Coping with Secondary Traumatic Stress
Abstract
:1. Introduction
1.1. Coping with Secondary Trauma
1.2. Current Study
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Procedure
2.4. Data Analysis
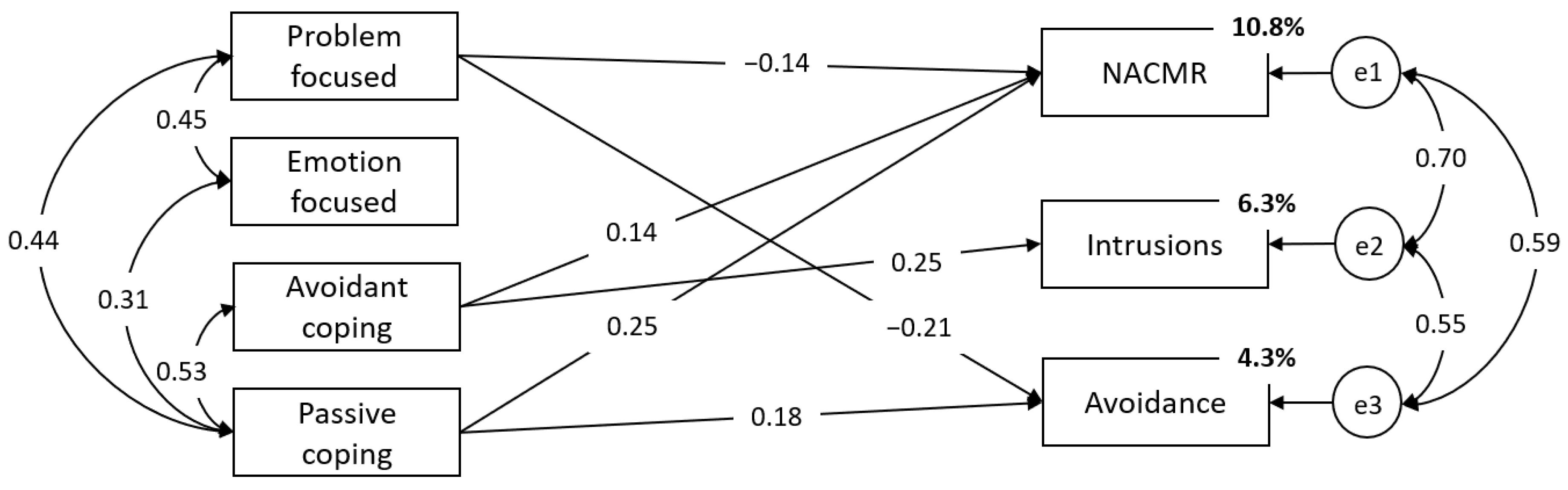
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Figley, C.R. Victimization, Trauma, and Traumatic Stress. Couns Psychol. 1988, 16, 635–641. [Google Scholar] [CrossRef]
- Figley, C.R. Compassion Fatigue as Secondary Traumatic Stress Disorder: An Overview; Routledge: New York, NY, USA, 1995. [Google Scholar]
- Figley, C.R. The Transmission of Trauma; Routledge: New York, NY, USA, 1995. [Google Scholar]
- Weitkamp, K.; Daniels, J.K.; Klasen, F. Psychometric properties of the Questionnaire for Secondary Traumatization. Eur. J. Psychotraumatol. 2014, 5, 21875. [Google Scholar] [CrossRef] [Green Version]
- Elwood, L.S.; Mott, J.; Lohr, J.M.; Galovski, T.E. Secondary trauma symptoms in clinicians: A critical review of the construct, specificity, and implications for trauma-focused treatment. Clin. Psychol. Rev. 2011, 31, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Živanović, M.; Vukčević Marković, M. Latent structure of secondary traumatic stress, its precursors, and effects on people working with refugees. PLoS ONE 2020, 15, 024154. [Google Scholar] [CrossRef] [PubMed]
- Živanović, M.; Vukčević Marković, M. Secondary traumatization. In Social Trauma–An international Textbook; Hamburger, A., Hancheva, C., Volkan, V., Eds.; Springer: Berlin/Heidelberg Germany; New York, NY, USA, 2020; pp. 295–302. [Google Scholar]
- Jacobs, I.; Charmillot, M.; Soelch, C.M.; Horsch, A. Validity, Reliability, and Factor Structure of the Secondary Traumatic Stress Scale-French Version. Front. Psychiatry 2019, 10, 191. [Google Scholar] [CrossRef]
- Bride, B.E.; Robinson, M.M.; Yegidis, B.; Figley, C.R. Development and Validation of the Secondary Traumatic Stress Scale. Res. Soc. Work Pract. 2004, 14, 27–35. [Google Scholar] [CrossRef] [Green Version]
- Mirsaleh, Y.R.; Ahmadi, K.; Davoudi, F.; Mousavi, S.Z. Validity, Reliability, and Factor Structure of Secondary Trauma Stress Scale (STSS) in a Sample of Warfare Victims’ Children. Iran J. Psychiatry Clin. Psychol. 2014, 20, 134–143. [Google Scholar]
- Bjornestad, A.G.; Schweinle, A.; Elhai, J.D. Measuring Secondary Traumatic Stress Symptoms in Military Spouses with the Posttraumatic Stress Disorder Checklist Military Version. J. Nerv. Ment. Dis. 2014, 202, 864–869. [Google Scholar] [CrossRef] [Green Version]
- Mordeno, I.G.; Go, G.P.; Yangson-serondo, A. Examining the dimensional structure models of secondary traumatic stress based on DSM-5 symptoms. Asian J. Psychiatr. 2017, 25, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Vukčević, M.M.; Živanović, M. Secondary Traumatization in Service Providers working with Refugees. In Forced Migration and Social Trauma; Hamburger, A., Hancheva, C., Ozcurumez, S., Scher, C., Stanković, B., Tutnjević, S., Eds.; Routledge: London, UK; New York, NY, USA, 2019; pp. 511–562. [Google Scholar]
- Hensel, J.M.; Ruiz, C.; Finney, C.; Dewa, C.S. Meta-Analysis of Risk Factors for Secondary Traumatic Stress in Therapeutic Work with Trauma Victims. J. Trauma Stress 2015, 28, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Guerra Vio, C.; Vidallet, J.L.S. Psychometric examination of the Secondary Traumatic Stress Scale: A study on Chileans professionals. Psicol. Conductual. 2007, 15, 441–456. [Google Scholar]
- Lazarus, R.S. Coping theory and research: Past, present, and future. Psychosom. Med. 1993, 55, 234–247. [Google Scholar] [CrossRef] [PubMed]
- Snyder, C.R.; Pulvers, K.M. Dr. Seuss, the Coping Machine, and “Oh, the Places You’ll Go.”. In Coping with Stress: Effective People and Processes; Snyder, C.R., Ed.; Oxford University Press: Oxford, UK, 2001; pp. 3–29. [Google Scholar]
- Littleton, H.; Horsley, S.; John, S.; Nelson, D.V. Trauma Coping Strategies and Psychological Distress: A Meta-Analysis. J. Trauma Stress 2007, 20, 977–988. [Google Scholar] [CrossRef] [PubMed]
- Mcgarry, S.; Girdler, S.; McDonald, A.; Valentine, J.; Lee, S.L.; Blair, E. Paediatric health-care professionals: Relationships between psychological distress, resilience and coping skills. J. Paediatr. Child Health. 2013, 49, 725–732. [Google Scholar] [CrossRef]
- Bourke, M.L.; Craun, S.W. Coping with secondary traumatic stress: Differences between U.K. and U.S. Child Exploitation Personnel. Traumatology 2014, 20, 57–64. [Google Scholar] [CrossRef]
- Volker, R.; Bernhard, B.; Anna, K.; Fabrizio, S.; Robin, R.; Jessica, P. Burnout, coping and job satisfaction in service staff treating opioid addicts-From Athens to Zurich. Stress Health 2010, 26, 149–159. [Google Scholar] [CrossRef]
- Thompson, I.A.; Amatea, E.S.; Thompson, E.S. Personal and contextual predictors of Mental Health Counselors. J. Ment. Health. Couns. 2014, 36, 58–77. [Google Scholar] [CrossRef]
- Turliuc, N.M.; Mairean, C. A correlational study of the relationships between coping strategies and vicarious trauma beliefs. Psychol. Ser. 2012, 21, 59–77. [Google Scholar]
- Akinsulure-Smith, A.M.; Espinosa, A.; Chu, T.; Hallock, R. Secondary Traumatic Stress and Burnout Among Refugee Resettlement Workers: The Role of Coping and Emotional Intelligence. J. Trauma. Stress 2018, 31, 202–212. [Google Scholar] [CrossRef] [PubMed]
- Manning-Jones, S.; De Terte, I.; Stephens, M. Secondary traumatic stress, vicarious posttraumatic growth, and coping among health professionals: A comparison study. N. Z. J. Psychol. 2016, 45, 1. [Google Scholar] [CrossRef]
- Killian, K.D. Helping till it hurts? A multimethod study of compassion fatigue, burnout, and self-care in clinicians working with trauma survivors. Traumatology 2008, 14, 32–44. [Google Scholar] [CrossRef] [Green Version]
- Townsend, S.M.; Campbell, R. Organizational correlates of secondary traumatic stress and burnout among sexual assault nurse examiners. J. Forensic. Nurs. 2009, 5, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Grundlingh, H.; Knight, L.; Naker, D.; Devries, K. Secondary distress in violence researchers: A randomised trial of the effectiveness of group debriefings. BMC Psychiatry 2017, 17, 1327. [Google Scholar] [CrossRef]
- Schauben, L.J.; Frazier, P.A. Vicarious trauma: The effects on female counselors of working with sexual violence survivors. Psychol. Women 1995, 19, 49–64. [Google Scholar] [CrossRef]
- Cantekin, D.; Gençöz, T. Mental Health of Syrian Asylum Seekers in Turkey: The Role of Pre-Migration and Post-Migration Risk Factors. J. Soc. Clin. Psychol. 2017, 36, 835–859. [Google Scholar] [CrossRef]
- Carswell, K.; Blackburn, P.; Barker, C. The Relationship Between Trauma, Post-Migration Problems and the Psychological Well-Being of Refugees and Asylum Seekers. Int. J. Soc. Psychiatry 2009, 57, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Vukčević, M.; Momirović, J.; Purić, D. Adaptation of Harvard Trauma Questionnaire for working with refugees and asylum seekers in Serbia. Psihologija 2016, 49, 277–299. [Google Scholar] [CrossRef]
- Vukčević, M.; Momirović, J.; Purić, D. Refugees in Serbia: On the way to a better life. Forced Migr. Rev. 2016, 51, 51–52. [Google Scholar]
- Hallas, P.; Hansen, A.R.; Stæhr, M.A.; Munk-Andersen, E.; Jorgensen, H.L. Length of stay in asylum centres and mental health in asylum seekers: A retrospective study from Denmark. BMC Public Health 2007, 7, 288. [Google Scholar] [CrossRef] [Green Version]
- Keller, A.S.; Rosenfeld, B.; Trinh-Shevrin, C.; Meserve, C.; Sachs, E.; Leviss, J.A. Mental health of detained asylum seekers. Lancet 2003, 362, 1721–1723. [Google Scholar] [CrossRef]
- Laban, C.J.; Gernaat, H.B.P.E.; Komproe, I.H.; Van Der Tweel, I.; De Jong, J.T.V.M. Postmigration living problems and common psychiatric disorders in Iraqi asylum seekers in the Netherlands. J. Nerv. Ment. Dis. 2005, 193, 825–832. [Google Scholar] [CrossRef]
- Priebe, S.; Giacco, D.; El-Nagib, R. Public health aspects of mental health among migrants and refugees: A review of the evidence on mental health care for refugees, asylum seekers and irregular migrants in the WHO European Region. Health Evid. Netw. Synth. Rep. 2016, 47, 1–27. [Google Scholar]
- Purić, D.; Vukčević Marković, M. Development and validation of the Stressful Experiences in Transit Questionnaire (SET-Q) and its Short Form (SET-SF). Eur. J. Psychotraumatol. 2019, 10, 1611091. [Google Scholar] [CrossRef] [Green Version]
- Raghavan, S.; Rasmussen, A.; Rosenfeld, B.; Keller, A.S. Correlates of Symptom Reduction in Treatment-Seeking Survivors of Torture. Psychol. Trauma Theory Res. Pract. Policy 2012, 5, 377–383. [Google Scholar] [CrossRef]
- Steel, Z.; Chey, T.; Silove, D.; Marnane, C.; Bryant, R.A.; Van Ommeren, M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA J. Am. Med. Assoc. 2009, 302, 537–549. [Google Scholar] [CrossRef]
- Vukčević, M.; Dobrić, J.; Purić, D. Mental Health of Asylum Seekers in Serbia; UNHCR: Belgrade, Serbia, 2014. [Google Scholar]
- Vukčević, M.M.; Gašić, J.; Bjekić, J. Refugees’ Mental Health; Psychosocial Innovation Network: Belgrade, Serbia, 2017. [Google Scholar]
- Bogic, M.; Njoku, A.; Priebe, S. Long-term mental health of war-refugees: A systematic literature review. BMC Int. Health Hum. Rights 2015, 15, 1. [Google Scholar] [CrossRef] [Green Version]
- Vukčević, M.M.; Stanković, I.; Bjekić, J. Psychological Well-Being of Refugees in Serbia; Psychosocial Innovation Network: Belgrade, Serbia, 2018. [Google Scholar]
- Vukčević, M.M.; Bobić, S.; Bjekić, J. Psychological Well-Being of Refugees and Asylum Seekers in Serbia; UNHCR: Belgrade, Serbia, 2019. [Google Scholar]
- Kindermann, D.; Schmid, C.; Derreza-Greeven, C.; Huhn, D.; Kohl, R.M.; Junne, F. Prevalence of and Risk Factors for Secondary Traumatization in Interpreters for Refugees: A Cross-Sectional Study. Psychopathology 2017, 50, 262–272. [Google Scholar] [CrossRef]
- Holmgren, H.; Søndergaard, H.; Elklit, A. Stress and coping in traumatised interpreters: A pilot study of refugee interpreters working for a humanitarian organiation. Intervention 2003, 1, 22–27. [Google Scholar]
- Gargano, M.C.; Ajduković, D.; Vukčević Marković, M. Mental Health in the Transit Context: Evidence from 10 Countries. Int. J. Environ. Res. Public Health 2022, 19, 3476. [Google Scholar] [CrossRef]
- Carver, C.S.; Scheier, M.F.; Weintraub, J.K. Assessing coping strategies: A theoretically based approach. J. Pers. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Litman, J.A. The COPE inventory: Dimensionality and relationships with approach- and avoidance-motives and positive and negative traits. Personal. Individ. Dif. 2006, 41, 273–284. [Google Scholar] [CrossRef]
- Devilly, G.J.; Wright, R.; Varker, T. Vicarious trauma, secondary traumatic stress or simply burnout? Effect of trauma therapy on mental health professionals. Aust. N. Z. J. Psychiatry 2009, 43, 373–385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Badger, K.; Royse, D.; Craig, C.D.; Vegas, L. Hospital Social Workers and Indirect Trauma Exposure: An Exploratory Study of Contributing Factors. Health Soc. Work 2008, 33, 63–71. [Google Scholar] [CrossRef]
- Bride, B.E.; Jones, J.L.; Macmaster, S.A. Correlates of Secondary Traumatic Stress in Child Protective Services Workers. J. Evid. Based Soc. Work 2007, 4, 69–80. [Google Scholar] [CrossRef]
- Makadia, R.; Sabin-Farrell, R.; Turpin, G. Indirect exposure to client trauma and the impact on trainee clinical psychologists: Secondary traumatic stress or vicarious traumatization? Clin. Psychol. Psychother. 2017, 24, 1059–1068. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christodoulou-Fella, M.; Middleton, N.; Papathanassoglou, E.D.E.; Karanikola, M.N.K. Exploration of the Association between Nurses’ Moral Distress and Secondary Traumatic Stress Syndrome: Implications for Patient Safety in Mental Health Services. Biomed. Res. Int. 2017. [Google Scholar] [CrossRef]
- Harrison, R.L.; Westwood, M.J. Preventing vicarious traumatization of mental health therapists: Identifying protective practices. Psychother. Theory Res. Pract. Train. 2009, 46, 203–219. [Google Scholar] [CrossRef] [Green Version]
- Bober, T.; Regehr, C. Strategies for reducing secondary or vicarious trauma: Do they work? Br. Treat Cris Interv. 2006, 6, 1. [Google Scholar] [CrossRef]
- Gershon, R.R.M.; Barocas, B.; Canton, A.N.; Xianbin Li Vlahov, D. Mental, physical, and behavioral outcomes associated with perceived work stress in police officers. Crim. Justice Behav. 2009, 36, 275–289. [Google Scholar] [CrossRef]
| M | SD | Min | Max | St. Sk | St. Ku | α | |
|---|---|---|---|---|---|---|---|
| Secondary traumatic stress | |||||||
| NACMR | 2.02 | 0.74 | 1.00 | 4.60 | 5.33 ** | 1.08 | 0.88 |
| Intrusions | 1.89 | 0.71 | 1.00 | 4.80 | 7.03 ** | 3.71 ** | 0.77 |
| Avoidance | 1.63 | 0.83 | 1.00 | 4.50 | 9.84 ** | 4.80 ** | 0.70 |
| STSS | 1.94 | 0.67 | 1.00 | 4.24 | 5.79 ** | 1.50 | 0.91 |
| Coping mechanisms | |||||||
| Acceptance | 2.75 | 0.56 | 1.25 | 4.00 | −1.16 | −0.59 | 0.68 |
| Active coping | 2.88 | 0.41 | 1.75 | 4.00 | 0.88 | 0.83 | 0.32 |
| Behavioral disengagement | 1.64 | 0.48 | 1.00 | 3.50 | 2.97 ** | −0.05 | 0.68 |
| Denial | 1.45 | 0.51 | 1.00 | 3.50 | 8.69 ** | 5.55 ** | 0.78 |
| Emotional social support | 2.84 | 0.67 | 1.00 | 4.00 | −1.74 | −1.10 | 0.81 |
| Humor | 2.31 | 0.80 | 1.00 | 4.00 | 1.51 | −2.44 * | 0.89 |
| Instrumental social support | 2.91 | 0.54 | 1.25 | 4.00 | −1.40 | −0.79 | 0.68 |
| Mental disengagement | 2.34 | 0.55 | 1.00 | 3.75 | −0.93 | −0.81 | 0.49 |
| Planning | 3.15 | 0.49 | 1.50 | 4.00 | −0.88 | 1.09 | 0.77 |
| Positive reinterpretation and growth | 3.13 | 0.45 | 2.00 | 4.00 | 0.06 | −0.81 | 0.64 |
| Religious coping | 1.68 | 0.87 | 1.00 | 4.00 | 8.08 ** | 0.94 | 0.94 |
| Restraint | 2.67 | 0.53 | 1.00 | 4.00 | −2.19 * | 1.32 | 0.51 |
| Substance use | 1.39 | 0.66 | 1.00 | 4.00 | 13.03 ** | 11.64 ** | 0.96 |
| Suppression of competing activities | 2.61 | 0.51 | 1.00 | 4.00 | −2.74 ** | 1.63 | 0.62 |
| Venting of emotions | 2.30 | 0.64 | 1.00 | 3.75 | 1.15 | −0.93 | 0.78 |
| STSS | NACMR | In | Av | |
|---|---|---|---|---|
| Acceptance | −0.02 | 0.02 | −0.06 | −0.10 |
| Active coping | −0.02 | −0.01 | −0.01 | −0.07 |
| Behavioral disengagement | 0.25 ** | 0.28 ** | 0.15 * | 0.016 ** |
| Denial | 0.21 ** | 0.20 ** | 0.21 ** | 0.10 |
| Emotional social support | −0.03 | 0.00 | −0.05 | −0.10 |
| Humor | 0.08 | 0.12 | 0.00 | 0.03 |
| Instrumental social support | −0.04 | −0.02 | −0.01 | −0.17 ** |
| Mental disengagement | 0.30 ** | 0.30 ** | 0.25 ** | 0.17 ** |
| Planning | −0.12 * | −0.11 | −0.08 | −0.16 ** |
| Positive reinterpretation and growth | −0.14 * | −0.11 | −0.15 * | −0.17 ** |
| Religious coping | 0.08 | 0.05 | 0.15 * | 0.04 |
| Restraint | 0.06 | 0.06 | 0.08 | 0.02 |
| Substance use | 0.29 ** | 0.29 ** | 0.19 ** | 0.27 ** |
| Suppression of competing activities | 0.10 | 0.09 | 0.13 * | −0.00 |
| Venting of emotions | 0.27 ** | 0.30 ** | 0.24 ** | 0.02 |
| 1 | 2 | 3 | 4 | h2 | |
|---|---|---|---|---|---|
| Planning | 0.94 | −0.02 | −0.08 | −0.16 | 0.79 |
| Active coping | 0.68 | 0.04 | 0.08 | −0.05 | 0.46 |
| Suppression of competing activities | 0.63 | 0.01 | 0.19 | 0.11 | 0.52 |
| Positive reinterpretation and growth | 0.58 | 0.08 | −0.14 | 0.10 | 0.45 |
| Emotional social support | −0.07 | 0.98 | −0.07 | 0.03 | 0.92 |
| Instrumental social support | 0.23 | 0.66 | 0.01 | −0.11 | 0.57 |
| Venting of emotions | −0.03 | 0.42 | 0.21 | 0.17 | 0.33 |
| Denial | 0.02 | −0.02 | 0.83 | −0.15 | 0.59 |
| Religious coping | 0.10 | −0.01 | 0.59 | −0.18 | 0.28 |
| Behavioral disengagement | −0.22 | 0.01 | 0.55 | 0.22 | 0.48 |
| Mental disengagement | 0.13 | 0.05 | 0.31 | 0.29 | 0.32 |
| Acceptance | 0.18 | 0.00 | −0.21 | 0.61 | 0.41 |
| Humor | 0.08 | −0.04 | 0.02 | 0.58 | 0.38 |
| Substance use | −0.20 | 0.05 | −0.12 | 0.47 | 0.16 |
| Restraint | 0.35 | −0.11 | 0.07 | 0.39 | 0.36 |
| λ | 3.00 | 2.24 | 1.81 | 2.18 |
| Factor | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. Problem-focused coping | 0.80 | 0.41 ** | 0.02 | 0.38 ** |
| 2. Socially supported emotion-focused coping | 0.73 | 0.09 | 0.30 ** | |
| 3. Avoidant coping | 0.62 | 0.46 ** | ||
| 4. Passive coping | 0.58 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vukčević Marković, M.; Živanović, M. Coping with Secondary Traumatic Stress. Int. J. Environ. Res. Public Health 2022, 19, 12881. https://doi.org/10.3390/ijerph191912881
Vukčević Marković M, Živanović M. Coping with Secondary Traumatic Stress. International Journal of Environmental Research and Public Health. 2022; 19(19):12881. https://doi.org/10.3390/ijerph191912881
Chicago/Turabian StyleVukčević Marković, Maša, and Marko Živanović. 2022. "Coping with Secondary Traumatic Stress" International Journal of Environmental Research and Public Health 19, no. 19: 12881. https://doi.org/10.3390/ijerph191912881
APA StyleVukčević Marković, M., & Živanović, M. (2022). Coping with Secondary Traumatic Stress. International Journal of Environmental Research and Public Health, 19(19), 12881. https://doi.org/10.3390/ijerph191912881






