A Systematic Review of Multiple Family Factors Associated with Oppositional Defiant Disorder
Abstract
1. Introduction
1.1. Oppositional Defiant Disorder
1.2. ODD and Maladaptive Family Environment
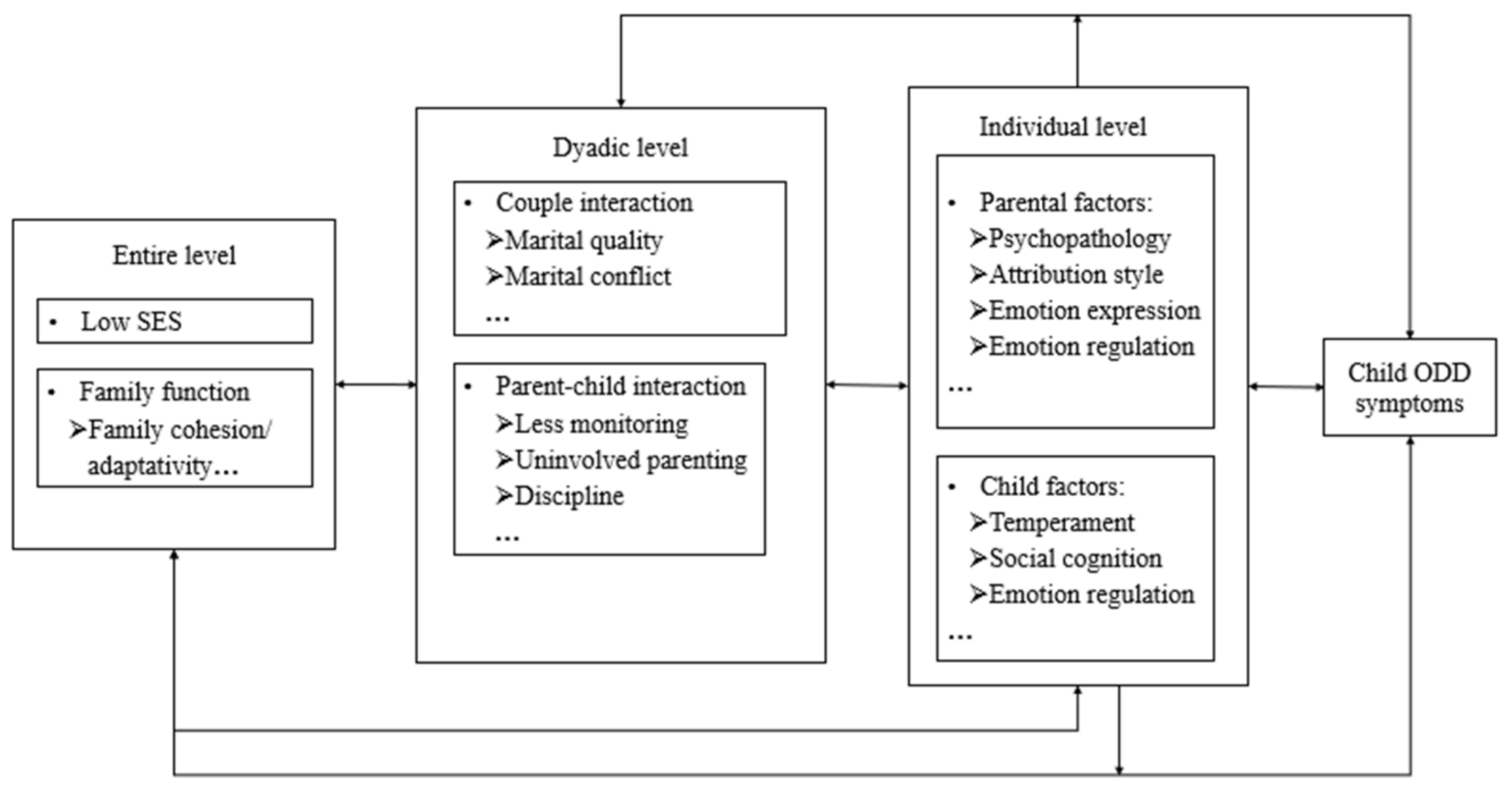
1.3. Multilevel Family Factors
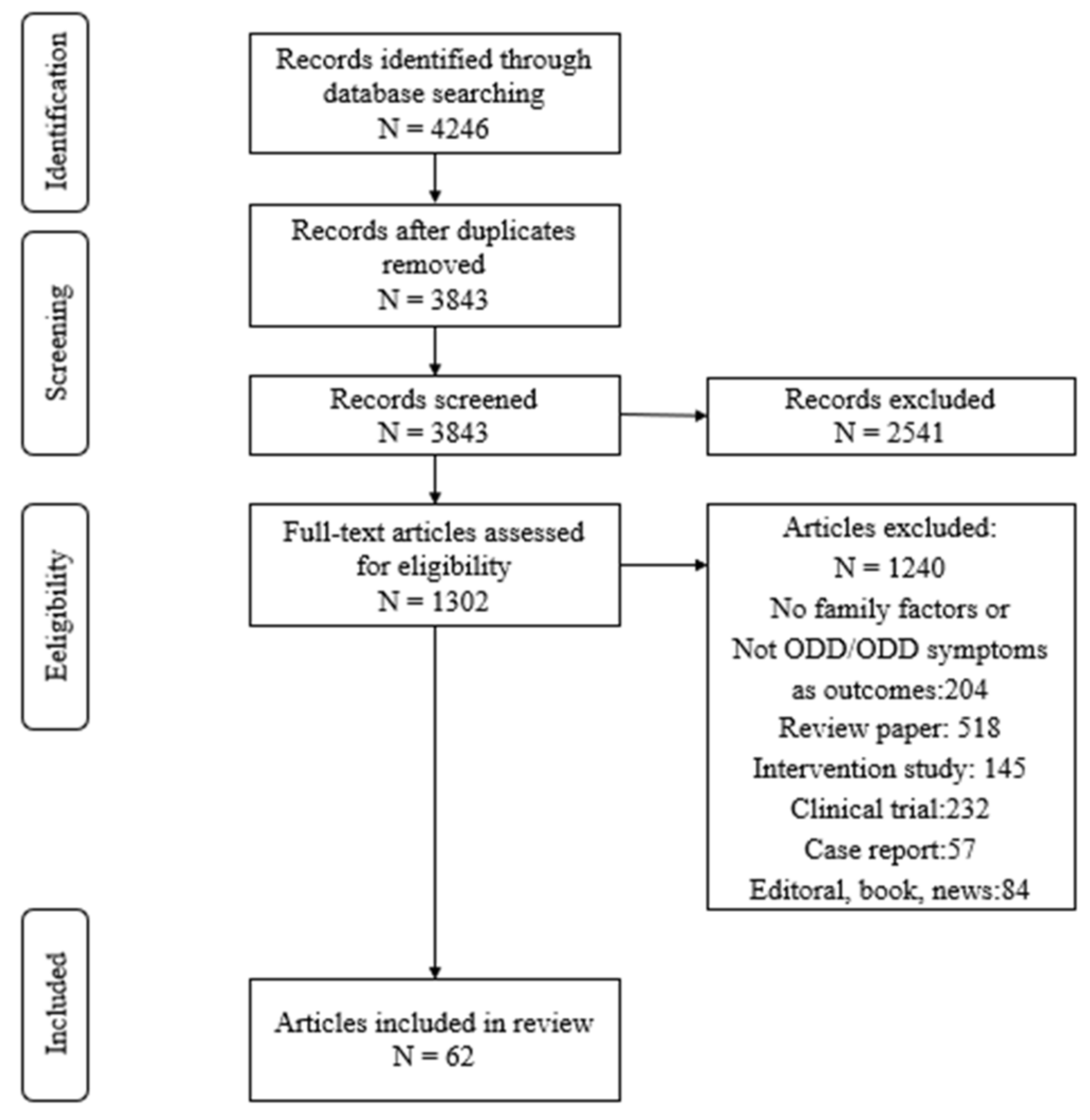
2. Method
2.1. Literature Search
2.2. Eligibility Criteria
3. Result
3.1. Family System Level
3.1.1. Socioeconomic Status
3.1.2. Family Function
3.2. Family Dyadic Level
3.2.1. Couple Interaction
3.2.2. Parent–Child Interaction
3.3. Family Individual Level
3.3.1. Parental Individual Level of Factors
3.3.2. Child Individual Level of Factors
3.4. Multi-Level Family Factors Interactions
3.4.1. Mediation/Moderation Effect between Family SES and Child ODD Symptoms
3.4.2. Mediation/Moderation Effect between Family Function and Child ODD Symptoms
3.4.3. Mediation/Moderation Effect between Couple Interaction and Child ODD Symptoms
3.4.4. Mediation/Moderation Effect between Parent–Child Interaction and Child ODD Symptoms
3.4.5. Three-Level Multiple Family Factors Framework
3.4.6. Future Prevention and Intervention Efforts
4. Discussion
Limitations and Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; APA: Arlington, VA, USA, 2013. [Google Scholar]
- Burke, J.; Loeber, R. Oppositional defiant disorder and the explanation of the comorbidity between behavioral disorders and depression. Clin. Psychol. Sci. Pract. 2010, 17, 319–326. [Google Scholar] [CrossRef]
- Greene, R.W.; Biederman, J.; Zerwas, S.; Monuteaux, M.C.; Goring, J.C.; Faraone, S.V. Psychiatric comorbidity, family dysfunction, and social impairment in referred youth with oppositional defiant disorder. Am. J. Psychiatry 2002, 159, 1214–1224. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Su, L.; Liu, Y. A study of current state and clinical characteristics of oppositional defiant disorder in a primary school and a middle school in Changsha, China. Chin. J. Psychiatry 2001, 4, 19–22. [Google Scholar]
- Burke, J.D.; Loeber, R.; Birmaher, B. Oppositional defiant disorder and conduct disorder: A review of the past 10 years, part II. J. Am. Acad. Child Adolesc. Psychiatry 2002, 41, 1275–1279. [Google Scholar] [CrossRef]
- Ding, W.; Meza, J.; Lin, X.; He, T.; Chen, H.; Wang, Y.; Qin, S. Oppositional defiant disorder symptoms and children’s feelings of happiness and depression: Mediating roles of interpersonal relationships. Child Indic. Res. 2020, 13, 215–235. [Google Scholar] [CrossRef]
- Li, L.; Lin, X.; Hinshaw, S.P.; Du, H.; Qin, S.; Fang, X. Longitudinal associations between oppositional defiant symptoms and interpersonal relationships among Chinese children. J. Abnorm. Child Psychol. 2018, 46, 1267–1281. [Google Scholar] [CrossRef]
- McKinney, C.; Renk, K. Emerging research and theory in the etiology of oppositional defiant disorder: Current concerns and future directions. Int. J. Behav. Consult. Ther. 2007, 3, 349–371. [Google Scholar] [CrossRef][Green Version]
- Lin, X.; Li, L.; Heath, M.A.; Chi, P.; Xu, S.; Fang, X. Multiple levels of family factors and oppositional defiant disorder symptoms among Chinese children. Fam. Process 2018, 57, 195–210. [Google Scholar] [CrossRef]
- Derella, O.J.; Burke, J.D.; Stepp, S.D.; Hipwell, A.E. Reciprocity in undesirable parent–child behavior? Verbal aggression, corporal punishment, and girls’ oppositional defiant symptoms. J. Clin. Child Adolesc. Psychol. 2019, 49, 420–433. [Google Scholar] [CrossRef]
- Polderman TJ, C.; Benyamin, B.; de Leeuw, C.A.; Sullivan, P.F.; van Bochoven, A.; Visscher, P.M.; Posthuma, D. Meta-analysis of the heritability of human traits based on fifty years of twin studies. Nat. Genet. 2015, 47, 702–709. [Google Scholar] [CrossRef]
- Noordermeer, S.D.S.; Luman, M.; Greven, C.U.; Veroude, K.; Faraone, S.V.; Hartman, C.A.; Hoekstra, P.J.; Franke, B.; Buitelaar, J.K.; Heslenfeld, D.J.; et al. Structural brain abnormalities of attention-deficit/hyperactivity disorder with oppositional defiant disorder. Biol. Psychiatry 2017, 82, 642–650. [Google Scholar] [CrossRef]
- Fanti, K.A.; Eisenbarth, H.; Goble, P.; Demetriou, C.; Kyranides, M.N.; Goodwin, D.; Zhang, J.; Bobak, B.; Cortese, S. Psychophysiological activity and reactivity in children and adolescents with conduct problems: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2019, 100, 98–107. [Google Scholar] [CrossRef]
- Lavigne, J.V.; Dahl, K.P.; Gouze, K.P.; LeBailly, A.A.; Hopkins, J. Multi-domain predictors of oppositional defiant disorder symptoms in preschool children: Cross-informant differences. Child Psychiatry Hum. Dev. 2015, 46, 308–319. [Google Scholar] [CrossRef]
- Lin, X.; Li, Y.; Xu, S.; Ding, W.; Qing, Z.; Du, H.; Chi, P. Family risk factors associated with oppositional defiant disorder symptoms, depressive symptoms, and aggressive behaviors among Chinese children with oppositional defiant disorder. Front. Psychol. 2019, 10, 2062. [Google Scholar] [CrossRef]
- Ghosh, A.; Ray, A.; Basu, A. Oppositional defiant disorder: Current insight. Psychol. Res. Behav. Manag. 2017, 10, 353–367. [Google Scholar] [CrossRef]
- Vose, J.J.C. Assessment of Family Functioning at Multiple Levels: An Exploratory Investigation of the Dynamic Assessment of Family Functioning Inventory–Demonstrated under Clinical Conditions (DAFFI-DUCC): How Despicable is the DAFFI-DUCC? Ph.D. Thesis, Alfred University, Alfred, NY, USA, 2010. [Google Scholar]
- Oliveira, S.C.; de Pavarini, S.C.I.; Orlandi, F.d.S.; Mendiondo, M.S.Z.d. Family functionality: A study of Brazilian institutionalized elderly individuals. Arch. Gerontol. Geriatr. 2014, 58, 170–176. [Google Scholar] [CrossRef]
- Lavigne, J.V.; Gouze, K.R.; Hopkins, J.; Bryant, F.B. A multidomain cascade model of early childhood risk factors associated with oppositional defiant disorder symptoms in a community sample of 6-year-olds. Dev. Psychopathol. 2016, 28, 1547–1562. [Google Scholar] [CrossRef]
- Ding, W.; Lin, X.; Su, J.; Jiang, Y.; Wu, Q.; He, T. The mutual influence between marital quality and child oppositional defiant disorder symptoms in Chinese families: Do child and parent’s gender matter? J. Child Fam. Stud. 2019, 28, 2086–2097. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMAP) 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef]
- Forssman, L.; Eninger, L.; Tillman, G.M.; Rodriguez, A.; Bohlin, G. Cognitive functioning and family risk factors in relation to symptom behaviors of ADHD and ODD in adolescents. J. Atten. Disord. 2010, 16, 284–294. [Google Scholar] [CrossRef]
- Harvey, E.A.; Metcalfe, L.A.; Herbert, S.D.; Fanton, J.H. The role of family experiences and ADHD in the early development of oppositional defiant disorder. J. Consult. Clin. Psychol. 2011, 79, 784–795. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.; Su, L.; Zhou, X. A correlation factors analysis in children with oppositional defiant disorder. Chin. J. Pract. Pediatrics 2007, 7, 12. [Google Scholar] [CrossRef]
- Rydell, A.M. Family factors and children’s disruptive behaviour: An investigation of links between demographic characteristics, negative life events and symptoms of ODD and ADHD. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 45, 233–244. [Google Scholar] [CrossRef]
- Boden, J.M.; Fergusson, D.M.; Horwood, L.J. Risk factors for conduct disorder and oppositional/defiant disorder: Evidence from a New Zealand birth cohort. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 1125–1133. [Google Scholar] [CrossRef]
- Evans, G.W. The environment of childhood poverty. Am. Psychol. 2004, 59, 77–92. [Google Scholar] [CrossRef]
- Lavigne, J.V.; Gouze, K.R.; Hopkins, G.J.; Bryant, F.B.; LeBailly, S.A. A multi-domain model of risk factors for ODD symptoms in a community sample of 4-year-olds. J. Abnorm. Child Psychol. 2012, 40, 741–757. [Google Scholar] [CrossRef]
- Conger, R.D.; Donnellan, M.B. An interactionist perspective on the socioeconomic context of human development. Annu. Rev. Psychol. 2007, 58, 175–199. [Google Scholar] [CrossRef]
- Rey, J.M.; Walter, G.; Plapp, J.M.; Denshire, E. Family environment in attention deficit hyperactivity, oppositional defiant and conduct disorders. Aust. N. Z. J. Psychiatry 2015, 34, 453–457. [Google Scholar] [CrossRef] [PubMed]
- Olson, D.H. Circumplex model of marital and family systems. J. Fam. Ther. 2000, 22, 144–167. [Google Scholar] [CrossRef]
- Crane, D.R.; Ngai, S.W.; Larson, J.H.; Hafen, M. The influence of family functioning and parent-adolescent acculturation on North American Chinese adolescent outcomes. Fam. Relat. 2005, 54, 400–410. [Google Scholar] [CrossRef]
- Lee, C. Theories of family adaptability: Toward a synthesis of Olson’s circumplex and the beavers systems models. Fam. Process 1988, 27, 73–85. [Google Scholar] [CrossRef]
- Chen, L.Y.; Luo, X.R.; Wei, Z.; Guan, B.Q. Parenting styles, parenting locus of control and family function of children with oppositional defiant disorder. Chin. J. Clin. Psychol. 2011, 19, 209–211. [Google Scholar]
- Miller, I.W.; Ryan, C.E.; Keitner, G.I.; Bishop, D.S.; Epstein, N.B. The McMaster approach to families: Theory, assessment, treatment and research. J. Fam. Ther. 2000, 22, 168–189. [Google Scholar] [CrossRef]
- Tang, Y.; Lin, X.; Chi, P.; Zhou, Q.; Hou, X. Multi-level family factors and affective and behavioral symptoms of oppositional defiant disorder in Chinese children. Front. Psychol. 2017, 8, 1123. [Google Scholar] [CrossRef]
- Cummings, E.M.; Davies, P.T. Depressed parents and family functioning: Interpersonal effects and children’s functioning and development. In The Interactional Nature of Depression; Joiner, T., Coyne, J.C., Eds.; American Psychological Association: Washington, DC, USA, 1999; pp. 299–327. [Google Scholar]
- Papp, L.M.; Goeke-Morey, M.C.; Cummings, E.M. Mothers’ and fathers’ psychological symptoms and marital functioning: Examination of direct and interactive links with child adjustment. J. Child Fam. Stud. 2004, 13, 469–482. [Google Scholar] [CrossRef]
- Krishnakumar, A.; Buehler, C. Interparental conflict and parenting behaviors: A meta-analytic review. Fam. Relat. 2000, 49, 25–44. [Google Scholar] [CrossRef]
- Bornovalova, M.A.; Cummings, J.R.; Hunt, E.; Blazei, R.; Malone, S.; Iacono, W.G. Understanding the relative contributions of direct environmental effects and passive genotype–environment correlations in the association between familial risk factors and child disruptive behavior disorders. Psychol. Med. 2014, 44, 831–844. [Google Scholar] [CrossRef]
- Wymbs, B.T.; Wymbs, F.A.; Dawson, A.E. Child ADHD and ODD behavior interacts with parent ADHD symptoms to worsen parenting and interparental communication. J. Abnorm. Child Psychol. 2015, 43, 107–119. [Google Scholar] [CrossRef]
- Chaudhury, P.; Bhattacharya, B.; Saha, P.K. Parent–child relationship and marital quality of parents of conduct or oppositional defiant disorder and unaffected individuals: A comparative study. Psychol. Stud. 2020, 65, 124–136. [Google Scholar] [CrossRef]
- Burnette, M.L. Gender and the development of oppositional defiant disorder: Contributions of physical abuse and early family environment. Child Maltreat. 2013, 18, 195–204. [Google Scholar] [CrossRef]
- Darling, N.; Steinberg, L. Parenting style as context: An integrative model. Psychol. Bull. 1993, 113, 487–496. [Google Scholar] [CrossRef]
- Alvarez, H.K.; Ollendick, T.H. Individual and psychosocial risk factors. In Conduct and Oppositional Defiant Disorders: Epidemiology, Risk Factors, and Treatment; Essau, C.A., Ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2003; pp. 97–116. [Google Scholar]
- Brown, C.A.; Granero, R.; Ezpeleta, L. The reciprocal influence of callous–unemotional traits, oppositional defiant disorder and parenting practices in preschoolers. Child Psychiatry Hum. Dev. 2017, 48, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Burke, J.D.; Pardini, D.A.; Loeber, R. Reciprocal relationships between parenting behavior and disruptive psychopathology from childhood through adolescence. J. Abnorm. Child Psychol. 2008, 36, 679–692. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, C.E.; Boyle, M.H. Preschoolers at risk for attention–deficit hyperactivity disorder and oppositional defiant disorder: Family, parenting, and behavioral correlates. J. Abnorm. Child Psychol. 2002, 30, 555–569. [Google Scholar] [CrossRef]
- Pederson, C.A.; Fite, P.J. The impact of parenting on the associations between child aggression subtypes and oppositional defiant disorder symptoms. Child Psychiatry Hum. Dev. 2014, 45, 728–735. [Google Scholar] [CrossRef]
- Stanger, C.; Dumenci, L.; Kamon, J.; Burstein, M. Parenting and children’s externalizing problems in substance-abusing families. J. Clin. Child Adolesc. Psychol. 2004, 33, 590–600. [Google Scholar] [CrossRef]
- Tung, I.; Lee, S.S. Negative parenting behavior and childhood oppositional defiant disorder: Differential moderation by positive and negative peer regard. Aggress. Behav. 2013, 40, 79–90. [Google Scholar] [CrossRef]
- Trepat, E.; Granero, R.; Ezpeleta, L. Parenting practices as mediating variables between parents’ psychopathology and oppositional defiant disorder in preschoolers. Psicothema 2014, 26, 497–504. [Google Scholar] [CrossRef]
- Li, Y.; Lin, X.; Hou, X.; Fang, X.; Liu, Y. The association of child maltreatment and migrant children’s oppositional defiant symptoms: The role of parent–child relationship. Psychol. Dev. Educ. 2016, 32, 214–225. [Google Scholar] [CrossRef]
- Liu, X.; Lin, X.; Zhou, Q.; Zhou, N.; Li, Y.; Lin, D. Family and individual risk and protective factors of depression among Chinese migrant children with oppositional defiant disorder symptoms. Front. Psychol. 2017, 8, 508. [Google Scholar] [CrossRef]
- Cruz–Alaniz, Y.; Martin, A.B.; Ballabriga, M.C.J. Parents’ executive functions, parenting styles, and oppositional defiant disorder symptoms: A relational model. Univ. Psychol. 2018, 17, 39–48. [Google Scholar] [CrossRef]
- Duncombe, M.E.; Havighurst, S.S.; Holland, K.A.; Frankling, E.J. The contribution of parenting practices and parent emotion factors in children at risk for disruptive behavior disorders. Child Psychiatry Hum. Dev. 2012, 43, 715–733. [Google Scholar] [CrossRef]
- Marmorstein, N.R.; Iacono, W.G.; McGue, M. Alcohol and illicit drug dependence among parents: Associations with offspring externalizing disorders. Psychol. Med. 2009, 1, 149–155. [Google Scholar] [CrossRef]
- Nordahl, H.M.; Ingul, J.M.; Nordvik, H.; Wells, A. Does maternal psychopathology discriminate between children with DSM-IV generalised anxiety disorder or oppositional defiant disorder? The predictive validity of maternal axis I and axis II psychopathology. Eur. Child Adolesc. Psychiatry 2007, 2, 87–95. [Google Scholar] [CrossRef]
- Liu, X.; Lin, X.; Xu, S.; Olson, S.L.; Li, Y.; Du, H. Depression among children with oppositional defiant disorder: Contributions of parent and child risk factors. J. Child Fam. Stud. 2017, 26, 3145–3155. [Google Scholar] [CrossRef]
- Antúnez, Z.; de la Osa, N.; Granero, R.; Ezpeleta, L. Parental psychopathology levels as a moderator of temperament and oppositional defiant disorder symptoms in preschoolers. J. Child Fam. Stud. 2016, 25, 3124–3135. [Google Scholar] [CrossRef]
- Rowe, R.; Maughan, B.; Pickles, A.; Costello, E.J.; Angold, A. The relationship between DSM-IV oppositional defiant disorder and conduct disorder: Findings from the great smoky mountains study. J. Child Psychol. Psychiatry 2010, 43, 365–373. [Google Scholar] [CrossRef]
- Weiner, B. Achievement Motivation and Attribution Theory; General Learning Press: Morristown, NJ, USA, 1974. [Google Scholar]
- Bugental, D.B.; Johnston, C. Parental and child cognitions in the context of the family. Annu. Rev. Psychol. 2000, 51, 315–344. [Google Scholar] [CrossRef]
- Johnston, C.; Ohan, J.L. The importance of parental attributions in families of children with attention-deficit/hyperactivity and disruptive behavior disorders. Clin. Child Fam. Psychol. Rev. 2005, 8, 167–182. [Google Scholar] [CrossRef]
- Wang, M.; Wang, J. Negative parental attribution and emotional dysregulation in Chinese early adolescents: Harsh fathering and harsh mothering as potential mediators. Child Abus. Negl. 2018, 81, 12–20. [Google Scholar] [CrossRef]
- McCabe, K.M.; Goebring, K.; Yeh, M.; Lau, A.S. Parental locus of control and externalizing behavior problems among Mexican American preschoolers. J. Emot. Behav. Disord. 2008, 16, 118–126. [Google Scholar] [CrossRef]
- Denham, S.A. Dealing with feelings: How children negotiate the worlds of emotions and social relationships. Cogn. Brain Behav. 2007, 1, 1–48. [Google Scholar] [CrossRef][Green Version]
- Dunsmore, J.C.; Booker, J.A.; Ollendick, T.H. Parental emotion coaching and child emotion regulation as protective factors for children with oppositional defiant disorder. Soc. Dev. 2013, 22, 444–466. [Google Scholar] [CrossRef] [PubMed]
- Weber-Milne, J.S.K. The Influence of Mother and Father Emotion Socialization of Angry Temperament on Children’s Oppositional Defiant Behaviors. Ph.D. Thesis, University of California, Davis, CA, USA, 2015. [Google Scholar]
- Suveg, C.; Shaffer, A.; Morelen, D.; Thomassin, K. Links between maternal and child psychopathology symptoms: Mediation through child emotion regulation and moderation through maternal behavior. Child Psychiatry Hum. Dev. 2011, 42, 507–520. [Google Scholar] [CrossRef]
- Jiang, Y.; Lin, X.; Zhou, Q.; Hou, X.; Ding, W.; Zhou, N. Longitudinal dyadic analyses of emotion dysregulation and mother-child relationship quality in Chinese children with teacher-reported oppositional defiant disorder. Soc. Dev. 2020, 29, 217–231. [Google Scholar] [CrossRef]
- Rettew, D.C.; Copeland, W.; Stanger, C.; Hudziak, J.J. Associations between temperament and DSM-IV externalizing disorders in children and adolescents. J. Dev. Behav. Pediatrics 2004, 25, 383–391. [Google Scholar] [CrossRef][Green Version]
- Schmeck, K.; Poustka, F. Temperament and disruptive behavior disorders. Psychopathology 2001, 34, 159–163. [Google Scholar] [CrossRef]
- Dougherty, L.R.; Buffered, S.J.; Carlson, G.A.; Dyson, M.; Olino, T.M.; Durbin, C.E.; Klein, D.N. Preschoolers’ observed temperament and psychiatric disorders assessed with a parent diagnostic interview. J. Clin. Child Adolesc. Psychol. 2011, 40, 295–306. [Google Scholar] [CrossRef]
- Stringaris, A.; Maughan, B.; Goodman, R. What’s in a disruptive disorder? Temperamental antecedents of oppositional defiant disorder: Findings from the Avon Longitudinal Study. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 474–483. [Google Scholar] [CrossRef]
- Kim, H.W.; Cho, S.C.; Kim, B.N.; Kim, J.W.; Shin, M.S.; Yeo, J.Y. Does oppositional defiant disorder have temperament and psychopathological profiles independent of attention deficit/hyperactivity disorder? Compr. Psychiatry 2010, 51, 412–418. [Google Scholar] [CrossRef]
- Joyce, D.; Oakland, T. Temperament differences among children with conduct disorder and oppositional defiant disorder. Calif. Sch. Psychol. 2005, 10, 125–136. [Google Scholar] [CrossRef]
- Melegari, M.G.; Nanni, V.; Lucidi, F.; Russo, P.M.; Donfranceso, R.; Cloninger, R. Temperamental and character profiles of preschool children with ODD, ADHD, and anxiety disorders. Compr. Psychiatry 2015, 58, 94–101. [Google Scholar] [CrossRef]
- Nielsen, I.K.M. The Impact of Temperamental Dimensions on Change in Symptoms of Oppositional Defiant Disorder from Preschool to First Grade. Master’s Thesis, Norwegian University of Science and Technology, Trondheim, Norway, 2014. [Google Scholar]
- Frick, M.A.; Brocki, K.C. A multi-factorial perspective on ADHD and ODD in school-aged children: What is the role of cognitive regulation, temperament, and parental support? J. Clin. Exp. Neuropsychol. 2019, 41, 933–945. [Google Scholar] [CrossRef]
- Long, E.C.; Hill, J.; Luna, B.; Verhulst, B.; Clark, D.B. Disruptive behavior disorders and indicators of disinhibition in adolescents: The BRIEF-SR, anti-saccade task, and D-KEFS color-word interference test. J. Adolesc. 2015, 44, 182–190. [Google Scholar] [CrossRef]
- Prior, M.; Smart, D.; Sanson, A.; Oberklaid, F. Longitudinal predictors of behavioural adjustment in pre-adolescent children. Austrialian N. Z. J. Psychiatry 2001, 35, 297–307. [Google Scholar] [CrossRef]
- Botero, J.C.R.; Medina, C.M.A.; Rizzo, A.A.; Aristizabal, A.C.G.; Zuluaga, E.H. Relationship between social cognition and executive functions in children with oppositional defiant disorder. Rev. Iberoam. Diagn. Eval. Psicol. 2016, 2, 49–58. [Google Scholar] [CrossRef]
- O’Kearney, R.; Salmon, K.; Liwag, M.; Fortune, C.; Dawel, A. Emotional abilities in children with oppositional defiant disorder (ODD): Impairments in perspective–taking and understanding mixed emotions are associated with high callous–unemotional traits. Child Psychiatry Hum. Dev. 2017, 48, 346–357. [Google Scholar] [CrossRef]
- Sharp, C.; Croudace, T.J.; Goodyer, I.M. Biased mentalizing in children aged seven to 11: Latent class confirmation of response styles to social scenarios and associations with psychopathology. Soc. Dev. 2007, 16, 181–202. [Google Scholar] [CrossRef]
- Sharp, C.; Ha, C.; Fonagy, P. Get them before they get you: Trust, trustworthiness, and social cognition in boys with and without externalizing behavior problems. Dev. Psychopathol. 2011, 23, 647–658. [Google Scholar] [CrossRef]
- Dinolfo, C.; Malti, T. Interpretive understanding, sympathy, and moral emotion attribution in oppositional defiant disorder symptomatology. Child Psychiatry Hum. Dev. 2013, 44, 633–645. [Google Scholar] [CrossRef]
- Osa ND, L.; Granero, R.; Domenech, J.M.; Shamay–Tsoory, S.; Ezpeletain, L. Cognitive and affective components of theory of mind in preschoolers with oppositional defiance disorder: Clinical evidence. Psychiatry Res. 2016, 241, 128–134. [Google Scholar] [CrossRef]
- Skoulos, V.; Tryon, G.S. Social skills of adolescents in special education who display symptoms of oppositional defiant disorder. Am. Second. Educ. 2007, 35, 103–115. Available online: https://www.gc.cuny.edu/CUNY_GC/media/CUNY-GraduateCenter/PDF/Programs/Ed%20Psych/Skoulos---Tryon-(2007).pdf (accessed on 19 November 2015).
- Lansford, J.E.; Malone, P.S.; Dodge, K.A.; Crozier, J.C.; Pettit, G.S.; Bates, J.E. A 12-year prospective study of patterns of social information processing problems and externalizing behaviors. J. Abnorm. Child Psychol. 2006, 34, 715–724. [Google Scholar] [CrossRef] [PubMed]
- Coy, K.; Speltz, M.L.; Deklyen, M.; Jones, K. Social–cognitive processes in preschool boys with and without oppositional defiant disorder. J. Abnorm. Child Psychol. 2001, 29, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Calkins, S.D.; Hill, A. Caregiver influences on emerging emotion regulation: Biological and environmental transactions in early development. In Handbook of Emotion Regulation; Gross, J.J., Ed.; Guilford Press: New York, NY, USA, 2007; pp. 229–248. [Google Scholar]
- Aldao, A.; Gee, D.G.; De Los Reyes, A.; Seager, I. Emotion regulation as a transdiagnostic factor in the development of internalizing and externalizing psychopathology: Current and future directions. Dev. Psychopathol. 2016, 28, 927–946. [Google Scholar] [CrossRef] [PubMed]
- Bridges, L.J.; Denham, S.A.; Ganiban, J.M. Definitional issues in emotion regulation research. Child Dev. 2004, 75, 340–345. [Google Scholar] [CrossRef]
- Burke, J.D. An affective dimension within oppositional defiant disorder symptoms among boys: Personality and psychopathology outcomes into early adulthood. J. Child Psychol. Psychiatry 2012, 53, 1176–1183. [Google Scholar] [CrossRef]
- Cavanagh, M.; Quinn, D.; Duncan, D.; Graham, T.; Balbuena, L. Oppositional defiant disorder is better conceptualized as a disorder of emotional regulation. J. Atten. Disord. 2016, 21, 381–389. [Google Scholar] [CrossRef]
- Stringaris, A.; Goodman, R. Three dimensions of oppositionality in youth. J. Child Psychol. Psychiatry Allied Discip. 2009, 50, 216–223. [Google Scholar] [CrossRef]
- Chen, H.; Lin, X.; Heath, M.A.; Ding, W. Family violence and oppositional defiant disorder symptoms in Chinese children: The role of parental alienation and child emotion regulation. Child Fam. Soc. Work 2020, 25, 964–972. [Google Scholar] [CrossRef]
- Cole, P.M.; Deater-Deckard, K. Emotion regulation, risk, and psychopathology. J. Child Psychol. Psychiatry 2009, 50, 1327–1330. [Google Scholar] [CrossRef]
- Southam-Gerow, M.A.; Kendall, P.C. Emotion regulation and understanding implications for child psychopathology and therapy. Clin. Psychol. Rev. 2002, 22, 189–222. [Google Scholar] [CrossRef]
- Yap MB, H.; Allen, N.B.; Sheeber, L. Using an emotion regulation framework to understand the role of temperament and family processes in risk for adolescent depressive disorders. Clin. Child Fam. Psychol. Rev. 2007, 10, 180–196. [Google Scholar] [CrossRef]
- Schoorl, J.; van Rijn, S.; de Wied, M.; van Goozen, S.; Swaab, H. Emotion regulation difficulties in boys with oppositional defiant disorder/conduct disorder and the relation with comorbid autism traits and attention deficit traits. PLoS ONE 2016, 11, e0159323. [Google Scholar] [CrossRef]
- Paliziyan, A.; Honarman, M.M.; Arshadi, N. Oppositional defiant disorder in students: The predicting role of emotion regulation, schema, and vandalism. Int. J. High Risk Behav. Addict. 2018, 7, e67691. [Google Scholar] [CrossRef]
- Bowen, M. Alcoholism as viewed through family systems theory and family psychotherapy. Ann. N. Y. Acad. Sci. 1974, 233, 115–122. [Google Scholar] [CrossRef]
- Granero, R.; Louwaars, L.; Ezpeleta, L. Socioeconomic status and oppositional defiant disorder in preschoolers: Parenting practices and executive functioning as mediating variables. Front. Psychol. 2015, 6, 1412. [Google Scholar] [CrossRef]
- Liu, X.; Lin, X.; Heath, M.A.; Zhou, Q.; Ding, W.; Qin, S. Longitudinal linkages between parenting stress and oppositional defiant disorder (ODD) symptoms among Chinese children with ODD. J. Fam. Psychology. 2018, 32, 1078. [Google Scholar] [CrossRef]
- Petitclerc, A.; Tremblay, R.E. Childhood disruptive behavior disorders: Review of their origin, development, and prevention. Can. J. Psychiatry 2009, 54, 222–231. [Google Scholar] [CrossRef]
- Chorpita, B.F.; Daleiden, E.L.; Ebesutani, C.; Young, J.; Becker, K.D.; Starace, N. Evidence-based treatments for children and adolescents: An updated review of indicators of efficacy and effectiveness. Clin. Psychol. Sci. Pract. 2011, 18, 154–172. [Google Scholar] [CrossRef]
- Forgatch, M.S.; Patterson, G.R. Parent management training—Oregon model: An intervention for antisocial behaviors in children and adolescents. In Evidenced-Based Psychotherapies for Children and Adolescents, 2nd ed.; Weisz, J.R., Kazdin, A.E., Eds.; Guilford Press: New York, NY, USA, 2010; pp. 159–178. [Google Scholar]
- Bronfenbrenner, U. The Ecology of Human Development: Experiments by Nature and Design; Harvard University Press: Cambridge, MA, USA, 1979. [Google Scholar]
| Characteristic | n | % Study Sample |
|---|---|---|
| Year of publication | ||
| 2000–2010 | 20 | 32.3% |
| 2011–2020 | 42 | 67.7% |
| Methodology | ||
| Cross-sectional | 19 | 30.7% |
| Longitudinal | 43 | 69.3% |
| Sample size | ||
| <100 | 8 | 12.9% |
| 101–300 | 26 | 41.9% |
| 301–600 | 12 | 19.4% |
| >600 | 16 | 25.8% |
| Mean age of child participants | ||
| <5 years | 16 | 25.8% |
| 6–12 years | 38 | 61.3% |
| 13–18 years | 8 | 12.9% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, X.; He, T.; Heath, M.; Chi, P.; Hinshaw, S. A Systematic Review of Multiple Family Factors Associated with Oppositional Defiant Disorder. Int. J. Environ. Res. Public Health 2022, 19, 10866. https://doi.org/10.3390/ijerph191710866
Lin X, He T, Heath M, Chi P, Hinshaw S. A Systematic Review of Multiple Family Factors Associated with Oppositional Defiant Disorder. International Journal of Environmental Research and Public Health. 2022; 19(17):10866. https://doi.org/10.3390/ijerph191710866
Chicago/Turabian StyleLin, Xiuyun, Ting He, Melissa Heath, Peilian Chi, and Stephen Hinshaw. 2022. "A Systematic Review of Multiple Family Factors Associated with Oppositional Defiant Disorder" International Journal of Environmental Research and Public Health 19, no. 17: 10866. https://doi.org/10.3390/ijerph191710866
APA StyleLin, X., He, T., Heath, M., Chi, P., & Hinshaw, S. (2022). A Systematic Review of Multiple Family Factors Associated with Oppositional Defiant Disorder. International Journal of Environmental Research and Public Health, 19(17), 10866. https://doi.org/10.3390/ijerph191710866






