Dry Needling Alone or in Combination with Exercise Therapy versus Other Interventions for Reducing Pain and Disability in Subacromial Pain Syndrome: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Eligibility Criteria
2.3. Information Sources and Search Strategy
2.4. Study Selection Process
2.5. Data Extraction and Quality Assessment
2.6. Synthesis Methods
3. Results
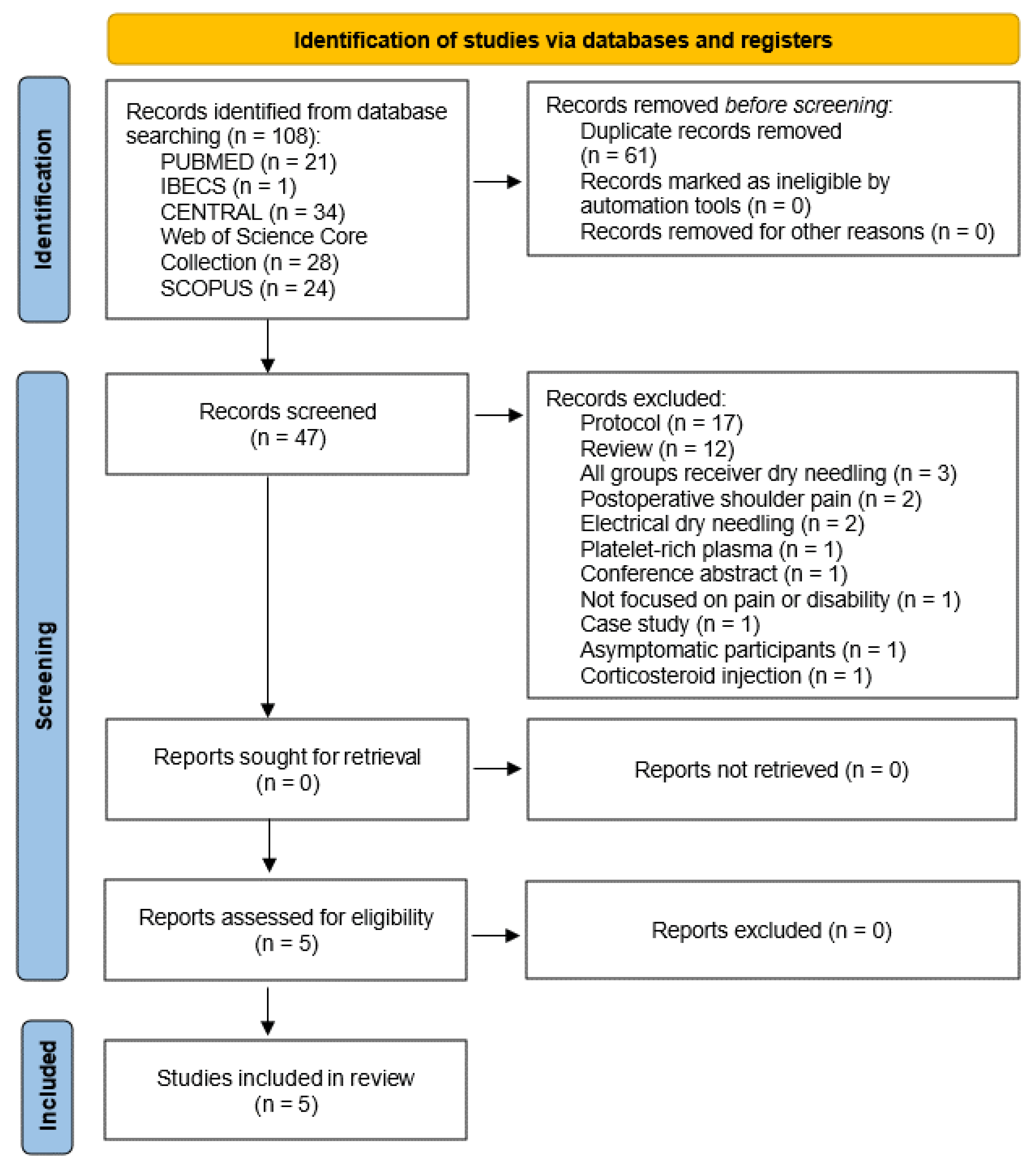
3.1. Study Identification and Selection Process
3.2. General Characteristics of Included Studies
3.3. Sample Characteristics
3.4. Intervention Characteristics
3.5. Measures
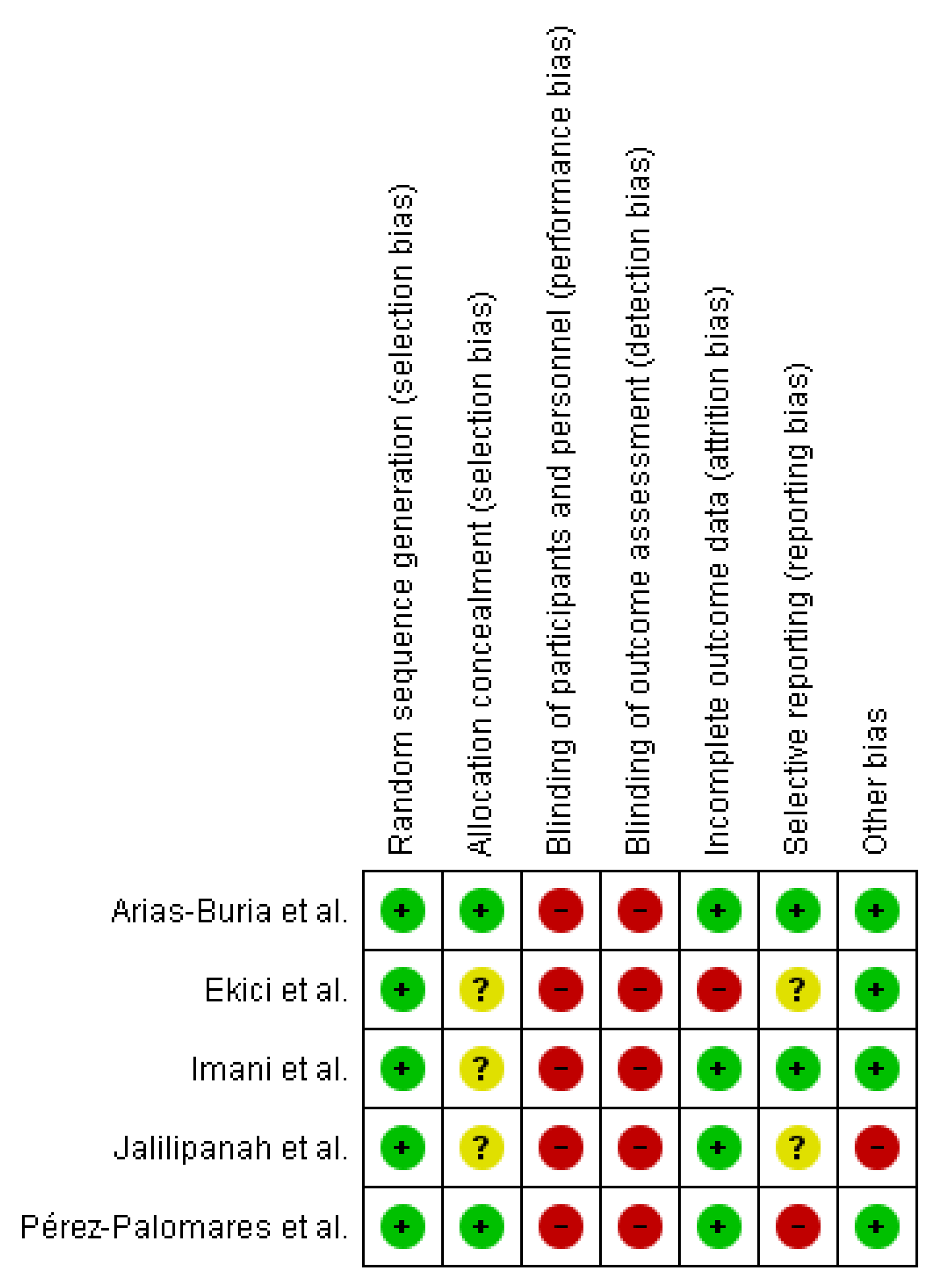
3.6. Risk of Bias
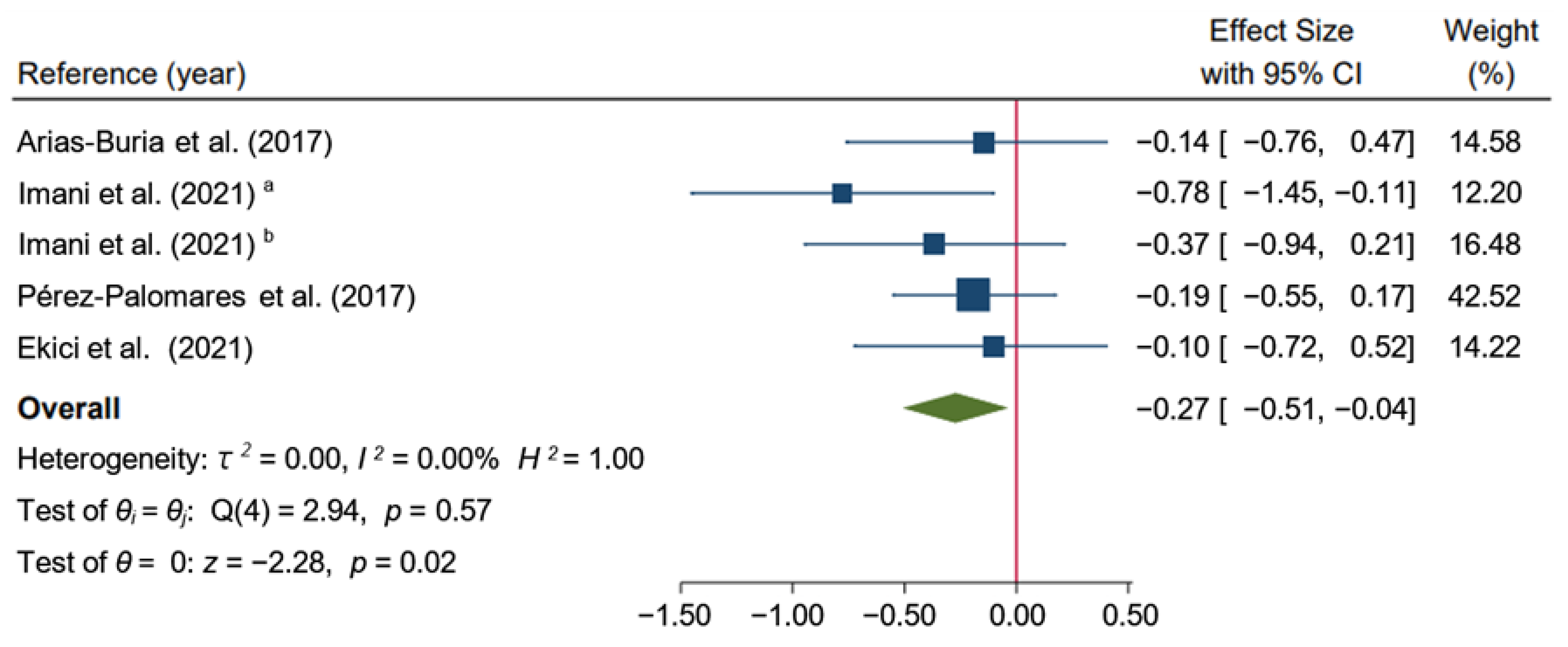
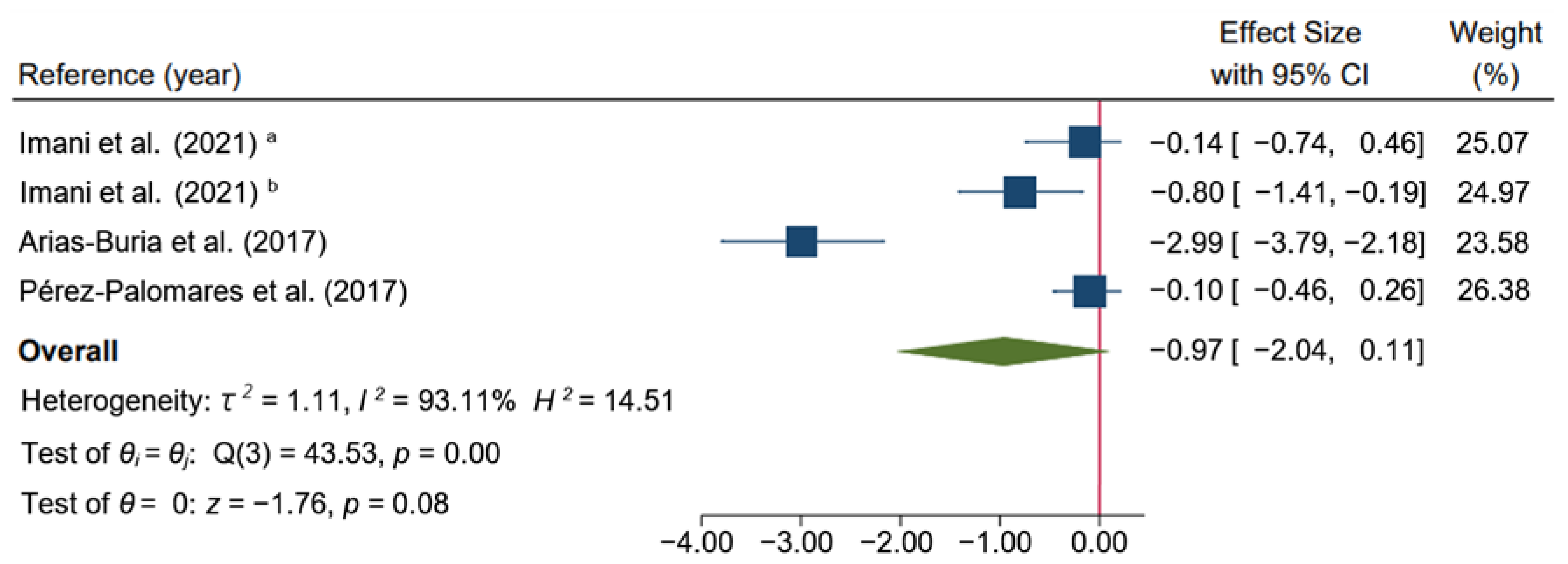
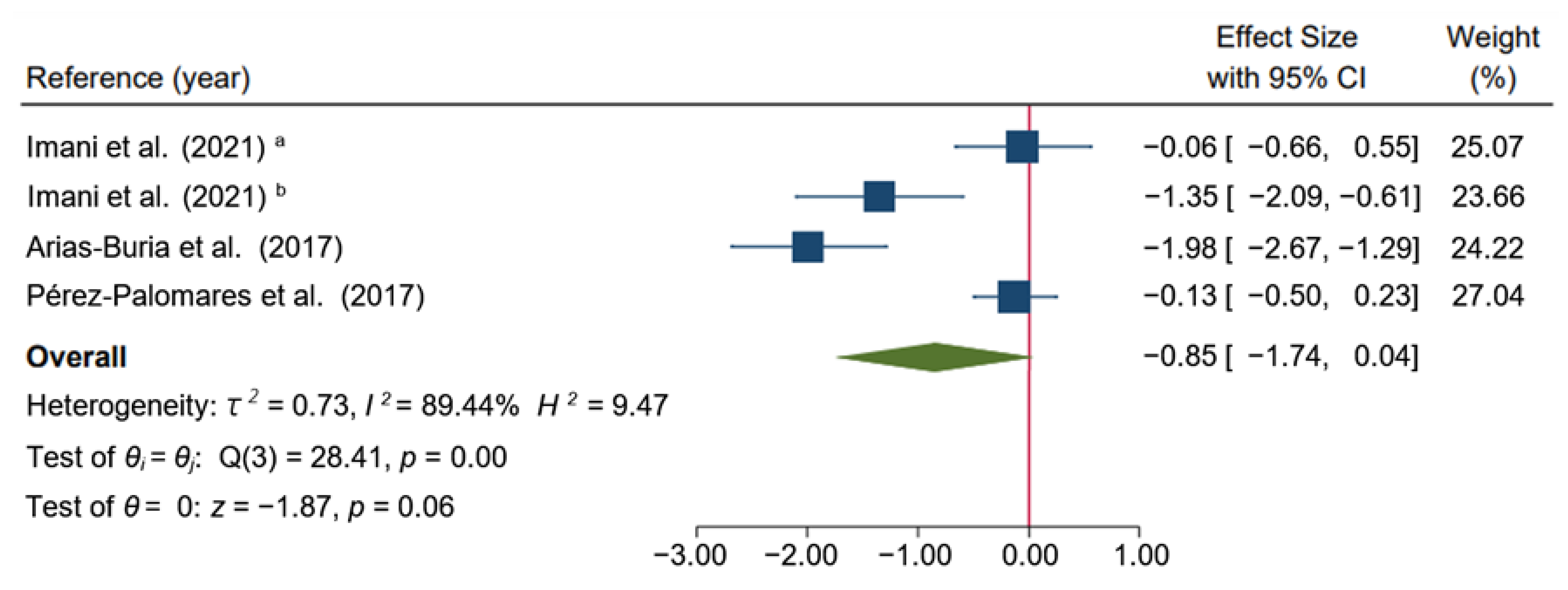
3.7. Intervention Results
3.8. Quality of Evidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Database | Search Terms (Date of Search: 3 July 2022) | |
|---|---|---|
| Pubmed | (“Shoulder Impingement Syndrome”[Mesh] AND “Dry Needling”[Mesh] AND “Pain”[Mesh]) OR ((“shoulder impingement syndrome”[tw] OR “subacromial pain syndrome”[tw] OR “rotator cuff”[tw]) AND “dry needling”[tw] AND (pain[tw] OR soreness[tw] OR disability[tw])) AND random*[tw] | |
| IBECS | mh:(“Shoulder Impingement Syndrome” AND “Dry Needling” AND “Pain”) OR tw:((“shoulder impingement syndrome” OR “subacromial pain syndrome”) AND “dry needling” AND (pain OR soreness OR disability)) | |
| CENTRAL | #1 | (“shoulder impingement syndrome” OR “subacromial pain syndrome” OR “rotator cuff”) (Word variations have been searched) |
| #2 | (“dry needling”) (Word variations have been searched) | |
| #3 | (Pain OR soreness OR disability) (Word variations have been searched) | |
| #4 | MeSH descriptor: [Shoulder Impingement Syndrome] explode all trees | |
| #5 | MeSH descriptor: [Dry Needling] explode all trees | |
| #6 | MeSH descriptor: [Pain] explode all trees | |
| #7 | (#1 AND #2 AND #3) OR (#4 AND #5 AND #6) | |
| Web of Science Core Collection | TS = ((“shoulder impingement syndrome” OR “subacromial pain syndrome” OR “rotator cuff”) AND “dry needling” AND (pain OR soreness OR disability) AND random*) | |
| SCOPUS | TITLE-ABS-KEY ((“shoulder impingement syndrome” OR “subacromial pain syndrome” OR “rotator cuff”) AND “dry needling” AND (pain OR soreness OR disability) AND random*) | |
References
- Engebretsen, K.B.; Grotle, M.; Natvig, B. Patterns of Shoulder Pain during a 14-Year Follow-up: Results from a Longitudinal Population Study in Norway. Shoulder Elbow 2015, 7, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Luime, J.J.; Koes, B.W.; Hendriksen, I.J.M.; Burdorf, A.; Verhagen, A.P.; Miedema, H.S.; Verhaar, J.A.N. Prevalence and Incidence of Shoulder Pain in the General Population; a Systematic Review. Scand. J. Rheumatol. 2004, 33, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Lazaro, R. Shoulder Impingement Syndromes: Implications on Physical Therapy Examination and Intervention. J. Jpn. Phys. Ther. Assoc. 2005, 8, 1–7. [Google Scholar] [CrossRef]
- Diercks, R.; Bron, C.; Dorrestijn, O.; Meskers, C.; Naber, R.; de Ruiter, T.; Willems, J.; Winters, J.; van der Woude, H.J. Guideline for Diagnosis and Treatment of Subacromial Pain Syndrome: A Multidisciplinary Review by the Dutch Orthopaedic Association. Acta Orthop. 2014, 85, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Michener, L.A.; McClure, P.W.; Karduna, A.R. Anatomical and Biomechanical Mechanisms of Subacromial Impingement Syndrome. Clin. Biomech. 2003, 18, 369–379. [Google Scholar] [CrossRef]
- Özsoy, M.H. Subakromiyal Sıkışma Sendromu. TOTBID Dergisi 2013, 12, 340–352. [Google Scholar] [CrossRef]
- Sergienko, S.; Kalichman, L. Myofascial Origin of Shoulder Pain: A Literature Review. J. Bodyw. Mov. Ther. 2015, 19, 91–101. [Google Scholar] [CrossRef]
- Ribeiro, D.C.; Belgrave, A.; Naden, A.; Fang, H.; Matthews, P.; Parshottam, S. The Prevalence of Myofascial Trigger Points in Neck and Shoulder-Related Disorders: A Systematic Review of the Literature. BMC Musculoskelet. Disord. 2018, 19, 1–13. [Google Scholar] [CrossRef]
- Navarro-Santana, M.J.; Gómez-Chiguano, G.F.; Cleland, J.A.; Arias-Buría, J.L.; Fernández-De-Las-Peñas, C.; Plaza-Manzano, G. Effects of Trigger Point Dry Needling for Nontraumatic Shoulder Pain of Musculoskeletal Origin: A Systematic Review and Meta-Analysis. Phys. Ther. 2021, 101, pzaa216. [Google Scholar] [CrossRef]
- Liu, L.; Huang, Q.M.; Liu, Q.G.; Ye, G.; Bo, C.Z.; Chen, M.J.; Li, P. Effectiveness of Dry Needling for Myofascial Trigger Points Associated with Neck and Shoulder Pain: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2015, 96, 944–955. [Google Scholar] [CrossRef]
- Simons, D.G.; Travell, J.G.; Simons, L.S. Travel & Simons’ Myofascial Pain and Dysfunction: The Trigger Point Manual; Lippincott Williams & Wilkins: Baltimore, MD, USA, 1999; Volume 1, ISBN 0683083635. [Google Scholar]
- Alonso-Blanco, C.; Fernández-de-las-Peñas, C.; Fernández-Mayoralas, D.M.; de-la-Llave-Rincón, A.I.; Pareja, J.A.; Svensson, P. Prevalence and Anatomical Localization of Muscle Referred Pain from Active Trigger Points in Head and Neck Musculature in Adults and Children with Chronic Tension-Type Headache. Pain Med. 2011, 12, 1453–1463. [Google Scholar] [CrossRef] [PubMed]
- Jalilipanah, P.; Okhovatian, F.; Serri, R.A.; Bagban, A.A.; Zamani, S. The Effect of Dry Needling & Muscle Energy Technique Separately and in Combination in Patients Suffering Shoulder Impingement Syndrome and Active Trigger Points of Infraspinatus. J. Bodyw. Mov. Ther. 2021, 26, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Quintner, J.L.; Bove, G.M.; Cohen, M.L. A Critical Evaluation of the Trigger Point Phenomenon. Rheumatology 2015, 54, 392–399. [Google Scholar] [CrossRef]
- Farfaras, S.; Roshani, L.; Mulder, J.; Mitsios, N.; Hallström, E.K.; Kartus, J.T. Increased Levels of Inflammatory Markers in the Subscapularis Tendon and Joint Capsule in Patients with Subacromial Impingement. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 2228. [Google Scholar] [CrossRef] [PubMed]
- Shah, J.P.; Danoff, J.V.; Desai, M.J.; Parikh, S.; Nakamura, L.Y.; Phillips, T.M.; Gerber, L.H. Biochemicals Associated with Pain and Inflammation Are Elevated in Sites near to and Remote from Active Myofascial Trigger Points. Arch. Phys. Med. Rehabil. 2008, 89, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Gerwin, R.D.; Dommerholt, J.; Shah, J.P. An Expansion of Simons’ Integrated Hypothesis of Trigger Point Formation. Curr. Pain Headache Rep. 2004, 8, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Pieters, L.; Lewis, J.; Kuppens, K.; Jochems, J.; Bruijstens, T.; Joossens, L.; Struyf, F. An Update of Systematic Reviews Examining the Effectiveness of Conservative Physical Therapy Interventions for Subacromial Shoulder Pain. J. Orthop. Sports Phys. Ther. 2020, 50, 131–141. [Google Scholar] [CrossRef] [PubMed]
- Dong, W.; Goost, H.; Lin, X.B.; Burger, C.; Paul, C.; Wang, Z.L.; Zhang, T.Y.; Jiang, Z.C.; Welle, K.; Kabir, K. Treatments for Shoulder Impingement Syndrome: A PRISMA Systematic Review and Network Meta-Analysis. Medicine 2015, 94, e510. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Plaza-Manzano, G.; Sanchez-Infante, J.; Gómez-Chiguano, G.F.; Cleland, J.A.; Arias-Buría, J.L.; López-De-Uralde-Villanueva, I.; Navarro-Santana, M.J. Is Dry Needling Effective When Combined with Other Therapies for Myofascial Trigger Points Associated with Neck Pain Symptoms? A Systematic Review and Meta-Analysis. Pain Res. Manag. 2021, 2021, 8836427. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Plaza-Manzano, G.; Sanchez-Infante, J.; Gómez-Chiguano, G.F.; Cleland, J.A.; Arias-Buría, J.L.; Navarro-Santana, M.J. The Importance of the Local Twitch Response during Needling Interventions in Spinal Pain Associated with Myofascial Trigger Points: A Systematic Review and Meta-Analysis. Acupunct. Med. J. Br. Med. Acupunct. Soc. 2022, 40, 299–311. [Google Scholar] [CrossRef]
- Sánchez-Infante, J.; Navarro-Santana, M.J.; Bravo-Sánchez, A.; Jiménez-Diaz, F.; Abián-Vicén, J. Is Dry Needling Applied by Physical Therapists Effective for Pain in Musculoskeletal Conditions? A Systematic Review and Meta-Analysis. Phys. Ther. 2021, 101, pzab070. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Nijs, J. Trigger Point Dry Needling for the Treatment of Myofascial Pain Syndrome: Current Perspectives within a Pain Neuroscience Paradigm. J. Pain Res. 2019, 12, 1899–1911. [Google Scholar] [CrossRef]
- Blanco-Díaz, M.; Ruiz-redondo, R.; Escobio-Prieto, I.; de la Fuente-Costa, M.; Albornoz-Cabello, M.; Casaña, J. A Systematic Review of the Effectiveness of Dry Needling in Subacromial Syndrome. Biology 2022, 11, 243. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Chichester, UK, 2019; pp. 1–694. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Eriksen, M.B.; Frandsen, T.F. The Impact of Patient, Intervention, Comparison, Outcome (PICO) as a Search Strategy Tool on Literature Search Quality: A Systematic Review. J. Med. Libr. Assoc. 2018, 106, 420–431. [Google Scholar] [CrossRef]
- Alarcón, M.; Ojeda, R.; Huaricancha, I.; Hilario, K. Análisis Crítico de Ensayos Clínicos Aleatorizados: Riesgo de Sesgo. Rev. Estomatol. Herediana 2016, 25, 304. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in Meta-Analysis Detected by a Simple, Graphical Test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Meader, N.; King, K.; Llewellyn, A.; Norman, G.; Brown, J.; Rodgers, M.; Moe-Byrne, T.; Higgins, J.P.T.; Sowden, A.; Stewart, G. A Checklist Designed to Aid Consistency and Reproducibility of GRADE Assessments: Development and Pilot Validation. Syst. Rev. 2014, 3, 82. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-Analysis in Clinical Trials. Control Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Imani, M.; Abbasi, L.; Taghizadeh, S.; Amiri, M. Comparison of the Effect of Two Different Types of Dry-Needling Techniques on Subacromial Impingement Syndrome. J. Bodyw. Mov. Ther. 2021, 25, 35–40. [Google Scholar] [CrossRef]
- Arias-Buría, J.L.; Fernández-de-Las-Peñas, C.; Palacios-Ceña, M.; Koppenhaver, S.L.; Salom-Moreno, J. Exercises and Dry Needling for Subacromial Pain Syndrome: A Randomized Parallel-Group Trial. J. Pain 2017, 18, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Palomares, S.; Oliván-Blázquez, B.; Pérez-Palomares, A.; Gaspar-Calvo, E.; Pérez-Benito, M.; López-Lapeña, E.; de La Torre-Beldarraín, M.L.; Magallón-Botaya, R. Contribution of Dry Needling to Individualized Physical Therapy Treatment of Shoulder Pain: A Randomized Clinical Trial. J. Orthop. Sports Phys. Ther. 2017, 47, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Ekici, G.; Özcan, Ş.; Öztürk, B.; Öztürk, B.; Ekici, B. Effects of Deep Friction Massage and Dry Needling Therapy on Night Pain and Shoulder Internal Rotation in Subacromial Pain Syndrome: 1-Year Follow up of a Randomised Controlled Trial. Int. J. Ther. Rehabil. 2021, 28, 1–12. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. Introduction to Meta-Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2009; pp. 1–421. [Google Scholar] [CrossRef]
- Hong, C.Z. Lidocaine Injection versus Dry Needling to Myofascial Trigger Point. The Importance of the Local Twitch Response. Am. J. Phys. Med. Rehabil. 1994, 73, 256–263. [Google Scholar] [CrossRef]
- Savović, J.; Jones, H.E.; Altman, D.G.; Harris, R.J.; Jüni, P.; Pildal, J.; Als-Nielsen, B.; Balk, E.M.; Gluud, C.; Gluud, L.L.; et al. Influence of Reported Study Design Characteristics on Intervention Effect Estimates from Randomized, Controlled Trials. Ann. Intern. Med. 2012, 157, 429–438. [Google Scholar] [CrossRef]
- Braithwaite, F.A.; Walters, J.L.; Li, L.S.K.; Lorimer Moseley, G.; Williams, M.T.; McEvoy, M.P. Effectiveness and Adequacy of Blinding in the Moderation of Pain Outcomes: Systematic Review and Meta-Analyses of Dry Needling Trials. PeerJ 2018, 6, e5318. [Google Scholar] [CrossRef]
- Balshem, H.; Helfand, M.; Schünemann, H.J.; Oxman, A.D.; Kunz, R.; Brozek, J.; Vist, G.E.; Falck-Ytter, Y.; Meerpohl, J.; Norris, S.; et al. GRADE Guidelines: 3. Rating the Quality of Evidence. J. Clin. Epidemiol. 2011, 64, 401–406. [Google Scholar] [CrossRef]
- Hall, M.L.; Mackie, A.C.; Ribeiro, D.C. Effects of Dry Needling Trigger Point Therapy in the Shoulder Region on Patients with Upper Extremity Pain and Dysfunction: A Systematic Review with Meta-Analysis. Physiotherapy 2018, 104, 167–177. [Google Scholar] [CrossRef]
- Cagnie, B.; Dewitte, V.; Barbe, T.; Timmermans, F.; Delrue, N.; Meeus, M. Physiologic Effects of Dry Needling. Curr. Pain Headache Rep. 2013, 17, 348. [Google Scholar] [CrossRef]
- Bron, C.; Dommerholt, J.D. Etiology of Myofascial Trigger Points. Curr. Pain Headache Rep. 2012, 16, 439–444. [Google Scholar] [CrossRef]
- Srbely, J.Z.; Dickey, J.P.; Lee, D.; Lowerison, M. Dry Needle Stimulation of Myofascial Trigger Points Evokes Segmental Anti-Nociceptive Effects. J. Rehabil. Med. 2010, 42, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Slade, S.C.; Dionne, C.E.; Underwood, M.; Buchbinder, R. Consensus on Exercise Reporting Template (CERT): Explanation and Elaboration Statement. Br. J. Sports Med. 2016, 50, 1428–1437. [Google Scholar] [CrossRef]
- Arias-Buría, J.L.; Martín-Saborido, C.; Cleland, J.; Koppenhaver, S.L.; Plaza-Manzano, G.; Fernández-de-las-Peñas, C. Cost-Effectiveness Evaluation of the Inclusion of Dry Needling into an Exercise Program for Subacromial Pain Syndrome: Evidence from a Randomized Clinical Trial. Pain Med. 2018, 19, 2336–2347. [Google Scholar] [CrossRef] [PubMed]
- Murad, M.H.; Chu, H.; Lin, L.; Wang, Z. The Effect of Publication Bias Magnitude and Direction on the Certainty in Evidence. BMJ Evid. Based Med. 2018, 23, 84–86. [Google Scholar] [CrossRef] [Green Version]


| Intervention | Comparison | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dry Needling | Exercise Therapy | Control Group | ||||||||||
| Studies | Subjects | Age Mean | Shoulder Pain Duration | Protocol | Area | Duration | Protocol | Duration | Subjects | Age Mean | Shoulder Pain Duration | Protocol |
| Arias-Buría et al. [33] | EG: n = 25 (28% W) | 49.0 (5.0) | ≥4 months | TrP-Dry needling | Anterior and middle deltoid, supraspinatus, infraspinatus, teres minor and major, and subscapularis | Twice daily (five weeks) | Three sets of 12 repetitions. Concentric and eccentric exercises | 20 to 25 min | CG: n = 25 (24% W) | 48.0 (6.0) | Four months | Eccentric and concentric exercises |
| Imani et al. [32] | EG: n = 21 (71.4% W) | 44.4 (9.0) | Not reported | Hong’s dry needling technique | Infraspinatus muscle | Third, fifth, and seventh session of treatment | Not included | Not included | CG: n = 22 (59.1% W) | 41.9 (10.1) | Not reported | Analgesic electrotherapy |
| Ekici et al. [35] | EG: n = 29 (61.9% W) | 52.0 (9.0) | ≥3 months | Dry needling up to local twitch response | Infraspinatus, supraspinatus, subscapularis, the upper part of the trapezius and levator scapula muscles | Six treatments over a four-week period | Not included | Not included | CG: n = 31 (90% W) | 50.9 (7.9) | ≥3 months | Deep friction massage to analgesia |
| Jalilipanah et al. [13] | EG: n = 13 (77% W) | 35.6 (8.7) | Not reported | Dry needling up to local twitch response | Infraspinatus muscle | Three sessions in a one-week | Not included | Not included | CG: n = 13 (46% W) | 36.6 (7.9) | Not reported | Post-isometric relaxation |
| Pérez-Palomares et al. [34] | EG: n = 57 (70% W) | 52.7 (11.8) | Not reported | Dry needling up to local twitch response and physical therapy | Supraspinatus, infraspinatus, sub-scapularis (medial, lateral superior, and lateral inferior), teres minor, and deltoid (anterior, medial, and posterior) muscles | First, fourth, and seventh session (three sessions) | Exercise and passive mobilization | 30 min | CG: n = 63 (56% W) | 54.3 (11.5) | Not reported | Exercise, massage, and passive mobilization |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Para-García, G.; García-Muñoz, A.M.; López-Gil, J.F.; Ruiz-Cárdenas, J.D.; García-Guillén, A.I.; López-Román, F.J.; Pérez-Piñero, S.; Abellán-Ruiz, M.S.; Cánovas, F.; Victoria-Montesinos, D. Dry Needling Alone or in Combination with Exercise Therapy versus Other Interventions for Reducing Pain and Disability in Subacromial Pain Syndrome: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 10961. https://doi.org/10.3390/ijerph191710961
Para-García G, García-Muñoz AM, López-Gil JF, Ruiz-Cárdenas JD, García-Guillén AI, López-Román FJ, Pérez-Piñero S, Abellán-Ruiz MS, Cánovas F, Victoria-Montesinos D. Dry Needling Alone or in Combination with Exercise Therapy versus Other Interventions for Reducing Pain and Disability in Subacromial Pain Syndrome: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(17):10961. https://doi.org/10.3390/ijerph191710961
Chicago/Turabian StylePara-García, Gonzalo, Ana María García-Muñoz, José Francisco López-Gil, Juan Diego Ruiz-Cárdenas, Ana Isabel García-Guillén, Francisco Javier López-Román, Silvia Pérez-Piñero, María Salud Abellán-Ruiz, Fernando Cánovas, and Desirée Victoria-Montesinos. 2022. "Dry Needling Alone or in Combination with Exercise Therapy versus Other Interventions for Reducing Pain and Disability in Subacromial Pain Syndrome: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 17: 10961. https://doi.org/10.3390/ijerph191710961
APA StylePara-García, G., García-Muñoz, A. M., López-Gil, J. F., Ruiz-Cárdenas, J. D., García-Guillén, A. I., López-Román, F. J., Pérez-Piñero, S., Abellán-Ruiz, M. S., Cánovas, F., & Victoria-Montesinos, D. (2022). Dry Needling Alone or in Combination with Exercise Therapy versus Other Interventions for Reducing Pain and Disability in Subacromial Pain Syndrome: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(17), 10961. https://doi.org/10.3390/ijerph191710961










