Predictive Factors of Anxiety, Depression, and Health-Related Quality of Life in Community-Dwelling and Institutionalized Elderly during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Overview of Procedure
2.2. Participants
2.3. Measures
2.3.1. Sociodemographic Questionnaire
2.3.2. Short-Form Health Survey 36 (SF-36)
2.3.3. UCLA Loneliness Scale—Version 3 (UCLA)
2.3.4. Hospital Anxiety and Depression Scale (HADS)
2.3.5. Functional Assessment of Chronic Illness Therapy—Spiritual Well-Being (FACIT-Sp)
2.4. Statistical Analysis
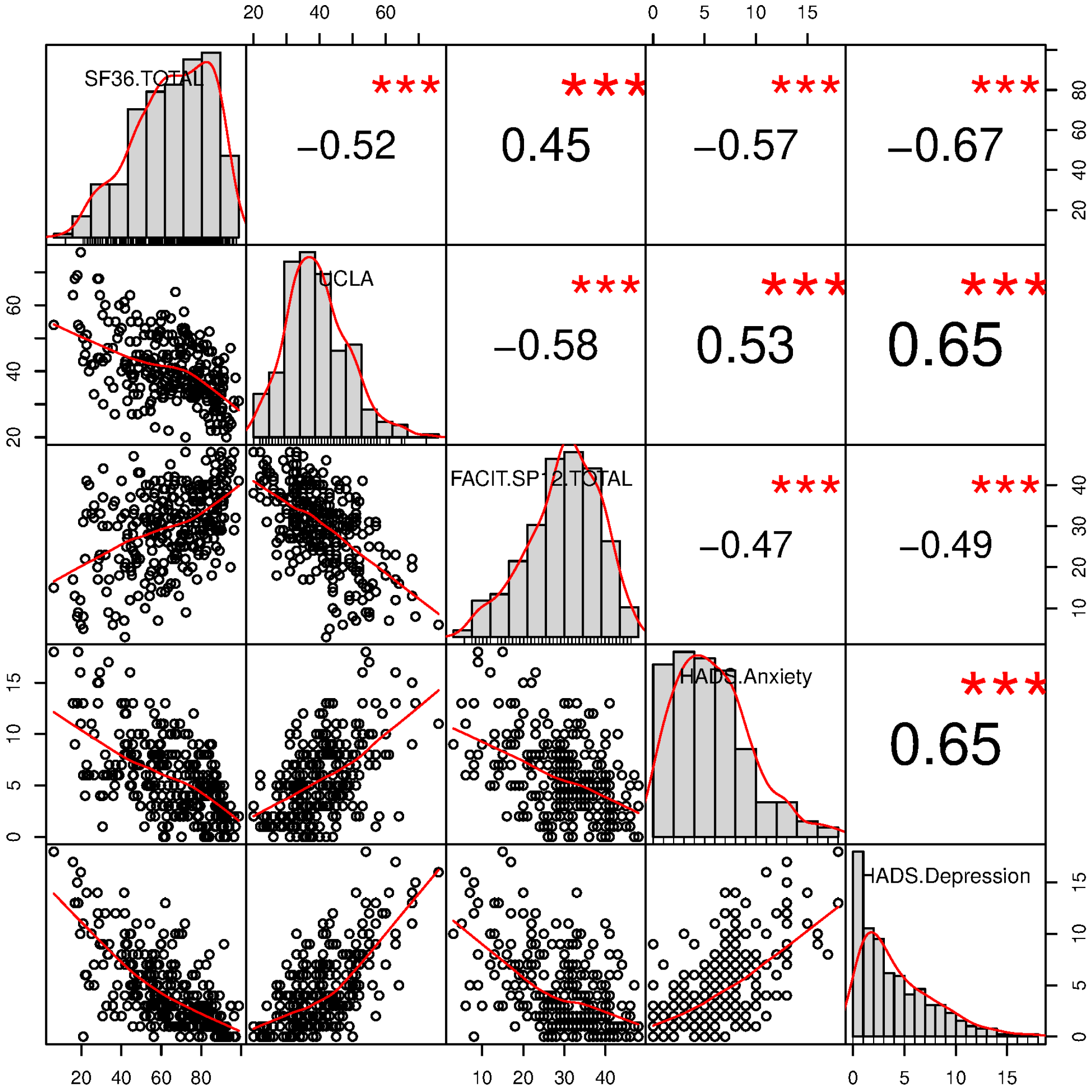
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mehra, A.; Rani, S.; Sahoo, S.; Parveen, S.; Singh, A.P.; Chakrabarti, S.; Grover, S. A crisis for elderly with mental disorders: Relapse of symptoms due to heightened anxiety due to COVID-19. Asian J. Psychiatr. 2020, 51, 102114. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.S.; Chee, C.Y.; Ho, R.C. Mental Health Strategies to Combat the Psychological Impact of Coronavirus Disease 2019 (COVID-19) Beyond Paranoia and Panic. Ann. Acad. Med. Singap. 2020, 49, 155–160. [Google Scholar] [CrossRef]
- World Health Organization. World Health Organization: Mental Health and Psychosocial Considerations During COVID-19 Outbreak. 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf (accessed on 1 June 2021).
- Cacioppo, J.T.; Cacioppo, S. Loneliness in the Modern Age: An Evolutionary Theory of Loneliness (ETL); Elsevier: New York, NY, USA, 2018. [Google Scholar]
- World Health Organization. Coronavirus. 2020. Available online: https://www.who.int/health-topics/coronavirus#tab=tab_1 (accessed on 15 September 2021).
- Manchia, M.; Gathier, A.W.; Yapici-Eser, H.; Schmidt, M.V.; de Quervain, D.; van Amelsvoort, T.; Bisson, J.I.; Cryan, J.F.; Howes, D.O.; Pinto, L.; et al. The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: A critical review across waves. Eur. Neuropsychopharmacol. 2022, 55, 22–83. [Google Scholar] [CrossRef] [PubMed]
- Verity, R.; Okell, L.C.; Dorigatti, I.; Winskill, P.; Whittaker, C.; Imai, N.; Cuomo-Dannenburg, G.; Thompson, H.; Walker, P.G.T.; Fu, H.; et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect. Dis. 2020, 20, 669–677. [Google Scholar] [CrossRef]
- Armitage, R.; Nellums, L.B. COVID-19 and the consequences of isolating the elderly. Lancet Public Health 2020, 5, e256. [Google Scholar] [CrossRef]
- Galea, S.; Merchant, R.M.; Lurie, N. The mental health consequences of COV_ID-19 and physical distancing: The need for prevention and early ıntervention. JAMA Intern. Med. 2020, 180, 817. [Google Scholar] [CrossRef]
- Steinman, M.A.; Perry, L.; Perissinotto, C.M. Meeting the care needs of older adults ısolated at home during the COVID-19 pandemic. JAMA Int. Med. 2020, 180, 89–820. [Google Scholar] [CrossRef]
- Fegert, J.M.; Vitiello, B.; Plener, P.L.; Clemens, V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health 2020, 14, 20. [Google Scholar] [CrossRef]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Matiz, A.; Fabbro, F.; Paschetto, A.; Urgesi, C.; Ciucci, E.; Baroncelli, A.; Crescentini, C. The impact of the COVID-19 pandemic on affect, fear, and personality of primary school children measured during the second wave of infections in 2020. Front. Psychiatry 2022, 12, 803270. [Google Scholar] [CrossRef]
- Crescentini, C.; Feruglio, S.; Matiz, A.; Paschetto, A.; Vidal, E.; Cogo, P.; Fabbro, F. Stuck Outside and Inside: An Exploratory Study on the Effects of the COVID-19 Outbreak on Italian Parents and Children’s Internalizing Symptoms. Front. Psychol. 2020, 11, 586074. [Google Scholar] [CrossRef] [PubMed]
- Eurofound. Impact of COVID-19 on Young People in the EU; Publications Office of the European Union: Luxembourg, 2021. [Google Scholar]
- Bassi, F.; Doria, M. Diffusion of COVID-19 among children and adolescents during the second and third waves of the pandemic in Italy. Eur. J. Pediatr. 2022, 181, 1619–1632. [Google Scholar] [CrossRef] [PubMed]
- Doraiswamy, S.; Mamtani, R.; Ameduri, M.; Abraham, A.; Cheema, S. Respiratory epidemics and older people. Age Ageing 2020, 49, 896–900. [Google Scholar] [CrossRef]
- Gerlach, L.; Solway, E.; Singer, D.; Kullgren, J.; Kirch, M.; Malani, P. Mental Health among Older Adults before and during the COVID-19 Pandemic. University of Michigan National Poll on Healthy Aging. May 2021. Available online: https://www.healthyagingpoll.org/reports-more/report/mental-health-among-older-adults-and-during-covid-19-pandemic (accessed on 1 October 2021).
- Delam, H.; Izanloo, S. Increased death anxiety in the elderly during coronavirus disease 2019 (COVID-19) pandemic. J. Health Sci. Surveill. Syst. 2020, 8, 173–174. [Google Scholar]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial 20 OMEGA—Journal of Death and Dying 0 stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Bala, R.; Maheshwari, S.K. Death anxiety and death depression among elderly. Int. J. Psychiatr. Nurs. 2018, 5, 55–59. [Google Scholar] [CrossRef]
- Khademi, F.; Moayedi, S.; Golitaleb, M.; Karbalaie, N. Letter to the edıtor. The COVID-19 pandemic and death anxiety in the elderly. Int. J. Ment. Health Nurs. 2021, 30, 346–349. [Google Scholar] [CrossRef]
- Meng, H.; Xu, Y.; Dai, J.; Zhang, Y.; Liu, B.; Yang, H. The psychological effect of COVID-19 on the elderly in China. Psychiatry Res. 2020, 289, 1–2. [Google Scholar]
- Vahia, I.V.; Jeste, D.V.; Reynolds, C.F. III. Older adults and the mental health effects of COVID-19. JAMA 2020, 324, 2253–2254. [Google Scholar] [CrossRef]
- Das, S.; Arun, P.; Rohilla, R.; Parashar, K.; Roy, A. Anxiety and depression in the elderly due to COVID-19 pandemic: A pilot study. Middle East Curr. Psychiatry 2021, 28, 67. [Google Scholar] [CrossRef]
- Carstensen, L.L.; Shavit, Y.Z.; Barnes, J.T. Age Advantages in Emotional Experience Persist Even Under Threat From the COVID-19 Pandemic. Psychol Sci. 2020, 31, 1374–1385. [Google Scholar] [CrossRef] [PubMed]
- Carbone, E.; Palumbo, R.; Sella, E.; Lenti, G.; Di Domenico, A.; Borella, E. Emotional, Psychological, and Cognitive Changes Throughout the COVID-19 Pandemic in Italy: Is There an Advantage of Being an Older Adult? Front. Aging Neurosci. 2021, 13, 712369. [Google Scholar] [CrossRef] [PubMed]
- Ceccato, I.; Palumbo, R.; Di Crosta, A.; La Malva, P.; Marchetti, D.; Maiella, R.; Verrocchio, M.C.; Marin, A.; Mammarella, N.; Palumbo, R.; et al. Age-related differences in the perception of COVID-19 emergency during the Italian outbreak. Aging Ment. Health 2020, 25, 1305–1313. [Google Scholar] [CrossRef] [PubMed]
- Young, N.A.; Waugh, C.E.; Minton, A.R.; Charles, S.T.; Haase, C.M.; Mikels, J.A. Reactive, agentic, apathetic, or challenged? Aging, emotion, and coping during the COVID-19 pandemic. Gerontologist 2021, 61, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Machielse, A. Theories on social contacts and social isolation. In Hortulanus R, Machielse A, Meeuwesen, L. Social Isolation in Modern Society; Routledge: New York, NY, USA, 2006; pp. 13–36. [Google Scholar]
- Pugh, S. The Social World of Older People: Understanding Loneliness and Social Isolation in Later Life (Growing Older); Victor, C., Scambler, S., Bond, J., Eds.; Open University Press/McGraw Hill Education: Berkshire, UK, 2009; Volume 100. [Google Scholar]
- Nicholson, N.R. A review of social isolation: An important but underassessed condition in older adults. J. Primary Prev. 2012, 33, 137–152. [Google Scholar] [CrossRef]
- Gray, K. A Conceptual Review of Loneliness Across the Adult Life Course (16+ Years); What Works Centre for Wellbeing: London, UK, 2019. [Google Scholar]
- Santini, Z.I.; Jose, P.E.; Cornwell, E.Y.; Koyanagi, A.; Nielsen, L.; Hinrichsen, C.; Meilstrup, C.; Madsen, K.R.; Koushede, V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health 2020, 5, e62–e70. [Google Scholar] [CrossRef]
- Das, A. Loneliness does (not) have cardiometabolic effects: A longitudinal study of older adults in two countries. Soc. Sci. Med. 2019, 223, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Ong, A.D.; Uchino, B.N.; Wethington, E. Loneliness and health in older adults: A mini-review and synthesis. Gerontology 2016, 62, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Evans, I.E.M.; Martyr, A.; Collins, R.; Brayne, C.; Clare, L. Social isolation and cognitive function in later life: A systematic review and meta-analysis. J. Alzheimers Dis. 2019, 70, S119-44. [Google Scholar] [CrossRef]
- Kuiper, J.S.; Zuidersma, M.; Oude Voshaar, R.C.; Zuidema, S.U.; van den Heuvel, E.R.; Stolk, R.P.; Smidt, N. Social relationships and risk of dementia: A systematic review and meta-analysis of longitudinal cohort studies. Ageing Res. Rev. 2015, 22, 39–57. [Google Scholar] [CrossRef]
- Lara, E.; Martín-María, N.; De la Torre-Luque, A.; Koyanagi, A.; Vancampfort, D.; Izquierdo, A.; Miret, M. Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Res. Rev. 2019, 52, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Leigh-Hunt, N.; Bagguley, D.; Bash, K.; Turner, V.; Turnbull, S.; Valtorta, N.; Caan, W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017, 152, 157–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dahlberg, L. Loneliness during the COVID-19 pandemic. Aging Ment. Health 2021. [CrossRef] [PubMed]
- UN. Policy Brief: The Impact of COVID-19 on Older Persons; United Nations: New York, NY, USA, 2020; Available online: https://unsdg.un.org/sites/default/files/2020-05/Policy-Brief-The-Impact-of-COVID-19-on-Older-Persons.pdf (accessed on 15 September 2021).
- Ayalon, L.; Chasteen, A.; Diehl, M.; Levy, B.R.; Neupert, S.D.; Rothermund, K.; Tesch-Romer, C.; Wahl, H.W. Aging in times of the COVID-19 pandemic: Avoiding ageism and fostering intergenerational solidarity. J. Gerontol. Ser. B 2021, 76, e49–e52. [Google Scholar] [CrossRef]
- Brooke, J.; Jackson, D. Older people and COVID-19: Isolation, risk and ageism. J. Clin. Nurs. 2020, 29, 2044–2046. [Google Scholar] [CrossRef]
- Pancani, L.; Marinucci, M.; Aureli, N.; Riva, P. Forced Social Isolation and Mental Health: A Study on 1006 Italians under COVID-19 Quarantine. 2020. Available online: https://psyarxiv.com/uacfj/download?format=pdf (accessed on 1 October 2021).
- Jopling, K. Promising Approaches Revisited: Effective Action on Loneliness in Later Life; Campaign to End Loneliness: London, UK, 2020; Available online: https://www.campaigntoendloneliness.org/wp-content/uploads/Promising_Approaches_Revisited_FULL_REPORT.pdf (accessed on 15 September 2021).
- World Health Organization. Global Report on Ageism; WHO: Geneva, Switzerland, 2021; Available online: https://apps.who.int/iris/rest/bitstreams/1336324/retrieve (accessed on 15 November 2021).
- Lu, C.; Chi, X.; Liang, K.; Chen, S.T.; Huang, L.; Guo, T.; Jiao, C.; Yu, Q.; Veronese, N.; Soares, F.C.; et al. Moving More and Sitting Less as Healthy Lifestyle Behaviors are Protective Factors for Insomnia, Depression, and Anxiety Among Adolescents During the COVID-19 Pandemic. Psychol. Res. Behav. Manag. 2020, 13, 1223–1233. [Google Scholar] [CrossRef]
- Fullana, M.A.; Hidalgo-Mazzei, D.; Vieta, E.; Radua, J. Coping behaviors associated with decreased anxiety and depressive symptoms during the COVID-19 pandemic and lockdown. J. Affect. Disord. 2020, 275, 80–81. [Google Scholar] [CrossRef]
- Ellul, M.A.; Benjamin, L.; Singh, B.; Lant, S.; Michael, B.D.; Easton, A.; Kneen, R.; Defres, S.; Sejvar, J.; Solomon, T. Neurological associations of COVID-19. Lancet Neurol. 2020, 19, 767–783. [Google Scholar] [CrossRef]
- Schuch, F.B.; Vancampfort, D.; Richards, J.; Rosenbaum, S.; Ward, P.B.; Stubbs, B. Exercise as a treatment for depression: A meta-analysis adjusting for publication bias. J. Psychiatr. Res. 2016, 77, 42–51. [Google Scholar] [CrossRef]
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The impact of physical activity on psychological health during COVID-19 pandemic in Italy. Heliyon 2020, 6, e04315. [Google Scholar] [CrossRef]
- Lange, K.W.; Nakamura, Y. Lifestyle factors in the prevention of COVID-19. Global Health J. 2020, 4, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Lange, K.W. Diet, Exercise, and Mental Disorders—Review Public Health Challenges of the Future; University of Regensburg, Institute of Psychology: Regensburg, Germany, 2018; Volume 2. [Google Scholar]
- Maunder, R.; Hunter, J.; Vincent, L.; Bennett, J.; Peladeau, N.; Leszcz, M.; Sadavoy, J.; Verhaeghe, L.M.; Steinberg, R.; Mazzulli, T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ 2003, 168, 1245–1251. [Google Scholar] [PubMed]
- Rogers, J.P.; Chesney, E.; Oliver, D.; Pollak, T.A.; McGuire, P.; Fusar-Poli, P.; Zandi, M.S.; Lewis, G.; David, A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 611–627. [Google Scholar] [CrossRef]
- Gencer, N. Ritualization as alternative approach to the spiritual dimension of palliative care: A concept analysis. J. Relig. Stud. 2019, 22, 489–502. [Google Scholar]
- Klavuz, M.A.; Klavuz, E. The ımportance of spiritual counseling services in coping with losses in the aging period. In Spiritual Counseling and Guidance; Koc, A.M., Tınaz, N., Eds.; Dem Publishing: Zagreb, Croatia, 2016; pp. 17–38. [Google Scholar]
- Harris, G.M.; Allen, R.S.; Dunn, L.; Parmelee, P. “Trouble won’t last always”: Religious coping and meaning in the stress process. Qual. Health Res. 2013, 23, 773–781. [Google Scholar] [CrossRef]
- Rote, S.; Hill, T.D.; Ellison, C.G. Religious attendance and loneliness in later life. Gerontologist 2013, 53, 39–50. [Google Scholar] [CrossRef]
- Pink, J.; Jacobson, L.; Pritchard, M. The 21st century GP: Physician and priest? Br. J. Gen. Pract. 2007, 57, 840–842. [Google Scholar]
- Koenig, H.G. Ways of protecting religious older adults from the consequences of COVID-19. Am. J. Geriatr. Psychiatry 2020, 28, 776–779. [Google Scholar] [CrossRef]
- Archbald-Pannone, L. COVID-19: 4 Tips to Help the Elderly Stay Connected. 2020. Available online: https://www.weforum.org/agenda/2020/03/seniors-elderly-coronavirus-isolation/ (accessed on 1 June 2021).
- Savci, C.; Cil Akinci, A.; Yildirim Usenmez, S.; Keles, F. The effects of fear of COVID-19, loneliness, and resilience on the quality of life in older adults living in a nursing home. Geriatr. Nurs. 2021, 42, 1422–1428. [Google Scholar] [CrossRef]
- Madden, A.; Leen, B. Evidence Summary: What is the Impact of the Coronavirus Pandemic on the Mental Health of Elderly Nursing Home Residents? Health Service Executive: Dublin, Ireland, 2020.
- Kaelen, S.; van den Boogaard, W.; Pellecchia, U.; Spiers, S.; De Cramer, C.; Demaegd, G.; Fouqueray, E.; Van den Bergh, R.; Goublomme, S.; Decroo, T.; et al. How to bring residents’ psychosocial well-being to the heart of the fight against COVID-19 in Belgian nursing homes-A qualitative study. PLoS ONE. 2021, 16, e0249098. [Google Scholar] [CrossRef]
- Williams, J.; Lyons, B.; Rowland, D. Unmet long-term care needs of elderly people in the community: A review of the literature. Home Health Care Serv. Q 1997, 16, 93–119. [Google Scholar] [CrossRef] [PubMed]
- Shrivastava, S.R.; Shrivastava, P.S.; Ramasamy, J. Healthcare of elderly: Determinants, needs and services. Int. J. Prev. Med. 2013, 4, 1224–1225. [Google Scholar] [PubMed]
- Feruglio, S.; Matiz, A.; Cogo, P.; Vidal, E.; Paschetto, A.; Fabbro, F.; Crescentini, C. Isolated and blocked adolescents: A study on the psychological effects of the COVID-19 outbreak. Minerva Psichiatr. 2022, 63. [Google Scholar] [CrossRef]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- McHorney, C.A.; Ware, J.E.; Raczek, A.E. The Mos 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med. Care 1993, 31, 247–263. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E. SF-36 Health Survey. Manual and Interpretation Guide; The Health Institute, New England Medical Center: Boston, MA, USA, 1993. [Google Scholar]
- Ware, J.E.; Gandek, B.; Kosinski, M.; Aaronson, N.K.; Apolone, G.; Brazier, J.E.; Bullinger, M.; Kaasa, S.; Leplege, A.; Prieto, L.; et al. The equivalence of SF-36 Summary Health scores estimated using standard and country-specific algorithms in 10 countries: Results from the IQOLA Project. J. Clin. Epidemiol. 1998, 51, 1171–1178. [Google Scholar] [CrossRef]
- Russell, D. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. J. Personal. Assess. 1996, 66, 20–40. [Google Scholar] [CrossRef]
- Russell, D.; Peplau, L.A.; Ferguson, M.L. Developing a measure of loneliness. J. Personal. Assess. 1978, 42, 290–294. [Google Scholar] [CrossRef]
- Russell, D.; Peplau, L.A.; Cutrona, C.E. The Revised UCLA Loneliness Scale: Concurrent and discriminate validity evidence. J. Personal. Soc. Psychol. 1980, 39, 472–480. [Google Scholar] [CrossRef]
- Cutrona, C.; Russell, D.; Rose, J. Social support and adaptation to stress by the elderly. Psychol. Aging 1986, 1, 47–54. [Google Scholar] [CrossRef]
- Shaver, P.R.; Brennan, K.A. Measures of depression and loneliness. In Measures of personality and social psychological attitudes; Robinson, J.P., Shaver, P.R., Wrightsman, L.S., Eds.; Academic Press: Cambridge, MA, USA, 1991; pp. 195–289. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the hospital anxiety and depression scale-an updated literature review. J. Psychosom. Res. 2002, 52, 69–78. [Google Scholar] [CrossRef]
- Drageset, J.; Eide, G.E.; Ranhoff, A.H. Anxiety and depression among nursing home residents without cognitive impairment. Scand. J. Caring Sci. 2013, 27, 872–881. [Google Scholar] [CrossRef]
- Annunziata, M.; Muzzatti, B.; Altoe, G. Defining hospital anxiety and depression scale (HADS) structure by confirmatory factor analysis: A contribution to validation for oncological settings. Ann. Oncol. 2011, 22, 2330–2333. [Google Scholar] [CrossRef]
- Iani, L.; Lauriola, M.; Costantini, M. A confirmatory bifactor analysis of the hospital anxiety and depression scale in an Italian community sample. Health Qual. Life Outcomes 2014, 12, 1. [Google Scholar] [CrossRef]
- Djukanovic, I.; Carlsson, J.; Årestedt, K. Is the Hospital Anxiety and Depression Scale (HADS) a valid measure in a general population 65-80 years old? A psychometric evaluation study. Health Qual. Life Outcomes 2017, 15, 193. [Google Scholar] [CrossRef]
- McClain, C.S.; Rosenfeld, B.; Breitbart, W. Effect of Spiritual Well-Being on End-of-Life Despair in Terminally-Ill Cancer Patients. Lancet 2003, 361, 1603–1607. [Google Scholar] [CrossRef]
- Monod, S.; Lécureux, E.; Rochat, E.; Spencer, B.; Seematter-Bagnoud, L.; Martin-Durussel, A.; Büla, C. Validity of the FACIT-Sp to Assess Spiritual Well-Being in Elderly Patients. Psychology 2015, 6, 1311–1322. [Google Scholar] [CrossRef]
- Adams, K.B.; Sanders, S.; Auth, E.A. Loneliness and depression in independent living retirement communities: Risk and resilience factors. Aging Ment. Health 2004, 8, 475–485. [Google Scholar] [CrossRef]
- Apolone, G.; Mosconi, P. The Italian SF-36 Health Survey: Translation, validation and norming. J. Clin. Epidemiol. 1998, 51, 1025–1036. [Google Scholar] [CrossRef]
- Gatti, A.; Gottschling, J.; Brugnera, A.; Adorni, R.; Zarbo, C.; Compare, A.; Segal, D.L. An investigation of the psychometric properties of the Geriatric Anxiety Scale (GAS) in an Italian sample of community-dwelling older adults. Aging Ment. Health 2018, 22, 1176–1184. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.M.; Hammerman-Rozenberg, A.; Stessman, J. Frequency of Leaving the House and Mortality from Age 70 to 95. J. Am. Geriatr. Soc. 2018, 66, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Cori, L.; Curzio, O.; Adorni, F.; Prinelli, F.; Noale, M.; Trevisan, C.; Fortunato, L.; Giacomelli, A.; Bianchi, F. Fear of COVID-19 for individuals and family members: Indications from the national cross-sectional study of the epicovid19 web-based survey. Int. J. Environ. Res. Public Health 2021, 18, 3248. [Google Scholar] [CrossRef]
- EUROSTAT 2020. Ageing Europe—Looking at the Lives of Older People in the EU—2020 Edition; Eurostat: Luxembourg, 2020. [Google Scholar]
- Routasalo, P.; Pitkala, K.H. Loneliness among older people. Rev. Clin. Gerontol. 2003, 13, 303–311. [Google Scholar] [CrossRef]
- Luanaigh, C.Ó.; Lawlor, B.A. Loneliness and the health of older people. Int. J. Geriatr. Psychiatry 2008, 23, 1213–1221. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, Z.; Jagger, C.; Chiu, C.T.; Ofstedal, M.B.; Rojo, F.; Saito, Y. Spirituality, religiosity, aging and health in global perspective: A review. SSM Popul. Health 2016, 2, 373–381. [Google Scholar] [CrossRef]
- Thauvoye, E.; Vanhooren, S.; Vandenhoeck, A.; Dezutter, J. Spirituality and well-being in old age: Exploring the dimensions of spirituality in relation to late-life functioning. J. Relig. Health 2018, 57, 2167–2181. [Google Scholar] [CrossRef]
- Van As, B.A.L.; Imbimbo, E.; Franceschi, A.; Menesini, E.; Nocentini, A. The longitudinal association between loneliness and depressive symptoms in the elderly: A systematic review. Int. Psychogeriatr. 2021, 34, 1–13. [Google Scholar] [CrossRef]
- Stolz, E.; Mayerl, H.; Freidl, W. The impact of COVID-19 restriction measures on loneliness among older adults in Austria. Eur. J. Public Health 2021, 31, 44–49. [Google Scholar] [CrossRef]
- Macdonald, B.; Hülür, G. Well-being and loneliness in Swiss older adults during the COVID-19 pandemic: The role of social relationships. Gerontologist 2021, 61, 240–250. [Google Scholar] [CrossRef]
- Krendl, A.C.; Perry, B.L. The impact of sheltering in place during the COVID-19 pandemic on older adults’ social and mental well-being. J. Gerontol. Series B 2021, 76, e53–e58. [Google Scholar] [CrossRef] [PubMed]
- Zaninotto, P.; Iob, E.; Demakakos, P.; Steptoe, A. Immediate and longer-term changes in the mental health and well-being of older adults in England during the COVID-19 pandemic. JAMA Psychiatry 2022, 79, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Choi, I.; Kim, J.H.; Kim, N.; Choi, E.; Choi, J.; Suk, H.W.; Na, J. How COVID-19 affected mental well-being: An 11-week trajectories of daily well-being of Koreans amidst COVID-19 by age, gender and region. PLoS ONE 2021, 16, e0250252. [Google Scholar]
- Bu, F.; Steptoe, A.; Fancourt, D. Loneliness during a strict lockdown: Trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Soc. Sci. Med. 2020, 265, 113521. [Google Scholar] [CrossRef] [PubMed]
- Bidzan-Bluma, I.; Bidzan, M.; Jurek, P.; Bidzan, L.; Knietzsch, J.; Stueck, M.; Bidzan, M. A Polish and German population study of quality of life, well-being, and life satisfaction in older adults during the COVID-19 pandemic. Front. Psychiatry 2020, 11, 585813. [Google Scholar] [CrossRef]
- Jiang, D. Perceived stress and daily well-being during the COVID-19 outbreak: The moderating role of age. Front. Psychol. 2020, 11, 571873. [Google Scholar] [CrossRef]
- O’Connor, R.C.; Wetherall, K.; Cleare, S.; McClelland, H.; Melson, A.J.; Niedzwiedz, C.L.; O’Carroll, R.E.; O’Connor, D.B.; Platt, S.; Scowcroft, E.; et al. Mental health and well-being during the COVID-19 pandemic: Longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry 2021, 218, 326–333. [Google Scholar]
- Carney, A.K.; Graf, A.S.; Hudson, G.; Wilson, E. Age moderates perceived COVID-19 disruption on well-being. Gerontologist 2021, 61, 30–35. [Google Scholar] [CrossRef]
- Gallagher, M.W.; Smith, L.J.; Richardson, A.L.; Long, L.J. Six month trajectories of COVID-19 experiences and associated stress, anxiety, depression, and impairment in American adults. Cogn. Ther. Res. 2022, 46, 457–469. [Google Scholar] [CrossRef]
- Robinson, E.; Sutin, A.R.; Daly, M.; Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022, 296, 567–576. [Google Scholar] [CrossRef]
- Palmas, G.; Moriondo, M.; Trapani, S.; Ricci, S.; Calistri, E.; Pisano, L.; Perferi, G.; Galli, L.; Venturini, E.; Indolfi, G.; et al. Nasal swab as preferred clinical specimen for COVID-19 testing in children. Pediatr. Infect. Dis. J. 2020, 39, e267–e270. [Google Scholar] [CrossRef] [PubMed]
- Daly, M.; Robinson, E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J. Psychiatr. Res. 2020, 136, 603–609. [Google Scholar] [CrossRef] [PubMed]
- Infurna, F.J.; Luthar, S.S. Re-evaluating the notion that resilience is commonplace: A review and distillation of directions for future research, practice, and policy. Clin. Psychol. Rev. 2018, 65, 43–56. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.; Daly, M. Explaining the rise and fall of psychological distress during the COVID-19 crisis in the United States: Longitudinal evidence from the Understanding America study. Br. J. Health Psychol. 2021, 26, 570–587. [Google Scholar] [CrossRef]
- Fancourt, D.; Steptoe, A.; Bu, F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. Lancet Psychiatry 2020, 8, 141–149. [Google Scholar] [CrossRef]
- Giebel, C.; Lord, K.; Cooper, C.; Shenton, J.; Cannon, J.; Pulford, D.; Shaw, L.; Gaughan, A.; Tetlow, H.; Gabbay, M.; et al. A UK survey of COVID-19 related social support closures and their effects on older people, people with dementia, and carers. Int. J. Geriatr. Psychiatry 2021, 36, 393–402. [Google Scholar] [CrossRef]
- Wolitzky-Taylor, K.B.; Castriotta, N.; Lenze, E.J.; Stanley, M.A.; Craske, M.G. Anxiety disorders in older adults: A comprehensive review. Depress. Anxiety 2010, 27, 190–211. [Google Scholar] [CrossRef]
- Hinz, A.; Brähler, E. Normative values for the hospital anxiety and depression scale (HADS) in the general German population. J. Psychosom. Res. 2011, 71, 74–78. [Google Scholar] [CrossRef]
- Girgus, J.S.; Yang, K.; Ferri, C.V. The gender difference in depression: Are elderly women at greater risk for depression than elderly men? Geriatrics 2017, 2, 35. [Google Scholar] [CrossRef]
- Pilania, M.; Yadav, V.; Bairwa, M.; Behera, P.; Gupta, S.D.; Khurana, H.; Mohan, V.; Baniya, G.; Poongothai, S. Prevalence of depression among the elderly (60 years and above) population in India, 1997–2016: A systematic review and meta-analysis. BMC Public Health 2019, 19, 1–18. [Google Scholar] [CrossRef]
- Levkovich, I.; Shinan-Altman, S.; Essar Schvartz, N.; Alperin, M. Depression and health-related quality of life among elderly patients during the COVID-19 pandemic in Israel: A cross-sectional study. J. Prim. Care Community Health 2021, 12, 2150132721995448. [Google Scholar] [CrossRef] [PubMed]
- Byers, A.L.; Vittinghoff, E.; Lui, L.Y.; Hoang, T.; Blazer, D.G.; Covinsky, K.E.; Ensrud, K.E.; Cauley, J.A.; Hillier, T.A.; Fredman, L.; et al. Twenty-year depressive trajectories among older women. Arch. Gen. Psychiatry 2012, 69, 1073–1079. [Google Scholar] [CrossRef] [PubMed]
- Sutin, A.R.; Terracciano, A.; Milaneschi, Y.; An, Y.; Ferrucci, L.; Zonderman, A.B. The trajectory of depressive symptoms across the adult life span. JAMA Psychiatry 2013, 70, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Borowiak, E.; Kostka, T. Predictors of quality of life in older people living at home and in institutions. Aging Clin. Exp. Res. 2004, 16, 212–220. [Google Scholar] [CrossRef]
- Salguero, A.; Martínez-García, R.; Molinero, O.; Márquez, S. Physical activity, quality of life and symptoms of depression in community-dwelling and institutionalized older adults. Arch. Gerontol. Geriatr. 2011, 53, 152–157. [Google Scholar] [CrossRef]
- Rodda, J.; Walker, Z.; Carter, J. Depression in older adults. BMJ 2011, 343, d5219. [Google Scholar] [CrossRef]
- Saraiva, M.D.; Apolinario, D.; Avelino-Silva, T.J.; de Assis Moura Tavares, C.; Gattás-Vernaglia, I.F.; Marques Fernandes, C.; Juliano, M. The impact of frailty on the relationship between life-space mobility and quality of life in older adults during the COVID-19 pandemic. J. Nutr. Health Aging 2021, 25, 440–447. [Google Scholar] [CrossRef]
- El Haj, M.; Altintas, E.; Chapelet, G.; Kapogiannis, D.; Gallouj, K. High depression and anxiety in people with Alzheimer’s disease living in retirement homes during the covid-19 crisis. Psychiatry Res. 2020, 291, 113294. [Google Scholar] [CrossRef]
| Variable | N | % |
|---|---|---|
| Sex | ||
| female | 163 | 57.8 |
| male | 119 | 42.2 |
| Age | ||
| 65–74 years | 171 | 60.6 |
| 75–89 years | 111 | 39.4 |
| Residence | ||
| in own home | 216 | 76.6 |
| in nursing home | 66 | 23.4 |
| Frequency of leaving home in the previous 2 weeks | ||
| never or sometimes | 140 | 49.6 |
| often or daily | 142 | 50.4 |
| Physical activity during the pandemic | ||
| interrupted or diminished | 108 | 38.3 |
| unchanged or increased | 174 | 61.7 |
| Recreational activities during the pandemic | ||
| interrupted or diminished | 45 | 16.0 |
| unchanged or increased | 237 | 84.0 |
| Meetings with family/friends during the pandemic | ||
| interrupted or diminished | 221 | 78.4 |
| unchanged or increased | 61 | 21.6 |
| Fear of COVID-19 | ||
| none or low | 79 | 28.0 |
| moderate or high | 203 | 72.0 |
| Variable Level | SF-36 | UCLA | FACIT-Sp | HADS Anxiety | HADS Depression | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||||
| female | 61.5 ± 20.3 | 41.4 ± 10.5 | 29.4 ± 10.1 | 6.3 ± 3.7 | 4.7 ± 3.7 | |||||
| male | 67.5 ± 20.5 | 39.7 ± 9.0 | 30.5 ± 9.1 | 5.3 ± 3.7 | 4.0 ± 3.6 | |||||
| Age | ||||||||||
| 65–74 years | 68.1 ± 19.7 | * | 39.5 ± 9.7 | 30.7 ± 9.3 | 5.9 ± 3.6 | 4.0 ± 3.5 | ||||
| 75–89 years | 57.7 ± 20.4 | 42.5 ± 9.9 | 28.6 ± 10.1 | 5.8 ± 4.0 | 4.9 ± 3.8 | |||||
| Residence | ||||||||||
| home-dwelling | 67.2 ± 19.7 | * | 39.6 ± 9.6 | * | 30.5 ± 8.9 | 5.8 ± 3.8 | 4.1 ± 3.6 | |||
| nursing home | 53.8 ± 20.2 | 44.2 ± 10.0 | 27.9 ± 11.7 | 6.0 ± 3.7 | 5.3 ± 3.7 | |||||
| Frequency of leaving home in the previous 2 weeks | ||||||||||
| never or sometimes | 55.9 ± 21.3 | * | 43.1 ± 10.7 | * | 28.1 ± 10.8 | * | 6.5 ± 4.0 | * | 5.2 ± 4.1 | * |
| often or daily | 72.1 ± 16.3 | 38.3 ± 8.4 | 31.7 ± 8.0 | 5.2 ± 3.3 | 3.5 ± 3.0 | |||||
| Physical activity during the pandemic | ||||||||||
| interrupted or diminished | 63.1 ± 19.0 | 41.5 ± 9.5 | 30.3 ± 8.9 | 6.5 ± 3.9 | 4.7 ± 3.6 | |||||
| unchanged or increased | 64.7 ± 21.5 | 40.2 ± 10.2 | 29.6 ± 10.2 | 5.4 ± 3.6 | 4.1 ± 3.6 | |||||
| Recreational activities during the pandemic | ||||||||||
| interrupted or diminished | 52.8 ± 21.9 | * | 44.8 ± 8.0 | * | 28.6 ± 8.5 | 7.2 ± 4.0 | 6.3 ± 4.2 | * | ||
| unchanged or increased | 66.2 ± 19.6 | 39.9 ± 10.0 | 30.1 ± 9.9 | 5.6 ± 3.6 | 4.0 ± 3.4 | |||||
| Meetings with family/friends during the pandemic | ||||||||||
| interrupted or diminished | 63.7 ± 20.5 | 40.5 ± 9.9 | 30.1 ± 9.4 | 6.1 ± 3.7 | 4.5 ± 3.7 | |||||
| unchanged or increased | 65.4 ± 21.0 | 41.2 ± 10.0 | 29.0 ± 10.6 | 4.9 ± 3.6 | 4.0 ± 3.4 | |||||
| Fear of COVID-19 | ||||||||||
| none or low | 66.0 ± 20.5 | 41.0 ± 10.9 | 29.8 ± 10.7 | 4.5 ± 3.5 | * | 3.7 ± 3.6 | ||||
| moderate or high | 63.3 ± 20.6 | 40.6 ± 9.5 | 29.9 ± 9.3 | 6.3 ± 3.7 | 4.6 ± 3.7 | |||||
| Questionnaire | Present Study M ± SD | Reference Study M ± SD |
|---|---|---|
| SF-36 | 64.0 ± 20.6 | 73.0 ± 7.7 [88] 48.5 ± 8.8 [89] |
| UCLA | 40.7 ± 9.9 | 38.6 ± 8.7 [87] |
| FACIT-SP12 | 29.9 ± 9.7 | 29.6 ± 7.8 [86] |
| HADS Anxiety | 5.8 ± 3.7 | 8.0 ± 4.5 [83] |
| HADS Depression | 4.4 ± 3.6 | 6.3 ± 4.1 [83] |
| HADS Anxiety Score | HADS Depression Score | SF-36 Total Score | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictor | B (SE) | β | p | B (SE) | β | p | B (SE) | β | p |
| Sex (0 = female, 1 = male) | −0.30 (0.33) | −0.04 | 0.374 | 0.09 (0.29) | 0.01 | 0.766 | 2.10 (1.70) | 0.05 | 0.216 |
| Age (0 = 65–74 years; 1 = 75–89 years) | −0.68 (0.37) | −0.09 | 0.066 | −0.20 (0.32) | −0.03 | 0.530 | −5.35 (1.84) | −0.13 | 0.004 ** |
| Residence (0 = home-dwelling; 1 = nursing home) | −0.55 (0.48) | −0.06 | 0.250 | −0.08 (0.42) | −0.01 | 0.856 | −3.51 (2.43) | −0.07 | 0.151 |
| Frequency of leaving home in the previous 2 weeks (0 = never or sometimes; 1 = often or daily) | 0.14 (0.39) | 0.02 | 0.728 | 0.35 (0.34) | 0.05 | 0.301 | 7.24 (1.94) | 0.18 | <0.001 *** |
| Physical activity during the pandemic (0 = interrupted or diminished; 1 = unchanged or increased) | −0.66 (0.35) | −0.09 | 0.058 | −0.20 (0.30) | −0.03 | 0.519 | −1.48 (1.77) | −0.04 | 0.401 |
| Recreational activities during the pandemic (0 = interrupted or diminished; 1 = unchanged or increased) | 0.14 (0.47) | 0.01 | 0.762 | −0.51 (0.41) | −0.05 | 0.222 | 2.95 (2.40) | 0.05 | 0.220 |
| Meetings with family/friends during the pandemic (0 = interrupted or diminished; 1 = unchanged or increased) | −0.91 (0.41) | −0.10 | 0.026 * | −0.28 (0.36) | −0.03 | 0.432 | −0.99 (2.09) | −0.02 | 0.638 |
| Fear of COVID-19 (0 = none or low; 1 = moderate or high) | 1.22 (0.39) | 0.15 | 0.002 ** | 0.56 (0.34) | 0.07 | 0.103 | −2.13 (2.01) | −0.05 | 0.290 |
| SF-36 Total score | −0.07 (0.01) | −0.39 | <0.001 *** | −0.08 (0.01) | −0.45 | <0.001 *** | − | − | − |
| UCLA score | 0.09 (0.02) | 0.25 | <0.001 *** | 0.14 (0.02) | 0.38 | <0.001 *** | −0.01 (0.12) | −0.00 | 0.949 |
| FACIT-Sp score | −0.07 (0.02) | −0.18 | 0.001 ** | −0.03 (0.02) | −0.08 | 0.088 | 0.18 (0.11) | 0.08 | 0.108 |
| HADS Anxiety score | − | − | − | − | − | − | −1.24 (0.31) | −0.23 | <0.001 *** |
| HADS Depression score | − | − | − | − | − | − | −2.24 (0.34) | −0.40 | <0.001 *** |
| R2 = 0.500 | R2 = 0.598 | R2 = 0.577 | |||||||
| adjusted R2 = 0.479 | adjusted R2 = 0.582 | adjusted R2 = 0.559 | |||||||
| p < 0.001 *** | p < 0.001 *** | p < 0.001 *** | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pascut, S.; Feruglio, S.; Crescentini, C.; Matiz, A. Predictive Factors of Anxiety, Depression, and Health-Related Quality of Life in Community-Dwelling and Institutionalized Elderly during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 10913. https://doi.org/10.3390/ijerph191710913
Pascut S, Feruglio S, Crescentini C, Matiz A. Predictive Factors of Anxiety, Depression, and Health-Related Quality of Life in Community-Dwelling and Institutionalized Elderly during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2022; 19(17):10913. https://doi.org/10.3390/ijerph191710913
Chicago/Turabian StylePascut, Stefania, Susanna Feruglio, Cristiano Crescentini, and Alessio Matiz. 2022. "Predictive Factors of Anxiety, Depression, and Health-Related Quality of Life in Community-Dwelling and Institutionalized Elderly during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 19, no. 17: 10913. https://doi.org/10.3390/ijerph191710913
APA StylePascut, S., Feruglio, S., Crescentini, C., & Matiz, A. (2022). Predictive Factors of Anxiety, Depression, and Health-Related Quality of Life in Community-Dwelling and Institutionalized Elderly during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 19(17), 10913. https://doi.org/10.3390/ijerph191710913









