Sex Differences in Cardiovascular Disease Mortality in Brazil between 1996 and 2019
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
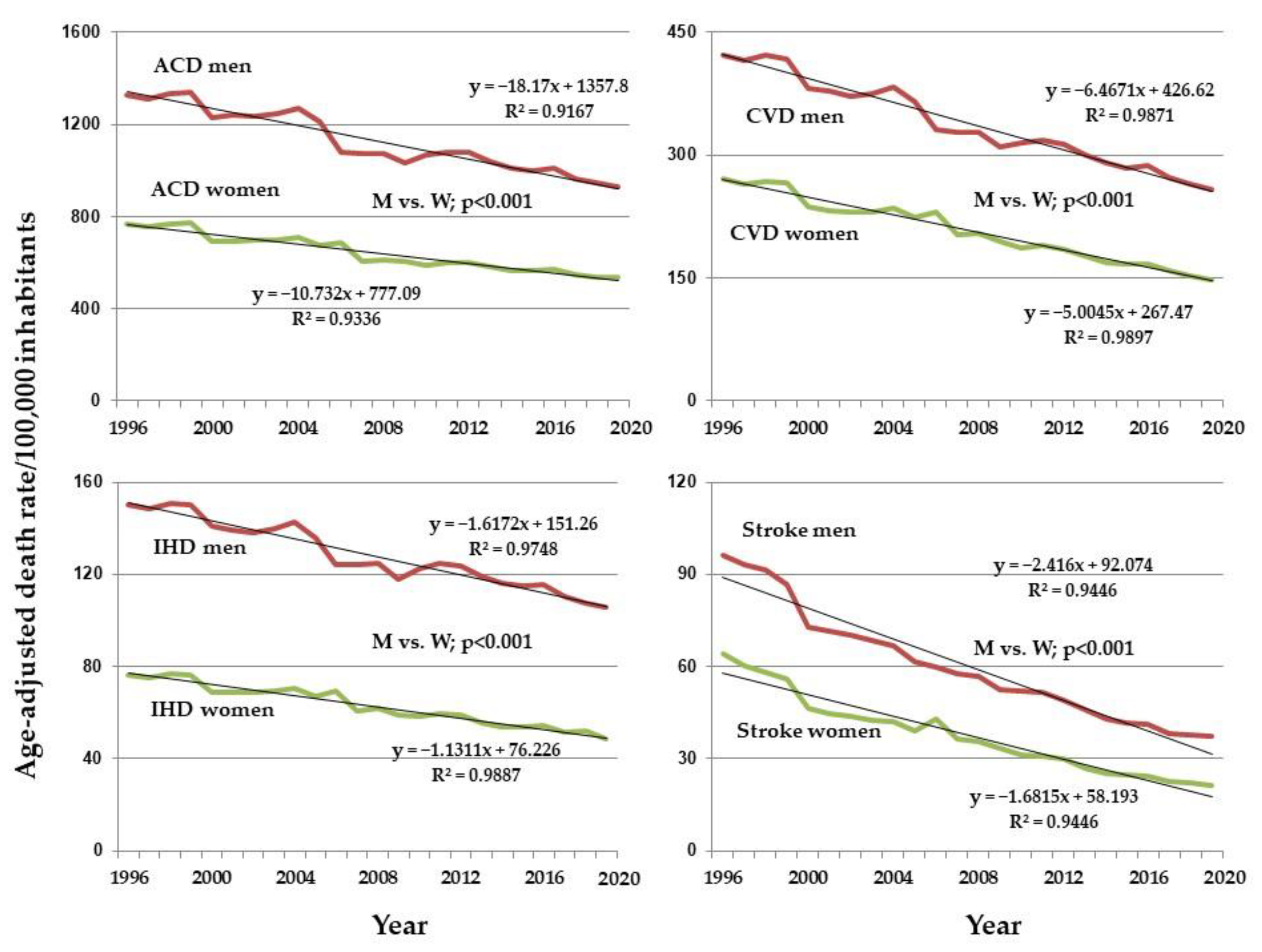
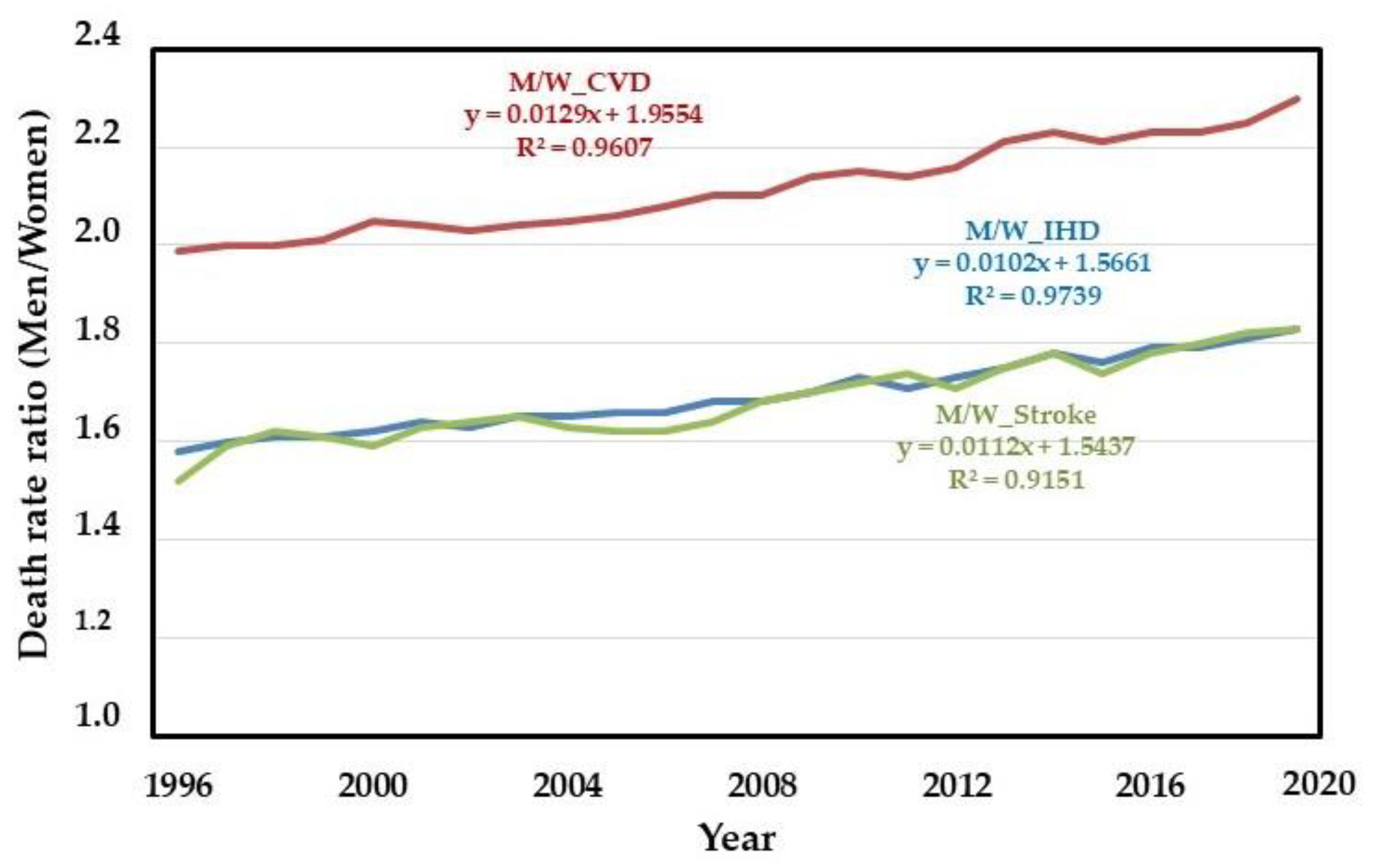
3. Results
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef]
- GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Lopez-Jaramillo, P.; Joseph, P.; Lopez-Lopez, J.P.; Lanas, F.; Avezum, A.; Diaz, R.; Yusuf, S. Risk factors, cardiovascular disease, and mortality in South America: A PURE substudy. Eur. Heart J. 2022, 43, 2841–2851. [Google Scholar] [CrossRef]
- Souza, M.F.M.; Alencar, A.P.; Malta, D.C.; Moura, L.; Mansur, A.P. Serial temporal analysis of ischemic heart disease and stroke death risk in five regions of Brazil from 1981 to 2001. Arq. Bras. Cardiol. 2006, 87, 735–740. [Google Scholar]
- Mansur, A.P.; Favarato, D. Trends in Mortality Rate from Cardiovascular Disease in Brazil, 1980–2012. Arq. Bras. Cardiol. 2016, 107, 20–25. [Google Scholar] [CrossRef]
- Shah, N.S.; Molsberry, R.; Rana, J.S.; Sidney, S.; Capewell, S.; O’Flaherty, M.; Carnethon, M.; Lloyd-Jones, D.M.; Khan, S.S. Heterogeneous trends in burden of heart disease mortality by subtypes in the United States, 1999–2018: Observational analysis of vital statistics. BMJ 2020, 370, m2688. [Google Scholar] [CrossRef]
- Emmerick, I.C.M.; Nascimento, J.M.; Pereira, M.A.; Luiza, V.L.; Ross-Degnan, D. Farmácia Popular Program: Changes in geographic accessibility of medicines during ten years of a medicine subsidy policy in Brazil. J. Pharm. Policy Pract. 2015, 8, 10. [Google Scholar] [CrossRef]
- Levy, D.; Almeida, L.M.; Szklo, A. The Brazil SimSmoke policy simulation model: The effect of strong tobacco control policies on smoking prevalence and smoking-attributable deaths in a middle income nation. PLoS Med. 2012, 9, e1001336. [Google Scholar] [CrossRef]
- da Saúde, M. Vigitel Brazil 2016 Private Health Insurance and Plans Beneficiaries: Protective and Risk Factors for Chronic Diseases by Telephone Survey; Ministério da Saúde: Brasília, Brazil, 2017. [Google Scholar]
- Lerner, D.J.; Kannel, W.B. Patterns of coronary heart disease morbidity and mortality in the sexes: A 26-year follow-up of the Framingham population. Am. Heart J. 1986, 111, 383–390. [Google Scholar] [CrossRef]
- Mansur, A.P.; Favarato, D. Cardiovascular and Cancer Death Rates in the Brazilian Population Aged 35 to 74 Years, 1996–2017. Taxas de Mortalidade por Doenças Cardiovasculares e Câncer na População Brasileira com Idade entre 35 e 74 Anos, 1996–2017. Arq. Bras. Cardiol. 2021, 117, 329–340. [Google Scholar] [CrossRef] [PubMed]
- Dai, H.; Much, A.A.; Maor, E.; Asher, E.; Younis, A.; Xu, Y.; Lu, Y.; Liu, X.; Shu, J.; Bragazzi, N.L. Global, regional, and national burden of ischemic heart disease and its attributable risk factors, 1990–2017: Results from the global Burden of Disease Study 2017. Eur. Heart J. Qual. Care Clin. Outcomes 2020, 8, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Cardiovascular Diseases Collaboration; Roth, G.A.; Johnson, C.O.; Abate, K.H.; Abd-Allah, F.; Ahmed, M.; Alam, K. The Burden of Cardiovascular Diseases Among US States, 1990–2016. JAMA Cardiol. 2018, 3, 375–389. [Google Scholar] [PubMed]
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ukwaja, K.N. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1–25. [Google Scholar] [CrossRef]
- Brasil. Ministério da Saúde. DATASUS. Brasília. 2021. Available online: http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sim/cnv/obt10uf.def (accessed on 30 January 2021).
- National Cancer Institute Division of Cancer Control and Population Sciences. Joinpoint Regression Program, Version 4.7.0.0. 26 February 2019. Available online: https://surveillance.cancer.gov/joinpoint/ (accessed on 30 January 2020).
- Currell, G. Scientific Data Analysis; Oxford University Press: Oxford, UK, 2015; 352p, Excel Analysis; Available online: https://www.youtube.com/watch?v=myL_qzuLHTQ (accessed on 30 January 2021).
- Vogel, B.; Acevedo, M.; Appelman, Y.; Bairey Merz, C.N.; Chieffo, A.; Figtree, G.A.; Guerrero, M.; Kunadian, V.; Lam, C.S.P.; Maas, A.H.E.M.; et al. The Lancet women and cardiovascular disease Commission: Reducing the global burden by 2030. Lancet 2021, 397, 2385–2438. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- National Center for Health Statistics. Health, United States, 2017: With Special Feature on Mortality; National Center for Health Statistics: Hyattsville, MD, USA, 2018. Available online: https://www.cdc.gov/nchs/data/hus/hus17.pdf (accessed on 1 April 2019).
- Timmis, A.; Townsend, N.; Gale, C.P.; Torbica, A.; Lettino, M.; Petersen, S.E.; Mossialos, E.A.; Maggioni, A.P.; Kazakiewicz, D.; May, H.T.; et al. European Society of Cardiology. European Society of Cardiology: Cardiovascular Disease Statistics 2019. Eur. Heart J 2020, 41, 12–85. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- Santos, R.D.; Bensenor, I.M.; Pereira, A.C.; Lotufo, P.A. Dyslipidemia according to gender and race: The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). J. Clin. Lipidol. 2016, 10, 1362–1368. [Google Scholar] [CrossRef] [PubMed]
- Pesquisa Nacional de Saúde 2013: Percepção do Estado de Saúde, Estilos de vida e Doenças Crônicas. Available online: https://biblioteca.ibge.gov.br/visualizacao/livros/liv94074.pdf (accessed on 23 June 2021).
- Bardach, A.; Alcaraz, A.; Roberti, J.; Ciapponi, A.; Augustovski, F.; Pichon-Riviere, A. Optimizing Tobacco Advertising Bans in Seven Latin American Countries: Microsimulation Modeling of Health and Financial Impact to Inform Evidence-Based Policy. Int. J. Environ. Res. Public Health 2021, 18, 5078. [Google Scholar] [CrossRef]
- Wang, L.; Li, X.; Wang, Z.; Bancks, M.P.; Carnethon, M.R.; Greenland, P.; Feng, Y.Q.; Wang, H.; Zhong, V.W. Trends in Prevalence of Diabetes and Control of Risk Factors in Diabetes Among US Adults, 1999–2018. JAMA 2021, 326, 704–716. [Google Scholar] [CrossRef]
- Malta, D.C.; Teixeira, R.; Oliveira, G.M.M.; Ribeiro, A.L.P. Cardiovascular Disease Mortality According to the Brazilian Information System on Mortality and the Global Burden of Disease Study Estimates in Brazil, 2000–2017. Arq. Bras. Cardiol. 2020, 115, 152–160. [Google Scholar]

| Cause of Death | Year | DRaj | Year | DRaj | AAPC | 99%CL | |
|---|---|---|---|---|---|---|---|
| ACD—0 Jp | 1996 | 1032.2 | 2019 | 721.79 | −1.6 * | −1.8 | −1.5 |
| ACD Men—3 Jp | 1996 | 1327.4 | 2004 | 1268.2 | −0.9 * | −1.6 | −0.1 |
| ACD Men—3 Jp | 2004 | 1268.2 | 2007 | 1071.8 | −5.1 | −11 | 1.1 |
| ACD Men—3 Jp | 2007 | 1071.8 | 2012 | 1077 | 0.2 | −1.7 | 2.1 |
| ACD Men—3 Jp | 2012 | 1077 | 2019 | 930.72 | −1.9 * | −2.7 | −1.2 |
| ACD Women—0 Jp | 1996 | 764.76 | 2019 | 721.79 | −1.6 * | −1.8 | −1.5 |
| CVD—0 Jp | 1996 | 342.85 | 2019 | 199.47 | −2.4 * | −2.5 | −2.2 |
| CVD Men—0 Jp | 1996 | 421.96 | 2019 | 258.03 | −2.1 * | −2.3 | −2 |
| CVD Women—0 Jp | 1996 | 270.84 | 2019 | 148.23 | −2.6 * | −2.8 | −2.4 |
| IHD—0 Jp | 1996 | 111.46 | 2019 | 75.15 | −1.7 * | −1.9 | −1.5 |
| IHD Men—0 Jp | 1996 | 150.23 | 2019 | 105.6 | −1.5 * | −1.7 | −1.3 |
| IHD Women—0 Jp | 1996 | 76.25 | 2019 | 48.29 | −1.9 * | −2.1 | −1.7 |
| Stroke—0 Jp | 1996 | 79.19 | 2019 | 28.62 | −4.3 * | −4.6 | −4.1 |
| Stroke Men—1 Jp | 1996 | 96.02 | 2001 | 71.57 | −5.9 * | −7.6 | −4.1 |
| Stroke Men—1 Jp | 2001 | 71.57 | 2019 | 37.1 | −3.8 * | −4.1 | −3.5 |
| Stroke Women—0 Jp | 1996 | 64.31 | 2019 | 21.39 | −4.6 * | −4.9 | −4.4 |
| Year | ACD | ACD Men | ACD Women | M/W ACD | CVD | CVD Men | CVD Women | M/W CVD | IHD | IHD Men | IHD Women | M/W IHD | Stroke | Stroke Men | Stroke Women | M/W Stroke |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1996 | 1032.24 | 1327.36 | 764.76 | 1.73 | 345.65 | 430.63 | 271.29 | 1.58 | 112.32 | 152.87 | 76.53 | 1.99 | 80.4 | 98.8 | 64.58 | 1.52 |
| 1997 | 1018.8 | 1310.72 | 754.19 | 1.73 | 332.98 | 417.15 | 259.53 | 1.6 | 108.66 | 148.25 | 73.8 | 2.00 | 75.53 | 94.43 | 59.36 | 1.59 |
| 1998 | 1038.12 | 1335.37 | 768.78 | 1.73 | 329.61 | 414.23 | 255.96 | 1.61 | 108.31 | 147.65 | 73.72 | 2.00 | 71.74 | 90.55 | 55.65 | 1.62 |
| 1999 | 1044.04 | 1341.6 | 774.38 | 1.73 | 320.31 | 402.7 | 248.95 | 1.61 | 105.67 | 144.5 | 71.62 | 2.01 | 66.97 | 84.37 | 52.23 | 1.61 |
| 2000 | 947.05 | 1230.61 | 694.99 | 1.77 | 312.32 | 393.65 | 242.08 | 1.62 | 105.11 | 144.96 | 70.37 | 2.05 | 60.62 | 75.93 | 47.66 | 1.59 |
| 2001 | 950.56 | 1238.86 | 694.44 | 1.78 | 302.6 | 383.43 | 233 | 1.64 | 102.42 | 141.02 | 68.88 | 2.04 | 57.94 | 73.45 | 44.91 | 1.63 |
| 2002 | 950.29 | 1236.21 | 696.25 | 1.77 | 293.14 | 370.97 | 226.47 | 1.63 | 100.14 | 137.56 | 67.75 | 2.03 | 56 | 71.18 | 43.28 | 1.64 |
| 2003 | 956.18 | 1247.73 | 697.18 | 1.78 | 289.91 | 368.81 | 222.43 | 1.65 | 99.28 | 136.91 | 66.83 | 2.04 | 53.43 | 68.18 | 41.09 | 1.65 |
| 2004 | 971.91 | 1268.24 | 708.56 | 1.78 | 290.18 | 369.09 | 222.82 | 1.65 | 99.32 | 137.14 | 66.73 | 2.05 | 51.44 | 65.23 | 39.96 | 1.63 |
| 2005 | 929.7 | 1214.74 | 676.4 | 1.79 | 274.89 | 350.44 | 210.59 | 1.66 | 93.69 | 129.6 | 62.85 | 2.06 | 47.22 | 59.84 | 36.74 | 1.62 |
| 2006 | 882.62 | 1080.01 | 685.65 | 1.57 | 277.62 | 354.03 | 212.69 | 1.66 | 95.37 | 132.41 | 63.65 | 2.08 | 51.01 | 64.56 | 39.75 | 1.62 |
| 2007 | 826.14 | 1071.8 | 605.89 | 1.76 | 271.32 | 347.83 | 206.5 | 1.68 | 93.82 | 130.88 | 62.14 | 2.1 | 48.42 | 61.68 | 37.44 | 1.64 |
| 2008 | 830.36 | 1073.61 | 611.06 | 1.75 | 269.73 | 345.68 | 205.51 | 1.68 | 93.93 | 131.1 | 62.24 | 2.1 | 47.28 | 60.8 | 36.09 | 1.68 |
| 2009 | 811.47 | 1035.07 | 604.95 | 1.71 | 259.86 | 335.4 | 196.15 | 1.7 | 90.51 | 127.3 | 59.22 | 2.14 | 44.57 | 57.61 | 33.87 | 1.7 |
| 2010 | 813.4 | 1066.34 | 590.27 | 1.8 | 255.18 | 331.04 | 191.35 | 1.73 | 90.94 | 127.99 | 59.5 | 2.15 | 42.61 | 55.4 | 32.1 | 1.72 |
| 2011 | 826.19 | 1081.02 | 601.41 | 1.79 | 252 | 326.22 | 189.68 | 1.71 | 90.62 | 127.55 | 59.36 | 2.14 | 41.18 | 53.75 | 30.88 | 1.74 |
| 2012 | 823.73 | 1077.03 | 600.31 | 1.79 | 241.2 | 313.31 | 180.68 | 1.73 | 87.63 | 123.65 | 57.16 | 2.16 | 38.42 | 49.81 | 29.1 | 1.71 |
| 2013 | 795.49 | 1038.66 | 580.19 | 1.79 | 236.63 | 309.23 | 175.93 | 1.75 | 86.26 | 122.73 | 55.51 | 2.21 | 36.23 | 47.48 | 27.05 | 1.75 |
| 2014 | 774.08 | 1011.47 | 563.68 | 1.79 | 228.78 | 300.69 | 168.72 | 1.78 | 83.97 | 119.95 | 53.7 | 2.23 | 33.88 | 44.67 | 25.08 | 1.78 |
| 2015 | 769.28 | 998.84 | 565.55 | 1.76 | 225.53 | 295.14 | 167.47 | 1.76 | 83.8 | 119.39 | 53.89 | 2.21 | 33.17 | 43.45 | 24.83 | 1.74 |
| 2016 | 775.63 | 1009.32 | 568.33 | 1.77 | 227.99 | 300.67 | 167.64 | 1.79 | 84.5 | 120.76 | 54.15 | 2.23 | 32.82 | 43.31 | 24.32 | 1.78 |
| 2017 | 744.67 | 964.96 | 548.76 | 1.75 | 217.06 | 286.06 | 159.79 | 1.79 | 80.98 | 115.86 | 51.79 | 2.23 | 30.58 | 40.54 | 22.52 | 1.8 |
| 2018 | 730.66 | 946.19 | 538.78 | 1.75 | 210.38 | 278.82 | 153.66 | 1.81 | 78.88 | 113.24 | 50.18 | 2.25 | 30.23 | 40.31 | 22.09 | 1.82 |
| 2019 | 721.79 | 930.72 | 535.64 | 1.73 | 205.38 | 273.56 | 149.02 | 1.83 | 77.26 | 111.72 | 48.53 | 2.3 | 29.65 | 39.65 | 21.61 | 1.83 |
| % | −30 * | −30 * | −30 * | 0 | −41 * | −36 * | −45 * | 14 * | −31 * | −27 * | −37 * | 13 * | −63 * | −60 * | −67 * | 17 * |
| All Causes of Death | Cardiovascular Diseases | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age Group | 1996 | 2019 | % Change | AAPC (%) | 99%CL | 1996 | 2019 | % Change | AAPC (%) | 99%CL | ||
| Total population | ||||||||||||
| 35–39 | 300.42 | 197.93 | −34 | −1.8 * | −2.1 | −1.5 | 45.03 | 25.92 | −47 | −2.4 * | −2.6 | −2.1 |
| 40–44 | 396.28 | 256.92 | −35 | −1.9 * | −2.1 | −1.7 | 84.67 | 46.59 | −47 | −2.7 * | −3.5 | −1.8 |
| 45–49 | 540.39 | 366.81 | −32 | −1.6 * | −2.0 | −1.3 | 145.27 | 82.49 | −46 | −2.4 * | −2.6 | −2.2 |
| 50–54 | 770.39 | 549.14 | −29 | −1.5 * | −1.8 | −1.1 | 238.53 | 140.98 | −43 | −2.2 * | −2.8 | −1.5 |
| 55–59 | 1104.86 | 789.71 | −29 | −1.5 * | −1.8 | −1.2 | 376.47 | 216.72 | −44 | −2.4 * | −2.7 | −2.2 |
| 60–64 | 1708.75 | 1247.23 | −27 | −1.3 * | −1.5 | −1.1 | 623.51 | 371.07 | −41 | −2.1 * | −2.2 | −2.0 |
| 65–69 | 2564.01 | 1885.53 | −26 | −1.4 * | −1.6 | −1.3 | 961.78 | 584.24 | −39 | −2.2 * | −2.6 | −1.8 |
| 70–74 | 3990.69 | 2948.01 | −26 | −1.3 * | −1.7 | −0.9 | 1548.07 | 942.15 | −40 | −2.0 * | −2.4 | −1.7 |
| Men | ||||||||||||
| 35–39 | 436.05 | 274.91 | −37 | −1.9 * | −2.3 | −1.5 | 53.95 | 31.93 | −41 | −2.3 * | −2.7 | −1.9 |
| 40–44 | 551.57 | 345.64 | −37 | −2.0 * | −2.2 | −1.8 | 104.83 | 58.50 | −44 | −2.6 * | −3.4 | −1.7 |
| 45–49 | 719.94 | 489.43 | −32 | −1.6 * | −2.0 | −1.3 | 179.69 | 104.09 | −42 | −2.4 * | −2.7 | −2.1 |
| 50–54 | 1002.23 | 736.42 | −27 | −1.3 * | −1.7 | −0.9 | 298.70 | 189.84 | −36 | −1.9 * | −2.5 | −1.4 |
| 55–59 | 1411.88 | 1052.21 | −25 | −1.3 * | −1.6 | −1.0 | 475.70 | 295.14 | −38 | −2.1 * | −2.4 | −1.8 |
| 60–64 | 2173.83 | 1651.83 | −24 | −1.1 * | −1.3 | −0.9 | 788.36 | 506.34 | −36 | −1.8 * | −1.9 | −1.6 |
| 65–69 | 3240.26 | 2470.58 | −24 | −1.3 * | −1.4 | −1.1 | 1195.81 | 779.52 | −35 | −1.8 * | −1.9 | −1.7 |
| 70–74 | 5060.29 | 3858.00 | −24 | −1.2 * | −1.6 | −0.7 | 1907.36 | 1249.21 | −35 | −1.7 * | −1.9 | −1.5 |
| Women | ||||||||||||
| 35–39 | 171.13 | 122.89 | −28 | −1.4 * | −1.6 | −1.2 | 36.53 | 20.06 | −45 | −2.5 * | −2.9 | −2.2 |
| 40–44 | 248.24 | 173.18 | −30 | −1.7 * | −2.3 | −1.1 | 65.45 | 35.35 | −46 | −2.6 * | −3.7 | −1.5 |
| 45–49 | 369.21 | 254.79 | −31 | −1.5 * | −1.7 | −1.3 | 112.45 | 62.76 | −44 | −2.5 * | −2.6 | −2.4 |
| 50–54 | 551.42 | 381.76 | −31 | −1.6 * | −2.0 | −1.2 | 181.71 | 97.33 | −46 | −2.5 * | −3.4 | −1.5 |
| 55–59 | 821.84 | 561.60 | −32 | −1.7 * | −2.0 | −1.4 | 285.00 | 148.58 | −48 | −2.8 * | −3.1 | −2.5 |
| 60–64 | 1295.04 | 907.28 | −30 | −1.4 * | −1.6 | −1.3 | 476.87 | 257.42 | −46 | −2.5 * | −2.6 | −2.4 |
| 65–69 | 1990.76 | 1415.45 | −29 | −1.6 * | −1.7 | −1.4 | 763.39 | 427.35 | −44 | −2.5 * | −2.8 | −2.3 |
| 70–74 | 3141.90 | 2266.47 | −28 | −1.3 * | −1.9 | −0.8 | 1262.95 | 712.18 | −44 | −2.3 * | −2.7 | −1.9 |
| Ischemic Heart Disease | Stroke | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age Group | 1996 | 2019 | % Change | AAPC | CI 99% | 1996 | 2019 | % Change | AAPC | CI 99% | ||
| (%) | (%) | |||||||||||
| Total Population | ||||||||||||
| 35–39 | 12.58 | 8.08 | −36 | −1.7 * | −2.4 | −1.1 | 6.29 | 1.96 | −69 | −5.0 * | −5.6 | −4.4 |
| 40–44 | 25.4 | 16.42 | −35 | −2.1 * | −2.9 | −1.3 | 13.83 | 3.58 | −74 | −5.5 * | −5.9 | −5 |
| 45–49 | 47 | 30.49 | −35 | −1.9 * | −2.4 | −1.4 | 27.92 | 8.11 | −71 | −5.4 * | −5.8 | −5.1 |
| 50–54 | 79.16 | 56.13 | −29 | −1.6 * | −1.7 | −1.4 | 49.95 | 15.14 | −70 | −5.3 * | −5.7 | −5 |
| 55–59 | 128.75 | 88.71 | −31 | −1.7 * | −1.9 | −1.4 | 83.49 | 25.45 | −70 | −5.0 * | −5.3 | −4.8 |
| 60–64 | 214.58 | 149.71 | −30 | −1.4 * | −1.5 | −1.2 | 142.88 | 50.89 | −64 | −4.3 * | −4.6 | −4.1 |
| 65–69 | 316.39 | 219.49 | −31 | −1.5 * | −1.6 | −1.4 | 237.74 | 95.28 | −60 | −3.9 * | −4.1 | −3.6 |
| 70–74 | 474.08 | 325.67 | −31 | −1.6 * | −1.8 | −1.3 | 413.86 | 176.15 | −57 | −3.4 * | −3.6 | −3.1 |
| Men | ||||||||||||
| 35–39 | 17.88 | 11.9 | −33 | −1.8 * | −2.4 | −1.1 | 6.72 | 1.97 | −71 | −5.1 * | −6.2 | −4 |
| 40–44 | 37.26 | 23.8 | −36 | −2.1 * | −2.9 | −1.4 | 15.84 | 3.93 | −75 | −5.7 * | −6.4 | −4.9 |
| 45–49 | 66.99 | 44.11 | −34 | −1.7 * | −2.1 | −1.3 | 31.64 | 9.39 | −70 | −5.1 * | −5.7 | −4.6 |
| 50–54 | 114.01 | 84.76 | −26 | −1.4 * | −1.6 | −1.2 | 58.44 | 18.8 | −68 | −4.9 * | −5.9 | −3.8 |
| 55–59 | 178.91 | 130.63 | −27 | −1.5 * | −1.8 | −1.2 | 103.29 | 34.39 | −67 | −5.0 * | −6 | −4 |
| 60–64 | 292.15 | 220.01 | −25 | −1.0 * | −1.2 | −0.9 | 178.53 | 69.16 | −61 | −4.0 * | −5 | −3 |
| 65–69 | 419.01 | 311.17 | −26 | −1.2 * | −1.3 | −1.1 | 297.89 | 130.9 | −56 | −3.6 * | −4.6 | −2.7 |
| 70–74 | 619 | 458.82 | −26 | −1.2 * | −1.5 | −0.9 | 515.64 | 240.4 | −53 | −3.4 * | −3.9 | −3 |
| Women | ||||||||||||
| 35–39 | 7.53 | 4.35 | −42 | −1.4 * | −1.8 | −1 | 5.88 | 1.95 | −67 | −5.6 * | −6.5 | −4.7 |
| 40–44 | 14.09 | 9.46 | −33 | −2.0 * | −3.1 | −0.9 | 11.91 | 3.25 | −73 | −5.3 * | −7.1 | −3.5 |
| 45–49 | 27.94 | 18.05 | −35 | −1.6 * | −1.9 | −1.4 | 24.38 | 6.94 | −72 | −5.8 * | −6.7 | −5 |
| 50–54 | 46.25 | 30.54 | −34 | −1.8 * | −2.2 | −1.3 | 41.93 | 11.88 | −72 | −5.3 * | −6.4 | −4.2 |
| 55–59 | 82.52 | 52.28 | −37 | −1.8 * | −2 | −1.6 | 65.23 | 17.68 | −73 | −5.5 * | −6.4 | −4.7 |
| 60–64 | 145.58 | 90.64 | −38 | −1.9 * | −2 | −1.7 | 111.17 | 35.54 | −68 | −4.7 * | −5.7 | −3.7 |
| 65–69 | 229.4 | 145.83 | −36 | −1.9 * | −2 | −1.8 | 186.74 | 66.66 | −64 | −4.6 * | −5.7 | −3.5 |
| 70–74 | 359.08 | 225.95 | −37 | −1.9 * | −2 | −1.8 | 333.09 | 128.04 | −62 | −4.1 * | −4.7 | −3.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mansur, A.d.P.; Favarato, D.; Strunz, C.M.C.; Avakian, S.D.; Pereira-Barretto, A.C.; Bocchi, E.A.; César, L.A.M. Sex Differences in Cardiovascular Disease Mortality in Brazil between 1996 and 2019. Int. J. Environ. Res. Public Health 2022, 19, 12827. https://doi.org/10.3390/ijerph191912827
Mansur AdP, Favarato D, Strunz CMC, Avakian SD, Pereira-Barretto AC, Bocchi EA, César LAM. Sex Differences in Cardiovascular Disease Mortality in Brazil between 1996 and 2019. International Journal of Environmental Research and Public Health. 2022; 19(19):12827. https://doi.org/10.3390/ijerph191912827
Chicago/Turabian StyleMansur, Antonio de Padua, Desidério Favarato, Célia Maria Cassaro Strunz, Solange Desirée Avakian, Antonio Carlos Pereira-Barretto, Edimar Alcides Bocchi, and Luiz Antonio Machado César. 2022. "Sex Differences in Cardiovascular Disease Mortality in Brazil between 1996 and 2019" International Journal of Environmental Research and Public Health 19, no. 19: 12827. https://doi.org/10.3390/ijerph191912827
APA StyleMansur, A. d. P., Favarato, D., Strunz, C. M. C., Avakian, S. D., Pereira-Barretto, A. C., Bocchi, E. A., & César, L. A. M. (2022). Sex Differences in Cardiovascular Disease Mortality in Brazil between 1996 and 2019. International Journal of Environmental Research and Public Health, 19(19), 12827. https://doi.org/10.3390/ijerph191912827








