Optimal Care Pathways for People in Suicidal Crisis Who Interact with First Responders: A Scoping Review
Abstract
1. Introduction
Aims
- Examine the existing care pathways for people in a suicidal crisis who have come to the attention of first responders;
- Examine programs which could be used by first responders for suicide prevention;
- Evaluate the outcome evidence for these programs.
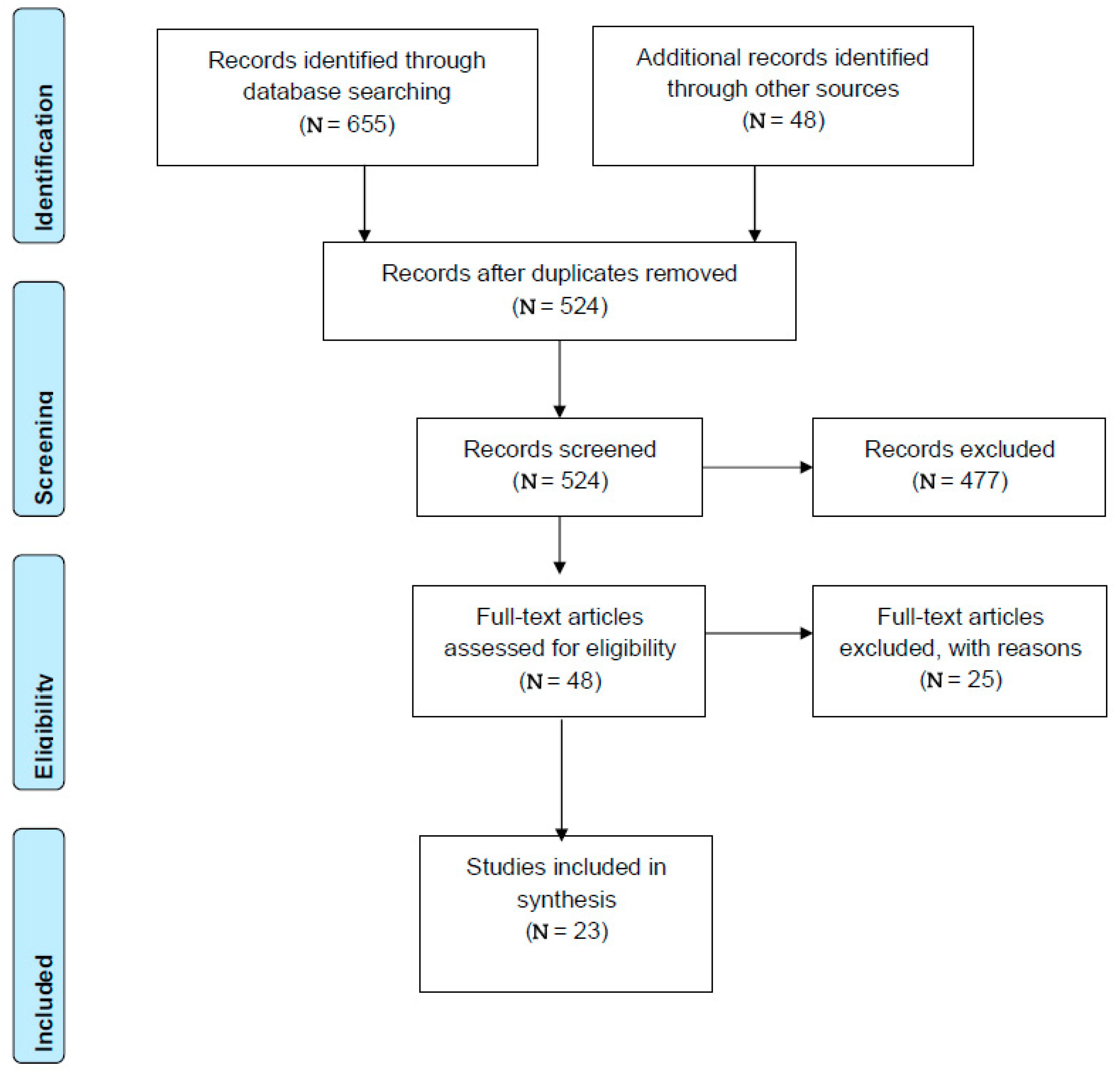
2. Method
2.1. Search Strategy
2.2. Inclusion Criteria
- Developed explicitly for populations in suicide or mental health crises who come in contact with first responders; OR
- Judged by the authors to share important similar features with other models that met criteria 1; OR
- Judged by the authors to be a model which could be utilised by first responders in the future.
2.3. Screening and Data Extraction
2.4. Analysis
3. Results
3.1. Models of Care
3.2. Service User Characteristics
Demographics
3.3. Outcome Evidence
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Suicide. World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/suicide (accessed on 28 June 2022).
- Australian Bureau of Statistics. Causes of Death Australia. Australian Bereau of Statistics. Available online: https://www.abs.gov.au/statistics/health/causes-death/causes-death-australia/latest-release#intentional-self-harm-suicides-key-characteristics (accessed on 8 February 2021).
- Johnston, A.; Pirkis, J.; Burgess, P. Suicidal thoughts and behaviours among Australian adults: Findings from the 2007 National Survey of Mental Health and Wellbeing. Aust. N. Z. J. Psychiatry 2009, 43, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Bostwick, J.M.; Pabbati, C.; Geske, J.; McKean, A.J. Suicide attempt as a risk factor for completed suicide: Even more lethal than we knew. Am. J. Psychiatry 2016, 173, 1094–1100. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Preventing Suicide: A Resource for Police, Firefighters and Other First Line Responders. Available online: https://apps.who.int/iris/bitstream/handle/10665/44175/9789241598439_eng.pdf;jsessionid=66BF276976BE727A2DFD475DD3C462BF?sequence=1 (accessed on 22 October 2018).
- Meurk, C.; Wittenhagen, L.; Bosley, E.; Steele, M.; Bunting, D.; Waterson, E.; Edwards, B.; Martain, B.; Heffernan, E. Suicide crisis calls to emergency services: Cohort profile and findings from a data linkage study in Queensland, Australia. Aust. N. Z. J. Psychiatry 2021, 56, 144–153. [Google Scholar] [CrossRef] [PubMed]
- McPhedran, S.; De Leo, D. Pathways to Care: To Examine the Mechanisms in Place Across Australia to Respond to and Provide Care to People at Imminent Risk of Suicide; The Australian Institute for Suicide Research & Prevention: Sydney, NSW, Australia, 2013; Available online: http://hdl.handle.net/10072/168961 (accessed on 11 November 2019).
- Australasian College for Emergency Medicine. Waiting Times in the Emergency Department for People with Acute Mental and Behavioural Conditions. Available online: https://acem.org.au/getmedia/0857d22e-af03-40bb-8e9f-f01a2a2bf607/ACEM_Mental-Health-Access-Block.aspx (accessed on 28 December 2018).
- Duggan, M.; Harris, B.; Chislett, W.-K.; Calder, R. Nowhere else to Go: Why Australia’s Health System Results in People with Mental Illness Getting ‘Stuck’ in Emergency Departments; Discussion Paper; Mitchell Institute, Victoria University: Melbourne, Australia, 2020; Available online: https://vuir.vu.edu.au/id/eprint/41956 (accessed on 20 January 2021).
- Productivity Commission. Report of Government Services, Part E, Chapter 13: Mental Health Management. Australian Government Productivity Commission. Available online: https://www.pc.gov.au/research/ongoing/report-on-government-services/2019/health/mental-health-management/rogs-2019-parte-chapter13.pdf (accessed on 9 September 2019).
- Queensland Forensic Mental Health Service Metro North Hospital and Health Service and Queensland Centre for Mental Health Research. Partners in Prevention: Understanding and Enhancing First Responses to Suicide Crisis Situations—Perspectives from Lived Experience. 2020. Available online: PiP_LivedExp_online.pdf(qcmhr.org) (accessed on 20 January 2021).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Puntis, S.; Perfect, D.; Kirubarajan, A.; Bolton, S.; Davies, F.; Hayes, A.; Harriss, E.; Molodynski, A. A Systematic Review of Co-responder Models of Police Mental Healt ‘street’ triage. BMC Psychiatry 2018, 18, 1–11. Available online: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-018-1836-2 (accessed on 11 November 2019). [CrossRef] [PubMed]
- Rodgers, M.; Thomas, S.; Dalton, J.; Harden, M.; Eastwood, A. Police-related triage interventions for mental health-related incidents: A rapid evidence synthesis. Health Serv. Deliv. Res. 2019, 7, 1–164. [Google Scholar] [CrossRef] [PubMed]
- Bouveng, O.; Bengtsson, F.; Carlborg, A. First-year follow-up of the Psychiatric Emergency Response Team (PAM) in Stockholm County, Sweden: A descriptive study. Int. J. Ment. Health 2017, 46, 65–73. [Google Scholar] [CrossRef]
- The Allen Consulting Group. Police, Ambulance and Clinical Early Response (PACER) Evaluation. Report to Department of Health. Available online: file:///C:/Users/katel_000/Downloads/PACER_Eval_18April2012_FinalFinal%20-%20PDF.pdf (accessed on 8 November 2018).
- Lee, S.; Thomas, P.; Doulis, C.; Bowles, D.; Henderson, K.; Keppich-Arnold, S.; Perez, E.; Stafrace, S. Outcomes achieved by and police and clinician perspectives on a joint police officer and mental health clinician mobile response unit. Int. J. Ment. Health Nurs. 2015, 24, 538–546. [Google Scholar] [CrossRef] [PubMed]
- McKenna, B.; Furness, T.; Brown, S.; Tacey, M.; Hiam, A.; Wise, M. Police and clinician diversion of people in mental health crisis from the emergency department: A trend analysis and cross comparison study. BMC Emerg. Med. 2015, 15, 1–6. Available online: https://bmcemergmed.biomedcentral.com/track/pdf/10.1186/s12873-015-0040-7.pdf (accessed on 11 November 2019). [CrossRef] [PubMed]
- Meehan, T.; Brack, J.; Mansfield, Y.; Stedman, T. Do police-mental health co-responder programmes reduce emergency department presentations or simply delay the inevitable? Australas. Psychiatry 2019, 27, 18–20. [Google Scholar] [CrossRef] [PubMed]
- Heslin, M.; Callaghan, L.; Packwood, M.; Badu, V.; Byford, S. Decision analytic model exploring the cost and cost-offset implications of street triage. BMJ Open 2016, 6, e009670. Available online: https://bmjopen.bmj.com/content/6/2/e009670 (accessed on 11 November 2019). [CrossRef] [PubMed]
- Coffman, J.M.; Blash, L.; Amah, G. Update of Evaluation of California’s Community Paramedicine Pilot Program. Available online: https://emsa.ca.gov/wp-content/uploads/sites/71/2017/11/2019-Public-Report-on-California-Community-Paramedicine-Project-2.27.19.pdf (accessed on 11 November 2019).
- O’Neill, K. Distress Brief Intervention: Programme Manager’s Six Monthly Report 18 April–18 September, Issue 4. Available online: https://www.dbi.scot/general/dbi-programme-manager-six-monthly-progress-report-issue-4-apr-2018-sept-2018/ (accessed on 26 January 2019).
- Griffiths, A.; Gale, K. Independent Evaluation of the North East Hampshire and Farnham Vanguard: Aldershot Safe Haven Service. Available online: https://wessexahsn.org.uk/img/projects/Safe%20Haven%20Evaluation_FINAL_October%202017.pdf (accessed on 11 November 2019).
- Price Waterhouse Coopers. Economic Impact of the Safe Haven Cafe, Melbourne. Available online: https://www.thecentrehki.com.au/wp-content/uploads/2019/06/Safe-haven-Cafe-Cost-Benefit-Analysis._FINAL.pdf (accessed on 9 March 2019).
- My Mental Health. Brisbane North Safe Spaces Network Report. Available online: https://www.mymentalhealth.org.au/page/services/self-care-and-informal-support/safe-space-network/ (accessed on 28 December 2018).
- Wesley Mission Queensland. Safe Spaces Network for Brisbane North: Project Report. Available online: http://www.northbrisbane.pirinitiative.com.au/wp-content/uploads/2014/02/Safe-Space-Final-project-report-2017.pdf (accessed on 28 December 2018).
- Heyland, M.; Emery, C.; Shattell, M. The Living Room, a community crisis respite program: Offering people in crisis an alternative to emergency departments. Glob. J. Community Psychol. Pract. 2013, 4, 1–8. [Google Scholar] [CrossRef]
- Heyland, M.; Johnson, M. Evaluating an alternative to the emergency department for adults in mental health crisis. Issues Ment. Health Nurs. 2017, 38, 557–561. [Google Scholar] [CrossRef] [PubMed]
- National Action Alliance for Suicide Prevention: Crisis Services Task Force. Crisis Now: Transforming Services Is within Our Reach. Available online: https://theactionalliance.org/sites/default/files/crisisnow.pdf (accessed on 26 December 2018).
- Dudgeon, P.; Milroy, J.; Luxford, Y.; Holland, C. Report of the Critical Response Pilot Project: Aboriginal and Torres Strait Islander Suicide Prevention Evaluation Project. Available online: https://www.atsispep.sis.uwa.edu.au/__data/assets/pdf_file/0019/3050029/FINAL-CriticalResponsePilotProjectReport-WEB.pdf (accessed on 12 March 2019).
- Thirrili. National Indigenous Critical Response Service. Available online: https://thirrili.com.au/ (accessed on 12 March 2019).
- Beyond Blue. The Way Back Support Service—Northern Territory: Final Evaluation Report for Beyondblue. Available online: https://www.beyondblue.org.au/docs/default-source/default-document-library/the-way-back-nt-final-evaluation-report-2016.pdf (accessed on 28 December 2018).
- Wilhelm, K.; Finch, A.; Kotze, B.; Arnold, K.; McDonald, G.; Sternhell, P.; Hudson, B. The Green Card Clinic: Overview of a brief patient-centred intervention following deliberate self-harm. Australas. Psychiatry 2007, 15, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Surgenor, P.; Freeman, J.; O’Connor, C. Developing the Pieta House suicide intervention model: A quasi-experimental, repeated measures design. BMC Psychol. 2015, 3, 1–8. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Department of Veterans’ Affairs. Veterans Suicide Prevention Pilot. Available online: https://www.dva.gov.au/health-and-wellbeing/mental-health/veteran-suicide-prevention-pilot (accessed on 12 March 2019).
- Australian Bureau of Statistics. 4125.0 Gender Indicators, Australia, September 2018. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4125.0Sep%202018Main%20FeaturesSafety%20and%20Justice8#::text=In%202016%E2%80%9317%20there%20were,that%20of%20female%20offender%20rates (accessed on 26 February 2021).
| Author and Year | Evaluation Type | Consumer Characteristics (Age, Gender, and Characteristics of Presentation) | Referral Reasons | Study Period and Sample Size | Outcome Measures Utilised (Yes/No) |
|---|---|---|---|---|---|
| |||||
| Puntis et al., 2018 [13]. | Systematic review of descriptive and qualitative studies. | Individuals with mental health problems. Males more likely to be referred to the service (range 47–77% of referrals). | N/A | N/A | No. |
| Rodgers et al., 2019, [14]. | Rapid evidence synthesis of systematic reviews, quantitative and qualitative studies. | Individuals with mental illness or in mental health crises. | N/A | N/A | No. |
| Bouveng et al., 2017 [15]. | Descriptive study. | Individuals with severe mental illness or in suicidal crisis. No age restrictions. Age range of cohort seen 5–100 years. Ages 18–29 were the highest service users. 56% female, 43% male, 0.4% unknown. Stockholm, Sweden. | 97% deemed high or medium priority.
| 2015–2016, 12 months. N = 1580 requests for service, data reported on N = 1036 individual. | No. |
| The Allen Consulting Group, 2012 [16]. | Pre-post study with control group. | Individuals in a suicidal or mental health crisis. No age restrictions reported. Gender not reported. Victoria, Australia |
| 2009–2011, 16 months. N = 783 assistance requests for service. | No. |
| Lee et al., 2015 [17]. | Descriptive study (mixed methods). | Individuals in a suicidal or mental health crisis. No age restrictions reported. 60% male, 40% female. Victoria, Australia. |
| 2011–2012, 6 months. N = 296 contacts for service. | No. |
| McKenna et al., 2015 [18]. | Pre-post study (interrupted time series). | Individuals in a mental health crisis. No age restrictions reported. 58.3% male, 41.7% female. Victoria, Australia |
| November 2011–January 2014, 27 months N = 243 people seen. | No. |
| Meehan et al., 2019 [19]. | Pre-post study (interrupted time series). | Individuals with a suicidal or mental health crisis. No age restrictions. 51% aged 20–39 years. 49% Female. West Moreton, Queensland, Australia. |
7% were currently case managed by a mental health service. | 2017, 4 months. N = 171 individuals; N = 226 occasions of service. Direct contact with N = 137. | No. |
| Heslin et al., 2016 [20]. | Pre-post study (interrupted time series) and cost-offset analysis. | Individuals in a mental health crisis. Age and gender not reported. Sussex, England. | Not reported. | For comparison of actual street triage outcomes, 4 month period, June–September, 2014. For overall outcomes, 6 month period before (1 April–30 September, 2013) and 6 month period after implementation (1 April–30 September, 2014) compared, allowing for a settling in period. N = 358 (before period). N = 358 (after period) of which N = 233 were attended by the street triage. | No. |
| Coffman et al., 2019 [21]. | Descriptive study. | Individuals thought to have a mental health problem as identified by a 911 dispatcher or other emergency services. Inclusion = person on an involuntary treatment hold by police and who were uninsured or on Medi-Cal (Santa Clara/Gilroy site); person being on an involuntary treatment hold or those with acute mental health needs who voluntarily consent for services (Stanislaus and Fresno sites). Age and gender not reported. California, United States of America. | Not reported. | September 2015–March 2019, 42 months (3.5 years). N = 2045 people enrolled in the pilots across three sites. | No. |
| |||||
| O’Neill, 2018 [22]. | Currently underway. | Individuals in distress who come to the attention of police, ambulance, hospital EDs, or primary care. Adults. Undergoing expansion in stages to include 16 and 17 year olds, and scoping feasibility for those aged 15 years and younger. 57% female, 43% male. Four trial sites across Scotland. | 24% self-reported being under the influence of alcohol/substances at point of referral. Presenting problems, reported, included:
| 2016–2021, 4.5 years. Interim findings reported on N = 1322 referrals received from 2016 to September, 2018. | No. |
| |||||
| Griffiths and Gale, 2017 [23]. | Mixed design. Interrupted time series of impacts, descriptive study of client satisfaction. | Individuals needing mental health support out of hours. Indicates the service is for adults (18 years and over). Gender not reported. Aldershot, Hampshire, United Kingdom. |
| 2016–2017, 12 months. N = 4275 attendances at the service. N = 670 individuals. | None. |
| Price Waterhouse Coopers, 2018 [24]. | Cost-benefit analysis. | People seeking mental health support or social connection. Age 18 and over. Gender not reported. Melbourne, Victoria, Australia. | Not reported. | May–September, 2018, 5 month period compared with (1) the same 5 month period 12 months prior and (2) the 6 months immediately prior to implementation of the service. N = 62 individuals made 400 visits to the café during the evaluation period. N = 41 participants completed a survey. | None reported. |
| N/A Brisbane North Safe Space (My Mental Health, 2018; Wesley Mission Queensland, 2017) [25,26]. | No evaluation. | Experiencing or recently experienced psychological distress. 18 years of age or over. Gender not reported. Brisbane, Queensland, Australia. | Not reported. | N/A | None reported. |
| Heyland et al., 2013. Heyland and Johnson, 2017 [27,28]. | Descriptive study. | Individuals in mental health crisis. 18 years of age or over. Age range 20–59. Gender not reported. Chicago, Illinois, United States of America. |
| 2015, 8 weeks (clients followed up 30 days post separation with service) Total N = 228 visits by 87 individuals. Evaluation included N = 56 visits by 16 clients. | Yes. |
| |||||
| Crisis Now (NAASP, 2016) [29] | No evaluation currently. | N/A | N/A | N/A | N/A |
| |||||
| Dudgeon et al., 2017 [30]. | Not described. | Aboriginal and Torres Strait Islander individuals, family, kin and community affected by critical incidents, including suicide or high risk of suicide, murders or multiple casualty events that place those known to the deceased at elevated suicide risk. No age restrictions reported. Gender not reported. Four trial sites across Western Australia, Australia. | Not reported. | 2015–2016, ~12 months N = 46 Aboriginal Torres Strait Islander families affected by suicide or critical incident. | None. |
| N/A National Indigenous Crisis Response Service (NICRS); Similar to ATSIPEP (above). Thirrili., 2017 [31]. | None currently. | N/A | N/A | N/A | N/A |
| |||||
| beyondblue, 2016 [32]. | Mixed design. Pre-post study (quantitative and qualitative). Descriptive study of client characteristics. | People recently discharged from hospital for a suicide attempt of suicidal crisis. No age restrictions reported. 78% under 45 years of age. Age range 15–75. 40% male, 60% female. Darwin, Northern Territory, Australia. | Not reported. | 2014–2015, 18 months N = 122 referrals, N = 87 individuals who were recently discharged from hospital due to suicide attempt or suicide crisis. N = 46 interviews with stakeholders. | Yes. |
| N/A Peer Acceptance, Understanding, Support and Empathy (PAUSE); (Schneck, 2019) (Kezia Schneck, Peer Support Worker Brook RED. Personal communication via telephone. 15 January 2019.) | Evaluation currently underway. | People identified as requiring peer support following suicidality. Brisbane, Queensland, Australia. | N/A | N/A | N/A |
| Wilhelm et al., 2007 [33]. | Mixed design. Pre-post study of outcomes, descriptive study of client characteristics and feedback. | People who present to St Vincent’s hospital ED for deliberate self-harm or suicidal ideation. No age restrictions reported. Mean age = 31.6 years. Age range 16–80. 57% female, 43% male. Sydney, New South Wales, Australia | Reasons for ED presentations:
| 1998–2005, 7 years. N = 456 individuals. | Yes. |
| Surgenor et al., 2015 [34]. | Pre-post study. | Individuals in suicidal crisis. No age restrictions reported. Age range 18–74. Mean age 38.1, 44.4% male, 55.6% female. Ireland. | Not reported. | No date range given. N = 432 individuals invited to participate pre-therapy. | Yes. |
| N/A Veteran Suicide Prevention Pilot; Department of Veterans Affairs, 2018 [35]. | No evaluation currently. | Military veterans following discharge from hospital after a suicidal crisis. Australia. | N/A | N/A | N/A |
| Model | Author | Assessment | Outcomes |
|---|---|---|---|
| Safe Haven | Heyland and Johnson, 2017, [28]. | Subjective Units of Distress Ratings (SUDS; 0 = no distress with 10 = highest distress). Pre and post. | Reduction of approximately 2 points. |
| Aftercare | beyondblue, 2016 [32]. | WHO-5—World Health Organisation Well-Being Index (0 = worst imaginable well-being—25 = best imaginable well-being). | On average a 10 point improvement was noted (from 12.5 to 22.5). |
| Aftercare | Wilhelm et al., 2007 [33]. | 1. Centre for Epidemiological Studies Depression Scale (CES-D; score range 0–60) 2. FANTASTIC lifestyle checklist (0–50. Higher score indicates greater control over one’s lifestyle). | 1. Mean CES-D on intake (N = 282) was 35.7 (SD = 12.0) with 95% of guests scoring 16 or more, indicating possible depression and 85% scoring 23 or more, indicating significant depression. Statistically significant reduction in scores for participants who completed all three sessions and the post-test (N = 40, m = 17.9, SD = 12.9). Mean FANTASTIC scores 25.9 (SD = 7.3) at intake, no follow up scores available. |
| Aftercare | Surgenor et al., 2015 [34]. | 1. Single item indicator (“I have high self-esteem”) rated on 5-point scale (1 = lowest self-esteem; 5 = highest self-esteem) 2. Patient Health Questionnaire (PHQ-9). Lower score indicates less depression. 3. The Positive and Negative Suicide Ideation Inventory (PANSI). Four positive and four negative items were utilised. Lower scores for negative items indicate fewer negative symptoms. Higher scores for positive items (for protective behaviours) indicate greater protective factors. | 1. Mean self-esteem score was 1.76 (SD = 1.07) pre-test and 2.79 (SD = 1.08) post-test. 2. Mean PHQ-9 score was 18.58 (SD = 5.77) pre-test and 10.87 (SD = 7.47) post-test. 3. Mean negative suicidal ideation was 13.04 (SD = 4.22) pre-test and 7.77 (SD = 4.82) post-test. Mean positive suicidal ideation was 9.48 (SD = 3.69) pre-test and 13.76 (SD = 3.66) at post-test. Changes in scores pre- and post-treatment were statistically significant (p < 0.001) for all measures. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kerr, K.; Heffernan, E.; Hawgood, J.; Edwards, B.; Meurk, C. Optimal Care Pathways for People in Suicidal Crisis Who Interact with First Responders: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 11510. https://doi.org/10.3390/ijerph191811510
Kerr K, Heffernan E, Hawgood J, Edwards B, Meurk C. Optimal Care Pathways for People in Suicidal Crisis Who Interact with First Responders: A Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(18):11510. https://doi.org/10.3390/ijerph191811510
Chicago/Turabian StyleKerr, Katelyn, Ed Heffernan, Jacinta Hawgood, Bronwen Edwards, and Carla Meurk. 2022. "Optimal Care Pathways for People in Suicidal Crisis Who Interact with First Responders: A Scoping Review" International Journal of Environmental Research and Public Health 19, no. 18: 11510. https://doi.org/10.3390/ijerph191811510
APA StyleKerr, K., Heffernan, E., Hawgood, J., Edwards, B., & Meurk, C. (2022). Optimal Care Pathways for People in Suicidal Crisis Who Interact with First Responders: A Scoping Review. International Journal of Environmental Research and Public Health, 19(18), 11510. https://doi.org/10.3390/ijerph191811510







