The Effect of Physical Activity Interventions Carried Out in Outdoor Natural Blue and Green Spaces on Health Outcomes: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources and Search Strategy
2.2. Quality Assessment and Data Extraction
3. Results
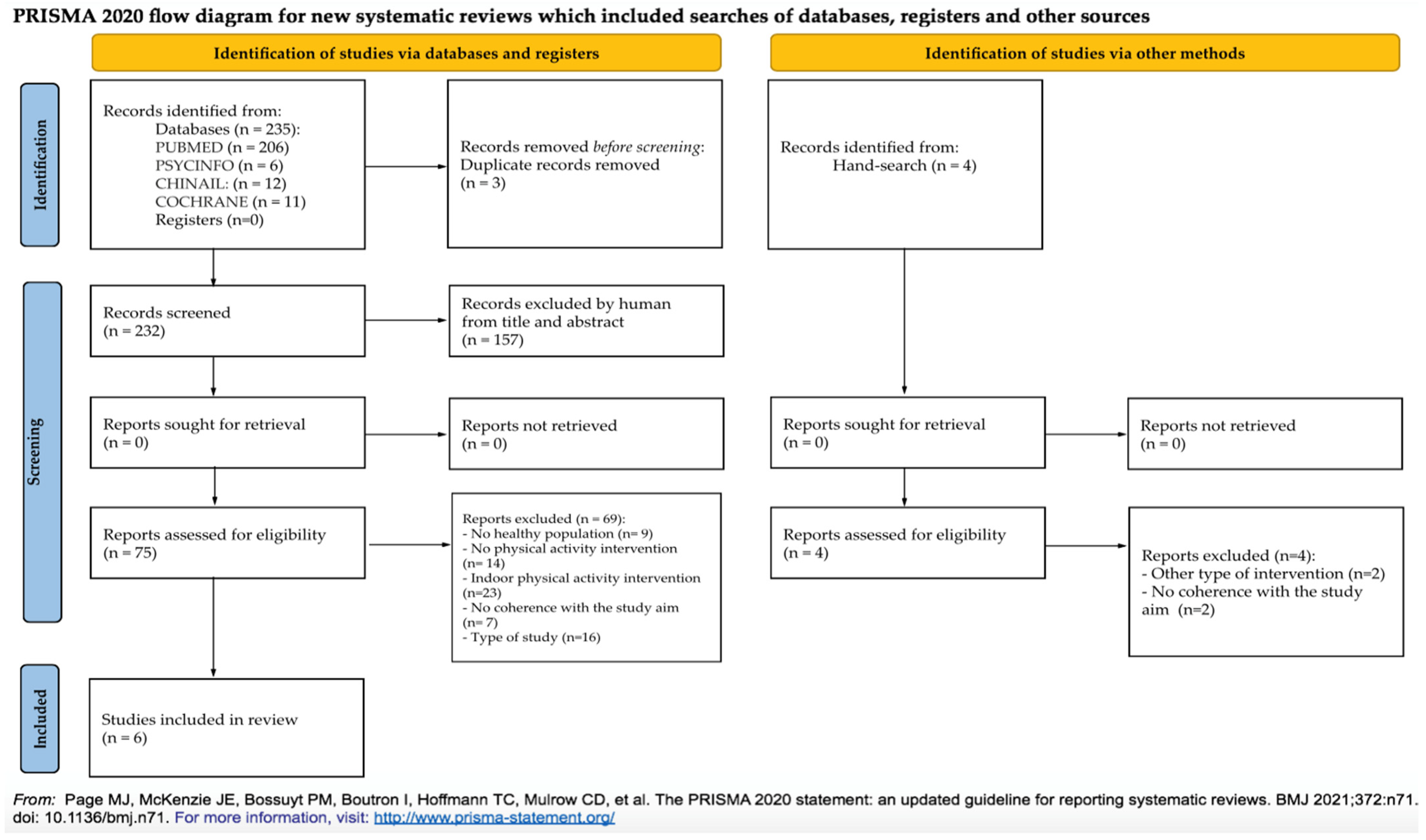
3.1. Study Selection and Characteristics
3.2. Risk of Bias Assessment
3.3. Data Extraction of the Included Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dadvand, P.; Bartoll, X.; Basagaña, X.; Dalmau-Bueno, A.; Martinez, D.; Ambros, A.; Cirach, M.; Triguero-Mas, M.; Gascon, M.; Borrell, C.; et al. Green Spaces and General Health: Roles of Mental Health Status, Social Support, and Physical Activity. Environ. Int. 2016, 91, 161–167. [Google Scholar] [CrossRef]
- Grellier, J.; White, M.P.; Albin, M.; Bell, S.; Elliott, L.R.; Gascón, M.; Gualdi, S.; Mancini, L.; Nieuwenhuijsen, M.J.; Sarigiannis, D.A.; et al. BlueHealth: A Study Programme Protocol for Mapping and Quantifying the Potential Benefits to Public Health and Well-Being from Europe’s Blue Spaces. BMJ Open 2017, 7, e016188. [Google Scholar] [CrossRef]
- State of World Population. 2007. Available online: https://www.unfpa.org/publications/state-world-population-2007 (accessed on 10 August 2022).
- Gascon, M.; Zijlema, W.; Vert, C.; White, M.P.; Nieuwenhuijsen, M.J. Outdoor Blue Spaces, Human Health and Well-Being: A Systematic Review of Quantitative Studies. Int. J. Hyg. Environ. Health 2017, 220, 1207–1221. [Google Scholar] [CrossRef]
- Coventry, P.A.; Brown Jennifer, V.E.; Pervin, J.; Brabyn, S.; Pateman, R.; Breedvelt, J.; Gilbody, S.; Stancliffe, R.; McEachan, R.; White, P.C.L. Nature-Based Outdoor Activities for Mental and Physical Health: Systematic Review and Meta-Analysis. SSM-Popul. Health 2021, 16, 100934. [Google Scholar] [CrossRef] [PubMed]
- Grigoletto, A.; Mauro, M.; Maietta Latessa, P.; Iannuzzi, V.; Gori, D.; Campa, F.; Greco, G.; Toselli, S. Impact of Different Types of Physical Activity in Green Urban Space on Adult Health and Behaviors: A Systematic Review. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 263–275. [Google Scholar] [CrossRef]
- Georgiou, M.; Morison, G.; Smith, N.; Tieges, Z.; Chastin, S. Mechanisms of Impact of Blue Spaces on Human Health: A Systematic Literature Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 2486. [Google Scholar] [CrossRef]
- Mizen, A.; Song, J.; Fry, R.; Akbari, A.; Berridge, D.; Parker, S.C.; Johnson, R.; Lovell, R.; Lyons, R.A.; Nieuwenhuijsen, M.; et al. Longitudinal Access and Exposure to Green-Blue Spaces and Individual-Level Mental Health and Well-Being: Protocol for a Longitudinal, Population-Wide Record-Linked Natural Experiment. BMJ Open 2019, 9, e027289. [Google Scholar] [CrossRef] [PubMed]
- Lynch, M.; Spencer, L.H.; Tudor Edwards, R. A Systematic Review Exploring the Economic Valuation of Accessing and Using Green and Blue Spaces to Improve Public Health. Int. J. Environ. Res. Public Health 2020, 17, 4142. [Google Scholar] [CrossRef] [PubMed]
- Markevych, I.; Schoierer, J.; Hartig, T.; Chudnovsky, A.; Hystad, P.; Dzhambov, A.M.; de Vries, S.; Triguero-Mas, M.; Brauer, M.; Nieuwenhuijsen, M.J.; et al. Exploring Pathways Linking Greenspace to Health: Theoretical and Methodological Guidance. Environ. Res. 2017, 158, 301–317. [Google Scholar] [CrossRef] [PubMed]
- Dadvand, P.; de Nazelle, A.; Figueras, F.; Basagaña, X.; Su, J.; Amoly, E.; Jerrett, M.; Vrijheid, M.; Sunyer, J.; Nieuwenhuijsen, M.J. Green Space, Health Inequality and Pregnancy. Environ. Int. 2012, 40, 110–115. [Google Scholar] [CrossRef]
- Fong, K.C.; Hart, J.E.; James, P. A Review of Epidemiologic Studies on Greenness and Health: Updated Literature Through 2017. Curr. Environ. Health Rep. 2018, 5, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Nieuwenhuijsen, M.J.; Khreis, H.; Triguero-Mas, M.; Gascon, M.; Dadvand, P. Fifty Shades of Green: Pathway to Healthy Urban Living. Epidem 2017, 28, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Shanahan, D.F.; Lin, B.B.; Bush, R.; Gaston, K.J.; Dean, J.H.; Barber, E.; Fuller, R.A. Toward Improved Public Health Outcomes from Urban Nature. Am. J. Public Health 2015, 105, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Shanahan, D.F.; Fuller, R.A.; Bush, R.; Lin, B.B.; Gaston, K.J. The Health Benefits of Urban Nature: How Much Do We Need? BioScience 2015, 65, 476–485. [Google Scholar] [CrossRef]
- Wolf, K.L.; Robbins, A.S.T. Metro Nature, Environmental Health, and Economic Value. Environ. Health Perspect. 2015, 123, 390–398. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2018; ISBN 978-92-4-151418-7. [Google Scholar]
- Sallis, J.F.; Cerin, E.; Conway, T.L.; Adams, M.A.; Frank, L.D.; Pratt, M.; Salvo, D.; Schipperijn, J.; Smith, G.; Cain, K.L.; et al. Physical Activity in Relation to Urban Environments in 14 Cities Worldwide: A Cross-Sectional Study. Lancet 2016, 387, 2207–2217. [Google Scholar] [CrossRef]
- Van den Bosch, M. Natural Environments, Health, and Well-Being. Available online: https://oxfordre.com/environmentalscience/view/10.1093/acrefore/9780199389414.001.0001/acrefore-9780199389414-e-333 (accessed on 22 April 2022).
- Lovell, R.; Depledge, M.; Maxwell, S. Health and the Natural Environment: A Review of Evidence, Policy, Practice and Opportunities for the Future; Department for Environment, Food and Rural Affairs: London, UK, 2018. [Google Scholar]
- Evenson, K.R.; Wen, F.; Hillier, A.; Cohen, D.A. Assessing the Contribution of Parks to Physical Activity Using GPS and Accelerometry. Med. Sci. Sport. Exerc. 2013, 45, 1981–1987. [Google Scholar] [CrossRef]
- Lin, W.; Chen, Q.; Jiang, M.; Tao, J.; Liu, Z.; Zhang, X.; Wu, L.; Xu, S.; Kang, Y.; Zeng, Q. Sitting or Walking? Analyzing the Neural Emotional Indicators of Urban Green Space Behavior with Mobile EEG. J. Urban Health 2020, 97, 191–203. [Google Scholar] [CrossRef]
- Hong, A.; Sallis, J.F.; King, A.C.; Conway, T.L.; Saelens, B.; Cain, K.L.; Fox, E.H.; Frank, L.D. Linking Green Space to Neighborhood Social Capital in Older Adults: The Role of Perceived Safety. Soc. Sci. Med. 2018, 207, 38–45. [Google Scholar] [CrossRef]
- Lachowycz, K.; Jones, A.P. Towards a Better Understanding of the Relationship between Greenspace and Health: Development of a Theoretical Framework. Landsc. Urban Plan. 2013, 118, 62–69. [Google Scholar] [CrossRef]
- Tamosiunas, A.; Grazuleviciene, R.; Luksiene, D.; Dedele, A.; Reklaitiene, R.; Baceviciene, M.; Vencloviene, J.; Bernotiene, G.; Radisauskas, R.; Malinauskiene, V.; et al. Accessibility and Use of Urban Green Spaces, and Cardiovascular Health: Findings from a Kaunas Cohort Study. Environ. Health 2014, 13, 20. [Google Scholar] [CrossRef] [PubMed]
- Barton, J.; Hine, R.; Pretty, J. The Health Benefits of Walking in Greenspaces of High Natural and Heritage Value. J. Integr. Environ. Sci. 2009, 6, 261–278. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. BMJ 2009, 7, 889–896. [Google Scholar] [CrossRef]
- Cochrane Handbook for Systematic Reviews of Interventions. Available online: https://training.cochrane.org/handbook (accessed on 9 August 2022).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A Tool for Assessing Risk of Bias in Non-Randomised Studies of Interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Song, C.; Ikei, H.; Igarashi, M.; Takagaki, M.; Miyazaki, Y. Physiological and Psychological Effects of a Walk in Urban Parks in Fall. Int. J. Environ. Res. Public Health 2015, 12, 14216–14228. [Google Scholar] [CrossRef]
- Sales, M.; Polman, R.; Hill, K.D.; Levinger, P. A Novel Exercise Initiative for Seniors to Improve Balance and Physical Function. J. Aging Health 2017, 29, 1424–1443. [Google Scholar] [CrossRef]
- Plotnikoff, R.C.; Wilczynska, M.; Cohen, K.E.; Smith, J.J.; Lubans, D.R. Integrating Smartphone Technology, Social Support and the Outdoor Physical Environment to Improve Fitness among Adults at Risk of, or Diagnosed with, Type 2 Diabetes: Findings from the ‘ECoFit’ Randomized Controlled Trial. Prev. Med. 2017, 105, 404–411. [Google Scholar] [CrossRef]
- Kim, D.-I.; Lee, D.H.; Hong, S.; Jo, S.-W.; Won, Y.-S.; Jeon, J.Y. Six Weeks of Combined Aerobic and Resistance Exercise Using Outdoor Exercise Machines Improves Fitness, Insulin Resistance, and Chemerin in the Korean Elderly: A Pilot Randomized Controlled Trial. Arch. Gerontol. Geriatr. 2018, 75, 59–64. [Google Scholar] [CrossRef]
- Müller-Riemenschneider, F.; Petrunoff, N.; Yao, J.; Ng, A.; Sia, A.; Ramiah, A.; Wong, M.; Han, J.; Tai, B.C.; Uijtdewilligen, L. Effectiveness of Prescribing Physical Activity in Parks to Improve Health and Wellbeing—The Park Prescription Randomized Controlled Trial. Int. J. Behav. Nutr. Phys. Activ. 2020, 17, 42. [Google Scholar] [CrossRef] [PubMed]
- Vert, C.; Gascon, M.; Ranzani, O.; Márquez, S.; Triguero-Mas, M.; Carrasco-Turigas, G.; Arjona, L.; Koch, S.; Llopis, M.; Donaire-Gonzalez, D.; et al. Physical and Mental Health Effects of Repeated Short Walks in a Blue Space Environment: A Randomised Crossover Study. Environ. Res. 2020, 188, 109812. [Google Scholar] [CrossRef] [PubMed]
- Burnet, K.; Kelsch, E.; Zieff, G.; Moore, J.B.; Stoner, L. How Fitting Is F.I.T.T.?: A Perspective on a Transition from the Sole Use of Frequency, Intensity, Time, and Type in Exercise Prescription. Physiol. Behav. 2019, 199, 33–34. [Google Scholar] [CrossRef]
- Brown, D.K.; Barton, J.L.; Pretty, J.; Gladwell, V.F. Walks4Work: Assessing the Role of the Natural Environment in a Workplace Physical Activity Intervention. Scand. J. Work Environ. Health 2014, 40, 390–399. [Google Scholar] [CrossRef] [PubMed]
- Pratt, M.; Macera, C.A.; Wang, G. Higher Direct Medical Costs Associated with Physical Inactivity. Phys. Sportsmed. 2000, 28, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Robertson, M.C.; Campbell, A.J.; Gardner, M.M.; Devlin, N. Preventing Injuries in Older People by Preventing Falls: A Meta-Analysis of Individual-Level Data. J. Am. Ger. Soc. 2002, 50, 905–911. [Google Scholar] [CrossRef]
- Aparicio, E.H.; Rodríguez, E.F.; Marbán, R.M.; Minguet, J.L.C. Análisis de los Circuitos Biosaludables para la Tercera Edad en la provincia de Málaga (España) (Analysis of the Public Geriatric Parks for Elderly People in Málaga (Spain)). Retos 2010, 17, 99–102. [Google Scholar] [CrossRef]
- Scott, A.; Stride, V.; Neville, L.; Hua, M. Design and Promotion of an Outdoor Gym for Older Adults: A Collaborative Project. Health Prom. J. Austr. 2014, 25, 212–214. [Google Scholar] [CrossRef]
- Fujita, K.; Fujiwara, Y.; Chaves, P.H.M.; Motohashi, Y.; Shinkai, S. Frequency of Going Outdoors as a Good Predictors for Incident Disability of Physical Function as Well as Disability Recovery in Community-Dwelling Older Adults in Rural Japan. J. Epidemiol. 2006, 16, 261–270. [Google Scholar] [CrossRef]
- Simpson, M.E.; Serdula, M.; Galuska, D.A.; Gillespie, C.; Donehoo, R.; Macera, C.; Mack, K. Walking Trends among U.S. Adults: The Behavioral Risk Factor Surveillance System, 1987–2000. Am. J. Prev. Med. 2003, 25, 95–100. [Google Scholar] [CrossRef]
- Furber, S.; Pomroy, H.; Grego, S.; Tavener-Smith, K. People’s Experiences of Using Outdoor Gym Equipment in Parks. Health Promot. J. Austr. 2014, 25, 211. [Google Scholar] [CrossRef] [PubMed]
- Greyling, G.A. The Usage of Outdoor Gyms in South Africa. Master’s Thesis, Nelson Mandela Metropolitan University, Gqeberha, South Africa, 2016. [Google Scholar]
- Mora, R. Moving Bodies: Open Gyms and Physical Activity in Santiago. J. Urban Des. 2012, 17, 485–497. [Google Scholar] [CrossRef]
- Chow, H. Outdoor Fitness Equipment in Parks: A Qualitative Study from Older Adults’ Perceptions. BMC Public Health 2013, 13, 1216. [Google Scholar] [CrossRef] [PubMed]
- Veitch, J.; Carver, A.; Abbott, G.; Giles-Corti, B.; Timperio, A.; Salmon, J. How Active Are People in Metropolitan Parks? An Observational Study of Park Visitation in Australia. BMC Public Health 2015, 15, 610. [Google Scholar] [CrossRef] [Green Version]
| Parameter | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | Healthy people Age range: adult (aged ≥ 18 years) | People with acute or chronic conditions People aged under 18 |
| Intervention | Outdoor PA intervention is carried out in the natural environment and natural and mixed settings (specifically green and blue spaces) | Absence of PA intervention; indoor PA intervention |
| Comparator | Standard treatment No PA intervention Another type of PA intervention | |
| Outcome | Physical fitness Quality of life Intervention satisfaction evaluation The physical performance or other indices of physical performance Anthropometric characteristics and anthropometric evaluation | No information about PA effects |
| Timing | 10-year publication date limit English language Full text available | Published before 2011 Not in the English language No full text is available |
| Study design | Experimental or observational study with original primary data | Study protocol or other studies without original data |
| Authors | Study Design | Tool for Assessment | Quality |
|---|---|---|---|
| Song et al., 2015 [32] | Quasi-experimental | ROBINS-I Scale | Moderate concerns |
| Sales et al., 2017 [33] | RCT | RoB2 Tool | Low risk |
| Plotnikoff et al., 2017 [34] | RCT | RoB2 Tool | Some concerns |
| Kim et al., 2018 [35] | RCT | RoB2 Tool | Low risk |
| Muller-Riemenschneider et al., 2020 [36] | RCT | RoB2 Tool | Low risk |
| Vert et al., 2020 [37] | RCT | RoB2 Tool | Some concerns |
| Study | Study Design | Population | Intervention | Outcome | Results |
|---|---|---|---|---|---|
| Song et al. 2015, Japan [32] | NRCT | N: 23 men (aged 22.3 ± 1.2, height 171.1 ± 4.7 cm, weight 63.4 ± 8.1 kg, BMI 21.5 ± 2.1 kg/m2) | Type: 15 min of walking in two different environments—an urban park and a city area; after walking, the subject returned to the waiting room and completed the questionnaires. Participants rested for approximately 20 min and repeated the experiment in the other environment. There were no significant differences in the average speed between the two environments. Frequency: twice a day Time: 3 days | Physiological relaxation, three different questionnaires were used to investigate the psychological responses after walking in each site. The questionnaires were the SD scores, POMS, and STAI score. Heart rate and its variability were measured to investigate automatic nerve activity i. | The participants showed statistically significant differences in their physiological and psychological responses to the walking in different environments. The natural logarithm of the HF component, which is an estimate of the parasympathetic nerve activity, was higher when subjects walked in the urban park than when they walked in the city area. The mean ln(HF) was significantly higher in the urban-park walking than city-area walking (p ≤ 0.01). Then, the estimation of the sympathetic nerve activity was lower during the urban-park walking than city-area walking. The mean heart rate was significantly lower in the urban-park walking than city-area walking (p ≤ 0.01). A significantly higher SD score was observed following the urban-park walking than those following the city-area walking for the three adjectives: comfortable, natural, and relaxed. The negative subscale of tension–anxiety, anger–hostility, fatigue, and confusion was significantly lower after walking in the urban park than walking in the city area (p ≤ 0.05). On the contrary, the positive mood state vigor was significantly higher for walking in the urban park (p ≤ 0.001). The total STAI score was 19.3% significantly lower after walking in the urban park than after walking in the city area (p ≤ 0.01) |
| Sales et al. 2017, Australia [33] | RCT | N: 48 CG: 21 (age 70.2 ± 8.2, 77% women, BMI 28.1 ± 5.0, 6% current smoker, 29% ex-smoker, 52% daily alcohol assumption, 61.9% had previous falls history, 47.6% had falls over 12 months) EG: 27 (age 75.1 ± 7.9, 64% women, BMI 28.9 ± 5.3, 3% current smoker, 42% ex-smoker, 41% daily alcohol assumption, 62.9% had previous falls history, 40.7% had falls over 12 months) | Type: different kinds of outdoor exercises with different exercise stations: push-ups, modified pull-ups, balance stool, sit to stand, ramp + net + climb through, balance beam, steps, step-ups or taps on platform, gangway, calf raises + finger steps, round snake pipe, sharp snake pipe, hip extension, screws and turners, and hip abduction. Exercisers were paired in stations, and an exercise session could include up to eight stations. Frequency: two times a week, approximately 1–15 h, with 5–10 min of warm-up, followed by 45–75 min on the equipment station and 5–10 min of cool-down exercises. Time: 18 weeks of interventions | BOOMER test, to assess the effectiveness of the exercise park to improve balance; handgrip strength, to measure the physical strength; single leg test standing, to measure the static balance; 2 min walk test, to assess physical tolerance, functional mobility; 30 min sit-to-stand test, to evaluate the strength of the knee extender muscle; feasibility, defined as the number of participants recruited and retained over the recruitment period; physical composite scores, shortfalls efficacy scale international, numbers of falls over 12 months | No significant improvement in the BOOMER test (CG, 13.5 ± 1.7 pre, 13.9 ± 1.4 post, p = 0.6 EG 13.6 ± 1.4 pre, 13.7 ± 1.3 post, p = 0.6, p between groups = 0.4) and the improvement in quality of life (CG 49.1 ± 7.91 pre, 48.9 ± 7.6 post, p = 0.2, for the physical component, 51.4 ± 6.1 pre, 51.6 ± 7.9 post, p = 0.6, for the mental component; EG 46.9 ± 7.6 pre, 49.6 ± 8.3 post, p = 0.4, for the physical component, 53.1 ± 9.8 pre, 54.5 ± 7.0 post, p = 0.6, for the mental component) and falls efficacy (CG 11.3 ± 4.0 pre, 10.9 ± 3.7 post, p = 0.4, EG 10.3 ± 3.4 pre, 9.3 ± 2.5, post, p = 0.4, p between groups = 0.1). EG showed significant improvements in knee strength (84.2 ± 36.5 pre, 96.4 ± 44.4 post, p = 0.01), balance (single leg stance, 15.6 ± 11.0 pre, 17.3 ± 11.3 post, p = 0.01), 2 min walk test (140.6 ± 30.5 pre, 152.1 ± 28.7 post, p = 0.01), and sit to stand (10.5 ± 3.0 pre, 12.1 ± 2.7 post, p = 0.01). Regarding feasibility, 87% of EG completed the 18-week intervention with mean attendance to the session of 79.6% and 14% of the CG attended the social meeting offered. |
| Plotnikoff et al. 2017, Australia [34] | RCT | N:84 (aged 44.7 ± 14.0, BMI 33.3 ± 5.7 kg/m2) CG: 42, aged 45.1 ± 14.7, BMI 31.7 ± 5.1 kg/m2, EG: 42, aged 44.2 ± 13.5, BMI 35.0 ± 5.9 kg/m2 | Type: EG—five face-to-face group intervention, each intervention lasted for 90 min and consisted of 30 min of cognitive group and 60 min of small group outdoor training and outdoor PA with the eCoFit smartphone app that included workout circuits, and a description of where and how to use an outdoor physical environment to be more physically active. CG: no interventions Frequency: once a week Time: 20 weeks of interventions; phase 1: 1–10 weeks face-to-face group intervention; phase 2: 11–20 weeks eCoFit smartphone app | Aerobic fitness to assess aerobic fitness; lower body muscular fitness using the chair stand test; steps/day measured using pedometers; functional mobility using the Timed Up and Go test; waist circumferences, BMI, and systolic and diastolic blood pressure | After 10 weeks, EG improved aerobic fitness (4.50 mL/kg/min), the strength of the lower body, numbers of steps (1330 steps), mobility (−1.8 s), and systolic blood pressure, and there was a decrease in waist circumference (−2.8 cm). After 20 weeks, EG showed effects on the upper and lower body strength, blood pressure, and functional mobility. Survey conducted at the end of the intervention showed positive feedback for group cognitive session, outdoor training, and use of the eCoFit app. |
| Kim et al. 2018, South Korea [35] | RCT | N: 35 (aged 73.20 ± 4.90, women characteristics (32): BMI 25.48 ± 2.41, kg/m2 height 151.98 ± 5.90 cm, weight 58.73 ± 8.19 kg, lean mass 19.64 ± 2.50 kg, body fat 36.84 ± 3.36%; men characteristics (3): BMI 24.70 ± 2.87 kg/m2, weight 69.40 ± 8.39 kg, 168.20 ± 4.75 cm, lean mass 27.00 ± 3.72 kg, body fat 28.66 ± 3.95%) RC: 12, CoG: 13 CG: 10 | Type: RC—outdoor resistance training using leg extension, pull weight, chair pull, for a total of 50 min of training; CoG: outdoor aerobic and resistance training using leg extension, pull weight, chair pull, sky-walker, cross-country, for a total of 70 min; CG: no interventions Time: 6 weeks of interventions at different intensity evaluated with the Borg scale | Fitness was evaluated with five fitness tests designed for the elderly (30 s chair stand, 30 s arm curl, 244 cm up and go, one-leg stand, and 2 min step), as well as number of pushups and 6 min walking | Improvement in upper-body strength in both groups (RC 19.16 ± 11.40 pre, 30.16 ± 13.13 post; CoG 11.07 ± 9.62 pre, 22.23 ± 12.95 post); lower-body endurance was higher in the CoG (561.84 ± 67.22 m) than the CG (486.44 ± 96.14 m). |
| MullerRiemnschneider et al. 2020, Singapore [36] | RCT | N: 160 (aged 51.1 ± 6.3, 127 women, total MVPA 442.7 ± 534.7 min/week) EG: 80 (aged 52.1 ± 6.5, 65 women) CG: 80 (aged 50.0 ± 6.0, 62 women) | Type: EG—face-to-face counseling on PA; they completed a park prescription sheet where they committed to a goal that specified the frequency, intensity, time, and location of exercise parks. Participants received two brochures developed for the trial: one provided information on the main parks and their different features, including walking trails and location of fitness corners. The second was generally about the Singapore National Park s Board. + invitation to weekly exercise sessions in parks; in addition, participants received half-way through the trial a brief counseling phone call to assess progress and included modification of the goal if necessary. CG: continued their daily routine; they received standard PA materials. Time: 6-week intervention. | Time spent on MVPA measured by an accelerometer and by questionnaire, total volume of PA, time spent on light and sedentary activity, time spent at the park, physical activity at the park, recreational MVPA, mental well-being (measured by SF-12, K-10, WHO5, and WHOQOL-BREF). | No differences between EG and CG were observed with regard to physiological distress and overall quality of life. The only difference was found for the psychological quality of life, which was higher in EG than in CG (p = 0.047). The difference was not statistically significant regarding the mean differences in MVPA among participants. EG showed a significant increase in the time of recreational PA (EG 142 ± 155.4 min/week, CG 93.6 ± 131.0 min/week, p = 0.044), time spent in parks (EG 333.9 ± 506.2 min/month, CG 186.4 ± 85.4 min/month, p = 0.047), and PA in parks (EG 333.0 ± 499.3 min/month, CG 140.5 ± 270.7 min/month, p = 0.005). |
| Vert et al. 2020, Spain [37] | RCT | N: 49 (aged 29, min 19, max 49, 69.5% women, BMI 22.6 ± 3.5 kg/m2, 88.1% saw blue space at work, 89.9% met the PA of WHO guidelines) | Type: for each study week, each participant was assigned to a different environment (blue, urban, or control site). All participants were exposed to all environments upon completion of the study. They walked 20 min in blue, urban, or control site. Participants were distributed in two turns: the first started at 10.00 a.m. and the second at 11.30 a.m. Frequency: 4 days a week Time: 3 weeks intervention | Participants completed a set of questionnaires (SWB, WHO-5, TMD, 4SDQ, and SF-36) to assesses their well-being, mood, and psychological responses, before and after each walking. In addition, sleep characteristics and general health were assessed. Blood pressure, pulse rate, and heart rate variabilities were continuously measured before and after the walking. | Better well-being and mood responses after walking in a blue space versus an urban space or control site (p ≤ 0.05). For SWB, no significant differences were found. For WHO-5, the “total well-being score” was increased when participants were exposed to blue environment (p ≤ 0.05). TMD was significantly lower for the negative subscales after walking along the blue route compared with urban space and control site (p ≤ 0.05). 4SDQ did not show significant differences between the environments. Statistically significant increase was found in systolic blood pressure and pulse rate in the blue and urban environments compared with the control site. Increase in SNS activity during and after walking in blue and urban spaces. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marini, S.; Mauro, M.; Grigoletto, A.; Toselli, S.; Maietta Latessa, P. The Effect of Physical Activity Interventions Carried Out in Outdoor Natural Blue and Green Spaces on Health Outcomes: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 12482. https://doi.org/10.3390/ijerph191912482
Marini S, Mauro M, Grigoletto A, Toselli S, Maietta Latessa P. The Effect of Physical Activity Interventions Carried Out in Outdoor Natural Blue and Green Spaces on Health Outcomes: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(19):12482. https://doi.org/10.3390/ijerph191912482
Chicago/Turabian StyleMarini, Sofia, Mario Mauro, Alessia Grigoletto, Stefania Toselli, and Pasqualino Maietta Latessa. 2022. "The Effect of Physical Activity Interventions Carried Out in Outdoor Natural Blue and Green Spaces on Health Outcomes: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 19: 12482. https://doi.org/10.3390/ijerph191912482
APA StyleMarini, S., Mauro, M., Grigoletto, A., Toselli, S., & Maietta Latessa, P. (2022). The Effect of Physical Activity Interventions Carried Out in Outdoor Natural Blue and Green Spaces on Health Outcomes: A Systematic Review. International Journal of Environmental Research and Public Health, 19(19), 12482. https://doi.org/10.3390/ijerph191912482










