Intervention Activities Associated with the Implementation of a Comprehensive School Tobacco Policy at Danish Vocational Schools: A Repeated Cross-Sectional Study
Abstract
:1. Introduction
Aim
2. Materials and Methods
2.1. Setting
2.2. The Smoke-Free Vocational Schools Intervention
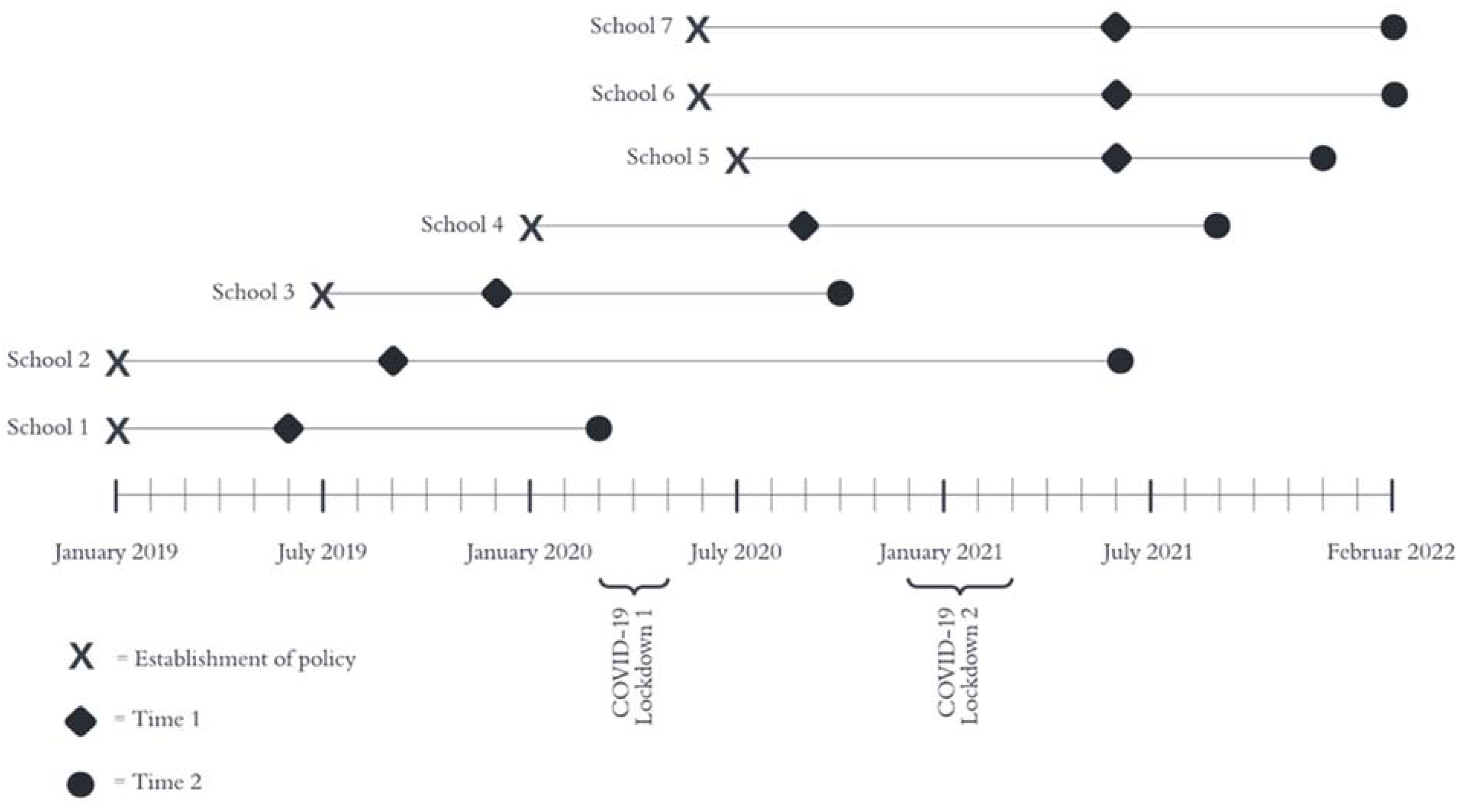
2.3. Study Design
2.4. Data Collection
2.5. Study Population
2.6. Measures
2.6.1. Implementation Fidelity Measures—Dependent Variables
2.6.2. Intervention Activities—Independent Variables
2.6.3. Context—Confounding Variables
2.7. Statistical Analysis
3. Results
4. Discussion
4.1. Key Findings
4.2. Interpretation of Results
4.3. Operationalization of Policy Implementation Outcomes
4.4. Strengths and Limitations
4.5. Implications for Research and Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schreuders, M. Smoke-Free School Policies: Understanding Their Implementation and Impact by Using the Realist Approach. Ph.D. Thesis, Universiteit van Amsterdam, Amsterdam, The Netherlands, 2020. [Google Scholar]
- de Looze, M.; ter Bogt, T.; Hublet, A.; Kuntsche, E.; Richter, M.; Zsiros, E.; Godeau, E.; Vollebergh, W. Trends in educational differences in adolescent daily smoking across Europe, 2002–10. Eur. J. Public Health 2013, 23, 846–852. [Google Scholar] [CrossRef]
- Klinker, C.D.; Aaby, A.; Ringgaard, L.W.; Hjort, A.V.; Hawkins, M.; Maindal, H.T. Health Literacy is Associated with Health Behaviors in Students from Vocational Education and Training Schools: A Danish Population-Based Survey. Int. J. Environ. Res. Public Health 2020, 17, 671. [Google Scholar] [CrossRef]
- Pisinger, V.; Thorsted, A.; Jezek, A.H.; Jørgensen, A.; Christensen, A.I.; Thygesen, L.C. UNG19—Sundhed og trivsel på gymnasiale uddannelser 2019 [The Health and Wellbeing Survey in Danish Generel Upper Secondary Education]; Statens Institut for Folkesundhed, SDU: Copenhagen, Denmark, 2019; ISBN 978-87-7899-489-9. [Google Scholar]
- Lund, L.; Bast, L.S. Danskernes Rygevaner 2020 [The Danish smoking habits in 2020], The Danish Health Authority. 2021. Available online: https://www.sst.dk/-/media/Udgivelser/2021/Tobak/Danskernes-Rygevaner-2020_delrapport-1_04_03_2021.ashx?la=da&hash=8077A894BA39F6DC18B6A4CCFFFC4120768D1BD0 (accessed on 1 September 2022).
- Galanti, M.R.; Coppo, A.; Jonsson, E.; Bremberg, S.; Faggiano, F. Anti-tobacco policy in schools: Upcoming preventive strategy or prevention myth? A review of 31 studies. Tob Control 2014, 23, 295. [Google Scholar] [CrossRef]
- Schreuders, M.; Nuyts, P.A.W.; van den Putte, B.; Kunst, A.E. Understanding the impact of school tobacco policies on adolescent smoking behaviour: A realist review. Soc. Sci. Med. 2017, 183, 19–27. [Google Scholar] [CrossRef]
- Steckler, A.B.; Linnan, L. (Eds.) Process Evaluation for Public Health Interventions and Research, 1st ed.; Jossey-Bass: San Francisco, CA, USA, 2002. [Google Scholar]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D.; et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015, 350, h1258. [Google Scholar] [CrossRef]
- Borsika, R.A.; Brownson, R.C. Chapter 2: Terminology for dissemination and implementation research. In Dissemination and Implementation Research in Health: Translating Science to Practice, 2nd ed.; Oxford University Press: Oxford, UK, 2018. [Google Scholar] [CrossRef]
- May, C.; Finch, T. Implementing, Embedding, and Integrating Practices: An Outline of Normalization Process Theory. Sociology 2009, 43, 535–554. [Google Scholar] [CrossRef]
- Murray, E.; Treweek, S.; Pope, C.; MacFarlane, A.; Ballini, L.; Dowrick, C.; Finch, T.; Kennedy, A.; Mair, F.; O’Donnell, C.; et al. Normalisation process theory: A framework for developing, evaluating and implementing complex interventions. BMC Med. 2010, 8, 63. [Google Scholar] [CrossRef]
- May, C.R.; Mair, F.; Finch, T.; MacFarlane, A.; Dowrick, C.; Treweek, S.; Rapley, T.; Ballini, L.; Ong, B.N.; Rogers, A.; et al. Development of a theory of implementation and integration: Normalization Process Theory. Implement. Sci. 2009, 4, 29. [Google Scholar] [CrossRef] [PubMed]
- Proctor, E.; Silmere, H.; Raghavan, R.; Hovmand, P.; Aarons, G.; Bunger, A.; Griffey, R.; Hensley, M. Outcomes for Implementation Research: Conceptual Distinctions, Measurement Challenges, and Research Agenda. Adm. Policy Ment. Health 2011, 38, 65–76. [Google Scholar] [CrossRef] [Green Version]
- Linnansaari, A.; Schreuders, M.; Kunst, A.E.; Rimpelä, A.; Lindfors, P. Understanding school staff members’ enforcement of school tobacco policies to achieve tobacco-free school: A realist review. Syst. Rev. 2019, 8, 177. [Google Scholar] [CrossRef]
- Barnett, T.A.; Gauvin, L.; Lambert, M.; O’Loughlin, J.; Paradis, G.; McGrath, J.J. The Influence of School Smoking Policies on Student Tobacco Use. Arch. Pediatr. Adolesc. Med. 2007, 161, 842. [Google Scholar] [CrossRef] [PubMed]
- Darling, H.; Reeder, A.I.; Williams, S.; McGee, R. Is there a relation between school smoking policies and youth cigarette smoking knowledge and behaviors? Health Educ. Res. 2006, 21, 108–115. [Google Scholar] [CrossRef]
- Hamilton, G.; Cross, D.; Lower, T.; Resnicow, K.; Williams, P. School policy: What helps to reduce teenage smoking? Nicotine Tob. Res. 2003, 5, 507–513. [Google Scholar] [CrossRef]
- Kuipers, M.A.G.; de Korte, R.; Soto, V.E.; Richter, M.; Moor, I.; Rimpelä, A.H.; Perelman, J.; Federico, B.; Kunst, A.E.; Lorant, V. School smoking policies and educational inequalities in smoking behaviour of adolescents aged 14–17 years in Europe. J. Epidemiol. Community Health 2016, 70, 132–139. [Google Scholar] [CrossRef]
- Lipperman-Kreda, S.; Paschall, M.J.; Grube, J.W. Perceived enforcement of school tobacco policy and adolescents’ cigarette smoking. Prev. Med. 2009, 48, 562–566. [Google Scholar] [CrossRef]
- Rozema, A.; Hiemstra, M.; Mathijssen, J.; Jansen, M.; van Oers, H. Impact of an Outdoor Smoking Ban at Secondary Schools on Cigarettes, E-Cigarettes and Water Pipe Use among Adolescents: An 18-Month Follow-Up. Int. J. Environ. Res. Public Health 2018, 15, 205. [Google Scholar] [CrossRef]
- Wakefield, M.A. Effect of restrictions on smoking at home, at school, and in public places on teenage smoking: Cross sectional study. BMJ 2000, 321, 333–337. [Google Scholar] [CrossRef]
- Dusenbury, L.; Brannigan, R.; Falco, M.; Hansen, W.B. A review of research on fidelity of implementation: Implications for drug abuse prevention in school settings. Health Educ. Res. 2003, 18, 237–256. [Google Scholar] [CrossRef]
- Bast, L.S.; Due, P.; Bendtsen, P.; Ringgard, L.; Wohllebe, L.; Damsgaard, M.T.; Grønbæk, M.; Ersbøll, A.K.; Andersen, A. High impact of implementation on school-based smoking prevention: The X:IT study—A cluster-randomized smoking prevention trial. Implement. Sci. 2015, 11. [Google Scholar] [CrossRef] [Green Version]
- Mélard, N.; Grard, A.; Robert, P.-O.; Kuipers, M.A.G.; Schreuders, M.; Rimpelä, A.H.; Leão, T.; Hoffmann, L.; Richter, M.; Kunst, A.E.; et al. School tobacco policies and adolescent smoking in six European cities in 2013 and 2016: A school-level longitudinal study. Prev. Med. 2020, 138, 106142. [Google Scholar] [CrossRef] [PubMed]
- Schreuders, M.; Kuipers, M.A.; Mlinarić, M.; Grard, A.; Linnansaari, A.; Rimpela, A.; Richter, M.; Perelman, J.; Lorant, V.; van den Putte, B.; et al. The association between smoke-free school policies and adolescents’ anti-smoking beliefs: Moderation by family smoking norms. Drug Alcohol Depend. 2019, 204, 107521. [Google Scholar] [CrossRef]
- Kumar, R.; O’Malley, P.M.; Johnston, L.D. School Tobacco Control Policies Related to Students’ Smoking and Attitudes Toward Smoking: National Survey Results, 1999–2000. Health Educ. Behav. 2005, 32, 780–794. [Google Scholar] [CrossRef] [PubMed]
- Piontek, D.; Buehler, A.; Donath, C.; Floeter, S.; Rudolph, U.; Metz, K.; Gradl, S.; Kroeger, C. School Context Variables and Students’ Smoking. Eur. Addict. Res. 2008, 14, 53–60. [Google Scholar] [CrossRef]
- Sabiston, C.M.; Lovato, C.Y.; Ahmed, R.; Pullman, A.W.; Hadd, V.; Campbell, H.S.; Nykiforuk, C.; Brown, K.S. School Smoking Policy Characteristics and Individual Perceptions of the School Tobacco Context: Are They Linked to Students’ Smoking Status? J. Youth Adolesc. 2009, 38, 1374–1387. [Google Scholar] [CrossRef]
- Wiium, N.; Wold, B. Actions taken by schools when tobacco policies are violated: Associations with adolescent smoking prevalence: Violation of policy, actions taken and smoking. Scand. J. Psychol. 2011, 52, 494–501. [Google Scholar] [CrossRef] [PubMed]
- Evans-Whipp, T.J.; Bond, L.; Toumbourou, J.W.; Catalano, R.F. School, Parent, and Student Perspectives of School Drug Policies. J. Sch. Health 2007, 77, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Andersen, S.; Pisinger, V.; Rod, M.H.; Tolstrup, J. Associations of school tobacco policies and legislation with youth smoking: A cross-sectional study of Danish vocational high schools. BMJ Open 2019, 9, e028357. [Google Scholar] [CrossRef] [PubMed]
- Lovato, C.Y.; Zeisser, C.; Campbell, H.S.; Watts, A.W.; Halpin, P.; Thompson, M.; Eyles, J.; Adlaf, E.; Brown, K.S. Adolescent Smoking: Effect of school and community characteristics. Am. J. Prev. Med. 2010, 39, 507–514. [Google Scholar] [CrossRef]
- Balloun, J.L.; Barrett, H.; Weinstein, A. One is Not Enough: The Need for Multiple Respondents in Survey Research of Organizations. J. Mod. App. Stat. Meth. 2011, 10, 287–299. [Google Scholar] [CrossRef] [Green Version]
- Rozema, A.D.; Mathijssen, J.J.P.; van Kesteren, J.N.; van Oers, J.A.M.; Jansen, M.W.J. Results of outdoor smoking bans at secondary schools on adolescents smoking behaviour: A quasi-experimental study. Eur. J. Public Health 2019, 29, 765–771. [Google Scholar] [CrossRef]
- Murnaghan, D.A.; Leatherdale, S.T.; Sihvonen, M.; Kekki, P. School-based tobacco-control programming and student smoking behaviour. Chronic Dis. Can 2009, 29, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Trinidad, D.R.; Gilpin, E.A.; Pierce, J.P. Compliance and support for smoke-free school policies. Health Educ. Res. 2005, 20, 466–475. [Google Scholar] [CrossRef] [PubMed]
- Kunst, A. SILNE-R (Horizon2020). Tob. Prev. Cessat. 2016, 2. [Google Scholar] [CrossRef]
- Schreuders, M.; van den Putte, B.; Kunst, A.E. Smoke-free school policies in Europe: Challenges for the future. Prev. Med. 2020, 138, 106130. [Google Scholar] [CrossRef]
- Hjort, A.V.; Schreuders, M.; Rasmussen, K.H.; Klinker, C.D. Are Danish vocational schools ready to implement “smoke-free school hours”? A qualitative study informed by the theory of organizational readiness for change. Implement. Sci. Commun. 2021, 2. [Google Scholar] [CrossRef] [PubMed]
- Hjort, A.V.; Christiansen, T.B.; Stage, M.; Rasmussen, K.H.; Pisinger, C.; Tjørnhøj-Thomsen, T.; Klinker, C.D. Programme theory and realist evaluation of the ‘Smoke-Free Vocational Schools’ research and intervention project: A study protocol. BMJ Open 2021, 11, e042728. [Google Scholar] [CrossRef]
- Ringgaard, L.W.; Heinze, C.; Andersen, N.B.S.; Hansen, G.I.L.; Hjort, A.V.; Klinker, C.D. UNG19—Sundhed og trivsel på Erhvervsuddannelser 2019 [The Health and Wellbeing Survey in Danish Vocational Education and Training]; Region Hovedstaden: Herlev, Denmark, 2020; ISBN 978-87-92759-32-0. [Google Scholar]
- Sundheds-og Ældreministeriet [Ministry of Health]. Bekendtgørelse om Information og Samtykke i Forbindelse Med Behandling og ved Videregivelse og Indhentning af Helbredsoplysninger m.v. BEK nr 359 af 04/04/2019. [Executive Order on Information and Consent in Connection with Processing and in the Transmission and Gathering of Health Information, etc. BEK nr 359 af 04/04/2019]. 2019. Available online: https://www.retsinformation.dk/eli/lta/2019/359 (accessed on 1 December 2020).
- Finch, T.L.; Girling, M.; May, C.R.; Mair, F.S.; Murray, E.; Treweek, S.; McColl, E.; Steen, I.N.; Cook, C.; Vernazza, C.R.; et al. Improving the normalization of complex interventions: Part 2—validation of the NoMAD instrument for assessing implementation work based on normalization process theory (NPT). BMC Med. Res. Methodol. 2018, 18, 135. [Google Scholar] [CrossRef] [PubMed]
- Boyce, J.C.; Mueller, N.B.; Hogan-Watts, M.; Luke, D.A. Evaluating the Strength of School Tobacco Policies: The Development of a Practical Rating System. J. Sch. Health 2009, 79, 495–504. [Google Scholar] [CrossRef]
- Wenger-Trayner, É. Communities of Practice: Learning, Meaning, and Identity; 18th Printing; Cambridge University Press: Cambridge, UK, 2008. [Google Scholar]
- Eldridge, S.M.; Ukoumunne, O.C.; Carlin, J.B. The Intra-Cluster Correlation Coefficient in Cluster Randomized Trials: A Review of Definitions. Int. Stat. Rev. 2009, 77, 378–394. [Google Scholar] [CrossRef]
- Twisk, J.W.R. Applied Multilevel Analysis: A Practical Guide; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2006. [Google Scholar]
- Killip, S. What Is an Intracluster Correlation Coefficient? Crucial Concepts for Primary Care Researchers. Ann. Fam. Med. 2004, 2, 204–208. [Google Scholar] [CrossRef]
- Linton, J.D. Implementation research: State of the art and future directions. Technovation 2002, 22, 65–79. [Google Scholar] [CrossRef]
- Andersen, S.; Tolstrup, J.S.; Rod, M.H.; Ersbøll, A.K.; Sørensen, B.B.; Holmberg, T.; Johansen, C.; Stock, C.; Laursen, B.; Zinckernagel, L.; et al. Shaping the Social: Design of a settings-based intervention study to improve well-being and reduce smoking and dropout in Danish vocational schools. BMC Public Health 2015, 15, 568. [Google Scholar] [CrossRef]
- Schreuders, M.; Klompmaker, L.; van den Putte, B.; Kunst, A. Adolescent Smoking in Secondary Schools that Have Implemented Smoke-Free Policies: In-Depth Exploration of Shared Smoking Patterns. Int. J. Environ. Res. Public Health 2019, 16, 2100. [Google Scholar] [CrossRef]
- Andersen, S.; Rod, M.H.; Ersbøll, A.K.; Stock, C.; Johansen, C.; Holmberg, T.; Zinckernagel, L.; Ingholt, L.; Sørensen, B.B.; Tolstrup, J.S. Effects of a settings-based intervention to promote student wellbeing and reduce smoking in vocational schools: A non-randomized controlled study. Soc. Sci. Med. 2016, 161, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Sigfusdottir, I.D.; Thorlindsson, T.; Kristjansson, A.L.; Roe, K.M.; Allegrante, J.P. Substance use prevention for adolescents: The Icelandic Model. Health Promot. Int. 2008, 24, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Record, R.A.; Helme, D.; Savage, M.W.; Harrington, N.G. Let’s Clear the Air: A campaign that effectively increased compliance with a university’s tobacco-free policy. J. Appl. Commun. Res. 2017, 45, 79–95. [Google Scholar] [CrossRef]
- Wilson, N.; Thomson, G. Surveying all outdoor smokefree signage in contrasting suburbs: Methods and results. Health Promot. J. Austr. 2017, 28, 264–265. [Google Scholar] [CrossRef]
- Piontek, D.; Buehler, A.; Rudolph, U.; Metz, K.; Kroeger, C.; Gradl, S.; Floeter, S.; Donath, C. Social contexts in adolescent smoking: Does school policy matter? Health Educ. Res. 2007, 23, 1029–1038. [Google Scholar] [CrossRef]
- Martinez, R.G.; Lewis, C.C.; Weiner, B.J. Instrumentation issues in implementation science. Implement. Sci. 2014, 9, 118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glasgow, R.E.; Riley, W.T. Pragmatic Measures. Am. J. Prev. Med. 2013, 45, 237–243. [Google Scholar] [CrossRef]
- Jakobsen, G.; Danielsen, D.; Jensen, M.; Vinther, J.; Pisinger, C.; Holmberg, T.; Krølner, R.; Andersen, S. Reducing smoking in youth by a smoke-free school environment: A stratified cluster randomized controlled trial of Focus, a multicomponent program for alternative high schools. Tob. Prev. Cessat. 2021, 7, 42. [Google Scholar] [CrossRef]
- Baillie, L.E.; Lovato, C.Y.; Taylor, E.; Rutherford, M.B.; Smith, M. The pit and the pendulum: The impact on teen smokers of including a designated smoking area in school tobacco control policy. Health Educ. Res. 2007, 23, 1008–1015. [Google Scholar] [CrossRef]
- Turner, K.M. Butt in, butt out: Pupils’ views on the extent to which staff could and should enforce smoking restrictions. Health Educ. Res. 2004, 19, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Proctor, E.K.; Brownson, R.C. Chapter 13: Measurement Issues in Dissemination and Implementation Research. In Dissemination and Implementation Research in Health: Translating Science to Practice, 2nd ed.; Oxford University Press: Oxford, UK, 2018. [Google Scholar] [CrossRef]
- Leatherdale, S.T.; Brown, K.S.; Cameron, R.; McDonald, P.W. Social modeling in the school environment, student characteristics, and smoking susceptibility: A multi-level analysis. J. Adolesc. Health 2005, 37, 330–336. [Google Scholar] [CrossRef]
- Lewis, C.C.; Weiner, B.J.; Stanick, C.; Fischer, S.M. Advancing implementation science through measure development and evaluation: A study protocol. Implement. Sci. 2015, 10, 102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Intervention Activity | Description | Purpose | Target Population |
|---|---|---|---|
| New school-break facilities | During a participatory workshop, students co-created ideas on how to improve the social environment, and the school received funding to implement ideas (€15,000 per school). | To replace social smoking with locally acceptable activities. | Students |
| Smoke-free signage | Smoke-free signage (e.g., posters, go-cards) was provided for the schools, and the schools had the option to create their own smoke-free signage (e.g., a smoke-free logo). | To make the policy visible to students (and others). | Students |
| Help for students to cope with not smoking during school hours | Selected staff and managers participated in a two-day motivational interviewing course, which was tailored to target students enrolled in upper-secondary education. During the course, the participants learned about the social, psychological, and physical aspects of nicotine dependence and how to address the students who were struggling with not smoking during school hours in a positive, communicative way. (Average of n = 10 educated staff at each intervention school.) | To provide support to students who find it difficult not to smoke during school hours | Students |
| Smoking cessation assistance | Smoking cessation courses were offered in collaboration with the local municipality. The courses were offered to both students and staff/managers (separate courses). | To facilitate smoking cessation for students who were motivated to quit smoking. | Students |
| A joint workshop before policy implementation | A joint workshop for all staff and managers was held to discuss the purpose and legitimacy of the smoke-free school hours policy. At the workshop, the principal presented the school’s motives for adopting the policy as well as the rules for sanctioning and enforcement. Knowledge about organizational change processes and the complexity of nicotine dependence was also presented by a psychologist from a public health NGO. In addition, facilitated group discussions and exercises took place. (n = 1 joint workshop at each school.) | To stimulate a shared understanding of why the school is implementing the policy. Additional goals were to develop a shared language and tools that can be used in the implementation process. | Staff/managers |
| Internalization of fixed enforcement procedures | The schools were obliged to develop school-specific rules for sanctioning and enforcement. The schools were advised to establish rules with a progressive application of disciplinary measures. The rules were then integrated into the schools’ rules of conduct and communicated to all staff and students. | To clearly communicate the rules, so staff and managers know what to do if students violate the policy. | Staff/managers |
| Support from public health NGOs and local municipality | Throughout the intervention, the schools were supported by both the local municipality and two Danish public health NGOs (the Danish Heart Foundation and the Danish Cancer Society). The NGOs delivered the intervention activities at the schools. Approximately n = 5–6 encounters per school in addition to the intervention activities. | To provide support for the schools in the implementation process, when needed. | Staff/managers |
| Implementation Fidelity Concepts | Definition | Items | Response Categories. Satisfactory Levels of Implementation for the Binary Transformation in Bold |
|---|---|---|---|
| Student level | |||
| Adherence | Familiarity with policy entailments | What are the school’s rules on smoking? | We are allowed to smoke everywhere on school property/We are allowed to smoke in designated smoking areas/We are only allowed to smoke outside school premises/We are not allowed to smoke during the entire school day-neither on school grounds nor outside school grounds/I don’t know the school’s rules on smoking/The school doesn’t have rules on smoking |
| Dose | Exposure to smoking during school hours | How often do you see school students smoking during school hours? | Every day or several times a day/Almost daily or a couple of times per week/Circa once a week/Less than once a week/A few times per month/Rarer/Never |
| Quality of delivery | Enforcement of policy | What normally happens when students break the school’s rules on smoking? | Reprimand or negative sanctioning/Help to cope with not smoking during school hours (e.g., referral to school or municipal smoking cessation counselors)/Other/Nothing happens/I don’t know |
| Participant responsiveness | Sense of policy implementation | At your school, do you sense that students smoke during school hours? | Yes, on the school premises/Yes, outside the school premises/No/I don’t know |
| Staff/manager level | |||
| Adherence | Familiarity with policy entailments | Is it currently permitted for school students to smoke cigarettes during the school day? | Yes/Yes, outside school premises/No/I don’t know |
| Dose | Exposure to smoking during school hours | How often do you see school students smoking during school hours? | Every day or several times a day/Almost daily or a couple of times per week/Circa once a week/Less than once a week/A few times per month/Rarer/Never |
| Quality of delivery | Enforcement of policy | New variable constructed by a crosstab of: How often do you articulate/enforce the smoke-free school hours policy? AND ‘Exposure to smoking during school hours’ construct (Dose) | Policy is enforced every day/Almost daily/Circa once a week/Less than once a week/A few times per month AND Students are seen smoking every day/Almost daily/Circa once a week Policy is enforced every day/Almost daily/Circa once a week/Less than once a week/A few times per month AND Students are seen smoking less than once a week/A few times per month/Rarer/NeverPolicy is never/rarely enforced AND Students are seen smoking less than once a week/A few times per month/Rarer/Never Policy is never/rarely enforced AND Students are seen smoking every day/Almost daily/Circa once a week |
| Participant responsiveness | Sense of policy implementation | To what extent do you feel that smoke-free school hours are currently a normal part of everyday life at school? | 1 = Very little extent, 2 = Little extent, 3 = Neutral, 4 = Large extent, 5 = Very large extent |
| Intervention Activity | Definition | Items | Responses Categories | Timing |
|---|---|---|---|---|
| Student level | ||||
| New school-break facilities | Appraisal | Do you agree or disagree with the following statement: After the school established smoke-free school hours, there are a lot of things to do during school breaks | 1 = Strongly disagree, 2 = Disagree, 3 = Neutral, 4 = Agree, 5 = Strongly agree | At T1 and T2 |
| Smoke-free signage | Prominence of smoke-free signage | To what extent do you think the smoke-free school hours signage is visible at your school? | 1 = Very little extent, 2 = Little extent, 3 = Neutral, 4 = Large extent, 5 = Very large extent | At T1 and T2 |
| Motivational interviewing | Support to cope with not smoking during school hours and smoking cessation assistance | To what extent do you experience that there are staff at this school who can… (1) help you deal with smoking urges during school hours, (2) help you with smoking cessation | 1 = Very little extent, 2 = Little extent, 3 = Neutral, 4 = Large extent, 5 = Very large extent | At T1 and T2 |
| Smoking cessation assistance | ||||
| Staff/manager level | ||||
| Joint workshop for all organizational members | A shared understanding, new competences and ideas, and a shared language (mutual engagement, joint enterprise, and shared repertoire) | Do you agree or disagree with the following statements: The joint meeting contributed to… (1) give us a shared understanding of why we have/are going to have smoke-free school hours, (2) give us concrete ideas about how to support students to cope with smoke-free school hours, (3) give me new knowledge about the complexity of nicotine dependence, (4) set in motion a dialogue about smoke-free school hours at the school, (5) give us a shared language, which we use when we talk about smoke-free school hours among employees | 1 = Strongly disagree, 2 = Disagree, 3 = Neutral, 4 = Agree, 5 = Strongly agree | Before policy |
| Internalization of fixed enforcement procedures | Internalization of fixed enforcement procedures | To what extent do you feel equipped to enforce smoke-free school hours? (i.e., know what to do or who to refer to do) | 1 = Very little extent, 2 = Little extent, 3 = Neutral, 4 = Large extent, 5 = Very large extent | At T1 and T2 |
| Experienced support from NGOs and local municipality | Appraisal | Do you agree or disagree with the following statement: External help from the municipality or The Danish Cancer Society or The Danish Heart Foundation is supportive in relation to our work with smoke-free school hours | 1 = Strongly disagree, 2 = Disagree, 3 = Neutral, 4 = Agree, 5 = Strongly agree | At T1 and T2 |
| Students T1 | Students T2 | Staff/Managers T1 | Staff/Managers T2 | |
|---|---|---|---|---|
| Individuals, N (%) | 1222 (100) | 1452 (100) | 419 (100) | 452 (100) |
| Age, range | 15–63 | 15–66 | 20–67 | 17–76 |
| Age, mean (SD) | 23.5 (9.3) | 22.5 (8.5) | 48.6 (9.8) | 46.9 (10.2) |
| Male gender, % | 59.0 | 58.5 | 42.7 | 42.7 |
| Smoking prevalence *, % | 30.5 | 27.3 | 12.9 | 12.4 |
| Educational track, % | ||||
| Care, health, and pedagogy | 29.2 | 28.2 | NA | NA |
| Administration, commerce, and business service | 17.9 | 27.7 | NA | NA |
| Food, agriculture, and hospitality | 5.8 | 7.0 | NA | NA |
| Technology, construction, and transportation | 47.1 | 37.0 | NA | NA |
| Educational level, % | ||||
| Vocational school-normal | 74.0 | 66.0 | NA | NA |
| Vocational school-higher | 26.0 | 34.0 | NA | NA |
| School position, % | ||||
| Manager | NA | NA | 11.0 | 5.7 |
| Teacher | NA | NA | 62.8 | 65.9 |
| Counsellor | NA | NA | 6.7 | 6.9 |
| Administrative | NA | NA | 11.7 | 11.0 |
| Other positions | NA | NA | 7.9 | 10.6 |
| Special function in relation to health promotion **, % | NA | NA | 47.5 | 47.0 |
| Intervention Activities * | Students T1 Mean (SD) | Students T2 Mean (SD) | Staff/Managers T1 Mean (SD) | Staff/Managers T2 Mean (SD) |
|---|---|---|---|---|
| New school-break facilities | 2.82 (±1.1) | 2.91 (±1.2) | NA | NA |
| Smoke-free signage | 2.58 (±1.3) | 2.52 (±1.3) | NA | NA |
| Help to deal with not smoking during school hours and smoking cessation assistance | 2.01 (±1.2) | 1.73 (±1.0) | NA | NA |
| Joint workshop before policy implementation | NA | NA | 3.35 (±0.9) | 3.35 (±0.9) |
| Internalization of fixed enforcement procedures | NA | NA | 3.07 (±1.1) | 2.98 (±1.0) |
| Experienced support from NGOs and local municipality | NA | NA | 3.46 (±0.9) | 3.36 (±0.8) |
| Students T1 % | Students T2 % | Staff/Managers T1 % | Staff/Managers T2 % | |
|---|---|---|---|---|
| Adherence | 87.3 | 86.8 | 93.6 | 93.8 |
| Dose | 28.2 | 32.7 | 65.4 | 68.6 |
| Quality of delivery | 91.1 | 92.6 | 70.6 | 62.8 |
| Participant responsiveness | 25.3 | 28.4 | 51.1 | 67.7 |
| Total implementation fidelity, mean (SD) * | 2.24 (0.8) | 2.36 (0.8) | 2.80 (0.8) | 2.92 (0.7) |
| Odds Ratio (OR) with 95% Confidence Interval (95% CI) p-Value | Linear Effect with 95% CI and p-Value | ||||
|---|---|---|---|---|---|
| Intervention Activities | Adherence | Dose | Quality of Delivery | Participant Responsiveness | Total Implementation Fidelity |
| Student level-time 1 (T1) | |||||
| New school-break facilities | 1.24 [1.05–1.45] 0.008 | 1.16 [1.03–1.31] 0.009 | 1.26 [1.02–1.56] 0.002 | 1.06 [0.94–1.20] 0.290 | 0.08 [0.03–0.12] 0.000 |
| Smoke-free signage | 1.43 [1.24–1.65] 0.000 | 0.94 [0.86–1.04] 0.291 | 1.15 [0.96–1.37] 0.119 | 0.93 [0.87–1.04] 0.223 | 0.02 [−0.008–0.06] 0.145 |
| Help to cope with not smoking during school hours and smoking cessation assistance | 1.06 [0.77–1.46] 0.687 | 1.04 [0.86–1.26] 0.665 | 1.70 [1.02–2.83] 0.037 | 1.05 [0.84–1.30] 0.654 | 0.06 [−0.008–0.12] 0.082 |
| Student level-time 2 (T2) | |||||
| New school-break facilities | 0.89 [0.77–1.03] 0.139 | 1.18 [1.06–1.31] 0.001 | 1.25 [1.04–1.50] 0.017 | 1.27 [1.14–1.43] 0.000 | 0.07 [0.03–0.11] 0.000 |
| Smoke-free signage | 1.39 [1.22–1.58] 0.000 | 0.92 [0.84–1.00] 0.06 | 1.14 [0.97–1.35] 0.103 | 0.94 [0.86–1.03] 0.175 | 0.01 [−0.01–0.05] 0.255 |
| Help to cope with not smoking during school hours and smoking cessation assistance * | 1.02 [0.72–1.46] 0.881 | 0.89 [0.71–1.13] 0.364 | 0.99 [0.59–1.65] 0.978 | 1.05 [0.84–1.32] 0.631 | −0.003 [−0.08–0.07] 0.934 |
| Odds Ratio (OR) with 95% Confidence Interval (95% CI) p-Value | Linear Effect with 95% CI and p-Value | ||||
|---|---|---|---|---|---|
| Intervention Activities | Adherence | Dose | Quality of Delivery | Participant Responsiveness | Total Implementation Fidelity |
| Staff/manager level-Time 1 (T1) | |||||
| Joint workshop before policy implementation | 1.45 [0.50–4.21] 0.489 | 0.95 [0.65–1.40] 0.821 | 1.17 [0.81–1.68] 0.394 | 1.66 [1.13–2.46] 0.010 | 0.13 [0.02–0.25] 0.022 |
| Internalization of fixed enforcement procedures | 1.92 [1.28–2.88] 0.001 | 1.09 [0.89–1.33] 0.402 | 1.17 [0.95–1.44] 0.131 | 1.59 [1.29–1.97] 0.000 | 0.19 [0.13–0.26] 0.000 |
| Experienced support from NGOs and local municipality | 1.08 [0.69–1.68] 0.702 | 1.09 [0.86–1.39] 0.442 | 1.19 [0.93–1.51] 0.150 | 1.51 [1.18–1.95] 0.001 | 0.14 [0.05–0.22] 0.001 |
| Staff/manager level-Time 2 (T2) | |||||
| Joint workshop before policy implementation | 1.46 [0.46–4.65] 0.514 | 1.03 [0.65–1.64] 0.869 | 1.10 [0.69–1.73] 0.679 | 1.73 [1.08–2.76] 0.021 | 0.13 [0.004–0.24] 0.05 |
| Internalization of fixed enforcement procedures | 1.57 [1.05–2.34] 0.023 | 1.17 [0.94–1.45] 0.140 | 1.05 [0.86–1.28] 0.617 | 1.66 [1.33–2.06] 0.000 | 0.16 [0.10–0.23] 0.000 |
| Experienced support from NGOs and local municipality | 0.80 [0.48–1.31] 0.383 | 1.01 [0.77–1.33] 0.926 | 1.12 [0.87–1.45] 0.352 | 1.09 [0.83–1.43] 0.504 | 0.04 [−0.05–0.12] 0.421 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hjort, A.V.; Kuipers, M.A.G.; Stage, M.; Pisinger, C.; Klinker, C.D. Intervention Activities Associated with the Implementation of a Comprehensive School Tobacco Policy at Danish Vocational Schools: A Repeated Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 12489. https://doi.org/10.3390/ijerph191912489
Hjort AV, Kuipers MAG, Stage M, Pisinger C, Klinker CD. Intervention Activities Associated with the Implementation of a Comprehensive School Tobacco Policy at Danish Vocational Schools: A Repeated Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(19):12489. https://doi.org/10.3390/ijerph191912489
Chicago/Turabian StyleHjort, Anneke Vang, Mirte A. G. Kuipers, Maria Stage, Charlotta Pisinger, and Charlotte Demant Klinker. 2022. "Intervention Activities Associated with the Implementation of a Comprehensive School Tobacco Policy at Danish Vocational Schools: A Repeated Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 19: 12489. https://doi.org/10.3390/ijerph191912489
APA StyleHjort, A. V., Kuipers, M. A. G., Stage, M., Pisinger, C., & Klinker, C. D. (2022). Intervention Activities Associated with the Implementation of a Comprehensive School Tobacco Policy at Danish Vocational Schools: A Repeated Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(19), 12489. https://doi.org/10.3390/ijerph191912489






