Abstract
Financial incentives offered to those who quit smoking have been found effective, also in persons with low socioeconomic status (SES), but no previous study has investigated who benefits most: smokers with low or high SES. In this community-randomized trial (“Richer without smoking”), three Danish municipalities were randomized to reward persons who were abstinent when attending the municipal smoking cessation program (FIMs) and three municipalities were randomized to spend the same amount on smoking cessation campaigns recruiting smokers to the smoking cessation program (CAMs). The municipalities each received approximately USD 16,000. An intention-to-treat approach was used in analyses. In regression analyses adjusted for individual- and municipal-level differences, we found that smokers with high SES living in FIMs had significantly higher proportion of validated long-term successful quitters (OR (95% CI): 2.59 (1.6–4.2)) than high-SES smokers living in CAM. Smokers with low SES, however, did not experience the same benefit of financial incentives as smokers with high SES. Neither the FIMs nor the CAMs succeeded in attracting more smokers with low SES during the intervention year 2018 than the year before. Our study showed that smokers with low SES did not experience the same benefit of financial incentives as smokers with high SES.
1. Introduction
Even though smoking prevalence has decreased significantly in many countries, population growth has led to an increase in the total number of smokers worldwide, with tobacco smoking causing almost eight million deaths—including one in five deaths in males worldwide [1].
Article 14 of the WHO Framework Convention on Tobacco Control recommends that all countries provide evidence-based support for smoking cessation, such as behavioral support and smoking cessation pharmacotherapy. However, quit rates are often low and, therefore, new ways to help smokers quit are still sought-after.
Incentives, such as money, might have a strong psychological and motivational power. Experiments have shown that interpersonal rejection and physical pain caused desire for money to increase, while handling money, compared with handling paper, reduced distress over social exclusion and diminished the physical pain of immersion in hot water [2]. A Cochrane review from 2019, based on 33 randomized controlled trials (RCTs), performed in many countries across the world, presented a conclusion of high-certainty evidence that successful quitting in the long term is improved by financial incentives [3].
Our research group tested the use of financial incentives for smoking cessation in a community-randomized trial, “Richer without smoking”, taking part in six Danish municipalities in 2018 [4]. This study showed no difference between financial incentives and professional campaigns regarding recruitment of smokers to a smoking cessation program, but financial incentives had significantly greater effect in terms of helping smokers remain smokefree for a year.
Financial incentives have been found effective in many settings (e.g., primary care, college, rural village) and in many different populations (e.g., persons with mental health problems, cancer patients, pregnant women) [3]. However, no previous study has, to the best of our knowledge, investigated who benefits most from financial incentives: smokers with low or those with high socioeconomic status (SES).
It is well documented that there is a strong social gradient in smoking. The poorer and/or less educated a person is and the more mental health or abuse problems a person has, the higher the prevalence of smoking [5,6,7]. Studies have suggested that the high smoking prevalence may be a result of low tobacco health risk awareness, widespread smoking among family and friends, low social support for quitting, stronger addiction to tobacco, lower likelihood of using pharmacotherapy or completing smoking cessation courses, psychological differences such as lack of self-efficacy, and tobacco industry marketing [7,8]. As a result of this, poor, low-educated persons carry the heaviest burden of smoking [9]. Evidence of interventions that work among lower socioeconomic groups is sparse.
All smokers in Denmark have access to smoking cessation interventions in the local community without referral and free of charge. A national smoking cessation gold standard program was developed and is shown to be highly effective [10], even for disadvantaged smokers [11]. The smoking cessation gold standard program offers repeated counselling, including recommended smoking cessation pharmacotherapy by specially trained counsellors.
The “Richer without smoking” study was performed in a general population, in municipalities offering the smoking cessation gold standard program. Already, from the conceptualization phase of the study, we hypothesized that smokers with low SES would benefit more from financial incentives than smokers with high SES, as the reward would be perceived as being higher among those with low SES and would therefore be more appreciated and more motivating. We have information on length of education and employment status which opens the possibility to explore the effect of financial incentives across SES.
The aim of this paper was to investigate if smokers with low SES included in the “Richer without smoking” study [4] in municipalities who offered financial incentives (FIMs) achieved higher levels of abstinence compared to smokers with low SES in municipalities who used the resources on smoking cessation campaigns (CAMs). The same was investigated for smokers with high SES. Further, we wanted to investigate if FIMs were able to attract more smokers with low SES in their smoking cessation program compared with CAMs.
2. Materials and Methods
In this community-randomized trial (Figure 1) called “Rigere uden røg” (Richer without smoking), we randomized six Danish municipalities to be either financial incentives municipalities (FIMs) (three municipalities) or campaign municipalities (CAMs) (three municipalities). To reflect a real-world implementation, the influence of the researchers was kept at a minimum throughout the trial.
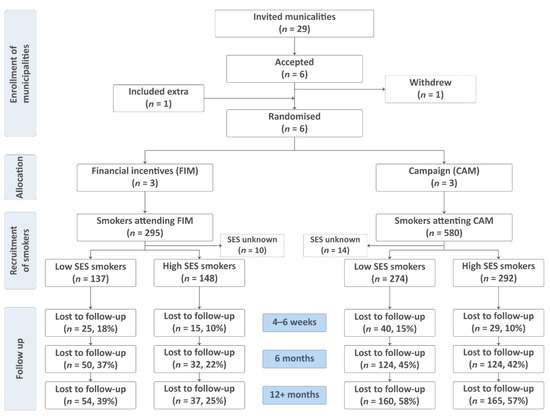
Figure 1.
Flowchart of the allocation of municipalities and recruitment and follow-up status of smokers included in the community-randomized trial “Richer without smoking”, Denmark.
Inclusion of the intervention municipalities: The principal investigator invited all 29 municipalities in the Capital Region of Denmark to take part in the research project, and six agreed (Figure 1). The local ethics committee decided that there was no need for approval (Journal-nr.: 18024988). The Danish Data Protection Agency also decided that approval was not needed, as the national Smoking Cessation Database [12] (registered and analyzed data) and the national quit line (performed follow-up on long-term abstinence) already had existing data processor agreements. The ClinicalTrials.Gov ID is NCT03849092. Investigating the outcomes across socioeconomic groups was the original plan of the study. No personal data were available to the researchers at any time during the study.
For details, please see Pisinger et al. (“Are financial incentives more effective than health campaigns to quit smoking? A community-randomized smoking cessation trial in Denmark”) [4].
2.1. Participants
In this trial we employed no eligibility criteria as the participants were included through already implemented smoking cessation programs in existing smoking cessation services. All smokers enrolling in a municipal smoking cessation gold standard program were included, but the smoking cessation counsellors aimed to enlist as many low-SES smokers as possible (based on short education and/or unemployment).
2.2. Randomization and Blinding
Given the nature of the trial, blinding of neither the researchers nor the statistician was possible. However, the statistician was the only one with access to the data. For details, please see [4].
2.3. Interventions in the Randomized Trial
2.3.1. Intervention in Financial Incentives Municipalities (FIMs)
The purpose of the three FIMs was to reward smokers for being smokefree when they attended the smoking cessation gold standard program. To do so, each FIM received DKK 100,000 (approximately USD 16,000). Each ex-smoker could receive a maximum of DKK 1200 (approximately USD 190), given as up to four vouchers for a local shopping mall (with a grocery store). Vouchers worth DKK 200 (approximately USD 32) were issued to ex-smokers at the third, fourth, and fifth session. Being smokefree at the last session (abstinence for a total of 4–6 weeks) triggered a final voucher worth DKK 600 (approximately USD 95) (see Appendix A for a graphical presentation of the intervention). Smokers who did not know about the financial incentives when they signed up for the smoking cessation group also received incentives when being abstinent. Abstinence from smoking was confirmed by carbon monoxide levels < 10 ppm [13], measured by the smoking cessation counsellor. The FIMs did not receive any money for recruitment of smokers. The municipalities had different recruitment methods before the study started, and little money ear-marked for recruitment. All advertised for their smoking cessation services on their website and most of them had some collaboration with pharmacies and/or general practitioners. We gave very simple examples of how/where they might recruit but no assistance to recruit smokers. The smoking cessation counsellors advertised on their website, informed general practitioners and pharmacies about the project, and provided them with flyers. Further, they hung up homemade photocopied A4/A3 posters, e.g., in vocational schools or in residential areas with many persons with low SES. The intervention was fully delivered in one in three municipalities only. In one municipality, one of the two smoking cessation counsellors was on sick leave for half of the intervention year. In another municipality, all smoking cessation activities were stopped after approximately eight months due to a local political decision. For details, please see [4].
2.3.2. Intervention in Campaign Municipalities (CAMs)
The purpose of the three CAMs was to run campaigns to attract and encourage smokers with low socioeconomic status to sign up for a municipal smoking cessation gold standard program. To do so, each CAM received DKK 100,000. Several advertising agencies were contacted by the CAMs, and, finally, they chose an agency offering a combination of postcards, big and small posters, and online and social media solutions. The campaign material included photos, e.g., of a dog begging to be taken outside or an elderly couple hugging, and each had a short humorous rhyme. Photos, e.g., of a young car mechanic or ordinary elderly people, that hopefully would arouse recognition and appeal to persons with low SES were chosen. The material incorporated the fact that smokers could increase their chances of becoming smokefree on the order of five times (based on Danish data) when participating in a smoking cessation gold standard program compared to trying themselves. Smokers could send a text to 1231 to be contacted by a smoking cessation counsellor. Banners and posters were placed on buses, at bus stops, at main roads, near malls, etc. Postcards/leaflets were placed in public buildings and selected workplaces, as well as being distributed in deprived areas via private mailboxes. Digital marketing was surfaced, e.g., in buses, on main roads, and on Facebook. Smokers attending a smoking cessation gold standard program in a campaign municipality (CAM) were not rewarded financially for abstinence.
2.4. Outcome
The intervention took place throughout 2018. Outcomes were registered in the intervention year (2018), as well as in 2017. The primary outcome regarding recruitment was the number of smokers attending a smoking cessation gold standard program. Successful quitting was measured multiple times. In this paper, we present (1) “Carbon-monoxide-validated continuous abstinence after 4–6 weeks” (at the last smoking cessation gold standard program session), (2) “Self-reported 6-months continuous abstinence (not smoking at all after the quit date)”, and (3) “Carbon-monoxide-validated 12+-months point prevalence (smokefree for at least the last 14 days) in the randomized trial. Six- and 12+-months information was obtained by the national quit line. Participants who reported to be smokefree after 12+-months were contacted by a local smoking cessation counsellor to arrange for a carbon monoxide measurement to verify the abstinence.
2.5. Statistics
Results were reported as percentages and absolute numbers, and the χ2 test was used to compare baseline characteristics.
The variable socioeconomic status was defined by education and employment status. Low SES was defined as having no education except school for up to 12 years, or short work-related courses only or as being unemployed (and receiving welfare benefits while being of working age; “housewives” and students were not included in this group) [11].
In the recruitment analyses, the numeric change in number of participants between 2017 and 2018 was calculated for each municipality. The differences were then tested using a linear regression model, adjusted for free/subsidized nicotine replacement therapy ((NRT); not given to all smokers by all municipalities) and number of smokers in 2017, as these diverged significantly across the municipalities.
Successful quitting was presented as raw abstinence rates (proportion of successful quitters at follow-up) stratified by random allocation and SES. In the main analyses of successful quitting, we used the intention-to-treat (ITT) approach assuming all non-respondents to be smokers. Odds ratios (ORs) and 95% confidence intervals (95% CI) were estimated by running a mixed-effect logistic regression analysis using the municipality as the first-level cluster (random effect), while all other predictors were modeled as fixed effects.
Initially, analyses were performed to test for interaction between random allocation and SES, and the following analyses were stratified by random allocation and SES.
First, the univariate analyses were conducted, followed by the fitting of the multivariable model, including predictors based on the initial results and factors known from the literature to be associated with the outcome. Furthermore, we included municipality-level factors, taking the difference between municipalities into account. The fully adjusted model included sex (male/female), age (15–24, 25–34, 35–44, 45–54, 55–66, 67+ (retirement age)), Fagerström Test for Nicotine Dependence [14] (low: 0–6 points/high: 7–10 points), number of cigarettes smoked per day, and the quit rate in 2017. Finally, the proportion of smokers who received free/subsidized nicotine replacement treatment (NRT) was included. All variables were entered together and listwise deletion was employed, excluding smokers with missing values from the analyses. Sensitivity analyses using smokers with valid follow-up only (complete case approach) were performed, using the same adjusted model.
3. Results
3.1. Attrition and Loss to Follow-Up
In 2018, a total of 295 smokers attended the smoking cessation gold standard program in the financial incentives municipalities (FIMs), and 580 in the campaign municipalities (CAMs). The distribution of smokers with low and high SES was the same in both intervention groups (48% low SES and 52% high SES). Loss to follow-up was higher among smokers with low SES in both the FIMs and the CAMs at all timepoints. After 6 and 12+-months, the attrition was much higher in the CAM groups compared to the FIMs (Figure 1). Loss to follow-up did not differ statistically among the groups at the end of the smoking cessation gold standard program (p = 0.057), but after 6 and 12+-months there was a statistically significant difference between the four groups (p ≤ 0.001 at both timepoints).
3.2. Baseline Characteristics of Smokers
The majority of the participants were 45 to 66 years old, and approximately six in ten were women (Table 1). Roughly three in ten were highly addicted to nicotine, and about half of the smokers had low SES. There was no difference in the share of smokers with low SES between the FIMs and the CAMs. The median number of cigarettes per day was 20 across the groups, except for the high-SES group in the FIMs, where it was 16 cigarettes per day.

Table 1.
Baseline characteristics of smokers with high and low socioeconomic status (SES) included in the community-randomized trial “Richer without smoking”, Denmark.
3.3. Recruitment
Neither the financial incentives municipalities (FIMs) nor the campaign municipalities (CAMs) succeeded in attracting more smokers with low SES during 2018 compared with 2017 (p = 0.438 and 0.879, respectively) (Table 2). In the adjusted regression analyses, there was no statistically significant difference in recruitment of smokers with low SES between the FIMs and the CAMs during the intervention year (p = 0.147). Sensitivity analyses taking the reduced activity in two of three municipalities in the FIMs into account did not change the conclusion (p = 0.869).

Table 2.
Recruitment of smokers in the FIMs and CAMs in the year of intervention (2018) and the year before (2017). Data are presented according to socioeconomic status (SES).
3.4. Abstinence
Regarding the crude abstinence rates, the highest proportion of successful quitters were seen among participants with high SES in the FIMs, both at the end of the smoking cessation gold standard program, after 6 months, and after 12+-months (Figure 2). In both the FIMs and the CAMs, persons with low SES achieved lower abstinence rates than person with high SES. Abstinence rates among the persons with low SES in the FIMs, however, were almost the same as among persons with high SES in the CAMs.
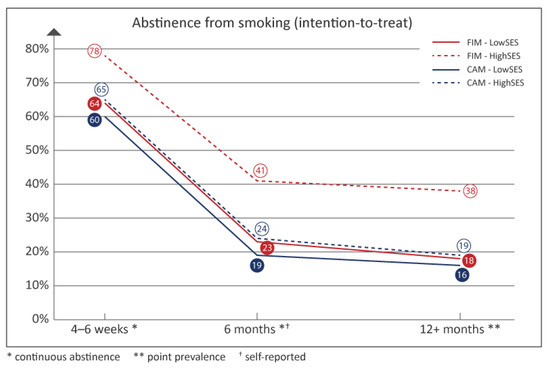
Figure 2.
Abstinence rates from smoking in the “Richer without smoking” study, based on the intention-to-treat principle; Denmark, 2018. Validated abstinence rates at the end of the intervention (4–6 weeks), after 12+-months, and self-reported abstinence rates after 6 months. FIM: financial incentive municipality, CAM: campaign municipality, SES: socioeconomic status.
Successful quitting based on a complete case approach can be seen in Appendix B. The highest crude abstinence rates were seen among participants with high SES in the FIMs.
3.5. Adjusted ITT Analyses
Statistically significant interactions were found between the intervention groups (FIMs/CAMs) and SES (high/low) after 6 and 12+-months (p = 0.003 and p = 0.038, respectively). This interaction was not seen at the end of the smoking cessation intervention (p = 0.514).
Based on these interactions, the following regression analyses were stratified according to SES (Table 3).

Table 3.
Unadjusted and adjusted logistic regression analysis of the effect (successful quitting) in the financial incentives municipalities (FIMs) compared with the campaign municipalities (CAMs) at the end of the intervention, and after 6 and 12+-months. The results are based on the intention-to-treat principle and stratified by socioeconomic status (SES). OR: odds ratio, CI: confidence interval.
3.6. Complete Case Analyses (Appendix C)
Adjusted and unadjusted analyses resulted in essentially similar results. Additionally, we did not observe any noticeable differences between self-reported continuous abstinence after 6 months and validated successful quitting after 12+-months in either the crude or the fully adjusted analyses.
4. Discussion
In this large community-randomized trial, we have previously shown that smokers living in municipalities offering financial incentives to those who quit when attending a municipal smoking cessation program achieved significantly higher long-term abstinence rates than smokers living in municipalities using professional campaigns but not offering financial incentives. In this paper, we show that smokers with high SES living in municipalities offering financial incentives achieved significantly higher long-term abstinence rates than smokers with high SES living in municipalities not offering financial incentives. However, it seems that smokers with low SES did not experience the same benefit of financial incentives as smokers with high SES. Furthermore, neither the financial incentives municipalities (FIMs) nor the campaign municipalities (CAMs) succeeded in attracting more smokers with low SES during the intervention year than the year before.
Despite no difference in intention to quit or number of quit attempts, people with low SES are significantly less successful in their quit attempts than those with higher SES [15]. Some of the reasons for this are strong tobacco addiction, less use of smoking cessation pharmacotherapy, quitting of treatment, early drop-out from smoking cessation programs, reduced social support for quitting and low self-efficacy [7,16,17,18]. Few studies have tested which interventions are effective among smokers with low SES [19] and it is crucial that we search new ways to help those with low SES who want to quit.
In 2019, a Cochrane review identified 33 randomized controlled trials (RCTs) investigating the effect of financial incentives [3]. Since then, several other RCTs have confirmed that incentives are an efficient, cheap, and safe method to improve quit rates [4,20,21,22,23,24,25]. Results from several studies indicate that offering small financial incentives for smoking abstinence are also efficient in disadvantaged persons [26,27,28]. The Cochrane review suggested a favorable benefit of incentives for smoking cessation at longest follow-up in substance users. Although confidence intervals were wide due to small number of studies and participants, the point estimate was consistent with the overall meta-analysis [3]. The same was found in studies offering financial incentives to pregnant women who smoked [3]. It is well known that many women who continue smoking during pregnancy have a low SES. A recent RCT including female smokers who were 250% below the federal poverty level also found a beneficial effect of offering incentives [24]. Another study found that use of financial incentives to engage with tobacco quit line treatment is a cost-effective option to enhance smoking cessation rates for low-income smokers [29].
Therefore, we hypothesized that smokers with low SES would have a high benefit of financial incentives, even higher than smokers with high SES. Interviews (unpublished) with persons attending the smoking cessation gold standard program in the FIMs revealed that those with low income especially really appreciated the vouchers, when confirmed smokefree. Unadjusted analyses (Figure 2) showed quit rates comparable with persons with high SES in the CAMs not offering financial incentives. It was therefore surprising that the adjusted analyses could not confirm that smokers with low SES significantly benefited from financial incentives. One explanation could be that our study was under-powered due to the high drop-out rates. The adjusted OR for persons with low SES living in FIMs were higher at one-year follow-up than in low-SES persons in the CAMs, but not significantly higher. Another explanation could be that our definition of persons with low SES did not exclusively include those who were poor and therefore they did not experience the economic reward as very motivating. In Denmark, unemployed persons receive high financial support from the government for a long period of time, and persons with low education might be rich craftsmen or self-employed entrepreneurs. Potentially, a retired person with high education might have a lower income, even though he/she is defined as having a high SES.
It is interesting that persons with high SES responded so strongly to financial incentives, even though they probably did not need them. We hypothesize that it might have given them a bit of a bad conscience that they received the voucher, even though they were not poor. This bad conscience might have been a motivating factor for resourceful persons to stay abstinent. The finding can be very useful for, e.g., private companies with many high-SES employees, as these probably would have a great benefit of being offered a financial incentive if they quit smoking.
Why do incentives work? Surprisingly, the amount of money seems to be of little importance. The Cochrane review found no significant difference in the effect of smoking cessation between trials paying smaller or larger amounts of rewards [3]. Some studies including smokers with low SES found that financial incentives were associated with a higher use of cessation medication [21,30]; in our study, many smokers were offered free/subsidized NRT by the six municipalities. Further, a couple of studies have investigated whether incentives increase self-efficacy. A large workplace study found that the effect of financial incentives on successful quitting was mediated by a higher self-efficacy [30], but another study found that self-efficacy did not mediate the relation between the incentives and smoking cessation in the overall sample [31]. However, there was significant moderating effect of sex, with a stronger association between incentives and greater self-efficacy among females than males, which in turn influenced the likelihood of smoking cessation [31]. One study suggested that the perceived importance of earning abstinence-contingent incentives early in a quit attempt may indicate whether an individual will be responsive to the magnitude of incentives offered [32]. In conclusion, we do not fully know the exact mediators of the effect of incentives.
Even though we hypothesized a greater effect of the financial incentive intervention in low-SES smokers than in high-SES smokers, it is not a unique finding that smokers with low SES benefit less from smoking cessation interventions. A study found that, in general, smoking cessation interventions in Europe seem to have increased inequalities in smoking [33]. An exemption seems to be the United Kingdom’s National Health Service (NHS) stop smoking services. Efforts were made to advertise smoking cessation in disadvantaged communities and to train volunteers or community workers as advisers, an approach that was found to be an effective strategy in treating disadvantaged smokers [34]. In all areas there was “positive discrimination”, meaning that services were reaching a higher proportion of smokers living in the most disadvantaged areas compared with more affluent areas [35]. It was concluded that the smoking cessation service probably made a modest contribution to reducing inequalities in smoking prevalence [36]. Population-level tobacco control interventions might have the potential to benefit more disadvantaged groups and thereby contribute to reducing health inequalities [37], and high tobacco taxes seem to particularly benefit lower socioeconomic groups [38].
Our study indicates that using financial incentives in the general population might, as other smoking cessation interventions, widen the socioeconomic inequality in smoking. This finding needs to be confirmed by other studies investigating the differential impact of financial incentives across socioeconomic groups. If they confirm our finding, one could argue that financial incentives are offered primarily to smokers with low SES to avoid a widening of socioeconomic inequalities in smoking. Several high-quality interventions, mentioned above, have shown that financial incentives do benefit smokers with low SES. On the other hand, denying smokers with high SES an effective treatment might be seen as discrimination. Financial incentives are not only an evidence-based and highly effective smoking cessation method, but the strategy also seems to be highly cost-effective (a good investment) [39,40,41,42]. Therefore, one could argue that it should be offered to as many smokers as possible. Evidence on smoking cessation interventions that work among lower socioeconomic groups and do not widen the socioeconomic inequality in smoking is needed.
Our study also found that neither the FIMs nor the CAMs succeeded in attracting more smokers with low SES during the intervention year than the year before. Previous studies indicated that financial incentives can be a good recruitment method to smoking cessation activities [43,44], even for disadvantaged smokers [39]. Evidence on interventions that are successful in attracting smokers with low SES to smoking cessation services is needed.
4.1. Strengths
It is a strength that this pragmatic RCT, in addition to testing the effect of the intervention, also tested the feasibility of implementing an offer of financial incentives to smokers on a municipal level. It is also a strength that we adjusted for several important confounders both at the municipal and at the individual level. Both intention-to-treat and sensitivity analyses using the complete case approach were performed, and abstinence was validated by carbon monoxide measurements at the end of the smoking cessation gold standard program and after 12+-months.
4.2. Weaknesses
It was a challenge to evaluate these community interventions in a real-life setting as it deviates from the framework of an RCT which has strict requirements for evaluation and is conducted within a more rigorously controlled clinical research environment [45]. The high attrition, especially after 12+-months, is considered the most important weakness. The definition of socioeconomic status has weaknesses. We had information on employment and education but not on economy. A person with low education who has had very good income but is unemployed or on sick leave for a shorter period of time would be categorized as having low SES. A person with, e.g., abuse, no education, very bad finances, and no employment during most of his/her life would end up in the same category. Additionally, it must be considered that the study was performed in a high-income country. The amount a participant could earn was relatively small in a Danish context, while the same amount would have a much greater relative value in a low-income country. Therefore, the results are not necessarily transferable to low-income countries. For further considerations on weaknesses in the design of the study, please see the previous paper [4].
5. Conclusions
In a large community-randomized trial, we found that smokers with high socioeconomic status (SES) living in municipalities offering financial incentives achieved significantly higher long-term abstinence rates than smokers with high SES living in municipalities not offering financial incentives but instead running campaigns to attract smokers to smoking cessation services. Consequently, smokers with low SES did not experience the same benefit of financial incentives as smokers with high SES. Furthermore, neither the financial incentive municipalities nor the campaign municipalities succeeded in attracting more smokers with low SES during the intervention year than the year before. Evidence on recruitment methods to smoking cessation services and on smoking cessation interventions that work among lower socioeconomic groups is needed.
Author Contributions
Conceptualization, C.P., C.G.T. and M.R.; methodology, C.P. and M.R.; software, M.R.; validation, M.R. and C.P.; formal analysis, C.P. and M.R.; investigation, C.P. and C.G.T.; resources, C.P.; data curation, M.R.; writing—original draft preparation, C.P. and M.R.; writing—review and editing, C.P., M.R. and C.G.T.; visualization, C.P. and M.R.; project administration, C.P.; funding acquisition, C.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Tryg Foundation (Trygfonden), Denmark (an independent charity that funds research and development related to health and social issues; grant 119404). Furthermore, the Danish Heart Foundation funded C.P.’s professorship during work on this paper. The Parker Institute, Bispebjerg and Frederiksberg Hospital is supported by a core grant from the Oak Foundation (an independent charity that funds research and development related to social issues; grant OCAY-18-774-OFIL).
Institutional Review Board Statement
Ethical review and approval were waived for this study as the study took part in established smoking cessation services, did not include testing of new pharmacotherapy, and did not expose the participants to any discomfort.
Informed Consent Statement
Patient consent was waived due to the reasons that the study took part in established smoking cessation services, did not include testing of new pharmacotherapy, and did not expose the participants to any discomfort.
Data Availability Statement
Data used in this study were obtained via an agreement with the national Danish Smoking Cessation Database. These data are not publicly available and therefore cannot be made available according to the regulations of the database.
Acknowledgments
We thank the smoking cessation counsellors in the intervention municipalities for their excellent work and commitment to the study.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Appendix A
Recommended meetings and quit date for the smoking cessation gold standard program, offered in both financial incentives municipalities (FIMs) and in campaign municipalities (CAMs), and the time and amount of rewards used in the FIMs only.
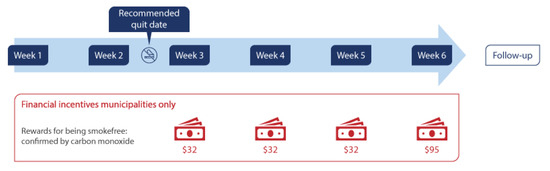
Figure A1.
A graphical presentation of the timing and frequency of the meetings in the gold standard smoking cessation intervention used in both the financial incentives municipalities (FIM) and the campaign municipalities (CAM), and of the timing and amount of the rewards used in the FIM only.
Appendix B
Crude proportions of successful quitters when based on complete cases only.
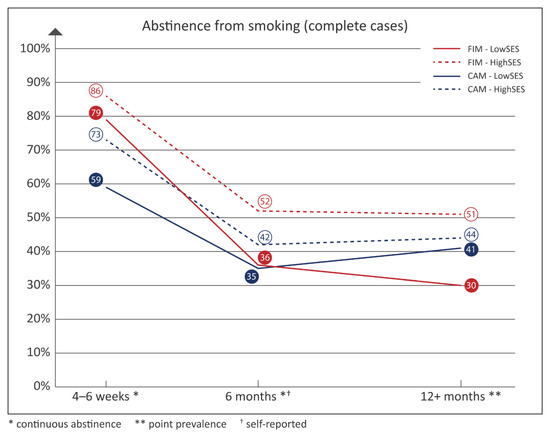
Figure A2.
Abstinence rates from smoking in the “Richer without smoking” study, based on a complete case approach; Denmark, 2018. Validated abstinence rates at the end of the intervention (4–6 weeks), after 12+-months, and self-reported abstinence rates after 6 months. FIM: financial in-centive municipality, CAM: campaign municipality, SES: socioeconomic status.
Appendix C
Unadjusted and adjusted logistic regression analysis of the effect of successful quitting in the financial incentives municipalities (FIMs) compared with the campaign municipalities (CAMs) at the end of the intervention, and after 6 and 12+-months. Results are based on complete case analyses and stratified by socioeconomic status (SES). OR: odds ratio, CI: confidence interval.

Table A1.
Unadjusted and adjusted logistic regression analysis of the effect (successful quitting) in the financial incentives municipalities (FIMs) compared with the campaign municipalities (CAMs) at the end of the intervention, and after 6 and 12+-months. The results are based on a complete case approach and stratified by socioeconomic status (SES). OR: odds ratio, CI: confidence interval.
Table A1.
Unadjusted and adjusted logistic regression analysis of the effect (successful quitting) in the financial incentives municipalities (FIMs) compared with the campaign municipalities (CAMs) at the end of the intervention, and after 6 and 12+-months. The results are based on a complete case approach and stratified by socioeconomic status (SES). OR: odds ratio, CI: confidence interval.
| Unadjusted Analyses | Adjusted Analyses | |||||||
|---|---|---|---|---|---|---|---|---|
| Intervention | OR | [CI 95%] | p | OR | [CI 95%] | p | ||
| Low SES | ||||||||
| CAMs | 1.00 | |||||||
| FIMs (4–6 weeks) | 2.55 | [1.51, 4.30] | ≤0.001 | * | 2.89 | [1.31, 6.38] | 0.009 | * |
| FIMs (6 months) | 1.01 | [0.58, 1.76] | 0.963 | 0.72 | [0.29, 1.81] | 0.490 | ||
| FIMs (12+-months) | 0.80 | [0.43, 1.48] | 0.475 | 0.74 | [0.37, 1.46] | 0.381 | ||
| High SES | ||||||||
| CAMs | 1.00 | |||||||
| FIMs (4–6 weeks) | 2.41 | [1.37, 4.24] | 0.002 | * | 2.74 | [1.28, 5.84] | 0.009 | * |
| FIMs (6 months) | 1.50 | [0.93, 2.41] | 0.095 | 1.64 | [0.90, 2.98] | 0.107 | ||
| FIMs (12+-months) | 1.43 | [0.85, 2.43] | 0.179 | 1.53 | [0.87, 2.68] | 0.136 | ||
Adjusted analyses included age, sex, Fagerström score, number of cigarettes smoked daily, abstinence in 2017, proportion of smokers receiving free/subsidized nicotine replacement therapy (NRT), and municipality. * Statistically significant.
References
- GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: A systematic analysis from the Global Burden of Disease Study 2019. Lancet 2021, 397, 2337–2360. [Google Scholar] [CrossRef]
- Zhou, X.; Vohs, K.D.; Baumeister, R.F. The symbolic power of money: Reminders of money alter social distress and physical pain. Psychol. Sci. 2009, 20, 700–706. [Google Scholar] [CrossRef] [PubMed]
- Notley, C.; Gentry, S.; Livingstone-Banks, J.; Bauld, L.; Perera, R.; Hartmann-Boyce, J. Incentives for smoking cessation. Cochrane Database Syst. Rev. 2019, 7, Cd004307. [Google Scholar] [CrossRef] [PubMed]
- Pisinger, C.; Toxværd, C.G.; Rasmussen, M. Are financial incentives more effective than health campaigns to quit smoking? A community-randomised smoking cessation trial in Denmark. Prev. Med. 2022, 154, 106865. [Google Scholar] [CrossRef]
- Prochaska, J.J.; Das, S.; Young-Wolff, K.C. Smoking, Mental Illness, and Public Health. Annu. Rev. Public Health 2017, 38, 165–185. [Google Scholar] [CrossRef]
- National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General; Centers for Disease Control and Prevention (US): Atlanta, GA, USA, 2014.
- Hiscock, R.; Bauld, L.; Amos, A.; Fidler, J.A.; Munafò, M. Socioeconomic status and smoking: A review. Ann. N. Y. Acad. Sci. 2012, 1248, 107–123. [Google Scholar] [CrossRef]
- Milcarz, M.; Polanska, K.; Bak-Romaniszyn, L.; Kaleta, D. Tobacco Health Risk Awareness among Socially Disadvantaged People-A Crucial Tool for Smoking Cessation. Int. J. Env. Res. Public Health 2018, 15, 2244. [Google Scholar] [CrossRef]
- Cockerham, W.C.; Hamby, B.W.; Oates, G.R. The Social Determinants of Chronic Disease. Am. J. Prev. Med. 2017, 52, S5–S12. [Google Scholar] [CrossRef]
- Rasmussen, M.; Fernández, E.; Tønnesen, H. Effectiveness of the Gold Standard Programme compared with other smoking cessation interventions in Denmark: A cohort study. BMJ Open 2017, 7, e013553. [Google Scholar] [CrossRef]
- Neumann, T.; Rasmussen, M.; Ghith, N.; Heitmann, B.L.; Tønnesen, H. The Gold Standard Programme: Smoking cessation interventions for disadvantaged smokers are effective in a real-life setting. Tob. Control 2013, 22, e9. [Google Scholar] [CrossRef] [Green Version]
- Rasmussen, M.; Tønnesen, H. The Danish smoking cessation database. Clin. Health Promot. 2016, 6, 36–41. [Google Scholar] [CrossRef]
- Goldstein, A.O.; Gans, S.P.; Ripley-Moffitt, C.; Kotsen, C.; Bars, M. Use of Expired Air Carbon Monoxide Testing in Clinical Tobacco Treatment Settings. Chest 2018, 153, 554–562. [Google Scholar] [CrossRef]
- Heatherton, T.F.; Kozlowski, L.T.; Frecker, R.C.; Fagerström, K.O. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. Br. J. Addict. 1991, 86, 1119–1127. [Google Scholar] [CrossRef]
- Kotz, D.; West, R. Explaining the social gradient in smoking cessation: It’s not in the trying, but in the succeeding. Tob. Control 2009, 18, 43–46. [Google Scholar] [CrossRef]
- Siahpush, M.; McNeill, A.; Borland, R.; Fong, G.T. Socioeconomic variations in nicotine dependence, self-efficacy, and intention to quit across four countries: Findings from the International Tobacco Control (ITC) Four Country Survey. Tob. Control 2006, 15 (Suppl. S3), iii71–iii75. [Google Scholar] [CrossRef] [PubMed]
- Boland, V.C.; Mattick, R.P.; McRobbie, H.; Siahpush, M.; Courtney, R.J. I’m not strong enough; I’m not good enough. I can’t do this, I’m failing—A qualitative study of low-socioeconomic status smokers’ experiences with accesssing cessation support and the role for alternative technology-based support. Int. J. Equity Health 2017, 16, 196. [Google Scholar] [CrossRef] [PubMed]
- Hiscock, R.; Judge, K.; Bauld, L. Social inequalities in quitting smoking: What factors mediate the relationship between socioeconomic position and smoking cessation? J. Public Health 2011, 33, 39–47. [Google Scholar] [CrossRef]
- Courtney, R.J.; Naicker, S.; Shakeshaft, A.; Clare, P.; Martire, K.A.; Mattick, R.P. Smoking Cessation among Low-Socioeconomic Status and Disadvantaged Population Groups: A Systematic Review of Research Output. Int. J. Environ. Res. Public Health 2015, 12, 6403–6422. [Google Scholar] [CrossRef]
- Berlin, I.; Berlin, N.; Malecot, M.; Breton, M.; Jusot, F.; Goldzahl, L. Financial incentives for smoking cessation in pregnancy: Multicentre randomised controlled trial. BMJ 2021, 375, e065217. [Google Scholar] [CrossRef]
- Ladapo, J.A.; Tseng, C.H.; Sherman, S.E. Financial Incentives for Smoking Cessation in Hospitalized Patients: A Randomized Clinical Trial. Am. J. Med. 2020, 133, 741–749. [Google Scholar] [CrossRef]
- White, J.S.; Lowenstein, C.; Srivirojana, N.; Jampaklay, A.; Dow, W.H. Incentive programmes for smoking cessation: Cluster randomized trial in workplaces in Thailand. BMJ 2020, 371, m3797. [Google Scholar] [CrossRef]
- Kurti, A.N.; Nighbor, T.D.; Tang, K.; Bolívar, H.A.; Evemy, C.G.; Skelly, J.; Higgins, S.T. Effect of Smartphone-Based Financial Incentives on Peripartum Smoking Among Pregnant Individuals: A Randomized Clinical Trial. JAMA Netw. Open 2022, 5, e2211889. [Google Scholar] [CrossRef]
- Parks, M.J.; Hughes, K.D.; Keller, P.A.; Lachter, R.B.; Kingsbury, J.H.; Nelson, C.L.; Slater, J.S. Financial incentives and proactive calling for reducing barriers to tobacco treatment among socioeconomically disadvantaged women: A factorial randomized trial. Prev. Med. 2019, 129, 105867. [Google Scholar] [CrossRef] [PubMed]
- Stotts, A.L.; Northrup, T.F.; Green, C.; Suchting, R.; Hovell, M.F.; Khan, A.; Villarreal, Y.R.; Schmitz, J.M.; Velasquez, M.M.; Hammond, S.K.; et al. Reducing Tobacco Smoke Exposure in High-Risk Infants: A Randomized, Controlled Trial. J. Pediatr. 2020, 218, 35–41.e1. [Google Scholar] [CrossRef] [PubMed]
- Businelle, M.S.; Kendzor, D.E.; Kesh, A.; Cuate, E.L.; Poonawalla, I.B.; Reitzel, L.R.; Okuyemi, K.S.; Wetter, D.W. Small financial incentives increase smoking cessation in homeless smokers: A pilot study. Addict. Behav. 2014, 39, 717–720. [Google Scholar] [CrossRef]
- Kendzor, D.E.; Businelle, M.S.; Poonawalla, I.B.; Cuate, E.L.; Kesh, A.; Rios, D.M.; Ma, P.; Balis, D.S. Financial incentives for abstinence among socioeconomically disadvantaged individuals in smoking cessation treatment. Am. J. Public Health 2015, 105, 1198–1205. [Google Scholar] [CrossRef] [PubMed]
- Fraser, D.L.; Fiore, M.C.; Kobinsky, K.; Adsit, R.; Smith, S.S.; Johnson, M.L.; Baker, T.B. A Randomized Trial of Incentives for Smoking Treatment in Medicaid Members. Am. J. Prev. Med. 2017, 53, 754–763. [Google Scholar] [CrossRef] [PubMed]
- Mundt, M.P.; Baker, T.B.; Fraser, D.L.; Smith, S.S.; Piper, M.E.; Fiore, M.C. Paying Low-Income Smokers to Quit? The Cost-Effectiveness of Incentivizing Tobacco Quit Line Engagement for Medicaid Recipients Who Smoke. Value Health 2019, 22, 177–184. [Google Scholar] [CrossRef]
- Van den Brand, F.A.; Candel, M.; Nagelhout, G.E.; Winkens, B.; van Schayck, C.P. How Financial Incentives Increase Smoking Cessation: A Two-Level Path Analysis. Nicotine Tob. Res. 2021, 23, 99–106. [Google Scholar] [CrossRef]
- Waters, A.F.; Businelle, M.S.; Frank, S.G.; Hébert, E.T.; Kendzor, D.E. Understanding the link between contingency management and smoking cessation: The roles of sex and self-efficacy. Addict. Behav. 2018, 84, 99–105. [Google Scholar] [CrossRef]
- Alexander, A.C.; Hébert, E.T.; Businelle, M.S.; Kendzor, D.E. Greater perceived importance of earning abstinence-contingent incentives is associated with smoking cessation among socioeconomically disadvantaged adults. Addict. Behav. 2019, 95, 202–205. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.; Platt, S.; Amos, A. Equity impact of European individual-level smoking cessation interventions to reduce smoking in adults: A systematic review. Eur. J. Public Health 2014, 24, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Judge, K.; Bauld, L.; Chesterman, J.; Ferguson, J. The English smoking treatment services: Short-term outcomes. Addiction 2005, 100 (Suppl. S2), 46–58. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, J.; Bauld, L.; Chesterman, J.; Judge, K. The English smoking treatment services: One-year outcomes. Addiction 2005, 100 (Suppl. S2), 59–69. [Google Scholar] [CrossRef] [PubMed]
- Bauld, L.; Judge, K.; Platt, S. Assessing the impact of smoking cessation services on reducing health inequalities in England: Observational study. Tob. Control 2007, 16, 400–404. [Google Scholar] [CrossRef]
- Thomas, S.; Fayter, D.; Misso, K.; Ogilvie, D.; Petticrew, M.; Sowden, A.; Whitehead, M.; Worthy, G. Population tobacco control interventions and their effects on social inequalities in smoking: Systematic review. Tob. Control 2008, 17, 230–237. [Google Scholar] [CrossRef]
- Hu, Y.; van Lenthe, F.J.; Platt, S.; Bosdriesz, J.R.; Lahelma, E.; Menvielle, G.; Regidor, E.; Santana, P.; de Gelder, R.; Mackenbach, J.P. The Impact of Tobacco Control Policies on Smoking Among Socioeconomic Groups in Nine European Countries, 1990–2007. Nicotine Tob. Res. 2017, 19, 1441–1449. [Google Scholar] [CrossRef] [PubMed]
- Mundt, M.P.; Baker, T.B.; Piper, M.E.; Smith, S.S.; Fraser, D.L.; Fiore, M.C. Financial incentives to Medicaid smokers for engaging tobacco quit line treatment: Maximising return on investment. Tob. Control 2020, 29, 320–325. [Google Scholar] [CrossRef]
- Boyd, K.A.; Briggs, A.H.; Bauld, L.; Sinclair, L.; Tappin, D. Are financial incentives cost-effective to support smoking cessation during pregnancy? Addiction 2016, 111, 360–370. [Google Scholar] [CrossRef]
- McCabe, C.; Claxton, K.; Culyer, A.J. The NICE cost-effectiveness threshold: What it is and what that means. Pharmacoeconomics 2008, 26, 733–744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tappin, D.; Bauld, L.; Purves, D.; Boyd, K.; Sinclair, L.; MacAskill, S.; McKell, J.; Friel, B.; McConnachie, A.; de Caestecker, L.; et al. Financial incentives for smoking cessation in pregnancy: Randomised controlled trial. BMJ 2015, 350, h134. [Google Scholar] [CrossRef] [PubMed]
- Halpern, S.D.; Harhay, M.O.; Saulsgiver, K.; Brophy, C.; Troxel, A.B.; Volpp, K.G. A Pragmatic Trial of E-Cigarettes, Incentives, and Drugs for Smoking Cessation. N. Engl. J. Med. 2018, 378, 2302–2310. [Google Scholar] [CrossRef] [PubMed]
- Weng, X.; Wu, Y.; Luk, T.T.; Li, W.H.C.; Cheung, D.Y.T.; Tong, H.S.C.; Lai, V.; Lam, T.H.; Wang, M.P. Active referral plus a small financial incentive upon cessation services use on smoking abstinence: A community-based, cluster-randomised controlled trial. Lancet Reg. Health West Pac. 2021, 13, 100189. [Google Scholar] [CrossRef]
- Moores, C.J.; Miller, J.; Perry, R.A.; Chan, L.L.H.; Daniels, L.A.; Vidgen, H.A.; Magarey, A.M. CONSORT to community: Translation of an RCT to a large-scale community intervention and learnings from evaluation of the upscaled program. BMC Public Health 2017, 17, 918. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).