COVID-19 Mortality in Patients Aged 80 and over Residing in Nursing Homes—Six Pandemic Waves: OCTA-COVID Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Variables
2.3. Statistical Analysis
3. Results
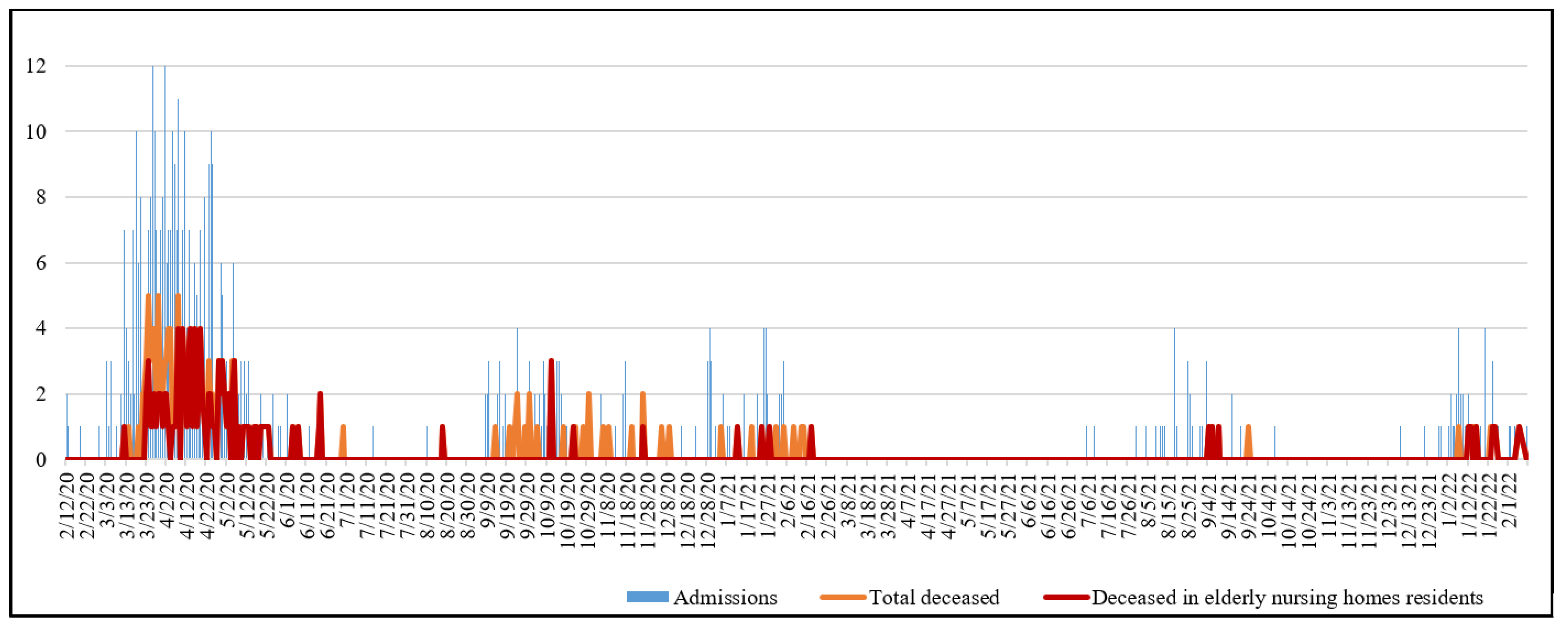
3.1. Descriptive Analysis, Temporal Evolution, and Univariate Analysis
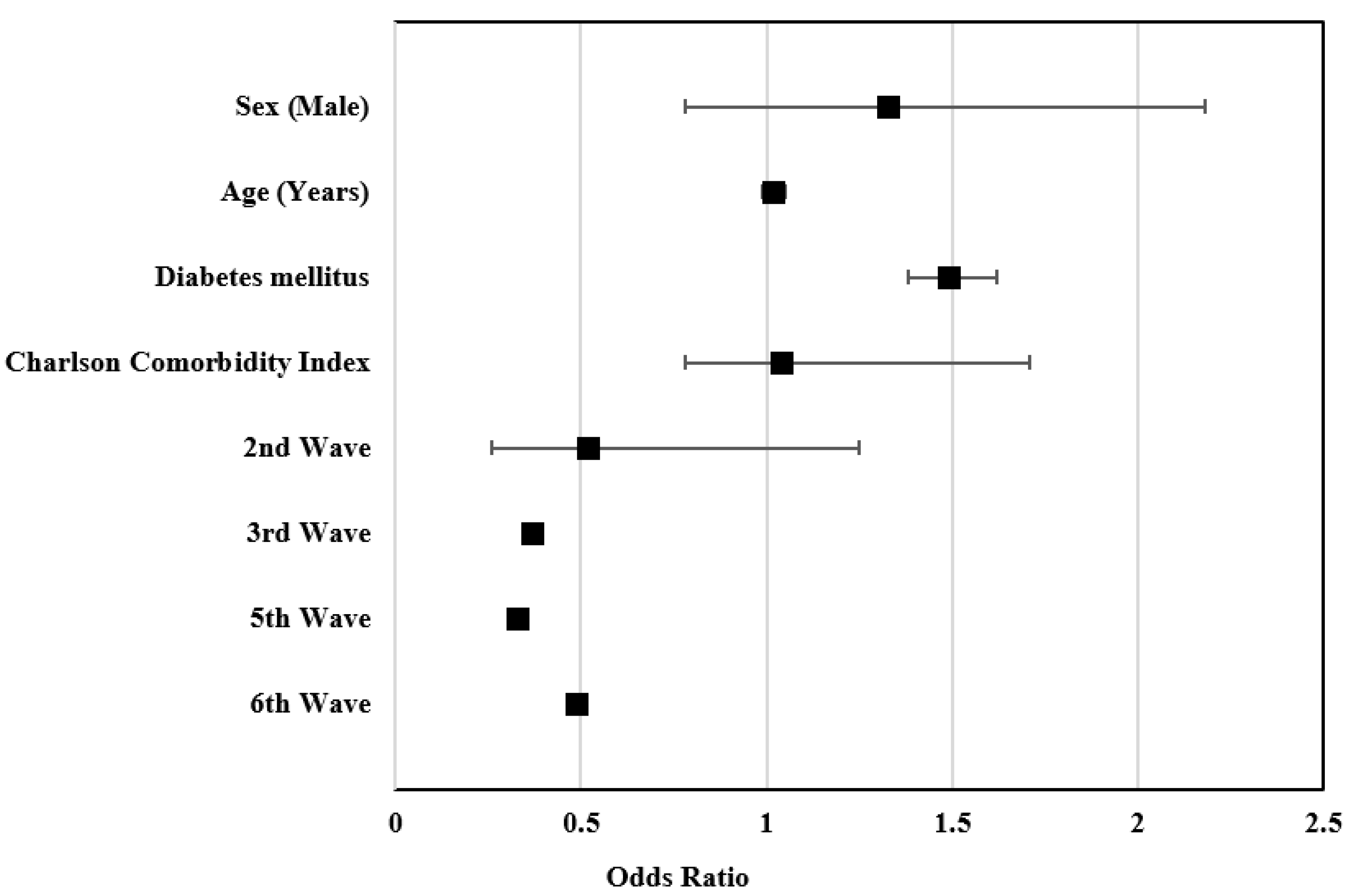
3.2. Multivariate Analysis
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Medeiros Figueiredo, A.; Daponte-Codina, A.; Moreira Marculino Figueiredo, D.C.; Toledo Vianna, R.P.; Costa de Lima, K.; Gil-García, E. Factors associated with the incidence and mortality from COVID-19 in the autonomous communities of Spain. Gac. Sanit. 2021, 35, 445–452. [Google Scholar] [CrossRef] [PubMed]
- CNM (ISCIII); CNE; RENAVE. Equipo COVID-19 Informe No 33. Análisis de Los Casos de COVID-19 Hasta El 10 de Mayo En España. Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/Informe%20n%C2%BA%2033.%20An%C3%A1lisis%20de%20los%20casos%20de%20COVID-19%20hasta%20el%2010%20de%20mayo%20en%20Espa%C3%B1a%20a%2029%20de%20mayo%20de%202020.pdf (accessed on 3 June 2022).
- Comunidad de Madrid Informe Epidemiológico Diario de Madrid. Situación 29 de Mayo 2020. Available online: https://www.comunidad.madrid/sites/default/files/doc/sanidad/200529_cam_covid19.pdf (accessed on 3 June 2022).
- Liu, K.; Chen, Y.; Lin, R.; Han, K. Clinical Features of COVID-19 in Elderly Patients: A Comparison with Young and Middle-Aged Patients. J. Infect. 2020, 80, e14–e18. [Google Scholar] [CrossRef]
- Zhao, H.-L.; Huang, Y.-M.; Huang, Y. Mortality in Older Patients with COVID-19. J. Am. Geriatr. Soc. 2020, 68, 1685–1687. [Google Scholar] [CrossRef]
- Bonanad, C.; García-Blas, S.; Tarazona-Santabalbina, F.; Sanchis, J.; Bertomeu-Gonzalez, V.; Fácila, L.; Ariza, A.; Núñez, J.; Cordero, A. The Effect of Age on Mortality in Patients With COVID-19: A Meta-Analysis With 611,583 Subjects. J. Am. Med. Dir. Assoc. 2020, 21, 915–918. [Google Scholar] [CrossRef] [PubMed]
- Borobia, A.M.; Carcas, A.J.; Arnalich, F.; Álvarez-Sala, R.; Monserrat-Villatoro, J.; Quintana, M.; Figueira, J.C.; Torres Santos-Olmo, R.M.; García-Rodríguez, J.; Martín-Vega, A.; et al. A Cohort of Patients with COVID-19 in a Major Teaching Hospital in Europe. J. Clin. Med. 2020, 9, 1733. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad; Centro de Coordinación de Alertas y Emergencias Sanitarias. Emergencias Sanitarias Enfermedad Por Coronavirus, COVID-19 Información Científica-Técnica. Available online: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/ITCoronavirus.pdf (accessed on 3 June 2022).
- Comas-Herrera, A.; Zalakain, J.; Litwin, C.; Hsu, A.T.; Lane, N.; Fernandez, J.-L. Mortality Associated with COVID-19 Outbreaks in Care Homes: Early International Evidence International Long-Term Care Policy Network (CPEC-LSE, 2020). Available online: https://www.euskadi.eus/sociosanitario//contenidos/documentacion/doc_sosa_mortality_long_term_c/es_def/index.shtml (accessed on 3 June 2022).
- Colino, R.M. Evolución de la COVID-19 en las residencias de personas mayores desde la segunda ola hasta la vacunación. Descripción de un programa de coordinación entre atención primaria, geriatría y salud pública. Rev. Española De Salud Pública 2021, 95, e1–e11. [Google Scholar]
- Ministerio de Sanidad; Centro de Coordinación de Alertas y Emergencias Sanitaria. Actualización No 599. Enfermedad Por El Coronavirus (COVID-19). Available online: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Actualizacion_599_COVID-19.pdf (accessed on 3 June 2022).
- Centro Nacional de Epidemiologia; Red Nacional de Vigilancia Epidemiológica. Informe No129 Situación de COVID-19 En España a 18 de Mayo de 2022. Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/INFORMES%20COVID-19%202022/Informe%20n%c2%ba129%20Situaci%c3%b3n%20de%20COVID-19%20en%20Espa%c3%b1a%20a%2018%20de%20mayo%20de%202022.pdf (accessed on 18 June 2022).
- Henry, D.A.; Jones, M.A.; Stehlik, P.; Glasziou, P.P. Effectiveness of COVID-19 Vaccines: Findings from Real World Studies. Med. J. Aust. 2021, 215, 149–151.e1. [Google Scholar] [CrossRef]
- Antonio, N.; Rita, P.; Saraiva, P. Effectiveness of COVID-19 Vaccines: Evidence from the First-Year Rollout of Vaccination Programs. Vaccines 2022, 10, 409. [Google Scholar] [CrossRef]
- Català, M.; Li, X.; Prats, C.; Prieto-Alhambra, D. The Impact of Prioritisation and Dosing Intervals on the Effects of COVID-19 Vaccination in Europe: An Agent-Based Cohort Model. Sci. Rep. 2021, 11, 18812. [Google Scholar] [CrossRef]
- Ministerio de Sanidad; Centro de Coordinación de Alertas y Emergencias Sanitaria. Información Sobre La Inmunidad Frente a COVID-19. Available online: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/20211015_INMUNIDAD_y_VACUNAS.pdf (accessed on 3 June 2022).
- Monge, S.; Olmedo, C.; Alejos, B.; Lapeña, M.F.; Sierra, M.J.; Limia, A. Direct and Indirect Effectiveness of MRNA Vaccination against Severe Acute Respiratory Syndrome Coronavirus 2 in Long-Term Care Facilities, Spain. Emerg. Infect. Dis. 2021, 27, 2595–2603. [Google Scholar] [CrossRef]
- New COVID-19 Variant Detected in South Africa-NICD. Available online: https://www.nicd.ac.za/new-covid-19-variant-detected-in-south-africa/ (accessed on 3 June 2022).
- Instituto Nacional de Estadística (INE). Estimación del Número de Defunciones Semanales (EDeS) Durante el Brote de COVID-19. Available online: https://www.ine.es/experimental/defunciones/experimental_defunciones.htm#tablas_resultados (accessed on 3 June 2022).
- Centro Nacional de Epidemiologia; Red Nacional de Vigilancia Epidemiológica. Informe No 112 Situación de COVID-19 En España a 5 de Enero de 2022. Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/INFORMES%20COVID-19%202022/Informe%20n%C2%BA%20112%20Situaci%C3%B3n%20de%20COVID-19%20en%20Espa%C3%B1a%20a%205%20de%20enero%20de%202022.pdf (accessed on 3 June 2022).
- Ministerio de Sanidad ECIE-Maps-CIE-10-ES Diagnósticos. Available online: https://eciemaps.mscbs.gob.es/ecieMaps/browser/index_10_mc_old.html (accessed on 2 January 2020).
- Consejería de Sanidad Memoria Año 2019 Del Hospital Central de La Cruz Roja San José y Santa Adela. Available online: https://www.comunidad.madrid/sites/default/files/doc/sanidad/memo/hosp-memoria2019_h_cruz_roja-ok.pdf (accessed on 3 June 2022).
- Golubev, A.G. COVID-19: A Challenge to Physiology of Aging. Front. Physiol. 2020, 11, 584248. [Google Scholar] [CrossRef] [PubMed]
- Berenguer, J.; Ryan, P.; Rodríguez-Baño, J.; Jarrín, I.; Carratalà, J.; Pachón, J.; Yllescas, M.; Arriba, J.R.; Aznar Muñoz, E.; Gil Divasson, P.; et al. Characteristics and Predictors of Death among 4035 Consecutively Hospitalized Patients with COVID-19 in Spain. Clin. Microbiol. Infect. 2020, 26, 1525–1536. [Google Scholar] [CrossRef] [PubMed]
- Bielza, R.; Sanz, J.; Zambrana, F.; Arias, E.; Malmierca, E.; Portillo, L.; Thuissard, I.J.; Lung, A.; Neira, M.; Moral, M.; et al. Clinical Characteristics, Frailty, and Mortality of Residents With COVID-19 in Nursing Homes of a Region of Madrid. J. Am. Med. Dir. Assoc. 2021, 22, 245–252.e2. [Google Scholar] [CrossRef]
- Hewitt, J.; Carter, B.; Vilches-Moraga, A.; Quinn, T.J.; Braude, P.; Verduri, A.; Pearce, L.; Stechman, M.; Short, R.; Price, A.; et al. The Effect of Frailty on Survival in Patients with COVID-19 (COPE): A Multicentre, European, Observational Cohort Study. Lancet Public Health 2020, 5, e444–e451. [Google Scholar] [CrossRef]
- Casas-Rojo, J.M.; Antón-Santos, J.M.; Millán-Núñez-Cortés, J.; Lumbreras-Bermejo, C.; Ramos-Rincón, J.M.; Roy-Vallejo, E.; Artero-Mora, A.; Arnalich-Fernández, F.; García-Bruñén, J.M.; Vargas-Núñez, J.A.; et al. Clinical Characteristics of Patients Hospitalized with COVID-19 in Spain: Results from the SEMI-COVID-19 Registry. Rev. Clin. Esp. 2020, 220, 480–494. [Google Scholar] [CrossRef] [PubMed]
- Jiménez, E.; Fontán-Vela, M.; Valencia, J.; Fernández-Jiménez, I.; Álvaro-Alonso, E.; Izquierdo-García, E.; Cebas, A.L.; Ruiz-Elvira, E.G.; Troya, J.; Tebar-Martínez, A.J.; et al. Characteristics, Complications and Outcomes among 1549 Patients Hospitalised with COVID-19 in a Secondary Hospital in Madrid, Spain: A Retrospective Case Series Study. BMJ Open 2020, 10, e042398. [Google Scholar] [CrossRef]
- Onder, G.; Rezza, G.; Brusaferro, S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA 2020, 323, 1775–1776. [Google Scholar] [CrossRef] [PubMed]
- Docherty, A.B.; Harrison, E.M.; Green, C.A.; Hardwick, H.E.; Pius, R.; Norman, L.; Holden, K.A.; Read, J.M.; Dondelinger, F.; Carson, G.; et al. Features of 20 133 UK Patients in Hospital with COVID-19 Using the ISARIC WHO Clinical Characterisation Protocol: Prospective Observational Cohort Study. BMJ 2020, 369, m1985. [Google Scholar] [CrossRef]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; the Northwell COVID-19 Research Consortium; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef]
- Guan, W.-J.; Ni, Z.-Y.; Hu, Y.; Liang, W.-H.; Ou, C.-Q.; He, J.-X.; Liu, L.; Shan, H.; Lei, C.-L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Shahid, Z.; Kalayanamitra, R.; McClafferty, B.; Kepko, D.; Ramgobin, D.; Patel, R.; Aggarwal, C.S.; Vunnam, R.; Sahu, N.; Bhatt, D.; et al. COVID-19 and Older Adults: What We Know. J. Am. Geriatr. Soc. 2020, 68, 926–929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lippi, G.; Mattiuzzi, C.; Sanchis-Gomar, F.; Henry, B.M. Clinical and Demographic Characteristics of Patients Dying from COVID-19 in Italy vs China. J. Med. Virol. 2020, 92, 1759–1760. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Peromingo, J.; Serra-Rexach, J.A. Long-Term Care Facilities and the COVID-19 Pandemic: Lessons Learned in Madrid. J. Am. Geriatr. Soc. 2020, 68, 1920–1922. [Google Scholar] [CrossRef] [PubMed]
- Bernabeu-Wittel, M.; Gómez-Huelgas, R.; Nieto-Martín, D. SEMI-COVID-19 Network COMMENTSTime to Stop the Tragedy in Spanish Nursing Homes During the COVID-19 Pandemic. J. Am. Geriatr. Soc. 2021, 69, 320–322. [Google Scholar] [CrossRef]
- Geriatric Medicine Research Collaborative; COVID Collaborative; Welch, C. Age and Frailty Are Independently Associated with Increased COVID-19 Mortality and Increased Care Needs in Survivors: Results of an International Multi-Centre Study. Age Ageing 2021, 50, 617–630. [Google Scholar] [CrossRef]
- Lozano-Montoya, I.; Quezada-Feijoo, M.; Jaramillo-Hidalgo, J.; Garmendia-Prieto, B.; Lisette-Carrillo, P.; Gómez-Pavón, F.J. Mortality Risk Factors in a Spanish Cohort of Oldest-Old Patients Hospitalized with COVID-19 in an Acute Geriatric Unit: The OCTA-COVID Study. Eur. Geriatr. Med. 2021, 12, 1169–1180. [Google Scholar] [CrossRef]
- Coll Benejam, T.; Palacio Lapuente, J.; Añel Rodríguez, R.; Gens Barbera, M.; Jurado Balbuena, J.J.; Perelló Bratescu, A. Organización de La Atención Primaria En Tiempos de Pandemia. Aten. Primaria 2021, 53, 102209. [Google Scholar] [CrossRef]
- San Román, J.; Candel, F.J.; Sanz, J.C.; López, P.; Menéndez-Colino, R.; Barreiro, P.; Carretero, M.D.M.; Pérez-Abeledo, M.; Viñuela-Prieto, J.M.; Ramos, B.; et al. Humoral and Cellular Response after MRNA Vaccination in Nursing Homes: Influence of Age and of History of COVID-19. Vaccines 2022, 10, 383. [Google Scholar] [CrossRef]
- Candel, F.J.; Barreiro, P.; San Román, J.; Carretero, M.M.; Sanz, J.C.; Perez-Abeledo, M.; Ramos, B.; Viñuela-Prieto, J.M.; Canora, J.; Martínez-Peromingo, F.J.; et al. The Demography and Characteristic of SARS-CoV-2 Sero-Positive Residents and Staff of Nursing Homes for Older Adults in the Community of Madrid: The SeroSOS Study. Age Ageing 2021, 50, 1038–1047. [Google Scholar] [CrossRef]
- Consejo Interterritorial; Sistema Nacional de Salud. Estrategia de Vacunación Frente a COVID-19 En España. Actualización 8. Available online: https://www.sanidad.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/covid19/Actualizaciones_Estrategia_Vacunacion/docs/COVID-19_Actualizacion8_EstrategiaVacunacion.pdf (accessed on 3 June 2022).
- Abdullah, F.; Myers, J.; Basu, D.; Tintinger, G.; Ueckermann, V.; Mathebula, M.; Ramlall, R.; Spoor, S.; de Villiers, T.; Van der Walt, Z.; et al. Decreased Severity of Disease during the First Global Omicron Variant COVID-19 Outbreak in a Large Hospital in Tshwane, South Africa. Int. J. Infect. Dis. 2022, 116, 38–42. [Google Scholar] [CrossRef]
- Maslo, C.; Friedland, R.; Toubkin, M.; Laubscher, A.; Akaloo, T.; Kama, B. Characteristics and Outcomes of Hospitalized Patients in South Africa During the COVID-19 Omicron Wave Compared With Previous Waves. JAMA 2022, 327, 583–584. [Google Scholar] [CrossRef] [PubMed]
- Monge, S.; Rojas-Benedicto, A.; Olmedo, C.; Mazagatos, C.; Sierra, M.J.; Limia, A.; Martín-Merino, E.; Larrauri, A.; Hernán, M.A.; Moreno, D.; et al. Effectiveness of MRNA Vaccine Boosters against Infection with the SARS-CoV-2 Omicron (B.1.1.529) Variant in Spain: A Nationwide Cohort Study. Lancet Infect. Dis. 2022, 22, 1313–1320. [Google Scholar] [CrossRef]
- Orlando, V.; Coscioni, E.; Guarino, I.; Mucherino, S.; Perrella, A.; Trama, U.; Limongelli, G.; Menditto, E. Drug-Utilisation Profiles and COVID-19. Sci. Rep. 2021, 11, 8913. [Google Scholar] [CrossRef] [PubMed]
- Spini, A.; Crescioli, G.; Donnini, S.; Ziche, M.; Collini, F.; Gemmi, F.; Virgili, G.; Vannacci, A.; Lucenteforte, E.; Gini, R.; et al. Sex Differences in the Utilization of Drugs for COVID-19 Treatment among Elderly Residents in a Sample of Italian Nursing Homes. Pharmacoepidemiol. Drug Saf. 2022, 31, 489–494. [Google Scholar] [CrossRef] [PubMed]
| Living at Home | Nursing Home | Total | p-Value | ||
|---|---|---|---|---|---|
| Factor, n (%) | (n = 210) | (n = 336) | (n = 546) | ||
| Sex | Female | 118 (33.2) | 237 (66.8) | 355 (65) | 0.001 |
| Male | 92 (48.2) | 99 (51.8) | 191 (35) | 0.001 | |
| Mean Age (±SD); Years | 88.2 (±4.6) | 90.3 (±5.1) | 89.5 (±5) | 0.000 | |
| Age Group | 80–89 years old | 130 (47.3) | 145 (52.7) | 275 (50.4) | 0.000 |
| ≥90 years old | 80 (29.5) | 191 (70.5) | 271 (49.6) | 0.000 | |
| COVID-19 Diagnosis | Confirmed | 178 (42.3) | 243 (57.7) | 421 (77.1) | 0.001 |
| Probable | 32 (25.6) | 93 (74.4) | 125 (22.9) | 0.001 | |
| Risk Factors | Chronic respiratory disease | 33 (45.8) | 39 (54.2) | 72 (13.2) | 0.168 |
| Diabetes mellitus | 61 (39.1) | 95 (60.9) | 156 (28.6) | 0.846 | |
| Arterial hypertension | 93 (37.3) | 156 (62.7) | 249 (45.6) | 0.625 | |
| Cerebrovascular disease | 126 (41.9) | 175 (58.1) | 301 (55.1) | 0.070 | |
| Chronic renal insufficiency | 46 (38) | 75 (62) | 121 (22.2) | 0.909 | |
| Chronic hepatic disease | 2 (66.7) | 1 (33.3) | 3 (0.5) | 0.314 | |
| Neurological disorders | 24 (26.7) | 66 (73.3) | 90 (16.5) | 0.012 | |
| Neoplastic disease | 29 (38.2) | 47 (61.8) | 76 (13.9) | 0.953 | |
| Dementia | 39 (25.5) | 114 (74.5) | 153 (28) | 0.000 | |
| Neurological sequelae | 27 (65.9) | 14 (34.1) | 41 (7.5) | 0.000 | |
| Charlson Comorbidity Index; Mean (±SD) | 6.8 (±2) | 7.2 (±1.8) | 7.1 (±1.9) | 0.021 | |
| Charlson Index | 4 points | 24 (68.6) | 11 (31.4) | 35 (6.4) | 0.020 |
| 5 points | 36 (40.9) | 52 (59.1) | 88 (16.1) | 0.020 | |
| 6 points | 35 (33.7) | 69 (66.3) | 104 (19) | 0.020 | |
| 7 points | 47 (39.2) | 73 (60.8) | 120 (22) | 0.020 | |
| ≥8 points | 68 (34.2) | 131 (65.8) | 199 (36.4) | 0.020 | |
| Length of Hospital Stay; Mean (±SD); Days | 17.6 (±15.1) | 13.3 (±10.2) | 14.9 (±12.5) | 0.000 | |
| Lethality | 70 (33.3) | 117 (34.8) | 187 (34.2) | 0.721 | |
| 1st Wave | 2nd Wave | 3rd Wave | 5th Wave | 6th Wave | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Living at Home | Nursing Home | Living at Home | Nursing Home | Living at Home | Nursing Home | Living at Home | Nursing Home | Living at Home | Nursing Home | ||
| Factor, n (%) | (n = 121) | (n = 249) | (n = 38) | (n = 24) | (n = 26) | (n = 20) | (n = 12) | (n = 17) | (n = 13) | (n = 26) | |
| Sex | Female | 72 (29.6) | 171 (70.4) | 20 (51.3) | 19 (48.7) * | 11 (44) | 14 (56) | 7 (36.8) | 12 (63.2) | 8 (27.6) | 21 (72.4) |
| Male | 49 (38.6) | 78 (61.4) | 18 (78.3) | 5 (21.7) * | 15 (71.4) | 6 (28.6) | 5 (50) | 5 (50) | 5 (50) | 5 (50) | |
| Mean Age (±SD); Years | 88.1 (±4.6) | 90.1 (±5.1) * | 87.9 (±5) | 92.7 (±4.9) * | 88.8 (±3.9) | 89.9 (±4.5) | 88.3 (±5) | 90 (±5.2) | 88.2 (±4.3) | 89.8 (±5.2) | |
| Age Group | 80–89 years old | 77 (41.2) | 110 (58.8) * | 23 (82.1) | 5 (17.9) * | 15 (65.2) | 8 (34.8) | 8 (50) | 8 (50) | 7 (33.3) | 14 (66.7) |
| ≥90 years old | 44 (24) | 139 (76) * | 15 (44.1) | 19 (55.9) * | 11 (47.8) | 12 (52.2) | 4 (30.8) | 9 (69.2) | 6 (33.3) | 12 (66.7) | |
| Risk Factors | Chronic respiratory disease | 18 (40) | 27 (60) | 6 (75) | 2 (25) | 5 (83.3) | 1 (16.7) | 1 (25) | 3 (75) | 3 (33.3) | 6 (66.7) |
| Diabetes mellitus | 32 (30.8) | 72 (69.2) | 16 (72.7) | 6 (27.3) | 5 (41.7) | 7 (58.3) | 5 (55.6) | 4 (44.4) | 3 (33.3) | 6 (66.7) | |
| Arterial hypertension | 48 (31.4) | 105 (68.6) | 20 (58.8) | 14 (41.2) | 7 (43.8) | 9 (56.3) | 5 (41.7) | 7 (58.3) | 13 (38.2) | 21 (61.8) | |
| Neurological disorders | 15 (23.1) | 50 (76.9) | 4 (66.7) | 2 (33.3) | 3 (30) | 7 (70) | 1 (25) | 3 (75) | 1 (20) | 4 (80) | |
| Dementia | 26 (25) | 78 (75) * | 4 (44.4) | 5 (55.6) | 5 (35.7) | 9 (64.3) | 2 (40) | 3 (60) | 2 (9.5) | 19 (90.5) * | |
| Charlson Comorbidity Index; Mean (±SD) | 6.6 (±1.9) | 7.2 (±1.8) * | 7.2 (±2.1) | 6.8 (±1.7) | 7.2 (±2.1) | 7.3 (±2.1) | 6.9 (±1.5) | 7.3 (±1.5) | 6.5 (±1.3) | 7.1 (±1.8) | |
| Length of Hospital Stay; Mean (±SD); Days | 16.4 (±14.8) | 12.8 (±10) * | 17 (±13) | 13.7 (±10.1) | 20.2 (±14.2) | 16.5 (±9.4) | 25 (±25.6) | 18.2 (±14.5) | 18.6 (±11.5) | 11.6 (±9.4) * | |
| Lethality | 38 (31.4) | 98 (39.4) | 20 (52.6) | 6 (25) * | 7 (26.9) | 4 (20) | 2 (16.7) | 3 (17.6) | 3 (23.1) | 6 (23.1) | |
| Factor, n (%) | Survivors | Deceased | Total | p-Value | |
|---|---|---|---|---|---|
| (n = 359) | (n = 187) | (n = 546) | |||
| Sex | Female | 248 (69.9) | 107 (30.1) | 355 (65) | 0.006 |
| Male | 111 (58.1) | 80 (41.9) | 191 (35) | 0.006 | |
| Mean Age (±SD); Years | 89.1 (±5) | 90.2 (±4.9) | 89.5 (±5) | 0.012 | |
| Age Group | 80–89 years old | 189 (68.7) | 86 (31.3) | 275 (50.4) | 0.331 |
| ≥90 years old | 170 (62.7) | 101 (37.3) | 271 (49.6) | 0.331 | |
| Living Arrangement | Living at home | 140 (66.7) | 70 (33.3) | 210 (38.5) | 0.721 |
| Nursing home | 219 (65.2) | 117 (34.8) | 336 (61.5) | 0.721 | |
| COVID-19 Diagnosis | Confirmed | 279 (66.3) | 142 (33.7) | 421 (77.1) | 0.639 |
| Probable | 80 (64) | 45 (36) | 125 (22.9) | 0.639 | |
| Pandemic Waves | 1st wave | 234 (63.2) | 136 (36.8) | 370 (67.8) | 0.030 |
| 2nd wave | 36 (58.1) | 26 (41.9) | 62 (11.4) | 0.030 | |
| 3rd wave | 35 (76.1) | 11 (23.9) | 46 (8.4) | 0.030 | |
| 5th wave | 24 (82.8) | 5 (17.2) | 29 (5.3) | 0.030 | |
| 6th wave | 30 (76.9) | 9 (23.1) | 39 (7.1) | 0.030 | |
| Risk Factors | Chronic respiratory disease | 44 (61.1) | 28 (38.9) | 72 (13.2) | 0.373 |
| Diabetes mellitus | 90 (57.7) | 66 (42.3) | 156 (28.6) | 0.012 | |
| Arterial hypertension | 170 (68.3) | 79 (31.7) | 249 (45.6) | 0.255 | |
| Cerebrovascular disease | 188 (62.5) | 113 (37.5) | 301 (55.1) | 0.072 | |
| Chronic renal insufficiency | 71 (58.7) | 50 (41.3) | 121 (22.2) | 0.063 | |
| Chronic hepatic disease | 2 (66.7) | 1 (33.3) | 3 (0.5) | 0.973 | |
| Neurological disorders | 57 (63.3) | 33 (36.7) | 90 (16.5) | 0.597 | |
| Neoplastic disease | 45 (59.2) | 31 (40.8) | 76 (13.9) | 0.195 | |
| Dementia | 105 (68.6) | 48 (31.4) | 153 (28) | 0.377 | |
| Neurological sequelae | 24 (58.5) | 17 (41.5) | 41 (7.5) | 0.311 | |
| Charlson Comorbidity Index; Mean (±SD) | 6.8 (±1.8) | 7.5 (±1.8) | 7.1 (±1.9) | 0.000 | |
| Charlson Index | 4 points | 29 (82.9) | 6 (17.1) | 35 (6.4) | 0.008 |
| 5 points | 69 (78.4) | 19 (21.6) | 88 (16.1) | 0.008 | |
| 6 points | 66 (63.5) | 38 (36.5) | 104 (19) | 0.008 | |
| 7 points | 78 (65) | 42 (35) | 120 (22) | 0.008 | |
| ≥8 points | 117 (58.8) | 82 (41.2) | 199 (36.4) | 0.008 | |
| Length of hospital stay; Mean (±SD); Days | 16.8 (±12.6) | 11.3 (±11.5) | 14.9 (±12.5) | 0.000 | |
| Variables | OR (CI 95%) | p-Value | Adjusted OR(CI 95%) | p-Value |
|---|---|---|---|---|
| Sex (Male) | 1.67 (1.16–2.41) | 0.006 | 1.72 (1.17–2.52) | 0.006 |
| Age (Years) | 1.05 (1.01–1.08) | 0.012 | 1.04 (1.00–1.08) | 0.036 |
| Living Arrangement (Nursing Home) | 1.07 (0.74–1.54) | 0.721 | 1.00 (0.67–1.49) | 0.990 |
| Diabetes Mellitus | 1.63 (1.11–2.39) | 0.012 | 1.42 (0.92–2.18) | 0.115 |
| Charlson Comorbidity Index | 1.20 (1.09–1.32) | 0.000 | 1.14 (1.02–1.27) | 0.019 |
| 2nd Wave | 1.24 (0.72–2.15) | 0.436 | 1.19 (0.67–2.12) | 0.551 |
| 3rd Wave | 0.54 (0.27–1.10) | 0.090 | 0.49 (0.23–1.02) | 0.055 |
| 5th Wave | 0.36 (0.13–0.96) | 0.041 | 0.34 (0.13–0.93) | 0.036 |
| 6th Wave | 0.52 (0.24–1.12) | 0.094 | 0.55 (0.25–1.22) | 0.141 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruiz-Huerta, C.; Canto, M.V.; Ruiz, C.; González, I.; Lozano-Montoya, I.; Quezada-Feijoo, M.; Gómez-Pavón, F.J. COVID-19 Mortality in Patients Aged 80 and over Residing in Nursing Homes—Six Pandemic Waves: OCTA-COVID Study. Int. J. Environ. Res. Public Health 2022, 19, 12019. https://doi.org/10.3390/ijerph191912019
Ruiz-Huerta C, Canto MV, Ruiz C, González I, Lozano-Montoya I, Quezada-Feijoo M, Gómez-Pavón FJ. COVID-19 Mortality in Patients Aged 80 and over Residing in Nursing Homes—Six Pandemic Waves: OCTA-COVID Study. International Journal of Environmental Research and Public Health. 2022; 19(19):12019. https://doi.org/10.3390/ijerph191912019
Chicago/Turabian StyleRuiz-Huerta, Claudia, Marcelle V. Canto, Carmen Ruiz, Ildefonso González, Isabel Lozano-Montoya, Maribel Quezada-Feijoo, and Francisco J. Gómez-Pavón. 2022. "COVID-19 Mortality in Patients Aged 80 and over Residing in Nursing Homes—Six Pandemic Waves: OCTA-COVID Study" International Journal of Environmental Research and Public Health 19, no. 19: 12019. https://doi.org/10.3390/ijerph191912019
APA StyleRuiz-Huerta, C., Canto, M. V., Ruiz, C., González, I., Lozano-Montoya, I., Quezada-Feijoo, M., & Gómez-Pavón, F. J. (2022). COVID-19 Mortality in Patients Aged 80 and over Residing in Nursing Homes—Six Pandemic Waves: OCTA-COVID Study. International Journal of Environmental Research and Public Health, 19(19), 12019. https://doi.org/10.3390/ijerph191912019







