Abstract
There is no universal postoperative classification of extracapsular hip fractures (ECFs). We wondered if infection (according to infection after fracture fixation criteria (IAFF)), immediate partial weight bearing (PWB) and/or the new GammaTScore tool could predict early cut-out. We also examined the correlation between GammaTScore and time to consolidation and studied long-term survival. This was a retrospective cohort study of low-energy complete ECFs operated with Gamma3T nailing in 2014 and fully monitoring, in patients aged over 65. Ten not distally locked cases, one late cut-out, one cut-through, one osteonecrosis and one pseudarthrosis were discarded. Patients were classified into early cut-out (7/204; 3.55%) and no early cut-out (197/204; 96.45%). There was a lower percentage of A2 fractures according to the AO Foundation/Orthopaedic Trauma Association classification (AO/OTA, 1997) in early cut-out. IAFF and only the GammaTScore reduction parameter were different for early cut-out, in opposition to immediate PWB, tip-to-apex distance (TAD) or the Baumgaertner–Fogagnolo classification. GammaTScore inversely correlated with consolidation (p < 0.01). Long-term survival time was not statistically significantly lower in the early cut-out group. Small sample of cases may limit our results. Apart from an important role of IAFF, GammaTScore would be useful for predicting consolidation, avoiding complications and reducing costs. Further studies are needed for reliability.
1. Introduction
Extracapsular hip fractures (ECFs) in elderly patients have a high morbidity and mortality rate, which represents a serious international public health problem [1]. Most of these fractures are treated surgically. Confirming healing and minimizing complications is essential [2], as the clinical consequences of failure can be devastating [3]. ECFs treated with nailing almost always consolidate [4]. The cause for the approximately 5% that do not is mainly summarized as non-traumatic mechanical complications (NTMCs) [5].
The most common NTMC reported is cut-out. Parker first defined it in 1992 as the “projection of the lag screw from the femoral head by more than 1 mm”, referring to the dynamic hip screw (DHS) [6], but later on, it changed to “the collapse of the neck-shaft angle into varus, leading to extrusion of the screw from the femoral head“ (Baumgaertner, 1995) [7]. The compilation of cut-out cases presents three main difficulties:
- -
- Physiopathology: It is probably underdiagnosed when we only observe disrotation without migration. However, there are some cases when the cut-out does not progress and the fracture consolidates, but we do not know when and why this occurs [8];
- -
- Differential diagnosis: Cut-in [9] and cut-through [10] are still mistaken for cut-out;
- -
- Time of diagnosis: Bojan considered as early NTMCs those detected within 3 months postoperatively [11]. A recent article [12] includes them as “Early Mechanical Complications” (EMCs) if they occur before the first postoperative year.
It seems that the cut-out rate experienced in fractures treated with short nails is the same as in those treated with long ones [13]. In addition, recent clinical works reject the theoretical superiority of blade versus screw as proximal locking devices (PLDs) [14]. Its incidence has progressively decreased from 16% to less than 8%, and it is currently 1.6–4.3% [15]. This phenomenon can probably be explained by the following reasons:
- -
- Design improvements [16]: Smaller nail diameters and advances in PLDs;
- -
- Learning curve [17]: The quick widespread use of nails in all ECFs (instead of DHSs);
- -
- Biomechanical factors: Cleveland and Bosworth [18] wrote that the PLD distal end in the centre–centre or posteroinferior quadrant prevents from this complication. Parker [6] pointed out that the ideal position was central or inferior in anteroposterior view and central in lateral view. There is no consensus on the peripheral position with worst prognosis [4]. Baumgaertner demonstrated that a < 25 mm tip–apex distance (TAD), as the sum of anteroposterior and axial projections, is a protective factor [7]. Subsequently, new factors or modifications of previous ones have been described, but they have not been as universally accepted or recognized [19]: calcar-referenced TAD < 25 mm [20], varus reduction [21], ECF extension to the femoral neck [22], posterior subtype of Ikuta’s classification [23], vertical shear fracture [24] and intraoperative breakage/lack of lateral wall competency [25].
Heretofore, postoperative infection has not been clearly implicated in early cut-out, but it is especially difficult to confirm really depth ones [26]. Moreover, there is a clear tendency to immediately allow patients to perform partial weight bearing (PWB) postoperatively, but there are many protocols, and not all patients collaborate, so the role this factor plays is undefined [27].
Preoperative classifications have only found that the DHS is not indicated in unstable and reverse fracture patterns [21,28]. The AO Foundation/Orthopaedic Trauma Association classification (AO/OTA 1997, updated in 2007), widely used in research [29], has poor inter- and intra-observer reliability. Massoud [30] has introduced the “basicervical-equivalent” concept, but it has not succeeded. Postoperatively, ECFs fractures are stable or unstable; classic unstable patterns include insufficient posteromedial cortex contact/comminution, subtrochanteric extension and/or reverse obliquity. Baumgaertner–Fogagnolo [31] classified them based solely on reduction. In 2013, another tool was developed, but with a complex scoring system [32].
We believe it is important to know the risk factors with prognostic value. We researched if IAFF (infection after fixation fracture), immediate PWB and/or the use of a new postoperative tool, GammaTScore, could predict early cut-out and if there was a correlation between early cut-out and time to consolidation. Finally, we focused on long-term survival in both complicated and non-complicated cases.
2. Materials and Methods
This study was performed at Hospital Universitario de Salamanca (HUS), which is a third-level university hospital and a regional centre of reference for certain services.
The design used to achieve the objective and test the hypothesis of this work consisted of a historical cohort study of ECF-diagnosed patients in our department who were over 65 years old in 2014. Our previous publication [33] outlines the sample collection, with inclusion and exclusion criteria, as well as the material and methods employed for consolidation definition, radiological views and measurements, and follow-up protocol and survival. All our patients were considered osteoporotic, given the recruitment.
We evaluated 204 titanium Gamma 3 trochanteric nails (hereafter Gamma3T)—length of 180 mm and distal width of 11 mm, with neck–shaft angle between 120° and 130° (Stryker® Trauma GmbH, Schörnkirchen, Germany)—with a total of 7 cases called “Early cut-out” (3.55%) and 197 called “No early cut-out” (96.55%). Four major mechanical complications were excluded due to possible interference: one late cut-out, one cut-through, one pseudarthrosis and one osteonecrosis (Figure 1).
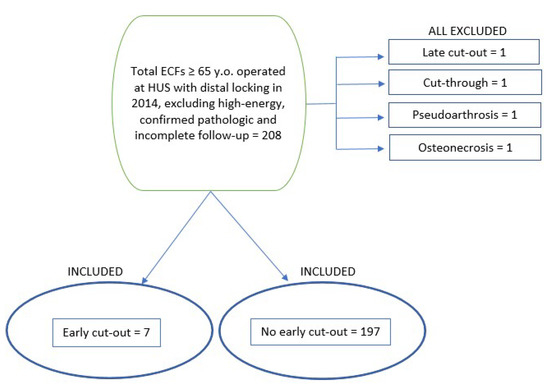
Figure 1.
Organization chart (ECF, extracapsular fracture; HUS, Hospital Universitario de Salamanca; Sx., surgery.).
Early cut-out was defined as any grade of disrotation and/or migration of the PLD in the cephalic fragment, without (incomplete, grades I and II) or with (complete, grade III) articular damage, at any point throughout follow-up until 6 months postoperatively. All infections were considered as depth infections and met at least one of the confirmatory criteria for IAFF. Immediate postoperative PWB was authorized if reduction was considered good as per the Baumgaertner–Fogagnolo classification [31] criteria.
To elaborate GammaTScore, we empirically identified and classified most of the unfavourable prognostic variables into 3 parameters based on reduction, osteosynthesis and instability, with a score ranging from 1 to 3 points. The final rate of the 3 × 3 algorithm was considered good for 8–9 points, moderate for 5–7 points and poor for 3–4 points (Figure 2 and Figure 3).
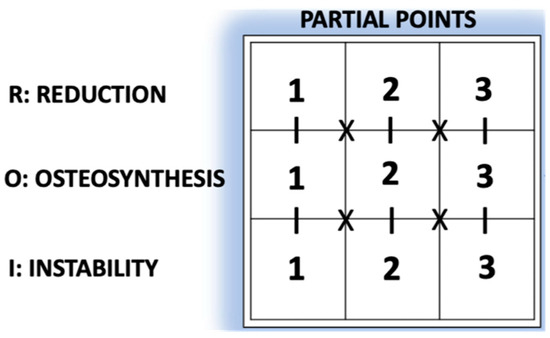
Figure 2.
GammaTScore scoring system.
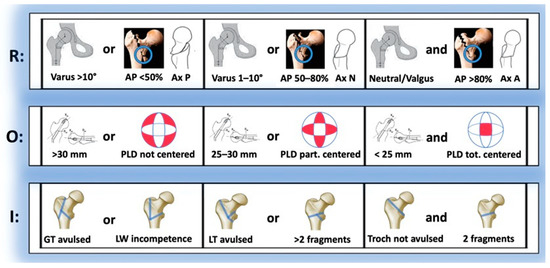
Figure 3.
GammaTScore algorithm obtention chart.
- Reduction parameter (R):
- CCD (Varus/Neutral/Valgus): Difference between the caput–collum–diaphyseal (CCD) angle of the currently operated hip and that of the contralateral one (if the latter was previously operated on, this CCD was taken as a reference);
- AP%: Percentage of cortical contact in AP view;
- P, N or A: Posterior, normal or anterior types (Ikuta’s classification, axial view).
- Osteosynthesis parameter (O):
- TAD: Tip-to-apex distance;
- PLD: Location of the proximal locking device (PLD) in the femoral head (Cleveland–Bostworth classification).
- Instability parameter (I):
- Avulsion: Defined as a radiolucent space > 5 mm in any radiological view of the greater trochanter (GT) or the lesser trochanter (LT);
- LW (lateral wall) in/competence (AO Foundation/Orthopaedic Trauma Association classification; AO/OTA classification 2018).
Descriptive statistics generated using SPSS 20.0 (SPSS, Inc., Chicago, IL, USA) were utilized for data analysis. Kolmogorov–Smirnov’s normality tests were used to check if the continuous variables matched a normal distribution, and comparisons were performed with Mann–Whitney’s U tests. For categorical variables, Pearson’s chi-square tests and Fisher’s exact tests were used, and the median test was used to calculate discrete continuous variable risk score. All p-values were two-sided, and p-values below 0.05 were considered significant. Mantel–Cox’s log-rank, Breaslow’s (generalized Wilcoxon) and Tarone-Ware’s tests were used to evaluate survival, yielding no significant differences. Boxplots and bar diagrams were generated to compare the main outcomes.
3. Results
3.1. Preoperative Variables (Table 1)
Cohorts were similar, including social situation, dependency (Barthel’s index [34]), comorbidity (Charlson’s comorbidity index, CMI [35]), cognitive impairment (Pffeifer’s classification [36]), osteoporosis (OP; Nuti’s classification [37]), previous OP treatment, anti-platelet therapy/anti-coagulation therapy (APT/ACT) and ASA score [38].

Table 1.
Preoperative variables. Tests: a, Fisher’s exact test; b, Pearson’s chi-square test; c, Mann–Whitney’s U test; d, median test (Sx., surgery; CMI, Charlson’s comorbidity index; OP, osteoporosis; Fx., fracture; APT, anti-platelet therapy; ACT, anti-coagulation therapy; AAS, acetylsalicylic acid; LMWH, low-molecular-weight heparin; ASA, American Society of Anesthesiologists). # Upon admission, no calcium and/or vitamin D.
Table 1.
Preoperative variables. Tests: a, Fisher’s exact test; b, Pearson’s chi-square test; c, Mann–Whitney’s U test; d, median test (Sx., surgery; CMI, Charlson’s comorbidity index; OP, osteoporosis; Fx., fracture; APT, anti-platelet therapy; ACT, anti-coagulation therapy; AAS, acetylsalicylic acid; LMWH, low-molecular-weight heparin; ASA, American Society of Anesthesiologists). # Upon admission, no calcium and/or vitamin D.
| Variable | Early Cut-Out | No Early Cut-Out | p |
|---|---|---|---|
| Age (years-old) | 83 (SD 10.31) (65;99) | 85.82 (SD 6.59) (65;103) | 0.512 c |
| Sex | 0.640 a | ||
| -Female | 5 (71.4%) | 156 (79.2%) | |
| -Male | 2 (28.6%) | 41 (20.8%) | |
| Side | 1.000 a | ||
| -Left | 3 (42.4%) | 81 (41.1%) | |
| -Right | 4 (57.6%) | 116 (58.9%) | |
| Social situation | 0.121 a | ||
| -Home, alone | 3 (42.9%) | 26 (13.2%) | |
| -Home, not alone | 3 (42.9%) | 104 (52.8%) | |
| -Institutionalized | 1 (14.3%) | 67 (34.0%) | |
| Dependency | |||
| -Barthel pre-Sx. | 86.43 (SD 16.51) (55;100) | 75.28 (SD 21.57) (10;100) | 0.150 c |
| -Barthel post-Sx. | 43.57 (SD 21.74) (15;75) | 46.78 (SD 20.93) (10;85) | 0.697 c |
| Comorbidity | |||
| -Non-age-adjusted CMI | 2.57 (SD 1.13) (1;4) | 2.15 (SD 1.29) (0;7) | 0.293 c |
| -Age-adjusted CMI | 6.42 (SD 1.27) (5;8) | 6.11 (SD 1.30) (4;11) | 0.467 c |
| Cognitive status | 1.000 a | ||
| -None | 1 (14.3%) | 33 (16.8%) | |
| -Mild | 5 (71.4%) | 130 (66.0%) | |
| -Moderate | 1 (14.3%) | 33 (16.8%) | |
| -Severe | 0 (0%) | 1 (0.5%) | |
| Previous Fx. | 1.000 a | ||
| -None | 5 (71.4%) | 114 (57.9%) | |
| -Traumatic | 0 (0%) | 6 (3.0%) | |
| -OP fracture | |||
| --Hip | 0 (0%) | 15 (7.6%) | |
| --Other locations | 2 (28.6%) | 54 (27.4%) | |
| --Both locations | 0 (0%) | 8 (4.1%) | |
| OP treatment # | 0.596 b | ||
| -No | 129 (85.4%) | 47 (82.5%) | |
| -Yes | 22 (14.6%) | 10 (17.5%) | |
| APT/ACT | 0.882 a | ||
| -None | 5 (71.4%) | 110 (55.8%) | |
| -AAS 100 | 2 (28.6%) | 39 (19.8%) | |
| -AAS 300 | 0 (0%) | 17 (8.6%) | |
| -Clopidogrel | 0 (0%) | 1 (0.5%) | |
| -Acenocumarol | 0 (0%) | 26 (13.2%) | |
| -Direct Xa | 0 (0%) | 2 (2.0%) | |
| -LMWH | 0 (0%) | 2 (2.0%) | |
| ASA | 3 (1;4) | 3 (1;4) | 0.503 d |
3.2. Perioperative Variables (Table 2)
There were only significant differences in the AO/OTA classification (1997) [29] (less A2 cases), but not in Jensen [28] or Massoud [30], nor in the medical variables.

Table 2.
Perioperative variables. Tests: a, Fisher’s exact test; b, Pearson’s chi-square test; c, Mann–Whitney’s U test (AO/OTA, AO Foundation/Orthopaedic Trauma Association classification; Sx., surgery; [RBC], red blood cells concentrate). *, Statistically significative.
Table 2.
Perioperative variables. Tests: a, Fisher’s exact test; b, Pearson’s chi-square test; c, Mann–Whitney’s U test (AO/OTA, AO Foundation/Orthopaedic Trauma Association classification; Sx., surgery; [RBC], red blood cells concentrate). *, Statistically significative.
| Variable | Early Cut-Out | No Early Cut-Out | p |
|---|---|---|---|
| Jensen | 0.345 a | ||
| Stability (Jensen) | 0.713 a | ||
| -Stable (I + II) | 3 (42.9%) | 73 (37.1%) | |
| -Unstable (III + IV + V) | 4 (57.1%) | 124 (62.9%) | |
| AO/OTA, 2007 * | 0.033 b, * | ||
| -A1 | 3 (42.9%) | 59 (29.9%) | |
| -A2 | 1 (14.3%) | 111 (56.3%) | |
| -A3 | 2 (28.6%) | 17 (8.6%) | |
| Stability(AO/OTA, 2007) | 0.305 b | ||
| Stable | 3 (42.9%) | 118 (59.9%) | |
| Unstable | 3 (42.9%) | 69 (35.0%) | |
| Basicervical (B2.1) | 1 (14.3%) | 10 (5.1%) | |
| Massoud | 1.000 b | ||
| -Stable | 4 (57.1%) | 68 (34.5%) | |
| -Unstable | 3 (42.9%) | 129 (65.5%) | |
| Average stay (days) | 9.57 (SD 2.63) (6;13) | 9.71 (SD 3.36) (4;26) | 0.880 c |
| Pre-Sx. stay (days) | 3.00 (SD 2.00) (0;5) | 3.30 (SD 2.56) (0;9) | 0.749 c |
| Post-Sx. stay (days) | 6.57 (SD 2.22) (3;9) | 6.37 (SD 2.79) (3;25) | 0.431 c |
| Blood loss (g/dl Hb) | 1.42 (SD 1.16) (0;3.0) | 1.92 (SD 1.75) (−3.5;5.9) | 0.323 c |
| Transfusions [RBC] | 1.85 (SD 1.67) (0;5) | 1.35 (SD 1.37) (0;8) | 0.427 c |
3.3. Postperative Variables
IAFF was associated with a higher risk of early cut-out. We did not detect differences in TAD, Baumgaertner–Fogagnolo classification [31] or immediate PWB (Table 3).

Table 3.
Tests: a, Fisher’s exact test; c, Mann–Whitney U test (TAD, tip-to-apex distance; IAFF, infection after fracture fixation; Sx., surgery; PWB, partial weight bearing). *, Statistically significative.
Only the reduction parameter was statistically significant, whereas the osteosynthesis and instability parameters and the GammaTScore final rate did not show any differences (Figure 4).
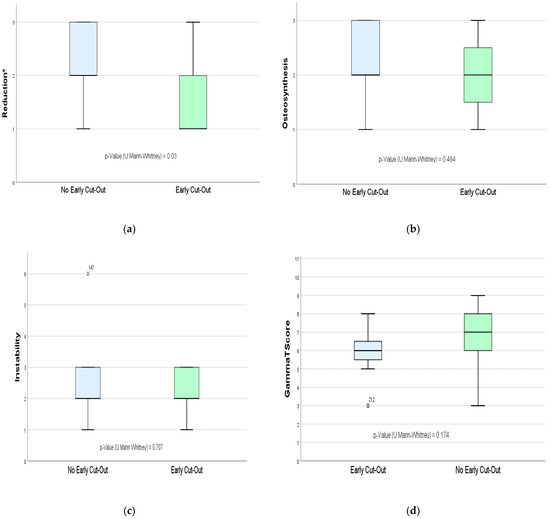
Figure 4.
Representation of results of the GammaTScore tool, from top to bottom and from left to the right: (a) GammaTScore parameter—reduction; (b) GammaTScore parameter—osteosynthesis; (c) GammaTScore parameter—instability; (d) GammaTScore final rate. *, Statistically significative.
3.4. Consolidation (Figure 5)
We observed a highly significant correlation with GammaTScore, with an R2 value of 0.108.
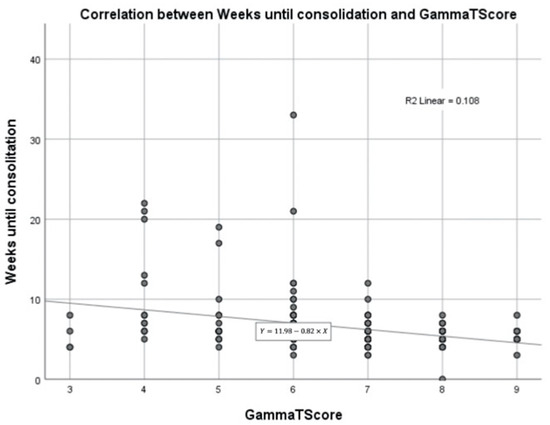
Figure 5.
Correlation between weeks until consolidation and GammaTScore.
3.5. Survival (Figure 6)
Long-term survival was similar in both groups (p = 0.518) after almost 6 years of follow-up.
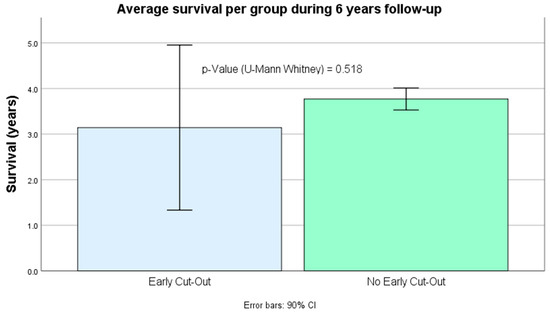
Figure 6.
Average survival per group during almost 6 years follow-up.
3.6. Summary of Evolution of Early Cut-Out Cohort (Table 4)
Of the total of seven early cut-out cases, four cases were considered complete, and three cases were considered incomplete. For their resolution, prosthesis implantation was chosen in three cases, the removal of the material in three others (one consolidated) and observation in the remaining one, which consolidated without progressing.

Table 4.
Summary of the early cut-out cohort. (M, male; F, female; AO/OTA, AO Foundation/Orthopaedic Trauma Association classification; PWB, partial weight bearing; IAFF, infection after fracture fixation; ROM, removal of osteosynthesis material; PHA, partial hip arthroplasty; THA, total hip arthroplasty).
Table 4.
Summary of the early cut-out cohort. (M, male; F, female; AO/OTA, AO Foundation/Orthopaedic Trauma Association classification; PWB, partial weight bearing; IAFF, infection after fracture fixation; ROM, removal of osteosynthesis material; PHA, partial hip arthroplasty; THA, total hip arthroplasty).
| No. | Sex/(Age) | Jensen Stability | AO/OTA (1997) Stability | Massoud Stability | Immediate PWB | Detection Grade (Weeks) | IAFF (Weeks) | Consolidation/Reintervention (Weeks) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | 2.1 | Yes | No | ||||||
| 1 | M (88) | √ | × | √ | × | × | × | √ | Yes | III (4.7) | Yes (10.0) | No/ROM (10.7) |
| 2 | F (88) | × | √ | × | √ | × | × | √ | No | III (23) | Yes (0.71) | No/ROM (25.7) |
| 3 | F (79) | × | √ | × | √ | × | √ | × | No | II (13) | Yes (29.4) | Yes/ROM (30.0) |
| 4 | M (77) | × | √ | × | √ | × | √ | × | No | II (3.0) | No | No/PHA (3.7) |
| 5 | F (65) | √ | × | × | × | √ | √ | × | No | III (5.0) | No | No/THA (16.4) |
| 6 | F (87) | × | √ | √ | × | × | × | √ | No | I (4.3) | No | Yes/- |
| 7 | F (97) | √ | × | √ | × | × | √ | × | Yes | III (2.1) | No | No/PHA (2.86) |
4. Discussion
ECF surgery is a very frequent and standardized procedure that occupies a large part of our activity. Although it has traditionally been considered to be relatively easy, ideal for residents in their early stages to perform, its complications are extremely serious, given that the vast majority occur in elderly patients with associated comorbidity. As a consequence, in recent years, some publications have been released that warn of the often fatal clinical consequences of those cases that require reintervention [39], as well as others that standardize every surgical step [40] in order to avoid errors in osteosynthesis.
For many years, OP has been postulated as a theoretical risk factor or even a confounding factor. In patients with hip fracture, its study using densitometric criteria is practically unfeasible [41]. Consequently, the current World Health Organization (WHO) classification [42], which is based on the severity of osteopenia severity in densitometry, has been criticized for years. Accordingly, we opted for Nuti’s classification [37], as it is simpler and easier for discriminating OP grades, which were similar in both cohorts. Elliot-Gibson stated that barely a third of osteoporotic patients are prescribed antiresorptive/osteoformative therapy and that, of these, less than a third complete the entire treatment [43]. In our study, less than 20% were treated in both groups, with no differences.
We did not find any previous work indicating confirmed IAFF [26] as a risk factor for early cut-out, which we explain it as being caused by the difficult follow-up, its apparently easy control or resolution with antibiotherapy or its insufficient registration (they are usually diagnosed and treated by primary care physicians). Note that in two complicated cases, IAFF occurred weeks later, which makes suspicion even more relevant. Bojan [8] only observed it in some cases of late cut-out. We believe that it is necessary to draw attention to any infectious complication of the surgical wound, which should be always registered in the medical records, using standardized criteria.
There is a clear trend among multiple protocols towards endorsing immediate PWB [44], regardless of whether patients are really able to comply with it [5]. However, its benefit/risk ratio has not actually been proven for intracapsular fractures, and we did not find any article on effective load and early cut-out. In our case, this variable was approved in a similar proportion in both groups. This argues for its limited role in the main NTMC, although the low power of our study opens the door to ulterior investigation.
Current classifications of ECFs are still based on preoperative radiological images, and do not include postoperative aspects that may influence the final outcome, such as obtained reduction [45], PLD osteosynthesis [46] or instability factors [25]. All these reasons motivated the creation of the GammaTScore as an immediate and simple postoperative prognostic tool that could help us reducing the costs involved.
Its reduction parameter showed differences, confirming that it appears to be more crucial than the rest [5]. Ikuta’s classification [23] enhanced it, and fracture varization has recently been postulated as fundamental [47]. Although it was already first intuited by Baumgaertner and Fogagnolo [31], the new tool seems to be more sensitive.
The GammaTScore osteosynthesis parameter was statistically similar, despite TAD being greater than 25 mm in the early cut-out group. Limited TAD and centre–centre positioning have been incorporated since the 1990s and are generally accepted in routine practice, as they are in our centre. Their minor role is probably due to minimal absolute differences in PLD procedures between cut-out and non-cut-out cases, as occurs in our work, which could explain the fact that these variables are currently being challenged [17].
Similarly, the instability parameter result was not statistically significant. Since the avulsion of the lesser trochanter has already been described as a classic instability factor [48], this work incorporated it postoperatively. The same occurred for the greater trochanter, which is clearly related to lateral wall incompetence, admitted in the latest AO/OTA classification [49]. Probably the small sample size of cases and few existing differences explain this outcome.
Both the Baumgaertner–Fogagnolo classification and the final score of GammaTScore were not sensitive enough, even though the former is focused on reduction. Assuming that increased attention to the surgical outcome led to more uniform radiological results, it was really difficult to establish any relevant differences. Anyway, the proportion of early cut-out seemed to be stabilized in less than 5% of cases, which was in line with our cumulative incidence (3.55%); therefore, other non-mechanical risk factors could have been behind them.
We also demonstrated an inverse relationship between GammaTScore and time to consolidation, which could serve for better patient management in office. However, data must be interpreted with caution because they only explained nearly 11% of the total.
Although long-term survival in early cut-out cases was lower, we paradoxically did not find a significant relationship. Less aggressive secondary surgeries, and even conservative final treatment in one case, are possibly sufficient to justify this finding.
We used a highly selected sample and neutralized many of the confounding factors involved, with a long, systematic follow-up that allowed us to evaluate survival. Our study also had some weaknesses, especially the small number of early cut-out cases and its retrospective, non-randomized design that might limit results and reliability.
5. Conclusions
Besides the new role description of IAFF in the main NTMCs of ECFs, the GammaTScore prognostic tool could be useful for preventing early cut-out, which often implies ulterior and severe reinterventions. Moreover, it could provide an easier monitoring prediction until consolidation. All of this might reduce important associated costs. In addition, if proven reliable, it could be applied to other single-PLD-based osteosyntheses.
Author Contributions
Conceptualization, C.H.-P. and J.Á.S.-S.; methodology, J.H.-R. and C.F.S.-V.; investigation, C.H.-P., C.P.-H. and M.V.-M.; writing—original draft preparation, C.H.-P.; writing—review and editing, C.H.-P. and J.Á.S.-S.; visualization, C.H.-P., J.Á.S.-S., J.H.-R. and C.F.S.-V.; supervision, J.A.M.-C.; project administration, J.A.M.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Research Ethics Committee of Hospital Universitario de Salamanca (cod: PI 2021 03 711).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author.
Acknowledgments
We thank María Teresa Prendes-González, Secretary of the Department of Trauma and Orthopaedic Surgery, for her valuable support in data collection and Ángel Sánchez-Hernández, in Mathematics, for his valuable support with source-data handling and database improvements.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Abrahamsen, B.; van Staa, T.; Ariely, R.; Olson, M.; Cooper, C. Excess mortality following hip fracture: A systematic epidemiological review. Osteoporos. Int. 2009, 20, 1633–1650. [Google Scholar] [CrossRef] [PubMed]
- Bretherton, C.P.; Parker, M.J. Femoral Medialization, Fixation Failures, and Functional Outcome in Trochanteric Hip Fractures Treated With Either a Sliding Hip Screw or an Intramedullary Nail From Within a Randomized Trial. J. Orthop. Trauma 2016, 30, 642–646. [Google Scholar] [CrossRef] [PubMed]
- Docquier, P.L.; Manche, E.; Autrique, J.C.; Geulette, B. Complications associated with gamma nailing. A review of 439 cases. Acta Orthop. Belg. 2002, 68, 251–257. [Google Scholar] [PubMed]
- Aguado-Maestro, I.; Escudero-Marcos, R.; García-García, J.M.; Alonso-García, N.; Pérez-Bermejo, D.D.; Aguado-Hernández, H.J.; Nistal-Rodríguez, J.; García-Alonso, M. Results and complications of pertrochanteric hip fractures using an intramedullary nail with a helical blade (proximal femoral nail antirotation) in 200 patients. Rev. Esp. Cirugía Ortop. Traumatol. 2013, 57, 201–207. [Google Scholar] [CrossRef]
- Morvan, A.; Boddaert, J.; Cohen-Bittan, J.; Picard, H.; Pascal-Mousselard, H.; Khiami, F. Risk factors for cut-out after internal fixation of trochanteric fractures in elderly subjects. Orthop. Traumatol.-Surg. Res. 2018, 104, 1183–1187. [Google Scholar] [CrossRef]
- Parker, M.J. Cutting-out of the dynamic hip screw related to its position. J. Bone Jt. Surg. Br. 1992, 74, 625. [Google Scholar] [CrossRef]
- Baumgaertner, M.R.; Curtin, S.L.; Lindskog, D.M.; Keggi, J.M. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J. Bone Jt. Surg. Am. 1995, 77, 1058–1064. [Google Scholar] [CrossRef]
- Bojan, A.J.; Beimel, C.; Speitling, A.; Taglang, G.; Ekholm, C.; Jönsson, A. 3066 consecutive Gamma Nails. 12 years experience at a single centre. BMC Musculoskelet. Disord. 2010, 11, 133. [Google Scholar] [CrossRef]
- Flint, J.H.; Sanchez-Navarro, C.F.; Buckwalter, J.A.; Marsh, J.L. Intrapelvic migration of a gamma nail lag screw: Review of the possible mechanisms. Orthopedics 2010, 33, 1–5. [Google Scholar] [CrossRef]
- Frei, H.C.; Hotz, T.; Cadosch, D.; Rudin, M.; Käch, K. Central head perforation, or “cut through,” caused by the helical blade of the proximal femoral nail antirotation. J. Orthop. Trauma 2012, 26, e102–e107. [Google Scholar] [CrossRef]
- Bojan, A.J.; Beimel, C.; Taglang, G.; Collin, D.; Ekholm, C.; Jönsson, A. Critical factors in cut-out complication after Gamma Nail treatment of proximal femoral fractures. BMC Musculoskelet. Disord. 2013, 14, 1. [Google Scholar] [CrossRef] [PubMed]
- Ehlinger, M.; Favreau, H.; Eichler, D.; Adam, P.; Bonnomet, F. Early mechanical complications following fixation of proximal femur fractures: From prevention to treatment. Orthop. Traumatol. Surg. Res. 2020, 106, S79–S87. [Google Scholar] [CrossRef] [PubMed]
- Bovbjerg, P.E.; Larsen, M.S.; Madsen, C.F.; Schønnemann, J. Failure of short versus long cephalomedullary nail after intertrochanteric fractures. J. Orthop. 2020, 18, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, I.; Appleton, P.T.; Wixted, J.J.; DeAngelis, J.P.; Rodriguez, E.K. Implant cut-out following cephalomedullary nailing of intertrochanteric femur fractures: Are helical blades to blame? Injury 2019, 50, 926–930. [Google Scholar] [CrossRef] [PubMed]
- Aktselis, I.; Papadimas, D.; Fragkomichalos, E.; Deligeorgis, A.; Kokoroghiannis, C. Intramedullary nailing of trochanteric fractures--operative technical tips. Injury 2012, 43, 961–965. [Google Scholar] [CrossRef]
- Mereddy, P.; Kamath, S.; Ramakrishnan, M.; Malik, H.; Donnachie, N. The AO/ASIF proximal femoral nail antirotation (PFNA): A new design for the treatment of unstable proximal femoral fractures. Injury 2009, 40, 428–432. [Google Scholar] [CrossRef]
- Li, S.; Chang, S.M.; Niu, W.X.; Ma, H. Comparison of tip apex distance and cut-out complications between helical blades and lag screws in intertrochanteric fractures among the elderly: A meta-analysis. J. Orthop. Sci. 2015, 20, 1062–1069. [Google Scholar] [CrossRef]
- Cleveland, M.; Bosworth, D.M.; Thompson, F.R.; Wilson, H.J., Jr.; Ishizuka, T. A ten-year analysis of intertrochanteric fractures of the femur. J. Bone Jt. Surg. Am. 1959, 41-A, 1399–1408. [Google Scholar] [CrossRef]
- Turgut, A.; Kalenderer, O.; Karapinar, L.; Kumbaraci, M.; Akkan, H.A.; Agus, H. Which factor is most important for occurrence of cutout complications in patients treated with proximal femoral nail antirotation? Retrospective analysis of 298 patients. Arch. Orthop. Trauma Surg. 2016, 136, 623–630. [Google Scholar] [CrossRef]
- Lopes-Coutinho, L.; Dias-Carvalho, A.; Esteves, N.; Sousa, R. Traditional distance “tip-apex” vs. new calcar referenced “tip-apex”—which one is the best peritrochanteric osteosynthesis failure predictor? Injury 2020, 51, 674–677. [Google Scholar] [CrossRef]
- Parker, M.; Raval, P.; Gjertsen, J.E. Nail or plate fixation for A3 trochanteric hip fractures: A systematic review of randomised controlled trials. Inj.-Int. J. Care Inj. 2018, 49, 1319–1323. [Google Scholar] [CrossRef] [PubMed]
- Khan, W.; Williams, R.; Hopwood, S.; Agarwal, S. Combined Intracapsular And Extracapsular Neck Of Femur Fractures Case Series, Literature Review And Management Recommendations. Open Orthop. J. 2017, 11, 600–608. [Google Scholar] [CrossRef] [PubMed]
- Ikuta, Y.; Nagata, Y.; Iwasaki, Y. Preoperative radiographic features of trochanteric fractures irreducible by closed reduction. Injury 2019, 50, 2014–2021. [Google Scholar] [CrossRef]
- Enocson, A.; Lapidus, L.J. The vertical hip fracture—A treatment challenge. A cohort study with an up to 9 year follow-up of 137 consecutive hips treated with sliding hip screw and antirotation screw. BMC Musculoskelet. Disord. 2012, 13, 171. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.E.; Shih, C.M.; Wang, C.C.; Huang, K.C. Lateral femoral wall thickness: A reliable predictor of post-operative lateral wall fracture in intertrochanteric fractures. Bone Jt. J. 2013, 95-B, 1134–1138. [Google Scholar] [CrossRef] [PubMed]
- Metsemakers, W.J.; Morgenstern, M.; McNally, M.A.; Moriarty, T.F.; McFadyen, I.; Scarborough, M.; Athanasou, N.A.; Ochsner, P.E.; Kuehl, R.; Raschke, M.; et al. Fracture-related infection: A consensus on definition from an international expert group. Injury 2018, 49, 505–510. [Google Scholar] [CrossRef]
- Tarazona-Santabalbina, F.J.; Ojeda-Thies, C.; Figueroa Rodríguez, J.; Cassinello-Ogea, C.; Caeiro, J.R. Orthogeriatric Management: Improvements in Outcomes during Hospital Admission Due to Hip Fracture. Int. J. Environ. Res. Public Health 2021, 18, 3049. [Google Scholar] [CrossRef]
- Jensen, J.S. Classification of trochanteric fractures. Acta Orthop. Scand. 1980, 51, 803–810. [Google Scholar] [CrossRef]
- Marsh, J.L.; Slongo, T.F.; Agel, J.; Broderick, J.S.; Creevey, W.; DeCoster, T.A.; Prokuski, L.; Sirkin, M.S.; Ziran, B.; Henley, B.; et al. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J. Orthop. Trauma 2007, 21, S1–S133. [Google Scholar] [CrossRef]
- Massoud, E.I. Fixation of basicervical and related fractures. Int. Orthop. 2010, 34, 577–582. [Google Scholar] [CrossRef]
- Fogagnolo, F.; Kfuri, M.; Paccola, C.A. Intramedullary fixation of pertrochanteric hip fractures with the short AO-ASIF proximal femoral nail. Arch. Orthop. Trauma Surg. 2004, 124, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.R.; Kim, S.T.; Yoon, M.G.; Moon, M.S.; Heo, J.H. The stability score of the intramedullary nailed intertrochanteric fractures: Stability of nailed fracture and postoperative patient mobilization. Clin. Orthop. Surg. 2013, 5, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Pascual, C.; Santos-Sánchez, J.; García-González, J.M.; Silva-Viamonte, C.F.; Pablos-Hernández, C.; Ramos-Pascua, L.; Mirón-Canelo, J.A. Long-term outcomes of distal locking in extracapsular fractures treated with trochanteric Gamma3 nails. J. Orthop. Traumatol. 2021, 22, 48. [Google Scholar] [CrossRef]
- Mahoney, F.; Barthel, D. Functional Evaluation: The Barhel index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Martínez de la Iglesia, J.; Dueñas Herrero, R.; Onís Vilches, M.C.; Aguado Taberné, C.; Albert Colomer, C.; Luque Luque, R. Spanish language adaptation and validation of the Pfeiffer’s questionnaire (SPMSQ) to detect cognitive deterioration in people over 65 years of age. Med. Clin. 2001, 117, 129–134. [Google Scholar] [CrossRef]
- Nuti, R.; Brandi, M.L.; Isaia, G.; Tarantino, U.; Silvestri, S.; Adami, S. New perspectives on the definition and the management of severe osteoporosis: The patient with two or more fragility fractures. J. Endocrinol. Investig. 2009, 32, 783–788. [Google Scholar] [CrossRef]
- Fitz-Henry, J. The ASA classification and peri-operative risk. Ann. R. Coll. Surg. Engl. 2011, 93, 185–187. [Google Scholar] [CrossRef]
- Horner, N.S.; Samuelsson, K.; Solyom, J.; Bjørgul, K.; Ayeni, O.R.; Östman, B. Implant-Related Complications and Mortality After Use of Short or Long Gamma Nail for Intertrochanteric and Subtrochanteric Fractures: A Prospective Study with Minimum 13-Year Follow-up. JB JS Open Access 2017, 2, e0026. [Google Scholar] [CrossRef]
- Chehade, M.J.; Carbone, T.; Awward, D.; Taylor, A.; Wildenauer, C.; Ramasamy, B.; McGee, M. Influence of Fracture Stability on Early Patient Mortality and Reoperation After Pertrochanteric and Intertrochanteric Hip Fractures. J. Orthop. Trauma 2015, 29, 538–543. [Google Scholar] [CrossRef]
- Bonnaire, F.; Weber, A.; Bösl, O.; Eckhardt, C.; Schwieger, K.; Linke, B. “Cutting out” in pertrochanteric fractures—problem of osteoporosis? Unfallchirurg 2007, 110, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Lorich, D.G.; Geller, D.S.; Nielson, J.H. Osteoporotic pertrochanteric hip fractures: Management and current controversies. Instr. Course Lect. 2004, 53, 441–454. [Google Scholar] [CrossRef] [PubMed]
- Elliot-Gibson, V.; Bogoch, E.R.; Jamal, S.A.; Beaton, D.E. Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: A systematic review. Osteoporos. Int. 2004, 15, 767–778. [Google Scholar] [CrossRef] [PubMed]
- Lizano-Díez, X.; Keel, M.J.B.; Siebenrock, K.A.; Tey, M.; Bastian, J.D. Rehabilitation protocols in unstable trochanteric fractures treated with cephalomedullary nails in elderly: Current practices and outcome. Eur. J. Trauma Emerg. Surg. 2020, 46, 1267–1280. [Google Scholar] [CrossRef]
- Li, J.; Zhang, L.; Zhang, H.; Yin, P.; Lei, M.; Wang, G.; Wang, S.; Tang, P. Effect of reduction quality on post-operative outcomes in 31-A2 intertrochanteric fractures following intramedullary fixation: A retrospective study based on computerised tomography findings. Int. Orthop. 2019, 43, 1951–1959. [Google Scholar] [CrossRef]
- De Bruijn, K.; den Hartog, D.; Tuinebreijer, W.; Roukema, G. Reliability of predictors for screw cutout in intertrochanteric hip fractures. J. Bone Jt. Surg. Am. 2012, 94, 1266–1272. [Google Scholar] [CrossRef]
- Murena, L.; Moretti, A.; Meo, F.; Saggioro, E.; Barbati, G.; Ratti, C.; Canton, G. Predictors of cut-out after cephalomedullary nail fixation of pertrochanteric fractures: A retrospective study of 813 patients. Arch. Orthop. Trauma Surg. 2018, 138, 351–359. [Google Scholar] [CrossRef]
- Haidukewych, G.J. Intertrochanteric fractures: Ten tips to improve results. J. Bone Jt. Surg. Am. 2009, 91, 712–719. [Google Scholar]
- Meinberg, E.G.; Agel, J.; Roberts, C.S.; Karam, M.D.; Kellam, J.F. Fracture and Dislocation Classification Compendium-2018. J. Orthop. Trauma 2018, 32 (Suppl. S1), S1–S170. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).