Cluster Analysis to Distinguish Patients Most Likely to Benefit from Outpatient Cardiac Rehabilitation—A Prospective, Multicenter Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting and Rehabilitation Plan
2.2. Participants
2.3. Assessments
2.4. Statistical Analysis
3. Results
3.1. Cluster Analysis and Baseline Characteristics
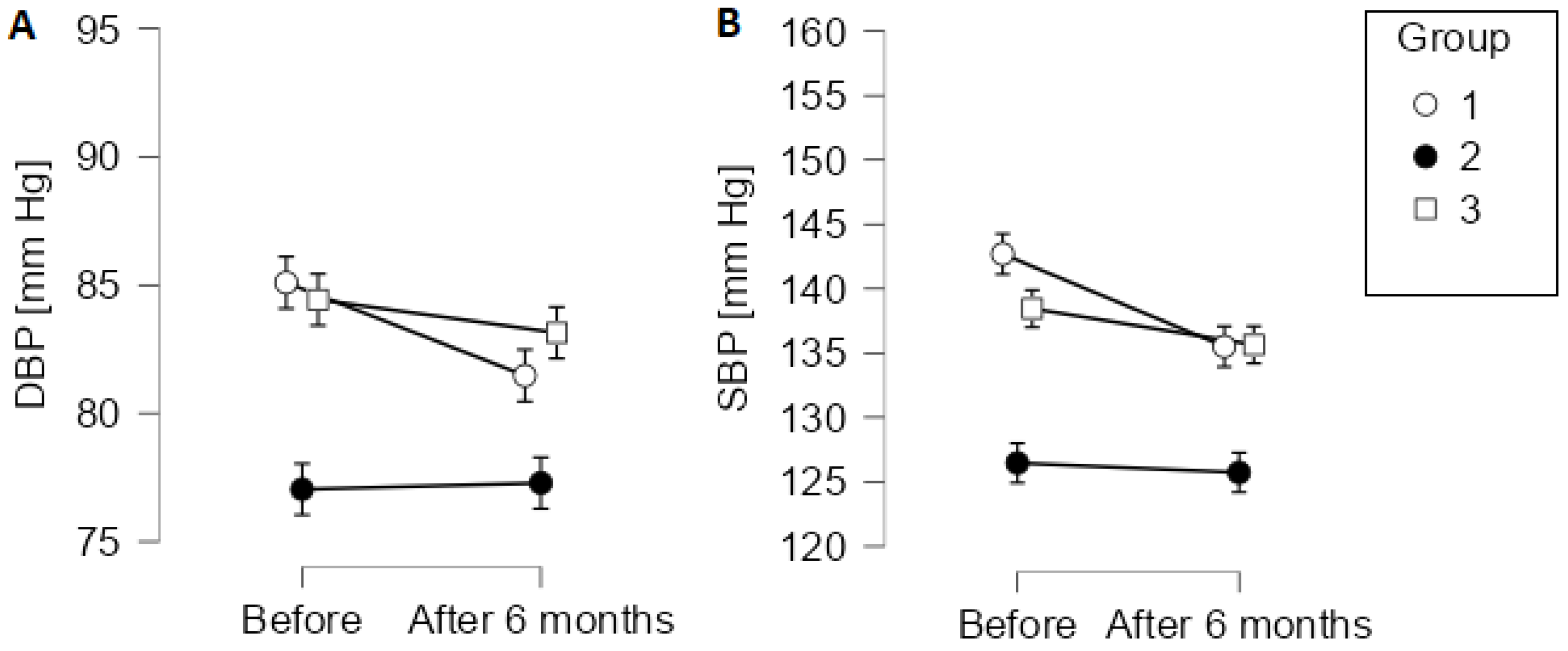
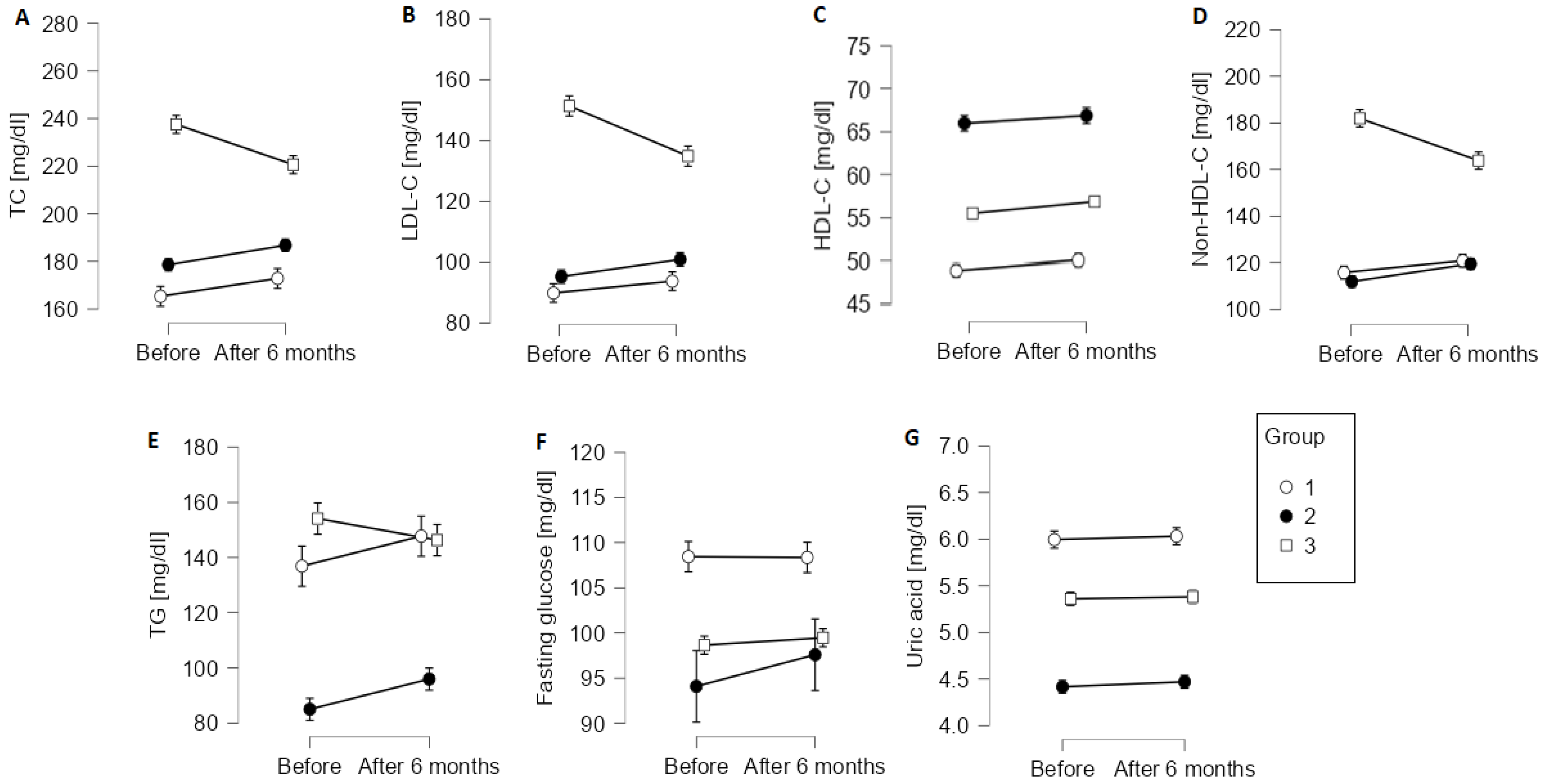
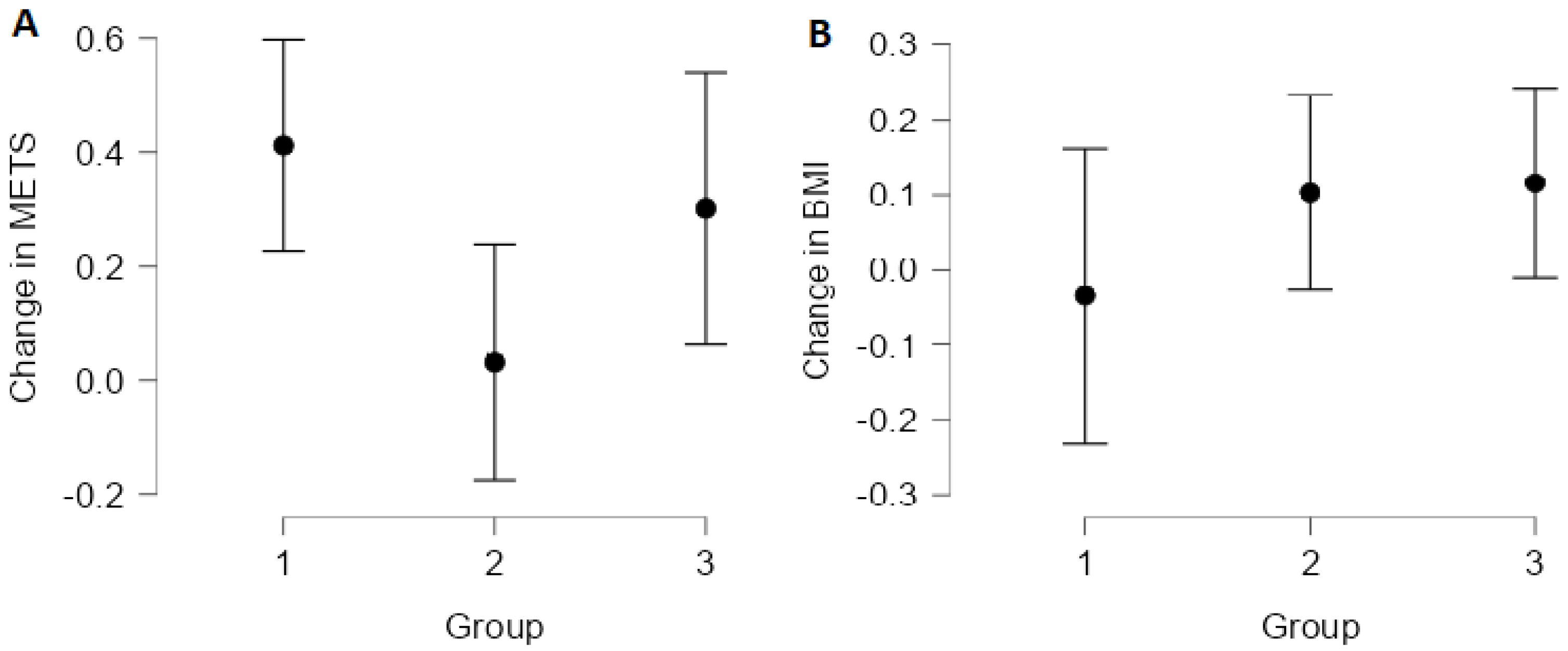
3.2. Change in Outcomes from Baseline to 6 Months after the End of Cardiac Rehabilitation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. List of Centres Providing Cardiac Rehabilitation
- Center for Cardiac Rehabilitation Optima Care. Żeromskiego 49; 81-198 Kosakowo
- Clinica Medica. Mireckiego 11; 81-229 Gdynia
- Almed Clinica, Dworcowa 14; 82-200 Malbork
- Hospital in Sztum. Reja 12; 82-400 Sztum
- Hospitals in Tczew. 30 Stycznia 57/58; 83-110 Tczew
- COPERNICUS Podmiot Leczniczy Sp. z o.o., St. Adalbert’ Hospital. Jana Pawła II 50; 80-462 Gdańsk
- Korczak Voivodship Hospital. Hubalczyków 1; 76-200 Słupsk
- Medpharma Clinic. Jana Pawła II 5; 83-200 Starogard Gdański
- Rehabilitation Clinic Wieżyca. Wieżyca 29; 83-315 Szymbark
- Center for Cardiac Rehabilitation Optima Care. Wolności 40a; 84-300 Lębork
References
- Dalal, H.M.; Doherty, P.; Taylor, R.S. Cardiac rehabilitation. BMJ 2015, 351, h5000. [Google Scholar] [CrossRef]
- Dibben, G.; Faulkner, J.; Oldridge, N.; Rees, K.; Thompson, D.R.; Zwisler, A.-D.; Taylor, R.S. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. 2021, 2021. [Google Scholar] [CrossRef]
- Global Initiative for Asthma Global Strategy for Asthma Management and Prevention (2018 Update). Available online: https://ginasthma.org/wp-content/uploads/2018/04/wms-GINA-2018-report-tracked_v1.3.pdf (accessed on 16 November 2018).
- Ribeiro, G.S.; Melo, R.D.; Deresz, L.F.; Dal Lago, P.; Pontes, M.R.; Karsten, M. Cardiac rehabilitation programme after transcatheter aortic valve implantation versus surgical aortic valve replacement: Systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2017, 24, 688–697. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.S.; Dalal, H.M.; McDonagh, S.T.J. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat. Rev. Cardiol. 2021, 19, 180–194. [Google Scholar] [CrossRef] [PubMed]
- Turk-Adawi, K.; Supervia, M.; Lopez-Jimenez, F.; Pesah, E.; Ding, R.; Britto, R.R.; Bjarnason-Wehrens, B.; Derman, W.; Abreu, A.; Babu, A.S.; et al. Cardiac Rehabilitation Availability and Density around the Globe. eClinicalMedicine 2019, 13, 31–45. [Google Scholar] [CrossRef]
- Ades, P.A.; Keteyian, S.J.; Wright, J.S.; Hamm, L.F.; Lui, K.; Newlin, K.; Shepard, D.S.; Thomas, R.J. Increasing Cardiac Rehabilitation Participation From 20% to 70%: A Road Map from the Million Hearts Cardiac Rehabilitation Collaborative. Mayo Clin. Proc. 2017, 92, 234–242. [Google Scholar] [CrossRef]
- Mamataz, T.; Uddin, J.; Ibn Alam, S.; Taylor, R.S.; Pakosh, M.; Grace, S.L. Effects of cardiac rehabilitation in low-and middle-income countries: A systematic review and meta-analysis of randomised controlled trials. Prog. Cardiovasc. Dis. 2021, 70, 119–174. [Google Scholar] [CrossRef]
- Lee, B.S.; Sen, P.K.; Park, N.S.; Boothroyd, R.A.; Peters, R.H.; Chiriboga, D.A. A clustering method to identify who benefits most from the treatment group in clinical trials. Health Psychol. Behav. Med. 2014, 2, 723–734. [Google Scholar] [CrossRef]
- Bian, Y.; Le, Y.; Du, H.; Chen, J.; Zhang, P.; He, Z.; Wang, Y.; Yu, S.; Fang, Y.; Yu, G.; et al. Efficacy and Safety of Anticoagulation Treatment in COVID-19 Patient Subgroups Identified by Clinical-Based Stratification and Unsupervised Machine Learning: A Matched Cohort Study. Front. Med. 2021, 8, 786414. [Google Scholar] [CrossRef] [PubMed]
- Jegier, A.; Szalewska, D.; Mawlichanów, A.; Bednarczyk, T.; Eysymontt, Z.; Gałaszek, M.; Mamcarz, A.; Mierzyńska, A.; Piotrowicz, E.; Piotrowicz, R.; et al. Kompleksowa rehabilitacja kardiologiczna podstawą prewencji wtórnej chorób układu sercowo-naczyniowego. Opinia ekspertów Sekcji Rehabilitacji Kardiologicznej i Fizjologii Wysiłku Polskiego Towarzystwa Kardiologicznego. Kardiol. Pol. Pol. Heart J. 2021, 79, 28–45. [Google Scholar]
- WHO. Rehabilitation after Cardiovascular Diseases, with Special Emphasis on Developing Countries: Report of a WHO Expert Committee; WHO: Geneva, Switzerland, 1991.
- Kargarfard, M.; Rouzbehani, R.; Basati, F. Effects of exercise rehabilitation on blood pressure of patients after myocardial infarction. Int. J. Prev. Med. 2010, 1, 124–130. [Google Scholar]
- Mazumdar, S.; Kumar, A.; Verma, S.K. Effect of Cardiac Rehabilitation on Blood Pressure in Stable Angina Patients. J. Exerc. Sci. Physiother. 2014, 10, 54. [Google Scholar] [CrossRef] [Green Version]
- Parvand, M.; Goosheh, B.; Sarmadi, A.R. Effect of cardiac rehabilitation on heart rate and functional capacity in patients after myocardial infarction. Iran. Rehabil. J. 2016, 14, 157–162. [Google Scholar] [CrossRef]
- Mohammed, H.G.; Shabana, A.M. Effect of cardiac rehabilitation on cardiovascular risk factors in chronic heart failure patients. Egypt. Hear. J. 2018, 70, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Valentino, G.; Galgani, J.E.; Álamos, M.; Orellana, L.; Adasme, M.; Berríos, A.; Acevedo, M. Anthropometric and blood pressure changes in patients with or without nutritional counselling during cardiac rehabilitation: A retrospective study. J. Hum. Nutr. Diet. 2021, 34, 402–412. [Google Scholar] [CrossRef] [PubMed]
- Sahin, A.A.; Ozben, B.; Sunbul, M.; Yagci, I.; Sayar, N.; Cincin, A.; Gurel, E.; Tigen, K.; Basaran, Y. The effect of cardiac rehabilitation on blood pressure, and on left atrial and ventricular functions in hypertensive patients. J. Clin. Ultrasound 2021, 49, 456–465. [Google Scholar] [CrossRef]
- Reich, B.; Benzer, W.; Harpf, H.; Hofmann, P.; Mayr, K.; Ocenasek, H.; Podolsky, A.; Pokan, R.; Porodko, M.; Puelacher, C.; et al. Efficacy of extended, comprehensive outpatient cardiac rehabilitation on cardiovascular risk factors: A nationwide registry. Eur. J. Prev. Cardiol. 2020, 27, 1026–1033. [Google Scholar] [CrossRef]
- Adeba Garcia, A.; Vigil-Escalera Diaz, M.; Alvarez Velasco, R.; Martin Fernandez, M.; Barriales Alvarez, V.; Soroa Ortuno, M.; Barja Gonzalez, N.; Santamaria Rubio, J.; Junco Vicente, A.; Martinez Leon, A.; et al. The importance of cardiac rehabilitation programmes in the control of LDL cholesterol after an acute coronary syndrome. Eur. J. Prev. Cardiol. 2021, 28, zwab061-282. [Google Scholar] [CrossRef]
- Lavie, C.J.; Milani, R.V. Effects of cardiac rehabilitation and exercise training on low-density lipoprotein cholesterol in patients with hypertriglyceridemia and coronary artery disease. Am. J. Cardiol. 1994, 74, 1192–1195. [Google Scholar] [CrossRef]
- Fard, N.M.; Zadegan, N.S.; Sajadi, F.; Rafiei, M.; Abdar, N. Effect of cardiac rehabilitation on lipid profile. J. Assoc. Physicians India 2003, 51, 12–15. [Google Scholar]
- Schwaab, B.; Zeymer, U.; Jannowitz, C.; Pittrow, D.; Gitt, A. Improvement of low-density lipoprotein cholesterol target achievement rates through cardiac rehabilitation for patients after ST elevation myocardial infarction or non-ST elevation myocardial infarction in Germany: Results of the PATIENT CARE registry. Eur. J. Prev. Cardiol. 2019, 26, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Wittlinger, T.; Schwaab, B.; Völler, H.; Bongarth, C.; Heinze, V.; Eckrich, K.; Guha, M.; Richter, M.; Schlitt, A. Efficacy of Lipid-Lowering Therapy during Cardiac Rehabilitation in Patients with Diabetes Mellitus and Coronary Heart Disease. J. Cardiovasc. Dev. Dis. 2021, 8, 105. [Google Scholar] [CrossRef] [PubMed]
- Dun, Y.; Thomas, R.J.; Medina-Inojosa, J.R.; Squires, R.W.; Huang, H.; Smith, J.R.; Liu, S.; Olson, T.P. High-Intensity Interval Training in Cardiac Rehabilitation: Impact on Fat Mass in Patients with Myocardial Infarction. Mayo Clin. Proc. 2019, 94, 1718–1730. [Google Scholar] [CrossRef]
- Świątkiewicz, I.; Di Somma, S.; De Fazio, L.; Mazzilli, V.; Taub, P.R. Effectiveness of Intensive Cardiac Rehabilitation in High-Risk Patients with Cardiovascular Disease in Real-World Practice. Nutrients 2021, 13, 3883. [Google Scholar] [CrossRef]
- Verges, B.L.; Patois-Verges, B.; Cohen, M.; Casillas, J.M. Comprehensive Cardiac Rehabilitation Improves the Control of Dyslipidemia in Secondary Prevention. J. Cardiopulm. Rehabil. 1998, 18, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Buckley, J.P.; Riddell, M.; Mellor, D.; Bracken, R.M.; Ross, M.-K.; LaGerche, A.; Poirier, P. Acute glycaemic management before, during and after exercise for cardiac rehabilitation participants with diabetes mellitus: A joint statement of the British and Canadian Associations of Cardiovascular Prevention and Rehabilitation, the International Coun. Br. J. Sports Med. 2021, 55, 709–720. [Google Scholar] [CrossRef]
- Ndrepepa, G. Uric acid and cardiovascular disease. Clin. Chim. Acta 2018, 484, 150–163. [Google Scholar] [CrossRef]
- Turk-Adawi, K.; Sarrafzadegan, N.; Grace, S.L. Global availability of cardiac rehabilitation. Nat. Rev. Cardiol. 2014, 11, 586–596. [Google Scholar] [CrossRef]
- Bjarnason-Wehrens, B.; McGee, H.; Zwisler, A.-D.; Piepoli, M.F.; Benzer, W.; Schmid, J.-P.; Dendale, P.; Pogosova, N.-G.V.; Zdrenghea, D.; Niebauer, J.; et al. Cardiac rehabilitation in Europe: Results from the European Cardiac Rehabilitation Inventory Survey. Eur. J. Cardiovasc. Prev. Rehabil. 2010, 17, 410–418. [Google Scholar] [CrossRef]
- Walli-Attaei, M.; Joseph, P.; Rosengren, A.; Chow, C.K.; Rangarajan, S.; Lear, S.A.; AlHabib, K.F.; Davletov, K.; Dans, A.; Lanas, F.; et al. Variations between women and men in risk factors, treatments, cardiovascular disease incidence, and death in 27 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet 2020, 396, 97–109. [Google Scholar] [CrossRef]
| Group 1 | Group 2 | Group 3 | |
|---|---|---|---|
| BMI | 31.06 (4.52) | 24.45 (3.34) | 28.88 (4.00) |
| SBP (mm Hg) | 142.69 (16.46) | 126.46 (14.42) | 138.45 (16.25) |
| DBP (mm Hg) | 85.09 (10.40) | 77.04 (8.67) | 84.43 (9.96) |
| Pulse rate (/min) | 75.15 (12.31) | 73.87 (14.00) | 74.38 (12.83) |
| TC (mg/dL) | 165.39 (27.18) | 178.59 (32.11) | 237.54 (26.79) |
| LDL-C (mg/dL) | 89.62 (23.16) | 95.38 (26.08) | 151.23 (24.44) |
| HDL-C (mg/dL) | 48.91 (11.65) | 66.01 (14.36) | 55.51 (12.50) |
| Non-HDL-C (mg/dL) | 115.80 (26.23) | 111.89 (26.90) | 181.96 (25.83) |
| TG (mg/dL) | 137.07 (61.35) | 85.00 (31.85) | 154.12 (61.70) |
| Fasting glucose (mg/dL) | 108.40 (18.02) | 94.13 (9.34) | 98.65 (12.94) |
| Uric acid (mg/dL) | 5.98 (1.13) | 4.42 (0.99) | 5.35 (1.03) |
| Age years | 54.94 (9.95) | 53.01 (7.94) | 49.34 (11.06) |
| Group 1 | Group 2 | Group 3 | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Sex | Women | 75 | 32.33 | 139 | 58.65 | 159 | 70.98 |
| Men | 157 | 67.67 | 98 | 41.35 | 65 | 29.02 | |
| Education | Primary | 2 | 0.86 | 3 | 1.27 | 4 | 1.79 |
| Occupational | 34 | 14.66 | 20 | 8.44 | 20 | 8.93 | |
| Secondary | 118 | 50.86 | 105 | 44.30 | 81 | 36.16 | |
| Tertiary | 78 | 33.62 | 109 | 45.99 | 119 | 53.13 | |
| Smoking | No | 210 | 90.52 | 202 | 85.23 | 196 | 87.50 |
| Yes | 22 | 9.48 | 35 | 14.77 | 28 | 12.50 | |
| Social situation | Lives alone | 11 | 4.74 | 12 | 5.06 | 18 | 8.04 |
| Lives with family | 221 | 95.26 | 225 | 94.94 | 206 | 91.96 | |
| Family history | No | 162 | 69.83 | 153 | 64.56 | 165 | 73.66 |
| Yes | 70 | 30.17 | 84 | 35.44 | 59 | 26.34 | |
| Medications | No | 25 | 10.82 | 62 | 26.61 | 88 | 39.46 |
| Yes | 206 | 89.18 | 171 | 73.39 | 135 | 60.54 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hincz, J.; Sterliński, M.; Kostrzewa, D.; Dąbrowski, R.; Smolis-Bąk, E. Cluster Analysis to Distinguish Patients Most Likely to Benefit from Outpatient Cardiac Rehabilitation—A Prospective, Multicenter Study. Int. J. Environ. Res. Public Health 2022, 19, 11000. https://doi.org/10.3390/ijerph191711000
Hincz J, Sterliński M, Kostrzewa D, Dąbrowski R, Smolis-Bąk E. Cluster Analysis to Distinguish Patients Most Likely to Benefit from Outpatient Cardiac Rehabilitation—A Prospective, Multicenter Study. International Journal of Environmental Research and Public Health. 2022; 19(17):11000. https://doi.org/10.3390/ijerph191711000
Chicago/Turabian StyleHincz, Jacek, Maciej Sterliński, Dariusz Kostrzewa, Rafał Dąbrowski, and Edyta Smolis-Bąk. 2022. "Cluster Analysis to Distinguish Patients Most Likely to Benefit from Outpatient Cardiac Rehabilitation—A Prospective, Multicenter Study" International Journal of Environmental Research and Public Health 19, no. 17: 11000. https://doi.org/10.3390/ijerph191711000
APA StyleHincz, J., Sterliński, M., Kostrzewa, D., Dąbrowski, R., & Smolis-Bąk, E. (2022). Cluster Analysis to Distinguish Patients Most Likely to Benefit from Outpatient Cardiac Rehabilitation—A Prospective, Multicenter Study. International Journal of Environmental Research and Public Health, 19(17), 11000. https://doi.org/10.3390/ijerph191711000







