The Role of Staff-Assessed Care Quality in the Relationship between Job Demands and Stress in Human Service Work: The Example of Dentistry
Abstract
1. Introduction
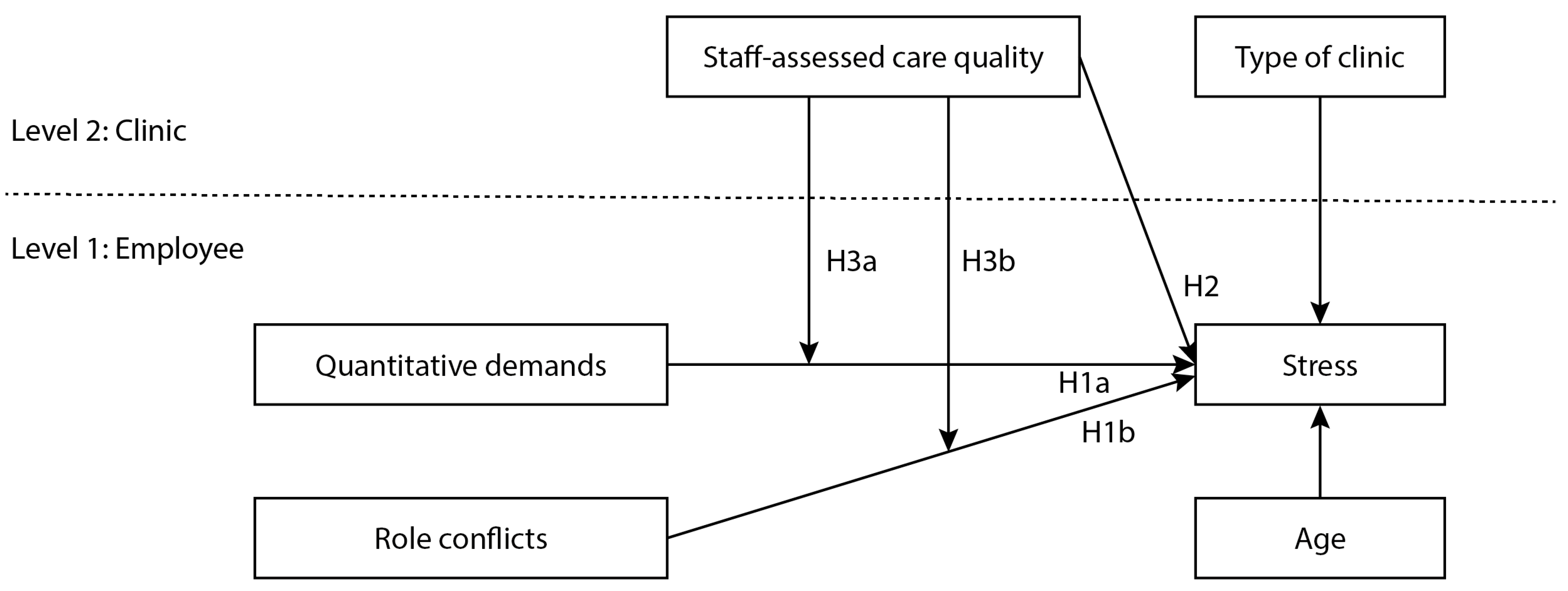
Aim/Hypotheses
2. Materials and Methods
2.1. Study Population
2.2. Measures
2.3. Data Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dollard, M.F.; Winefield, H.R.; Winefield, A.H. Occupational Strain and Efficacy in Human Service Workers: When the Rescuer Becomes the Victim; Kluwer Academic Publishers: Dordrecht, The Netherlands, 2001; pp. 1–12. ISBN 0-7923-6852-5. [Google Scholar]
- Bretherton, R.; Chapman, H.R.; Chipchase, S. A study to explore specific stressors and coping strategies in primary dental care practice. Br. Dent. J. 2016, 220, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Locker, D. Work stress, job satisfaction and emotional well-being among Canadian dental assistants. Community Dent. Oral Epidemiol. 1996, 24, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Myers, H.; Myers, L. It’s difficult being a dentist: Stress and health in the general dental practitioner. Br. Dent. J. 2004, 197, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.; Coward, P.; Capewell, J.; Laidler, T.L.; Rigby, A.C.; Shaw, T.J. Perceived sources of occupational stress in general dental practitioners. Br. Dent. J. 1998, 184, 499–502. [Google Scholar] [CrossRef]
- Gorter, R.C.; Freeman, R. Burnout and engagement in relation with job demands and resources among dental staff in Northern Ireland. Community Dent. Oral Epidemiol. 2011, 39, 87–95. [Google Scholar] [CrossRef]
- Moore, R.; Brødsgaard, I. Dentists’ perceived stress and its relation to perceptions about anxious patients. Community Dent. Oral Epidemiol. 2001, 29, 73–80. [Google Scholar] [CrossRef]
- Murray, E.; Kutzer, Y.; Lusher, J. Dentists’ experiences of dentally anxious patients in a specialist setting: An interpretative phenomenological analysis. J. Health Psychol. 2019, 24, 288–298. [Google Scholar] [CrossRef]
- Hasenfeld, Y. The attributes of Human Service Organizations. In Human Services as Complex Organizations, 2nd ed.; Hasenfeld, Y., Ed.; Sage Publications: London, UK, 2010; pp. 291–310. ISBN 781412956949. [Google Scholar]
- Geisler, M.; Berthelsen, H.; Hakanen, J.J. No job demand is an island–Interaction effects between emotional demands and other types of job demands. Front. Psychol. 2019, 10, 873. [Google Scholar] [CrossRef]
- Ayers, K.M.S.; Thomson, W.M.; Newton, J.T.; Rich, A.M. Job stressors of New Zealand dentists and their coping strategies. Occup. Med. 2008, 58, 275–281. [Google Scholar] [CrossRef]
- Marklund, S.; Huang, K.; Zohouri, D.; Wahlström, J. Dentists working conditions—Factors associated with perceived workload. Acta Odontol. Scand. 2020, 79, 296–301. [Google Scholar] [CrossRef]
- Hakanen, J.J.; Seppälä, P.; Peeters, M.C.W. High Job Demands, Still Engaged and Not Burned Out? The Role of Job Crafting. Int. J. Behav. Med. 2017, 24, 619–627. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.L.; Mallinger, M.; Kahn, R. Identifying sources of occupational stress among dentists. J. Occup. Psychol. 1978, 51, 227–234. [Google Scholar] [CrossRef]
- Crawford, L.; Gutierrez, G.; Harber, P. Work Environment and Occupational Health of Dental Hygienists: A Qualitative Assessment. J. Occup. Environ. Med. 2005, 47, 623–632. [Google Scholar] [CrossRef]
- LaPorta, L.D. Occupational stress in oral and maxillofacial surgeons: Tendencies, traits, and triggers. Oral Maxillofac. Surg. Clin. N. Am. 2010, 22, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Burr, H.; Berthelsen, H.; Moncada, S.; Nübling, M.; Dupret, E.; Demiral, Y.; Oudyk, J.; Kristensen, T.S.; Llorens, C.; Navarro, A.; et al. The third version of the Copenhagen Psychosocial Questionnaire. Saf. Health Work 2019, 10, 482–503. [Google Scholar] [CrossRef]
- Carneiro, S.C.A.; Vasconcelos, B.C.; Nascimiento, M.M.M.; Leal, J.L.F.; Orestes, M.S.; Porto, G.G. Occupational stress among Brazilian oralmaxillofacial surgeons. Med. Oral Patol. Oral Cir. Bucal 2009, 14, e646–e649. [Google Scholar] [CrossRef]
- Semmer, N.; Jacobshagen, N.; Meier, L.; Elfering, A. Occupational stress research: The Stress-As-Offense-To-Self Perspective. In Occupational Health Psychology: European Perspectives on Research, Education and Practice; McIntyre, S., Houdmont, J., Eds.; Nottingham University Press: Nottingham, UK, 2007; Volume 2, pp. 41–58. [Google Scholar] [CrossRef]
- Semmer, N.K.; Tschan, F.; Jacobshagen, N.; Beehr, T.A.; Elfering, A.; Kälin, W.; Meier, L.L. Stress as Offense to Self: A Promising Approach Comes of Age. Occup. Health Sci. 2019, 3, 205–238. [Google Scholar] [CrossRef]
- Semmer, N.K.; Jacobshagen, N.; Meier, L.L.; Elfering, A.; Beehr, T.A.; Kälin, W.; Tschan, F. Illegitimate tasks as a source of work stress. Work Stress 2015, 29, 32–56. [Google Scholar] [CrossRef]
- Thun, S.; Halsteinli, V.; Løvseth, L. A study of unreasonable illegitimate tasks, administrative tasks, and sickness presenteeism amongst Norwegian physicians: An everyday struggle? BMC Health Serv. Res. 2018, 18, 407. [Google Scholar] [CrossRef]
- Bodenheimer, T.; Sinsky, C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann. Fam. Med. 2014, 12, 573–576. [Google Scholar] [CrossRef]
- Dewa, C.S.; Loong, D.; Bonato, S.; Trojanovski, L.; Rea, M. The relationship between resident burnout and safety-related and acceptability-related quality of healthcare: A systematic literature review. BMC Med. Educ. 2017, 17, 195. [Google Scholar] [CrossRef] [PubMed]
- Salyers, M.P.; Bonfils, K.A.; Luther, L.; Firmin, R.L.; White, D.A.; Adams, E.L.; Rollins, A.L. The Relationship Between Professional Burnout and Quality and Safety in Healthcare: A Meta-Analysis. J. Gen. Intern. Med. 2017, 32, 475–482. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; Organisation for Economic Co-Operation and Development; International Bank for Reconstruction; Development/The World Bank. Delivering Quality Health Services: A Global Imperative for Universal Health Coverage; World Health Organization, Organisation for Economic Co-operation and Development, & International Bank for Reconstruction and Development/The World Bank: Geneva, Switzerland, 2018; ISBN 9789241513906. Available online: https://apps.who.int/iris/handle/10665/272465 (accessed on 8 August 2022).
- Donabedian, A. The Quality of Care: How Can It Be Assessed? JAMA 1988, 260, 1742–1748. [Google Scholar] [CrossRef]
- Teoh, K.R.H.; Kinman, G.; Hassard, J. The Relationship Between Healthcare Staff Wellbeing and Patient Care: It’s Not That Simple. In Integrating the Organization of Health Services, Worker Wellbeing and Quality of Care; Tevik Løvseth, L., de Lange, A.H., Eds.; Springer: Cham, Switzerland, 2021; pp. 221–244. [Google Scholar] [CrossRef]
- Berthelsen, H.; Owen, M.; Wretlind, K.; Westerlund, H. Does staff-assessed care quality predict early failure of dental fillings? A prospective study. Community Dent. Oral Epidemiol. 2020, 48, 387–394. [Google Scholar] [CrossRef]
- Krämer, T.; Schneider, A.; Spieß, E.; Angerer, P.; Weigl, M. Associations between job demands, work-related strain and perceived quality of care: A longitudinal study among hospital physicians. Int. J. Qual. Health Care 2016, 28, 824–829. [Google Scholar] [CrossRef]
- Kravitz, A.; Bullock, A.; Cowpe, J.; Barnes, E. EU Manual of Dental Practice; Edition 5.1; Cardiff University: Wales, UK, 2015; pp. 1–420. [Google Scholar]
- Ordell, S.; Unell, L.; Söderfeldt, B. An analysis of present dental professions in Sweden. Swed. Dent. J. 2006, 30, 155–164. [Google Scholar]
- Berthelsen, H.; Westerlund, H.; Bergström, G.; Burr, H. Validation of the Copenhagen psychosocial questionnaire version III and establishment of benchmarks for psychosocial risk Management in Sweden. Int. J. Environ. Res. Public Health 2020, 17, 3179. [Google Scholar] [CrossRef]
- Berthelsen, H.; Conway, P.M.; Clausen, T. Is organizational justice climate at the workplace associated with individual-level quality of care and organizational affective commitment? A multi-level, cross-sectional study on dentistry in Sweden. Int. Arch. Occup. Environ. Health 2018, 91, 237–245. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Bliese, P.D. Group size, ICC values, and group-level correlations: A simulation. Organ. Res. Methods 1998, 1, 355–373. [Google Scholar] [CrossRef]
- Bliese, P.D. Within-group agreement, non-independence, and reliability: Implications for data aggregation and analysis. In Multilevel Theory, Research, and Methods in Organizations; Klein, K.J., Kozlowski, S.W., Eds.; Jossey-Bass: San Francisco, CA, USA, 2000; pp. 349–381. [Google Scholar]
- Bliese, P.D.; Maltarich, M.A.; Hendricks, J.L.; Hofmann, D.A.; Adler, A.B. Improving the measurement of group-level constructs by optimizing between-group differentiation. J. Appl. Psychol. 2019, 104, 293–302. [Google Scholar] [CrossRef] [PubMed]
- LeBreton, J.M.; Senter, J.L. Answers to 20 questions about interrater reliability and interrater agreement. Organ. Res. Methods 2007, 11, 815–852. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Fiabane, E.; Dordoni, P.; Setti, I.; Cacciatori, I.; Grossi, C.; Pistarini, C.; Argentero, P. Emotional dissonance and exhaustion among healthcare professionals: The role of the perceived quality of care. Int. J. Occup. Med. Environ. Health 2019, 32, 841–851. [Google Scholar] [CrossRef]
- Andrews, D.R.; Burr, J.; Bushy, A. Nurses’ Self-Concept and Perceived Quality of Care. J. Nurs. Care Qual. 2011, 26, 69–77. [Google Scholar] [CrossRef]
- Berthelsen, H.; Hjalmers, K.; Pejtersen, J.H.; Soderfeldt, B. Good Work for dentists—A qualitative analysis. Community Dent. Oral Epidemiol. 2010, 38, 159–170. [Google Scholar] [CrossRef]
- Wang, Y.; Gao, Y.; Xun, Y. Work engagement and associated factors among dental nurses in China. BMC Oral Health 2021, 21, 402. [Google Scholar] [CrossRef]
- Gorter, R.C.; Albrecht, G.; Hoogstraten, J.; Eijkman, M.A.J. Measuring work stress among Dutch dentists. Int. Dent. J. 1999, 49, 144–152. [Google Scholar] [CrossRef]
- Craven, R.C.; Blinkhorn, A.S.; Roberts, C. A survey of job stress and job satisfaction among DSAs in the north-west of England. Br. Dent. J. 1995, 178, 101–104. [Google Scholar] [CrossRef]
- Uziel, N.; Meyerson, J.; Birenzweig, Y.; Eli, I. Professional burnout and work stress among Israeli dental assistants. Psychol. Health Med. 2019, 24, 59–67. [Google Scholar] [CrossRef]
- Edwards, J.A.; Guppy, A.; Cockerton, T. A longitudinal study exploring the relationships between occupational stressors, non-work stressors, and work performance. Work Stress 2007, 21, 99–116. [Google Scholar] [CrossRef]
- Lang, R.J.; Gilpin, J.L.; Gilpin, A.R. Stress-Related Symptoms among Dental Hygienists. Psychol. Rep. 1990, 66, 715–722. [Google Scholar] [CrossRef] [PubMed]

| N | % | Mean (SD) | |
|---|---|---|---|
| Gender | |||
| Women | 936 | 92.5 | |
| Men | 76 | 7.5 | |
| Age (years) | 48.1 (11.3) | ||
| Weekly hours with patient contact | 29.9 (9.2) | ||
| Job profile | |||
| Dental nurses | 575 | 56.8 | |
| Dental hygienists | 200 | 19.8 | |
| Dentists | 237 | 23.4 |
| Scale | Occupation | Mean (SD) | p | Post Hoc Tests * |
|---|---|---|---|---|
| Quantitative demands | 1. Dental nurses | 43.2 (17.8) | ≤0.001 | |
| 2. Dental hygienists | 45.5 (16.5) | 3 > 2 | ||
| 3. Dentists | 54.5 (20.0) | 3 > 1 | ||
| Role conflicts | 1. Dental nurses | 33.9 (17.4) | ≤0.001 | |
| 2. Dental hygienists | 36.4 (16.2) | 3 > 2 | ||
| 3. Dentists | 44.2 (16.6) | 3 > 1 | ||
| Staff-assessed care quality | 1. Dental nurses | 83.0 (13.8) | ≤0.001 | 1 > 3 |
| 2. Dental hygienists | 80.5 (13.2) | 1 > 2 | ||
| 3. Dentists | 78.3 (14.4) | |||
| Stress | 1. Dental nurses | 28.3 (24.2) | ≤0.001 | |
| 2. Dental hygienists | 31.8 (24.2) | 3 > 2 | ||
| 3. Dentists | 38.1 (24.7) | 3 > 1 |
| Dental Nurses (N = 567/99) | Dentists (N = 235/90) | |
|---|---|---|
| B (SE) | B (SE) | |
| Model 1 (empty model) | ||
| Intercept | 28.35 (1.32) *** | 37.65 (1.91) ** |
| ICC | 0.12 | 0.18 |
| AIC | 5275.8 | 2180.6 |
| Model 2 (direct paths model) | ||
| Staff-assessed care quality (level 2) | −0.54 (0.18) ** | −1.27 (0.26) *** |
| Specialized practice (versus general) (level 2) | −3.27 (3.12) | 8.05 (4.56) |
| Age (level 1) | −0.28 (0.10) ** | −0.40 (0.12) *** |
| Role conflicts (level 1) | 0.26 (0.06) *** | 0.26 (0.12) * |
| Quantitative demands (level 1) | 0.22 (0.06) *** | 0.27 (0.10) ** |
| Intercept | 43.69 (5.38) *** | 52.97 (5.28) *** |
| ICC | 0.10 | 0.10 |
| AIC | 5161.55 | 2134.15 |
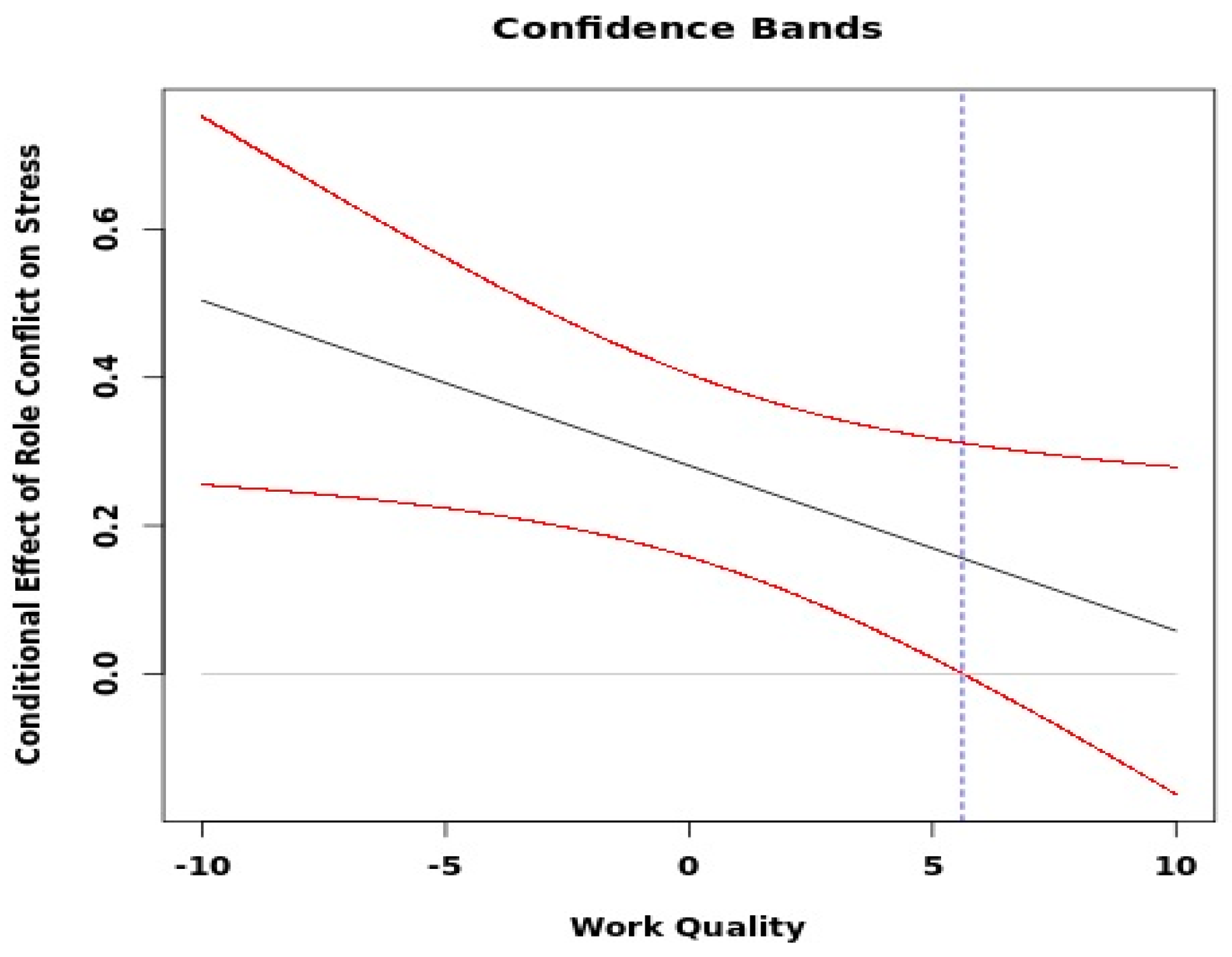
| Model 3 (moderated model) | ||
| Staff-assessed care quality (level 2) | −0.54 (0.18) ** | −1.27 (0.26) *** |
| Specialized practice (versus general) (level 2) | −3.28 (3.13) | 7.93 (4.57) |
| Age (level 1) | −0.28 (0.10) ** | −0.39 (0.12) ** |
| Role conflicts (level 1) | 0.28 (0.06) *** | 0.24 (0.13) |
| Quantitative demands (level 1) | 0.21 (0.06) *** | 0.27 (0.10) ** |
| Staff-assessed care quality * Role conflicts | −0.02 (0.01) * | 0.01 (0.02) |
| Staff-assessed care quality * Quantitative demands | −0.00 (0.01) | −0.02 (0.02) |
| Intercept | 43.39(5.37) | 52.49(5.32) |
| ICC | 0.10 | 0.10 |
| AIC | 5174.90 | 2149.26 |
| Model | Hypotheses | Dental Nurses | Dentists | |
|---|---|---|---|---|
| Model 2 (Direct paths model) | 1a | Individually rated quantitative demands are positively correlated with individually rated stress | Supported | Supported |
| 1b | Individually rated role conflicts are positively correlated with individually rated stress | Supported | Supported | |
| 2 | Staff-assessed care quality at the clinic is negatively correlated with individually rated stress | Supported | Supported | |
| Model 3 model (Moderated model) | 1a | Individually rated quantitative demands are positively correlated with individually rated stress | Supported | Supported |
| 1b | Individually rated role conflicts are positively correlated with individually rated stress | Supported | Not supported | |
| 2 | Staff-assessed care quality at the clinic is negatively correlated with individually rated stress | Supported | Supported | |
| 3a | Staff-assessed care quality at the clinic mitigates the relationship between individually rated quantitative demands and stress | Not supported | Not supported | |
| 3b | Staff-assessed care quality at the clinic mitigates the relationship between individually rated role conflicts and stress | Supported | Not supported | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karatuna, I.; Owen, M.; Westerlund, H.; Berthelsen, H. The Role of Staff-Assessed Care Quality in the Relationship between Job Demands and Stress in Human Service Work: The Example of Dentistry. Int. J. Environ. Res. Public Health 2022, 19, 12795. https://doi.org/10.3390/ijerph191912795
Karatuna I, Owen M, Westerlund H, Berthelsen H. The Role of Staff-Assessed Care Quality in the Relationship between Job Demands and Stress in Human Service Work: The Example of Dentistry. International Journal of Environmental Research and Public Health. 2022; 19(19):12795. https://doi.org/10.3390/ijerph191912795
Chicago/Turabian StyleKaratuna, Işıl, Mikaela Owen, Hugo Westerlund, and Hanne Berthelsen. 2022. "The Role of Staff-Assessed Care Quality in the Relationship between Job Demands and Stress in Human Service Work: The Example of Dentistry" International Journal of Environmental Research and Public Health 19, no. 19: 12795. https://doi.org/10.3390/ijerph191912795
APA StyleKaratuna, I., Owen, M., Westerlund, H., & Berthelsen, H. (2022). The Role of Staff-Assessed Care Quality in the Relationship between Job Demands and Stress in Human Service Work: The Example of Dentistry. International Journal of Environmental Research and Public Health, 19(19), 12795. https://doi.org/10.3390/ijerph191912795






