Long-Term Effects of Ambient Particulate and Gaseous Pollutants on Serum High-Sensitivity C-Reactive Protein Levels: A Cross-Sectional Study Using KoGES-HEXA Data
Abstract
1. Introduction
2. Materials and Methods
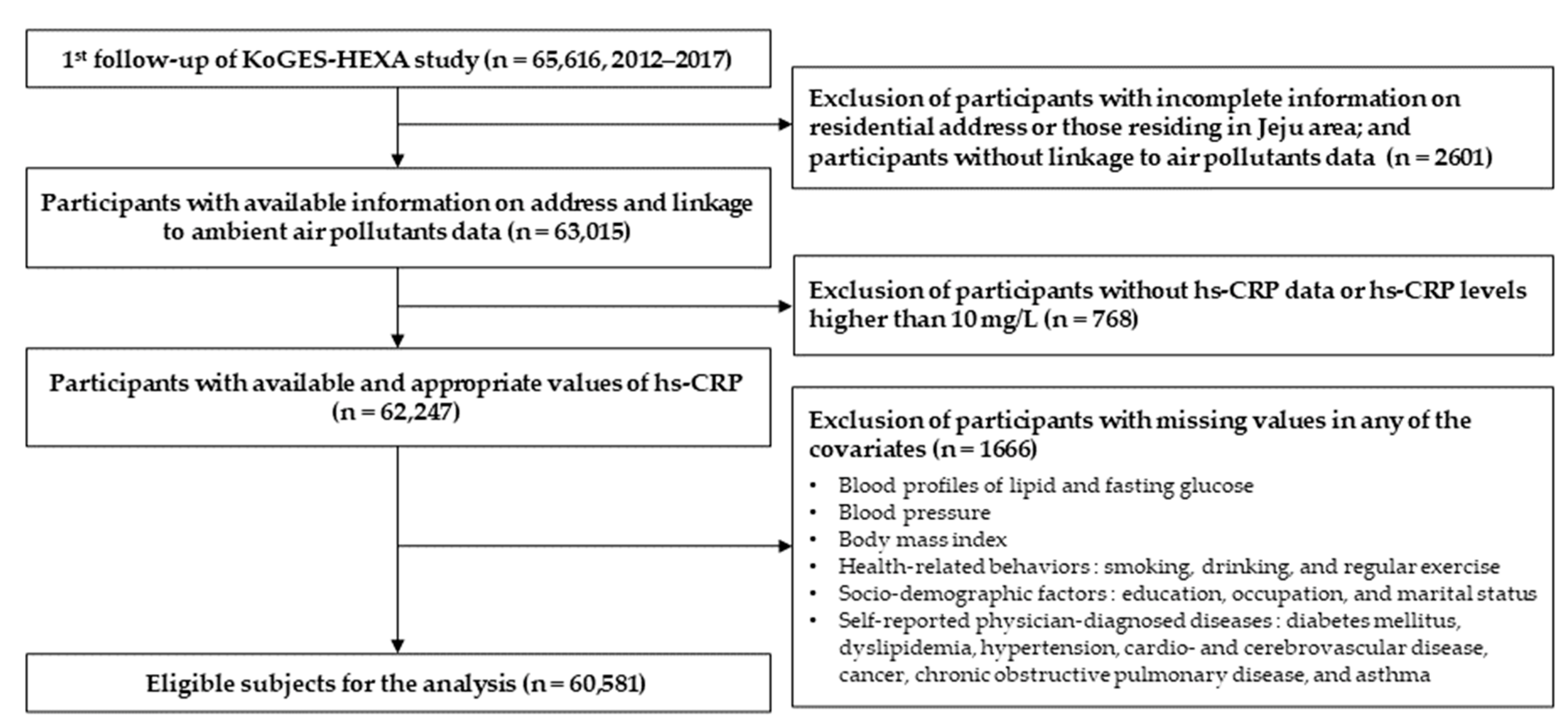
2.1. Study Population
2.2. Participant Selection
2.3. Ambient Air Pollution and Meteorological Factors
- Geographic estimation of air pollution and meteorological factors
- Geocoding of the study participants
- Merging the estimated air pollution and meteorological data with the participants
2.4. Inflammatory Marker
2.5. Covariates
2.6. Statistical Analyses
3. Results
3.1. Study Population
3.2. Air Pollutants
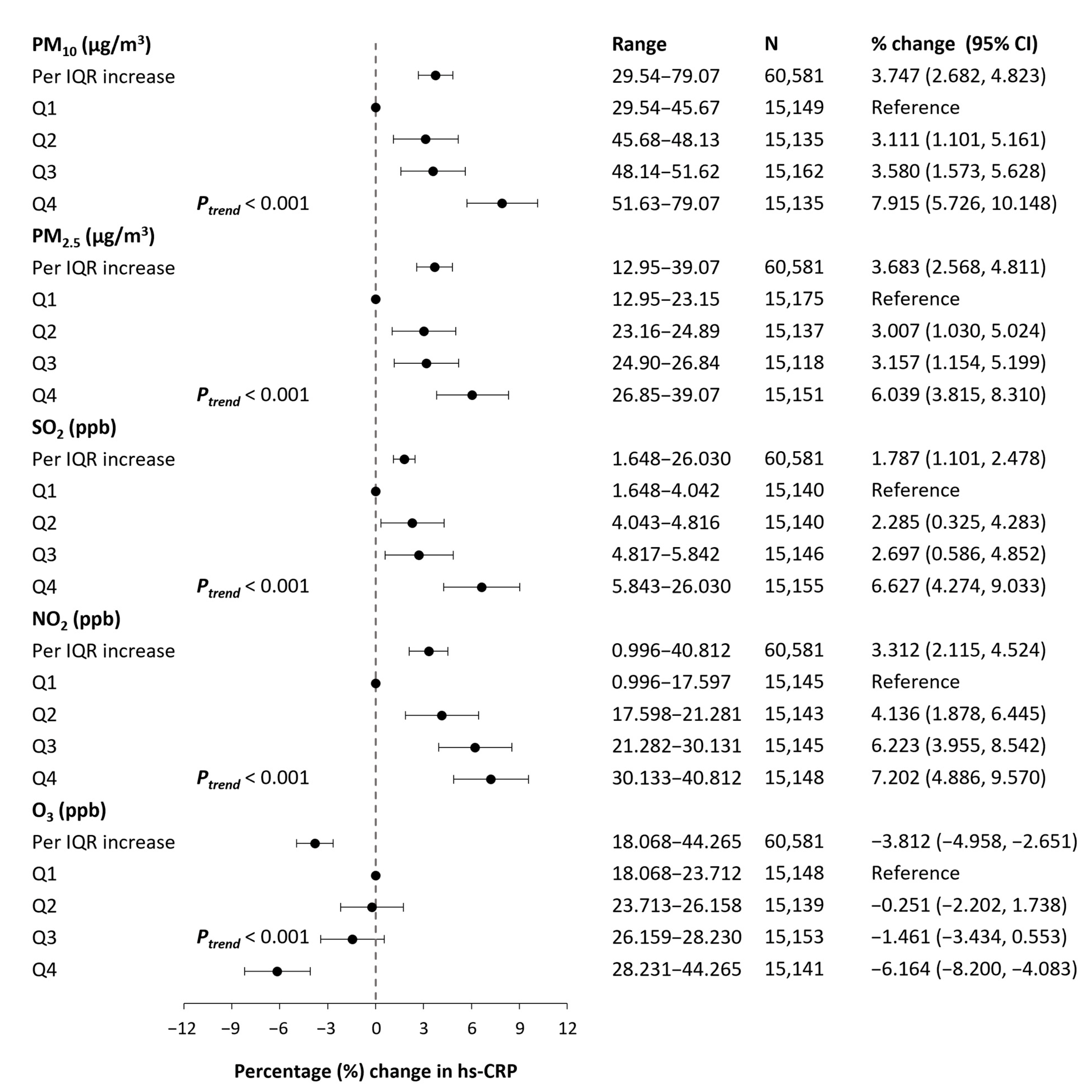
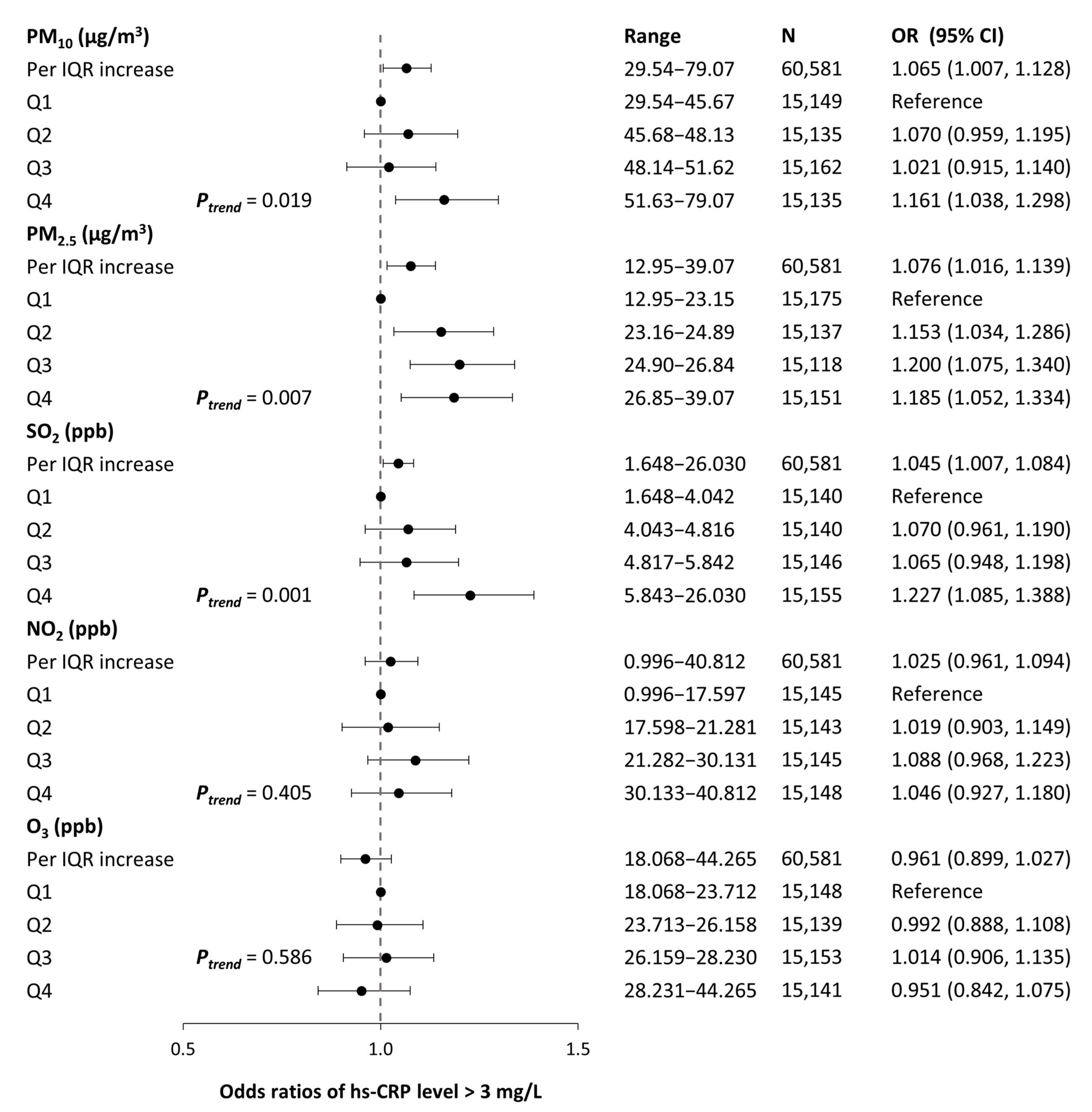
3.3. Effects of Long-Term Exposure to Air Pollutants on Inflammatory Markers
3.4. Sensitivity Analyses
4. Discussion
4.1. Summary
4.2. Comparisons of Findings
4.3. Sensitivity Analyses on Effect Modifications
4.4. Sensitivity Analyses on Extended Models including Short-Term Measures and Co-Pollutants
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Ambient Air Pollution: A global Assessment of Exposure and Burden of Disease. 2016. Available online: https://apps.who.int/iris/handle/10665/250141 (accessed on 20 February 2022).
- Cohen, A.J.; Brauer, M.; Burnett, R.; Anderson, H.R.; Frostad, J.; Estep, K.; Balakrishnan, K.; Brunekreef, B.; Dandona, L.; Dandona, R. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the Global Burden of Diseases Study 2015. Lancet 2017, 389, 1907–1918. [Google Scholar] [CrossRef]
- Stanaway, J.D.; Afshin, A.; Gakidou, E.; Lim, S.S.; Abate, D.; Abate, K.H.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd Allah, F. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef]
- Cohen, A.J.; Ross Anderson, H.; Ostro, B.; Pandey, K.D.; Krzyzanowski, M.; Künzli, N.; Gutschmidt, K.; Pope, A.; Romieu, I.; Samet, J.M. The global burden of disease due to outdoor air pollution. J. Toxicol. Environ. Health A 2005, 68, 1301–1307. [Google Scholar] [CrossRef] [PubMed]
- Burnett, R.; Chen, H.; Szyszkowicz, M.; Fann, N.; Hubbell, B.; Pope, C.A.; Apte, J.S.; Brauer, M.; Cohen, A.; Weichenthal, S. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc. Natl. Acad. Sci. USA 2018, 115, 9592–9597. [Google Scholar] [CrossRef] [PubMed]
- Franklin, B.A.; Brook, R.; Pope III, C.A. Air pollution and cardiovascular disease. Curr. Probl. Cardiol. 2015, 40, 207–238. [Google Scholar] [CrossRef]
- Kelly, F.; Fussell, J. Air pollution and airway disease. Clin. Exp. Allergy 2011, 41, 1059–1071. [Google Scholar] [CrossRef]
- Block, M.L.; Calderón Garcidueñas, L. Air pollution: Mechanisms of neuroinflammation and CNS disease. Trends Neurosci. 2009, 32, 506–516. [Google Scholar] [CrossRef]
- Arias Pérez, R.D.; Taborda, N.A.; Gómez, D.M.; Narvaez, J.F.; Porras, J.; Hernandez, J.C. Inflammatory effects of particulate matter air pollution. Environ. Sci. Pollut. Res. 2020, 27, 42390–42404. [Google Scholar] [CrossRef]
- Fiorito, G.; Vlaanderen, J.; Polidoro, S.; Gulliver, J.; Galassi, C.; Ranzi, A.; Krogh, V.; Grioni, S.; Agnoli, C.; Sacerdote, C. Oxidative stress and inflammation mediate the effect of air pollution on cardio-and cerebrovascular disease: A prospective study in nonsmokers. Environ. Mol. Mutagen. 2018, 59, 234–246. [Google Scholar] [CrossRef]
- Van Eeden, S.F.; Tan, W.C.; Suwa, T.; Mukae, H.; Terashima, T.; Fujii, T.; Qui, D.; Vincent, R.; Hogg, J.C. Cytokines involved in the systemic inflammatory response induced by exposure to particulate matter air pollutants (PM10). Am. J. Respir. Crit. Care Med. 2001, 164, 826–830. [Google Scholar] [CrossRef]
- Stoner, L.; Lucero, A.A.; Palmer, B.R.; Jones, L.M.; Young, J.M.; Faulkner, J. Inflammatory biomarkers for predicting cardiovascular disease. Clin. Biochem. 2013, 46, 1353–1371. [Google Scholar] [CrossRef] [PubMed]
- Pearson, T.A.; Mensah, G.A.; Alexander, R.W.; Anderson, J.L.; Cannon III, R.O.; Criqui, M.; Fadl, Y.Y.; Fortmann, S.P.; Hong, Y.; Myers, G.L. Markers of inflammation and cardiovascular disease: Application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 2003, 107, 499–511. [Google Scholar] [CrossRef] [PubMed]
- Pilz, V.; Wolf, K.; Breitner, S.; Rückerl, R.; Koenig, W.; Rathmann, W.; Cyrys, J.; Peters, A.; Schneider, A.; for the KORA-Study Group. C-reactive protein (CRP) and long-term air pollution with a focus on ultrafine particles. Int. J. Hyg. Environ. Health 2018, 221, 510–518. [Google Scholar] [CrossRef] [PubMed]
- Castro, A.R.; Silva, S.O.; Soares, S.C. The use of high sensitivity C-reactive protein in cardiovascular disease detection. J. Pharm. Pharm. Sci. 2018, 21, 496–503. [Google Scholar] [CrossRef]
- Ito, F.; Sono, Y.; Ito, T. Measurement and clinical significance of lipid peroxidation as a biomarker of oxidative stress: Oxidative stress in diabetes, atherosclerosis, and chronic inflammation. Antioxidants 2019, 8, 72. [Google Scholar] [CrossRef]
- Liu, Q.; Gu, X.; Deng, F.; Mu, L.; Baccarelli, A.A.; Guo, X.; Wu, S. Ambient particulate air pollution and circulating C-reactive protein level: A systematic review and meta-analysis. Int. J. Hyg. Environ. Health 2019, 222, 756–764. [Google Scholar] [CrossRef]
- Xu, Z.; Wang, W.; Liu, Q.; Li, Z.; Lei, L.; Ren, L.; Deng, F.; Guo, X.; Wu, S. Association between gaseous air pollutants and biomarkers of systemic inflammation: A systematic review and meta-analysis. Environ. Pollut. 2022, 292, 118336. [Google Scholar] [CrossRef]
- Koenig, W. Update on C-reactive protein as a risk marker in cardiovascular disease. Kidney Int. 2003, 63, S58–S61. [Google Scholar] [CrossRef]
- Huttunen, K.; Siponen, T.; Salonen, I.; Yli-Tuomi, T.; Aurela, M.; Dufva, H.; Hillamo, R.; Linkola, E.; Pekkanen, J.; Pennanen, A. Low-level exposure to ambient particulate matter is associated with systemic inflammation in ischemic heart disease patients. Environ. Res. 2012, 116, 44–51. [Google Scholar] [CrossRef]
- Wang, X.Y.; Hu, W.; Tong, S. Long-term exposure to gaseous air pollutants and cardio-respiratory mortality in Brisbane, Australia. Geospat. Health 2009, 3, 257–263. [Google Scholar] [CrossRef]
- Hwang, M.J.; Sung, J.; Yoon, M.; Kim, J.H.; Yun, H.Y.; Choi, D.R.; Koo, Y.S.; Oh, K.; Yun, S.; Cheong, H.K. Establishment of the Korea National Health and Nutrition Examination Survey air pollution study dataset for the researchers on the health impact of ambient air pollution. Epidemiol. Health 2021, 43, e2021015. [Google Scholar] [CrossRef] [PubMed]
- Hoek, G. Methods for assessing long-term exposures to outdoor air pollutants. Curr. Environ. Health Rep. 2017, 4, 450–462. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Myung, W.; Jeong, B.H.; Choi, H.; Jhun, B.W.; Kim, H. Short-and long-term exposure to ambient air pollution and circulating biomarkers of inflammation in non-smokers: A hospital-based cohort study in South Korea. Environ. Int. 2018, 119, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Han, B.G.; Group, K. Cohort profile: The Korean genome and epidemiology study (KoGES) consortium. Int. J. Epidemiol. 2017, 46, e20. [Google Scholar] [CrossRef]
- Kim, H.J.; Min, J.Y.; Seo, Y.S.; Min, K.B. Association between exposure to ambient air pollution and renal function in Korean adults. Ann. Occup. Environ. Med. 2018, 30, 14. [Google Scholar] [CrossRef]
- Koo, Y.S.; Choi, D.R.; Yun, H.Y.; Yoon, G.W.; Lee, J.B. A Development of PM Concentration Reanalysis Method using CMAQ with Surface Data Assimilation and MAIAC AOD in Korea. J. Korean Soc. Atmos. 2020, 36, 558–573. [Google Scholar] [CrossRef]
- Oudin, A.; Forsberg, B.; Strömgren, M.; Beelen, R.; Modig, L. Impact of residential mobility on exposure assessment in longitudinal air pollution studies: A sensitivity analysis within the ESCAPE project. Sci. World J. 2012, 2012. [Google Scholar] [CrossRef]
- Aretz, B.; Janssen, F.; Vonk, J.M.; Heneka, M.T.; Boezen, H.M.; Doblhammer, G. Long-term exposure to fine particulate matter, lung function and cognitive performance: A prospective Dutch cohort study on the underlying routes. Environ. Res. 2021, 201, 111533. [Google Scholar] [CrossRef]
- Jiang, M.; Kim, E.; Woo, Y. The relationship between economic growth and air pollution-a regional comparison between China and South Korea. Int. J. Environ. Res. Public Health 2020, 17, 2761. [Google Scholar] [CrossRef]
- Cho, S.M.J.; Lee, H.; Lee, H.H.; Baek, J.; Heo, J.E.; Joo, H.J.; Hong, S.J.; Kim, H.C. Dyslipidemia fact sheets in Korea 2020: An analysis of nationwide population-based data. J. Lipid Atheroscler. 2021, 10, 202–209. [Google Scholar] [CrossRef]
- World Health Organization Regional Office for the Western Pacific. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. 2000. Available online: https://apps.who.int/iris/handle/10665/206936 (accessed on 20 February 2022).
- Tolbert, P.E.; Klein, M.; Peel, J.L.; Sarnat, S.E.; Sarnat, J.A. Multipollutant modeling issues in a study of ambient air quality and emergency department visits in Atlanta. J. Expo. Sci. Environ. Epidemiol. 2007, 17, S29–S35. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Global Air Quality Guidelines. Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide. Licence: CC BY-NC-SA 3.0 IGO. 2021. Available online: https://www.who.int/publications/i/item/9789240034228 (accessed on 20 February 2022).
- Trnka, D. Policies, regulatory framework and enforcement for air quality management: The case of Korea. OECD Environ. Work Pap. 2020, 158. [Google Scholar] [CrossRef]
- Ryou, H.G.; Heo, J.; Kim, S.Y. Source apportionment of PM10 and PM2.5 air pollution, and possible impacts of study characteristics in South Korea. Environ. Pollut. 2018, 240, 963–972. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.H.; Yen, T.H.; Chan, M.J.; Su, Y.J. Environmental carbon monoxide level is associated with the level of high-sensitivity C-reactive protein in peritoneal dialysis patients. Medicine 2014, 93, e181. [Google Scholar] [CrossRef]
- Viehmann, A.; Hertel, S.; Fuks, K.; Eisele, L.; Moebus, S.; Möhlenkamp, S.; Nonnemacher, M.; Jakobs, H.; Erbel, R.; Jöckel, K.H. Long-term residential exposure to urban air pollution, and repeated measures of systemic blood markers of inflammation and coagulation. Occup. Environ. Med. 2015, 72, 656–663. [Google Scholar] [CrossRef]
- Wolf, K.; Popp, A.; Schneider, A.; Breitner, S.; Hampel, R.; Rathmann, W.; Herder, C.; Roden, M.; Koenig, W.; Meisinger, C. Association between long-term exposure to air pollution and biomarkers related to insulin resistance, subclinical inflammation, and adipokines. Diabetes 2016, 65, 3314–3326. [Google Scholar] [CrossRef]
- Adebayo Ojo, T.C.; Wichmann, J.; Arowosegbe, O.O.; Probst Hensch, N.; Schindler, C.; Künzli, N. Short-Term Joint Effects of PM10, NO2 and SO2 on Cardio-Respiratory Disease Hospital Admissions in Cape Town, South Africa. Int. J. Environ. Res. Public Health 2022, 19, 495. [Google Scholar] [CrossRef]
- Forbes, L.J.; Patel, M.D.; Rudnicka, A.R.; Cook, D.G.; Bush, T.; Stedman, J.R.; Whincup, P.H.; Strachan, D.P.; Anderson, R.H. Chronic exposure to outdoor air pollution and markers of systemic inflammation. Epidemiology 2009, 20, 245–253. [Google Scholar] [CrossRef]
- Liu, K.; Cao, H.; Li, B.; Guo, C.; Zhao, W.; Han, X.; Zhang, H.; Wang, Z.; Tang, N.; Niu, K. Long-term exposure to ambient nitrogen dioxide and ozone modifies systematic low-grade inflammation: The CHCN-BTH study. Int. J. Hyg. Environ. Health 2022, 239, 113875. [Google Scholar] [CrossRef]
- Nuvolone, D.; Petri, D.; Voller, F. The effects of ozone on human health. Environ. Sci. Pollut. Res. Int. 2018, 25, 8074–8088. [Google Scholar] [CrossRef]
- Day, D.B.; Xiang, J.; Mo, J.; Li, F.; Chung, M.; Gong, J.; Weschler, C.J.; Ohman Strickland, P.A.; Sundell, J.; Weng, W. Association of ozone exposure with cardiorespiratory pathophysiologic mechanisms in healthy adults. JAMA Intern. Med. 2017, 177, 1344–1353. [Google Scholar] [CrossRef] [PubMed]
- Zhao, T.; Markevych, I.; Standl, M.; Schikowski, T.; Berdel, D.; Koletzko, S.; Jörres, R.A.; Nowak, D.; Heinrich, J. Short-term exposure to ambient ozone and inflammatory biomarkers in cross-sectional studies of children and adolescents: Results of the GINIplus and LISA birth cohorts. Environ. Pollut. 2019, 255, 113264. [Google Scholar] [CrossRef] [PubMed]
- Simoni, M.; Baldacci, S.; Maio, S.; Cerrai, S.; Sarno, G.; Viegi, G. Adverse effects of outdoor pollution in the elderly. J. Thorac. Dis. 2015, 7, 34–45. [Google Scholar] [CrossRef]
- Boss, G.R.; Seegmiller, J.E. Age-related physiological changes and their clinical significance. West. J. Med. 1981, 135, 434–440. [Google Scholar]
- Elbarbary, M.; Oganesyan, A.; Honda, T.; Morgan, G.; Guo, Y.; Guo, Y.; Negin, J. Systemic inflammation (C-Reactive Protein) in older Chinese adults is associated with long-term exposure to ambient air pollution. Int. J. Environ. Res. Public Health 2021, 18, 3258. [Google Scholar] [CrossRef] [PubMed]
- Dubowsky, S.D.; Suh, H.; Schwartz, J.; Coull, B.A.; Gold, D.R. Diabetes, obesity, and hypertension may enhance associations between air pollution and markers of systemic inflammation. Environ. Health Perspect. 2006, 114, 992–998. [Google Scholar] [CrossRef] [PubMed]
- Ruckerl, R.; Ibald-Mulli, A.; Koenig, W.; Schneider, A.; Woelke, G.; Cyrys, J.; Heinrich, J.; Marder, V.; Frampton, M.; Wichmann, H.E. Air pollution and markers of inflammation and coagulation in patients with coronary heart disease. Am. J. Respir. Crit. Care Med. 2006, 173, 432–441. [Google Scholar] [CrossRef]
- Dadvand, P.; Nieuwenhuijsen, M.J.; Agustí, À.; De Batlle, J.; Benet, M.; Beelen, R.; Cirach, M.; Martinez, D.; Hoek, G.; Basagaña, X. Air pollution and biomarkers of systemic inflammation and tissue repair in COPD patients. Eur. Respir. J. 2014, 44, 603–613. [Google Scholar] [CrossRef]
- Ostro, B.; Malig, B.; Broadwin, R.; Basu, R.; Gold, E.B.; Bromberger, J.T.; Derby, C.; Feinstein, S.; Greendale, G.A.; Jackson, E.A. Chronic PM2.5 exposure and inflammation: Determining sensitive subgroups in mid-life women. Environ. Res. 2014, 132, 168–175. [Google Scholar] [CrossRef]
- Oliveira, M.S.d.; Leon, A.P.d.; Mattos, I.E.; Koifman, S. Differential susceptibility according to gender in the association between air pollution and mortality from respiratory diseases. Cad. Saude Publica 2011, 27, 1827–1836. [Google Scholar] [CrossRef]
- Lee, J.; Taneja, V.; Vassallo, R. Cigarette smoking and inflammation: Cellular and molecular mechanisms. J. Dent. Res. 2012, 91, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Yanbaeva, D.G.; Dentener, M.A.; Creutzberg, E.C.; Wesseling, G.; Wouters, E.F. Systemic effects of smoking. Chest 2007, 131, 1557–1566. [Google Scholar] [CrossRef] [PubMed]
- Turner, M.C.; Cohen, A.; Burnett, R.T.; Jerrett, M.; Diver, W.R.; Gapstur, S.M.; Krewski, D.; Samet, J.M.; Pope III, C.A. Interactions between cigarette smoking and ambient PM2.5 for cardiovascular mortality. Environ. Res. 2017, 154, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Hajat, A.; Allison, M.; Diez Roux, A.V.; Jenny, N.S.; Jorgensen, N.W.; Szpiro, A.A.; Vedal, S.; Kaufman, J.D. Long-term exposure to air pollution and markers of inflammation, coagulation, and endothelial activation: A repeat-measures analysis in the Multi-Ethnic Study of Atherosclerosis (MESA). Epidemiology 2015, 26, 310–320. [Google Scholar] [CrossRef] [PubMed]
- Dabass, A.; Talbott, E.O.; Venkat, A.; Rager, J.; Marsh, G.M.; Sharma, R.K.; Holguin, F. Association of exposure to particulate matter (PM2.5) air pollution and biomarkers of cardiovascular disease risk in adult NHANES participants (2001–2008). Int. J. Hyg. Environ. Health 2016, 219, 301–310. [Google Scholar] [CrossRef]
- Baccarelli, A.; Zanobetti, A.; Martinelli, I.; Grillo, P.; Hou, L.; Lanzani, G.; Mannucci, P.M.; Bertazzi, P.A.; Schwartz, J. Air pollution, smoking, and plasma homocysteine. Environ. Health Perspect. 2007, 115, 176–181. [Google Scholar] [CrossRef]
- Panasevich, S.; Leander, K.; Rosenlund, M.; Ljungman, P.; Bellander, T.; de Faire, U.; Pershagen, G.; Nyberg, F. Associations of long-and short-term air pollution exposure with markers of inflammation and coagulation in a population sample. Occup. Environ. Med. 2009, 66, 747–753. [Google Scholar] [CrossRef]
- Hoffmann, B.; Moebus, S.; Dragano, N.; Stang, A.; Möhlenkamp, S.; Schmermund, A.; Memmesheimer, M.; Bröcker Preuss, M.; Mann, K.; Erbel, R. Chronic residential exposure to particulate matter air pollution and systemic inflammatory markers. Environ. Health Perspect. 2009, 117, 1302–1308. [Google Scholar] [CrossRef]
- Zhang, Z.; Hoek, G.; Chang, L.Y.; Chan, T.C.; Guo, C.; Chuang, Y.C.; Chan, J.; Lin, C.; Jiang, W.K.; Guo, Y. Particulate matter air pollution, physical activity and systemic inflammation in Taiwanese adults. Int. J. Hyg. Environ. Health 2018, 221, 41–47. [Google Scholar] [CrossRef]
- Kim, S.R.; Choi, S.; Keum, N.N.; Park, S.M. Combined effects of physical activity and air pollution on cardiovascular disease: A population-based study. J. Am. Heart Assoc. 2020, 9, e013611. [Google Scholar] [CrossRef]
- Tainio, M.; de Nazelle, A.J.; Götschi, T.; Kahlmeier, S.; Rojas-Rueda, D.; Nieuwenhuijsen, M.J.; de Sá, T.H.; Kelly, P.; Woodcock, J. Can air pollution negate the health benefits of cycling and walking? Prev. Med. 2016, 87, 233–236. [Google Scholar] [CrossRef] [PubMed]
- An, R.; Ji, M.; Yan, H.; Guan, C. Impact of ambient air pollution on obesity: A systematic review. Int. J. Obes. 2018, 42, 1112–1126. [Google Scholar] [CrossRef] [PubMed]
- Hennig, F.; Fuks, K.; Moebus, S.; Weinmayr, G.; Memmesheimer, M.; Jakobs, H.; Bröcker Preuss, M.; Führer Sakel, D.; Möhlenkamp, S.; Erbel, R. Association between source-specific particulate matter air pollution and hs-CRP: Local traffic and industrial emissions. Environ. Health Perspect. 2014, 122, 703–710. [Google Scholar] [CrossRef] [PubMed]
- Billionnet, C.; Sherrill, D.; Annesi Maesano, I. Estimating the health effects of exposure to multi-pollutant mixture. Ann. Epidemiol. 2012, 22, 126–141. [Google Scholar] [CrossRef]
- Vedal, S.; Kaufman, J.D. What does multi-pollutant air pollution research mean? Am. J. Respir. Crit. Care Med. 2011, 183, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Dominici, F.; Peng, R.D.; Barr, C.D.; Bell, M.L. Protecting human health from air pollution: Shifting from a single-pollutant to a multi-pollutant approach. Epidemiology 2010, 21, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Q.; Liu, Y.; Mulholland, J.A.; Russell, A.G.; Darrow, L.A.; Tolbert, P.E.; Strickland, M.J. Pediatric emergency department visits and ambient Air pollution in the US State of Georgia: A case-crossover study. Environ. Health 2016, 15, 115. [Google Scholar] [CrossRef]
- Sarnat, J.A.; Schwartz, J.; Catalano, P.J.; Suh, H.H. Gaseous pollutants in particulate matter epidemiology: Confounders or surrogates? Environ. Health Perspect. 2001, 109, 1053–1061. [Google Scholar] [CrossRef]
- Zijlema, W.L.; Smidt, N.; Klijs, B.; Morley, D.W.; Gulliver, J.; de Hoogh, K.; Scholtens, S.; Rosmalen, J.G.; Stolk, R.P. The LifeLines Cohort Study: A resource providing new opportunities for environmental epidemiology. Arch. Public Health 2016, 74, 32. [Google Scholar] [CrossRef]
- Song, J.; Zhu, J.; Tian, G.; Li, H.; Li, H.; An, Z.; Jiang, J.; Fan, W.; Wang, G.; Zhang, Y. Short time exposure to ambient ozone and associated cardiovascular effects: A panel study of healthy young adults. Environ. Int. 2020, 137, 105579. [Google Scholar] [CrossRef]
- Armstrong, B.G. Effect of measurement error on epidemiological studies of environmental and occupational exposures. Occup. Environ. Med. 1998, 55, 651–656. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Qiu, X.; Yazdi, M.D.; Shtein, A.; Shi, L.; Yang, J.; Peralta, A.A.; Coull, B.A.; Schwartz, J.D. The impact of exposure measurement error on the estimated concentration–response relationship between long-term exposure to PM2.5 and mortality. Environ. Health Perspect. 2022, 130, 077006. [Google Scholar] [CrossRef] [PubMed]
- Hao, H.; Chang, H.H.; Holmes, H.A.; Mulholland, J.A.; Klein, M.; Darrow, L.A.; Strickland, M.J. Air pollution and preterm birth in the US state of Georgia (2002–2006): Associations with concentrations of 11 ambient air pollutants estimated by combining Community Multiscale Air Quality Model (CMAQ) simulations with stationary monitor measurements. Environ. Health Perspect. 2016, 124, 875–880. [Google Scholar] [CrossRef] [PubMed]
- Senthilkumar, N.; Gilfether, M.; Metcalf, F.; Russell, A.G.; Mulholland, J.A.; Chang, H.H. Application of a fusion method for gas and particle air pollutants between observational data and chemical transport model simulations over the contiguous United States for 2005–2014. Int. J. Environ. Res. Public Health 2019, 16, 3314. [Google Scholar] [CrossRef]
- Hu, Y.; Zang, Z.; Chen, D.; Ma, X.; Liang, Y.; You, W.; Pan, X.; Wang, L.; Wang, D.; Zhang, Z. Optimization and evaluation of SO2 emissions based on WRF-Chem and 3DVAR data assimilation. Remote Sens. 2022, 14, 220. [Google Scholar] [CrossRef]
| Characteristics | Total (n = 60,581) | Hs-CRP ≤ 3 mg/L (n = 57,630) | Hs-CRP > 3 mg/L (n = 2951) | p-Value a |
|---|---|---|---|---|
| Age [years (mean ± SD)] | 58.7 ± 8.1 | 58.6 ± 8.1 | 60.1 ± 8.3 | <0.001 |
| Age in categories [n (%)] | ||||
| 41–64 years | 44,856 (74.0) | 42,855 (74.4) | 2001 (67.8) | <0.001 |
| ≥65 years | 15,725 (26.0) | 14,775 (25.6) | 950 (32.2) | |
| Sex [n (%)] | ||||
| Males | 20,282 (33.5) | 19,110 (33.2) | 1172 (39.7) | <0.001 |
| Females | 40,299 (66.5) | 38,520 (66.8) | 1779 (60.3) | |
| Body mass index [kg/m2 (mean ± SD)] | 23.9 ± 2.9 | 23.8 ± 2.9 | 24.9 ± 3.4 | <0.001 |
| Body mass index in categories [n (%)] | ||||
| <25 kg/m2 | 40,993 (67.7) | 39,370 (68.3) | 1623 (55.0) | <0.001 |
| ≥25 kg/m2 | 19,588 (32.3) | 18,260 (31.7) | 1328 (45.0) | |
| Smoking status [n (%)] | ||||
| Non-smoker | 45,647 (75.4) | 43,601 (75.7) | 2046 (69.3) | <0.001 |
| Ex-smoker | 10,252 (16.9) | 9699 (16.8) | 553 (18.7) | |
| Current smoker | 4682 (7.7) | 4330 (7.5) | 352 (11.9) | |
| Drinking status [n (%)] | ||||
| Non-drinker | 31,544 (52.1) | 30,036 (52.1) | 1508 (51.1) | 0.023 |
| Ex-drinker | 4118 (6.8) | 3881 (6.7) | 237 (8.0) | |
| Current drinker | 24,919 (41.1) | 23,713 (41.2) | 1206 (40.9) | |
| Regular exercise [n (%)] | ||||
| Yes | 35,617 (58.8) | 34,058 (59.1) | 1559 (52.8) | <0.001 |
| No | 24,964 (41.2) | 23,572 (40.9) | 1392 (47.2) | |
| Occupation [n (%)] | ||||
| Professional, administrative | 6339 (10.5) | 6072 (10.5) | 267 (9.1) | 0.015 |
| Office, sales, and service | 13,578 (22.4) | 12,946 (22.5) | 632 (21.4) | |
| Laborer, agricultural | 9037 (14.9) | 8569 (14.9) | 468 (15.9) | |
| Others, unemployed | 31,627 (52.2) | 30,043 (52.1) | 1584 (53.7) | |
| Education [n (%)] | ||||
| Less than middle school (<9 years) | 9158 (15.1) | 8606 (14.9) | 552 (18.7) | <0.001 |
| High school (9–12 years) | 32,834 (54.2) | 31,211 (54.2) | 1623 (55.0) | |
| College or more (>12 years) | 18,589 (30.7) | 17,813 (30.9) | 776 (26.3) | |
| Marital status [n (%)] | ||||
| Married, cohabitating | 53,778 (88.8) | 51,181 (88.8) | 2597 (88.0) | 0.186 |
| Single, divorced, widowed, separation, others | 6803 (11.2) | 6449 (11.2) | 354 (12.0) | |
| Medical history | ||||
| Diabetes [n (%)] | ||||
| Yes | 8161 (13.5) | 7584 (13.2) | 577 (19.6) | <0.001 |
| No | 52,420 (86.5) | 50,046 (86.8) | 2374 (80.4) | |
| Hypertension [n (%)] | ||||
| Yes | 20,982 (34.6) | 19,690 (34.2) | 1292 (43.8) | <0.001 |
| No | 39,599 (65.4) | 37,940 (65.8) | 1659 (56.2) | |
| Dyslipidemia [n (%)] | ||||
| Yes | 25,092 (41.4) | 23,746 (41.2) | 1346 (45.6) | <0.001 |
| No | 35,489 (58.6) | 33,884 (58.8) | 1605 (54.4) | |
| CCVD [n (%)] | ||||
| Yes | 3390 (5.6) | 3183 (5.5) | 207 (7.0) | 0.001 |
| No | 57,191 (94.4) | 54,447 (94.5) | 2744 (93.0) | |
| Cancer [n (%)] | ||||
| Yes | 3637 (6.0) | 3427 (5.9) | 210 (7.1) | 0.010 |
| No | 56,944 (94.0) | 54,203 (94.1) | 2741 (92.9) | |
| Asthma [n (%)] | ||||
| Yes | 1348 (2.2) | 1255 (2.2) | 93 (3.2) | 0.001 |
| No | 59,233 (97.8) | 56,375 (97.8) | 2858 (96.8) | |
| COPD [n (%)] | ||||
| Yes | 110 (0.2) | 98 (0.2) | 12 (0.4) | 0.007 |
| No | 60,471 (99.8) | 57,532 (99.8) | 2939 (99.6) | |
| Season [n (%)] | ||||
| Spring (March–May) | 8815 (14.6) | 8413 (14.6) | 402 (13.6) | <0.001 |
| Summer (June–August) | 20,781 (34.3) | 19,854 (34.5) | 927 (31.4) | |
| Fall (September–November) | 23,693 (39.1) | 22,478 (39.0) | 1215 (41.2) | |
| Winter (December–February) | 7292 (12.0) | 6885 (12.0) | 407 (13.8) | |
| Residential area [n (%)] | ||||
| Metropolitan | 37,860 (62.5) | 36,068 (62.6) | 1792 (60.7) | 0.044 |
| Non-metropolitan | 22,721 (37.5) | 21,562 (37.4) | 1159 (39.3) | |
| Hs-CRP [mg/L (mean ± SD)] | 0.89 ± 1.14 | 0.68 ±0.57 | 4.95 ±1.77 | <0.001 |
| Pollutant (Unit) | Mean ± SD | Max | Q3 | Median | Q1 | Min | IQR | Spearman’s Correlation Coefficient | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PM10 | PM2.5 | SO2 | NO2 | O3 | Temp | RH | ||||||||
| PM10 (μg/m3) | 48.34 ± 4.25 | 79.07 | 51.62 | 48.14 | 45.67 | 29.54 | 5.95 | 1.00 | 0.59 * | 0.17 * | 0.50 * | −0.66 * | 0.002 | −0.03 * |
| PM2.5 (μg/m3) | 25.20 ± 2.69 | 39.07 | 26.85 | 24.89 | 23.15 | 12.95 | 3.70 | 1.00 | −0.10 * | −0.13 * | −0.09 * | −0.001 | 0.13 * | |
| SO2 (ppb) | 5.40 ± 2.07 | 26.03 | 5.84 | 4.82 | 4.04 | 1.65 | 1.80 | 1.00 | 0.62 * | −0.22 * | 0.02 * | −0.16 * | ||
| NO2 (ppb) | 23.46 ± 7.96 | 40.81 | 30.13 | 21.28 | 17.60 | 1.00 | 12.54 | 1.00 | −0.78 * | 0.05 * | −0.24 * | |||
| O3 (ppb) | 25.86 ± 2.97 | 44.27 | 28.23 | 26.16 | 23.71 | 18.07 | 4.52 | 1.00 | −0.04 * | 0.14 * | ||||
| Temp (°C) | 16.73 ± 8.60 | 33.08 | 23.21 | 18.95 | 11.35 | -18.40 | 11.86 | 1.00 | 0.31 * | |||||
| RH (%) | 70.76 ± 12.32 | 99.95 | 79.84 | 71.73 | 62.82 | 18.96 | 17.02 | 1.00 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.H.; Woo, H.D.; Choi, S.; Song, D.S.; Lee, J.H.; Lee, K. Long-Term Effects of Ambient Particulate and Gaseous Pollutants on Serum High-Sensitivity C-Reactive Protein Levels: A Cross-Sectional Study Using KoGES-HEXA Data. Int. J. Environ. Res. Public Health 2022, 19, 11585. https://doi.org/10.3390/ijerph191811585
Kim JH, Woo HD, Choi S, Song DS, Lee JH, Lee K. Long-Term Effects of Ambient Particulate and Gaseous Pollutants on Serum High-Sensitivity C-Reactive Protein Levels: A Cross-Sectional Study Using KoGES-HEXA Data. International Journal of Environmental Research and Public Health. 2022; 19(18):11585. https://doi.org/10.3390/ijerph191811585
Chicago/Turabian StyleKim, Ji Hyun, Hae Dong Woo, Sunho Choi, Dae Sub Song, Jung Hyun Lee, and Kyoungho Lee. 2022. "Long-Term Effects of Ambient Particulate and Gaseous Pollutants on Serum High-Sensitivity C-Reactive Protein Levels: A Cross-Sectional Study Using KoGES-HEXA Data" International Journal of Environmental Research and Public Health 19, no. 18: 11585. https://doi.org/10.3390/ijerph191811585
APA StyleKim, J. H., Woo, H. D., Choi, S., Song, D. S., Lee, J. H., & Lee, K. (2022). Long-Term Effects of Ambient Particulate and Gaseous Pollutants on Serum High-Sensitivity C-Reactive Protein Levels: A Cross-Sectional Study Using KoGES-HEXA Data. International Journal of Environmental Research and Public Health, 19(18), 11585. https://doi.org/10.3390/ijerph191811585










