The Effect of Household Technology on Child Health: Evidence from China’s “Home Appliances Going to the Countryside” Policy
Abstract
:1. Introduction
2. Background
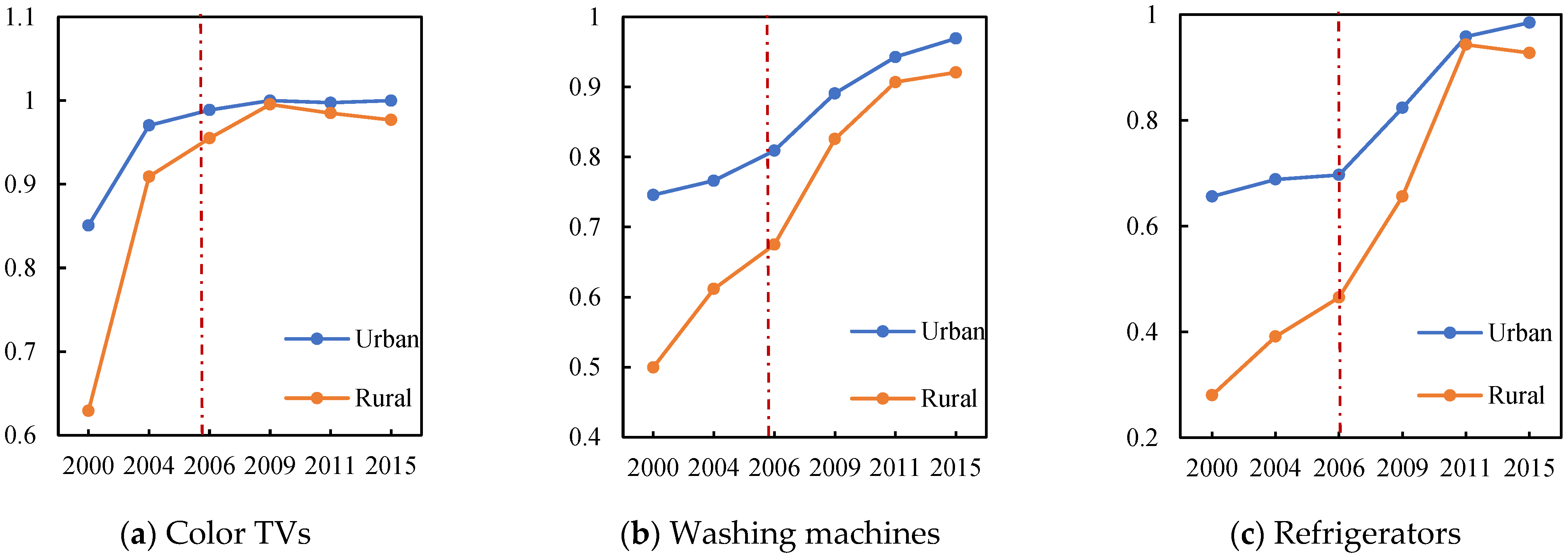
2.1. China’s “Home Appliances Going to the Countryside” Policy
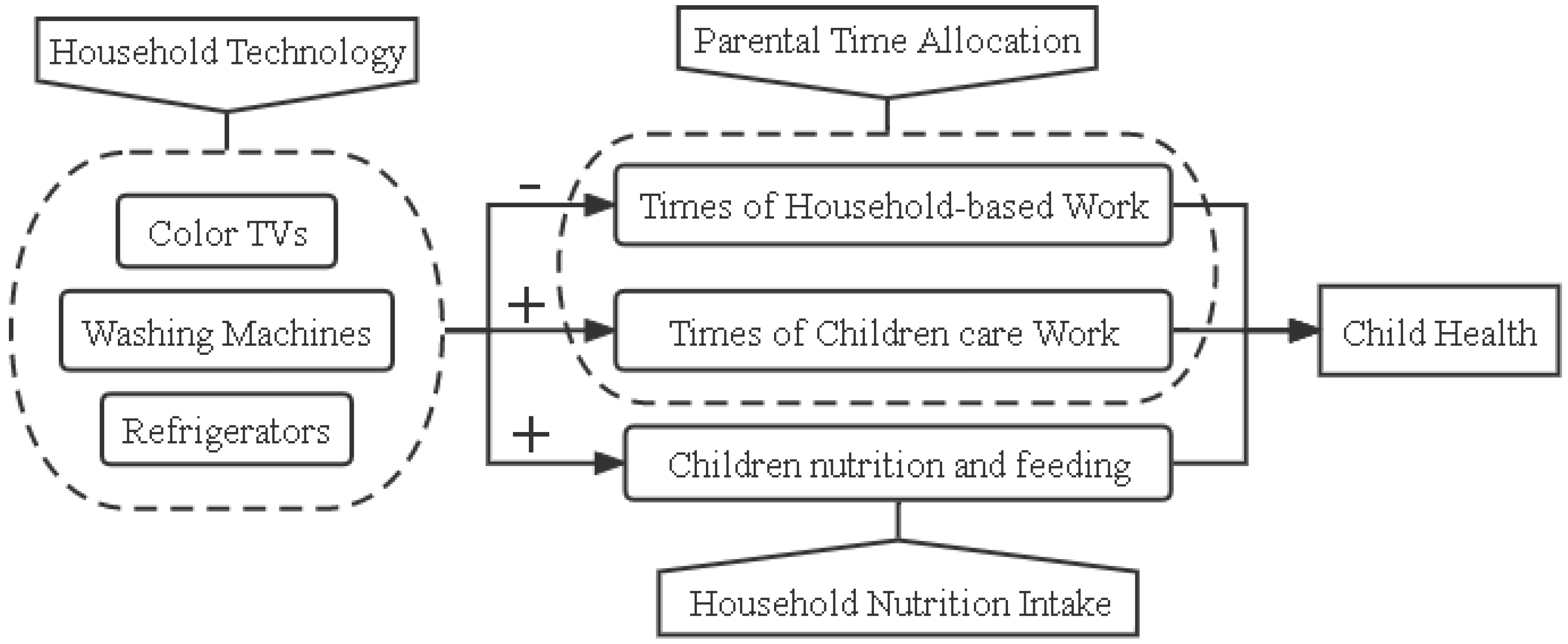
2.2. Conceptual Framework
3. Data, Variables, and Method
3.1. Data
3.2. Variables
3.2.1. Dependent Variables
3.2.2. Independent Variables
3.2.3. Control Variables
3.3. Estimation Strategy: Difference-in-Differences
4. Results
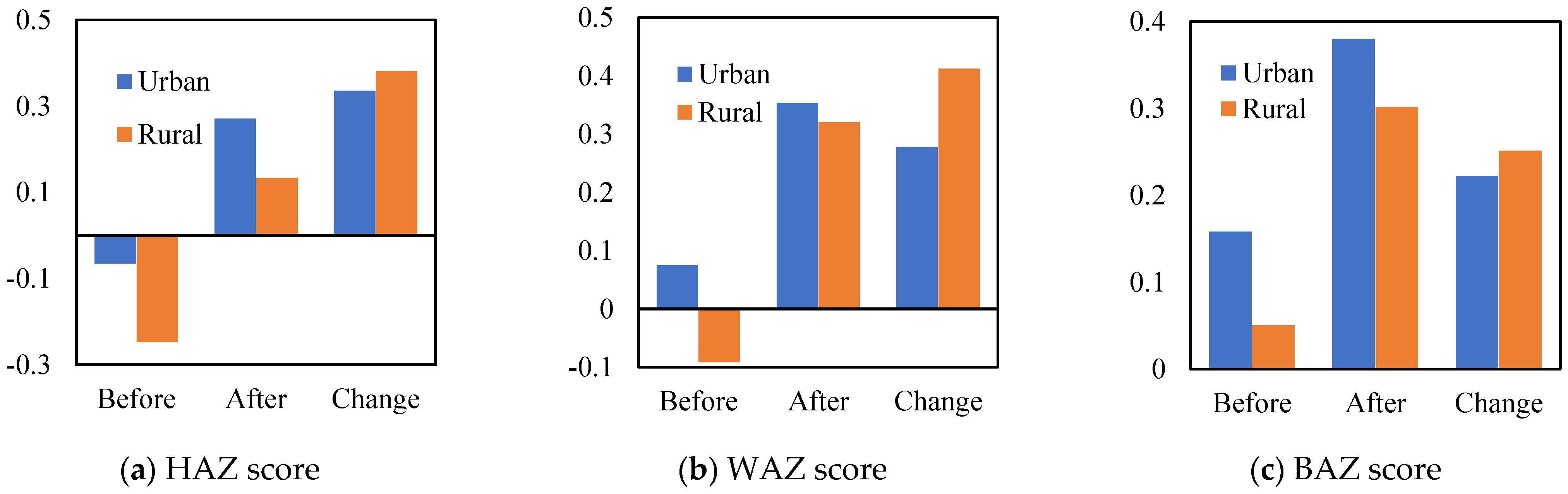
4.1. Summary of Statistics
4.2. Baseline Results
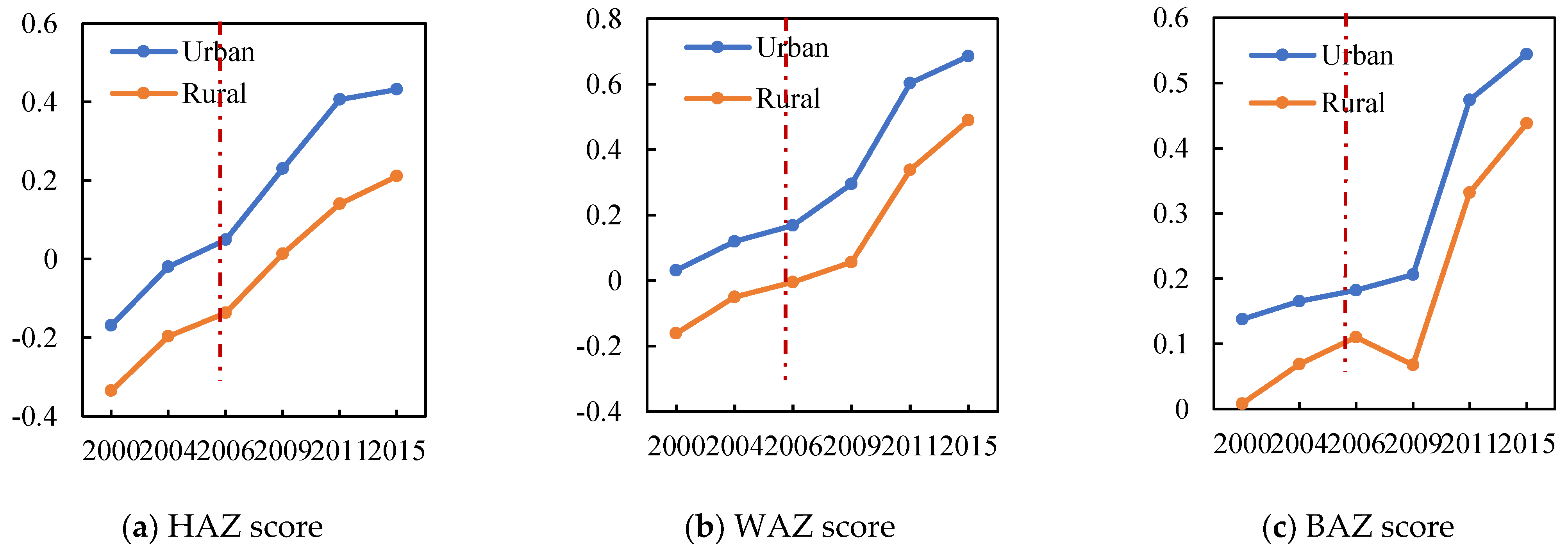
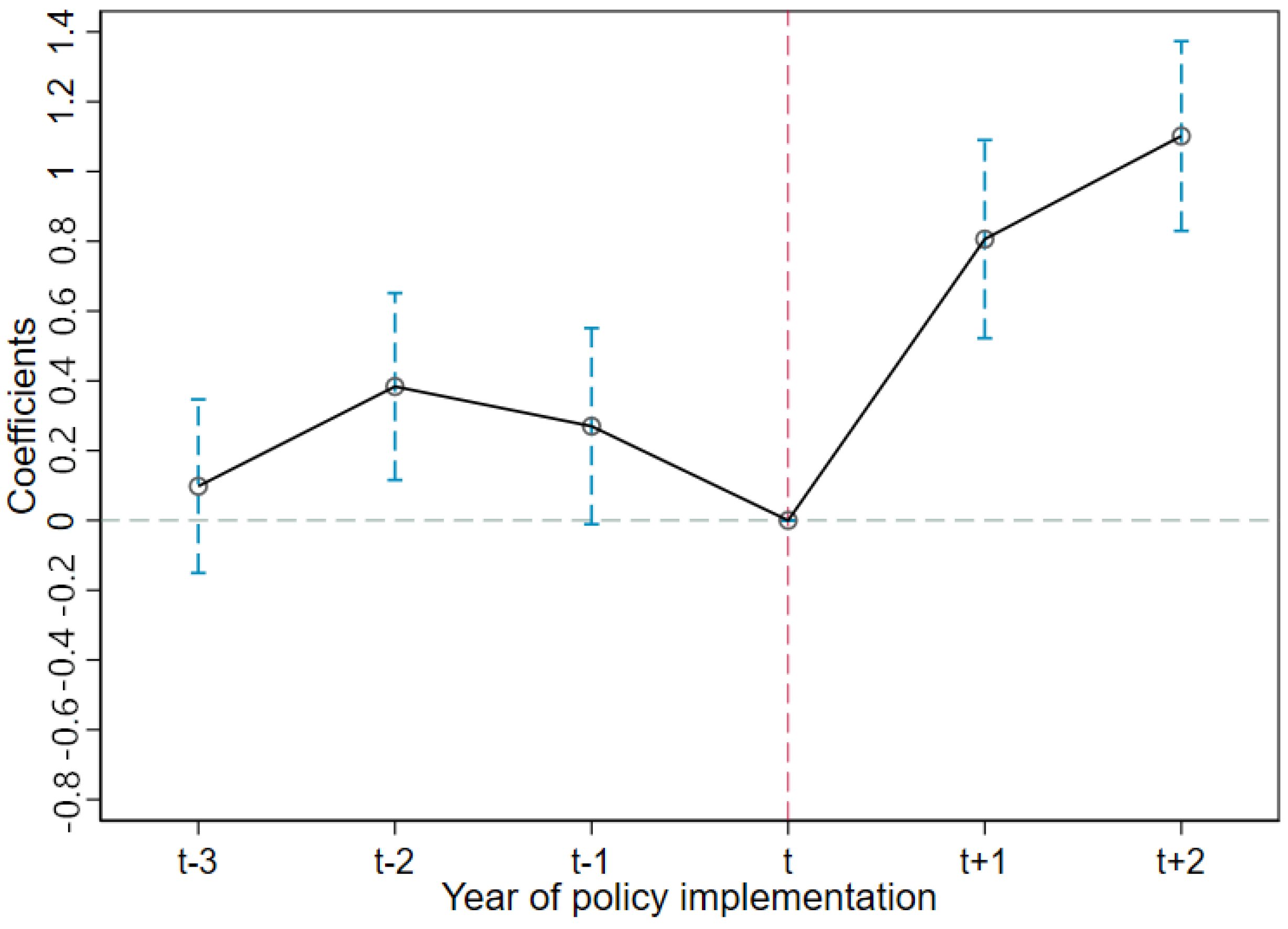
4.3. Test for Parallel Trends Assumption
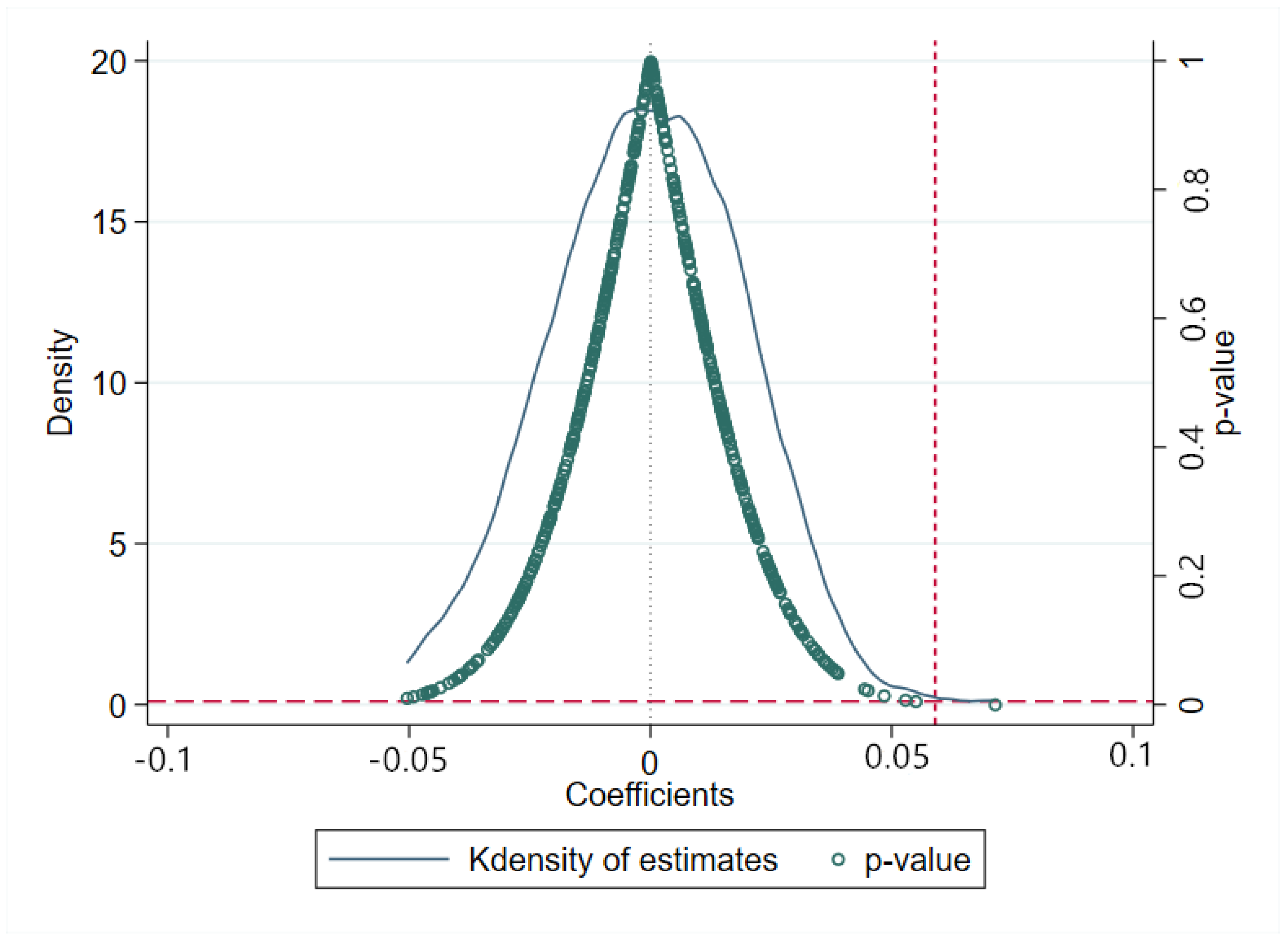
4.4. Placebo Test
4.5. Robustness Checks
4.6. Heterogeneity Analysis
4.7. Mechanism Analysis
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Goldschmidt, K. The COVID-19 pandemic: Technology use to support the wellbeing of children. J. Pediatric Nurs. 2020, 53, 88. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Chou, S.-Y.; Thornton, R.J. The Effect of Household Technology on Weight and Health Outcomes among Chinese Adults: Evidence from China’s “Home Appliances Going to the Countryside” Policy. J. Hum. Cap. 2015, 9, 364–401. [Google Scholar] [CrossRef]
- Coen-Pirani, D.; León, A.; Lugauer, S. The effect of household appliances on female labor force participation: Evidence from microdata. Labour Econ. 2010, 17, 503–513. [Google Scholar] [CrossRef]
- Kerr, A. Household investment in durable appliances and outcomes for children: Evidence from China. Labour Econ. 2019, 58, 110–127. [Google Scholar] [CrossRef]
- Karlsson, O.; Kim, R.; Joe, W.; Subramanian, S.V. The relationship of household assets and amenities with child health outcomes: An exploratory cross-sectional study in India 2015–2016. SSM Popul. Health 2020, 10, 100513. [Google Scholar] [CrossRef]
- Case, A.; Lubotsky, D.; Paxson, C. Economic Status and Health in Childhood: The Origins of the Gradient. Am. Econ. Rev. 2002, 92, 1308–1334. [Google Scholar] [CrossRef]
- Forrest, C.; Riley, A. Childhood Origins Of Adult Health: A Basis For Life-Course Health Policy. Health Aff. 2004, 23, 155–164. [Google Scholar] [CrossRef]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; De Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Katoch, O.R. Determinants of malnutrition among children: A systematic review. Nutrition 2022, 96, 111565. [Google Scholar] [CrossRef]
- Gao, M.; Wells, J.C.K.; Johnson, W.; Li, L. Socio-economic disparities in child-to-adolescent growth trajectories in China: Findings from the China Health and Nutrition Survey 1991–2015. Lancet Reg. Health West. Pac. 2022, 21, 100399. [Google Scholar] [CrossRef]
- Chen, L.; Chu, L. Does health insurance coverage lead to better child health? Evidence from China. China Popul. Dev. Stud. 2019, 3, 1–23. [Google Scholar] [CrossRef]
- Jin, M. Asset Holdings and Undernutrition of Young Children: Evidence from China Health and Nutrition Survey. Ph.D. Thesis, Washington University, St. Louis, MI, USA, 2014. [Google Scholar] [CrossRef]
- Tewari, I.; Wang, Y. Durable Ownership, Time Allocation, and Female Labor Force Participation: Evidence from China’s “Home Appliances to the Countryside” Rebate. Econ. Dev. Cult. Change 2021, 70, 87–127. [Google Scholar] [CrossRef]
- Greenwood, J.; Seshadri, A.; Yorukoglu, M. Engines of Liberation. Rev. Econ. Stud. 2005, 72, 109–133. [Google Scholar] [CrossRef]
- Skoufias, E. Labor market opportunities and intrafamily time allocation in rural households in South Asia. J. Dev. Econ. 1993, 40, 277–310. [Google Scholar] [CrossRef]
- Minagawa, J.; Upmann, T. A note on parental time allocation. Labour Econ. 2013, 25, 153–157. [Google Scholar] [CrossRef]
- Nicoletti, C.; Tonei, V. Do parental time investments react to changes in child’s skills and health? Eur. Econ. Rev. 2020, 127, 103491. [Google Scholar] [CrossRef]
- Mokyr, J. Why “more work for mother?” Knowledge and household behavior, 1870-1945. J. Econ. Hist. 2000, 60, 1–41. [Google Scholar] [CrossRef]
- Heard, B.R.; Thi, H.T.; Burra, D.D.; Heller, M.C.; Miller, S.A.; Duong, T.T.; Simioni, M.; Jones, A.D. The Influence of Household Refrigerator Ownership on Diets in Vietnam. Econ. Hum. Biol. 2020, 39, 100930. [Google Scholar] [CrossRef]
- Brown, D.C. Save the Babies: American Public Health Reform and the Prevention of Infant Mortality, 1850–1929. Hist. Rev. New Books 1991, 19, 106. [Google Scholar] [CrossRef]
- Nickles, S. “ Preserving women”: Refrigerator design as social process in the 1930s. Technol. Cult. 2002, 43, 693–727. [Google Scholar] [CrossRef]
- Lloyd, C.R. Washing machine usage in remote aboriginal communities. Aust. New Zealand J. Public Health 1998, 22, 695–699. [Google Scholar] [CrossRef] [PubMed]
- Bowden, S.; Offer, A. Household appliances and the use of time: The United States and Britain since the 1920s. Econ. Hist. Rev. 1994, 47, 725–748. [Google Scholar] [CrossRef]
- Ramey, V.A. Time spent in home production in the twentieth-century United States: New estimates from old data. J. Econ. Hist. 2009, 69, 1–47. [Google Scholar] [CrossRef]
- Nandi, A.; Charters, T.; Quamruzzaman, A.; Strumpf, E.; Kaufman, J.; Heymann, J.; Mukherji, A.; Harper, S. Health care services use, stillbirth, and neonatal and infant survival following implementation of the Maternal Health Voucher Scheme in Bangladesh: A difference-in-differences analysis of Bangladesh Demographic and Health Survey data, 2000 to 2016. PLoS Med. 2022, 19, e1004022. [Google Scholar] [CrossRef]
- WHO. WHO Child Growth Standards: Growth Velocity Based on Weight, Length and Head Circumference: Methods and Development; WHO: Geneva, Switzerland, 2009.
- Goode, A.; Mavromaras, K. Family income and child health in China. China Econ. Rev. 2014, 29, 152–165. [Google Scholar] [CrossRef]
- Song, Q.; Smith, J.P. Hukou system, mechanisms, and health stratification across the life course in rural and urban China. Health Place 2019, 58, 102150. [Google Scholar] [CrossRef]
- Basu, S.; Gorry, D. Consequences of teenage childbearing on child health. Econ. Hum. Biol. 2021, 42, 101019. [Google Scholar] [CrossRef]
- Hernández-Murillo, R.; Martinek, C. The Effects of Education on Health. Econ. Synop. 2011, 2011. [Google Scholar] [CrossRef]
- Fink, G.; Günther, I.; Hill, K. The effect of water and sanitation on child health: Evidence from the demographic and health surveys 1986–2007. Int. J. Epidemiol. 2011, 40, 1196–1204. [Google Scholar] [CrossRef] [Green Version]
- Mangyo, E. The effect of water accessibility on child health in China. J. Health Econ. 2008, 27, 1343–1356. [Google Scholar] [CrossRef]
- Aslam, M.; Kingdon, G.G. Parental education and child health—understanding the pathways of impact in Pakistan. World Dev. 2012, 40, 2014–2032. [Google Scholar] [CrossRef]
- Case, A.; Paxson, C. Parental behavior and child health. Health Aff. 2002, 21, 164–178. [Google Scholar] [CrossRef] [PubMed]
- Beck, T.; Levine, R.; Levkov, A. Big bad banks? The winners and losers from bank deregulation in the United States. J. Financ. 2010, 65, 1637–1667. [Google Scholar] [CrossRef]
- Currie, J.; Stabile, M. Socioeconomic Status and Child Health: Why Is the Relationship Stronger for Older Children? Am. Econ. Rev. 2003, 93, 1813–1823. [Google Scholar] [CrossRef]
- Cochrane, S.H.; Ohara, D.J.; Leslie, J. The Effects of Education on Health; World Bank: Washington, DC, USA, 1980; Volume 24, pp. 960–992. [Google Scholar]
- Zee, P.C.; Turek, F.W. Sleep and health: Everywhere and in both directions. Arch. Intern. Med. 2006, 166, 1686–1688. [Google Scholar] [CrossRef] [PubMed]
- Chou, S.-Y.; Liu, J.-T.; Grossman, M.; Joyce, T. Parental education and child health: Evidence from a natural experiment in Taiwan. Am. Econ. J. Appl. Econ. 2010, 2, 33–61. [Google Scholar] [CrossRef]
- La Ferrara, E.; Chong, A.; Duryea, S. Soap operas and fertility: Evidence from Brazil. Am. Econ. J. Appl. Econ. 2012, 4, 1–31. [Google Scholar] [CrossRef]
- Liu, Q.; Lu, Y. Firm investment and exporting: Evidence from China’s value-added tax reform. J. Int. Econ. 2015, 97, 392–403. [Google Scholar] [CrossRef]
- Asadullah, M.N.; Mansoor, N.; Randazzo, T.; Wahhaj, Z. Is son preference disappearing from Bangladesh? World Dev. 2021, 140, 105353. [Google Scholar] [CrossRef]
- Rahman, A. Cultural Norms and Son Preference in Intrahousehold Food Distribution: A Case Study of Two Asian Rural Economies. Rev. Income Wealth 2019, 65, 415–461. [Google Scholar] [CrossRef]
- Bittman, M.; Rice, J.M.; Wajcman, J. Appliances and their impact: The ownership of domestic technology and time spent on household work. Br. J. Sociol. 2004, 55, 401–423. [Google Scholar] [CrossRef] [PubMed]
- Bugental, D.B.; Beaulieu, D.A.; Silbert-Geiger, A. Increases in parental investment and child health as a result of an early intervention. J. Exp. Child Psychol. 2010, 106, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Luo, S.; Xia, H.; Gao, Y.; Jin, J.S.; Athauda, R. Smart fridges with multimedia capability for better nutrition and health. In Proceedings of the 2008 International Symposium on Ubiquitous Multimedia Computing, Hobart, Australia, 13–15 October 2008; pp. 39–44. [Google Scholar]
- Mundo-Rosas, V.; Rodríguez-Ramírez, S.; Shamah-Levy, T. Energy and nutrient intake in Mexican children 1 to 4 years old: Results from the Mexican National Health and Nutrition Survey 2006. Salud Pública México 2009, 51, S530–S539. [Google Scholar] [CrossRef] [PubMed]
- Lazarou, C.; Soteriades, E.S. Children’s physical activity, TV watching and obesity in Cyprus: The CYKIDS study. Eur. J. Public Health 2010, 20, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Auffhammer, M.; Wolfram, C.D. Powering up China: Income distributions and residential electricity consumption. Am. Econ. Rev. 2014, 104, 575–580. [Google Scholar] [CrossRef] [Green Version]

| Variable | Abbreviation | Description |
|---|---|---|
| Dependent variable | ||
| HAZ score | HAZ | Continuous variable |
| WAZ score | WAZ | Continuous variable |
| BAZ score | BAZ | Continuous variable |
| Self-rated health | SRH | 1 = Poor;2 = Fair;3 = Good;4 = Excellent |
| Independent variables | ||
| Whether a child’s household was in a rural area | Rural | 1 = rural area; otherwise, 0 |
| Whether the survey year was 2009 or later | Post | 1 = 2009 or later; otherwise 0 |
| Control variables | ||
| Age in years | Age | Continuous variable |
| Child education in years | Education | Continuous variable |
| Medical insurance | Insurance | 1 = with access to Insurance; otherwise, 0 |
| Sleep time in hours | Sleep time | Continuous variable |
| Flushing toilet availability | Toilet | 1 = available flush toilet; 0 = otherwise |
| Tap water availability | Water | 1 = available tap water; 0 = otherwise |
| Household income | Ln(income) | Continuous variable, inflated to Chinese CNY in 2015 |
| Parents’ housework time in hours | P_H time | Continuous variable |
| Do parents smoke | P_Smoke | 1 = at least one parent smoked; 0 = otherwise |
| Parental average education in years | P_Education | Continuous variable |
| Path variables | ||
| Parents’ child-care time in hours | P_C time | Continuous variable |
| Color TV ownership | Color TV | 1 = Own Color TV; 0 = otherwise |
| Washing machine ownership | Washing machine | 1 = Own Washing machine; 0 = otherwise |
| Refrigerator ownership | Refrigerator | 1 = Own Refrigerator; 0 = otherwise |
| Average three-day energy intake | Kcal | Continuous variable |
| Average three-day carbohydrate intake | Carbohydrate | Continuous variable |
| Average three-day fat intake | Fat | Continuous variable |
| Average three-day protein intake | Protein | Continuous variable |
| Before | After | |||||||
|---|---|---|---|---|---|---|---|---|
| Rural | Urban | Rural | Urban | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Dependent variable | ||||||||
| HAZ | −0.25 | 0.92 | −0.06 | 0.95 | 0.13 | 1.02 | 0.27 | 1.00 |
| WAZ | −0.09 | 0.73 | 0.10 | 0.84 | 0.32 | 1.15 | 0.35 | 1.12 |
| BAZ | 0.05 | 0.70 | 0.16 | 0.81 | 0.30 | 1.14 | 0.38 | 1.20 |
| SRH | 2.05 | 1.24 | 2.13 | 1.37 | 2.34 | 1.74 | 2.23 | 1.40 |
| Control variables | ||||||||
| Age | 10.13 | 4.84 | 10.99 | 4.95 | 8.34 | 4.95 | 9.39 | 5.07 |
| Education | 9.52 | 5.40 | 12.15 | 5.81 | 11.73 | 13.02 | 18.00 | 6.31 |
| Insurance | 0.23 | 0.42 | 0.25 | 0.43 | 0.90 | 0.30 | 0.88 | 0.33 |
| Sleep time | 9.51 | 1.74 | 9.07 | 1.71 | 9.49 | 1.80 | 9.21 | 1.83 |
| Toilet | 0.26 | 0.44 | 0.64 | 0.48 | 0.57 | 0.50 | 0.86 | 0.34 |
| Water | 0.60 | 0.49 | 0.89 | 0.31 | 0.79 | 0.41 | 0.96 | 0.20 |
| Ln(income) | 9.67 | 0.92 | 9.99 | 0.98 | 10.52 | 1.08 | 10.75 | 1.16 |
| P_H time | 81.32 | 63.47 | 104.82 | 81.34 | 140.78 | 104.55 | 184.97 | 132.54 |
| P_Smoke | 0.01 | 0.11 | 0.01 | 0.10 | 0.00 | 0.05 | 0.01 | 0.10 |
| P_Education | 18.53 | 6.04 | 21.41 | 6.28 | 21.20 | 5.73 | 25.15 | 5.82 |
| Path variables | ||||||||
| P_C time | 10.11 | 44.41 | 12.08 | 48.18 | 21.97 | 42.00 | 20.15 | 44.60 |
| Color TV | 0.75 | 0.43 | 0.89 | 0.31 | 0.98 | 0.13 | 0.99 | 0.09 |
| Washing machine | 0.55 | 0.50 | 0.74 | 0.44 | 0.84 | 0.36 | 0.92 | 0.27 |
| Refrigerator | 0.31 | 0.46 | 0.62 | 0.48 | 0.78 | 0.42 | 0.90 | 0.31 |
| Kcal | 1727.92 | 672.65 | 1811.72 | 682.24 | 1517.73 | 619.60 | 1543.99 | 609.51 |
| Carbohydrate | 264.10 | 107.48 | 245.85 | 100.12 | 210.87 | 89.78 | 190.52 | 85.17 |
| Fat | 51.68 | 33.79 | 65.49 | 36.32 | 53.24 | 34.59 | 61.50 | 32.30 |
| Protein | 51.47 | 21.76 | 59.47 | 27.85 | 48.56 | 21.11 | 56.67 | 24.22 |
| Observations | 1.423 | 1.216 | 1.308 | 1.138 | ||||
| Variables | (1) | (2) | (3) |
|---|---|---|---|
| HAZ | WAZ | BAZ | |
| Rural × Post | 0.059 ** | 0.083 *** | 0.069 ** |
| (0.029) | (0.030) | (0.031) | |
| Age | −0.086 *** | −0.064 *** | −0.025 *** |
| (0.007) | (0.008) | (0.008) | |
| Education | 0.042 *** | 0.023 *** | 0.002 |
| (0.005) | (0.005) | (0.005) | |
| Insurance | 0.109 *** | 0.073 ** | 0.024 |
| (0.030) | (0.032) | (0.032) | |
| Sleep time | −0.064 *** | −0.060 *** | −0.029 ** |
| (0.011) | (0.012) | (0.012) | |
| Water | 0.008 | 0.010 | 0.012 |
| (0.034) | (0.036) | (0.037) | |
| Toilet | 0.165 *** | 0.179 *** | 0.116 *** |
| (0.031) | (0.032) | (0.033) | |
| Ln(income) | 0.021 * | 0.013 | 0.007 |
| (0.012) | (0.013) | (0.013) | |
| P_H time | 0.000 | 0.000 * | 0.000 |
| (0.000) | (0.000) | (0.000) | |
| P_Smoke | −0.342 *** | 0.020 | −0.290 ** |
| (0.126) | (0.132) | (0.136) | |
| P_Education | 0.018 *** | 0.018 *** | 0.012 *** |
| (0.003) | (0.003) | (0.003) | |
| Constant | 0.100 | 0.373 ** | 0.287 |
| (0.176) | (0.185) | (0.189) | |
| R-squared | 0.081 | 0.061 | 0.023 |
| Observations | 5.085 | 5.085 | 5.085 |
| Alternative Health | Alternative Model (PSM–DID) | |||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| SRH | HAZ | WAZ | BAZ | |
| Rural × Post | 0.141 *** | |||
| (0.051) | ||||
| Pilot × After | 0.099 * | 0.087 * | 0.167 *** | |
| (0.051) | (0.046) | (0.056) | ||
| Constant | 2.985 *** | −0.010 | 0.100 *** | 0.282 *** |
| (0.318) | (0.029) | (0.027) | (0.031) | |
| Control variables | Y | Y | Y | Y |
| R-squared | 0.011 | 0.140 | 0.002 | 0.811 |
| Observations | 4.797 | 1.562 | 1.562 | 1.540 |
| Boys | Girls | |||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| HAZ | WAZ | BAZ | HAZ | WAZ | BAZ | |
| Rural × Post | 0.035 | 0.066 | 0.052 | 0.077 * | 0.093 ** | 0.078 * |
| (0.039) | (0.041) | (0.042) | (0.043) | (0.045) | (0.046) | |
| Constant | 0.001 | 0.108 | −0.015 | 0.278 | 0.689 ** | 0.638 ** |
| (0.238) | (0.250) | (0.255) | (0.264) | (0.276) | (0.284) | |
| Control variables | Y | Y | Y | Y | Y | Y |
| R-squared | 0.080 | 0.066 | 0.029 | 0.084 | 0.061 | 0.023 |
| Observations | 2.716 | 2.716 | 2.716 | 2.369 | 2.369 | 2.369 |
| Age < 12 | Age > 12 | |||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| HAZ | WAZ | BAZ | HAZ | WAZ | BAZ | |
| Rural × Post | 0.044 | 0.055 | 0.052 | 0.108 ** | 0.145 *** | 0.110 ** |
| (0.041) | (0.042) | (0.043) | (0.047) | (0.049) | (0.050) | |
| Constant | −0.190 | 0.010 | −0.035 | −1.225 *** | −0.385 | 0.128 |
| (0.248) | (0.258) | (0.259) | (0.286) | (0.301) | (0.307) | |
| Control variables | Y | Y | Y | Y | Y | Y |
| R-squared | 0.058 | 0.054 | 0.025 | 0.073 | 0.039 | 0.012 |
| Observations | 2.564 | 2.564 | 2.564 | 2.099 | 2.099 | 2.099 |
| (1) | (2) | |
|---|---|---|
| P_H Time | P_C Time | |
| Rural × Post | −13.854 ** | 5.949 *** |
| (6.643) | (0.465) | |
| Constant | 124.753 *** | 6.705 *** |
| (2.291) | (0.259) | |
| Control variables | Y | Y |
| R-squared | 0.587 | 0.022 |
| Observations | 5.085 | 5.085 |
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Kcal | Carbohydrate | Fat | Protein | |
| Rural × Post | 143.138 *** | 21.570 *** | 5.605 ** | 14.667 *** |
| (46.808) | (7.015) | (2.711) | (0.968) | |
| Constant | 1,628.123 *** | 233.022 *** | 54.160 *** | 49.036 *** |
| (12.483) | (1.871) | (0.723) | (0.344) | |
| Control variables | Y | Y | Y | Y |
| R-squared | 0.635 | 0.640 | 0.573 | 0.593 |
| Observations | 5.085 | 5.085 | 5.085 | 5.085 |
| (1) | (2) | (3) | |
|---|---|---|---|
| HAZ | HAZ | BAZ | |
| TV_color | 0.050 | −0.037 | −0.048 |
| (0.060) | (0.063) | (0.064) | |
| Washing_machine | 0.131 *** | 0.084 ** | 0.017 * |
| (0.036) | (0.037) | (0.038) | |
| Refrigerator | 0.199 *** | 0.259 *** | 0.216 *** |
| (0.033) | (0.035) | (0.036) | |
| Constant | 0.131 | 0.495 *** | 0.407 ** |
| (0.180) | (0.189) | (0.195) | |
| Control variables | Y | Y | Y |
| R-squared | 0.094 | 0.075 | 0.100 |
| Observations | 5085 | 5085 | 5085 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shi, J.; Wang, F.; Wang, H. The Effect of Household Technology on Child Health: Evidence from China’s “Home Appliances Going to the Countryside” Policy. Int. J. Environ. Res. Public Health 2022, 19, 11976. https://doi.org/10.3390/ijerph191911976
Shi J, Wang F, Wang H. The Effect of Household Technology on Child Health: Evidence from China’s “Home Appliances Going to the Countryside” Policy. International Journal of Environmental Research and Public Health. 2022; 19(19):11976. https://doi.org/10.3390/ijerph191911976
Chicago/Turabian StyleShi, Junhui, Fang Wang, and Huan Wang. 2022. "The Effect of Household Technology on Child Health: Evidence from China’s “Home Appliances Going to the Countryside” Policy" International Journal of Environmental Research and Public Health 19, no. 19: 11976. https://doi.org/10.3390/ijerph191911976
APA StyleShi, J., Wang, F., & Wang, H. (2022). The Effect of Household Technology on Child Health: Evidence from China’s “Home Appliances Going to the Countryside” Policy. International Journal of Environmental Research and Public Health, 19(19), 11976. https://doi.org/10.3390/ijerph191911976






