; Cushman, M.; Folsom, A.R. Contrasting Associations of Prudent and Western Dietary Patterns with Risk of Developing Venous Thromboembolism. Am. J. Med. 2021, 134, 763–768.e3. [Google Scholar] [CrossRef] [PubMed]


| Diet Attribute | Body Mass Index | A Body Shape Index | Hip Index | Anthropometric Risk Indicator | |
|---|---|---|---|---|---|
| Energy | Unadjusted | 8 ± 8 | 35 *** ± 9 | −25 ** ± 8 | 15 *** ± 3 |
| Adjusted | 19 * ± 8 | 18 * ± 8 | −23 ** ± 8 | 12 *** ± 3 | |
| Carbohydrate | Unadjusted | −53 *** ± 8 | −26 ** ± 9 | 22 * ± 9 | −15 *** ± 3 |
| Adjusted | −85 *** ± 8 | 5 ± 9 | 20 * ± 9 | −11 *** ± 3 | |
| Protein | Unadjusted | 112 *** ± 8 | −46 *** ± 9 | −2 ± 9 | 2 ± 3 |
| Adjusted | 99 *** ± 8 | −15 ± 9 | 0 ± 9 | 10 *** ± 3 | |
| Plant protein | Unadjusted | −57 *** ± 8 | −10 ± 8 | 66 *** ± 8 | −15 *** ± 3 |
| Adjusted | −53 *** ± 8 | −13 ± 8 | 55 *** ± 9 | −10 *** ± 3 | |
| Animal protein | Unadjusted | 125 *** ± 8 | −43 *** ± 9 | −22 * ± 9 | 7 * ± 3 |
| Adjusted | 109 *** ± 8 | −11 ± 9 | −17 ± 9 | 12 *** ± 3 | |
| Fat | Unadjusted | 70 *** ± 8 | 27 ** ± 9 | −16 ± 9 | 15 *** ± 3 |
| Adjusted | 62 *** ± 8 | 1 ± 9 | −21 * ± 9 | 10 *** ± 3 | |
| Plant fat | Unadjusted | −50 *** ± 8 | 7 ± 9 | 37 *** ± 9 | −13 *** ± 3 |
| Adjusted | −35 *** ± 8 | −20 * ± 9 | 17 ± 9 | −11 *** ± 3 | |
| Animal fat | Unadjusted | 115 *** ± 8 | 23 ** ± 9 | −47 *** ± 9 | 26 *** ± 3 |
| Adjusted | 91 *** ± 8 | 18 * ± 8 | −35 *** ± 9 | 19 *** ± 3 |
| Diet Attribute | Mortality Hazard | AIC | |
|---|---|---|---|
| Coefficient | (Linear/Nonlinear) | ||
| Energy | Unadjusted | 42 *** ± 12 | 10.4/31.3 |
| Adjusted | 37 ** ± 12 | 7.7/10.9 | |
| Carbohydrate | Unadjusted | −68 *** ± 12 | 31.1/50.3 |
| Adjusted | −33 * ± 13 | 4.6/10.5 | |
| Protein | Unadjusted | 2 ± 12 | −2.0/14.3 |
| Adjusted | 41 ** ± 13 | 8.4/8.6 | |
| Plant protein | Unadjusted | −63 *** ± 12 | 25.6/39.8 |
| Adjusted | −17 ± 12 | −0.1/2.8 | |
| Animal protein | Unadjusted | 20 ± 12 | 0.7/11.1 |
| Adjusted | 44 *** ± 13 | 10.0/16.4 | |
| Fat | Unadjusted | 19 ± 12 | 0.3/14.3 |
| Adjusted | 7 ± 13 | −1.7/−0.2 | |
| Plant fat | Unadjusted | −90 *** ± 12 | 51.4/61.4 |
| Adjusted | −52 *** ± 13 | 15.0/18.3 | |
| Animal fat | Unadjusted | 90 *** ± 12 | 52.6/58.1 |
| Adjusted | 47 *** ± 12 | 12.7/13.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krakauer, N.Y.; Krakauer, J.C. Diet Composition, Anthropometrics, and Mortality Risk. Int. J. Environ. Res. Public Health 2022, 19, 12885. https://doi.org/10.3390/ijerph191912885
Krakauer NY, Krakauer JC. Diet Composition, Anthropometrics, and Mortality Risk. International Journal of Environmental Research and Public Health. 2022; 19(19):12885. https://doi.org/10.3390/ijerph191912885
Chicago/Turabian StyleKrakauer, Nir Y., and Jesse C. Krakauer. 2022. "Diet Composition, Anthropometrics, and Mortality Risk" International Journal of Environmental Research and Public Health 19, no. 19: 12885. https://doi.org/10.3390/ijerph191912885
APA StyleKrakauer, N. Y., & Krakauer, J. C. (2022). Diet Composition, Anthropometrics, and Mortality Risk. International Journal of Environmental Research and Public Health, 19(19), 12885. https://doi.org/10.3390/ijerph191912885






