Abstract
The estimated number of Substance Users (SU) globally has currently reached a very high number and is still increasing. This aspect necessitates appropriate interventions for prevention and specific treatments. The literature shows that digital treatments can be useful in the context of health services and substance abuse. This systematic review focuses mainly on research on the effectiveness of digital treatments for SU. Data sources included studies found on PsycINFO, PubMed, SCOPUS, and WebOfScience (WOS) database searches. The following keywords were used: TITLE (digital OR computer OR software OR tablet OR app OR videogame OR seriousgame OR virtualreality) AND ABSTRACT((mental AND health) AND (addiction OR dependence OR substance OR drug)). We focused on peer-reviewed articles published from 2010 through 2021 using PRISMA guidelines. A total of 18 studies met the inclusion criteria (i.e., type of intervention, efficacy in terms of misuse of substances and scored outcomes from questionnaire or toxicology tests, study methodology). The studies included investigations of specific digital treatments for SU of various kinds of drugs. The interventions were administered using personal computers, smartphones, or, in a few cases, tablets. Most of the interventions focused on the cognitive behavior therapy (CBT) model and/or on the use strategies, tips, or feedback. A minority provided information or training programs. The current review shows that digital treatments and interventions are effective in reducing the frequency of use, augmenting abstinence, or reducing the gravity of dependence for most of the studies at post-treatment. However, due to the heterogeneity of the variables (i.e., substance type, digital tool used, and treatment administered), there was a reduced generalizability of the results. This review highlights the need to continue the research in this field, and above all, to create effective digital protocols.
Keywords:
substance use; digital treatments; alcohol; marijuana/cannabis; amphetamines; cocaine; tobacco; opioids; heroin; benzodiazepines 1. Introduction
Digital treatments can be useful in the context of health services. Our attention is directed to digital treatments for mental health [1] and, especially, to dependence disorders [2,3,4,5]. There is increasing evidence of the expansion of digital tools and systems for assessment, intervention, support, and prevention in the field of mental health thanks to, in part, the evidence provided by many studies and scientific research on the effectiveness of these treatments in helping people with mental health disorders [6]. The convergence of digital technologies with the fields of mental health and health care, which we can refer to as digital health or mHealth, has allowed for the increasing development and diffusion of these technological tools, resulting in continuous innovation. This field is increasingly active and growing, and treatments range from screening and monitoring to diagnosis and therapies (often administered alongside traditional therapies) [7,8,9,10,11,12,13,14]. It makes use of ‘wearable’ devices—such as virtual reality helmets, patches, digital patches, and tattoos—that have innumerable screening and monitoring functions and make use of increasingly innovative technologies using artificial intelligence algorithms and nanotechnology. By contrast, ‘nonwearable’ technologies are based on the use of smartphone applications, computer software and programs, internet platforms with psychoeducational or therapeutic purposes, video games or training, avatars, or typical chat tools (such as chatbots) implementing artificial intelligence technologies [15]. The relationship between health and digitalization was strongly highlighted by the COVID-19 pandemic [16,17]. These unprecedented times led to a big ‘boom’ in the use of technology in the health and mental health fields, as many people experienced the difficulties of accessing services in the traditional way [18]. These technologies can help fill possible gaps due to difficult access to care, especially for younger people, who are more prone to seeking technology-based healthcare services. Digital interventions also have other advantages, such as availability at any day of the week and at any hour (especially if they do not require an operator, as in the case of chatbot interventions) and can be ‘on-demand’. In addition, many interventions have lower costs than traditional treatments. Finally, they can help people who do not access services in the traditional way due to shame and social stigma, thus increasing the number of people who can use them [19]. Illness has costs for the individual and society; therefore, it is necessary to find as many solutions as possible to promote health and increase access to health services (including digital healthcare solutions). Among health preservation services, special attention should be paid to addiction or substance abuse [4,20]. Although many studies and reviews [12,13] have focused on SU, more research is needed to prove the effectiveness of specific digital treatments.
This is the reason why in this systematic review we focus on the digital based treatments for SU [21,22]. SU is referred to habitual substance users and can also include substance use disorders. A body of literature [5,23,24,25,26] shows the benefit of using digital mode to reach people who have limited access to treatments or presents other limitations in accessing standard protocols. However, the field of digital interventions for treating the use of substances is vast and varied, and likewise, the interventions for such disorders, and the digital tools currently available.
A principal point to consider in SU is that a dependent person lacks sufficient control over the use of a drug, thus acting with behavioral dyscontrol and in a discontinuum. A principal characteristic of dependence syndromes is the uncontrollable desire to use substances such as drugs, alcohol, or tobacco. The literature also underlines that in dependence syndromes, returning to substance use after a period of abstinence causes a more rapid reappearance of the features of the syndrome that occur in nondependent subjects [27].
In addition, SU sometimes are refractory to any type of treatment and have very high drop-out rates. Whereas in-person treatments have been validated and have provided effective protocols, digital treatments do not have such a long history, and very often, their protocols is not tied to the interface. If there are existing effective protocols, there needs to be more connection between those who make the content and those who create the technological instruments. Teamwork is needed to integrate the strengths of in-person interventions with those of digital interventions. There is also a lack of individualized treatments at the technology level. Hence, more focus is needed on this aspect.
This systematic review was made in order to better understand (i) the effectiveness of digital treatments for SU, (ii) results indicated in each study, and (iii) which kind of digital treatment is more effective in relation to the population of the study and to the specific substance used. Furthermore, this review was designed to provide a framework that would aid researchers in evaluating new literature, give new directions for future research, and help to create useful and shareable treatments with adequate digital support.
2. Methods
2.1. Overview
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines [28,29].
PsycINFO, PubMed, SCOPUS, and Web of Science (WOS) databases were systematically searched, using the following keywords: TITLE (digital OR computer OR software OR tablet OR app OR videogame OR seriousgame OR virtualreality) AND ABSTRACT ((mental AND health) AND (addiction OR dependence OR substance OR drug)). The search strategy has been included as Supplementary Materials S1. We focused on peer-reviewed articles published from 2010 through 2021. Results were limited to English, Italian, and Spanish language peer-reviewed journal publications. Primary searches were completed in December 2021.
2.2. Inclusion and Exclusion Criteria
To be included in the review, studies had to report treatments using digital technology (i.e., using a computer, APP, tablet, or smartphone) for SU. SU participants should have been selected either through formal diagnosis or self-identification of current or past problematic substance use. Outcomes have to be measured through validated and/or standardized questionnaires (e.g., Alcohol Use Disorders Identification Test or AUDIT) or through the Visual Analogue Scale, or questions asked by the authors of participants and directly related to SU. Studies were also included if they refer to participants with several psychiatric disorders, including SU.
Book chapters, meta-analyses, reviews, comments, letters, and theoretical papers were excluded. Studies were also excluded if they: (i) did not report a digital technology treatment for SU; (ii) considered problematic internet, app, or computer use; (iii) reported use of the tools (e.g., computer or tablet) to administer surveys; (iv) used Virtual Reality to reproduce the effects of drugs (e.g., hallucinations); (v) reported a standardization or validation of a treatment using an app or a serious game. Moreover, ad hoc, or non-validated instruments or indirect outcomes (e.g., depression or anxiety) were not considered as outcomes.
2.3. Study Selection and Extraction Steps
All identified citations were imported into the bibliographic manager software Zotero 5.0 (Corporation for Digital Scholarship, Vienna, VA, USA). Duplicates were identified and removed, after which abstracts, and titles were screened by two independent reviewers (MLM and NSB) for eligibility. Discordant eligibility determinations were resolved by consensus.
The full texts of the eligible records were then obtained and screened for eligibility according to the exclusion criteria. Any doubts or conflicts were resolved by discussion between the three reviewers (M.L.M., N.S.B., and M.P.P.), to reach a consensus.
2.4. Data Extraction
Two independent reviewers (M.L.M. and N.S.B.) created a data extraction standardized form in Microsoft Word (Microsoft Corporation, Redmond, WA, USA). The first author, year of publication, number of participants, diagnosis of participants, age, study setting, comparator, outcomes, type of treatments, and devices used were extracted from each included study. Any discrepancies in the extracted data were resolved by a third reviewer (M.P.P.).
2.5. Synthesis
The study quality and characteristics of interest were tabulated and narratively described. Two independent reviewers (M.L.M. and N.S.B.) assessed the quality of retrieved studies [30]. A standardized quality tool was used based on the following quality criteria (see Supplemental Material S2): a minimum of 50 subjects per sample, validated measures, follow-up, pre-post training design, randomized subject selection and/or condition, presence of control condition, presence of placebo condition, and evidence of utility.
Each criterion was recorded as 1 (present) or 0 (absent). Score ranged from 0 to 8. The higher the score the higher the quality of the study.
3. Results
3.1. Study Selections and Extractions
A total of 530 abstracts were located, of which 325 were removed, being duplicates. A total of 205 studies were screened against titles and abstracts. Subsequently, 139 studies were excluded, and among the 66 studies assessed for full-text eligibility, 48 studies were excluded. A total of 18 studies finally met our inclusion criteria and were included (Figure 1). In the final selection, only English studies were included.
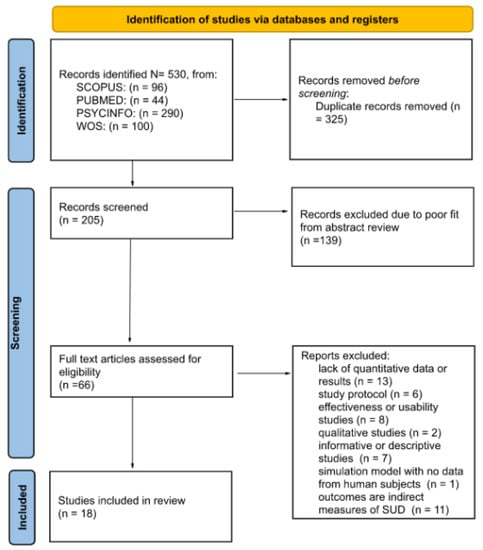
Figure 1.
Systematic literature search, screening, and relevance assessment conducted according to PRISMA guidelines.
3.2. Study Characteristics
We summarized the key results of the study characteristics in Table 1.

Table 1.
Characteristics of publications of treatment(s) with digital technology included in review (N = 18).
A sample size of a total of 25,475 subjects were involved in all the selected studies, of which 7161 were male, 9216 females, and 17 were classified as other gender categories. Two studies did not report gender numerosity. The average age for the participants was 40.9. For most of the studies, the principal substance selected for treatment was alcohol (n = 12), followed by marijuana/cannabis (n = 8), stimulants (e.g., amphetamines or cocaine) (n = 7), tobacco (n = 5), opioids (n = 4), heroin (n = 4), other drugs (n = 3), and benzodiazepines (n = 2). One study did not specify the type of drugs selected.
The majority of the interventions were administered through a personal computer (PC)—i.e., with an on-line platform (n = 14). The use of smartphones (i.e., app for smartphones) was less common (n = 5), as well as tablets (n = 2).
Moreover, the selected studies reported a heterogeneity of the type of approaches and models used for digital treatment. The majority used Cognitive Behavioral Therapy (CBT) (n = 7), followed by Brief Alcohol Intervention (BAI) (n = 2), Informative intervention (n = 2), Attentional Bias (n = 2), Interactive Voice Response (IVR) (n = 1), Digital Recovery Support Services (D-RSS) (n = 1), e-Learning (n = 1), Computer-Guided Therapy (CBI) (n = 1), Self-Determination Therapy (SDT) (n = 1), Health Action Process Approach model (n = 1), Effectiveness of Computer-tailored Smoking Cessation Advice in Primary Care (ESCAPE) (n = 1), and the Information-Motivation-Behavior model (n = 1).
Substance use outcomes were measured with validated measures (n = 13), or as a means of frequencies of substances use (e.g., days of use, quantity of use) (n = 11), abstinence (e.g., days of abstinence) (n = 3), recovery measures (e.g., functioning in domains that are implicated in SUDs) (n = 5), or with biological tests (e.g., urine test) (n = 3).
As regards methodology and study design, most of the selected studies used follow-up assessment (n = 16) or a pre-post evaluation after intervention (n = 2). Fewer studies have divided samples in subgroups (e.g., separate conditions) (n = 10). Of these, nine studies have randomized conditions and seven studies have added control groups/conditions. No studies used a placebo condition.
As regards the results, 17 out of 18 studies indicated obtaining positive results at least for one of the outcomes, as a means of reduced abstinence, days of use, or reduced gravity of addiction. However, only four out of nine studies reported differences of utility between groups or conditions, and three studies did not compare groups or conditions (see Supplemental Material S2).
4. Discussion
This paper aimed to detect effectiveness of existing digital tools in reducing substance use. We used restricted criteria to identify relevant studies and report (i) the type of intervention, (ii) its efficacy in terms of substance misuse and scored outcomes from questionnaire or toxicology tests, and (iii) the study methodology.
Despite the optimism surrounding the use of digital interventions to reduce the misuse of substances such as alcohol and tobacco, the evidences presented on the effects of such interventions are weak. Digitally delivered interventions for substance misuse are likely to require robust evidence of their effectiveness if they are to be widely adopted and compared to real-world interventions and settings.
4.1. Outcomes and Measurements
Overall, 17 out of 18 studies reported at least one positive outcome for the reduction of substance misuse in the evaluated population. Although the study quality and data analysis were generally weak, the results suggested that digital interventions may produce some reduction in substance misuse. However, not all of the selected studies measured substance misuse or the gravity of dependence as primary outcomes.
We found that digital treatments and interventions are effective in reducing substance misuse—more precisely, decreasing the frequency of use, augmenting abstinence, or reducing the gravity of dependence in most of the studies at post-treatment.
In addition, most studies have demonstrated treatment effectiveness as a function of frequency measures, such as abstinence (n = 2) or the reduction in the amount of substance use (n = 9), rather than standardized (n = 3) or objective (n = 1) measures. It would be desirable, in our opinion, to prove the effectiveness of treatment using primarily standardized instruments that measure the severity of addiction and use objective instruments (e.g., biomarkers). In fact, some of the studies selected in this review reported, for example, a reduction in the frequency of use and in scoring scores, albeit not always statistically significant.
Moreover, most of the studies also measured treatment effectiveness for only one substance. A treatment effect on the main substance (reported by the subject) does not imply abstinence from other substances. In fact, the literature shows that people are more likely to use more than one substance (poly-dependence) rather than one (mono-dependence), resulting in increased severity of dependence and difficulty in treatment. Therefore, to obviate possible bias in the results, one should measure the subject’s level of addiction rather than the use of a specific substance.
Finally, only two studies used cognitive bias as a measure of dependence, and only one found a reduction in bias at follow-up. Cognitive bias (e.g., the Stroop effect) is a very reliable proxy measure because it is an objective measure of a subject’s level of addiction. The use of a proxy measure, such as a cognitive bias (widely used in the literature), could increase the reliability of the effectiveness of a digital treatment. The variation in outcome measures and the main use of frequency and abstinence as outcomes—instead of more objective measures—reflects the variability of the aims of the selected studies (e.g., evaluating the cost effectiveness of an intervention), in which substance misuse was considered merely a secondary outcome. It should be noted that this could also reflect the lack of a gold standard for measurements [49], as mentioned by some of the authors in the limitations section of their study [44], despite the existing literature on some of the most studied substances [50,51,52]. A few studies have used an alternative and more objective measure to cover this deficiency: toxicology screening tests [32,42,45]. Nevertheless, toxicology screenings have their own disadvantages, such as the inability to detect mild use and the lack of privacy—users might prefer to avoid face-to-face contact with professionals [2,3].
A minority of the selected studies computed the effect size [38,39,40] and found low or medium effect sizes. If we compare the effect sizes resulting from digital interventions, as reported in this review, with those of real-world interventions, we observe that real-world treatment interventions produce not only small or medium but also large effect sizes [53,54]. Therefore, we suggest that future studies investigate novel approaches to increasing the effect sizes of digital interventions.
4.2. Models and Approaches
Most of the interventions focused on the CBT model and/or on the use of strategies (i.e., coping strategies), tips, or feedbacks. A minority provided information or training programs (i.e., attentional bias). However, the variability of models and approaches on which the interventions in the selected studies were based and the presence of very few studies reporting multi-interventions-combinations of digital intervention [31,34,36] and comparisons with the control condition (see Supplemental Material S1) reduce the generalizability of the determined utility and effectiveness of the strategies used.
Regarding the effectiveness of treatments, those based on continuous programs to be carried out in different steps, tailored with exercises and training, seem to be more effective than short or spot interventions. For example, some teach how to use coping strategies and require the subjects to follow a program over a certain period, some engage subjects in psychoeducation or behavioral change programs (such as CBT) structured over a long period, while others are tailored to the patients’ needs and provide counseling forums and materials. In our opinion, greater effectiveness might be achieved by (a) medium- and long-term treatments requiring continuity from the subject or (b) by having a solid theoretical basis that has been proven to be effective in treating addiction. From this point of view, it might be the treatment itself that is already effective, regardless of whether digital technology is used or not.
4.3. Methodology and Intervention Design
Only three studies were able to blind personnel [31,36,52] and no studies reported blinding participants to ensure that they were unaware of the other conditions and that the outcome measures were unaffected by possible knowledge of the received intervention. This leads to a high risk of performance and detection bias that, however, depends on the nature of the digitally delivered behavioral interventions in most of the included studies.
Follow-up assessments indicated that the post-treatment effects were sustained for up to three months from the interventions. This indicates that digital intervention is a suitable approach to achieve a lasting small reduction in substance use. However, many studies evaluate interventions within 12 months and only one study evaluates intervention over 12 months [33]. Future research should aim to evaluate the effectiveness of digital intervention programs beyond three years to better understand how program effects can be sustained. Moreover, only a few studies compared and reported differences between the groups, despite having divided their samples into subgroups. This could be a methodological weakness leading to nongeneralized results.
However, the moderate successes of digital interventions support the notion that interventions for substance misuse may have an impact of utility. Although not the focus of this study, it has been widely acknowledged that digital interventions are more likely to be successful in populations that have played an active role in their design [55,56]. Therefore, future interventions should employ a centered design and intervention (UCDI) approach throughout their design, development, and evaluation to elicit their potential in substance misuse reduction. To pursue this aim, it is essential that the core user is carefully defined in the design of these digital interventions to increase the likelihood of addressing user needs and expectations. This may be achieved through techniques such as persona building, storytelling, and role playing [57]. User engagement and the acceptability of an intervention are crucial to its success, indicating that UCDI processes may be a way to increase the effectiveness of digital interventions and should be considered integral to the evaluation process. The use of a UCDI is also important if we assume that most people using drugs (e.g., club drugs) do not want to engage with traditional treatments or support services for fear of stigma and due to concerns about relevance [58,59]
5. Conclusions
The effectiveness of existing digital treatments for reducing substance misuse among SU in a wider population was reviewed. Unfortunately, the overall quality of the 18 included studies was weak; thus, definitive conclusions regarding the effectiveness of these interventions could not be drawn.
There is a clear lack of studies with long-term follow-ups (more than 12 months), control conditions, randomized samples, and blinded conditions. Moreover, there is a lack of evidence for other populations, such as employees and ethnic minority groups. Future primary studies and reviews should include these aspects. In addition, most of the useful results were obtained with self-assessment outcomes and measures, such as frequency of use and days of abstinence. Useful results on validated addiction assessment instruments or through objective tools such as biomarkers and cognitive bias would certainly have given greater reliability to the effectiveness of the treatments used.
A good portion of the studies selected for this review still provided useful results. However, it is possible that these results depended mainly on the use of theoretical models and techniques whose effectiveness are already known from literature. The lack of placebo conditions and comparisons with control conditions represents another weak point that does not help to determine how effective a digital intervention is.
In order to increasingly improve digital health interventions, it is desirable that authors and creators of digital health tools increasingly involve users in the construction of the intervention itself and in the design and guidelines of APPs and software. For example, training and serious games (i.e., serious video games) seem to play a particularly significant role in the field of mHealth. Especially serious games are becoming increasingly relevant. For years, the video game industry has been developing products that not only entertain but are also educational, pedagogical, and therapeutic, focusing on learning, memory, and rehabilitation, and so on, enabling them to reach an increasingly broad audience. In the field of rehabilitation, for example, they make it possible to activate a dynamic process of adaptive and programmed change in the user, in response to an unplanned change due to a problem, disorder, or trauma that the individual presents. The possibilities offered by treatments that use technologies such as serious games and training administered through tablets or PCs are their functionality, their use even at a distance, and above all the possibility of activating a process of short- and long-term changes, thanks to the continuous and constant use of the serious game. The effectiveness of this type of intervention is, thus, in line with the transformations taking place in the field of care services. Certainly, what is crucial is to continue to pursue research in this area that can ensure comprehensive services that are accessible to all, can be functional, effective, reach the greatest number of users, and can be shareable.
In this sense, it is necessary to design studies that involve users, health professionals, designers, and developers to have truly applicable programs for reducing substance abuse and addiction.
However, the results showed in this review suggest that the success of digital interventions may not only be confined to the misuse of illicit substances, but also to other aspects, such as the changing of strategies, self-regulation, and behavioral mechanisms delivered by the interventions [60,61]. Therefore, while digital interventions are a promising development area, it is important that interventions undergo robust creation and evaluation processes, and that effective implementation strategies be used that are best suited to their context [62].
6. Limitations
This study has several strengths and limitations which should be noted. Even though a rigorous search criterion was used, few databases were considered for searching. Moreover, we did not include a gray literature search and reference list screening; thus, relevant studies were potentially missed. The main use of only two reviewers throughout the screening and quality appraisal processes could have led to the risk of bias. Finally, we did not undertake a rigorous quality assessment of the reviews.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph191811309/s1.
Author Contributions
Conceptualization, N.S.B., M.L.M., S.C., and M.P.P.; methodology, N.S.B. and M.L.M.; formal analysis, N.S.B., M.L.M., S.C., and M.P.P.; writing—original draft preparation, N.S.B., M.L.M., S.C., and M.P.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Satre, D.D.; Meacham, M.C.; Asarnow, L.D.; Fisher, W.S.; Fortuna, L.R.; Iturralde, E. Opportunities to Integrate Mobile App-Based Interventions into Mental Health and Substance Use Disorder Treatment Services in the Wake of COVID-19. Am. J. Health Promot. 2021, 35, 1178–1183. [Google Scholar] [CrossRef] [PubMed]
- Boumparis, N.; Schulte, M.H.J.; Riper, H. Digital Mental Health for Alcohol and Substance Use Disorders. Curr. Treat. Options Psychiatry 2019, 6, 352–366. [Google Scholar] [CrossRef]
- Boumparis, N.; Loheide-Niesmann, L.; Blankers, M.; Ebert, D.D.; Korf, D.; Schaub, M.P.; Spijkerman, R.; Tait, R.J.; Riper, H. Short- and Long-Term Effects of Digital Prevention and Treatment Interventions for Cannabis Use Reduction: A Systematic Review and Meta-Analysis. Drug Alcohol Depend. 2019, 200, 82–94. [Google Scholar] [CrossRef] [PubMed]
- Marsch, L.A. Digital Health and Addiction. Curr. Opin. Syst. Biol. 2020, 20, 1–7. [Google Scholar] [CrossRef]
- Steinkamp, J.M.; Goldblatt, N.; Borodovsky, J.T.; LaVertu, A.; Kronish, I.M.; Marsch, L.A.; Schuman-Olivier, Z. Technological Interventions for Medication Adherence in Adult Mental Health and Substance Use Disorders: A Systematic Review. JMIR Ment. Health 2019, 6, e12493. [Google Scholar] [CrossRef]
- Bonfiglio, N.S.; Mascia, M.L.; Penna, M.P. Digital Treatment Paths for Substance Use Disorders (SUDs). Int. J. Environ. Res. Public Health 2022, 19, 7322. [Google Scholar] [CrossRef]
- Musyoka, C.M.; Mbwayo, A.; Donovan, D.M.; Mathai, M. mHealth-Based Peer Mentoring for Prevention of Alcohol and Substance Abuse among First Year University Students: Protocol for Quasi-Experimental Intervention. J. Subst. Use 2021, 26, 53–59. [Google Scholar] [CrossRef]
- Dick, S.; O’Connor, Y.; Thompson, M.J.; O’Donoghue, J.; Hardy, V.; Joseph Wu, T.S.; O’Sullivan, T.; Chirambo, G.B.; Heavin, C. Considerations for Improved Mobile Health Evaluation: Retrospective Qualitative Investigation. JMIR mHealth uHealth 2020, 8, e12424. [Google Scholar] [CrossRef] [PubMed]
- Berrouiguet, S.; Baca-García, E.; Brandt, S.; Walter, M.; Courtet, P. Fundamentals for Future Mobile-Health (mHealth): A Systematic Review of Mobile Phone and Web-Based Text Messaging in Mental Health. J. Med. Internet Res. 2016, 18, e5066. [Google Scholar] [CrossRef]
- Anastasiadou, D.; Folkvord, F.; Lupiañez-Villanueva, F. A Systematic Review of MHealth Interventions for the Support of Eating Disorders. Eur. Eat. Disord. Rev. 2018, 26, 394–416. [Google Scholar] [CrossRef]
- Hutton, A.; Prichard, I.; Whitehead, D.; Thomas, S.; Rubin, M.; Sloand, E.; Powell, T.W.; Frisch, K.; Newman, P.; Goodwin Veenema, T. MHealth Interventions to Reduce Alcohol Use in Young People: A Systematic Review of the Literature. Compr. Child Adolesc. Nurs. 2020, 43, 171–202. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, D.M.; Troutman-Jordan, M.; Whitfield, J.E.; Pappa, E.V. Effectiveness of EHealth Technology-Based Interventions in Reducing Substance Misuse among Older Adults: A Systematic Review. J. Gerontol. Nurs. 2021, 47, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, D.M.; Borsari, B.; Levine, M.J.; Li, S.; Lamberson, K.A.; Matta, L.A. A Systematic Review of the MHealth Interventions to Prevent Alcohol and Substance Abuse. J. Health Commun. 2017, 22, 413–432. [Google Scholar] [CrossRef] [PubMed]
- Rathbone, A.L.; Prescott, J. The Use of Mobile Apps and SMS Messaging as Physical and Mental Health Interventions: Systematic Review. J. Med. Internet Res. 2017, 19, e7740. [Google Scholar] [CrossRef]
- Batra, S.; Baker, R.A.; Wang, T.; Forma, F.; Dibiasi, F.; Peters-Strickland, T. Digital Health Technology for Use in Patients with Serious Mental Illness: A Systematic Review of the Literature. Med. Devices 2017, 10, 237. [Google Scholar] [CrossRef]
- López-Pelayo, H.; Aubin, H.-J.; Drummond, C. “The Post-COVID Era”: Challenges in the Treatment of Substance Use Disorder (SUD) after the Pandemic. BMC Med. 2020, 18, 241. [Google Scholar] [CrossRef]
- Bergman, B.G.; Kelly, J.F. Online Digital Recovery Support Services: An Overview of the Science and Their Potential to Help Individuals with Substance Use Disorder during COVID-19 and Beyond. J. Subst. Abuse Treat. 2021, 120, 108152. [Google Scholar] [CrossRef]
- Balcombe, L.; de Leo, D.; Bustin, S. Digital Mental Health Amid COVID-19. Encyclopedia 2021, 1, 1047–1057. [Google Scholar] [CrossRef]
- Srivastava, V.K. Anatomy of Stigma: Understanding COVID-19. Soc. Chang. 2020, 50, 385–398. [Google Scholar] [CrossRef]
- Marsch, L.A.; Campbell, A.; Campbell, C.; Chen, C.H.; Ertin, E.; Ghitza, U.; Lambert-Harris, C.; Hassanpour, S.; Holtyn, A.F.; Hser, Y.I.; et al. The Application of Digital Health to the Assessment and Treatment of Substance Use Disorders: The Past, Current, and Future Role of the National Drug Abuse Treatment Clinical Trials Network. J. Subst. Abuse Treat. 2020, 112, 4–11. [Google Scholar] [CrossRef]
- Copeland, J.; Martin, G. Web-Based Interventions for Substance Use Disorders: A Qualitative Review. J. Subst. Abuse Treat. 2004, 26, 109–116. [Google Scholar] [CrossRef]
- Nesvåg, S.; Mckay, J.R. Feasibility and Effects of Digital Interventions to Support People in Recovery From Substance Use Disorders: Systematic Review. J. Med. Internet Res. 2018, 20, e9873. [Google Scholar] [CrossRef] [PubMed]
- Eilert, N.; Wogan, R.; Leen, A.; Richards, D. Internet-Delivered Interventions for Depression and Anxiety Symptoms in Children and Young People: Systematic Review and Meta-Analysis. JMIR Pediatrics Parent. 2022, 5, e33551. [Google Scholar] [CrossRef] [PubMed]
- Dugdale, S.; Davies, E.-D. Glyn Are Computer-Based Treatment Programs Effective at Reducing Symptoms of Substance Misuse and Mental Health Difficulties Within Adults? A Systematic Review. J. Dual Diagn. 2019, 15, 291–311. [Google Scholar] [CrossRef] [PubMed]
- Tofighi, B.; Abrantes, A.; Stein, M.D. The Role of Technology-Based Interventions for Substance Use Disorders in Primary Care: A Review of the Literature. Med. Clin. 2018, 102, 715–731. [Google Scholar] [CrossRef]
- Wang, K.; Varma, D.S.; Prosperi, M. A Systematic Review of the Effectiveness of Mobile Apps for Monitoring and Management of Mental Health Symptoms or Disorders. J. Psychiatr. Res. 2018, 107, 73–78. [Google Scholar] [CrossRef]
- O’brien, C. Addiction and Dependence in DSM-V. Addiction 2010, 106, 866–867. [Google Scholar] [CrossRef]
- Page, M.J.; Mckenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Cohen, J.F.; Deeks, J.J.; Hooft, L.; Salameh, J.P.; Korevaar, D.A.; Gatsonis, C.; Hopewell, S.; Hunt, H.A.; Hyde, C.J.; Leeflang, M.M.; et al. Preferred Reporting Items for Journal and Conference Abstracts of Systematic Reviews and Meta-Analyses of Diagnostic Test Accuracy Studies (PRISMA-DTA for Abstracts): Checklist, Explanation, and Elaboration. BMJ 2021, 372, n265. [Google Scholar] [CrossRef]
- dos Santos, W.M.; Secoli, S.R.; de Araújo Püschel, V.A. The Joanna Briggs Institute Approach for Systematic Reviews. Rev. Lat. Am. Enferm. 2018, 26, e3074. [Google Scholar] [CrossRef] [Green Version]
- Chander, G.; Hutton, H.E.; Xu, X.; Canan, C.E.; Gaver, J.; Finkelstein, J.; Lesko, C.R.; McCaul, M.E.; Lau, B. Computer Delivered Intervention for Alcohol and Sexual Risk Reduction among Women Attending an Urban Sexually Transmitted Infection Clinic: A Randomized Controlled Trial. Addict. Behav. Rep. 2021, 14, 100367. [Google Scholar] [CrossRef] [PubMed]
- Cucciare, M.A.; Combs, A.S.; Joshi, G.; Han, X.; Humphreys, K. Computer-Delivered Brief Alcohol Intervention for Patients with Liver Disease: A Randomized Controlled Trial. Addiction 2021, 116, 1076–1087. [Google Scholar] [CrossRef] [PubMed]
- Curtis, B.; Bergman, B.; Brown, A.; McDaniel, J.; Harper, K.; Eisenhart, E.; Hufnagel, M.; Heller, A.T.; Ashford, R. Characterizing Participation and Perceived Engagement Benefits in an Integrated Digital Behavioral Health Recovery Community for Women: A Cross-Sectional Survey. JMIR Ment. Health 2019, 6, e13352. [Google Scholar] [CrossRef] [PubMed]
- Danaher, B.G.; Tyler, M.S.; Crowley, R.C.; Brendryen, H.; Seeley, J.R. Outcomes and Device Usage for Fully Automated Internet Interventions Designed for a Smartphone or Personal Computer: The Mobilequit Smoking Cessation Randomized Controlled Trial. J. Med. Internet Res. 2019, 21, e13290. [Google Scholar] [CrossRef]
- De Ruijter, D.; Hoving, C.; Evers, S.; Hudales, R.; de Vries, H.; Smit, E. An Economic Evaluation of a Computer-Tailored e-Learning Program to Promote Smoking Cessation Counseling Guideline Adherence among Practice Nurses. Patient Educ. Couns. 2019, 102, 1802–1811. [Google Scholar] [CrossRef]
- Drislane, L.E.; Waller, R.; Martz, M.E.; Bonar, E.E.; Walton, M.A.; Chermack, S.T.; Blow, F.C. Therapist and Computer-Based Brief Interventions for Drug Use within a Randomized Controlled Trial: Effects on Parallel Trajectories of Alcohol Use, Cannabis Use and Anxiety Symptoms. Addiction 2020, 115, 158–169. [Google Scholar] [CrossRef]
- Elison-Davies, S.; Märtens, K.; Yau, C.; Davies, G.; Ward, J. Associations between Baseline Opioid Use Disorder Severity, Mental Health and Biopsychosocial Functioning, with Clinical Responses to Computer-Assisted Therapy Treatment. Am. J. Drug Alcohol Abus. 2021, 47, 360–372. [Google Scholar] [CrossRef]
- Elison-Davies, S.; Hayhurst, K.; Jones, A.; Welch, Z.; Davies, G.; Ward, J. Associations between Participant Characteristics, Digital Intervention Engagement and Recovery Outcomes for Participants Accessing ‘Breaking Free Online’ at ‘Change Grow Live’. J. Subst. Use 2021, 26, 497–504. [Google Scholar] [CrossRef]
- Elison-Davies, S.; Wardell, J.D.; Quilty, L.C.; Ward, J.; Davies, G. Examining Correlates of Cannabis Users’ Engagement with a Digital Intervention for Substance Use Disorder: An Observational Study of Clients in UK Services Delivering Breaking Free Online. J. Subst. Abuse Treat. 2021, 123, 108261. [Google Scholar] [CrossRef]
- Elison, S.; Jones, A.; Ward, J.; Davies, G.; Dugdale, S. Examining Effectiveness of Tailorable Computer-Assisted Therapy Programmes for Substance Misuse: Programme Usage and Clinical Outcomes Data from Breaking Free Online. Addict. Behav. 2017, 74, 140–147. [Google Scholar] [CrossRef]
- Han, H.; Zhang, J.Y.; Hser, Y.I.; Liang, D.; Li, X.; Wang, S.S.; Du, J.; Zhao, M. Feasibility of a Mobile Phone App to Support Recovery from Addiction in China: Secondary Analysis of a Pilot Study. JMIR mHealth uHealth 2018, 6, e46. [Google Scholar] [CrossRef] [PubMed]
- Kay-Lambkin, F.J.; Simpson, A.L.; Bowman, J.; Childs, S. Dissemination of a Computer-Based Psychological Treatment in a Drug and Alcohol Clinical Service: An Observational Study. Addict. Sci. Clin. Pract. 2014, 9, 15. [Google Scholar] [CrossRef] [PubMed]
- Leightley, D.; Puddephatt, J.A.; Jones, N.; Mahmoodi, T.; Chui, Z.; Field, M.; Drummond, C.; Rona, R.J.; Fear, N.T.; Goodwin, L. A Smartphone App and Personalized Text Messaging Framework (InDex) to Monitor and Reduce Alcohol Use in Ex-Serving Personnel: Development and Feasibility Study. JMIR mHealth uHealth 2018, 6, e10074. [Google Scholar] [CrossRef] [PubMed]
- Wernette, G.T.; Plegue, M.; Kahler, C.W.; Sen, A.; Zlotnick, C. A Pilot Randomized Controlled Trial of a Computer-Delivered Brief Intervention for Substance Use and Risky Sex during Pregnancy. J. Women’s Health 2018, 27, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Wodarski, J.S.; MacMaster, S.; Miller, N.K. The Use of Computer Technology to Reduce and Prevent College Drinking. Soc. Work Public Health 2012, 27, 270–282. [Google Scholar] [CrossRef]
- Wu, Q.; Parrott, S.; Godfrey, C.; Gilbert, H.; Nazareth, I.; Leurent, B.; Sutton, S.; Morris, R. Cost-Effectiveness of Computer-Tailored Smoking Cessation Advice in Primary Care: A Randomized Trial (ESCAPE). Nicotine Tob. Res. 2014, 16, 270–278. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.W.B.; Heng, S.; Song, G.; Fung, D.S.S.; Smith, H.E. Development of a Co-Designed Gamified Attention Bias Modification App for Individuals with Opioid Use Disorder. Technol. Health Care 2021, 29, 521–526. [Google Scholar] [CrossRef]
- Zhu, Y.; Jiang, H.; Su, H.; Zhong, N.; Li, R.; Li, X.; Chen, T.; Tan, H.; Du, J.; Xu, D.; et al. A Newly Designed Mobile-Based Computerized Cognitive Addiction Therapy App for the Improvement of Cognition Impairments and Risk Decision Making in Methamphetamine Use Disorder: Randomized Controlled Trial. JMIR mHealth uHealth 2018, 6, e10292. [Google Scholar] [CrossRef]
- Carroll, K.M. Methodological Issues and Problems in the Assessment of Substance Use. Psychol. Assess. 1995, 7, 349–358. [Google Scholar] [CrossRef]
- Shorter, G.W.; Heather, N.; Bray, J.W.; Giles, E.L.; Holloway, A.; Barbosa, C.; Berman, A.H.; O’Donnell, A.J.; Clarke, M.; Stockdale, K.J.; et al. The “Outcome Reporting in Brief Intervention Trials: Alcohol” (ORBITAL) Framework: Protocol to Determine a Core Outcome Set for Efficacy and Effectiveness Trials of Alcohol Screening and Brief Intervention. Trials 2017, 18, 611. [Google Scholar] [CrossRef] [Green Version]
- Bonfiglio, N.S.; Renati, R.; Agus, M.; Penna, M.P. Validation of a Substance Craving Questionnaire (SCQ) in Italian Population. Addict. Behav. Rep. 2019, 9, 100172. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Liu, J. Education in and After Covid-19: Immediate Responses and Long-Term Visions. Postdigital Sci. Educ. 2020, 2, 695–699. [Google Scholar] [CrossRef]
- Prendergast, M.; Podus, D.; Finney, J.; Greenwell, L.; Roll, J. Contingency Management for Treatment of Substance Use Disorders: A Meta-Analysis. Addiction 2006, 101, 1546–1560. [Google Scholar] [CrossRef] [PubMed]
- Prendergast, M.L.; Podus, D.; Chang, E.; Urada, D. The Effectiveness of Drug Abuse Treatment: A Meta-Analysis of Comparison Group Studies. Drug Alcohol Depend. 2002, 67, 53–72. [Google Scholar] [CrossRef]
- van Gemert-Pijnen, J.E.; Nijland, N.; Van Limburg, M.; Ossebaard, H.C.; Saskia, M.; Kelders, M.; Eysenbach, G.; Seydel, E.R. A Holistic Framework to Improve the Uptake and Impact of EHealth Technologies. J. Med. Internet Res. 2011, 13, e111. [Google Scholar] [CrossRef]
- Mazzoleni, M.; Previdi, F.; Bonfiglio, N.S. Classification Algorithms Analysis for Brain–Computer Interface in Drug Craving Therapy. Biomed. Signal. Process Control. 2019, 52, 463–472. [Google Scholar] [CrossRef]
- Gulliksen, J.; Göransson, B.; Boivie, I.; Blomkvist, S.; Persson, J.; Cajander, Å. Key Principles for User-Centred Systems Design. Behav. Inf. Technol. 2010, 22, 397–409. [Google Scholar] [CrossRef]
- Tait, R.J.; Kirkman, J.J.L.; Schaub, M.P. A Participatory Health Promotion Mobile App Addressing Alcohol Use Problems (The Daybreak Program): Protocol for a Randomized Controlled Trial. JMIR Res. Protoc. 2018, 7, e148. [Google Scholar] [CrossRef]
- Tait, R.J.; McKetin, R.; Kay-Lambkin, F.; Carron-Arthur, B.; Bennett, A.; Bennett, K.; Christensen, H.; Griffiths, K.M. A Web-Based Intervention for Users of Amphetamine-Type Stimulants: 3-Month Outcomes of a Randomized Controlled Trial. JMIR Ment. Health 2014, 1, e1. [Google Scholar] [CrossRef]
- Renati, R.; Salvatore Bonfiglio, N.; Patrone, L.; Rollo, D.; Pietronilla Penna, M. The Use of Cognitive Training and TDCS for the Treatment of an High Potential Subject: A Case Study. In Proceedings of the 2021 IEEE International Symposium on Medical Measurements and Applications (MeMeA 2021–Conference Proceedings 2021), Lausanne, Switzerland, 23–25 June 2021. [Google Scholar] [CrossRef]
- Bonfiglio, N.S.; Rollo, D.; Renati, R.; Penna, M.P.; Di Lucia, K. The Use of Cognitive Training, Combined with TDCS, for Craving Reduction and Inhibitory Control Improvement in Cocaine Dependence: A Case Study. In Proceedings of the 2021 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Lausanne, Switzerland, 23–25 June 2021. [Google Scholar] [CrossRef]
- Bonfiglio, N.S.; Parodi, D.; Rollo, D.; Renati, R.; Pessa, E.; Penna, M.P. Use of Training with BCI (Brain Computer Interface) in the Management of Impulsivity. In Proceedings of the IEEE Medical Measurements and Applications (MeMeA 2020—Conference Proceedings 2020), Bari, Italy, 1 June–1 July 2020. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).