Estimating the Burden of Stroke: Two-Year Societal Costs and Generic Health-Related Quality of Life of the Restore4Stroke Cohort
Abstract
:1. Introduction
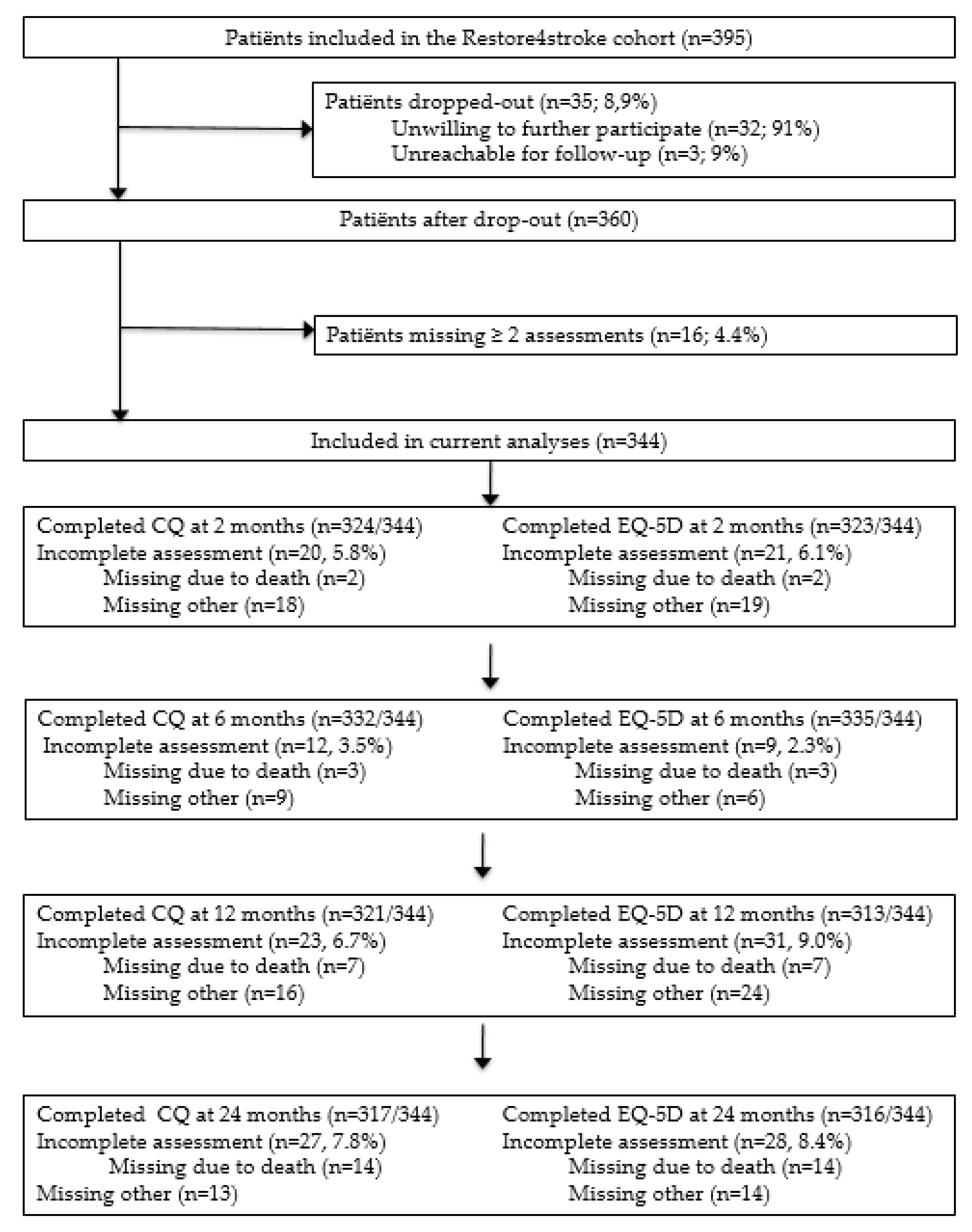
2. Materials and Methods
2.1. Study Design
2.2. Setting and Participants
2.3. Procedures
2.4. Costing
2.5. Quality of Life (QoL) Measurement
2.6. Handling of Missing Data
2.7. Statistics
2.8. Sensitivity and Subgroup Analyses
3. Results
3.1. Patient Characteristics
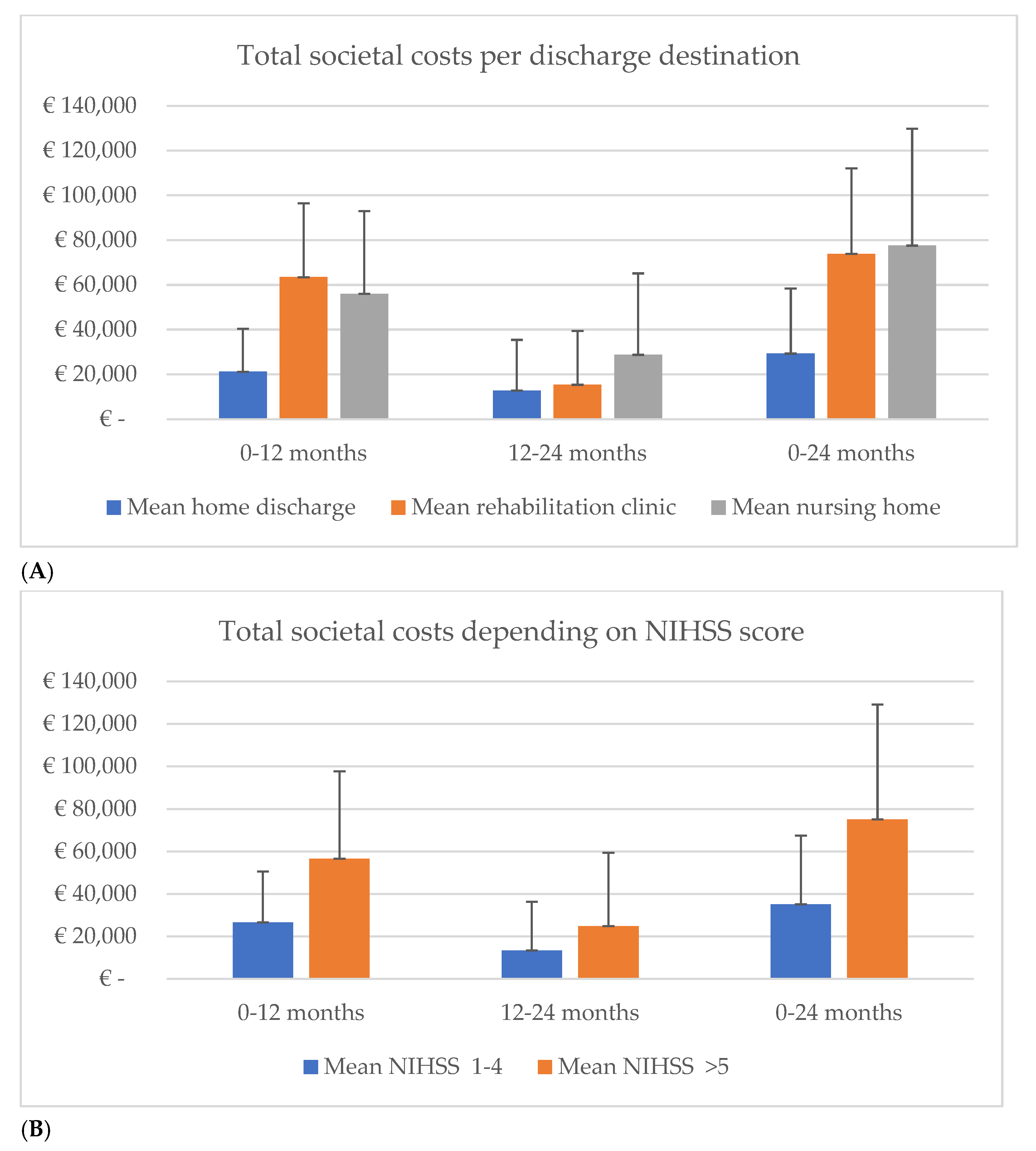
3.2. The Total Societal Costs over Two Years Post-Stroke
3.3. Healthcare and Non-Healthcare Costs in the First and Second-Year Costs after Stroke
3.4. Generic Health-Related Quality of Life 2 Years Post-Stroke
3.5. Sensitivity Analyses & Subgroup Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Feigin, V.L.; Nguyen, G.; Cercy, K.; Johnson, C.O.; Alam, T.; Collaborators GBDLRoS. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N. Engl. J. Med. 2018, 379, 2429–2437. [Google Scholar] [CrossRef] [PubMed]
- Gorelick, P.B. The global burden of stroke: Persistent and disabling. Lancet Neurol. 2019, 18, 417–418. [Google Scholar] [CrossRef]
- Campbell, B.C.V.; Khatri, P. Stroke. Lancet 2020, 396, 129–142. [Google Scholar] [CrossRef]
- Ovbiagele, B.; Goldstein, L.B.; Higashida, R.T.; Howard, V.J.; Johnston, S.C.; Khavjou, O.A.; Lackland, D.T.; Lichtman, J.H.; Mohl, S.; Sacco, R.L.; et al. Forecasting the future of stroke in the United States: A policy statement from the American heart association and American stroke association. Stroke 2013, 44, 2361–2375. [Google Scholar] [CrossRef] [PubMed]
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. American Heart Association council on epidemiology and prevention statistics committee and stroke statistics subcommittee. heart disease and stroke statistics-2021 update: A report from the American Heart Association. Circulation 2021, 23, e254–e743. [Google Scholar] [CrossRef]
- Luengo-Fernandez, R.; Violato, M.; Candio, P.; Leal, J. Economic burden of stroke across Europe: A population-based cost analysis. Eur. Stroke J. 2020, 5, 17–25. [Google Scholar] [CrossRef]
- Eeden, M.V.; Heugten, C.V.; Mastrigt, G.A.P.G.V.; Mierlo, M.V.; Visser-Meily, J.M.; Evers, S.M. The burden of stroke in the Netherlands: Estimating quality of life and costs for 1 year poststroke. BMJ Open 2015, 5, e008220. [Google Scholar] [CrossRef]
- Rajsic, S.; Gothe, H.; Borba, H.H.; Sroczynski, G.; Vujicic, J.; Toell, T.; Siebert, U. Economic burden of stroke: A systematic review on post-stroke care. Eur. J. Health Econ. 2019, 20, 107–134. [Google Scholar] [CrossRef]
- Carod-Artal, F.J.; Egido, J.A. Quality of life after stroke: The importance of a good recovery. Cerebrovasc. Dis. 2009, 27, 204–214. [Google Scholar] [CrossRef]
- Rebchuk, A.D.; O’Neill, Z.R.; Szefer, E.K.; Hill, M.D.; Field, T.S. Health utility weighting of the modified rankin scale: A systematic review and meta-analysis. JAMA Netw. Open 2020, 3, e203767. [Google Scholar] [CrossRef]
- Wassenius, C.; Claesson, L.; Blomstrand, C.; Jood, K.; Carlsson, G. Integrating consequences of stroke into everyday life-Experiences from a long-term perspective. Scand. J. Occup. Ther. 2022, 29, 126–138. [Google Scholar] [CrossRef]
- Campos, L.M.D.; Martins, B.M.; Cabral, N.L.; Franco, S.C.; Pontes-Neto, O.M.; Mazin, S.C.; Reis, F.I.D. How many patients become functionally dependent after a stroke? A 3-year population-based study in Joinville, Brazil. PLoS ONE 2017, 12, e0170204. [Google Scholar] [CrossRef] [PubMed]
- Eeden, M.V.; Heugten, C.M.V.; Evers, S.M. The economic impact of stroke in the Netherlands: The €-Restore4stroke study. BMC Public Health 2012, 12, 122. [Google Scholar] [CrossRef] [PubMed]
- Joo, H.; George, M.G.; Fang, J.; Wang, G. A literature review of indirect costs associated with stroke. J. Stroke Cerebrovasc. Dis. 2014, 23, 1753–1763. [Google Scholar] [CrossRef]
- Luengo-Fernandez, R.; Gray, A.M.; Rothwell, P.M. Costs of stroke using patient-level data: A critical review of the literature. Stroke 2009, 40, e18–e23. [Google Scholar] [CrossRef]
- Lopez-Bastida, J.; Oliva Moreno, J.; Worbes Cerezo, M.; Perestelo Perez, L.; Serrano-Aguilar, P.; Montón-Álvarez, F. Social and economic costs and health-related quality of life in stroke survivors in the Canary Islands, Spain. BMC Health Serv. Res. 2012, 12, 315. [Google Scholar] [CrossRef]
- Mierlo, M.L.V.; Heugten, C.M.V.; Post, M.W.M.; Lindeman, E.; Kort, P.L.M.D.; Visser-Meily, J.M.A. A longitudinal cohort study on quality of life in stroke patients and their partners: Restore4stroke cohort. Int. J. Stroke 2014, 9, 148–154. [Google Scholar] [CrossRef]
- Verberne, D.; Moulaert, V.; Verbunt, J.; Heugten, C.V. Factors predicting quality of life and societal participation after survival of a cardiac arrest: A prognostic longitudinal cohort study. Resuscitation 2018, 123, 51–57. [Google Scholar] [CrossRef]
- Zorginstituut Nederland, Guideline for Cost Research: Methodology and Reference Prices for Economic Evaluations in Healthcare (in Dutch). 2016. Available online: https://www.genesyze.com/resource_guide/zorginstitut-nederland-2016-guideline-economic-evaluations-healthcare-netherlands/ (accessed on 9 September 2019).
- Husereau, D.; Drummond, M.; Augustovski, F.; de Bekker-Grob, E.; Briggs, A.H.; Carswell, C.; Caulley, L.; Chaiyakunapruk, N.; Greenberg, D.; Loder, E.; et al. Consolidated health economic evaluation reporting standards 2022 (CHEERS 2022) statement: Updated reporting guidance for health economic evaluations. Value Health 2022, 1, 3–9. [Google Scholar] [CrossRef]
- Elm, E.V.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the reporting of observational studies in epidemiolog (STROBE) statement: Guidelines for reporting observational studies. Lancet 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [Green Version]
- Collin, C.; Wade, D.T.; Davies, S.; Horne, V. The Barthel ADL index: A reliability study. Int. Disabil. Stud. 1988, 10, 61–63. [Google Scholar] [CrossRef] [PubMed]
- Meijer, R.; Limbeek, J.V.; Haan, R.D. Development of the stroke-unit discharge guideline: Choice of assessment instruments for prediction in the subacute phase post-stroke. Int. J. Rehabil. Res. 2006, 29, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Federatie Medisch Specialisten. Herseninfarct en Hersenbloeding. Available online: https://richtlijnendatabase.nl/richtlijn/herseninfarct_en_hersenbloeding/startpagina_herseninfarct_-bloeding.html (accessed on 13 December 2019).
- Brooks, R. Euroqol: The current state of play. Health Policy 1996, 37, 53–72. [Google Scholar] [CrossRef]
- Tan, S.S.; Bouwmans-Frijters, C.; Roijen, L.H.V. Cost research guide: Methods and reference prices for economic evaluations in health care (in Dutch). Tijds. Gezondheids. Wet. 2012, 90, 367–372. [Google Scholar] [CrossRef]
- Medicijnkosten.nl. Available online: https://medicijnkosten.nl/ (accessed on 10 September 2019).
- Koopmanschap, M.A.; Rutten, F.F.; Ineveld, B.M.V.; Roijen, L.V. The friction cost method for measuring indirect costs of disease. J. Health Econ. 1995, 14, 171–189. [Google Scholar] [CrossRef]
- Hunger, M.; Sabariego, C.; Stollenwerk, B.; Cieza, A.; Leidl, R. Validity, reliability and responsiveness of the eq-5D in German stroke patients undergoing rehabilitation. Qual. Life Res. 2012, 21, 1205–1216. [Google Scholar] [CrossRef]
- Lamers, L.M.; Stalmeier, P.F.; McDonnell, J.; Krabbe, P.F.; Busschbach, J.J.V. Measuring the quality of life in economic evaluations: The Dutch eq-5D tariff. Ned. Tijdschr. Voor Geneeskd. 2005, 149, 1574–1578. [Google Scholar]
- Norman, G.R.; Sloan, J.A.; Wyrwich, K.W. Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Med. Care 2003, 41, 582–592. [Google Scholar] [CrossRef] [PubMed]
- Jakobsen, J.C.; Gluud, C.; Wetterslev, J. When and how should multiple imputation be used for handling missing data in randomised clinical trials–a practical guide with flowcharts. BMC Med. Res. Methodol 2017, 17, 162. [Google Scholar] [CrossRef]
- Oostenbrink, J.B.; Al, M.J. The analysis of incomplete cost data due to dropout. Health Econ. 2005, 14, 763–776. [Google Scholar] [CrossRef]
- Dolan, P. Modeling valuations for Europol health states. Med. Care 1997, 35, 1095–1108. [Google Scholar] [CrossRef] [PubMed]
- Vogl, M. Improving patient-level costing in the English and German ‘DRG’ system. Health Policy 2013, 109, 290–300. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.S.; Rutten, F.F.; Ineveld, B.M.V.; Redekop, W.K.; Roijen, L.H.V. Comparing methodologies for the cost estimation of hospital services. Eur. J. Health Econ. 2009, 10, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Ghatnekar, O.; Persson, U.; Asplund, K.; Glader, E.L. Costs for stroke in Sweden 2009 and developments since 1997. Int. J. Technol. Assess. Health Care 2014, 30, 203–209. [Google Scholar] [CrossRef]
- Gloede, T.D.; Halbach, S.M.; Thrift, A.G.; Dewey, H.M.; Pfaff, H.; Cadilhac, D.A. Long-term costs of stroke using 10-year longitudinal data from the northeast Melbourne stroke incidence study. Stroke 2014, 45, 3389–3394. [Google Scholar] [CrossRef]
- Kolominsky-Rabas, P.L.; Heuschmann, P.U.; Marschall, D.; Emmert, M.; Baltzer, N.; Neundorfer, B.; Schoffski, O.; Krobot, K.J. Lifetime cost of ischemic stroke in Germany: Results and national projections from a population-based stroke registry: The Erlangen stroke project. Stroke 2006, 37, 1179–1183. [Google Scholar] [CrossRef]
- Dewey, H.M.; Thrift, A.G.; Mihalopoulos, C.; Carter, R.; Macdonell, R.A.; McNeil, J.J.; Donnan, G.A. Cost of stroke in Australia from a societal perspective: Results from the northeast Melbourne stroke incidence study (nemesis). Stroke 2001, 32, 2409–2416. [Google Scholar] [CrossRef]
- Payne, K.A.; Huybrechts, K.F.; Caro, J.J.; Craig Green, T.J.; Klittich, W.S. Long term cost-of-illness in stroke: An international review. Pharmacoeconomics 2002, 20, 813–825. [Google Scholar] [CrossRef]
- Verbakel, E. How to understand informal caregiving patterns in Europe? The role of formal long-term care provisions and family care norms. Scand. J. Public Health 2018, 46, 436–447. [Google Scholar] [CrossRef]
- Van Exel, J.; Koopmanschap, M.A.; Van Wijngaarden, J.D.; Reimer, W.J.S.O. Costs of stroke and stroke services: Determinants of patient costs and a comparison of costs of regular care and care organised in stroke services. Cost Eff. Resour. Alloc. 2003, 1, 2. [Google Scholar] [CrossRef]
- Godwin, K.M.; Wasserman, J.; Ostwald, S. Cost associated with stroke: Outpatient rehabilitative services and medication. Stroke Rehabil. 2011, 18, 676–684. [Google Scholar] [CrossRef] [PubMed]
- Evers, S.M.; Struijs, J.N.; Ament, A.J.; Genugten, M.L.V.; Jager, J.H.; Bos, G.A.V.D. International comparison of stroke cost studies. Stroke 2004, 35, 1209–1215. [Google Scholar] [CrossRef] [PubMed]
- Tengs, T.O.; Lin, T.H. A meta-analysis of quality-of-life estimates for stroke. Pharmacoeconomics 2003, 21, 191–200. [Google Scholar] [CrossRef]
- Haacke, C.; Althaus, A.; Spottke, A.; Siebert, U.; Back, T.; Dodel, R. Long-term outcome after stroke: Evaluating health-related quality of life using utility measurements. Stroke 2006, 37, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Verberne, D.P.J.; Mastrigt, G.A.P.G.V.; Ponds, R.W.H.M.; Heugten, C.M.V.; Kroese, M.E.A.L. An economic evaluation of nurse-led stroke aftercare addressing long-term psychosocial outcome: A comparison to care-as-usual. BMJ Open 2021, 11, e039201. [Google Scholar] [CrossRef] [PubMed]
- Szende, A.; Janssen, B.; Cabases, J. Self-Reported Population Health: An International Perspective Based on EQ-5D; Springer publishing: Berlin, Germany, 2014. [Google Scholar]
- Joundi, R.A.; Adekanye, J.; Leung, A.A.; Ronksley, P.; Smith, E.E.; Rebchuk, A.D.; Field, T.S.; Hill, M.D.; Wilton, S.B.; Bresee, L.C. Health State Utility Values in People With Stroke: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2022, 11, 13. [Google Scholar] [CrossRef]
- Tarricone, R. Cost-of-illness analysis. What room in health economics? Health Policy 2006, 77, 51–63. [Google Scholar] [CrossRef]
- Lundstrom, E.; Smits, A.; Borg, J.; Terent, A. Four-fold increase in direct costs of stroke survivors with spasticity compared with stroke survivors without spasticity: The first year after the event. Stroke 2010, 41, 319–324. [Google Scholar] [CrossRef]
- Coughlin, S.S. Recall bias in epidemiologic studies. J. Clin. Epidemiol. 1990, 43, 87–91. [Google Scholar] [CrossRef]
- Larg, A.; Moss, J.R. Cost-of-illness studies: A guide to critical evaluation. Pharmacoeconomics 2011, 29, 653–671. [Google Scholar] [CrossRef]
- Oliva-Moreno, J.; Peña-Longobardo, L.M.; Mar, J.; Masjuan, J.; Soulard, S.; Gonzalez-Rojas, N.; Becerra, V.; Casado, M.Á.; Torres, C.; Yebenes, M.; et al. Determinants of informal care, burden, and risk of burnout in caregivers of stroke survivors: The CONOCES study. Stroke 2018, 49, 140–146. [Google Scholar] [CrossRef] [PubMed]
| N | Mean (SD) or % | |
|---|---|---|
| Age (in years) | 344 | 66.7 (12.2%) |
| Gender | 344 | |
| Female | 121 | 35.2% |
| Male | 223 | 64.8% |
| Marital status | 344 | |
| Living together | 240 | 69.8% |
| No relationship | 104 | 30.2% |
| Education | 341 | |
| Low | 250 | 73.3% |
| High | 91 | 26.7% |
| Stroke type | 343 | |
| Ischaemic stroke | 319 | 92.7% |
| Hemorrhagic stroke/Infarction stroke | 24 | 7.0% |
| Severity of stroke (NIHSS) | 344 | |
| No stroke symptoms (NIHSS 0) | 84 | 24.4% |
| Minor stroke symptoms (NIHSS 1–4) | 197 | 57.3% |
| Moderate stroke symptoms (NIHSS 5–12) | 58 | 16.8% |
| Moderate to severe stroke symptoms (NIHSS ≥ 13) | 5 | 1.5% |
| Residence after discharge | 344 | |
| Home | 247 | 71.7% |
| Rehabilitation center | 48 | 14.0% |
| Geriatric rehabilitation | 49 | 14.2% |
| Users | Resource Use Per Patient | Costs Per Patient | ||||||
|---|---|---|---|---|---|---|---|---|
| Unit | N | % | Mean | SD | Mean | SD | Median | |
| Healthcare costs | ||||||||
| General practitioner | Contact | 332 | 96.5 | 13.7 | 16.79 | €481 | €34 | €478 |
| Specialist | Contact | 335 | 97.4 | 11.2 | 9.45 | €1335 | €65 | €1333 |
| Allied health professionals | Contact | 269 | 78.2 | 32.2 | 46.33 | €1105 | €93 | €1104 |
| Mental healthcare professionals | Contact | 125 | 36.3 | 1.9 | 5.93 | €197 | €35 | €195 |
| Rehabilitation treatments | Day | 261 | 75.9 | 29.9 | 41.31 | €8664 | €673 | €8645 |
| Hospital | Night | 307 | 89.2 | 10.2 | 11.39 | €6864 | €448 | €6851 |
| Rehabilitation clinic | Night | 130 | 37.8 | 13.0 | 29.66 | €6301 | €822 | €6279 |
| Nursing home | Night | 94 | 27.3 | 5.9 | 36.40 | €1038 | €351 | €1012 |
| Psychiatric clinic | Night | 61 | 17.7 | 0.4 | 3.67 | €133 | €69 | €127 |
| Medication | Various | - | - | - | - | €1119 | €53 | €1118 |
| Total healthcare costs | €27,159 | €1611 | €27,174 | |||||
| Non-healthcare costs | ||||||||
| Paid home care | Hours | 153 | 44.5 | 185.7 | 569.81 | €3979 | €695 | €3925 |
| Informal care | Hours | 238 | 69.2 | 291.5 | 598.66 | €4320 | €512 | €4298 |
| Inability to perform unpaid labor | Day | 216 | 62.8 | 69.0 | 130.96 | €8284 | €895 | €8241 |
| Productivity Losses * | Day | 41 | 11.9 | 22.0 | 76.01 | €3810 | €406 | €3791 |
| Total non-healthcare costs | €20,330 | €1603 | €20,302 | |||||
| Total societal costs | €47,502 | €2628 | €47,384 | |||||
| Unit | 0–12 Months Post-Stroke | 12–24 Months Post-Stroke | Difference | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Per Patient | Resource Use | Cost | Resource Use | Cost | ||||||||
| Mean | SD | Mean | SD | Median | Mean | SD | Mean | SD | Median | Mean (95% CI) * | ||
| Healthcare Costs | ||||||||||||
| GP | Contact | 6.9 | 5.00 | €237 | €9.68 | €236 | 6.9 | 15.60 | €247 | €32 | €243 | €10 (−€44, €87) |
| Specialist | Contact | 8.1 | 6.73 | €946 | €44.67 | €947 | 3.2 | 5.11 | €391 | €37 | €389 | −€556 (−€667, −€437) |
| Allied HP | Contact | 21.2 | 28.03 | €718 | €55.13 | €717 | 11.0 | 27.38 | €386 | €56 | €385 | −€332 (−€487, −€181) |
| Mental HP | Contact | 1.3 | 4.12 | €136 | €23.92 | €135 | 0.6 | 3.15 | €61 | €19 | €59 | −€75 (−€138, −€15) |
| Rehabilitation treatments | Day | 22.9 | 29.86 | €6582 | €480.22 | €6595 | 7.0 | 23.49 | €2064 | €387 | €2050 | −€4518 (−€5,768, −€3226) |
| Hospital | Night | 8.4 | 8.68 | €5601 | €336.73 | €5587 | 1.8 | 6.74 | €1241 | €272 | €1233 | −€4360 (−€5233, −€3494) |
| Rehabilitation clinic | Night | 10.9 | 25.68 | €5205 | €713.72 | €5164 | 2.1 | 15.31 | €1089 | €455 | €1033 | −€4116 (−€5761, −€2478) |
| Nursing home | Night | 4.0 | 18.91 | €711 | €195.33 | €692 | 1.9 | 20.16 | €346 | €208 | €334 | −€365 (−€879, €210) |
| Psychiatric clinic | Night | 0.1 | 0.70 | €28 | €12.41 | €26 | 0.3 | 3.54 | €102 | €65 | €98 | €74 (−€14, €236) |
| Medication | Various | - | - | €531 | €23.77 | €531 | - | - | €536 | €38 | €533 | €5 (−€80, €96) |
| Total healthcare costs | €20,709 | €1282 | €20,639 | - | - | €6431 | €846 | €6406 | −€14,277 (−€17,319 −€11,236) | |||
| Paid home care | Hours | 97.4 | 349.47 | €2056 | €430 | €2023 | 88.3 | 385.73 | €1878 | €459 | €1836 | −€178 (−€1431, €1042) |
| Informal care | Hours | 159.7 | 359.73 | €2323 | €290 | €2304 | 131.8 | 423.28 | €1996 | €378 | €1970 | −€326 (−€1228, €660) |
| Inability to perform unpaid labor | Day | 27.4 | 50.98 | €3186 | €347 | €3180 | 41.7 | 106.17 | €5068 | €744 | €5081 | €1882 (€327, €3478) |
| Productivity Losses * | Day | 22.0 | 76.01 | €3819 | €389 | €3807 | - | - | 0 | 0 | 0 | −€3819 (−€4558, −€3065) |
| Total non-healthcare costs | €11,336 | €817 | €11,324 | €8910 | €1078 | €8874 | −€2426 (−€5079, €246) | |||||
| Total societal costs | €32,085 | €1743 | €31,984 | €15,383 | €1526 | €15,372 | −€16,703 (−€21,243, −€12,039) | |||||
| N | 12 Months Post-Stroke | 24 Months Post-Stroke | ||
|---|---|---|---|---|
| Dimensions EuroQoL | mean (SD) | mean (SD) | Mean difference * (95%CI) | |
| Mobility | 344 | 1.54 (0.59) | 1.60 (0.58) | 0.06 (−0.03, 0.15) |
| Self-care | 344 | 1.23 (0.52) | 1.30 (0.59) | 0.07 (−0.02, 0.16) |
| Usual activities | 344 | 1.67 (0.70) | 1.63 (0.69) | −0.04 (−0.15, 0.07) |
| Pain/discomfort | 344 | 1.56 (0.59) | 1.64 (0.64) | 0.08 (−0.02, 0.17) |
| Anxiety/depression | 344 | 1.38 (0.57) | 1.45 (0.62) | 0.06 (−0.03, 0.16) |
| Average utility score | 344 | 0.7400 (0.2662) | 0.7094 (0.3153) | −0.03 (−0.08, 0.01) |
| Utility score EuroQoL: Age | ||||
| <65 | 146 | 0.7611 (0.2546) | 0.7688 (0.2667) | 0.01 (−0.05, 0.07) |
| 65–75 | 99 | 0.7023 (0.3060) | 0.7277 (0.2894) | 0.03 (−0.06, 0.10) |
| >75 | 99 | 0.7467 (0.2378) | 0.6036 (0.37714) | −0.14 (−0.23, −0.05) |
| Utility score EuroQoL: Gender | ||||
| Male | 223 | 0.7497 (0.2619) | 0.7290 (0.3182) | −0.02 (−0.07, 0.03) |
| Female | 121 | 0.7222 (0.2744) | 0.6734 (0.3080) | −0.05 (−0.12,0.02) |
| Utility score EuroQoL: Severity of stroke | ||||
| No stroke symptoms (NIHSS 0) | 84 | 0.7305 (0.2782) | 0.7076 (0.3414) | 0.02 (−0.07, 0.11) |
| Minor stroke symptoms (NIHSS 1–4) | 197 | 0.7352 (0.2519) | 0.7280 (0.2892) | −0.01 (−0.06, 0.04) |
| Moderate stroke symptoms (NIHSS 5–12) | 58 | 0.7713 (0.2918) | 0.6501 (0.3550) | −0.12 (−0.23, 0.01) |
| Moderate to severe stroke symptoms (NIHSS ≥ 13) | 5 | 0.7302 (0.3668) | 0.6973 (0.37659) | −0.03 (−0.42, 0.38) |
| Sensitivity Analyses Costs | Base Case * | Sensitivity Analyses | |||||
|---|---|---|---|---|---|---|---|
| Costs | Mean Total Costs (€) | SD | Mean Total Costs (€) | SD | Mean Difference | 95% CI | |
| Method extrapolation costs | (18–24M)*2)/ (6–12M) + (18–24M) | €42,378 | €2225 | €46,282 | €2597 | €3904 | (€−2751, €11,146) |
| Perspective | (Societal/Healthcare) | €42,506 | €2389 | €27,125 | €1620 | €−15,382 | (€−21,244, €−9785) |
| Sensitivity analyses Quality of life | Utility | SD | Utility | SD | Mean difference | 95% CI | |
| Average utility 12M | Dutch/UK | 0.7110 | 0.0185 | 0.6604 | 0.0215 | −0.0506 | (−0.1104, 0.0081) |
| Average utility 24M | Dutch/UK | 0.7413 | 0.0156 | 0.6769 | 0.0192 | −0.0644 | (−0.1122, −0.0167) |
| Subgroup analysis of quality of life | 12 months post-stroke | 24 months post-stroke | |||||
| Characteristics | Group | Mean difference (utility) | 95% CI | Mean difference (utility) | 95% CI | ||
| Gender | Male/Female | −0.0277 | (−0.0883, 0.0301) | −0.0559 | (−0.1262, 0.0111) | ||
| Age | 65+/65− | −0.0361 | (−0.0932, 0.0193) | 0.1030 | (0.0395, 0.1664) | ||
| Stroke type | Infarction/Haemorrhage | −0.1245 | (−0.2638, 0.0058) | 0.0557 | (−0.0459, 0.1388) | ||
| Recurrent stroke | Yes/No | −0.0048 | (−0.0941, 0.0913) | 0.0502 | (−0.0610, 0.1699) | ||
| Education | High/Low | 0.0198 | (−0.0473, 0.0910) | 0.0118 | (−0.0722, 0.0901) | ||
| Home Discharge | Yes/No | −0.0292 | (−0.0960, 0.0351) | −0.1030 | (−0.1796, 0.0298) | ||
| Stroke severity | 0–4/>5 | 0.0343 | (−0.0426, 0.1100) | −0.0695 | (−0.1666, 0.0147) | ||
| Subgroup analysis costs | 0-12 months post-stroke | 12-24 months post-stroke | 0-24 months post-stroke | ||||
| Characteristic | Group | Mean difference (€) | 95% CI | Mean difference (€) | 95% CI | Mean difference (€) | 95% CI |
| Gender | Male/Female | −€1280 | (−€7583, €5729) | €3897 | (−€1620, €9587) | €2352 | (−€5555, €10,872) |
| Age | 65+/65− | −€3148 | (−€9339, €2894) | €4435 | (−€945, €9583) | €2224 | (−€6147, €10,050) |
| Stroke type | Infarction/Haemorrhage | €3323 | (−€10,441, €18,298) | €2806 | (−€9427, €18,949) | €7114 | (−€13,288, €31,104) |
| Recurrent stroke | Yes/No | €4631 | (−€3222, €11,567) | €5596 | (−€2933, €14,694) | −€814 | (−€11,490, €11,589) |
| Education | High/Low | €2870 | (−€4068, €9835) | €3276 | (−€2029, €8888) | €5311 | (−€4122, €14,389) |
| Home Discharge | Yes/No | €38,535 | (€31,117, €45,654) | €9347 | (€2602, €16,283) | €46,503 | (€36,877, €56,409) |
| Stroke severity | 0–4/>5 | €29,971 | (€19,768, €40,477) | €11,545 | (€2993, €20,705) | €40,144 | (€26,561, €54,317) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Mastrigt, G.; van Heugten, C.; Visser-Meily, A.; Bremmers, L.; Evers, S. Estimating the Burden of Stroke: Two-Year Societal Costs and Generic Health-Related Quality of Life of the Restore4Stroke Cohort. Int. J. Environ. Res. Public Health 2022, 19, 11110. https://doi.org/10.3390/ijerph191711110
van Mastrigt G, van Heugten C, Visser-Meily A, Bremmers L, Evers S. Estimating the Burden of Stroke: Two-Year Societal Costs and Generic Health-Related Quality of Life of the Restore4Stroke Cohort. International Journal of Environmental Research and Public Health. 2022; 19(17):11110. https://doi.org/10.3390/ijerph191711110
Chicago/Turabian Stylevan Mastrigt, Ghislaine, Caroline van Heugten, Anne Visser-Meily, Leonarda Bremmers, and Silvia Evers. 2022. "Estimating the Burden of Stroke: Two-Year Societal Costs and Generic Health-Related Quality of Life of the Restore4Stroke Cohort" International Journal of Environmental Research and Public Health 19, no. 17: 11110. https://doi.org/10.3390/ijerph191711110
APA Stylevan Mastrigt, G., van Heugten, C., Visser-Meily, A., Bremmers, L., & Evers, S. (2022). Estimating the Burden of Stroke: Two-Year Societal Costs and Generic Health-Related Quality of Life of the Restore4Stroke Cohort. International Journal of Environmental Research and Public Health, 19(17), 11110. https://doi.org/10.3390/ijerph191711110






