Breast Cancer Treatment in Integrated Care Process in Andalusia: The Challenge of Multidisciplinarity
Abstract
:1. Introduction
1.1. Epidemiologic Approach to Breast Cancer
1.2. Improvement in Survival Rates: Early Detection, Improvements in Treatment, and Greater Health System Efficiency
1.3. The Breast Pathology Units: A Key Site for the Improvement of Treatment and Its Functional and Structural Organisation
2. Materials and Methods
2.1. Research Design and Ethical Approval
2.2. Study Settings
2.3. Sample
2.3.1. Sample Inclusion Criteria
- Having at least 5 years of professional experience related to breast cancer care.
- Having Spanish nationality.
- Working in the public health system.
2.3.2. Recruitment of Participants
2.4. Data Collection
2.5. Analysis
2.6. Rigor
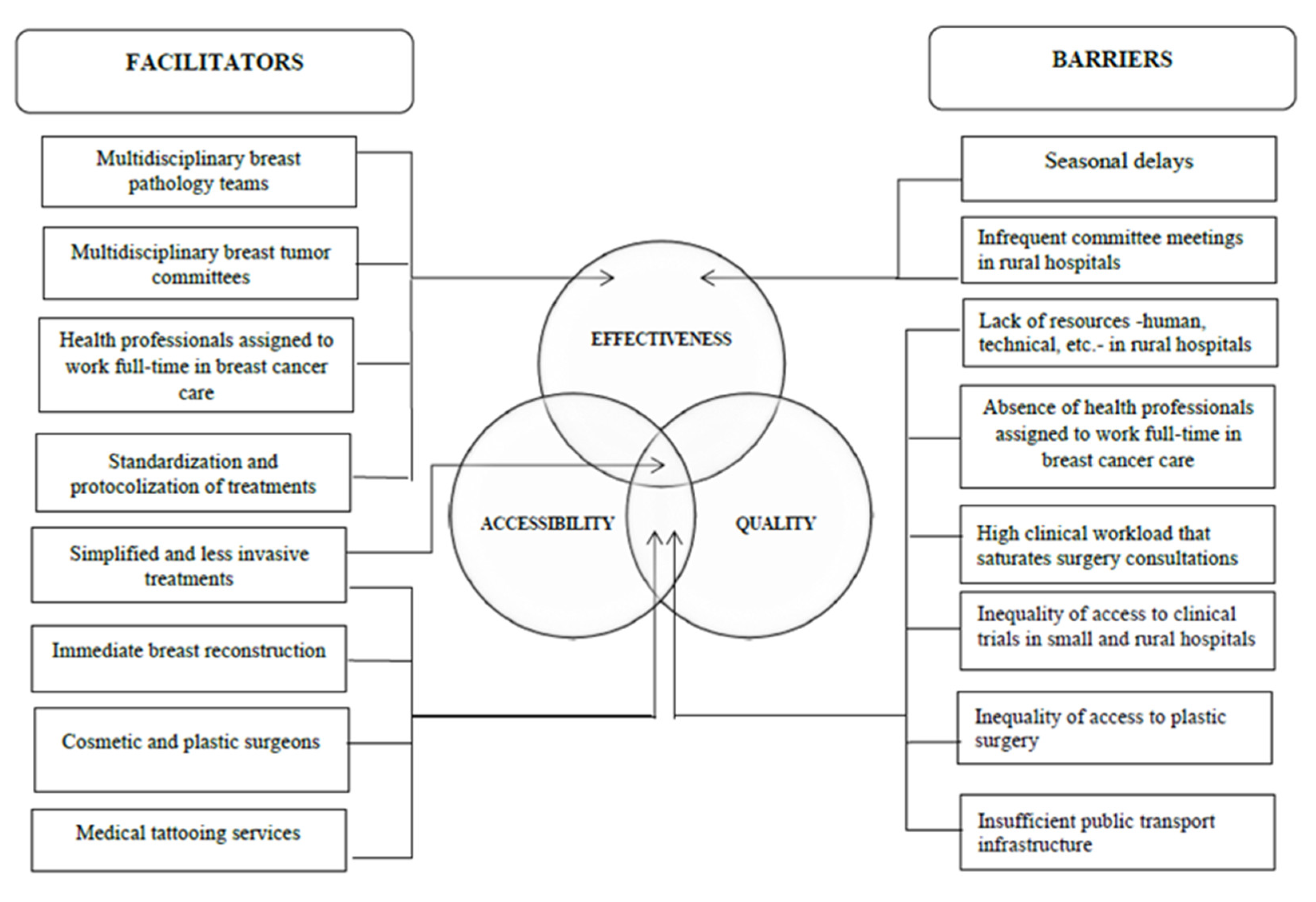
3. Results
3.1. The Therapeutic Strategy after Breast Cancer Diagnosis: Breast Pathology Units and Comprehensive Case Management
So it’s improved a lot, and the multidisciplinary management of breast cancer has improved a lot […]. The overall vision is much better.[RDHHU1]
I create an overall vision of things, not a committee where there’s only the surgeon and the radiologist, and they tie everything up between them. I always think that the more people, the better.[MNGHU1]
The only thing that didn’t happen in unison was the process [… ]. The Infanta Elena (Huelva hospital) has only just begun to treat breast cancer. And this started happening in 2016.[RDHHU1]
It was in 2006 when we set up the breast unit as it is here. The building work was done, and an ultrasound machine was bought because, later, the building work was extended with the merger, which brought in another ultrasound machine, and another mammographer.[RDHU1]
Why is gynaecology doing this and not surgery? Well, because it’s always been done that way […]. Traditionally we’ve done it, and we still do it ourselves. In other places, I know that only surgeons do it, and in other places, surgeons and gynaecologists. They all work just as well… many times for historical, traditional reasons rather than any other.[GGHU1]
A set of circumstances that made gynaecologists take charge of the breast cancer care process. I arrived in the 90s, and this was already underway. They were in charge of surgery and then systemic treatment.[RGHU2]
Systemic cancer treatment was performed by gynaecologists, not oncologists. Then we radiation oncologists did the radiation treatment. […] since the mid-1980s […]. Not now.[RGHU1]
But I think that… I don’t know; we’re still at the beginning. So far, there’s still some friction between gynaecologists and medical oncologists, but anyway, in the end, we all get along.[RGHU1]
When the cancer is confirmed, then what we do is staging through mammography and other complementary tests, resonances, etc., to decide which is the best treatment.[ORHHU1]
There’s the breast pathology consultant, the surgeon, who performs the clinical examination of the patient, which is very important. He’s the one who asks for the complementary tests and the extension study and the one who gives the final diagnosis of the pathological anatomy that you have a malignant tumour in the breast.[ORGHU2]
The extension study for us is a bone gammagraphy to see the bones, an abdominal echography to see the liver, and, in some cases, depending on the initial extension of the disease we see, a PET scan is requested, a positron emission tomography.[MNGHU1]
[…] women who have breast cancer are given a bone gammagraphy by protocol to check that they don’t have bone metastases, an extensive study of the abdomen and chest is done with the CT scan, in a word, to check things out… the basic extension study for all women.[ORHHU1]
The Tumour Committee: A Multidisciplinary Enclave
I think the committees are a sure winner. I think there should be committees in all hospitals and for everything. Having a multidisciplinary vision of things is always positive. Also, you can learn. […] First, your personal learning and second, that the patients, in my opinion, are much better attended to when there’s an overall vision.[MNGHU1]
I think it’s quite enriching because there are cases that are very simple, but also cases that lend themselves to discussion, and everyone participates. I think, for the patient, it’s much better when it’s not a single person making the decisions.[GGHU1]
When the case is clear, or it’s a small tumour, the surgeons operate on it from the start, but when there’s some alteration or something is a little out of the ordinary or raises doubts, then the action plan comes in… the action plan is agreed on.[OM2HHU1]
I think that it works well and that it makes decisions that, sometimes more and sometimes less, attempt to improve overall care for women with breast cancer.[OM1HHU1]
It ensures that the treatment is the most suitable because two heads are better than one, and everything’s taken into account. I think that’s a strong point.[ORGHU1]
I’m not the only one who decides what to do with that particular patient. That’s fine, especially when you’re not sure. The tiny nodule that goes for sentinel node surgery, no one has any doubts about it, but there are tumours that can be multifocal, that can be multicentric; it depends. The committee is an official body that supports the decision given for that particular woman.[GGHU1]
First, the objective of the committee is to present newly diagnosed patients to make joint, multidisciplinary therapeutic decisions. Those are the basics, shall we say. And then other objectives are to establish common work protocols, to set up common research studies, and often also to comment on functional problems, delay problems, basic surgical issues, and specific speciality issues. Basically, what I’ve told you: care protocols, also to present some relevant study or bibliographical session on the subject. There are many things, but the basic one is to present the patients.[OM1HHU1]
The truth is that we work really, really well because we have weekly committees.[OMGHU2]
[…] we have a really good relationship between professionals, and we’re very close, but I’d like, and this is something I’ve proposed to see if it could be done in the future, I’d like to meet at least once a week and for all the breast cancers diagnosed to be evaluated jointly by at least one oncologist, a surgeon and a radiologist, something that’s not being done at the moment. A tumour committee is held once a month for tumours in general […].[CHHR1]
There, the cases of most interest or that cause most doubts or that provoke debate as to whether one treatment or another is better are discussed. And the rest of the patients, well, through a consultation sheet or if not by phone or now with WhatsApp: "What about this patient?”.[ORHHU1]
Another advantage that I’ve seen is that it’s a lot of work for the committee members, but all cases are discussed at all times, to decide on surgery, to decide on radiotherapy treatment, to decide on the best option if there’s a relapse.[ORGHU1]
3.2. Surgical Treatment of the Disease: Territorial Inequalities
[…] in the past, when you had to operate on a patient, most of them underwent a mastectomy, axillary dissection and then chemotherapy; nowadays, this has changed a lot, fortunately.[CHHR1]
In fact, when conservative surgery is indicated, it’s conservative surgery, and it has to be as conservative as possible.[MNGHU1]
It could improve in terms of having more support, especially in plastic surgery. There are techniques that we have to refer to Seville as a reference centre. A lot of reconstructions, like abdominal grafts, aren’t done here; they’re done there.[CHHR1]
We’re beginning to improve things because, for example, until now, we didn’t offer oncoplastic surgery, the topic of immediate reconstruction. We’d neglected that area a bit… call it neglected, call it eh…. Well, it wasn’t very clear how we were going to deal with it. One of the improvements that we are going to be making from 2019 is to work with the plastic surgery service for patients who could be candidates for immediate reconstruction and patients who are going to undergo mastectomy; it can be done.[GGHU1]
Because the oncological results don’t vary. Because the cosmetic results practically don’t vary. And because of the pressure on care, the waiting list is greatly reduced, and it’s easier to operate on a patient once in a longer surgery than to have to operate on her twice. And the plastic surgery waiting lists are terrible. So for the patient whose breast we don’t reconstruct immediately, it’ll take a long time to reconstruct.[CGHU2]
A few months ago, we opened a tattoo consultation in nursing. So the patient, even if she loses her areola or her nipple in the six months needed for the whole healing process, she’s then referred to tattoos.[CGHU2]
The waiting time that we have for breast cancer is 30 days. 30 days after the diagnosis, an intervention is performed.[CHHU1]
Chemotherapy and Radiotherapy Treatment: Improvements and Inequalities in Access
At the level of chemotherapy, a lot more drugs have appeared, a lot more… A wider range of possibilities for women who perhaps were more limited by their molecular, hormonal or other profiles.
Four years ago, we used to do 25 sessions to treat a breast, and now we only do 15 because we’ve changed the divisions because new studies have come out that show that with the same efficacy, you can reduce women’s treatment by 10 sessions: “Wow! Well, that’s ten days less that they have to come for radiotherapy.[ORHHU1]
They’re normally poor people with few resources. Quite isolated towns in terms of public transport. For example, I have patients who come from towns where there’s one bus a day to Huelva. One, that’s it […]. And it’s three or two and a half hours walking from the town. […] You know? So that also limits you a lot when it comes to everything. […] There’s radiotherapy only in Huelva.[ORHHU1]
There are clinical trials, and we’d like to have more, obviously, when we think that a drug is going to benefit the patient. We’d like to have more. Sometimes among ourselves, if we think there’s a molecule that has good potential and it’s in Seville, we promote it. Patients are already asking us more and more about these possibilities.[CHHR1]
At the moment, we have five or six clinical trials in breast cancer, which is good because we don’t have as many in other pathologies, but, for example, the Virgen del Rocio Hospital has 44 breast cancers, Macarena has, I think, 20-something.[OM1HHU1]
Well, the service is very well organised. In other words, it’s really organised, and there are no delays […] the first visit that medical oncology does ranges between a week and 10 days.[OMHHU1]
Well, we, I do chemotherapy if I see the lady and I want to give her chemotherapy that day or the next day, if it’s urgent, it’s urgent. […] obviously, if I can schedule it a little, I do schedule it, but if I need it to be tomorrow, it’s tomorrow. [… ][OMGHU2]
Normally we don’t start radiotherapy until at least a month has passed since the surgery because the scars are open, and if we radiate a breast that hasn’t closed properly yet, the wound can open, and you can make a bloody mess of it.[ORHHU1]
Yes, I’m talking about my service, radiation oncology. Right now, at the moment, we’re up to date. Every patient who gets presented to the committee, we see them either that week or the next.[ORGHU2]
3.3. Human, Technical and Economic Resources in the Treatment of Breast Cancer: Seasonal Delays
There are periods that are more difficult. Vacations, vacations are more difficult because there’s less staff in all areas, in all services, so what normally can take 6 weeks, maybe takes 8.[OMGHU2]
On average, Christmas is coming now, and there’s no place to put all of them, so they have to wait till the next week.[GGHU1]
I believe that health should be something fundamental on the political level and shouldn’t be a subject for change for elections and a political football, now yes and now no, and now… So, from my point of view, the professionals who work, we get 100% involved in trying to make this go as well as possible, but the limitations are always from the hospital up. That there are no resources, there’s no money, and I won’t hire you anymore… I think that in radiotherapy, we’re working with three fewer technicians.[ORHHU1]
I don’t know if there’d be a possibility of… I think the manager’s doing it, looking for more activity in the afternoon, there’s an emergency plan, but sometimes anaesthesiologists are also lacking.[OMHHU1]
Health here in Andalusia is quite limited, but even so, we manage to meet the deadlines required of us.[ORHHU1]
The problem of small hospitals is always human resources. […] I see that most people who’ve just arrived come to one of these hospitals, earn points, gain experience, and when […] they’re already at the end of their training, they leave […] We‘ve lost two radiologists who left for the Macarena recently. Almost half of the staff of the surgery service had to be replaced. That’s the criticism I make of small hospitals, which is that management has to do something to retain staff because if staff isn’t retained, they have a quick turnover, and the quick turnover ultimately ends up resulting in a gradual deterioration of quality.[CHHR1]
More operating theatres, exactly, so that surgeons have more resources.[OMHHU1]
And the staff’s not only required for basic field care, which is what I say, but we also need resources to carry out the whole preliminary study, all the preliminary protocols and everything that needs to be done before starting up a test. Because the test isn’t done, and that’s it. It takes prior preparation that takes a long time. So, of course, we need resources.[ORGHU2]
The MRI often takes a month and delays the definitive diagnosis because the MRI should be shortened, we need more facilities for MRI, and that’s pending. I think that ultimately it’s resources, radiology resources and MRI resources to improve those times.[ORHHU1]
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sociedad Española de Oncología Médica (SEOM). Las Cifras del Cáncer en España; SEOM: Madrid, España, 2021. [Google Scholar]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Cancer Over Time. Available online: https://gco.iarc.fr/overtime/en (accessed on 22 August 2022).
- Autier, P.; Héry, C.; Haukka, J.; Boniol, M.; Byrnes, G. Advanced breast cancer and breast cancer mortality in randomized controlled trials on mammography screening. J. Clin. Oncol. 2009, 27, 5919–5923. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Steliarova-Foucher, E.; Lortet-Tieulent, J.; Rosso, S.; Coebergh, J.W.W.; Comber, H.; Forman, D.; Bray, F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries in 2012. Eur. J. Cancer 2013, 49, 1374–1403. [Google Scholar] [CrossRef] [Green Version]
- Héry, C.; Ferlay, J.; Boniol, M.; Autier, P. Quantification of changes in breast cancer incidence and mortality since 1990 in 35 countries with Caucasian-majority populations. Ann. Oncol. 2008, 19, 1187–1194. [Google Scholar] [CrossRef] [PubMed]
- Vidal, C.; Martínez, J.M.; Mateos, M.; Peris, M. Mortalidad por cáncer de mama: Evolución en España y sus comunidades autónomas durante el período 1980–2005. Rev. Esp. Salud Pública 2010, 84, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Burton, R.C.; Bell, R.J.; Thiagarajah, G.; Stevenson, C. Adjuvant therapy, not mammographic screening, accounts for most of the observed breast cancer specific mortality reductions in Australian women since the national screening program began in 1991. Breast Cancer Res. Treat. 2012, 131, 949–955. [Google Scholar] [CrossRef]
- Walters, S.; Maringe, C.; Butler, J.; Rachet, B.; Barrett-Lee, P.; Bergh, J.; Boyages, J.; Christiansen, P.; Lee, M.; Wärnberg, F. Breast cancer survival and stage at diagnosis in Australia, Canada, Denmark, Norway, Sweden and the UK, 2000–2007: A population-based study. Br. J. Cancer 2013, 108, 1195–1208. [Google Scholar] [CrossRef] [Green Version]
- Hanis, T.M.; Yaacob, J.M.; Hairon, S.M.; Abdullah, S. Net survival differences of breast cancer between stages at diagnosis and age groups in the east coast region of West Malaysia: A retrospective cohort study. BMJ Open 2021, 11, e043642. [Google Scholar] [CrossRef]
- Elmore, J.G.; Armstrong, K.; Lehman, C.D.; Fletcher, S.W. Screening for breast cancer. JAMA 2005, 293, 1245–1256. [Google Scholar] [CrossRef]
- Broeders, M.; Moss, S.; Nyström, L.; Njor, S.; Jonsson, H.; Paap, E.; Massat, N.; Duffy, S.; Lynge, E.; Paci, E.; et al. The impact of mammographic screening on breast cancer mortality in Europe: A review of observational studies. J. Med. Screen. 2012, 19, 14–25. [Google Scholar] [CrossRef]
- Njor, S.; Nyström, L.; Moss, S.; Paci, E.; Broeders, M.; Segnan, N.; Lynge, E.; EUROSCREEN Working Group. Breast cancer mortality in mammographic screening in Europe: A review of incidence-based mortality studies. J. Med. Screen. 2012, 19, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Paci, E.; EUROSCREEN Working Group. Summary of the evidence of breast cancer service screening outcomes in Europe and first estimate of the benefit and harm balance sheet. J. Med. Screen. 2012, 19, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Merino, J.A.; Torres, M.; Ros, L.H. Breast cancer in the 21st century: From early detection to new therapies. Radiología 2017, 59, 368–379. [Google Scholar] [CrossRef]
- Vervoort, M.M.; Draisma, G.; Fracheboud, J.; van de Poll-Franse, L.V.; de Koning, H.J. Trends in the usage of adjuvant systemic therapy for breast cancer in the Netherlands and its effect on mortality. Br. J. Cancer 2004, 91, 242–247. [Google Scholar] [CrossRef]
- Chia, S.; Bryce, C.; Gelmon, K. The 2000 EBCTCG overview: A widening gap. Lancet 2005, 365, 1665–1666. [Google Scholar] [CrossRef]
- Slamon, D.; Eiermann, W.; Robert, N.; Pienkowski, T.; Martin, M.; Press, M.; Mackey, J.; Glaspy, J.; Chan, A.; Pawlicki, M.; et al. Adjuvant trastuzumab in HER2-positive breast cancer. N. Engl. J. Med. 2011, 365, 1273–1283. [Google Scholar] [CrossRef] [Green Version]
- Gooiker, G.A.; van Gijn, W.; Post, P.N.; van de Velde, C.J.; Tollenaar, R.A.; Wouters, M.W. A systematic review and meta-analysis of the volume-outcome relationship in the surgical treatment of breast cancer: Are breast cancer patients better off with a high volume provider? Eur. J. Surg. Oncol. 2010, 36, 27–35. [Google Scholar] [CrossRef] [Green Version]
- Guller, U.; Safford, S.; Pietrobon, R.; Heberer, M.; Oertli, D.; Jain, N.B. High hospital volume is associated with better outcomes for breast cancer surgery: Analysis of 233,247 patients. World J. Surg. 2005, 29, 994–999. [Google Scholar] [CrossRef] [Green Version]
- Roohan, P.J.; Bickell, N.A.; Baptiste, M.S.; Therriault, G.D.; Ferrara, E.P.; Siu, A.L. Hospital volume differences and five-year survival from breast cancer. Am. J. Public Health 1998, 88, 454–457. [Google Scholar] [CrossRef] [Green Version]
- Pezzin, L.E.; Laud, P.; Yen, T.W.; Neuner, J.; Nattinger, A.B. Reexamining the relationship of breast cancer hospital and surgical volume to mortality: An instrumental variable analysis. Med. Care 2015, 53, 1033–1039. [Google Scholar] [CrossRef]
- Vrijens, F.; Stordeur, S.; Beirens, K.; Devriese, S.; Van Eycken, E.; Vlaven, J. Effect of hospital volume on processes of care and 5-year survival after breast cancer: A population-based study on 25000 women. The Breast. 2012, 21, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C.; Munro, A.J.; Glynne-Jones, R.; Griffith, C.; Trevatt, P.; Richards, M.; Ramirez, A.J. Multidisciplinary team working in cancer: What is the evidence? BMJ 2010, 340, c951. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blackwood, O.; Deb, R. Multidisciplinary team approach in breast cancer care: Benefits and challenges. Indian J. Pathol. Microbiol. 2020, 63, 105–112. [Google Scholar] [CrossRef]
- Pons-Tostivint, E.; Daubisse-Marliac, L.; Grosclaude, P.; Oum Sack, E.; Goddard, J.; Morel, C.; Dunet, C.; Sibrac, L.; Lagadic, C.; Bauvin, E.; et al. Multidisciplinary team meeting and EUSOMA Quality indicators in breast cancer care: A French regional multicenter study. Breast 2019, 46, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Whitehouse, M. A policy framework for commissioning cancer services. BMJ 1995, 310, 1425–1426. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, A.R.; Marotti, L.; Bianchi, S.; Biganzoli, L.; Claassen, S.; Decker, T.; Frigerio, A.; Goldhirsch, A.; Gustafsson, E.G.; Mansel, R.E.; et al. The requirements of a specialist Breast Centre. Eur. J. Cancer 2013, 49, 3579–3587. [Google Scholar] [CrossRef]
- Blamey, R.; Cataliotti, L. EUSOMA: The requirements of a specialist breast unit. Eur. J. Cancer 2000, 36, 2288–2293. [Google Scholar] [CrossRef]
- Cardoso, F.; Cataliotti, L.; Costa, A.; Knox, S.; Marotti, L.; Rutgers, E.; Beishon, M. European Breast Cancer Conference manifesto on breast centres/units. Eur. J. Cancer 2017, 72, 244–250. [Google Scholar] [CrossRef] [Green Version]
- Otegi, I.; Eguaras, I.; Goikoetxea, A.; Sánchez, P.; Guillén-Grima, F.; Vicente, F. Influence of the creation of a Breast Unit on the surgical parameters and quality criteria of the surgical treatment of breast cancer. Rev. Senol. Patol. Mamar. 2019, 32, 81–88. [Google Scholar] [CrossRef]
- Winchester, D.P. The United States’ national accreditation program for breast centers: A model for excellence in breast disease evaluation and management. Chin. Clin. Oncol. 2016, 5, 31. [Google Scholar] [CrossRef]
- Álvarez, M.; Santos, A.L.; Rioja, P.; García, I.; Ruiz, J. Multidisciplinary breast units. Rev. Senol. Patol. Mamar. 2012, 25, 116–124. [Google Scholar] [CrossRef]
- Escalera, C.; Bayo, E.; Fernández, J.M.; González, Y.; Granados, M.T.; Ilia, C.; La Calle, M.; Ruiz, J.; Serrano, P.; Torres, M.; et al. Cáncer de Mama. Detección Precoz de Cáncer de Mama; Consejería de Salud: Sevilla, España, 2005. [Google Scholar]
- Acebal Blanco, M.M.; Alba Conejo, E.; Álvarez Benito, M.; Bayo Lozano, E.; Del Río Urenda, S.; Dotor Gracia, M.; Dueñas Rodríguez, B.; Fernández Echegaray, R.; Fernández Temprano, J.M.; Galván Ruiz, A.; et al. Cáncer de Mama: Proceso Asistencial Integrado, 3rd ed.; Consejería de Salud: Sevilla, España, 2011. [Google Scholar]
- Dubois, C.; De Schutter, H.; Leroy, R.; Stordeur, S.; De Gendt, C.; Schillemans, V.; Kohn, L.; Van Eycken, L.; Vrijens, F. Multidisciplinary work in oncology: Population-based analysis for seven invasive tumours. Eur. J. Cancer Care 2018, 27, e12822. [Google Scholar] [CrossRef] [PubMed]
- Ulin, P.R.; Robinson, E.T.; Tolley, E.E. Investigación Aplicada en Salud Pública. Métodos Cualitativos; Publicación Científica y Técnica No. 614: Washington, DC, USA, 2006. [Google Scholar]
- Viñas, M.J.; Fernández, P.; Fajardo, M.L.; Gurucelain, J.L.; Alguacil, J. Distribución municipal de la incidencia de los tumores más frecuentes en un área de elevada mortalidad por cáncer. Gac. Sanit. 2017, 31, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Strauss, A.; Corbin, J. Basics of Qualitative Research: Techniques and Procedures for Feveloping Grounded Theory, 2nd ed.; Sage Publications: Thousand Oaks, CA, USA, 1998. [Google Scholar]
- Denzin, N.K.; Lincoln, Y.S. The Landscape of Qualitative Research: Theories and Issues, 2nd ed.; Sage Publications: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Valles, M.S. Técnicas Cualitativas de Investigación Social. Reflexión Metodológica y Práctica Professional; Síntesis: Madrid, Spain, 1997; ISBN 9788477384496. [Google Scholar]
- Tesch, R. Qualitative Research: Analysis Types and Software Tools; The Falmer Press: New York, NY, USA, 1990; ISBN 978-1850006091. [Google Scholar]
- Lincoln, Y.S.; Guba, E.G. Judging the quality of case study reports. Int. J. Qual. Stud. 1990, 3, 53–59. [Google Scholar] [CrossRef]
- Schwandt, T.A.; Lincoln, Y.S.; Guba, E.G. Judging interpretations: But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Dir. Eval. 2007, 114, 11–25. [Google Scholar] [CrossRef]
- Miguelena, J.M.; Dominguez, F. Formación del cirujano en patología mamaria. In Cirugía de la Mama. Guías Clínicas de la Asociación Española de Cirujanos; Domínguez, F., Ballester, J., de Castro, G., Eds.; Arán Ediciones: Madrid, Spain, 2017; pp. 126–137. [Google Scholar]
- Recari, E.; Obregozo, R.; Ezcurdia, M. Importancia del ginecólogo en la Unidad de Patología Mamaria. Rev. De Senol. Y Patol. Mamar. 1996, 9, 167–172. [Google Scholar]
- De León, J.M.; Frutos, J. El cirujano ante la patología mamaria, técnicas diagnósticas, clasificación BI-RADS. Cir. Andal. 2021, 32, 99–111. [Google Scholar] [CrossRef]
- Güler, S.A.; Güllüoğlu, B.M. Quality Assurance in Breast Health Care and Requirement for Accreditation in Specialized Units. J. Breast Health 2014, 10, 129–133. [Google Scholar] [CrossRef]
- Van Nes, J.G.H.; Van de Velde, C.J.H. Het multidisciplinair mammateam: Bevordering van goede zorg [The multidisciplinary breast cancer care team: Promoting better care]. Ned. Tijdschr. Geneeskd. 2005, 149, 1929–1931. [Google Scholar]
- Abdulrahman, G.O., Jr. The effect of multidisciplinary team care on cancer management. Pan. Afr. Med. J. 2011, 9, 20. [Google Scholar] [CrossRef]
- Bydder, S.; Nowak, A.; Marion, K.; Phillips, M.; Atun, R. The impact of case discussion at a multidisciplinary team meeting on the treatment and survival of patients with inoperable non-small cell lung cancer. Intern. Med. J. 2009, 39, 838–841. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.H.; Vines, E.; Bertsch, H.; Fraker, D.L.; Czerniecki, B.J.; Rosato, E.F.; Lawton, T.; Conant, E.F.; Orel, S.G.; Schuchter, L.; et al. The impact of a multidisciplinary breast cancer center on recommendations for patient management: The University of Pennsylvania experience. Cancer 2001, 91, 1231–1237. [Google Scholar] [CrossRef]
- Kesson, E.M.; Allardice, G.M.; George, W.D.; Burns, H.J.; Morrison, D.S. Effects of multidisciplinary team working on breast cancer survival: Retrospective, comparative, interventional cohort study of 13 722 women. BMJ 2012, 26, 344:e2718. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merck, B.; Ramos-Rincón, J.M.; Cansado, P.; Ballester, J.B.; Martínez-García, F.; Ramos-Boyero, M.; Calpena, R. Adecuación de las unidades de mama españolas a los criterios de EUSOMA. Cir. Esp. 2005, 77, 221–225. [Google Scholar] [CrossRef]
- Albert, U.S.; Wagner, U.; Kalder, M. Breast Centers in Germany. Breast Care 2009, 4, 225–230. [Google Scholar] [CrossRef]
- Yung, R.; Ray, R.M.; Roth, J.; Johnson, L.; Warnick, G.; Anderson, G.L.; Kroenke, C.H.; Chlebowski, R.T.; Simon, M.S.; Fung, C.; et al. The association of delay in curative intent treatment with survival among breast cancer patients: Findings from the Women’s Health Initiative. Breast Cancer Res. Treat. 2020, 180, 747–757. [Google Scholar] [CrossRef]
- Bleicher, R.J.; Ruth, K.; Sigurdson, E.R.; Beck, J.R.; Ross, E.; Wong, Y.; Patel, S.A.; Boraas, M.; Chang, E.I.; Topham, N.S.; et al. Time to Surgery and Breast Cancer Survival in the United States. JAMA Oncol. 2016, 2, 330–339. [Google Scholar] [CrossRef]
- Zhan, Q.; Fu, J.; Fu, F.; Zhang, J.; Wang, C. Survival and time to initiation of adjuvant chemotherapy among breast cancer patients: A systematic review and meta-analysis. Oncotarget 2017, 9, 2739–2751. [Google Scholar] [CrossRef] [Green Version]
- Panagopoulou, P.; Gogas, H.; Dessypris, N.; Maniadakis, N.; Fountzilas, G.; Petridou, E.T. Survival from breast cancer in relation to access to tertiary healthcare, body mass index, tumor characteristics and treatment: A Hellenic Cooperative Oncology Group (HeCOG) study. Eur. J. Epidemiol. 2012, 27, 857–866. [Google Scholar] [CrossRef]
- Kelly, C.; Hulme, C.; Farragher, T.; Clarke, G. Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open 2016, 6, e013059. [Google Scholar] [CrossRef] [Green Version]
- Skinner, K.A.; Helsper, J.T.; Deapen, D.; Ye, W.; Sposto, R. Breast cancer: Do specialists make a difference? Ann. Surg. Oncol. 2003, 10, 606–615. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, C.; Ferencz, J.; Brucker, S.Y.; Kreienberg, R.; Wesselmann, S. Quality of care in breast cancer centers: Results of benchmarking by the German Cancer Society and German Society for Breast Diseases. Breast 2015, 24, 118–123. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, R.; Sant, M.; Coleman, M.P.; Francisci, S.; Baili, P.; Pierannunzio, D.; Trama, A.; Visser, O.; Brenner, H.; Ardanaz, E.; et al. Cancer survival in Europe 1999-2007 by country and age: Results of EUROCARE--5-a population-based study. Lancet Oncol. 2014, 15, 23–34. [Google Scholar] [CrossRef]
- Informe Dinámico: Mortalidad. Available online: https://observatorio.contraelcancer.es/informes/informe-dinamico-mortalidad (accessed on 22 August 2022).
- Tasa de Riesgo de Pobreza por Comunidades Autónomas. Available online: https://www.ine.es/jaxiT3/Datos.htm?t=9963 (accessed on 22 August 2022).
| Speciality Area | N | Age | Sex | Province | Professional Background (Years) | Professional Background with Preferential Dedication to Breast Pathology (Years) |
|---|---|---|---|---|---|---|
| Surgeons | 3 | 60 | Man | Granada | 29 | 12 |
| 39 | Man | Huelva | 10 | -- | ||
| 55 | Woman | Huelva | 28 | 15 | ||
| Oncology | 4 | 34 | Woman | Granada | 9 | 4 |
| 48 | Woman | Granada | 16 | 12 | ||
| 32 | Man | Huelva | 8 | 7 | ||
| 58 | Man | Huelva | 30 | 20 | ||
| Diagnostic Radiology | 5 | 55 | Woman | Granada | 13 | 9 |
| 47 | Man | Granada | 28 | 15 | ||
| 50 | Man | Huelva | 20 | 18 | ||
| 62 | Man | Huelva | 24 | 11 | ||
| 55 | Woman | Huelva | 24 | 5 | ||
| Radiotherapy | 3 | 33 | Woman | Granada | 6 | 2 |
| 64 | Woman | Granada | 28 | 12 | ||
| 35 | Woman | Huelva | 11 | 7 | ||
| Pathological Anatomy | 2 | 44 | Woman | Granada | 18 | 6 |
| 47 | Woman | Huelva | 20 | -- | ||
| Gynecology | 2 | 43 | Woman | Granada | 17 | 4 |
| 65 | Man | Granada | 36 | 17 | ||
| Nuclear Medicine | 1 | 44 | Woman | Granada | 9 | 9 |
| Total | 19 |
| 1 | Can you describe the integrated care process for breast cancer in Andalusia? What are the strengths and barriers that exist? |
| 2 | In your opinion, how is the care process for breast cancer treatment in your hospital? What are the strengths and barriers that exist? |
| 3 | Specifically, how is your service working in relation to breast cancer treatment care? Is it effective? |
| 4 | Is there a multidisciplinary approach to breast treatment in your hospital? How is it achieved? What are the strengths and barriers that exist? |
| 5 | How is the coordination between the service with the rest of the services and professionals involved in the diagnosis, treatment, and follow-up of breast cancer patients? |
| 6 | Regarding human resources, how many professionals in your speciality with preferential attention to breast pathology does the hospital have? Do you consider them sufficient? Do you think there are aspects to improve? |
| 7 | How do you rate the financial resources of the hospital dedicated to breast pathology? Do you consider them sufficient? Do you think there are aspects to improve? |
| 8 | What decisions would you make to improve patient care in your hospital? |
| Criteria | Techniques Performed and Application Procedures |
|---|---|
| 1. Credibility | |
| 1.1. Prolonged Engagement | Fieldwork between 2019 and 2021. |
| 1.2. Persistent observation | Circular process of data collection and analysis. |
| 1.3. Triangulation of data | Researchers from different scientific disciplines contrasted the coding performed and the analysis of the information. |
| 1.4. Peer debriefing | Exposition of the research design (sample, recruitment strategies, and information collection instruments) to two researchers. |
| 2. Transferability | |
| 2.1. Thick Descriptive Data | A detailed description of the health context (integrated care process for breast cancer), study sites (rural and urban hospitals), and participants’ profiles. |
| 3. Dependability and Confirmability | The report was evaluated by an external researcher and health professional in breast cancer in the hospital. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Reinado, C.; Delgado-Parrilla, A.; Alguacil, J. Breast Cancer Treatment in Integrated Care Process in Andalusia: The Challenge of Multidisciplinarity. Int. J. Environ. Res. Public Health 2022, 19, 12728. https://doi.org/10.3390/ijerph191912728
Rodríguez-Reinado C, Delgado-Parrilla A, Alguacil J. Breast Cancer Treatment in Integrated Care Process in Andalusia: The Challenge of Multidisciplinarity. International Journal of Environmental Research and Public Health. 2022; 19(19):12728. https://doi.org/10.3390/ijerph191912728
Chicago/Turabian StyleRodríguez-Reinado, Carmen, Ana Delgado-Parrilla, and Juan Alguacil. 2022. "Breast Cancer Treatment in Integrated Care Process in Andalusia: The Challenge of Multidisciplinarity" International Journal of Environmental Research and Public Health 19, no. 19: 12728. https://doi.org/10.3390/ijerph191912728
APA StyleRodríguez-Reinado, C., Delgado-Parrilla, A., & Alguacil, J. (2022). Breast Cancer Treatment in Integrated Care Process in Andalusia: The Challenge of Multidisciplinarity. International Journal of Environmental Research and Public Health, 19(19), 12728. https://doi.org/10.3390/ijerph191912728






