Storyboarding HIV Infected Young People’s Adherence to Antiretroviral Therapy in Lower- to Upper Middle-Income Countries: A New-Materialist Qualitative Evidence Synthesis
Abstract
1. Introduction
Why Is It Important to Do the Current Review?
2. Methods and Materials
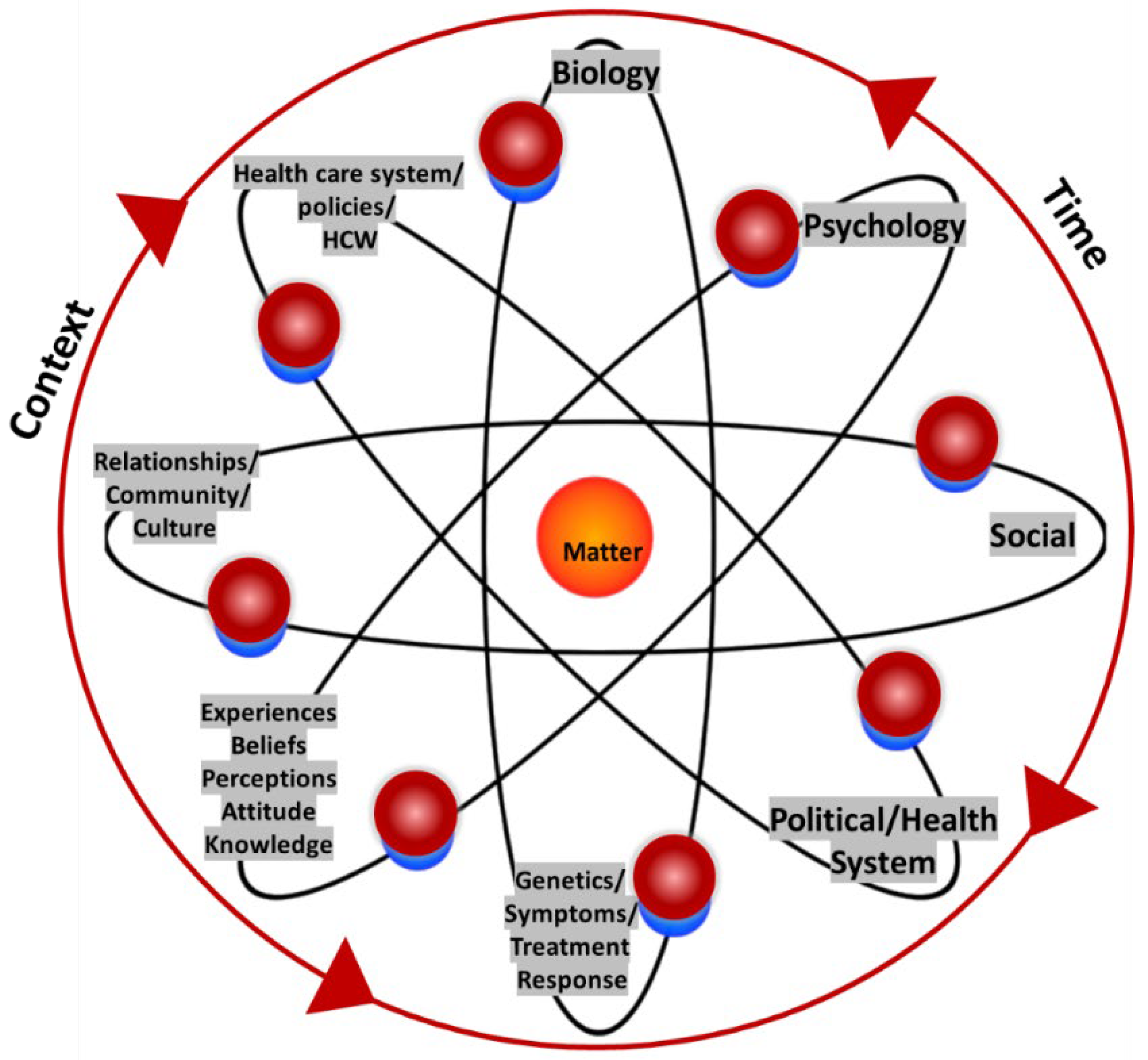
2.1. Conceptual Framework
2.2. Criteria for Considering Studies for This Review
2.2.1. Types of Studies
2.2.2. Context
2.2.3. Types of Participants
2.2.4. Phenomenon of Interest
2.2.5. Outcomes
2.3. Search Methods for Identification of Studies
2.4. Selection of Studies
2.5. Methodological Quality Assessment
2.6. Data Extraction
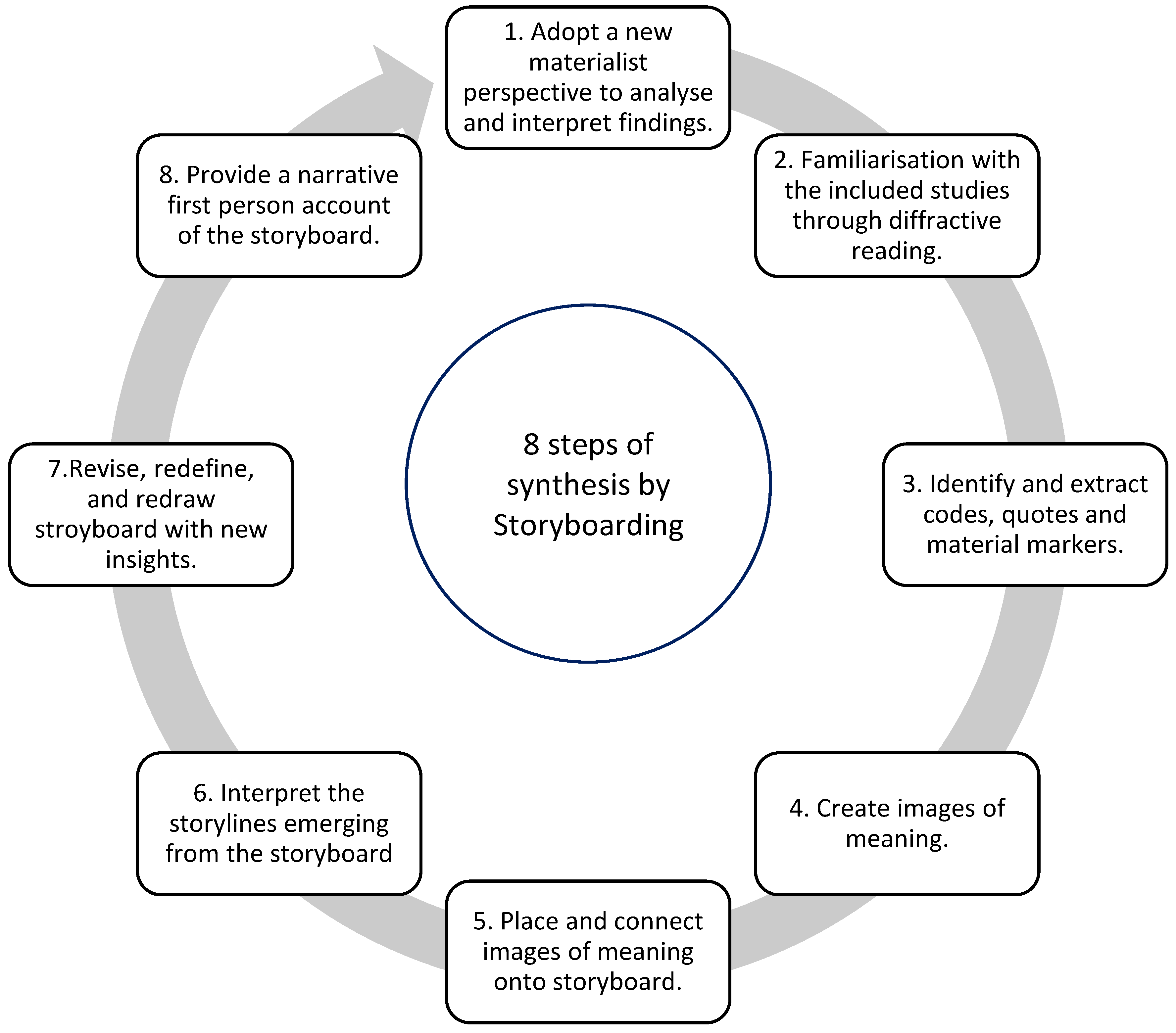
2.7. Data Synthesis by Storyboarding
3. Results
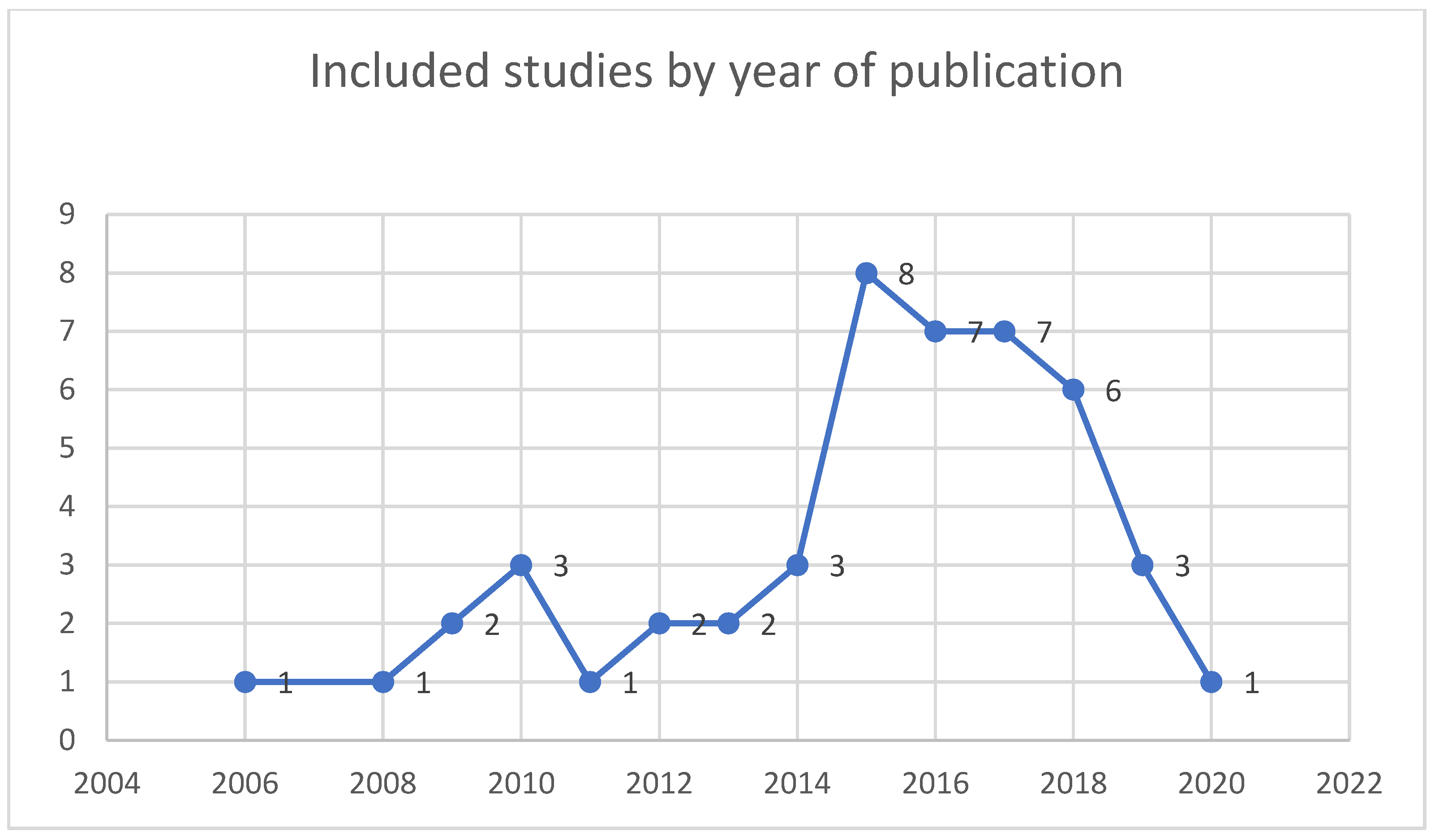
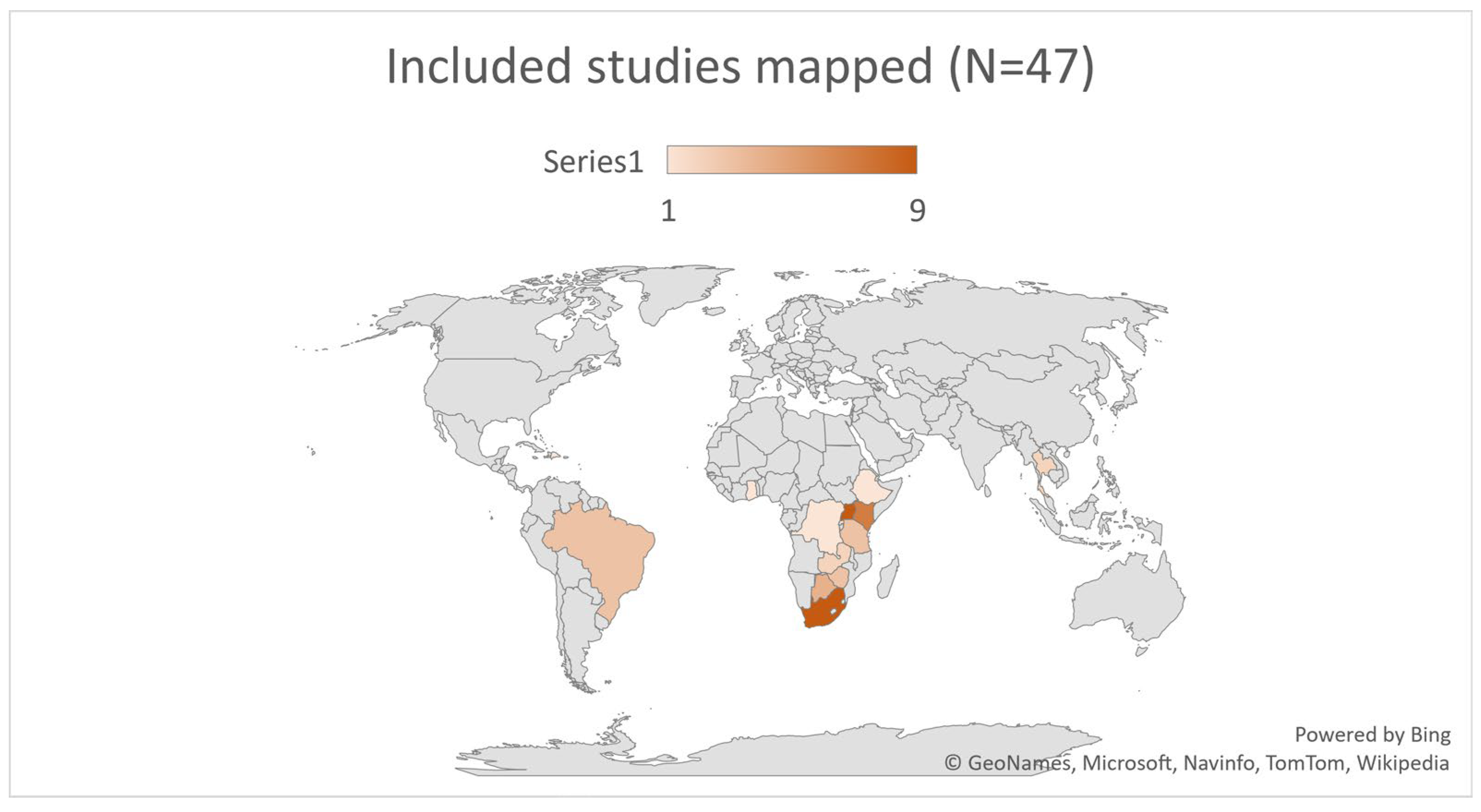
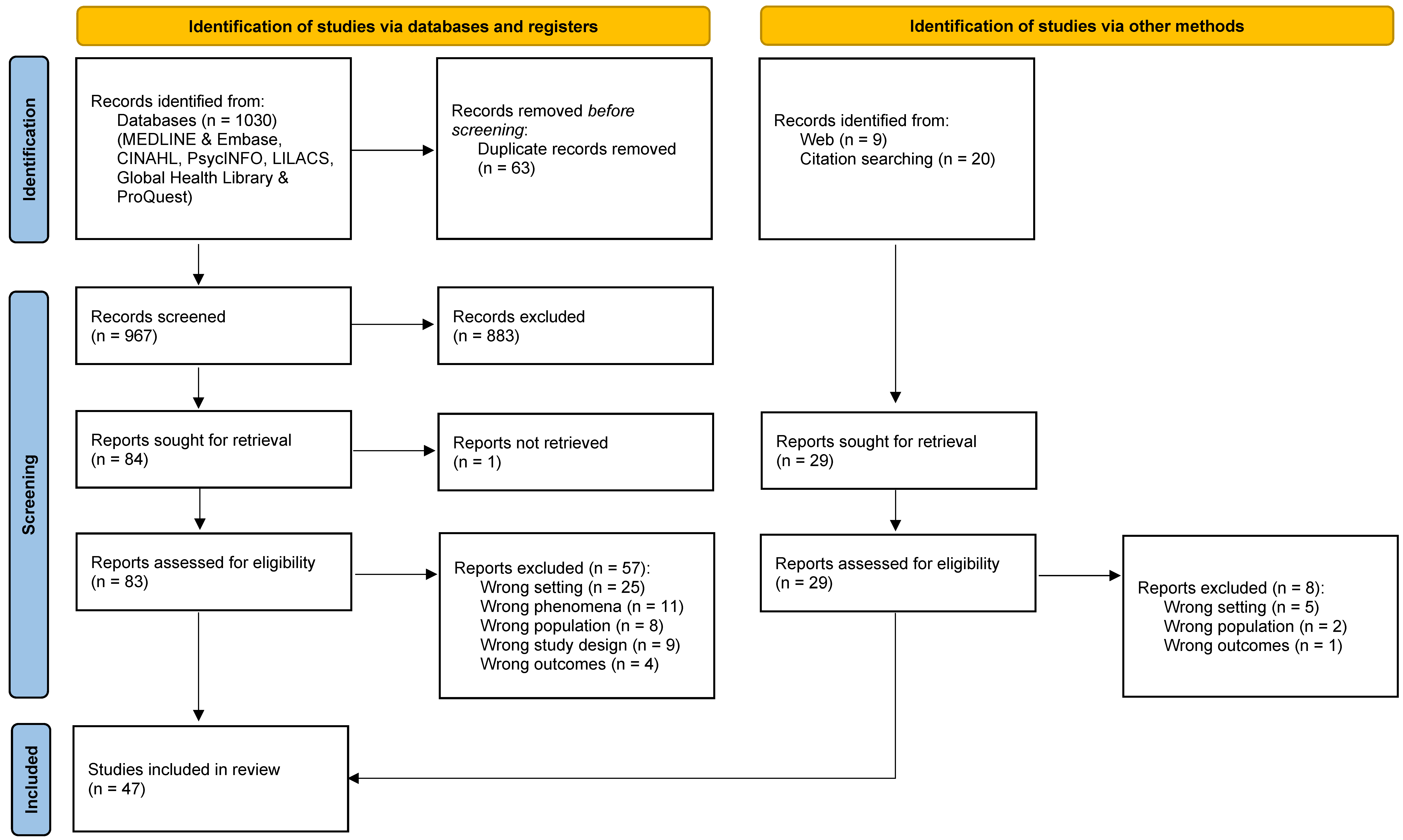
3.1. Results of the Search
3.2. Studies Included in This QES
3.3. Excluded Studies
3.4. Methodological Quality Assessment
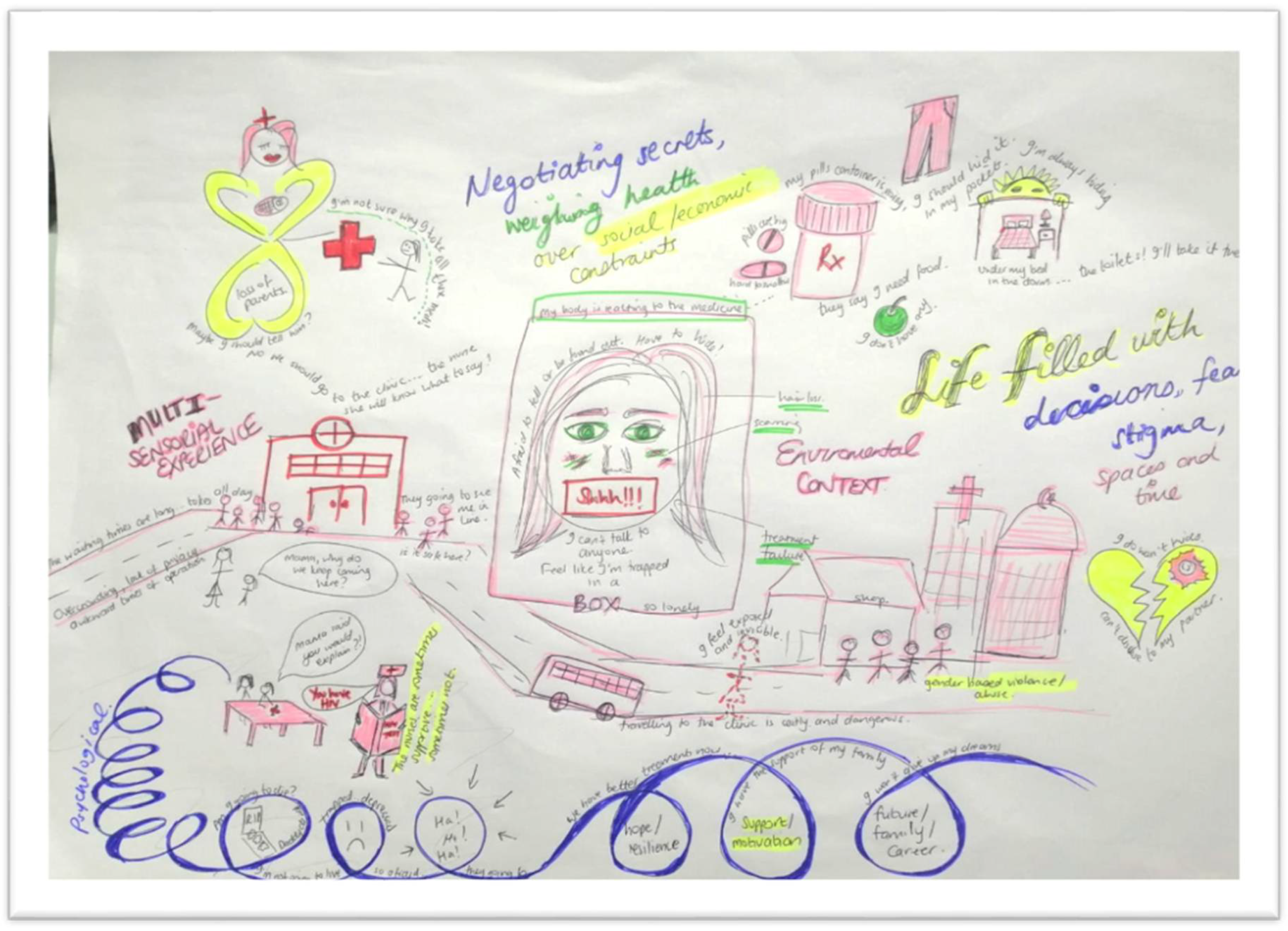
3.5. Exploring Adherence with A New Materialist Lens—Synthesis by Storyboarding
3.5.1. Theoretical Framework, Familiarisation, and Data Extraction
3.5.2. Creating the Images of Meaning, Interpreting Storylines, and the Storyboard
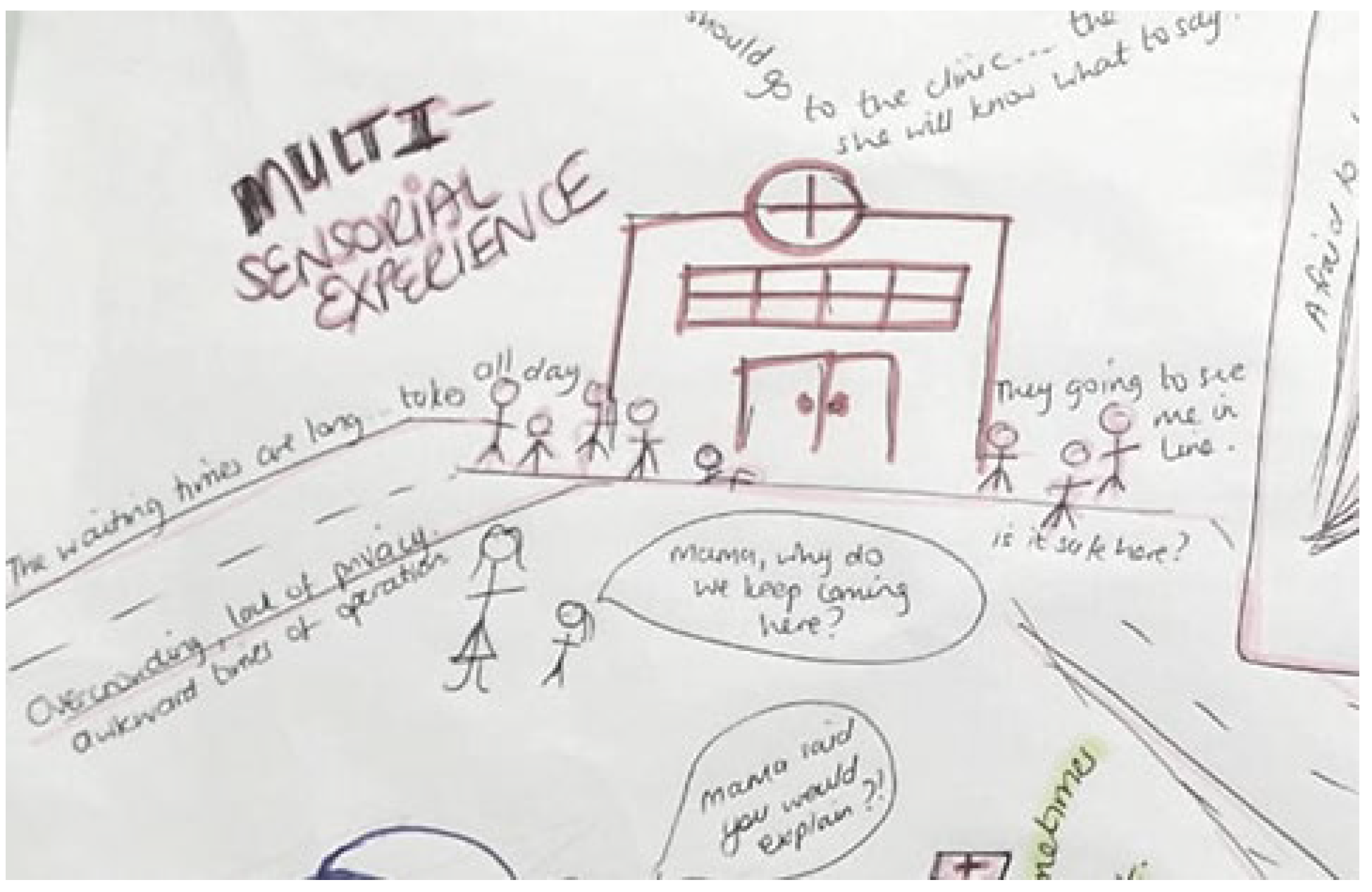
- Navigating clinic visits, health care workers, and privacy
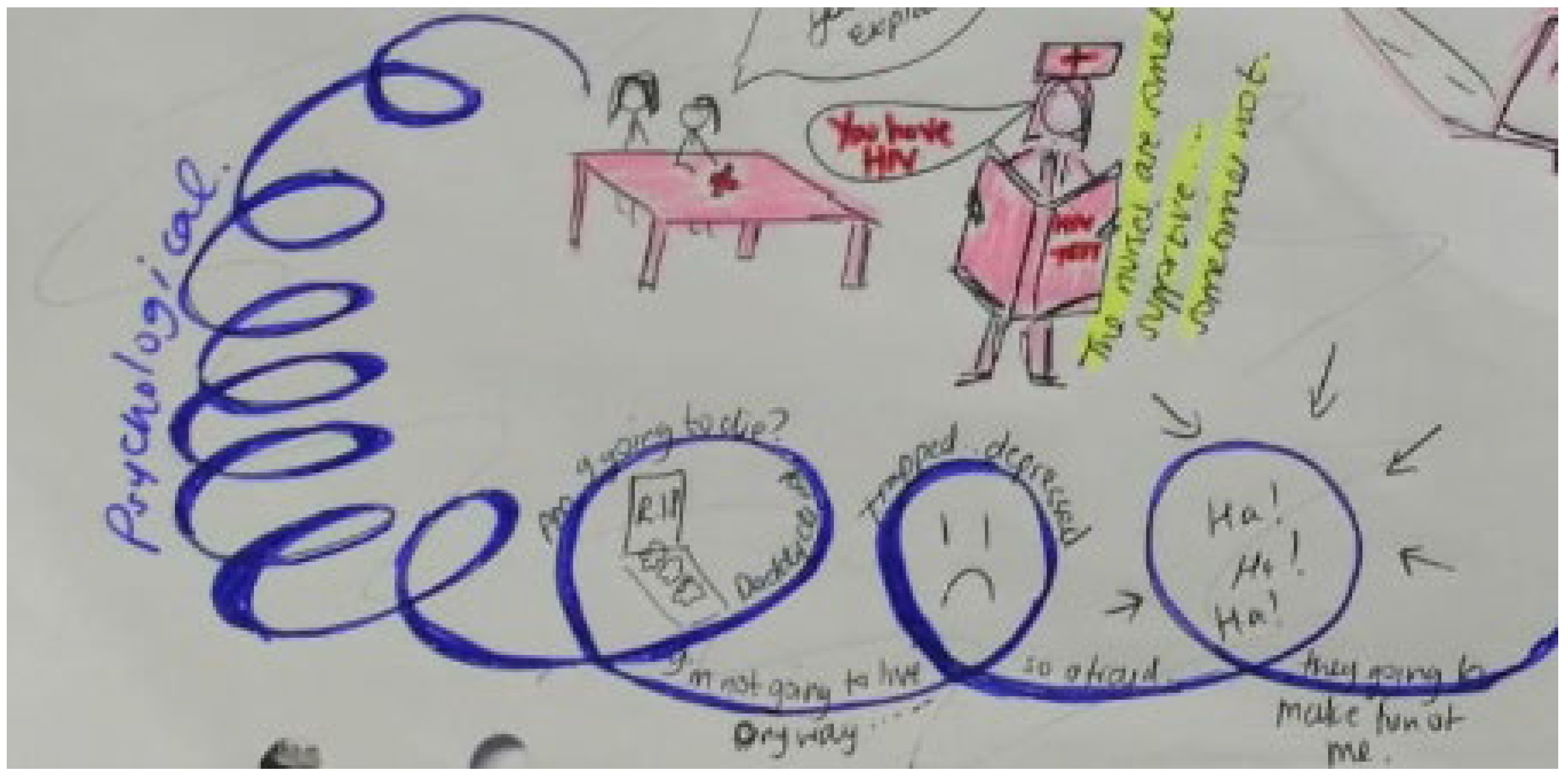
- Disclosure and psychological reactions to HIV diagnosis
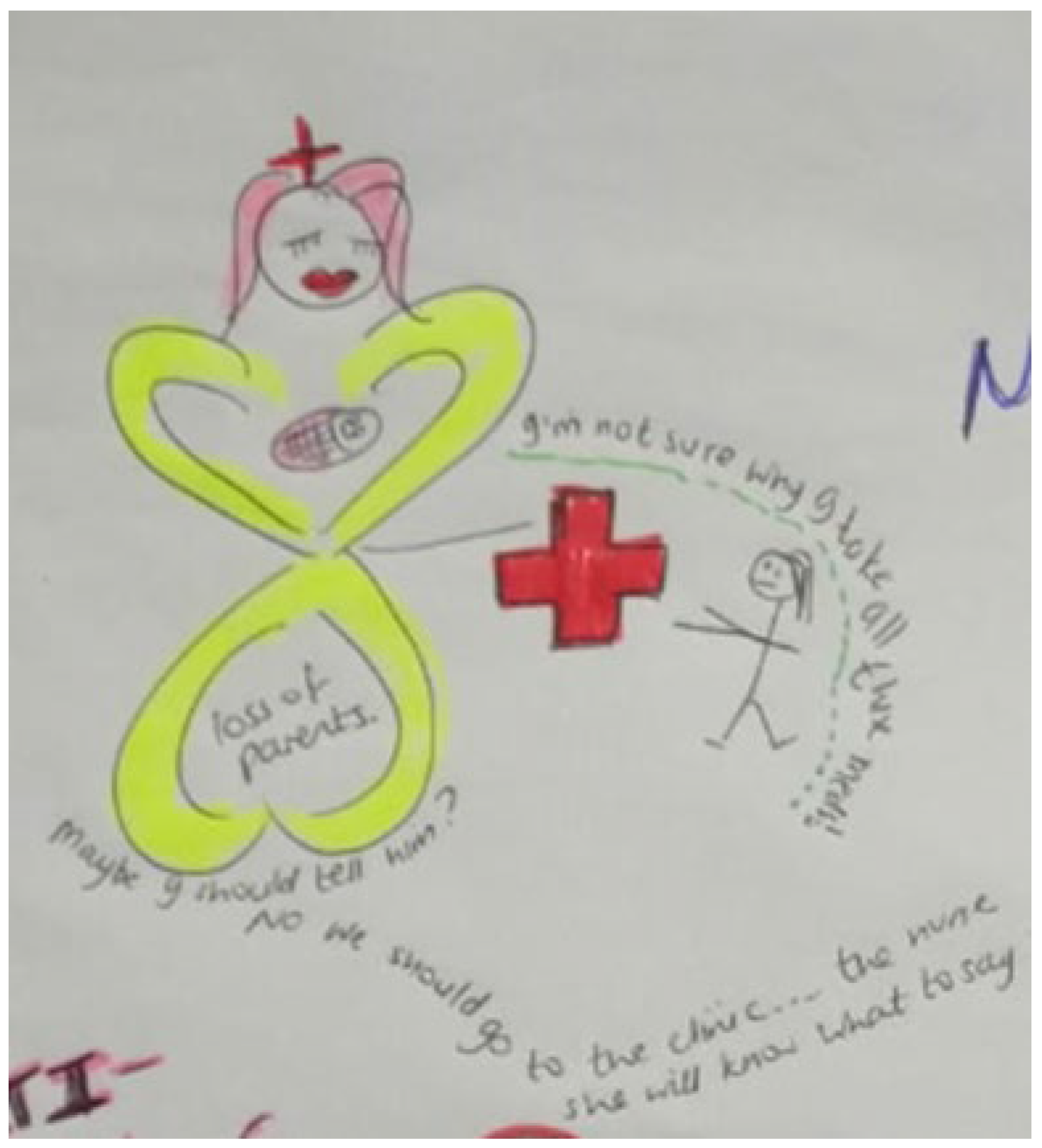
- Grieving loss of caregivers and challenging familial relationships
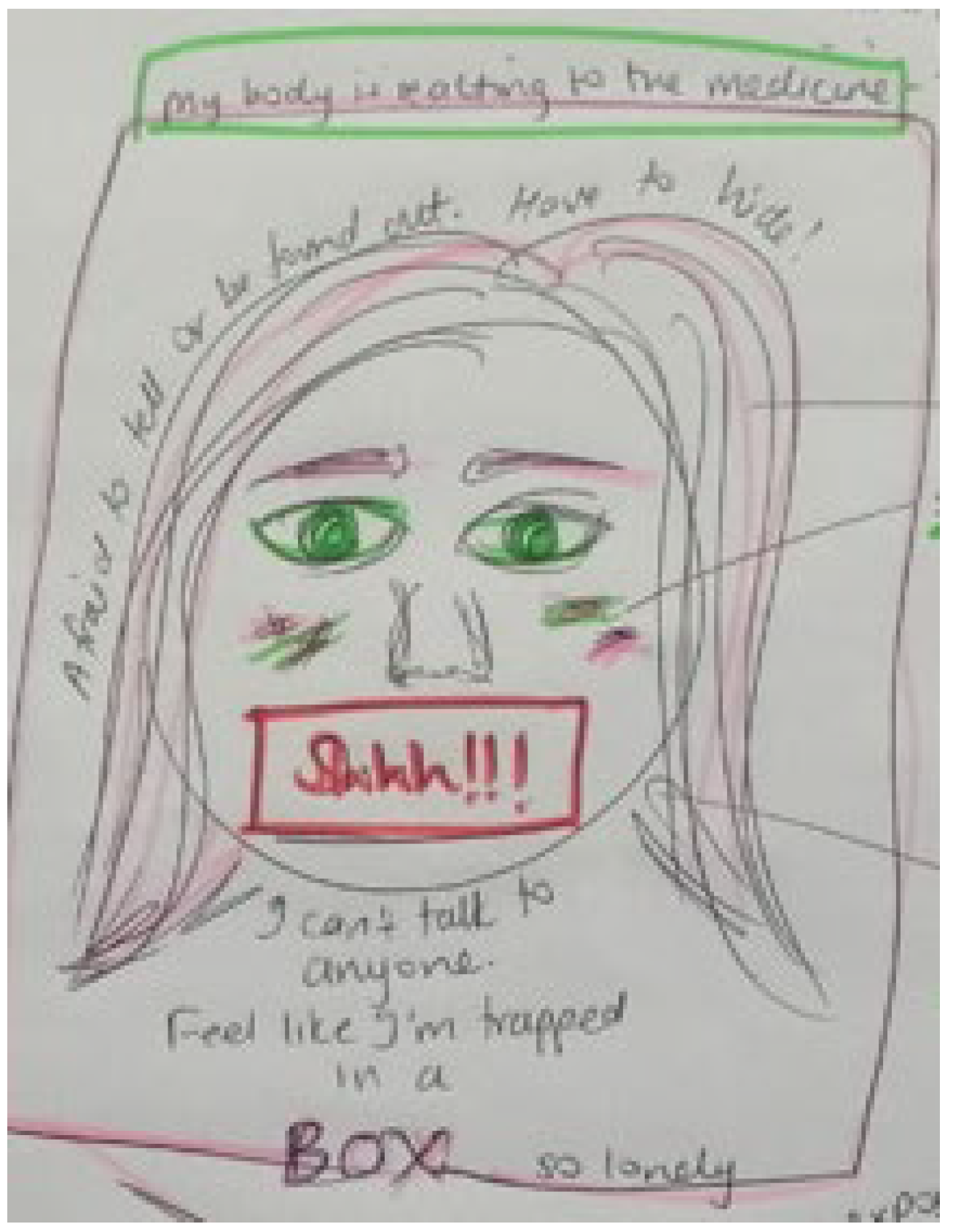
- Bodily changes, internal stigma, and suicidal ideation
- Negotiating power, sex, and risky behaviours
- Fear of false judgement and stigma forces YLPHIV to keep their pills and status a secret
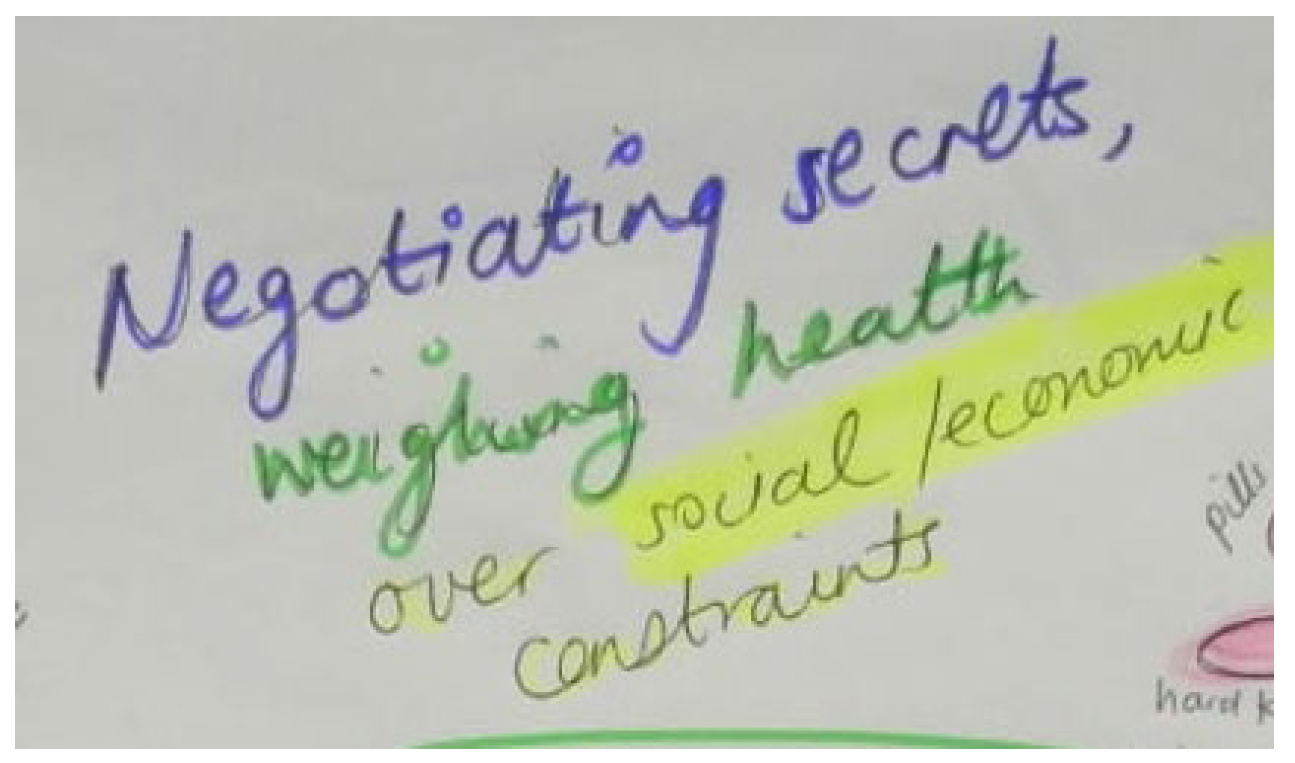
- Weighing up health against socio-economic constraints and educational priorities
- Resilience, motivation, and future goals prompt adherence as habitual behaviour
- Places and spaces in the community that support and threaten adherence
3.5.3. The Story within the Assemblage of Adherence to ART
- Storyline 1: Navigating Clinic Visits, Health Care Workers, and Privacy (Figure 7)
- Storyline 2: Disclosure and Psychological Reactions to HIV Diagnosis (Figure 8)
- Storyline 3: Grieving Loss of Caregivers and Challenging Familial Relationships (Figure 9)
- Storyline 4: Bodily Changes, Internal Stigma, and Suicidal Ideation (Figure 10)
- Storyline 5: Negotiating Power, Sex, and Risky Behaviours (Figure 11)

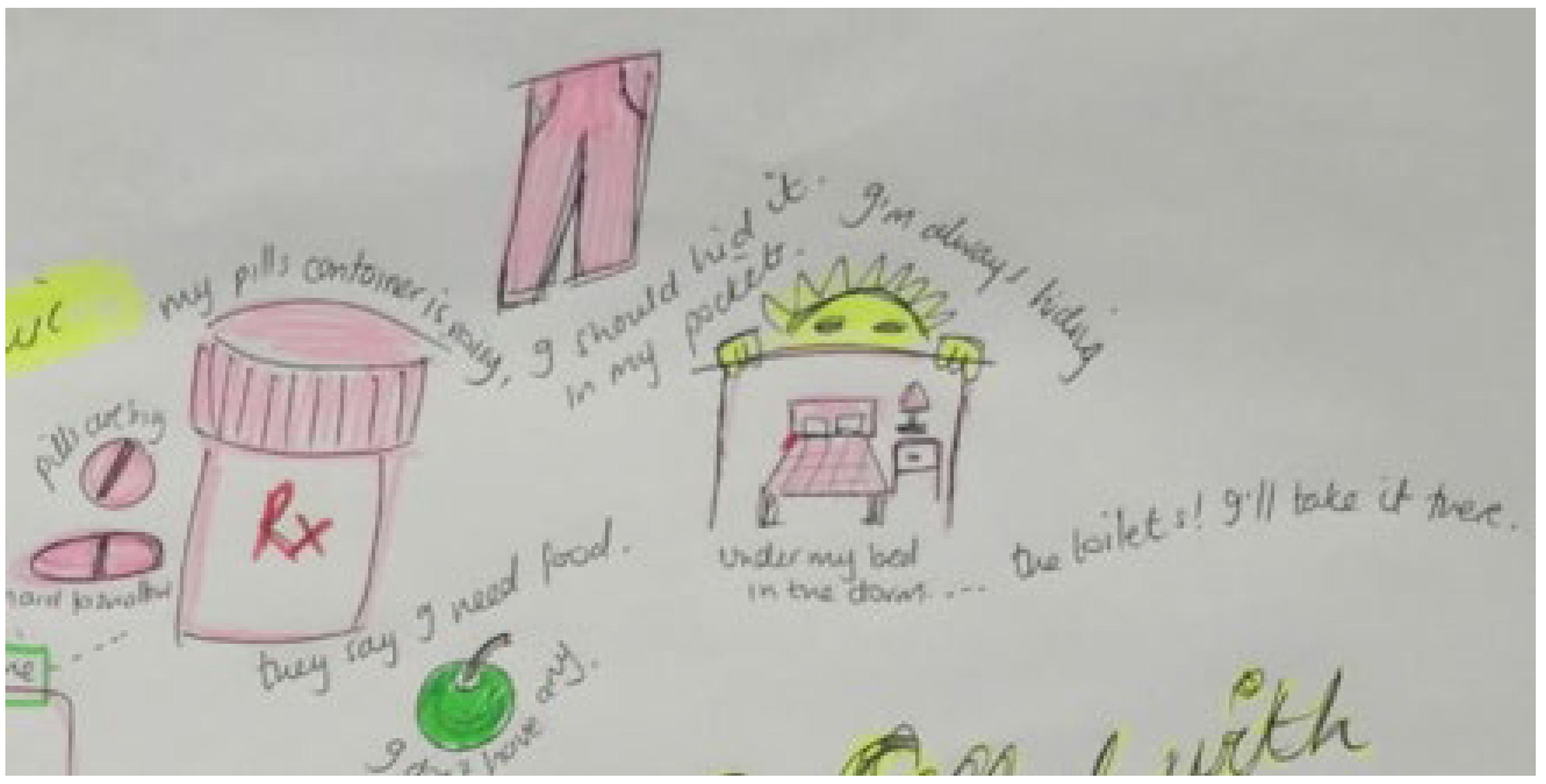
- Storyline 6: Fear of False Judgement and Stigma Forces YLPHIV to Keep Their Pills and Status a Secret (Figure 12)

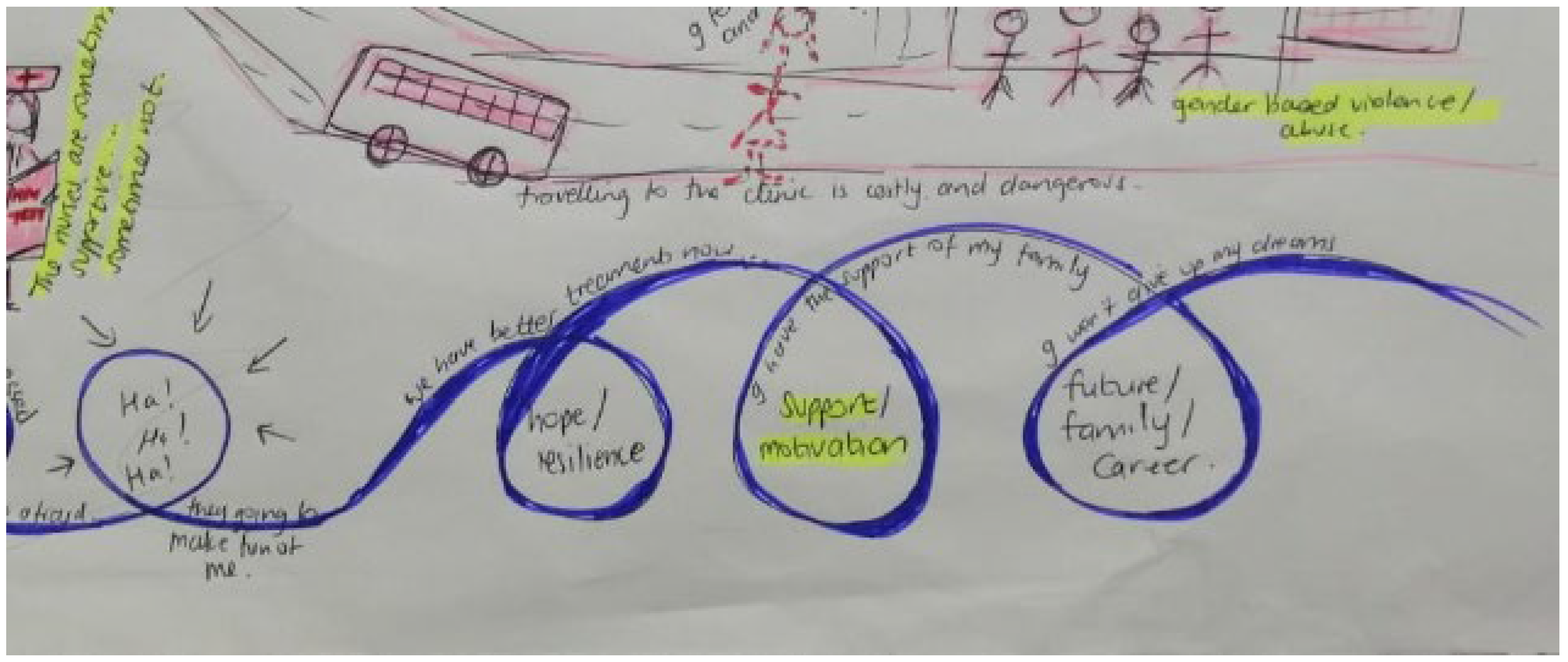
- Storyline 8: Resilience, Motivation, and Future Goals Prompts Adherence as Habitual Behaviour (Figure 15)
- Storyline 9: Places and Spaces in the Community that Support and Threaten Adherence (Figure 16)

4. Discussion
Strengths and Limitations of This Review
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- UNAIDS. Fact Sheet 2021-Latest Global and Regional HIV Statistics. 2021. Available online: https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf (accessed on 21 November 2021).
- Indicators for Monitoring the 2016 United Nations Political Declaration on Ending AIDS. Available online: http://www.unaids.org/sites/default/files/media_asset/global-aids-monitoring_en.pdf (accessed on 27 August 2018).
- AVERT. Global HIV and AIDS Statistics Avert. 2021. Available online: https://www.avert.org/global-hiv-and-aids-statistics (accessed on 21 November 2021).
- Enane, L.A.; Mokete, K.; Joel, D.; Daimari, R.; Tshume, O.; Anabwani, G.; Mazhani, L.; Steenhoff, A.P.; Lowenthal, E.D. “We did not know what was wrong”—Barriers along the care cascade among hospitalized adolescents with HIV in Gaborone, Botswana. PLoS ONE 2018, 13, e0195372. [Google Scholar] [CrossRef] [PubMed]
- Eshaun-Williams, I.; Rohwer, A.; Hendricks, L.; Young, T. Barriers and Facilitators to Linkage, Adherence and Retention among HIV Positive Patients: An Overview of Systematic Reviews. 2017. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=78155 (accessed on 27 August 2018).
- Bekker, L.G.; Hosek, S. HIV and adolescents: Focus on young key populations. J. Int. AIDS Soc. 2015, 18, 20076. [Google Scholar] [CrossRef]
- Hendricks, L.; Eshun-Wilson, I.; Rohwer, A. A mega-aggregation framework synthesis of the barriers and facilitators to linkage, adherence to ART and retention in care among people living with HIV. Syst. Rev. 2021, 10, 54. [Google Scholar] [CrossRef] [PubMed]
- Foster, C.; Ayers, S.; Fidler, S. Antiretroviral adherence for adolescents growing up with HIV: Understanding real life, drug delivery and forgiveness. Ther. Adv. Infect. Dis. 2020, 7, 2049936120920177. [Google Scholar] [CrossRef] [PubMed]
- Kariminia, A.; Law, M.; Davies, M.A.; Vinikoor, M.; Wools-Kaloustian, K.; Leroy, V.; Edmonds, A.; McGowan, C.; Vreeman, R.; Fairlie, L.; et al. Mortality and losses to follow-up among adolescents living with HIV in the IeDEA global cohort collaboration. J. Int. AIDS Soc. 2018, 21, e25215. [Google Scholar] [CrossRef]
- Enimil, A.; Nugent, N.; Amoah, C.; Norman, B.; Antwi, S.; Ocran, J.; Kwara, A.; Barker, D.H. Quality of life among Ghanaian adolescents living with perinatally acquired HIV: A mixed methods study. AIDS Care 2016, 28, 460–464. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2016-09811-010&site=ehost-livedbarker@lifespan.org (accessed on 29 November 2021). [CrossRef]
- Munro, S.; Lewin, S.; Swart, T.; Volmink, J. A review of health behaviour theories: How useful are these for developing interventions to promote long-term medication adherence for TB and HIV/AIDS? BMC Public Health BioMed Cent. 2007, 7, 104. Available online: https://link.springer.com/articles/10.1186/1471-2458-7-104 (accessed on 24 May 2021). [CrossRef]
- Borell-Carrió, F.; Suchman, A.L.; Epstein, R.M. The Biopsychosocial Model 25 Years Later: Principles, Practice, and Scientific Inquiry. Ann. Fam. Med. 2004, 2, 576–582. Available online: https://www.annfammed.org/content/2/6/576 (accessed on 29 November 2021). [CrossRef]
- Engel, G.L. The need for a new medical model: A challenge for biomedicine. Science 1977, 196, 129–136. Available online: https://science.sciencemag.org/content/196/4286/129 (accessed on 24 May 2021). [CrossRef]
- Holtzman, C.W.; Shea, J.A.; Glanz, K.; Jacobs, L.M.; Gross, R.; Hines, J.; Mounzer, K.; Samuel, R.; Metlay, J.P.; Yehia, B.R. Mapping Patient–Identified Barriers and Facilitators to Retention in HIV Care and Antiretroviral Therapy Adherence to Andersen’s Behavioral Model. AIDS Care. 2015, 27, 817–828. [Google Scholar] [CrossRef]
- Katz, I.T.; Ryu, A.E.; Onuegbu, A.G.; Psaros, C.; Weiser, S.D.; Bangsberg, D.R.; Tsai, A.C. Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. J. Int. AIDS Soc. 2013, 16, 18640. [Google Scholar] [CrossRef]
- Monforte, J. What is new in new materialism for a newcomer? Qual. Res. Sport Exerc. Health 2018, 10, 378–390. Available online: https://www.tandfonline.com/doi/abs/10.1080/2159676X.2018.1428678 (accessed on 21 November 2021). [CrossRef]
- Smith, B.; Monforte, J. Stories, new materialism and pluralism: Understanding, practising and pushing the boundaries of narrative analysis. Methods Psychol. 2020, 2, 100016. [Google Scholar] [CrossRef]
- Barad, K. Meeting the Universe Halfway: Quantum Physics and the Entanglement of Matter; Duke University Press: Durham, NC, USA, 2007; Available online: https://books.google.co.za/books/about/Meeting_the_Universe_Halfway.html?id=H41WUfTU2CMC&printsec=frontcover&source=kp_read_button&hl=en&redir_esc=y#v=onepage&q&f=false (accessed on 22 November 2021).
- Coole, D.; Frost, S. (Eds.) New Materialisms: Ontology, Agency and Politics; Duke University Press: Durham, NC, USA, 2010; Available online: http://read.dukeupress.edu/books/book/1465/New-MaterialismsOntology-Agency-and-Politics (accessed on 22 November 2021).
- Lemke, A.A.; Harris-Wai, J.N. Stakeholder engagement in policy development: Challenges and opportunities for human genomics. Genet. Med. 2015, 17, 949–957. [Google Scholar] [CrossRef] [PubMed]
- Braidotti, R. Posthuman Humanities. Eur. Educ. Res. J. 2013, 12, 1–19. Available online: https://journals.sagepub.com/doi/10.2304/eerj.2013.12.1.1 (accessed on 22 November 2021). [CrossRef]
- Colebrook, C.; Buchanan, I. Deleuze and Feminist Theory; Edinburgh University Press: Edinburgh, UK, 2000; p. 250. [Google Scholar]
- DeLanda, M. A New Philosophy of Society: Assemblage Theory and Social Complexity, 1st ed.; Bloomsbury Publishing: London, UK, 2006; Available online: https://www.bloomsbury.com/uk/new-philosophy-of-society-9781441114488/ (accessed on 22 November 2021).
- Fox, N.J.; Alldred, P. Social structures, power and resistance in monist sociology: (New) materialist insights. J. Sociol. 2018, 54, 315–330. Available online: http://www.ncbi.nlm.nih.gov/pubmed/30245583 (accessed on 24 May 2021). [CrossRef]
- Fox, N.J.; Alldred, P. Sociology, environment and health: A materialist approach. Public Health 2016, 141, 287–293. Available online: https://pubmed.ncbi.nlm.nih.gov/27780587/ (accessed on 24 May 2021). [CrossRef]
- Braidotti, R. A Theoretical Framework for the Critical Posthumanities. Theory Cult. Soc. 2018, 36, 31–61. Available online: https://journals.sagepub.com/doi/full/10.1177/0263276418771486 (accessed on 22 November 2021). [CrossRef]
- Slogrove, A.L.; Schomaker, M.; Davies, M.-A.; Williams, P.; Balkan, S.; Ben-Farhat, J.; Calles, N.; Chokephaibulkit, K.; Duff, C.; Eboua, T.F.; et al. The epidemiology of adolescents living with perinatally acquired HIV: A cross-region global cohort analysis. PLoS Med. 2018, 15, e1002514. [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS). 90-90-90: An Ambitious Treatment Target to Help End the AIDS Epidemic. 2014. Available online: http://www.unaids.org/sites/default/files/media_asset/90-90-90_en_0.pdf (accessed on 27 August 2018).
- Enane, L.A.; Apondi, E.; Toromo, J.; Bosma, C.; Ngeresa, A.; Nyandiko, W.; Vreeman, R.C. “A problem shared is half solved”—A qualitative assessment of barriers and facilitators to adolescent retention in HIV care in western Kenya. AIDS Care 2020, 32, 104–112. [Google Scholar] [CrossRef]
- UN General Assembly. Transforming Our World: The 2030 Agenda for Sustainable Development|Department of Economic and Social Affairs. 2015. Available online: https://sdgs.un.org/publications/transforming-our-world-2030-agenda-sustainable-development-17981 (accessed on 28 February 2022).
- Fernández-García, M.P.; Vallejo-Seco, G.; Livácic-Rojas, P.; Tuero-Herrero, E. The (Ir)responsibility of (under)estimating missing data. Front. Psychol. 2018, 9, 556. [Google Scholar] [CrossRef] [PubMed]
- Murris, K. The ‘Missing Peoples’ of critical posthumanism and new materialism. In Navigating the Postqualitative, New Materialist and Critical Posthumanist Terrain across Disciplines; Routledge: London, UK, 2020; pp. 62–84. Available online: https://www.taylorfrancis.com/chapters/edit/10.4324/9781003041177-4/missing-peoples-critical-posthumanism-new-materialism-karin-murris (accessed on 15 August 2022).
- Prüss-Üstün, A.; Wolf, J.; Corvalán, C.F.; Bos, R.; Neira, M.P. Preventing Disease through Healthy Environments: A Global Assessment of the Burden of Disease from Environmental Risks. 2016. Available online: https://apps.who.int/iris/handle/10665/204585 (accessed on 21 November 2021).
- Tong, A.; Flemming, K.; McInnes, E.; Oliver, S.; Craig, J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med. Res. Methodol. 2012, 12, 181. Available online: http://www.biomedcentral.com/1471-2288/12/181 (accessed on 23 May 2021). [CrossRef]
- The World Bank. New World Bank Country Classifications by Income Level: 2021–2022. 2021. Available online: https://blogs.worldbank.org/opendata/new-world-bank-country-classifications-income-level-2021-2022 (accessed on 28 November 2021).
- Critical Appraisal Skills, Programme. CASP Qualitative Studies Checklist. 2018. Available online: https://casp-uk.b-cdn.net/wp-content/uploads/2018/01/CASP-Cohort-Study-Checklist_2018.pdf (accessed on 23 May 2021).
- Ravisankar, R.N. Artmaking as Entanglement: Expanded Notions of Artmaking through New Material; Ohio State University: Columbus, OH, USA, 2019; Available online: https://etd.ohiolink.edu/apexprod/rws_etd/send_file/send?accession=osu1557001719441416&disposition=inline (accessed on 22 November 2021).
- Mayes, E. The mis/uses of ‘voice’ in (post)qualitative research with children and young people: Histories, politics and ethics. Int. J. Qual. Stud. Educ. 2019, 32, 1191–1209. Available online: https://www.tandfonline.com/doi/abs/10.1080/09518398.2019.1659438 (accessed on 14 March 2022). [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. Available online: https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-021-01626-4 (accessed on 28 November 2021). [CrossRef] [PubMed]
- Mutumba, M.; Bauermeister, J.A.; Musiime, V.; Byaruhanga, J.; Francis, K.; Snow, R.C.; Tsai, A.C. Psychosocial challenges and strategies for coping with HIV among adolescents in Uganda: A qualitative study. AIDS Patient Care STDS 2015, 29, 86–94. [Google Scholar] [CrossRef]
- Bakeera-Kitaka, S.; Nabukeera-Barungi, N.; Nöstlinger, C.; Addy, K.; Colebunders, R. Sexual risk reduction needs of adolescents living with HIV in a clinical care setting. AIDS Care 2008, 20, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Bikaako-Kajura, W.; Luyirika, E.; Purcell, D.W.; Downing, J.; Kaharuza, F.; Mermin, J.; Malamba, S.; Bunnell, R. Disclosure of HIV status and adherence to daily drug regimens among HIV-infected children in Uganda. AIDS Behav. 2006, 10 (Suppl. S7), 85–93. [Google Scholar] [CrossRef]
- Inzaule, S.C.; Hamers, R.L.; Kityo, C.; Rinke De Wit, T.F.; Roura, M. Long-term antiretroviral treatment adherence in HIV-infected adolescents and adults in Uganda: A qualitative study. PLoS ONE 2016, 11, e0167492. [Google Scholar] [CrossRef]
- Kawuma, R.; Bernays, S.; Siu, G.; Rhodes, T.; Seeley, J. Children will always be children: Exploring perceptions and experiences of HIV-positive children who may not take their treatment and why they may not tell. Afr. J. AIDS Res. 2014, 13, 189–195. [Google Scholar] [CrossRef]
- MacCarthy, S.; Saya, U.; Samba, C.; Birungi, J.; Okoboi, S.; Linnemayr, S. “How am I going to live?”: Exploring barriers to ART adherence among adolescents and young adults living with HIV in Uganda. BMC Public Health 2018, 18, 1158. [Google Scholar] [CrossRef]
- Nabukeera-Barungi, N.; Elyanu, P.; Asire, B.; Katureebe, C.; Lukabwe, I.; Namusoke, E.; Musinguzi, J.; Atuyambe, L.; Tumwesigye, N. Adherence to antiretroviral therapy and retention in care for adolescents living with HIV from 10 districts in Uganda. BMC Infect. Dis. 2015, 15, 520. [Google Scholar] [CrossRef] [PubMed]
- Ashaba, S.; Cooper-Vince, C.E.; Vořechovská, D.; Rukundo, G.Z.; Maling, S.; Akena, D.; Tsai, A.C. Community beliefs, HIV stigma, and depression among adolescents living with HIV in rural Uganda. Afr. J. AIDS Res. 2019, 18, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Siu, G.E.; Kennedy, C.E.; Bakeera-Kitaka, S. Young people with HIV attending a transition clinic in Kampala, Uganda: An exploratory study of social context, illness trajectories, and pathways to HIV testing and treatment. Child Youth Serv. Rev. 2016, 65, 9–16. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=115265471&site=ehost-live (accessed on 27 July 2021). [CrossRef]
- Petersen, I.; Bhana, A.; Myeza, N.; Alicea, S.; John, S.; Holst, H.; McKay, M.; Mellins, C. Psychosocial challenges and protective influences for socio-emotional coping of HIV+ adolescents in South Africa: A qualitative investigation. AIDS Care 2010, 22, 970–978. [Google Scholar] [CrossRef]
- Hodes, R.; Vale, B.; Toska, E.; Cluver, L.; Dowse, R.; Ashorn, M. ‘Yummy or crummy?’ The multisensory components of medicines-taking among HIV-positive youth. Glob. Public Health 2019, 14, 284–299. [Google Scholar] [CrossRef] [PubMed]
- Cluver, L.D.; Hodes, R.J.; Toska, E.; Kidia, K.K.; Orkin, F.M.; Sherrf, L.; Meinck, F. “HIV is like a tsotsi. ARVs are your guns”: Associations between HIV-disclosure and adherence to antiretroviral treatment among adolescents in South Africa. Aids 2015, 29 (Suppl. S1), S57–S65. [Google Scholar] [CrossRef] [PubMed]
- Loades, M.E.; Coetzee, B.; Du Toit, S.; Kagee, A. ‘But i’m still tired’: The experience of fatigue among South African adolescents receiving antiretroviral therapy. AIDS Care 2018, 30, 746–750. [Google Scholar] [CrossRef]
- Ritchwood, T.D.; Ba, A.; Ingram, L.; Atujuna, M.; Marcus, R.; Ntlapo, N.; Oduro, A.; Bekker, L.; Ritchwood, T.D.; Ba, A.; et al. Community perspectives of South African adolescents ’ experiences seeking treatment at local HIV clinics and how such clinics may influence engagement in the HIV treatment cascade: A qualitative study. AIDS Care 2020, 32, 83–88. [Google Scholar] [CrossRef]
- Rosenbaum, L. Exploring the Social Ecological Factors That Contribute to the Resilience of Adolescents Living with HIV in South Africa: A Photovoice Study; The Chicago School of Professional Psychology: Ann Arbor, MI, USA, 2017; Volume 10634289, Available online: https://www.proquest.com/openview/f6759469e8b50f660d5199c4271b2f17/1?pq-origsite=gscholar&cbl=18750 (accessed on 30 November 2021).
- Woollett, N.; Brahmbhatt, H.; Dodd, K.; Booth, M.; Berman, H.; Cluver, L. Revealing the impact of loss: Exploring mental health through the use of drawing/writing with HIV positive adolescents in Johannesburg. Child Youth Serv. Rev. 2017, 77, 197–207. [Google Scholar] [CrossRef][Green Version]
- Hornschuh, S.; Dietrich, J.J.; Tshabalala, C.; Laher, F. Antiretroviral Treatment Adherence: Knowledge and Experiences among Adolescents and Young Adults in Soweto, South Africa. AIDS Res. Treat. 2017, 2017, 5192516. [Google Scholar] [CrossRef]
- Li, R.J.; Jaspan, H.B.; O’Brien, V.; Rabie, H.; Cotton, M.F.; Nattrass, N. Positive futures: A qualitative study on the needs of adolescents on antiretroviral therapy in South Africa. AIDS Care 2010, 22, 751–758. [Google Scholar] [CrossRef]
- Abubakar, A.; Van De Vijver, F.J.R.; Fischer, R.; Hassan, A.S.; Gona, J.K.; Dzombo, J.T.; Bomu, G.; Katana, K.; Newton, C.R. “Everyone has a secret they keep close to their hearts”: Challenges faced by adolescents living with HIV infection at the Kenyan coast Infectious Disease epidemiology. BMC Public Health 2016, 16, 197. [Google Scholar] [CrossRef]
- Gachanja, G. A rapid assessment of post-disclosure experiences of urban HIV-positive and HIV-negative school-aged children in Kenya. Peer J. 2015, 3, e956. [Google Scholar] [CrossRef]
- Kunapareddy, C.J.; Nyandiko, W.; Inui, T.; Ayaya, S.; Marrero, D.G.; Vreeman, R. A Qualitative Assessment of Barriers to Antiretroviral Therapy Adherence among Adolescents in Western Kenya. J. HIV/AIDS Soc. Serv. 2014, 13, 383–401. [Google Scholar] [CrossRef] [PubMed]
- Luseno, W.K.; Iritani, B.; Zietz, S.; Maman, S.; Mbai, I.I.; Otieno, F.; Ongili, B.; Hallfors, D.D. Experiences along the HIV care continuum: Perspectives of Kenyan adolescents and caregivers. Afr. J. AIDS Res. 2017, 16, 241–250. [Google Scholar] [CrossRef]
- McHenry, M.S.; Nyandiko, W.M.; Scanlon, M.L.; Fischer, L.J.; McAteer, C.I.; Aluoch, J.; Naanyu, V.; Vreeman, R.C. HIV Stigma: Perspectives from Kenyan Child Caregivers and Adolescents Living with HIV. J. Int. Assoc. Provid. AIDS Care 2017, 16, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Vreeman, R.C.; Nyandiko, W.M.; Ayaya, S.O.; Walumbe, E.G.; Marrero, D.G.; Inui, T.S. The perceived impact of disclosure of pediatric HIV status on pediatric antiretroviral therapy adherence, child well-being, and social relationships in a resource-limited setting. AIDS Patient Care STDS. 2010, 24, 639–649. [Google Scholar] [CrossRef]
- Vreeman, R.C.; Nyandiko, W.M.; Ayaya, S.O.; Walumbe, E.G.; Marrero, D.G.; Inui, T.S. Factors sustaining pediatric adherence to antiretroviral therapy in Western Kenya. Qual. Health Res. 2009, 19, 1716–1729. [Google Scholar] [CrossRef] [PubMed]
- Madiba, S.; Josiah, U. Perceived Stigma and Fear of Unintended Disclosure are Barriers in Medication Adherence in Adolescents with Perinatal HIV in Botswana: A Qualitative Study. Biomed. Res. Int. 2019, 2019, 9623159. [Google Scholar] [CrossRef] [PubMed]
- Yang, E.; Mphele, S.; Moshashane, N.; Bula, B.; Chapman, J.; Okatch, H.; Pettitt, E.; Tshume, O.; Marukutira, T.; Anabwani, G.; et al. Distinctive barriers to antiretroviral therapy adherence among non-adherent adolescents living with HIV in Botswana. AIDS Care 2018, 30, 224–231. [Google Scholar] [CrossRef]
- Marukutira, T. Factors influencing adherence to antiretroviral therapy in adolescents at botswana-baylor children’s clinical centre of excellence-a qualitative study. Am. J. Trop. Med. Hyg. 2012, 1, 196. Available online: http://www.ajtmh.org/content/87/5_Suppl_1/150.full.pdf+html (accessed on 21 November 2021).
- Gichane, M.W.; Sullivan, K.A.; Shayo, A.M.; Mmbaga, B.T.; O’ Donnell, K.; Cunningham, C.K.; Dow, D.E. Caregiver role in HIV medication adherence among HIV-infected orphans in Tanzania. AIDS Care 2018, 30, 701–705. [Google Scholar] [CrossRef] [PubMed]
- Nyogea, D.; Mtenga, S.; Henning, L.; Franzeck, F.C.; Glass, T.R.; Letang, E.; Tanner, M.; Geubbels, E. Determinants of antiretroviral adherence among HIV positive children and teenagers in rural Tanzania: A mixed methods study. BMC Infect. Dis. 2015, 15, 28. [Google Scholar] [CrossRef]
- Ramaiya, M.K.; Sullivan, K.A.; O’Donnell, K.; Cunningham, C.K.; Shayo, A.M.; Mmbaga, B.T.; Dow, D.E. A qualitative exploration of the mental health and psychosocial contexts of HIV-positive adolescents in Tanzania. PLoS ONE 2016, 11, e0165936. [Google Scholar] [CrossRef] [PubMed]
- Galano, E.; Turato, E.R.; Delmas, P.; Côté, J.; Gouvea, A.d.F.T.B.; Succi, R.C.d.M.; Machado, D.M. Experiences of adolescents seropositive for HIV/AIDS: A qualitative study. Rev. Paul. Pediatr. 2016, 34, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Cruz, M.L.S.; Bastos, F.I.; Darmont, M.; Dickstein, P.; Monteiro, S. The “moral career” of perinatally HIV-infected children: Revisiting Goffman’s concept. AIDS Care 2015, 27, 6–9. [Google Scholar] [CrossRef]
- de Oliveira, L.L.; Della Negra, M.; Nogueira-Martins, M.C.F. Life Projects of Young Adults with HIV acquired by Vertical Transmission: An exploratory study with patients of an infectious diseases’ outpatients department. Saude Soc. 2012, 21, 928–939. [Google Scholar]
- Denison, J.A.; Banda, H.; Dennis, A.C.; Packer, C.; Nyambe, N.; Stalter, R.M.; Mwansa, J.K.; Katayamoyo, P.; McCarraher, D.R. The sky is the limit: Adhering to antiretroviral therapy and HIV self-management from the perspectives of adolescents living with HIV and their adult caregivers. J. Int. AIDS Soc. 2015, 18, 19358. [Google Scholar] [CrossRef] [PubMed]
- Mburu, G.; Ram, M.; Oxenham, D.; Haamujompa, C.; Iorpenda, K.; Ferguson, L. Responding to adolescents living with HIV in Zambia: A social-ecological approach. Child Youth Serv. Rev. 2014, 45, 9–17. [Google Scholar] [CrossRef]
- Nestadt, D.F.; Lakhonpon, S.; Pardo, G.; Saisaengjan, C.; Gopalan, P.; Bunupuradah, T.; McKay, M.M.K.; Ananworanich, J.; Mellins, C.A. A qualitative exploration of psychosocial challenges of perinatally HIV-infected adolescents and families in Bangkok, Thailand. Vulnerable Child. Youth Stud. 2018, 13, 158–169. [Google Scholar] [CrossRef]
- Xu, L.; Munir, K.; Kanabkaew, C.; Le Coeur, S. Factors influencing antiretroviral treatment suboptimal adherence among perinatally hivinfected adolescents in Thailand. PLoS ONE 2017, 12, e0172392. [Google Scholar]
- Biadgilign, S.; Deribew, A.; Amberbir, A.; Deribe, K. Barriers and facilitators to antiretroviral medication adherence among HIV-infected paediatric patients in Ethiopia: A qualitative study. Sahara J. 2009, 6, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Fetzer, B.C.; Mupenda, B.; Lusiama, J.; Kitetele, F.; Golin, C.; Behets, F. Barriers to and facilitators of adherence to pediatric antiretroviral therapy in a sub-Saharan setting: Insights from a qualitative study. AIDS Patient Care STDS. 2011, 25, 611–621. [Google Scholar] [CrossRef] [PubMed]
- Pinzon-Iregui, M.C.; Ibanez, G.; Beck-Sague, C.; Halpern, M.; Mendoza, R.M. “Like because you are a grownup, you do not need help”: Experiences of Transition from Pediatric to Adult Care among Youth with Perinatal HIV Infection, Their Caregivers, and Health Care Providers in the Dominican Republic. J. Int. Assoc. Provid. AIDS Care 2017, 16, 579–587. [Google Scholar] [CrossRef]
- Bernays, S.; Paparini, S.; Gibb, D.; Seeley, J. When information does not suffice: Young people living with HIV and communication about ART adherence in the clinic. Vulnerable Child. Youth Stud. 2016, 11, 60–68. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2016-12089-006&site=ehost-livesara.paparini@lshtm.ac.uk (accessed on 27 July 2021). [CrossRef]
- Mutwa, P.R.; Van Nuil, J.I.; Asiimwe-Kateera, B.; Kestelyn, E.; Vyankandondera, J.; Pool, R.; Ruhirimbura, J.; Kanakuze, C.; Reiss, P.; Geelen, S.; et al. Living situation affects adherence to combination antiretroviral therapy in HIV-infected adolescents in Rwanda: A qualitative study. PLoS ONE 2013, 8, e60073. [Google Scholar]
- Bernays, S.; Seeley, J.; Rhodes, T.; Mupambireyi, Z. What am I “living” with? Growing up with HIV in Uganda and Zimbabwe. Sociol. Health Illn. 2015, 37, 270–283. [Google Scholar] [CrossRef]
- Mavhu, W.; Berwick, J.; Chirawu, P.; Makamba, M.; Copas, A.; Dirawo, J.; Willis, N.; Araya, R.; Abas, M.A.; Corbett, E.L.; et al. Enhancing Psychosocial Support for HIV Positive Adolescents in Harare, Zimbabwe. PLoS ONE 2013, 8, e70254. [Google Scholar]
- Di Risio, M. Understanding the Barriers and Facilitators to HIV Drug Adherence among Adolescents: An Exploratory Study; University of Toronto (Canada): Ann Arbor, MI, USA, 2008; Volume MR38952, Available online: https://tspace.library.utoronto.ca/bitstream/1807/122921/3/MR38952.PDF (accessed on 21 November 2021).
- Allison, S.M.; Koenig, L.J.; Marhefka, S.L.; Carter, R.J.; Abrams, E.J.; Bulterys, M.; Tepper, V.; Palumbo, P.E.; Bachanas, P.J.; Farley, J.J. Assessing Medication Adherence of Perinatally HIV-Infected Children Using Caregiver Interviews. JANAC J. Assoc. Nurses AIDS Care 2010, 21, 478–488. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=104938563&site=ehost-live (accessed on 21 November 2021). [CrossRef] [PubMed]
- Brackis-Cott, E.; Mellins, C.A.; Abrams, E.; Reval, T.; Dolezal, C. Pediatric HIV medication adherence: The views of medical providers from two primary care programs. J. Pediatr. Healthc. 2003, 17, 252–260. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=106720212&site=ehost-live (accessed on 21 November 2021). [CrossRef]
- Fair, C.D.; Goldstein, B.; Dizney, R. Congruence of Transition Perspectives between Adolescents with Perinatally-Acquired HIV and Their Guardians: An Exploratory Qualitative Study. J. Pediatr. Nurs. 2015, 30, 684–690. [Google Scholar] [CrossRef]
- Fair, C.D.; Sullivan, K.; Dizney, R.; Stackpole, A. “It’s like losing a part of my family”: Transition expectations of adolescents living with perinatally acquired HIV and their guardians. AIDS Patient Care STDS 2012, 26, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Fair, C.D.; Sullivan, K.; Dizney, R.; Stackpole, A. Knowledge of disease markers and quality of patient–provider interaction among adolescents with perinatally acquired HIV: Implications for transition to adult care. Vulnerable Child. Youth Stud. 2014, 9, 167–173. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2014-07559-009&site=ehost-livecfair@elon.edu (accessed on 21 November 2021). [CrossRef]
- Fernet, M.; Lapointe, N.; Lévy, J.J.; Samson, J.; Otis, J.; Wong, K.; Morin, G.; Thériault, J.; Trottier, G. The importance of meanings of antiretroviral treatment and care providers for adherence and transitioning to adult services among youth with perinatally acquired HIV infection. J. HIV AIDS Soc. Serv. 2015, 14, 257–276. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2015-39334-001&site=ehost-livefernet.mylene@uqam.ca (accessed on 21 November 2021). [CrossRef]
- Fernet, M.; Richard, M.E.; Levy, J.J.; Otis, J.; Normand, L.; Johanne, S.; Normand, L.; Johanne, S.; Morin, G.; Wong, K.; et al. Transition to adult clinics in youth living with HIV since birth. Retrovirology 2010, 1, 116. Available online: https://doi.org/10.1186/1742-4690-7-S1-P116 (accessed on 21 November 2021). [CrossRef]
- Fields, E.L.; Bogart, L.M.; Thurston, I.B.; Hu, C.H.; Skeer, M.R.; Safren, S.A.; Mimiaga, M.J. Qualitative Comparison of Barriers to Antiretroviral Medication Adherence Among Perinatally and Behaviorally HIV-Infected Youth. Qual. Health Res. 2017, 27, 1177–1189. [Google Scholar] [CrossRef] [PubMed]
- Garcia, A. Personal Resilience: The Impact on Health Outcomes of Adolescents with Perinatally-Acquired HIV/AIDS; Barry University School of Social Work: Ann Arbor, MI, USA, 2009; Volume 3402010, Available online: http://ezproxy.lib.gla.ac.uk/login?url=https://search.proquest.com/docview/193665519?accountid=14540 (accessed on 27 November 2021).
- Garcia, A. Personal Resilience: The Impact on Health Outcomes of Adolescents with Perinatally-Acquired HIV/AIDS; ProQuest Information & Learning: Morrisville, NC, USA, 2010; Volume 71, Available online: http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2010-99190-496&site=ehost-live (accessed on 27 November 2021).
- Hammer-Fomuki, E.; Konigs, C. Growing up with HIV: Aspects during adolescence and transition. [German]. Padiatr. Prax. 2017, 88, 381–391. Available online: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed18&AN=619152697 (accessed on 27 November 2021).
- Kakkar, F.; Van der Linden, D.; Valois, S.; Maurice, F.; Onnorouille, M.; Lapointe, N.; Soudeyns, H.; Lamarre, V. Health outcomes and the transition experience of HIV-infected adolescents after transfer to adult care in Québec, Canada. BMC Pediatr. 2016, 16, 109. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=117045772&site=ehost-live (accessed on 27 November 2021). [CrossRef]
- Bundock, H.; Fidler, S.; Clarke, S.; Holmes-Walker, D.J.; Farrell, K.; McDonald, S.; Tudor-Williams, G.; Foster, C. Crossing the Divide: Transition Care Services for Young People with HIV-Their Views. AIDS Patient Care STDs. 2011, 25, 465–473. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=104663683&site=ehost-live (accessed on 27 November 2021). [CrossRef]
- Le Roux, E.; Gottot, S.; Aupiais, C.; Girard, T.; Teixeira, M.; Alberti, C. Professional’s Perspectives on Care Management of Young People with Perinatally Acquired HIV during Transition: A Qualitative Study in Adult Care Setting. PLoS ONE 2017, 12, e0169782. [Google Scholar] [CrossRef]
- Ledlie, S.W. The psychosocial issues of children with perinatally acquired HIV disease becoming adolescents: A growing challenge for providers. AIDS Patient Care STDS. 2000, 15, 231–236. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2001-07839-001&site=ehost-livesledlie@attglobal.net (accessed on 27 November 2021). [CrossRef] [PubMed]
- Leonard, E. Attachment, Depression, and Medication in Adolescents with HIV Infection; Institute for Clinical Social Work: Chicago, IL, USA, 2007; Volume 3334416, Available online: http://ezproxy.lib.gla.ac.uk/login?url=https://search.proquest.com/docview/304717805?accountid=14540 (accessed on 27 November 2021).
- MacDonell, K.; Naar-King, S.; Huszti, H.; Belzer, M. Barriers to medication adherence in behaviorally and perinatally infected youth living with HIV. AIDS Behav. 2013, 17, 86–93. Available online: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed14&AN=368649621 (accessed on 27 November 2021). [CrossRef] [PubMed]
- Marhefka, S.L.; Valentin, C.R.; Pinto, R.M.; Demetriou, N.; Wiznia, A.; Mellins, C.A. “I feel like I’m carrying a weapon.” Information and motivations related to sexual risk among girls with perinatally acquired HIV. AIDS Care 2011, 23, 1321–1328. [Google Scholar] [CrossRef]
- Meloni, A.; Tuveri, M.; Floridia, M.; Zucca, F.; Borghero, G.; Gariel, D.; Melis, G.B. Pregnancy care in two adolescents perinatally infected with HIV. AIDS Care 2009, 21, 796–798. Available online: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed11&AN=355647386 (accessed on 27 November 2021). [CrossRef]
- Navarra, A.-M.D.; Whittemore, R.; Bakken, S.; Rosenberg, M.J.; Gormley, M.; Bethea, J.; Gwadz, M.; Cleland, C.; Liang, E.; Melkus, G.D. Adherence Self-Management and the Influence of Contextual Factors Among Emerging Adults with Human Immunodeficiency Virus. Nurs. Res. 2020, 69, 197–209. [Google Scholar] [CrossRef]
- Rodriguez, J. Puerto Rican Adolescents Striving to Live a Normal Life with HIV: A Grounded Theory; The University of Arizona: Ann Arbor, MI, USA, 2009; Volume 3387384, Available online: http://ezproxy.lib.gla.ac.uk/login?url=https://search.proquest.com/docview/304845791?accountid=14540 (accessed on 27 November 2021).
- Szelag, B.J. Growing up with HIV: Disease Management among Perinatally Infected Adolescents; University of South Florida: Ann Arbor, MI, USA, 2011; Volume 3450352, Available online: http://ezproxy.lib.gla.ac.uk/login?url=https://search.proquest.com/docview/864275259?accountid=14540 (accessed on 27 November 2021).
- Williams, E.F.; Ferrer, K.; Lee, M.A.; Bright, K.; Williams, K.; Rakhmanina, N.Y. Growing up with perinatal human immunodeficiency virus—A life not expected. J. Clin. Nurs. 2017, 26, 4734–4744. [Google Scholar] [CrossRef]
- Chenneville, T.; Machacek, M.; Walsh, A.S.J.; Emmanuel, P.; Rodriguez, C. Medication Adherence in 13- to 24-Year-Old Youth Living With HIV. J. Assoc. Nurses AIDS Care 2017, 28, 383–394. [Google Scholar] [CrossRef]
- De Santis, J.P.; Garcia, A.; Chaparro, A.; Beltran, O. Integration versus disintegration: A grounded theory study of adolescent and young adult development in the context of perinatally-acquired HIV infection. J. Pediatr. Nurs. 2014, 29, 422–435. [Google Scholar] [CrossRef]
- Dodds, S.; Blakley, T.; Lizzotte, J.M.; Friedman, L.B.; Shaw, K.; Martinez, J.; Siciliano, C.; Walker, L.E.; Sotheran, J.L.; Sell, R.L.; et al. Retention, adherence, and compliance: Special needs of HIV-infected adolescent girls and young women. J. Adolesc. Health 2003, 33 (Suppl. S1), 39–45. [Google Scholar] [CrossRef]
- Elkington, K.S.; Bauermeister, J.A.; Robbins, R.N.; Gromadzka, O.; Abrams, E.J.; Wiznia, A.; Bamji, M.; Mellins, C.A. Individual and contextual factors of sexual risk behavior in youth perinatally infected with HIV. AIDS Patient Care STDS 2012, 26, 411–422. Available online: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed13&AN=365389351 (accessed on 27 November 2021). [CrossRef] [PubMed]
- Evangeli, M.; Greenhalgh, C.; Frize, G.; Foster, C.; Fidler, S. Parenting considerations in young adults with perinatally acquired HIV. AIDS Care 2014, 26, 813–816. [Google Scholar] [CrossRef] [PubMed]
- Ezekiel, M.J.; Talle, A.; Juma, J.M.; Klepp, K.I. “When in the body, it makes you look fat and HIV negative”: The constitution of antiretroviral therapy in local discourse among youth in Kahe, Tanzania. Soc. Sci. Med. 2009, 68, 957–964. [Google Scholar] [CrossRef] [PubMed]
- Fair, C.D.; Albright, J.N.; Clark, D.M.; Houpt, B. “I definitely want grandbabies”: Caregivers of adolescents with perinatally-acquired HIV reflect on dating and childbearing. Fam. Syst. Health 2016, 34, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Baker, A.N.; Bayer, A.M.; Kolevic, L.; Najarro, L.; Viani, R.M.; Deville, J.G. Child, Caregiver, and Health Care Provider Perspectives and Experiences Regarding Disclosure of HIV Status to Perinatally Infected Children in Lima, Peru. J. Int. Assoc. Provid. AIDS Care 2018, 17, 2325957417752257. [Google Scholar] [CrossRef] [PubMed]
- Bandason, T.; Langhaug, L.F.; Makamba, M.; Laver, S.; Hatzold, K.; Mahere, S.; Munyati, S.; Mungofa, S.; Corbett, E.L.; Ferrand, R.A. Burden of HIV among primary school children and feasibility of primary school-linked HIV testing in Harare, Zimbabwe: A mixed methods study. AIDS Care 2013, 25, 1520–1526. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=104157311&site=ehost-live (accessed on 27 November 2021). [CrossRef] [PubMed]
- Ferrand, R.A.; Trigg, C.; Bandason, T.; Ndhlovu, C.E.; Mungofa, S.; Nathoo, K.; Gibb, D.M.; Cowan, F.M.; Corbett, E.L. Perception of risk of vertically acquired HIV infection and acceptability of provider-initiated testing and counseling among adolescents in Zimbabwe. Am. J. Public Health 2011, 101, 2325–2332. [Google Scholar] [CrossRef] [PubMed]
- Hornschuh, S.; Laher, F.; Makongoza, M.; Tshabalala, C.; Kuijper, L.D.J.; Dietrich, J. Experiences of HIV-positive adolescents and young adults in care in Soweto, South Africa. J. HIV AIDS Soc. Serv. 2014, 13, 420–435. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2014-49216-010&site=ehost-livelaherf@phru.co.za (accessed on 27 November 2021). [CrossRef]
- Wolf, H.T.; Halpern-Felsher, B.L.; Bukusi, E.A.; Agot, K.E.; Cohen, C.R.; Auerswald, C.L. “It is all about the fear of being discriminated [against]⋯the person suffering from HIV will not be accepted”: A qualitative study exploring the reasons for loss to follow-up among HIV-positive youth in Kisumu, Kenya. BMC Public Health 2014, 14, 1154. [Google Scholar] [CrossRef]
- Wolf, H.T.; Davidoff, K.; Auerswald, C.L.; Halpern-Felsher, B.L.; Bukusi, E.A.; Lyon, M.; Cohen, C.R. Health Care Experiences of Youth Living with HIV Who Were Lost to Follow-up in Western Kenya. J. Assoc. Nurses AIDS Care 2019, 30, 539–547. [Google Scholar] [CrossRef]
- Adeniyi, V.O.; Thomson, E.; Ter Goon, D.; Ajayi, I.A. Disclosure, stigma of HIV positive child and access to early infant diagnosis in the rural communities of OR Tambo District, South Africa: A qualitative exploration of maternal perspective. BMC Pediatr. 2015, 15, 98. [Google Scholar] [CrossRef]
- Atuyambe, L.; Neema, S.; Otolok-Tanga, E.; Wamuyu-Maina, G.; Kasasa, S.; Wabwire-Mangen, F. The effects of enhanced access to antiretroviral therapy: A qualitative study of community perceptions in Kampala city, Uganda. Afr. Health Sci. 2008, 8, 13–19. [Google Scholar] [PubMed]
- Besada, D.; Goga, A.; Daviaud, E.; Rohde, S.; Chinkonde, J.R.; Villeneuve, S.; Clarysse, G.; Raphaely, N.; Okokwu, S.; Tumwesigye, N. Roles played by community cadres to support retention in PMTCT Option B+ in four African countries: A qualitative rapid appraisal. BMJ Open 2018, 8, e020754. [Google Scholar] [CrossRef] [PubMed]
- Black, S.; Zulliger, R.; Marcus, R.; Mark, D.; Myer, L.; Bekker, L.G. Acceptability and challenges of rapid ART initiation among pregnant women in a pilot programme, Cape Town, South Africa. AIDS Care 2014, 26, 736–741. [Google Scholar] [CrossRef] [PubMed]
- Buregyeya, E.; Naigino, R.; Mukose, A.; Makumbi, F.; Esiru, G.; Arinaitwe, J.; Musinguzi, J.; Wanyenze, R.K. Facilitators and barriers to uptake and adherence to lifelong antiretroviral therapy among HIV infected pregnant women in Uganda: A qualitative study. BMC Pregnancy Childbirth 2017, 17, 94. [Google Scholar] [CrossRef] [PubMed]
- Byakika-Tusiime, J.; Crane, J.; Oyugi, J.H.; Ragland, K.; Kawuma, A.; Musoke, P.; Bangsberg, D.R. Longitudinal antiretroviral adherence in HIV+ Ugandan parents and their children initiating HAART in the MTCT-Plus family treatment model: Role of depression in declining adherence over time. AIDS Behav. 2009, 13 (Suppl. S1), 82–91. [Google Scholar] [CrossRef]
- Catz, S.L.; Meredith, K.L.; Mundy, L.M. Women’s HIV transmission risk perceptions and behaviors in the era of potent antiretroviral therapies. AIDS Educ. Prev. 2001, 13, 239–251. [Google Scholar] [CrossRef]
- Taylor, B.S.; Reyes, E.; Levine, E.A.; Khan, S.Z.; Garduno, L.S.; Donastorg, Y.; Hammer, S.M.; Brudney, K.; Hirsch, J.S. Patterns of geographic mobility predict barriers to engagement in HIV care and antiretroviral treatment adherence. AIDS Patient Care STDS 2014, 28, 284–295. [Google Scholar] [CrossRef]
- Theuring, S.; Nchimbi, P.; Jordan-Harder, B.; Harms, G. Partner involvement in perinatal care and PMTCT services in Mbeya Region, Tanzania: The providers’ perspective. AIDS Care 2010, 22, 1562–1568. [Google Scholar] [CrossRef]
- Acree, M.E. Transition of Care for Youth with HIV. Pediatr. Ann. 2017, 46, E198–E202. [Google Scholar] [CrossRef]
- Buchanan, A.L.; Montepiedra, G.; Sirois, P.A.; Kammerer, B.; Garvie, P.A.; Storm, D.S.; Nichols, S.L. Barriers to medication adherence in HIV-infected children and youth based on self- and caregiver report. Pediatrics 2012, 129, e1244–e1251. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2012-11884-010&site=ehost-liveslnichols@ucsd.edu (accessed on 27 November 2021). [CrossRef]
- Cluver, L.; Pantelic, M.; Toska, E.; Orkin, M.; Casale, M.; Bungane, N.; Lorraine Sherr. STACKing the odds for adolescent survival: Health service factors associated with full retention in care and adherence amongst adolescents living with HIV in South Africa. J. Int. AIDS Soc. 2018, 21, 8. [Google Scholar] [CrossRef]
- DeLaMora, P.; Aledort, N.; Stavola, J. Caring for adolescents with HIV. Curr. HIV/AIDS Rep. 2006, 3, 74–78. [Google Scholar] [CrossRef]
- Garcia-Navarro, C.; Garcia, I.; Medin, G.; Ramos-Arnador, J.T.; Navarro-Gomez, M.; Mellado-Pena, M.J.; de José Gómez, M.I.; Cortés, M.; Crespo, B.Z.; Muñoz-Fernandez, M.A.; et al. Psychosocial aspects in a cohort of vertically transmitted human immunodeficiency virus-infected adolescents. Enferm. Infecc. Microbiol. Clin. 2014, 32, 631–637. [Google Scholar] [CrossRef]
- Kreniske, P.; Grilo, S.; Nakyanjo, N.; Nalugoda, F.; Wolfe, J.; Santelli, J.S. Narrating the Transition to Adulthood for Youth in Uganda: Leaving School, Mobility, Risky Occupations, and HIV. Health Educ. Behav. 2019, 46, 550–558. [Google Scholar] [CrossRef]
- Manaboriboon, B.; Lolekha, R.; Chokephaibulkit, K.; Leowsrisook, P.; Naiwatanakul, T.; Tarugsa, J.; Durier, Y.; Aunjit, N.; Vandepitte, W.P.; Boon-Yasidhi, V. Psychosocial needs of perinatally HIV-infected youths in Thailand: Lessons learnt from instructive counseling. AIDS Care 2016, 28, 1615–1622. [Google Scholar] [CrossRef] [PubMed]
- Mbika Cardorelle, A.; Toussoungamana-Peka, S.A.; Mapapa Miakassissa, C.; Okoko, A. Compliance with antiretroviral therapy in HIV-infected adolescents in Brazzaville, Congo. Arch. Pediatrie Organe Off. Soc. Fr. Pediatrie 2014, 21, 105–107. Available online: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med8&NEWS=N&AN=24290179 (accessed on 27 November 2021).
- Nicholson, O.; Mellins, C.; Dolezal, C.; Brackis-Cott, E.; Abrams, E.J. HIV treatment-related knowledge and self-efficacy among caregivers of HIV-infected children. Patient Educ. Couns. 2006, 61, 405–410. [Google Scholar] [CrossRef]
- Baptiste, D.R.; Bhana, A.; Petersen, I.; McKay, M.; Voisin, D.; Bell, C.; Martinez, D.D. Community collaborative youth-focused HIV/AIDS prevention in South Africa and Trinidad: Preliminary findings. J. Pediatr. Psychol. 2006, 31, 905–916. [Google Scholar] [CrossRef]
- Birungi, H.; Mugisha, J.F.; Obare, F.; Nyombi, J.K. Sexual Behavior and Desires among Adolescents Perinatally Infected with Human Immunodeficiency Virus in Uganda: Implications for Programming. J. Adolesc. Health 2009, 44, 184–187. Available online: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed11&AN=50303814 (accessed on 27 November 2021). [CrossRef] [PubMed]
- Earnshaw, V.A.; Kidman, R.C.; Violari, A. Stigma, Depression, and Substance Use Problems among Perinatally HIV-Infected Youth in South Africa. AIDS Behav. 2018, 22, 3892–3896. [Google Scholar] [CrossRef]
- Elkington, K.S.; Bauermeister, J.A.; Brackis-Cott, E.; Dolezal, C.; Mellins, C.A. Substance use and sexual risk behaviors in perinatally human immunodeficiency virus-exposed youth: Roles of caregivers, peers and HIV status. J. Adolesc. Health 2009, 45, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Levine, A.B.; Aaron, E.; Foster, J. Pregnancy in perinatally HIV-infected adolescents. J. Adolesc. Health 2006, 38, 765–768. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=106331043&site=ehost-live (accessed on 27 November 2021). [CrossRef] [PubMed]
- Haraway, D. A Manifesto for Cyborgs: Science, Technology, and Socialist Feminism in the 1980s. 1985. Available online: https://monoskop.org/images/4/4c/Haraway_Donna_1985_A_Manifesto_for_Cyborgs_Science_Technology_and_Socialist_Feminism_in_the_1980s.pdf (accessed on 22 November 2021).
| Dimension | Theme | Material Marker | Storyline |
|---|---|---|---|
| Biological | Changes in the body | Rashes, acne, hair loss, physically weaker or stronger | Bodily changes, internal stigma, and suicidal ideation |
| Poverty and food insecurity | Food and money | Weighing up health against socio-economic constraints and educational priorities | |
| Biological sensations | Nausea, hard to swallow big tablets | Bodily changes, internal stigma, and suicidal ideation | |
| Treatment failure | Returning to the clinic, feeling sick and weak, visits to clinic or hospitalisation | Bodily changes, internal stigma, and suicidal ideation Navigating clinic visits, health care workers, and privacy | |
| Psychological | Motivation, hope, and resilience | Condoms for protective sex, child/future children, desire for employment and ‘normal’ life | Resilience, motivation, and future goals prompts adherence as a habitual behaviour |
| Internal stigma, depression, and suicidal ideation | Linked to physical appearance. Whole world feels like a box you are trapped inside Rat poison, throw myself into a lake, cut my neck and die, and feeling trapped in a box | Bodily changes, internal stigma, and suicidal ideation | |
| Fear of disclosure and secrets | Not being honest with friends by hiding pills inside tables, under pillows and beds, and in pants pockets. Noisy pill bottles and the colour of the pills. | Fear of false judgement and stigma forces YLPHIV to keep their pills and status a secret | |
| Knowing and fearing loss | Loss of parent/s or family members. Fear of losing romantic partners. | Grieving loss of caregivers and challenging familial relationships Fear of false judgement and stigma forces YLPHIV to keep their status a secret | |
| Socio-cultural | Romantic relationships and intimate partner violence | Cheating with another person, condoms, protective sex, broken hearts, sperm, partner does not want to have sex, partner wants to have unprotected sex, gender-based violence/action of hitting, and words being said that are humiliating. | Negotiating power, sex, and risky behaviours |
| Familial relationships | YLPHIV treated differently to siblings, food is separate, only one taking medication, additional chores (brooms, dishes, and laundry), no expectation to finish school, loss of parents. | Grieving loss of caregivers and challenging familial relationships | |
| Peer pressure and friendships | Hiding pills away from friends, staying at home when not feeling well. | Fear of false judgement and stigma forces YLPHIV to keep their status a secret | |
| Substance use and abuse | Alcohol and other substances, no condoms. | Negotiating power, sex, and risky behaviours | |
| Places in communities | Church or mosque linked to hope, bus stops, and taxi ranks linked to travel to clinic and work, busy street, and long roads to walk to the clinic, community members seeing YLPHIV at the clinic or waiting in a queue. | Navigating clinic visits, health care workers, and privacy Places and spaces in the community that support and threaten | |
| Socio-economic context | Low-income community, community violence—guns, gangsters standing on street corners and in the roads, no food to take medicine | Weighing up health against socio-economic constraints and educational priorities | |
| Health system-political | Location of the clinic | May be too far to walk—need transport (bus, taxi, or car)—may be expensive (money) | Weighing up health against socio-economic constraints and educational priorities |
| Health care workers and consultations | The test, accompanying family member, space in clinic may be crowded with no privacy, patient folder, the health care worker, doctors | Navigating clinic visits, health care workers, and privacy Disclosure and psychological reactions to HIV diagnosis | |
| The clinic | Information pamphlets, posters on the wall, all the patients in the clinic, the building and what it represents to the community, collecting medicines, place to go when sick | Navigating clinic visits, health care workers, and privacy Places and spaces in the community that support and threaten | |
| School | Choose going to school versus going to clinic, hiding pills inside table or under bed at boarding school. Hiding pills in pants pockets, going to the toilet to take it | Navigating clinic visits, health care workers, and privacy Fear of false judgement and stigma forces YLPHIV to keep their status a secret Weighing up health against socio-economic constraints and educational priorities |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hendricks, L.A.; Young, T.; Van Wyk, S.S.; Matheï, C.; Hannes, K. Storyboarding HIV Infected Young People’s Adherence to Antiretroviral Therapy in Lower- to Upper Middle-Income Countries: A New-Materialist Qualitative Evidence Synthesis. Int. J. Environ. Res. Public Health 2022, 19, 11317. https://doi.org/10.3390/ijerph191811317
Hendricks LA, Young T, Van Wyk SS, Matheï C, Hannes K. Storyboarding HIV Infected Young People’s Adherence to Antiretroviral Therapy in Lower- to Upper Middle-Income Countries: A New-Materialist Qualitative Evidence Synthesis. International Journal of Environmental Research and Public Health. 2022; 19(18):11317. https://doi.org/10.3390/ijerph191811317
Chicago/Turabian StyleHendricks, Lynn A., Taryn Young, Susanna S. Van Wyk, Catharina Matheï, and Karin Hannes. 2022. "Storyboarding HIV Infected Young People’s Adherence to Antiretroviral Therapy in Lower- to Upper Middle-Income Countries: A New-Materialist Qualitative Evidence Synthesis" International Journal of Environmental Research and Public Health 19, no. 18: 11317. https://doi.org/10.3390/ijerph191811317
APA StyleHendricks, L. A., Young, T., Van Wyk, S. S., Matheï, C., & Hannes, K. (2022). Storyboarding HIV Infected Young People’s Adherence to Antiretroviral Therapy in Lower- to Upper Middle-Income Countries: A New-Materialist Qualitative Evidence Synthesis. International Journal of Environmental Research and Public Health, 19(18), 11317. https://doi.org/10.3390/ijerph191811317