Domains of Capacity Building in Whole-Systems Approaches to Prevent Obesity—A “Systematized” Review
Abstract
1. Introduction
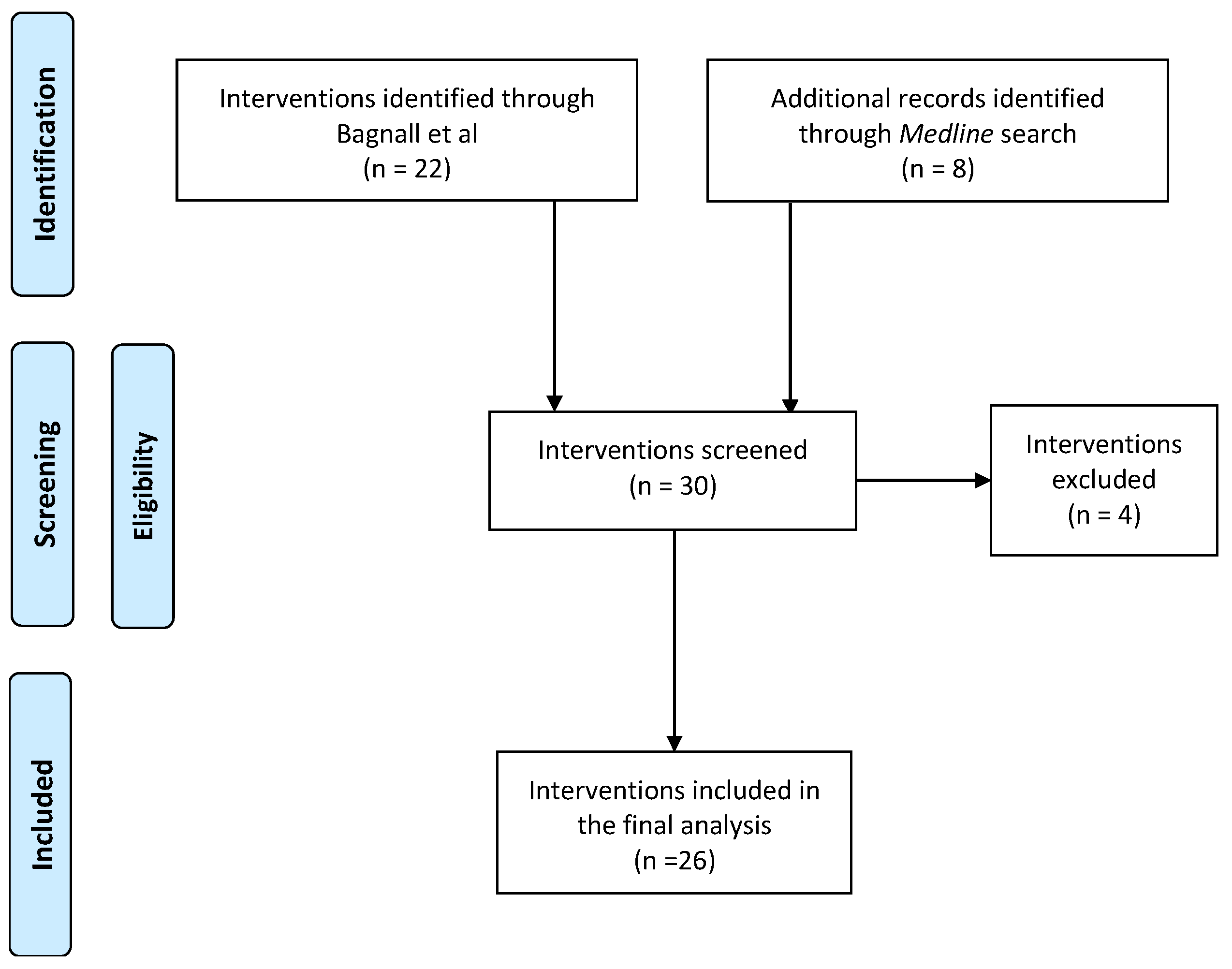
2. Materials and Methods
2.1. Search Strategy
2.2. Capacity Building Analysis
3. Results
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roberto, C.A.; Swinburn, B.; Hawkes, C.; Huang, T.T.; Costa, S.A.; Ashe, M.; Zwicker, L.; Cawley, J.H.; Brownell, K.D. Patchy progress on obesity prevention: Emerging examples, entrenched barriers, and new thinking. Lancet 2015, 385, 2400–2409. [Google Scholar] [CrossRef]
- Dobbs, R.; Sawers, C.; Thompson, F.; Manyika, J.; Woetzel, J.R.; Child, P.; McKenna, S.; Spatharou, A. Overcoming Obesity: An Initial Economic Analysis; McKinsey Global Institute: San Francisco, CA, USA, 2014. [Google Scholar]
- Butland, B.; Jebb, S.; Kopelman, P.; McPherson, K.; Thomas, S.; Mardell, J.; Parry, V. Tackling Obesities: Future Choices-Project Report; Citeseer: Forest Grove, OR, USA, 2007; Volume 10. [Google Scholar]
- Rutter, H.; Savona, N.; Glonti, K.; Bibby, J.; Cummins, S.; Finegood, D.T.; Greaves, F.; Harper, L.; Hawe, P.; Moore, L. The need for a complex systems model of evidence for public health. Lancet 2017, 390, 2602–2604. [Google Scholar] [CrossRef]
- Bagnall, A.-M.; Radley, D.; Jones, R.; Gately, P.; Nobles, J.; Van Dijk, M.; Blackshaw, J.; Montel, S.; Sahota, P. Whole systems approaches to obesity and other complex public health challenges: A systematic review. BMC Public Health 2019, 19, 8. [Google Scholar] [CrossRef] [PubMed]
- Hawe, P.; Shiell, A.; Riley, T. Theorising interventions as events in systems. Am. J. Community Psychol. 2009, 43, 267–276. [Google Scholar] [CrossRef]
- King, L.; Gill, T.; Allender, S.; Swinburn, B. Best practice principles for community-based obesity prevention: Development, content and application. Obes. Rev. 2011, 12, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R.M.; Speers, M.A.; McLeroy, K.; Fawcett, S.; Kegler, M.; Parker, E.; Smith, S.R.; Sterling, T.D.; Wallerstein, N. Identifying and defining the dimensions of community capacity to provide a basis for measurement. Health Educ. Behav. 1998, 25, 258–278. [Google Scholar] [CrossRef]
- Traverso-Yepez, M.; Maddalena, V.; Bavington, W.; Donovan, C. Community capacity building for health: A critical look at the practical implications of this approach. Sage Open 2012, 2, 2158244012446996. [Google Scholar] [CrossRef]
- Denney, L.; Valters, C. Evidence Synthesis: Security Sector Reform and Organisational Capacity Building; Department for International Development: London, UK, 2015.
- Jackson, P. Security sector reform and state building. Third World Q. 2011, 32, 1803–1822. [Google Scholar] [CrossRef]
- Bergeron, K.; Abdi, S.; DeCorby, K.; Mensah, G.; Rempel, B.; Manson, H. Theories, models and frameworks used in capacity building interventions relevant to public health: A systematic review. BMC Public Health 2017, 17, 914. [Google Scholar] [CrossRef]
- Smith, B.J.; Tang, K.C.; Nutbeam, D. WHO health promotion glossary: New terms. Health Promot. Int. 2006, 21, 340–345. [Google Scholar] [CrossRef]
- Millar, L.; Robertson, N.; Allender, S.; Nichols, M.; Bennett, C.; Swinburn, B. Increasing community capacity and decreasing prevalence of overweight and obesity in a community based intervention among Australian adolescents. Prev. Med. 2013, 56, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Wutzke, S.; Morrice, E.; Benton, M.; Wilson, A. Systems approaches for chronic disease prevention: Sound logic and empirical evidence, but is this view shared outside of academia? Public Health Res. Pract. 2016, 26, 2631632. [Google Scholar] [CrossRef] [PubMed]
- Leykum, L.K.; Pugh, J.; Lawrence, V.; Parchman, M.; Noël, P.H.; Cornell, J.; McDaniel, R.R. Organizational interventions employing principles of complexity science have improved outcomes for patients with Type II diabetes. Implement. Sci. 2007, 2, 28. [Google Scholar] [CrossRef]
- Lanham, H.J.; Leykum, L.K.; Taylor, B.S.; McCannon, C.J.; Lindberg, C.; Lester, R.T. How complexity science can inform scale-up and spread in health care: Understanding the role of self-organization in variation across local contexts. Soc. Sci. Med. 2013, 93, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Marcus, S.E.; Leischow, S.J.; Mabry, P.L.; Clark, P.I. Lessons learned from the application of systems science to tobacco control at the National Cancer Institute. Am. J. Public Health 2010, 100, 1163–1165. [Google Scholar] [CrossRef] [PubMed]
- Garside, R.; Pearson, M.; Hunt, H.; Moxham, T.; Anderson, R. Identifying the Key Elements and Interactions of a Whole System Approach to Obesity Prevention; Peninsula Technology Assessment Group (PenTAG): Exeter, UK, 2010. [Google Scholar]
- Swanepoel, E.; Fox, A.; Hughes, R. Practitioner consensus on the determinants of capacity building practice in high-income countries. Public Health Nutr. 2015, 18, 1898–1905. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Baillie, E.; Bjarnholt, C.; Gruber, M.; Hughes, R. A capacity-building conceptual framework for public health nutrition practice. Public Health Nutr. 2009, 12, 1031–1038. [Google Scholar] [CrossRef] [PubMed]
- Rowe, G.; Wright, G. The Delphi technique as a forecasting tool: Issues and analysis. Int. J. Forecast. 1999, 15, 353–375. [Google Scholar] [CrossRef]
- Bell, A.C.; Simmons, A.; Sanigorski, A.M.; Kremer, P.J.; Swinburn, B.A. Preventing childhood obesity: The sentinel site for obesity prevention in Victoria, Australia. Health Promot. Int. 2008, 23, 328–336. [Google Scholar] [CrossRef]
- de Groot, F.P.; Robertson, N.M.; Swinburn, B.A.; de Silva-Sanigorski, A.M. Increasing community capacity to prevent childhood obesity: Challenges, lessons learned and results from the Romp & Chomp intervention. BMC Public Health 2010, 10, 522. [Google Scholar]
- de Silva-Sanigorski, A.; Elea, D.; Bell, C.; Kremer, P.; Carpenter, L.; Nichols, M.; Smith, M.; Sharp, S.; Boak, R.; Swinburn, B. Obesity prevention in the family day care setting: Impact of the Romp & Chomp intervention on opportunities for children’s physical activity and healthy eating. Child: Care Health Dev. 2011, 37, 385–393. [Google Scholar]
- de Silva-Sanigorski, A.M.; Bell, A.C.; Kremer, P.; Nichols, M.; Crellin, M.; Smith, M.; Sharp, S.; de Groot, F.; Carpenter, L.; Boak, R. Reducing obesity in early childhood: Results from Romp & Chomp, an Australian community-wide intervention program. Am. J. Clin. Nutr. 2010, 91, 831–840. [Google Scholar] [PubMed]
- de Silva-Sanigorski, A.M.; Bolton, K.; Haby, M.; Kremer, P.; Gibbs, L.; Waters, E.; Swinburn, B. Scaling up community-based obesity prevention in Australia: Background and evaluation design of the Health Promoting Communities: Being Active Eating Well initiative. BMC Public Health 2010, 10, 65. [Google Scholar] [CrossRef] [PubMed]
- Johnson, B.; Kremer, P.; Swinburn, B.; de Silva-Sanigorski, A. Multilevel analysis of the Be Active Eat Well intervention: Environmental and behavioural influences on reductions in child obesity risk. Int. J. Obes. 2012, 36, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Sanigorski, A.M.; Bell, A.; Kremer, P.J.; Cuttler, R.; Swinburn, B.A. Reducing unhealthy weight gain in children through community capacity-building: Results of a quasi-experimental intervention program, Be Active Eat Well. Int. J. Obes. 2008, 32, 1060–1067. [Google Scholar] [CrossRef]
- Maitland, N.; Williams, M.; Jalaludin, B.; Allender, S.; Strugnell, C.; Brown, A.; Hayward, J.; Crooks, N.; Tredoux, J.; Li, V. Campbelltown–Changing our Future: Study protocol for a whole of system approach to childhood obesity in South Western Sydney. BMC Public Health 2019, 19, 1699. [Google Scholar] [CrossRef]
- Jenkins, E.; Lowe, J.; Allender, S.; Bolton, K.A. Process evaluation of a whole-of-community systems approach to address childhood obesity in western Victoria, Australia. BMC Public Health 2020, 20, 450. [Google Scholar] [CrossRef]
- Allender, S.; Millar, L.; Hovmand, P.; Bell, C.; Moodie, M.; Carter, R.; Swinburn, B.; Strugnell, C.; Lowe, J.; De la Haye, K. Whole of systems trial of prevention strategies for childhood obesity: WHO STOPS childhood obesity. Int. J. Environ. Res. Public Health 2016, 13, 1143. [Google Scholar] [CrossRef]
- Malakellis, M.; Hoare, E.; Sanigorski, A.; Crooks, N.; Allender, S.; Nichols, M.; Swinburn, B.; Chikwendu, C.; Kelly, P.M.; Petersen, S. School-based systems change for obesity prevention in adolescents: Outcomes of the Australian Capital Territory ‘It’s Your Move!’. Aust. New Zealand J. Public Health 2017, 41, 490–496. [Google Scholar] [CrossRef]
- Mathews, L.B.; Moodie, M.M.; Simmons, A.M.; Swinburn, B.A. The process evaluation of It’s Your Move!, an Australian adolescent community-based obesity prevention project. BMC Public Health 2010, 10, 448. [Google Scholar] [CrossRef]
- Millar, L.; Kremer, P.; de Silva-Sanigorski, A.; McCabe, M.; Mavoa, H.; Moodie, M.; Utter, J.; Bell, C.; Malakellis, M.; Mathews, L. Reduction in overweight and obesity from a 3-year community-based intervention in Australia: The ‘It’s Your Move!’project. Obes. Rev. 2011, 12, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Chomitz, V.R.; McGowan, R.J.; Wendel, J.M.; Williams, S.A.; Cabral, H.J.; King, S.E.; Olcott, D.B.; Cappello, M.; Breen, S.; Hacker, K.A. Healthy Living Cambridge Kids: A community-based participatory effort to promote healthy weight and fitness. Obesity 2010, 18, S45–S53. [Google Scholar] [CrossRef] [PubMed]
- Cousins, J.M.; Langer, S.M.; Thomas, C.; Rhew, L.K. Peer Reviewed: The Role of State Health Departments in Supporting Community-based Obesity Prevention. Prev. Chronic Dis. 2011, 8, A87. [Google Scholar] [PubMed]
- Serpas, S.; Brandstein, K.; McKennett, M.; Hillidge, S.; Zive, M.; Nader, P.R. San Diego Healthy Weight Collaborative: A systems approach to address childhood obesity. J. Health Care Poor Underserved 2013, 24, 80–96. [Google Scholar] [CrossRef]
- Economos, C.D.; Hyatt, R.R.; Goldberg, J.P.; Must, A.; Naumova, E.N.; Collins, J.J.; Nelson, M.E. A community intervention reduces BMI z-score in children: Shape Up Somerville first year results. Obesity 2007, 15, 1325–1336. [Google Scholar] [CrossRef]
- Gantner, L.A.; Olson, C.M. Evaluation of public health professionals’ capacity to implement environmental changes supportive of healthy weight. Eval. Program Plan. 2012, 35, 407–416. [Google Scholar] [CrossRef][Green Version]
- Schulz, A.J.; Zenk, S.; Odoms-Young, A.; Hollis-Neely, T.; Nwankwo, R.; Lockett, M.; Ridella, W.; Kannan, S. Healthy eating and exercising to reduce diabetes: Exploring the potential of social determinants of health frameworks within the context of community-based participatory diabetes prevention. Am. J. Public Health 2005, 95, 645–651. [Google Scholar] [CrossRef]
- Samuels, S.E.; Craypo, L.; Boyle, M.; Crawford, P.B.; Yancey, A.; Flores, G. The California endowment’s healthy eating, active communities program: A midpoint review. Am. J. Public Health 2010, 100, 2114–2123. [Google Scholar] [CrossRef]
- Mikkelsen, B.E.; Novotny, R.; Gittelsohn, J. Multi-level, multi-component approaches to community based interventions for healthy living—A three case comparison. Int. J. Environ. Res. Public Health 2016, 13, 1023. [Google Scholar] [CrossRef]
- Appel, J.M.; Fullerton, K.; Hennessy, E.; Korn, A.R.; Tovar, A.; Allender, S.; Hovmand, P.S.; Kasman, M.; Swinburn, B.A.; Hammond, R.A. Design and methods of Shape Up Under 5: Integration of systems science and community-engaged research to prevent early childhood obesity. PLoS ONE 2019, 14, e0220169. [Google Scholar]
- Schwarte, L.; Samuels, S.E.; Capitman, J.; Ruwe, M.; Boyle, M.; Flores, G. The Central California Regional Obesity Prevention Program: Changing nutrition and physical activity environments in California’s heartland. Am. J. Public Health 2010, 100, 2124–2128. [Google Scholar] [CrossRef] [PubMed]
- Kegler, M.C.; Norton, B.L.; Aronson, R. Achieving organizational change: Findings from case studies of 20 California healthy cities and communities coalitions. Health Promot. Int. 2008, 23, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Kegler, M.C.; Painter, J.E.; Twiss, J.M.; Aronson, R.; Norton, B.L. Evaluation findings on community participation in the California Healthy Cities and Communities program. Health Promot. Int. 2009, 24, 300–310. [Google Scholar] [CrossRef][Green Version]
- Twiss, J.M.; Duma, S.; Look, V.; Shaffer, G.S.; Watkins, A.C. Twelve years and counting: California’s experience with a statewide Healthy Cities and Community program. Public Health Rep. 2000, 115, 125. [Google Scholar] [CrossRef] [PubMed]
- Fialkowski, M.K.; DeBaryshe, B.; Bersamin, A.; Nigg, C.; Guerrero, R.L.; Rojas, G.; Vargo, A.; Belyeu-Camacho, T.; Castro, R.; Luick, B. A community engagement process identifies environmental priorities to prevent early childhood obesity: The children’s healthy living (CHL) program for remote underserved populations in the US affiliated pacific islands, Hawaii and Alaska. Matern. Child Health J. 2014, 18, 2261–2274. [Google Scholar] [CrossRef] [PubMed]
- Wilken, L.R.; Novotny, R.; Fialkowski, M.K.; Boushey, C.J.; Nigg, C.; Paulino, Y.; Guerrero, R.L.; Bersamin, A.; Vargo, D.; Kim, J. Children’s Healthy Living (CHL) Program for remote underserved minority populations in the Pacific region: Rationale and design of a community randomized trial to prevent early childhood obesity. BMC Public Health 2013, 13, 944. [Google Scholar] [CrossRef] [PubMed]
- Gittelsohn, J.; Roache, C.; Kratzmann, M.; Reid, R.; Ogina, J.; Sharma, S. Participatory research for chronic disease prevention in Inuit communities. Am. J. Health Behav. 2010, 34, 453–464. [Google Scholar] [CrossRef]
- Raine, K.D.; Plotnikoff, R.; Nykiforuk, C.; Deegan, H.; Hemphill, E.; Storey, K.; Schopflocher, D.; Veugelers, P.; Wild, T.C.; Ohinmaa, A. Reflections on community-based population health intervention and evaluation for obesity and chronic disease prevention: The Healthy Alberta Communities project. Int. J. Public Health 2010, 55, 679–686. [Google Scholar] [CrossRef]
- Raine, K.D.; Plotnikoff, R.; Schopflocher, D.; Lytvyak, E.; Nykiforuk, C.I.; Storey, K.; Ohinmaa, A.; Purdy, L.; Veugelers, P.; Wild, T.C. Healthy Alberta Communities: Impact of a three-year community-based obesity and chronic disease prevention intervention. Prev. Med. 2013, 57, 955–962. [Google Scholar] [CrossRef]
- Amed, S.; Naylor, P.-J.; Pinkney, S.; Shea, S.; Mâsse, L.C.; Berg, S.; Collet, J.-P.; Higgins, J.W. Creating a collective impact on childhood obesity: Lessons from the SCOPE initiative. Can. J. Public Health 2015, 106, e426–e433. [Google Scholar] [CrossRef]
- Amed, S.; Shea, S.; Pinkney, S.; Wharf Higgins, J.; Naylor, P.-J. Wayfinding the Live 5-2-1-0 initiative—at the intersection between systems thinking and community-based childhood obesity prevention. Int. J. Environ. Res. Public Health 2016, 13, 614. [Google Scholar] [CrossRef] [PubMed]
- McIntosh, B.; Daly, A.; Mâsse, L.C.; Collet, J.-P.; Higgins, J.W.; Naylor, P.-J.; Amed, S. Sustainable childhood obesity prevention through community engagement (SCOPE) program: Evaluation of the implementation phase. Biochem. Cell Biol. 2015, 93, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, D.M.; Cummins, S.; Sautkina, E.; Ogilvie, D.; Petticrew, M.; Jones, A.; Wheeler, K.; White, M. The role and status of evidence and innovation in the healthy towns programme in England: A qualitative stakeholder interview study. J. Epidemiol. Community Health 2013, 67, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Sautkina, E.; Goodwin, D.; Jones, A.; Ogilvie, D.; Petticrew, M.; White, M.; Cummins, S. Lost in translation? Theory, policy and practice in systems-based environmental approaches to obesity prevention in the Healthy Towns programme in England. Health Place 2014, 29, 60–66. [Google Scholar] [CrossRef]
- Middleton, G.; Henderson, H.; Evans, D. Implementing a community-based obesity prevention programme: Experiences of stakeholders in the north east of England. Health Promot. Int. 2014, 29, 201–211. [Google Scholar] [CrossRef]
- Lloyd, J.; Creanor, S.; Logan, S.; Green, C.; Dean, S.G.; Hillsdon, M.; Abraham, C.; Tomlinson, R.; Pearson, V.; Taylor, R.S. Effectiveness of the Healthy Lifestyles Programme (HeLP) to prevent obesity in UK primary-school children: A cluster randomised controlled trial. Lancet Child Adolesc. Health 2018, 2, 35–45. [Google Scholar] [CrossRef]
- Lloyd, J.J.; Wyatt, K.M.; Creanor, S. Behavioural and weight status outcomes from an exploratory trial of the Healthy Lifestyles Programme (HeLP): A novel school-based obesity prevention programme. BMJ Open 2012, 2, e000390. [Google Scholar] [CrossRef]
- Bloch, P.; Toft, U.; Reinbach, H.C.; Clausen, L.T.; Mikkelsen, B.E.; Poulsen, K.; Jensen, B.B. Revitalizing the setting approach–supersettings for sustainable impact in community health promotion. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 118. [Google Scholar] [CrossRef]
- Toft, U.; Bloch, P.; Reinbach, H.C.; Winkler, L.L.; Buch-Andersen, T.; Aagaard-Hansen, J.; Mikkelsen, B.E.; Jensen, B.B.; Glümer, C. Project SoL—A community-based, multi-component health promotion intervention to improve eating habits and physical activity among Danish families with young children. Part 1: Intervention development and implementation. Int. J. Environ. Res. Public Health 2018, 15, 1097. [Google Scholar] [CrossRef]
- Borys, J.-M.; Le Bodo, Y.; De Henauw, S.; Moreno, L.; Romon, M.; Seidell, J.; Visscher, T. Preventing Childhood Obesity: EPODE European Network Recommendations; Lavoisier: Cachan, France, 2011. [Google Scholar]
- Borys, J.M.; Le Bodo, Y.; Jebb, S.A.; Seidell, J.; Summerbell, C.; Richard, D.; De Henauw, S.; Moreno, L.; Romon, M.; Visscher, T. EPODE approach for childhood obesity prevention: Methods, progress and international development. Obes. Rev. 2012, 13, 299–315. [Google Scholar] [CrossRef]
- Romon, M.; Lommez, A.; Tafflet, M.; Basdevant, A.; Oppert, J.M.; Bresson, J.L.; Ducimetiere, P.; Charles, M.A.; Borys, J.M. Downward trends in the prevalence of childhood overweight in the setting of 12-year school-and community-based programmes. Public Health Nutr. 2009, 12, 1735–1742. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.Y.; Bartsch, S.M.; Mui, Y.; Haidari, L.A.; Spiker, M.L.; Gittelsohn, J. A systems approach to obesity. Nutr. Rev. 2017, 75, 94–106. [Google Scholar] [CrossRef] [PubMed]
- Hawe, P.; King, L.; Noort, M.; Gifford, S.M.; Lloyd, B. Working invisibly: Health workers talk about capacity-building in health promotion. Health Promot. Int. 1998, 13, 285–295. [Google Scholar] [CrossRef]
- Foucault, M. Discipline and Punish: The Birth of the Prison; Lane, A., Translator; Vintage Books: New York, NY, USA, 1991. [Google Scholar]
- Foucault, M.; Rabinow, P. The Foucault Reader: [An Introduction to Foucault’s Thought, with Major New Unpublished Material]; Penguin Books: London, UK, 1984. [Google Scholar]
- Olstad, D.L.; Raine, K.D.; McCargar, L.J. Adopting and implementing nutrition guidelines in recreational facilities: Public and private sector roles. A multiple case study. BMC Public Health 2012, 12, 376. [Google Scholar] [CrossRef]
- Sarrafzadegan, N.; Rabiei, K.; Wong, F.; Roohafza, H.; Zarfeshani, S.; Noori, F.; Grainger-Gasser, A. The sustainability of interventions of a community-based trial on children and adolescents’ healthy lifestyle. ARYA Atheroscler. 2014, 10, 107. [Google Scholar]
- Greaney, M.L.; Hardwick, C.K.; Spadano-Gasbarro, J.L.; Mezgebu, S.; Horan, C.M.; Schlotterbeck, S.; Austin, S.B.; Peterson, K.E. Implementing a multicomponent school-based obesity prevention intervention: A qualitative study. J. Nutr. Educ. Behav. 2014, 46, 576–582. [Google Scholar] [CrossRef][Green Version]
- Jain, A.; Langwith, C. Collaborative school-based obesity interventions: Lessons learned from 6 southern districts. J. Sch. Health 2013, 83, 213–222. [Google Scholar] [CrossRef]
- Dreisinger, M.L.; Boland, E.M.; Filler, C.D.; Baker, E.A.; Hessel, A.S.; Brownson, R.C. Contextual factors influencing readiness for dissemination of obesity prevention programs and policies. Health Educ. Res. 2012, 27, 292–306. [Google Scholar] [CrossRef]
- Khan, M.S.; Khan, I.; Qureshi, Q.A.; Ismail, H.M.; Rauf, H.; Latif, A.; Tahir, M. The styles of leadership: A critical review. Public Policy Adm. Res. 2015, 5, 87–92. [Google Scholar]
- Whelan, J.; Love, P.; Millar, L.; Allender, S.; Bell, C. Sustaining obesity prevention in communities: A systematic narrative synthesis review. Obes. Rev. 2018, 19, 839–851. [Google Scholar] [CrossRef]
- Tran, H.N.Q.; Killedar, A.; Tan, E.J.; Moodie, M.; Hayes, A.; Swinburn, B.; Nichols, M.; Brown, V. Cost-effectiveness of scaling up a whole-of-community intervention: The Romp & Chomp early childhood obesity prevention intervention. Pediatric Obes. 2022, 17, e12915. [Google Scholar]
- Finucane, M.M.; Stevens, G.A.; Cowan, M.J.; Danaei, G.; Lin, J.K.; Paciorek, C.J.; Singh, G.M.; Gutierrez, H.R.; Lu, Y.; Bahalim, A.N. National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9 1 million participants. Lancet 2011, 377, 557–567. [Google Scholar] [CrossRef]

| Capacity Domain | Focus Questions Evidence of: |
|---|---|
| Leadership |
|
| Intelligence |
|
| Partnerships |
|
| Workforce |
|
| Community |
|
| Project Management |
|
| Resource Mobilization |
|
| Study Region | Study Description/Summary of Capacity-Building Evidence | Leadership | Intelligence | Partnerships | Workforce | Community | Project Management | Resource Mobilization | Capacity-Building Score |
|---|---|---|---|---|---|---|---|---|---|
| Australia | Romp & Chomp: The intervention activities had a strong focus on community capacity building and developing sustainable changes in areas of policy, sociocultural, and physical environments by using a socioecological framework. The Romp & Chomp action plan was developed with extensive community consultation and stakeholder engagement, and a management committee of stakeholders oversaw its implementation [23,24,25,26]. | 1 | 3 | 2 | 3 | 3 | 3 | 2 | 17 |
| Be Active Eat Well: Building capacity was one of the key foci of this intervention (Objective 1 out of 10). It included broad actions around governance, partnerships, coordination, training, and resource allocation [27,28,29]. | 2 | 3 | 2 | 3 | 3 | 3 | 3 | 19 | |
| Campbelltown—Changing Our Future: The five-step approach: (1) set up a childhood obesity-monitoring system by collecting baseline data from children in primary schools across Campbelltown LGA to give a local context to the community when developing the systems map; (2) key stakeholders develop systems maps that inform the development of the interventions; (3) key stakeholders and community groups identify priority areas for action and form working groups; (4) implementation of the interventions; (5) evaluation of the interventions, entailing several important domains of CB [30]. | 1 | 3 | 1 | 1 | 3 | 3 | 1 | 13 | |
| Sustainable Eating Activity Change Portland: This intervention utilized asset-based community development (ABCD)—a strategy promoting sustainable community development—alongside applications of a collective impact framework that focused on efforts to connect and mobilize the community to act [31]. | 1 | 3 | 1 | 1 | 3 | 3 | 1 | 13 | |
| WHO Stops Childhood Obesity: Intensive training and support within each community was oriented around strengthening WHO systems building blocks (e.g., workforce development, resources intelligence) and the New South Wales capacity-building framework (e.g., partners and networks) in community settings. A key focus included mapping existing systems and using these maps to develop and implement whole-systems change with community members and implementation support to optimize interventions [32]. | 2 | 3 | 3 | 2 | 3 | 3 | 1 | 17 | |
| It’s Your Move—ACT: Capacity building among school project officers and student ambassadors (workshop and training opportunities) was a primary goal. The Analyses Grid for Environments Linked to Obesity (ANGELO) framework was modified to incorporate the World Health Organization systems building blocks, which include leadership, information, financing/resources, partnerships, and workforce development, into the development and implementation of the project to reduce unhealthy weight gain among adolescents through comprehensive school- and community-based systems change [23,33,34,35]. | 2 | 3 | 3 | 3 | 3 | 3 | 3 | 20 | |
| United States | Healthy Living Cambridge Kids: A community-based participatory research approach (i.e., The Healthy Children Task Force (Task Force) was utilized to engage community members in all aspects of the intervention process from research questions to design/implementation of the study and analysis/dissemination of findings [36]. | 1 | 3 | 2 | 2 | 3 | 2 | 2 | 15 |
| Childhood Obesity Prevention Demonstration Project: This included an implementation of numerous multi-level, multi-setting interventions for preventing and reducing obesity among children in a community, which for the most part ran as a collaboration between government- and community-level stakeholders. A specific focus included the application of lessons learned (regarding obesity prevention) from other geographical regions [37]. | 1 | 1 | 3 | 3 | 1 | 2 | 3 | 14 | |
| The San Diego Healthy Weight Collaborative: Jointly implemented strategies in a Latino, underserved community included: (1) building an effective and sustainable collaborative team; (2) disseminating a healthy weight message across sectors; (3) assessing weight status and healthy weight plans in primary care, school, and early childhood settings; and (4) implementing policy changes to support healthy eating and physical activity [38]. | 3 | 2 | 3 | 3 | 3 | 2 | 2 | 18 | |
| Shape Up Somerville: A community-based participatory research approach was implemented that focused on facilitating collaborative partnerships with the communities in all phases of the research: identifying the problem; designing, implementing, and evaluating the intervention; and identifying how data would inform actions to improve health within the community. Community engagement consisted of several forms, including meetings, focus groups, and key informant interviews, and led to the formation of several Shape Up Summerville advisory councils that remained actively involved throughout the study [39]. | 1 | 3 | 3 | 2 | 3 | 3 | 1 | 16 | |
| Healthy Start Partnership: Efforts were made to better understand the challenges faced by public health professionals in implementing environmental and policy interventions related to public health through (1) participant observation of regional- and county-level meetings and conference calls; (2) qualitative interviews with HSP partners; and (3) self-administered structured questionnaires with HSP partners [40]. | 1 | 2 | 3 | 2 | 2 | 2 | 1 | 13 | |
| Healthy Eating and Exercising to Reduce Diabetes: A community-based participatory intervention was implemented to identify facilitators of and barriers to sustained community efforts to address social factors that contribute to diabetes (and health). A concerted effort was put in to identify proximate (e.g., knowledge, diet) and intermediate (e.g., access to fresh produce) factors that contributed existing health trends. Education and community training sessions were conducted through the mediation of the steering committee. Further, partnership building and sourcing additional funds was actively addressed throughout the lifetime of the study [41]. | 2 | 3 | 2 | 3 | 2 | 2 | 2 | 16 | |
| Healthy Eating, Active Communities Program: Changes in foods and beverages sold at schools and in neighborhoods; changes in school and after-school physical activity programming and equipment; individual-level changes in children’s attitudes and behaviors related to food and physical activity; and HEAC-related awareness and engagement on the part of community members, stakeholders, and policymakers were achieved through: (1) Engaging parents and families as advocates for healthier food and physical activity; (2) developing policy advocacy capacity in residents; (3) committing healthcare spokespersons to testifying at school board meetings, planning commission meetings, and city council meetings, and (4) educating parents on how some businesses market unhealthy food and physical activity to children [42]. | 2 | 3 | 2 | 3 | 3 | 3 | 2 | 18 | |
| Baltimore Healthy Communities for Kids: A mixture of policy working groups, systems science modelling, regular meetings with key stakeholder groups, trainings (in person and online) of food source owners and youth leaders, and social media campaigns were utilized to increase affordability, availability, purchase, and consumption of healthy foods by low-income African American children and reduce obesity [43]. | 3 | 3 | 2 | 3 | 3 | 3 | 1 | 18 | |
| Shape Up Under 5: Stakeholder-driven community diffusion—a novel conceptual framework which entails many domains of capacity building—was implemented to better understand how and why stakeholder groups succeed and the conditions under which they create community-wide change in the context of childhood obesity [44]. | 1 | 3 | 2 | 2 | 2 | 2 | 1 | 13 | |
| Central California Regional Obesity Prevention Program: Promoting of safe places for physical activity, increased access to fresh fruits and vegetables, and supporting the community and youth engagement in local and regional efforts to change nutrition and physical activity environments for obesity prevention was undertaken using a regionally localized/focused workforce development, community engagement, and policy change approach [45]. | 2 | 3 | 3 | 3 | 3 | 3 | 1 | 18 | |
| California Healthy Cities and Communities: Numerous new health and well-being programs were developed, organizational policies and practices adopted, and new financial resources leveraged across 20 participating sites through organizational development (city governments, lead agencies and community organizations), enhancing leadership skills among community residents, strengthening relationships among neighbors, and providing opportunities for residents to get involved in the civic life of their communities [46,47,48]. | 2 | 2 | 3 | 2 | 3 | 2 | 3 | 17 | |
| Pacific | Children’s Healthy Living: Childhood obesity among Pacific children was investigated using multiple approaches including (1) program/data inventories and situational analyses; (2) training of professionals and paraprofessionals in obesity prevention; (3) development of a Pacific food, nutrition, and physical activity data management and evaluation system; (4) development and conduct of a community-based environmental intervention to prevent, maintain, or reduce young child overweight and obesity; (5) evaluation of the environmental intervention; and (6) incurring at least one obesity-prevention policy change per jurisdiction [43,49,50]. | 1 | 3 | 3 | 3 | 3 | 3 | 1 | 17 |
| Canada | Healthy Food North: Attempts to increase consumption of traditional foods (e.g., caribou, fish) and nutrient-dense, store-bought foods low in fat and sugar (e.g., fruits, vegetables); decrease consumption of non-nutrient-dense, high-fat, high-sugar foods (e.g., soda, chips); and increase engagement in moderate and vigorous physical activity while reducing sedentary activity were made including promotional materials, media, and interactive educational activities held in food shops, worksites, and other community venues as well as community-wide events [51]. | 1 | 3 | 3 | 3 | 3 | 3 | 1 | 17 |
| Healthy Alberta Communities: Attempts at: (1) reducing prevalence of overweight and chronic disease risk, (2) increasing community capacity to promote health, and (3) informing policy, practice, and research decisions about public health were made through a multitude of physical activity and nutrition intervention approaches that were built upon the premise of community-based participatory research [52,53]. | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 21 | |
| Sustainable Childhood Obesity Prevention through Community Engagement (SCOPE): A multi-setting, multi-component program designed to enhance community capacity to create and deliver solutions to promote healthy eating, physical activity, and healthy weights among school-aged children was implemented. Underpinned by social ecological theory, community-based and community-driven action facilitated by the best evidence and shared strategies across multiple stakeholders was utilized to promote healthy body weights [54,55,56]. | 2 | 3 | 3 | 3 | 3 | 3 | 1 | 18 | |
| United Kingdom and Europe | Healthy towns England: More than 200 individual interventions, primarily focused on promoting healthy diet and physical activity, were implemented with no reference to community capacity building [57,58]. | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 |
| Neighbourhood Renewal Fund—Obesity Prevention: A series of interventions aimed at changing nutrition and physical activity behaviors in the local community was implemented without any notable emphasis on capacity building [59]. | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 8 | |
| Healthy Lifestyle Program: A systematic process—Intervention Mapping (IM)—was applied to plan a school-based obesity-prevention intervention. Several domains of capacity building, including needs assessments, intelligence gathering, and stakeholder consultations, were included in this process [60,61]. | 1 | 3 | 1 | 3 | 2 | 2 | 1 | 13 | |
| Sundhed og Lokalsamfund: Promotion of healthier lifestyles among Danish children aged 3–8 years and their families was achieved through collaborating with the local educational programs for nurses, school, and kindergarten and by planning for a training of program ambassadors among the local workforces [43,62,63]. | 2 | 3 | 3 | 2 | 3 | 3 | 1 | 17 | |
| Ensemble Prévenons l’Obésité des Enfants: A coordinated, capacity-building approach aimed at reducing childhood obesity was implemented through the engagement of local environments, childhood settings, and family norms. Specific emphasis on minimizing cultural or societal stigmatization, step-by-step learning, and an experience of healthy lifestyle habits tailored to the needs of all socioeconomic groups was included with all objectives based around (1) political commitment and policy change; (2) securing sufficient fiscal and physical resources; (3) planning, coordinating, and providing the social marketing, communication, and support services for community practitioners and leaders; and (4) using evidence from a wide variety of sources [64,65,66]. | 1 | 3 | 2 | 2 | 3 | 3 | 3 | 17 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jayasinghe, S.; Soward, R.; Dalton, L.; Holloway, T.P.; Murray, S.; Patterson, K.A.E.; Ahuja, K.D.K.; Hughes, R.; Byrne, N.M.; Hills, A.P. Domains of Capacity Building in Whole-Systems Approaches to Prevent Obesity—A “Systematized” Review. Int. J. Environ. Res. Public Health 2022, 19, 10997. https://doi.org/10.3390/ijerph191710997
Jayasinghe S, Soward R, Dalton L, Holloway TP, Murray S, Patterson KAE, Ahuja KDK, Hughes R, Byrne NM, Hills AP. Domains of Capacity Building in Whole-Systems Approaches to Prevent Obesity—A “Systematized” Review. International Journal of Environmental Research and Public Health. 2022; 19(17):10997. https://doi.org/10.3390/ijerph191710997
Chicago/Turabian StyleJayasinghe, Sisitha, Robert Soward, Lisa Dalton, Timothy P. Holloway, Sandra Murray, Kira A. E. Patterson, Kiran D. K. Ahuja, Roger Hughes, Nuala M. Byrne, and Andrew P. Hills. 2022. "Domains of Capacity Building in Whole-Systems Approaches to Prevent Obesity—A “Systematized” Review" International Journal of Environmental Research and Public Health 19, no. 17: 10997. https://doi.org/10.3390/ijerph191710997
APA StyleJayasinghe, S., Soward, R., Dalton, L., Holloway, T. P., Murray, S., Patterson, K. A. E., Ahuja, K. D. K., Hughes, R., Byrne, N. M., & Hills, A. P. (2022). Domains of Capacity Building in Whole-Systems Approaches to Prevent Obesity—A “Systematized” Review. International Journal of Environmental Research and Public Health, 19(17), 10997. https://doi.org/10.3390/ijerph191710997








