Current Perspectives on the Determinants of Acceptability of Pre-Exposure Prophylaxis and Nonoccupational Post-Exposure Prophylaxis among People at Risk for HIV: A Scoping Review
Abstract
1. Introduction
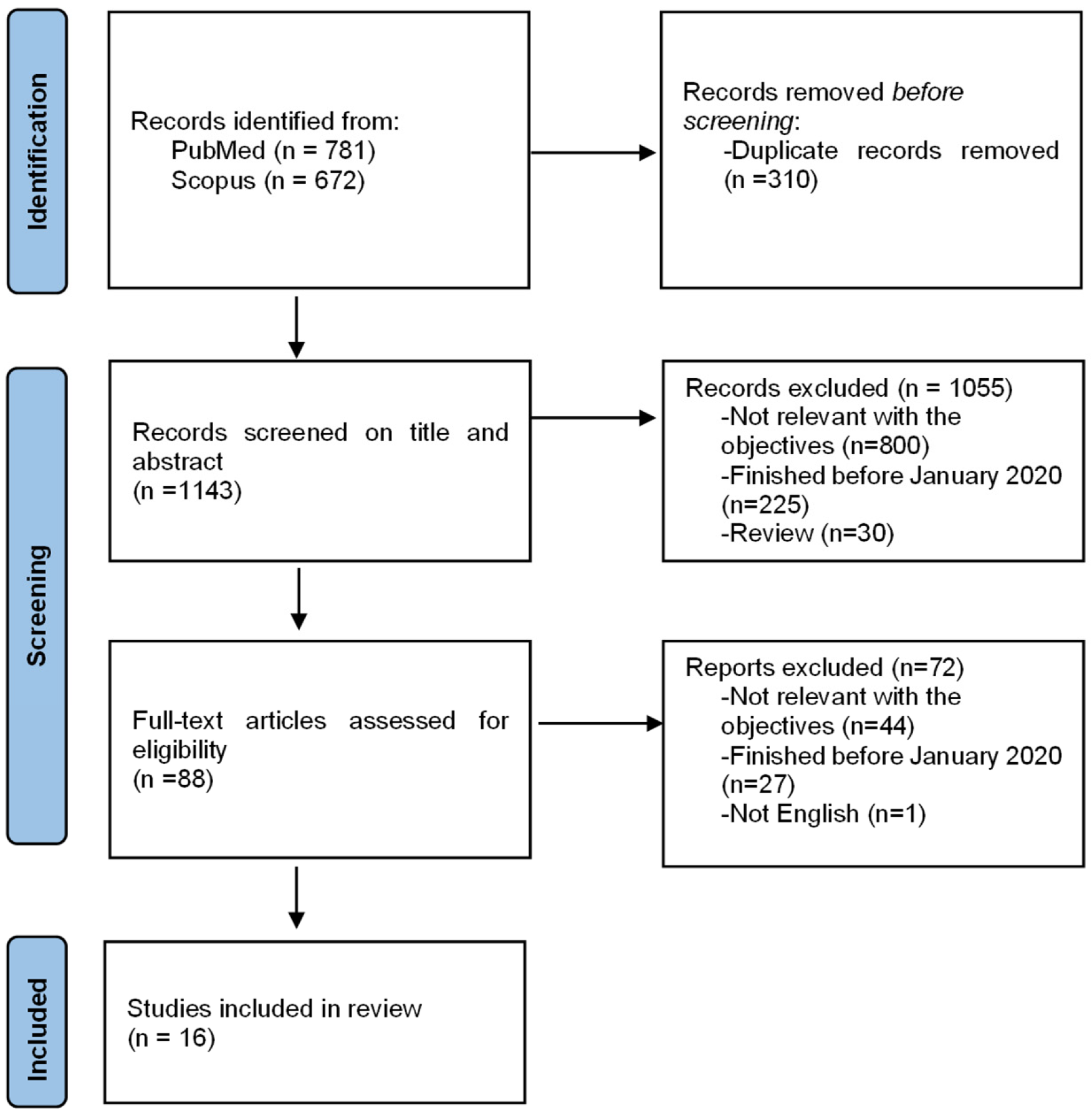
2. Methods
2.1. Eligibility Criteria
2.2. Information Sources and Search Strategy
2.3. Selection of Sources of Evidence
2.4. Data Charting Process
2.5. Data Items
2.6. Synthesis of Results
3. Results
3.1. Individual Factors
3.1.1. Demographic and Socio-Economic Characteristics of Participants
3.1.2. Awareness and Knowledge
3.1.3. Behavioral Factors
3.2. PrEP-Specific Factors
3.3. Psychosocial Factors
3.4. Health System Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
>Data Available Statement
Conflicts of Interest
References
- PEP|HIV Basics|HIV/AIDS|CDC. Available online: https://www.cdc.gov/hiv/basics/pep.html (accessed on 15 November 2019).
- Rey, D.; Bendiane, M.-K.; Moatti, J.-P.; Wellings, K.; Danziger, R.; MacDowall, W.; The European Study Group on HIV Testing Policies and Practices in Europe. Post-Exposure Prophylaxis after Occupational and Non-Occupational Exposures to HIV: An Overview of the Policies Implemented in 27 European Countries. AIDS Care 2000, 12, 695–701. [Google Scholar] [CrossRef] [PubMed]
- Fisher, M.; Benn, P.; Evans, B.; Pozniak, A.; Jones, M.; MacLean, S.; Davidson, O.; Summerside, J.; Hawkins, D.; Clinical Effectiveness Group (British Association for Sexual Health and HIV). UK Guideline for the Use of Post-Exposure Prophylaxis for HIV Following Sexual Exposure. Int. J. STD AIDS 2006, 17, 81–92. [Google Scholar] [CrossRef] [PubMed]
- WHO. Pre-Exposure Prophylaxis. Available online: http://www.who.int/hiv/topics/prep/en/ (accessed on 9 May 2020).
- Grant, R.M.; Lama, J.R.; Anderson, P.L.; McMahan, V.; Liu, A.Y.; Vargas, L.; Goicochea, P.; Casapía, M.; Guanira-Carranza, J.V.; Ramirez-Cardich, M.E.; et al. Preexposure Chemoprophylaxis for HIV Prevention in Men Who Have Sex with Men. N. Engl. J. Med. 2010, 363, 2587–2599. [Google Scholar] [CrossRef] [PubMed]
- WHO. Guidance on Oral Pre-Exposure Prophylaxis (PrEP) for Serodiscordant Couples, Men and Transgender Women Who Have Sex with Men at High Risk of HIV. Available online: https://www.who.int/hiv/pub/guidance_prep/en/ (accessed on 15 April 2020).
- Yu, S.; Cross, W.; Lam, L.L.Y.; Zhang, K.; Banik, B.; Li, X.; Wang, H. Willingness, Preferred Ways and Potential Barriers to Use Pre-Exposure Prophylaxis for HIV Prevention among Men Who Have Sex with Men in China. BMJ Open 2021, 11, e053634. [Google Scholar] [CrossRef] [PubMed]
- Galea, J.T.; Kinsler, J.J.; Salazar, X.; Lee, S.-J.; Giron, M.; Sayles, J.N.; Cáceres, C.; Cunningham, W.E. Acceptability of Pre-Exposure Prophylaxis as an HIV Prevention Strategy: Barriers and Facilitators to Pre-Exposure Prophylaxis Uptake among at-Risk Peruvian Populations. Int. J. STD AIDS 2011, 22, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Isano, S.; Wong, R.; Logan, J.; El-Halabi, S.; El-Khatib, Z. Barriers to Post Exposure Prophylaxis Use among Men Who Have Sex with Men in Sub-Saharan Africa: An Online Cross-Sectional Survey. Prev. Med. Rep. 2020, 19, 101100. [Google Scholar] [CrossRef]
- UNAIDS Data 2021. Available online: https://www.unaids.org/en/resources/documents/2021/2021_unaids_data (accessed on 30 April 2022).
- Weekly Epidemiological Update on COVID-19—20 April 2022. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---20-april-2022 (accessed on 23 April 2022).
- WHO. Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 23 April 2022).
- Deng, T.; Xu, T.; Lee, Y.J. Policy Responses to COVID-19 and Stock Market Reactions—An International Evidence. J. Econ. Bus. 2022, 119, 106043. [Google Scholar] [CrossRef]
- Jewell, B.L.; Mudimu, E.; Stover, J.; ten Brink, D.; Phillips, A.N.; Smith, J.A.; Martin-Hughes, R.; Teng, Y.; Glaubius, R.; Mahiane, S.G.; et al. Potential Effects of Disruption to HIV Programmes in Sub-Saharan Africa Caused by COVID-19: Results from Multiple Mathematical Models. Lancet HIV 2020, 7, e629–e640. [Google Scholar] [CrossRef]
- Qiao, S.; Li, Z.; Weissman, S.; Li, X.; Olatosi, B.; Davis, C.; Mansaray, A.B. Disparity in HIV Service Interruption in the Outbreak of COVID-19 in South Carolina. AIDS Behav. 2021, 25, 49–57. [Google Scholar] [CrossRef]
- Patel, V.V.; Beil, R.; Slawek, D.; Akiyama, M.J. HIV Prevention and Treatment in the Context of the COVID-19 in the Bronx, New York: Implications for Practice and Research. AIDS Rev. 2020, 22, 143–147. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Tolley, E.E.; Morrow, K.M.; Owen, D.H. Designing a Multipurpose Technology for Acceptability and Adherence. Antivir. Res. 2013, 100, S54–S59. [Google Scholar] [CrossRef] [PubMed]
- Holt, M. HIV Pre-Exposure Prophylaxis and Treatment as Prevention: A Review of Awareness and Acceptability among Men Who Have Sex with Men in the Asia-Pacific Region and the Americas. Sex. Health 2013, 11, 166–170. [Google Scholar] [CrossRef] [PubMed]
- Hulstein, S.H.; Zimmermann, H.M.L.; de la Court, F.; Matser, A.; Schim van der Loeff, M.F.; Hoornenborg, E.; Davidovich, U.; Prins, M.; de Vries, H.J.C. Factors Associated with the Intention to Use HIV Pre-Exposure Prophylaxis for Young and Older Men Who Have Sex with Men. Sex. Transm. Dis. 2022, 49, 343–352. [Google Scholar] [CrossRef]
- Chan, C.; Vaccher, S.; Fraser, D.; Grulich, A.E.; Holt, M.; Zablotska-Manos, I.; Prestage, G.P.; Bavinton, B.R. Preferences for Current and Future PrEP Modalities among PrEP-Experienced Gay and Bisexual Men in Australia. AIDS Behav. 2022, 26, 88–95. [Google Scholar] [CrossRef]
- Sharpe, J.D.; Sanchez, T.H.; Siegler, A.J.; Guest, J.L.; Sullivan, P.S. Association between the Geographic Accessibility of PrEP and PrEP Use among MSM in Nonurban Areas. J. Rural Health 2022, 38, 948–959. [Google Scholar] [CrossRef]
- Blair, K.J.; Torres, T.S.; Hoagland, B.; Bezerra, D.R.B.; Veloso, V.G.; Grinsztejn, B.; Clark, J.; Luz, P.M. Pre-Exposure Prophylaxis Use, HIV Knowledge, and Internalized Homonegativity among Men Who Have Sex with Men in Brazil: A Cross-Sectional Study. Lancet Reg. Health Am. 2022, 6, 100152. [Google Scholar] [CrossRef]
- Zhou, L.; Assanangkornchai, S.; Shi, Z.; Jiang, F.; Yang, D.; Shi, W. Acceptability of Pre-Exposure Prophylaxis and Non-Occupational Post-Exposure Prophylaxis among Men Who Have Sex with Men in Guilin, China. Int. J. Environ. Res. Public Health 2022, 19, 3579. [Google Scholar] [CrossRef]
- Liu, Y.; Russ, S.; Mitchell, J.; Przybyla, S.; Zhang, C. Assessing the Determinants of Quality of Life and the Impact on HIV Prevention Measures among HIV-Negative and Status-Unknown Young Men Who Have Sex with Men: A Study in Two U.S. Metropolitan Areas. Int. J. Environ. Res. Public Health 2022, 19, 726. [Google Scholar] [CrossRef]
- Gillespie, D.; Couzens, Z.; de Bruin, M.; Hughes, D.A.; Jones, A.; Ma, R.; Williams, A.; Wood, F.; Blee, K.; Bradshaw, H.S.; et al. PrEP Use, Sexual Behaviour, and PrEP Adherence among Men Who Have Sex with Men Living in Wales Prior to and during the COVID-19 Pandemic. AIDS Behav. 2022, 26, 2746–2757. [Google Scholar] [CrossRef]
- Chen, Y.T.; Duncan, D.T.; Del Vecchio, N.; Timmins, L.; Pagkas-Bather, J.; Lacap, S.; Hotton, A.; Knox, J.; Hanson, H.; Koli, K.; et al. COVID-19-Related Stressors, Sex Behaviors, and HIV Status Neutral Care among Black Men Who Have Sex With Men and Transgender Women in Chicago, USA. J. Acquir. Immune Defic. Syndr. 2021, 88, 261–271. [Google Scholar] [CrossRef] [PubMed]
- Sevelius, J.M.; Glidden, D.V.; Deutsch, M.; Welborn, L.; Contreras, A.; Salinas, A.; Venegas, L.; Grant, R.M. Uptake, Retention, and Adherence to Pre-Exposure Prophylaxis (PrEP) in TRIUMPH: A Peer-Led PrEP Demonstration Project for Transgender Communities in Oakland and Sacramento, California. J. Acquir. Immune Defic. Syndr. 2021, 88, S27–S38. [Google Scholar] [CrossRef] [PubMed]
- Chan, P.A.; Nunn, A.; van den Berg, J.J.; Cormier, K.; Sowemimo-Coker, G.; Napoleon, S.C.; Arnold, T.; Moitra, E. A Randomized Trial of a Brief Behavioral Intervention for PrEP Uptake among Men Who Have Sex with Men at Increased Risk for HIV Infection. J. Acquir. Immune Defic. Syndr. 2021, 87, 937–943. [Google Scholar] [CrossRef] [PubMed]
- Mueses-Marín, H.F.; Alvarado-Llano, B.; Torres-Isasiga, J.; Camargo-Plazas, P.; Bolívar-Rocha, M.C.; Galindo-Orrego, X.; Martínez-Cajas, J.L. Scales to Assess Knowledge, Motivation, and Self-Efficacy for HIV PrEP in Colombian MSM: PrEP-COL Study. AIDS Res. Treat. 2021, 2021, 4789971. [Google Scholar] [CrossRef] [PubMed]
- Gordián-Arroyo, A.; Garofalo, R.; Kuhns, L.M.; Pearson, C.; Bruce, J.; Batey, D.S.; Radix, A.; Belkind, U.; Hidalgo, M.A.; Hirshfield, S.; et al. Awareness, Willingness, and Perceived Efficacy of Pre-Exposure Prophylaxis among Adolescent Sexual Minority Males. J. Urban Health 2020, 97, 749–757. [Google Scholar] [CrossRef]
- Witte, S.S.; Filippone, P.; Ssewamala, F.M.; Nabunya, P.; Bahar, O.S.; Mayo-Wilson, L.J.; Namuwonge, F.; Damulira, C.; Tozan, Y.; Kiyingi, J.; et al. PrEP Acceptability and Initiation among Women Engaged in Sex Work in Uganda: Implications for HIV Prevention. EClinicalMedicine 2022, 44, 101278. [Google Scholar] [CrossRef]
- Guure, C.; Afagbedzi, S.; Torpey, K.; Chaurasia, A. Willingness to Take and Ever Use of Pre-Exposure Prophylaxis among Female Sex Workers in Ghana. Medicine 2022, 101, 28798. [Google Scholar] [CrossRef]
- Matambanadzo, P.; Busza, J.; Mafaune, H.; Chinyanganya, L.; Machingura, F.; Ncube, G.; Steen, R.; Phillips, A.; Cowan, F.M. “It Went through the Roof”: An Observation Study Exploring the Rise in PrEP Uptake among Zimbabwean Female Sex Workers in Response to Adaptations during COVID-19. J. Int. AIDS Soc. 2021, 24 (Suppl. 6), e25813. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, S.; Zhang, Y.; Tan, W.; Xie, W.; Gan, Y.; Zheng, C.; Li, H.; Yang, Z.; Jiang, L.; et al. Use of HIV Post-Exposure Prophylaxis among Men Who Have Sex with Men in Shenzhen, China: A Serial Cross-Sectional Study. AIDS Behav. 2022, 26, 3231–3241. [Google Scholar] [CrossRef]
- Crepaz, N.; Hess, K.L.; Purcell, D.W.; Hall, H.I. Estimating National Rates of HIV Infection among MSM, Persons Who Inject Drugs, and Heterosexuals in the United States. AIDS 2019, 33, 701–708. [Google Scholar] [CrossRef]
- Smith, D.K.; Grohskopf, L.A.; Black, R.J.; Auerbach, J.D.; Veronese, F.; Struble, K.A.; Cheever, L.; Johnson, M.; Paxton, L.A.; Onorato, I.M.; et al. Antiretroviral Postexposure Prophylaxis after Sexual, Injection-Drug Use, or Other Nonoccupational Exposure to HIV in the United States: Recommendations from the U.S. Department of Health and Human Services. MMWR Recomm. Rep. 2005, 54, 1–19. [Google Scholar] [PubMed]
- Yi, S.; Tuot, S.; Mwai, G.W.; Ngin, C.; Chhim, K.; Pal, K.; Igbinedion, E.; Holland, P.; Choub, S.C.; Mburu, G. Awareness and Willingness to Use HIV Pre-Exposure Prophylaxis among Men Who Have Sex with Men in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis. J. Int. AIDS Soc. 2017, 20, 21580. [Google Scholar] [CrossRef] [PubMed]
- Ezennia, O.; Geter, A.; Smith, D.K. The PrEP Care Continuum and Black Men Who Have Sex with Men: A Scoping Review of Published Data on Awareness, Uptake, Adherence, and Retention in PrEP Care. AIDS Behav. 2019, 23, 2654–2673. [Google Scholar] [CrossRef] [PubMed]
- Koechlin, F.M.; Fonner, V.A.; Dalglish, S.L.; O’Reilly, K.R.; Baggaley, R.; Grant, R.M.; Rodolph, M.; Hodges-Mameletzis, I.; Kennedy, C.E. Values and Preferences on the Use of Oral Pre-Exposure Prophylaxis (PrEP) for HIV Prevention among Multiple Populations: A Systematic Review of the Literature. AIDS Behav. 2017, 21, 1325–1335. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Gu, Q.; Dai, Y.; Zou, H.; Agins, B.; Chen, Q.; Li, P.; Shen, J.; Yang, Y.; Jiang, H. Increasing Awareness of HIV Pre-exposure Prophylaxis (PrEP) and Willingness to Use HIV PrEP among Men Who Have Sex with Men: A Systematic Review and Meta-analysis of Global Data. J. Int. AIDS Soc. 2022, 25, e25883. [Google Scholar] [CrossRef]
| First Authors, Year | Location, Study Population, N | Collection Year | Acceptability Measurements | PrEP/nPEP | |
|---|---|---|---|---|---|
| Barriers | Facilitators | ||||
| 1. PrEP 1 studies 1.1 MSM 2 | |||||
| Hulstein et al. [20] (2022) | The Netherlands. Young MSM aged ≤25 years(n = 93), | 2020 | Are you planning to use PrEP in the coming 6 months? | Perceiving PrEP as an important prevention tool, a high level of PrEP knowledge, believing that PrEP users take good care of themselves and others | |
| Chan et al. [21] (2022) | New South Wales. Australia. Gay and Bisexual Men (n = 1477) | 2019–2020 | “New forms of PrEP are currently under development. If all of these options were available, equally effective in preventing HIV, and had a similar cost, which of these would you want to use?”. | Younger age, being born in Australia, currently taking oral PrEP, not being worried about side effects, believing PrEP is affordable, believing that it is easy to remember to take pills, and not having difficulties with waiting for a PrEP appointment | |
| Sharpe et al. [22] (2022) | The non-urban USA. MSM (n = 4792), | 2020 | In the past 12 months, have you taken PrEP? | Residing in PrEP desert (Structure barrier) | |
| Blair et al. [23] (2022) | Brazil. MSM (n = 2398), | 2020 | Are you taking or have you taken PrEP? | Increasing Homosexuality Scale scores, 18–24 yeas-old, Black respondents | Increasing HIV knowledge scores |
| Zhou et al. [24] (2022) | Guilin, China. MSM (n = 219) | 2020–2021 | Overall, how likely would you use PrEP? | Separated/Divorced/Widowed, Labourer, Migrant worker/Farmer, Government employee, Higher Social support, Tested HIV before | |
| Liu et al. [25] (2022) | Nashville, Tennessee, and Buffalo, New York, USA. YMSM 3 (n = 347), convenience sampling | 2019–2020 | PrEP use (ever/current vs. never) | Quality of life domains: physical health, psychological health, and environment | |
| Gillespie et al. [26] (2022) | Wales, UK. MSM (n = 60) | 2019–2020 | Actual PrEP use | The introduction of pandemic-related control measures | |
| Chen et al. [27] (2021) | Chicago, USA. Black MSM and transgender women (n = 222) | 2020 | Self-reported previous use of PrEP | Having physical reactions (eg, sweating and pounding heart) in regards to worries or problems related to COVID-19 and if they reported being in close proximity to a person who had been diagnosed with COVID-19. | |
| Sevelius et al. [28] (2021) | California. USA. MSM (n = 185) | 2017–2020 | Actual PrEP use | Unaware of PrEP before enrolment | |
| Chan et al. [29] (2021) | US. MSM (n = 86) | 2019–2020 | PrEP uptake | Received motivational interviewing intervention | |
| Mueses-Marín et al. [30] (2021) | Colombia. MSM (n = 287) | 2020 | If PrEP is effective in reducing the risk of HIV by 90%, and in the next 12 months PrEP was offered for free in Colombia, would you like to use PrEP to prevent HIV? | Greater degree of PrEP stigma | Higher PrEP knowledge, more positive PrEP attitudes, more descriptive norms, and greater degree of subjective norms. |
| Gordián-Arroyo et al. [31] (2020) | New York City, Birmingham, Chicago, and Seattle. USA. Adolescent MSM (n = 761), convenience sampling | 2020 | Would you take one pill a day to prevent HIV?” (0 = No, 1 = Yes) | Asian participants | |
| 1. PrEP studies 1.2. FSW 4 | |||||
| Witte et al. [32] (2022) | Southwestern Uganda. Women engaged in sex work (n = 283) | 2019–2020 | If PrEP were safe, effective, and free, how likely would you be willing to use it? | Fewer years engaged in sex work, greater perceived social support from family | |
| Guure et al. [33] (2022) | Ghana. FSW (n = 5107). Time location sampling | 2020 | As PrEP has similar side effects to other drugs used to treat HIV, would you be willing to take it? | 25 to 24 years (vs less than 25 years), Ahafo, Bono, Eastern, Greater Accra, Upper west region (VS Ashanti region) | Ever heard about PrEP, screened for STIs, Muslims and other religions (vs. Christians), and had anal sex. |
| Matambanadzo et al. [34] (2021) | Zimbabwean. Female sex workers (n = 19,407). | 2020 | Actual PrEP uptake | Community-based PrEP service delivery model is effective and can be adapted for long-term use. | |
| 2. nPEP 5 studies | |||||
| Zhou et al. [24] (2022) | Guilin, China. MSM (n = 219), RDS 6 | 2020–2021 | Overall, how likely would you use nPEP? | Married or cohabited, Having an HIV-positive sexual partner | Higher Social support, Having HIV status unknown sexual partner, Tested HIV before |
| Wang et al. [35] (2022) | Shenzhen, China. MSM (n = 2833). time location sampling, RDS | 2018–2020 | Whether they have used PEP (Actual nPEP use) | Residence in Shenzhen, condom use in anal sex, lubricant use in anal sex, rush popper use | Having sexual intercourse with women, preferred finding sexual partners in MSM venues, multiple sexual partners (≥2), Viagra use, receiving HIV-related services in clinics or MSM venues, and interest in initiating PrEP. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, L.; Assanangkornchai, S. Current Perspectives on the Determinants of Acceptability of Pre-Exposure Prophylaxis and Nonoccupational Post-Exposure Prophylaxis among People at Risk for HIV: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 12605. https://doi.org/10.3390/ijerph191912605
Zhou L, Assanangkornchai S. Current Perspectives on the Determinants of Acceptability of Pre-Exposure Prophylaxis and Nonoccupational Post-Exposure Prophylaxis among People at Risk for HIV: A Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(19):12605. https://doi.org/10.3390/ijerph191912605
Chicago/Turabian StyleZhou, Lingmi, and Sawitri Assanangkornchai. 2022. "Current Perspectives on the Determinants of Acceptability of Pre-Exposure Prophylaxis and Nonoccupational Post-Exposure Prophylaxis among People at Risk for HIV: A Scoping Review" International Journal of Environmental Research and Public Health 19, no. 19: 12605. https://doi.org/10.3390/ijerph191912605
APA StyleZhou, L., & Assanangkornchai, S. (2022). Current Perspectives on the Determinants of Acceptability of Pre-Exposure Prophylaxis and Nonoccupational Post-Exposure Prophylaxis among People at Risk for HIV: A Scoping Review. International Journal of Environmental Research and Public Health, 19(19), 12605. https://doi.org/10.3390/ijerph191912605







