Everyday Experiences of People Living with Mild Cognitive Impairment or Dementia: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Search Strategy
2.3. Study Selection
2.4. Data Extraction and Analysis
3. Results
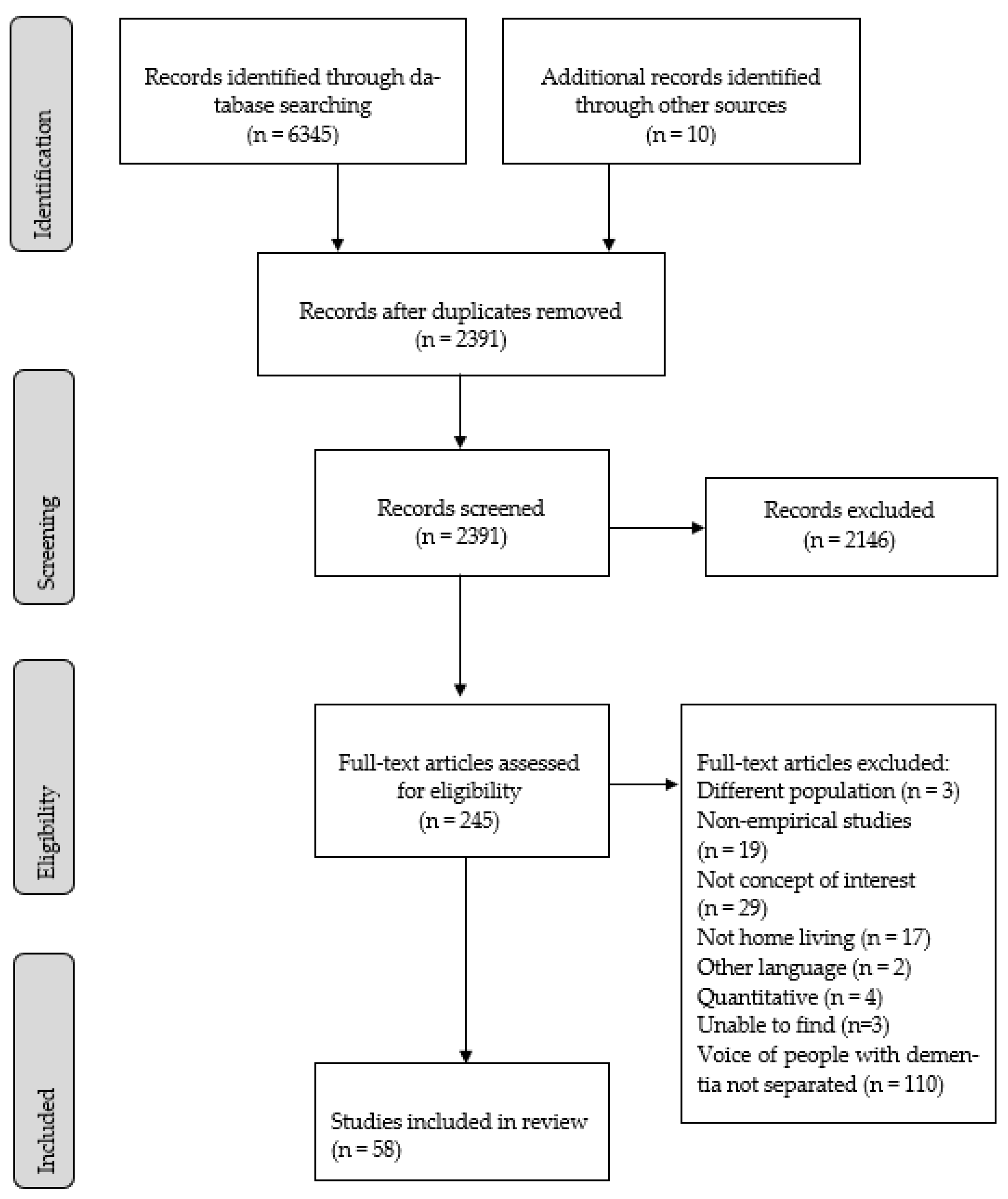
3.1. Selection of Evidence
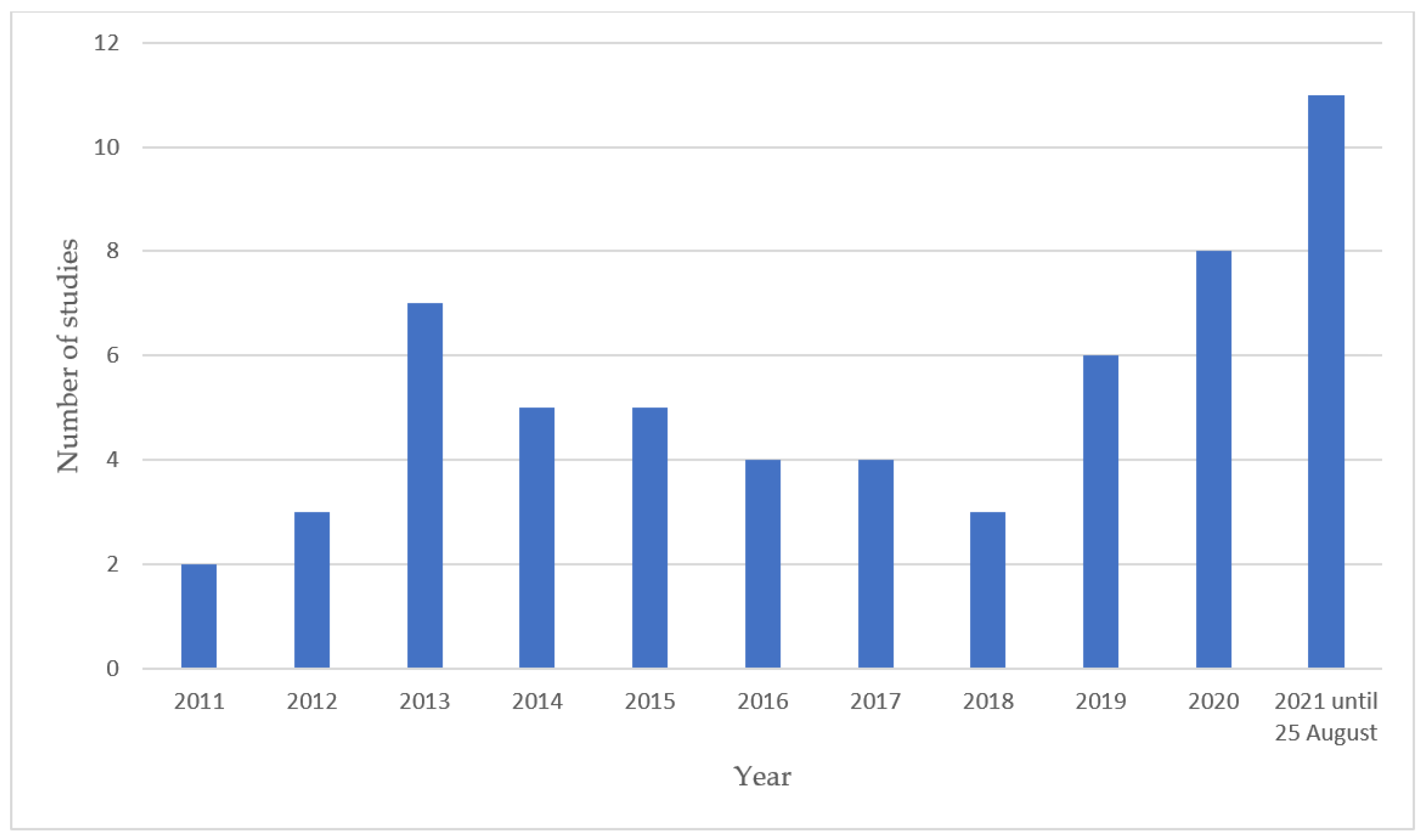
3.2. Characteristics of the Evidence
3.3. Descriptive Qualitative Content Analysis
3.3.1. Sphere 1: Dementia Condition
- Receiving the diagnosis
- 2.
- Changes and dealing with changes
- 3.
- Future living with dementia
3.3.2. Sphere 2: Sense of Self
- Self-evaluations
- 2.
- Emotions
- 3.
- Sense of body
3.3.3. Sphere 3: Relationships
- Relationship with partner and family
- 2.
- Relationships with friends
- 3.
- Relationships in the wider community
3.3.4. Sphere 4: Activities
- Activities of daily living
- 2.
- Participation
3.3.5. Sphere 5: Environment
- At home
- 2.
- Public space
3.3.6. Sphere 6: Experiences with Healthcare and Social Services
- Experiences with healthcare
- 2.
- Experiences with social services
3.3.7. Sphere 7: Public Opinions
4. Discussion
4.1. Strengths and Limitations
4.2. Implications for Research and Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Korsnes, M.S.; Winkler, A.S. Global, regional, and national burden of dementia, 1990–2016: Predictions need local calibration. Neurology 2020, 94, 718–719. [Google Scholar] [CrossRef] [PubMed]
- Livingston, G.; Sommerlad, A.; Orgeta, V.; Costafreda, S.G.; Huntley, J.; Ames, D.; Ballard, C.; Banerjee, S.; Burns, A.; Cohen-Mansfield, J.; et al. Dementia prevention, intervention, and care. Lancet 2017, 390, 2673–2734. [Google Scholar] [CrossRef]
- Birt, L.; Poland, F.; Csipke, E.; Charlesworth, G. Shifting dementia discourses from deficit to active citizenship. Sociol. Health Illn. 2017, 39, 199–211. [Google Scholar] [CrossRef] [PubMed]
- De Vugt, M.; Dröes, R.-M. Social health in dementia. Towards a positive dementia discourse. Aging Ment. Health 2017, 21, 1–3. [Google Scholar] [CrossRef]
- Fletcher, J.R. Destigmatising dementia: The dangers of felt stigma and benevolent othering. Dementia 2021, 20, 417–426. [Google Scholar] [CrossRef]
- Behuniak, S.M. The living dead? The construction of people with Alzheimer’s disease as zombies. Ageing Soc 2011, 31, 70–92. [Google Scholar] [CrossRef]
- Post, S.G. The Concept of Alzheimer Disease in a Hypercognitive Society. In Concepts of Alzheimer Disease: Biological, Clinical and Cultural Perspectives; Whitehouse, P.J., Maurer, K., Ballenger, J.F., Eds.; John Hopkins University Press: Baltimore, MD, USA, 2000; pp. 245–256. [Google Scholar]
- Beard, R.L.; Knauss, J.; Moyer, D. Managing Disability and Enjoying Life: How We Reframe Dementia through Personal Narratives. J. Aging Stud. 2009, 23, 227–235. [Google Scholar] [CrossRef]
- Kontos, P.; Miller, K.; Kontos, A.P. Relational Citizenship: Supporting Embodied Selfhood and Relationality in Dementia Care. Sociol. Health Illn. 2017, 39, 182–198. [Google Scholar] [CrossRef]
- Whitehouse, P.J. The Myth of Alzheimer’s: What You Aren’t Being Told about Today’s Most Dreaded Diagnosis; MacMillan: New York, NY, USA, 2008. [Google Scholar]
- Kitwood, T. The experience of dementia. Aging Ment. Health 1997, 1, 13–22. [Google Scholar] [CrossRef]
- Kitwood, T.; Bredin, K. Towards a theory of dementia care: Personhood and well-being. Ageing Soc. 1992, 12, 269–287. [Google Scholar] [CrossRef]
- Kelly, F. Abusive interactions: Research in locked wards for people with dementia. Soc. Policy Soc. 2010, 9, 267–277. [Google Scholar] [CrossRef]
- Mitchell, G.; Agnelli, J. Person-centred care for people with dementia: Kitwood reconsidered. Nurs. Stand. 2015, 30, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Kogan, A.C.; Wilber, K.; Mosqueda, L. Person-centered care for older adults with chronic conditions and functional impairment: A systematic literature review. J. Am. Geriatr. Soc. 2016, 64, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Terkelsen, A.S.; Petersen, J.V.; Kristensen, H.K. Mapping empirical experiences of Tom Kitwood’s framework of person-centred care for persons with dementia in institutional settings. A scoping review. Scand. J. Caring Sci. 2020, 34, 6–22. [Google Scholar] [CrossRef] [PubMed]
- Spector, A.; Orrell, M. Using a biopsychosocial model of dementia as a tool to guide clinical practice. Int. Psychogeriatr. 2010, 22, 957–965. [Google Scholar] [CrossRef]
- Kontos, P. Embodied Selfhood: Redefining Agency in Alzheimer’s Disease. In Old Age and Agency; Tulle, E., Ed.; Nova Science Publishers: Hauppauge, NY, USA, 2004; pp. 105–121. [Google Scholar]
- Kontos, P.C. Embodied Selfhood in Alzheimer’s Disease. Dementia 2005, 4, 553–570. [Google Scholar] [CrossRef]
- Kontos, P. Alzheimer Expressions or Expressions Despite Alzheimer’s?: Philosophical Reflections on Selfhood and Embodiment. Occas. Interdiscip. Stud. Humanit. 2012, 4, 1–12. [Google Scholar]
- Bellass, S.; Balmer, A.; May, V.; Keady, J.; Buse, C.; Capstick, A.; Burke, L.; Bartlett, R.; Hodgson, J. Broadening the Debate on Creativity and Dementia: A Critical Approach. Dementia 2019, 18, 2799–2820. [Google Scholar] [CrossRef]
- Camic, P.M.; Tischler, V.; Pearman, C.H. Viewing and Making Art Together: A Multi-Session Art-Gallery-Based Intervention for People with Dementia and Their Carers. Aging Ment. Health 2013, 18, 161–168. [Google Scholar] [CrossRef]
- Kinney, J.M.; Rentz, C.A. Observed Well-Being among Individuals with Dementia: Memories in the Making©, an Art Program, versus Other Structured Activity. Am. J. Alzheimer’s Dis. Other Dement. 2005, 20, 220–227. [Google Scholar] [CrossRef]
- MacPherson, S.; Bird, M.; Anderson, K.; Davis, T.; Blair, A. An Art Gallery Access Programme for People with Dementia: ‘You Do It for the Moment. ’ Aging Ment. Health 2009, 13, 744–752. [Google Scholar] [CrossRef] [PubMed]
- Hannemann, B.T. Creativity with Dementia Patients. Gerontology 2006, 52, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.; Culverwell, A.; Hulbert, S.; Robertson, M.; Camic, P.M. Museum Activities in Dementia Care: Using Visual Analog Scales to Measure Subjective Wellbeing. Dementia 2017, 16, 591–610. [Google Scholar] [CrossRef] [PubMed]
- Melhuish, R.; Beuzeboc, C.; Guzmán, A. Developing Relationships between Care Staff and People with Dementia through Music Therapy and Dance Movement Therapy: A Preliminary Phenomenological Study. Dementia 2017, 16, 282–296. [Google Scholar] [CrossRef]
- Lee, K.H.; Lee, J.Y.; Kim, B. Person-Centered Care in Persons Living with Dementia: A Systematic Review and Meta-Analysis. Gerontologist 2020, 62, e253–e264. [Google Scholar] [CrossRef]
- Daley, S.; Newton, D.; Slade, M.; Murray, J.; Banerjee, S. Development of a Framework for Recovery in Older People with Mental Disorder. Int. J. Geriatr. Psych. 2013, 28, 522–529. [Google Scholar] [CrossRef]
- Roberts, G.; Wolfson, P. The Rediscovery of Recovery: Open to All. Adv. Psychiatr. Treat. 2004, 10, 37–48. [Google Scholar] [CrossRef]
- Leamy, M.; Bird, V.; Boutillier, C.L.; Williams, J.; Slade, M. Conceptual Framework for Personal Recovery in Mental Health: Systematic Review and Narrative Synthesis. Brit. J. Psychiat. 2011, 199, 445–452. [Google Scholar] [CrossRef]
- Kröger, T. Care Research and Disability Studies: Nothing in Common? Crit. Soc. Policy 2009, 29, 398–420. [Google Scholar] [CrossRef]
- United Nations. Convention on the Rights of Persons with Disabilities and Optional Protocol; United Nations: New York, NY, USA, 2006. [Google Scholar]
- Kjellberg, A. Being a Citizen. Disabil. Soc. 2002, 17, 187–203. [Google Scholar] [CrossRef]
- Lin, J.-D.; Lin, L.-P.; Hsu, S.-W. Aging People with Intellectual Disabilities: Current Challenges and Effective Interventions. Rev. J. Autism. Dev. Disord. 2016, 3, 266–272. [Google Scholar] [CrossRef]
- Redley, M. Understanding the Social Exclusion and Stalled Welfare of Citizens with Learning Disabilities. Disabil. Soc. 2009, 24, 489–501. [Google Scholar] [CrossRef]
- Bartlett, R.; O’Connor, D. From personhood to citizenship: Broadening the lens for dementia practice and research. J. Aging Stud. 2007, 21, 107–118. [Google Scholar] [CrossRef]
- Bartlett, R. Citizenship in action: The lived experiences of citizens with dementia who campaign for social change. Disabil. Soc. 2014, 29, 1291–1304. [Google Scholar] [CrossRef]
- Downs, M.; Lord, K. Person-centered dementia care in the community: A perspective from the United Kingdom. J. Gerontol. Nurs. 2017, 43, 11–17. [Google Scholar] [CrossRef]
- Hydén, L.-C. Storytelling in dementia: Embodiment as a resource. Dementia 2013, 12, 359–367. [Google Scholar] [CrossRef]
- Oliver, M.; Sapey, R.; Thomas, P. Social Work with Disabled People, 4th ed.; Palgrave Macmillan: Basingstoke, UK, 2012. [Google Scholar]
- Shakespeare, T.; Zeilig, H.; Mittler, P. Rights in Mind: Thinking Differently about Dementia and Disability. Dementia 2019, 18, 1075–1088. [Google Scholar] [CrossRef]
- National Dementia Action Alliance. Dementia Statements. 2017. Available online: https://nationaldementiaaction.org.uk/dementia-statements/ (accessed on 22 August 2022).
- Peoples, H.; Varming, J.; Kristensen, H.K. Social Citizenship When Living with Dementia: A Qualitative Meta-Study. J. Occup. Sci. 2022, 5, 1–19. [Google Scholar] [CrossRef]
- Nedlund, A.-C.; Bartlett, R. Citizenship in-and-as-practice: A framework for improving life with dementia. In Living with Dementia; Hydén, L.-C., Antelius, E., Eds.; Palgrave: London, UK, 2017; pp. 49–67. [Google Scholar]
- Marsh, P.; Courtney-Pratt, H.; Campbell, M. The landscape of dementia inclusivity. Health Place 2018, 52, 174–179. [Google Scholar] [CrossRef]
- Woodbridge, R.; Sullivan, M.; Harding, E.; Crutch, S.; Gilhooly, K.; Gilhooly, M.; McIntyre, A.; Wilson, L. Use of the physical environment to support everyday activities for people with dementia: A systematic review. Dementia 2018, 17, 533–572. [Google Scholar] [CrossRef]
- Purkis, M.E.; Ceci, C. Problematising care burden research. Ageing Soc. 2015, 35, 1410–1428. [Google Scholar] [CrossRef]
- Zarit, S.H.; Femia, E.E. A future for family care and dementia intervention research? Challenges and strategies. Aging Ment. Health 2008, 12, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Morrisby, C.; Joosten, A.; Ciccarelli, M. Do services meet the needs of people with dementia and carers living in the community? A scoping review of the international literature. Int. Psychogeriatr. 2018, 30, 5–14. [Google Scholar] [CrossRef] [PubMed]
- McDermott, O.; Charlesworth, G.; Hogervorst, E.; Stoner, C.; Moniz-Cook, E.; Spector, A.; Csipke, E.; Orrell, M. Psychosocial interventions for people with dementia: A synthesis of systematic reviews. Aging Ment. Health 2018, 23, 393–403. [Google Scholar] [CrossRef]
- Ceci, C.; Brown, H.S.; Judge, H. Rethinking the assumptions of intervention research concerned with care at home for people with dementia. Dementia 2020, 19, 861–877. [Google Scholar] [CrossRef]
- Reilly, S.T.; Harding, A.J.E.; Morbey, H.; Ahmed, F.; Williamson, P.R.; Swarbrick, C.; Leroi, I.; Davies, L.; Reeves, D.; Holland, F.; et al. What is important to people with dementia living at home? A set of core outcome items for use in the evaluation of non-pharmacological community-based health and social care interventions. Age Ageing 2020, 49, 664–671. [Google Scholar] [CrossRef]
- Harding, A.; Reilly, S. Dementia trials, outcomes, and outcome measurement instruments for people living with dementia and family carers–Considerations on how to improve the “gold standard”. Int. Psychogeriatr. 2021, 33, 327–330. [Google Scholar] [CrossRef]
- Scott, S. Making Sense of Everyday Life; Polity Press: Cambridge, UK, 2009; pp. 1–9. [Google Scholar]
- Nedlund, A.-C.; Bartlett, R.; Clarke, C.L. Everyday Citizenship and People with Dementia.; Dunedin: Edinburgh, UK; London, UK, 2017; pp. 1–12. [Google Scholar]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. Jbi. Évid. Implement. 2021, 19, 3–10. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for Conducting Systematic Scoping Reviews. Int. J. Evid. Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef]
- Petersen, R.C.; Roberts, R.O.; Knopman, D.S.; Boeve, B.F.; Geda, Y.E.; Ivnik, R.J.; Smith, G.E.; Jack, C.R. Mild cognitive impairment: Ten years later. Arch. Neurol. Chic. 2009, 66, 1447–1455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noyes, J. Never mind the qualitative feel the depth! The evolving role of qualitative research in Cochrane Intervention Reviews. J. Res. Nurs. 2010, 15, 525–534. [Google Scholar] [CrossRef]
- Rathbone, J.; Carter, M.; Hoffmann, T.; Glasziou, P. Better duplicate detection for systematic reviewers: Evaluation of systematic review assistant-deduplication module. Syst. Rev. 2015, 4, 6. [Google Scholar] [CrossRef] [PubMed]
- Van de Schoot, R.; de Bruin, J.; Schram, R.; Zahedi, P.; de Boer, J.; Weijdema, F.; Kramer, B.; Huijts, M.; Hoogerwerf, M.; Ferdinands, G.; et al. An open source machine learning framework for efficient and transparent systematic reviews. Nat. Mach. Intell. 2021, 3, 125–133. [Google Scholar] [CrossRef]
- Barton, H. A health map for urban planners. Built Environ. 2005, 31, 339–355. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Bartlett, R.; Brannelly, T. On being outdoors: How people with dementia experience and deal with vulnerabilities. Soc. Sci. Med. 2019, 235, 112336. [Google Scholar] [CrossRef]
- Berg, A.I.; Wallin, A.; Nordlund, A.; Johansson, B. Living with stable MCI: Experiences among 17 individuals evaluated at a memory clinic. Aging Ment. Health 2013, 17, 293–299. [Google Scholar] [CrossRef]
- Borley, G.; Sixsmith, J.; Church, S. How does a woman with Alzheimer’s disease make sense of becoming cared for? Dementia 2016, 15, 1405–1421. [Google Scholar] [CrossRef]
- Brorsson, A.; Öhman, A.; Lundberg, S.; Nygård, L. Accessibility in public space as perceived by people with Alzheimer’s disease. Dementia 2011, 10, 587–602. [Google Scholar] [CrossRef]
- Buggins, S.-L.; Clarke, C.; Wolverson, E. Resilience in older people living with dementia–A narrative analysis. Dementia 2021, 20, 1234–1249. [Google Scholar] [CrossRef]
- Castaño, E. Discourse analysis as a tool for uncovering the lived experience of dementia: Metaphor framing and well-being in early-onset dementia narratives. Discourse Commun. 2020, 14, 115–132. [Google Scholar] [CrossRef]
- Cedervall, Y.; Torres, S.; Åberg, A.C. Maintaining well-being and selfhood through physical activity: Experiences of people with mild Alzheimer’s disease. Aging Ment. Health 2014, 19, 679–688. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.C.; Lin, H.R. The lived experiences of elderly dementia patients in Taiwan. Int. J. Ment. Health Nurs. 2019, 28, 784–792. [Google Scholar] [CrossRef] [PubMed]
- Chung, P. Experiences of older people with dementia: Homecare enablement to support transitions in daily life at home. Brit. J. Occup. 2019, 82, 716–725. [Google Scholar] [CrossRef]
- Clark, A.; Campbell, S.; Keady, J.; Kullberg, A.; Manji, K.; Rummery, K.; Ward, R. Neighbourhoods as relational places for people living with dementia. Soc. Sci. Med. 2020, 252, 112927. [Google Scholar] [CrossRef]
- Clemerson, G.; Walsh, S.; Isaac, C. Towards living well with young onset dementia: An exploration of coping from the perspective of those diagnosed. Dementia 2014, 13, 451–466. [Google Scholar] [CrossRef]
- Dooley, J.; Webb, J.; James, R.; Davis, H.; Read, S. Everyday experiences of post-diagnosis life with dementia: A co-produced photography study. Dementia 2021, 20, 1891–1909. [Google Scholar] [CrossRef]
- Duane, F.; Brasher, K.; Koch, S. Living alone with dementia. Dementia 2013, 12, 123–136. [Google Scholar] [CrossRef]
- Frazer, S.M.; Oyebode, J.R.; Cleary, A. How older women who live alone with dementia make sense of their experiences: An interpretative phenomenological analysis. Dementia 2012, 11, 677–693. [Google Scholar] [CrossRef]
- Griffin, J.; Oyebode, J.R.; Allen, J. Living with a diagnosis of behavioural-variant frontotemporal dementia: The person’s experience. Dementia 2016, 15, 1622–1642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hedman, A.; Lindqvist, E.; Nygård, L. How older adults with mild cognitive impairment relate to technology as part of present and future everyday life: A qualitative study. BMC Geriatr. 2016, 16, 73. [Google Scholar] [CrossRef] [PubMed]
- Hellström, I.; Eriksson, H.; Sandberg, J. Chores and sense of self: Gendered understandings of voices of older married women with dementia. Int. J. Older People Nurs. 2015, 10, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Hicks, B.; Innes, A.; Nyman, S.R. Experiences of rural life among community-dwelling older men with dementia and their implications for social inclusion. Dementia 2021, 20, 444–463. [Google Scholar] [CrossRef]
- Johannessen, A.; Möller, A. Experiences of persons with early-onset dementia in everyday life: A qualitative study. Dementia 2013, 12, 410–424. [Google Scholar] [CrossRef]
- Johannessen, A.; Möller, A.; Haugen, P.K.; Biong, S. A shifting sense of being: A secondary analysis and comparison of two qualitative studies on young-onset dementia. Int. J. Qual. Stud. Health 2014, 9, 24756. [Google Scholar] [CrossRef]
- Johannessen, A.; Engedal, K.; Haugen, P.K.; Dourado, M.C.; Thorsen, K. Coping with transitions in life: A four-year longitudinal narrative study of single younger people with dementia. J. Multidiscip. Healthc. 2019, 12, 479–492. [Google Scholar] [CrossRef]
- Johansson, L.; Christensson, L.; Sidenvall, B. Managing mealtime tasks: Told by persons with dementia. J. Clin. Nurs. 2011, 20, 2552–2562. [Google Scholar] [CrossRef]
- Johansson, M.; Marcusson, J.; Wressle, E. Cognitive impairment and its consequences in everyday life: Experiences of people with mild cognitive impairment or mild dementia and their relatives. Int. Psychogeriatr. 2015, 27, 949–958. [Google Scholar] [CrossRef]
- Lin, R.S.Y.; Yu, D.S.F.; Li, P.W.C.; Chau, P.H.; Lee, J.J. Lived experience of neuropsychiatric symptoms among females with mild cognitive impairment: A phenomenological study. J. Adv. Nurs. 2021, 78, 1100–1111. [Google Scholar] [CrossRef]
- Lloyd, B.T.; Stirling, C. The will to mobility: Life-space satisfaction and distress in people with dementia who live alone. Ageing Soc. 2015, 35, 1801–1820. [Google Scholar] [CrossRef]
- Margot-Cattin, I.; Kühne, N.; Öhman, A.; Brorsson, A.; Nygard, L. Familiarity and participation outside home for persons living with dementia. Dementia 2021, 20, 2526–2541. [Google Scholar] [CrossRef] [PubMed]
- Mazaheri, M.; Eriksson, L.E.; Heikkilä, K.; Nasrabadi, A.N.; Ekman, S.; Sunvisson, H. Experiences of living with dementia: Qualitative content analysis of semi-structured interviews. J. Clin. Nurs. 2013, 22, 3032–3041. [Google Scholar] [CrossRef] [PubMed]
- McDuff, J.; Phinney, A. Walking with meaning. Glob. Qual. Nurs. Res. 2015, 2, 2333393615605116. [Google Scholar] [CrossRef]
- Mitchell, G.; McTurk, V.; Carter, G.; Brown-Wilson, C. Emphasise capability, not disability: Exploring public perceptions, facilitators and barriers to living well with dementia in Northern Ireland. BMC Geriatr. 2020, 20, 525. [Google Scholar] [CrossRef]
- Moe, A.; Alnes, R.E.; Nordtug, B.; Blindheim, K.; Steinsheim, G.; Malmedal, W. Coping with everyday life for home-dwelling persons with dementia: A qualitative study. J. Multidiscip. Healthc. 2021, 14, 909–918. [Google Scholar] [CrossRef]
- Odzakovic, E.; Hellström, I.; Ward, R.; Kullberg, A. ‘Overjoyed that I can go outside’: Using walking interviews to learn about the lived experience and meaning of neighbourhood for people living with dementia. Dementia 2020, 19, 2199–2219. [Google Scholar] [CrossRef]
- Odzakovic, E.; Kullberg, A.; Hellström, I.; Clark, A.; Campbell, S.; Manji, K.; Rummery, K.; Keady, J.; Ward, R. ‘It’s our pleasure, we count cars here’: An exploration of the ‘neighbourhood-based connections’ for people living alone with dementia. Ageing Soc. 2021, 41, 645–670. [Google Scholar] [CrossRef]
- Parikh, P.K.; Troyer, A.K.; Maione, A.M.; Murphy, K.J. The impact of memory change on daily life in normal aging and mild cognitive impairment. Gerontologist 2016, 56, 877–885. [Google Scholar] [CrossRef]
- Pipon-Young, F.E.; Lee, K.M.; Jones, F.; Guss, R. I’m not all gone, I can still speak: The experiences of younger people with dementia. An action research study. Dementia 2012, 11, 597–616. [Google Scholar] [CrossRef]
- Portacolone, E.; Rubinstein, R.L.; Covinsky, K.E.; Halpern, J.; Johnson, J.K. The precarity of older adults living alone with cognitive impairment. Gerontologist 2018, 59, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Rabanal, L.I.; Chatwin, J.; Walker, A.; O’Sullivan, M.; Williamson, T. Understanding the needs and experiences of people with young onset dementia: A qualitative study. BMJ Open 2018, 8, e021166. [Google Scholar] [CrossRef] [PubMed]
- Renn, B.N.; Wool, J.L.; Belza, B. A typical week with mild cognitive impairment. Gerontologist 2021, 61, 1095–1106. [Google Scholar] [CrossRef]
- Roberts, J.L.; Clare, L. Meta-representational awareness in mild cognitive impairment: An interpretative phenomenological analysis. Aging Ment. Health 2013, 17, 300–309. [Google Scholar] [CrossRef] [PubMed]
- Robertson, J.M. Finding meaning in everyday life with dementia: A case study. Dementia 2014, 13, 525–543. [Google Scholar] [CrossRef]
- Robinson, P.; Giorgi, B.; Ekman, S.-L. The lived experience of early-stage Alzheimer’s disease: A three-year longitudinal phenomenological case study. J. Phenomenol. Psychol. 2012, 43, 216–238. [Google Scholar] [CrossRef]
- Rostad, D.; Hellzén, O.; Enmarker, I. The meaning of being young with dementia and living at home. Nurs. Rep. 2013, 3, 12–17. [Google Scholar] [CrossRef]
- Sakamoto, M.L.; Moore, S.L.; Johnson, S.T. “I’m still here”: Personhood and the early-onset dementia experience. J. Gerontol. Nurs. 2017, 43, 12–17. [Google Scholar] [CrossRef]
- Sandberg, L.; Rosenberg, L.; Sandman, P.-O.; Borell, L. Risks in situations that are experienced as unfamiliar and confusing–the perspective of persons with dementia. Dementia 2017, 16, 471–485. [Google Scholar] [CrossRef]
- Steeman, E.; Tournoy, J.; Grypdonck, M.; Godderis, J.; de Casterlé, B.D. Managing identity in early-stage dementia: Maintaining a sense of being valued. Ageing Soc. 2013, 33, 216–242. [Google Scholar] [CrossRef]
- Steenwinkel, I.V.; Audenhove, C.V.; Heylighen, A. Mary’s little worlds. Qual. Health Res. 2014, 24, 1023–1032. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strandenæs, M.G.; Lund, A.; Rokstad, A.M.M. Experiences of attending day care services designed for people with dementia–A qualitative study with individual interviews. Aging Ment. Health 2017, 22, 764–772. [Google Scholar] [CrossRef] [PubMed]
- Sturge, J.; Klaassens, M.; Lager, D.; Weitkamp, G.; Vegter, D.; Meijering, L. Using the concept of activity space to understand the social health of older adults living with memory problems and dementia at home. Soc. Sci. Med. 2020, 288, 113208. [Google Scholar] [CrossRef] [PubMed]
- Sturge, J.; Klaassens, M.; Jones, C.A.; Légaré, F.; Elf, M.; Weitkamp, G.; Meijering, L. Exploring assets of people with memory problems and dementia in public space: A qualitative study. Wellbeing Space Soc. 2021, 2, 100063. [Google Scholar] [CrossRef]
- Svanström, R.; Sundler, A.J. Gradually losing one’s foothold–A fragmented existence when living alone with dementia. Dementia 2015, 14, 145–163. [Google Scholar] [CrossRef]
- Talbot, C.V.; O’Dwyer, S.T.; Clare, L.; Heaton, J. The use of Twitter by people with young-onset dementia: A qualitative analysis of narratives and identity formation in the age of social media. Dementia 2021, 20, 2542–2557. [Google Scholar] [CrossRef]
- Thoft, D.S.; Ward, A. “Just ask me what it means to live with dementia”–People with mild dementia’s strategies and techniques shared through in-depth qualitative interviews. J. Clin. Nurs. 2021, 31, 1725–1737. [Google Scholar] [CrossRef]
- Thorsen, K.; Dourado, M.C.N.; Johannessen, A. Developing dementia: The existential experience of the quality of life with young-onset dementia–A longitudinal case study. Dementia 2020, 19, 878–893. [Google Scholar] [CrossRef]
- Trindade, P.G.E.; Santos, R.L.; Lacerda, I.B.; Johannessen, A.; Dourado, M.C.N. Awareness of disease in Alzheimer’s disease: What do patients realize about their own condition? Aging Ment. Health 2018, 23, 1292–1299. [Google Scholar] [CrossRef]
- Trindade, P.G.E.; Santos, R.L.; Johannessen, A.; Neto, J.P.S.; Dourado, M.C.N. Awareness of functional status: People with Alzheimer’s disease abilities to self-report impairment in activities of daily living. J. Alzheimer’s Dis. Rep. 2020, 4, 405–415. [Google Scholar] [CrossRef]
- van Vliet, D.; Persoon, A.; Bakker, C.; Koopmans, R.T.C.M.; de Vugt, M.E.; Bielderman, A.; Gerritsen, D.L. Feeling useful and engaged in daily life: Exploring the experiences of people with young-onset dementia. Int. Psychogeriatr. 2017, 29, 1889–1898. [Google Scholar] [CrossRef] [PubMed]
- Ward, A.; Thoft, D.S.; Lomax, H.; Parkes, J. A visual and creative approach to exploring people with dementia’s experiences of being students at a school in Denmark. Dementia 2020, 19, 786–804. [Google Scholar] [CrossRef]
- Van Wijngaarden, E.; Alma, M.; The, A.-M. ‘The eyes of others’ are what really matters: The experience of living with dementia from an insider perspective. PLoS ONE 2019, 14, e0214724. [Google Scholar] [CrossRef] [PubMed]
- Xanthopoulou, P.; McCabe, R. Subjective experiences of cognitive decline and receiving a diagnosis of dementia: Qualitative interviews with people recently diagnosed in memory clinics in the UK. BMJ Open 2019, 9, e026071. [Google Scholar] [CrossRef]
- Neal, S.; Murji, K. Sociologies of everyday life: Editors’ introduction to the special Issue. Sociology 2015, 49, 811–819. [Google Scholar] [CrossRef]
- Pink, S. Situating Everyday Life; SAGE: London, UK, 2012. [Google Scholar]
- Simplican, S.C.; Leader, G.; Kosciulek, J.; Leahy, M. Defining social inclusion of people with intellectual and developmental disabilities: An ecological model of social networks and community participation. Res. Dev. Disabil. 2015, 38, 18–29. [Google Scholar] [CrossRef]
- Pinkert, C.; Köhler, K.; von Kutzleben, M.; Hochgräber, I.; Cavazzini, C.; Völz, S.; Palm, R.; Holle, B. Social inclusion of people with dementia–An integrative review of theoretical frameworks, methods and findings in empirical studies. Ageing Soc. 2021, 41, 773–793. [Google Scholar] [CrossRef]
- Martyr, A.; Nelis, S.M.; Quinn, C.; Wu, Y.-T.; Lamont, R.A.; Henderson, C.; Clarke, R.; Hindle, J.V.; Thom, J.M.; Jones, I.R.; et al. Living well with dementia: A systematic review and correlational meta-analysis of factors associated with quality of life, well-being and life satisfaction in people with dementia. Psychol. Med. 2018, 48, 2130–2139. [Google Scholar] [CrossRef]
- Bruggencate, T.T.; Luijkx, K.G.; Sturm, J. Social needs of older people: A systematic literature review. Ageing Soc. 2018, 38, 1745–1770. [Google Scholar] [CrossRef]
- Cahill, S. New analytical tools and frameworks to understand dementia: What can a human rights lens offer? Ageing Soc. 2020, 42, 1–10. [Google Scholar] [CrossRef]
- Seamon, D. Body-Subject, Time-Space Routines, and Place-Ballets. In The Human Experience of Space and Place; Routledge: London, UK, 1980; Volume 1, pp. 148–165. [Google Scholar]
- Robertson, J.M.; Gibson, G.; Greasley-Adams, C.; McCall, V.; Gibson, J.; Mason-Duff, J.; Pengelly, R. ‘It gives you a reason to be in this world: The interdependency of communities, environments and social justice for quality of life in older people. Ageing Soc. 2020, 42, 1–25. [Google Scholar] [CrossRef]
- Gaugler, J.E.; Bain, L.J.; Mitchell, L.; Finlay, J.; Fazio, S.; Jutkowitz, E.; Alzheimer’s Association Psychosocial Measurement Workgroup. Reconsidering frameworks of Alzheimer’s dementia when assessing psychosocial outcomes. Alzheimer’s Dement. Transl Res. Clin. Interv. 2019, 5, 388–397. [Google Scholar] [CrossRef] [PubMed]
- Mast, B.T.; Molony, S.L.; Nicholson, N.; Keefe, C.K.; DiGasbarro, D. Person-centered assessment of people living with dementia: Review of existing measures. Alzheimer’s Dement. Transl. Res. Clin. Interv. 2021, 7, e12138. [Google Scholar] [CrossRef]
- Ward, R.; Rummery, K.; Odzakovic, E.; Manji, K.; Kullberg, A.; Keady, J.; Clark, A.; Campbell, S. Beyond the shrinking world: Dementia, localisation and neighbourhood. Ageing Soc. 2021, 1–22. [Google Scholar] [CrossRef]
- Abbott, P.; Wallace, C. Social quality: A way to measure the quality of society. Soc. Indic. Res. 2012, 108, 153–167. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, V.; Samsi, K.; Keady, J. New horizons and new opportunities for qualitative research to understand and improve mental health in later life. Int. J. Geriatr. Psych. 2022, 37. [Google Scholar] [CrossRef]
- Portacolone, E.; Chodos, A.; Halpern, J.; Covinsky, K.E.; Keiser, S.; Fung, J.; Rivera, E.; Tran, T.; Bykhovsky, C.; Johnson, J.K. The effects of the COVID-19 pandemic on the lived experience of diverse older adults living alone with cognitive impairment. Gerontologist 2021, 61, 251–261. [Google Scholar] [CrossRef]
- Talbot, C.V.; Briggs, P. ‘Getting back to normality seems as big of a step as going into lockdown’: The impact of the COVID-19 pandemic on people with early to middle stage dementia. Age Ageing 2021, 50, 657–663. [Google Scholar] [CrossRef]
- Keady, J.; Hydén, L.-C.; Johnson, A.; Swarbrick, C. Social Research Methods in Dementia Studies: Inclusion and Innovation; Routledge: London, UK, 2017. [Google Scholar]
- Phillipson, L.; Hammond, A. More Than Talking. Int. J. Qual. Meth. 2018, 17, 1–13. [Google Scholar] [CrossRef]
- Ahmad, M.; van den Broeke, J.; Saharso, S.; Tonkens, E. Dementia care-sharing and migration: An intersectional exploration of family carers’ experiences. J. Aging Stud. 2022, 60, 100996. [Google Scholar] [CrossRef]
- Bernstein, M.J.; Nielsen, M.W.; Alnor, E.; Brasil, A.; Birkving, A.L.; Chan, T.T.; Griessler, E.; de Jong, S.; van de Klippe, W.; Meijer, I.; et al. The societal readiness thinking tool: A practical resource for maturing the societal readiness of research projects. Sci. Eng. Ethics 2022, 28, 6. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Keady, J.; Ward, R. Neighbourhoods and Dementia: An Updated Realist Review of the Qualitative Literature to Inform Contemporary Practice and Policy Understanding. Dementia 2021, 20, 2957–2981. [Google Scholar] [CrossRef] [PubMed]
- Whelan, S.; Teahan, Á.; Casey, D. Fostering the resilience of people with dementia: A narrative literature review. Front. Med. 2020, 7, 45. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Global Action Against Dementia; WHO: Geneva, Switzerland, 2015; Available online: https://www.who.int/publications/i/item/global-action-plan-on-the-public-health-response-to-dementia-2017---2025 (accessed on 1 August 2022).
| Aspect | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Participants | People with all forms of dementia (such as Alzheimer’s disease, vascular, frontotemporal and Lewy Body dementia) and pre-dementia, such as mild cognitive impairment (MCI) | The perspectives of next of kin to people with dementia or health and social care professionals. |
| Concept | Everyday life, synonyms thereof, and related concepts that could give insight into (parts of) daily life. |
|
| Context | Living at home, in the community, or assisted living facilities | Living in long-term care residences such as nursing homes |
| Type of studies |
|
|
| Set | Category | Search Term |
|---|---|---|
| S1 AND | Participant | dementia OR Alzheimer Disease OR Lewy body OR vascular dement * OR frontotemporal dement * OR mild cognitive impairment OR MCI |
| S2 AND | Concept | daily life OR daily living OR day to day OR everyday OR living well OR lifeworld OR lived experience OR life experience |
| S3 | Study type | qualitative OR phenomenol * OR ethnograph * OR grounded theory OR experience * OR interview OR photo |
| Number of Articles | |
|---|---|
| Country: | |
| Asian countries | 2 |
| Australia | 2 |
| Belgium | 2 |
| Middle East | 1 |
| Scandinavia | 21 |
| South America | 2 |
| Switzerland | 1 |
| The Netherlands | 4 |
| United Kingdom (UK) | 18 |
| United States of America (USA)/Canada | 5 |
| Not reported | 1 |
| Age: | |
| People with young onset dementia | 12 |
| Older people (>65 years) | 23 |
| Mixed | 23 |
| Stage: | |
| Mild cognitive impairment | 6 |
| MCI and dementia | 2 |
| Dementia | 50 |
| Concept: | |
| Everyday life | 0 |
| Lived experiences, lifeworld | 10 |
| Part of everyday life or another concept | 48 |
| Data collection methods: | |
| Face-to-face interviews | 51 |
| Telephone interviews | 1 |
| Focus groups | 5 |
| Blogs | 1 |
| Sphere | Description |
|---|---|
| 1. Dementia | How people experience consequences related to the condition in their life |
| 2. Self | How people evaluate themselves personally and how they experience their emotions and body |
| 3. Relationships | How people experience relationships |
| 4. Activities | How people experience everyday activities |
| 5. Environment | How people experience their environment |
| 6. Healthcare and social services | How people describe experiences with healthcare and social services |
| 7. Public opinions | How people experience public opinions with regard to dementia |
| References | 1. Dementia | 1.1. Receiving Diagnosis | 1.2. Changes | 1.3. Future | 2. Self | 2.1. Self-Evaluations | 2.2. Emotions | 2.3. Body | 3. Relationships | 3.1. Partner/Family | 3.2. Friendships | 3.3. Neighbourhood | 4. Activities | 4.1. Activities of Daily Living | 4.2. Participation | 5. Environment | 5.1. Home | 5.2. Public Environment | 6. Health and Social Care | 6.1 Healthcare | 6.2 Social Care | 7. Public Opinions |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bartlett (2019) [66] | x | x | x | x | x | x | x | x | ||||||||||||||
| Berg (2013) [67] | x | x | x | x | x | x | x | x | x | x | ||||||||||||
| Borley (2016) [68] | x | x | x | x | x | x | x | x | x | |||||||||||||
| Brorsson (2011) [69] | x | x | x | x | x | x | ||||||||||||||||
| Buggins (2021) [70] | x | x | x | x | x | x | x | x | x | x | ||||||||||||
| Castaño (2019) [71] | x | x | x | x | x | x | x | x | x | x | ||||||||||||
| Cedervall (2015) [72] | x | x | x | x | x | x | x | x | ||||||||||||||
| Chen (2019) [73] | x | x | x | x | x | x | x | |||||||||||||||
| Chung (2019) [74] | x | x | x | x | x | x | x | x | x | |||||||||||||
| Clark (2020) [75] | x | x | x | x | x | x | x | x | x | x | x | |||||||||||
| Clemerson (2014) [76] | x | x | x | x | x | x | x | x | x | x | x | |||||||||||
| Dooley (2021) [77] | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||||
| Duane (2011) [78] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||||
| Frazer (2011) [79] | x | x | x | x | x | x | x | x | x | x | x | |||||||||||
| Griffin (2016) [80] | x | x | x | x | x | x | x | x | x | x | x | |||||||||||
| Hedman (2016) [81] | x | x | x | x | x | |||||||||||||||||
| Hellström (2015) [82] | x | x | x | x | x | |||||||||||||||||
| Hicks (2021) [83] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||||
| Johannessen (2013) [84] | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||||||
| Johannessen (2014) [85] | x | x | x | x | x | x | x | |||||||||||||||
| Johannessen (2019) [86] | x | x | x | x | x | x | x | x | x | x | x | |||||||||||
| Johansson (2011) [87] | x | x | ||||||||||||||||||||
| Johansson (2015) [88] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||
| Lin (2021) [89] | x | x | x | x | x | x | x | x | x | x | x | |||||||||||
| Lloyd (2015) [90] | x | x | x | x | x | x | ||||||||||||||||
| Margot-Cattin (2021) [91] | x | x | x | x | ||||||||||||||||||
| Mazaheri (2013) [92] | x | x | x | x | x | x | x | x | x | x | x | |||||||||||
| McDuff (2015) [93] | x | x | x | x | x | x | x | |||||||||||||||
| Mitchell (2020) [94] | x | x | x | x | x | x | x | x | x | x | ||||||||||||
| Moe (2021) [95] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||||
| Odzakovic (2020) [96] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||
| Odzakovic (2021) [97] | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||||
| Parikh (2016) [98] | x | x | x | x | x | x | x | x | x | x | x | |||||||||||
| Pipon-Young (2011) [99] | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||||
| Portacolone (2018) [100] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||||
| Rabanal (2018) [101] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||
| Renn (2021) [102] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||||
| Roberts (2013) [103] | x | x | x | x | x | x | x | x | x | x | x | |||||||||||
| Robertson (2014) [104] | x | x | x | x | x | x | x | x | x | |||||||||||||
| Robinson (2012) [105] | x | x | x | x | x | x | x | x | x | |||||||||||||
| Rostad (2013) [106] | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||||
| Sakamoto (2017) [107] | x | x | x | x | x | x | ||||||||||||||||
| Sandberg (2017) [108] | x | x | x | x | x | x | x | x | ||||||||||||||
| Steeman (2013) [109] | x | x | x | x | x | x | ||||||||||||||||
| Steenwinkel (2014) [110] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||
| Strandenæs (2017) [111] | x | x | ||||||||||||||||||||
| Sturge (2020) [112] | x | x | x | x | x | x | x | x | x | |||||||||||||
| Sturge (2021) [113] | x | x | x | x | x | x | x | x | x | x | x | |||||||||||
| Svanström (2015) [114] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||||
| Talbot (2021) [115] | x | x | x | x | x | x | x | x | ||||||||||||||
| Thoft (2020) [116] | x | x | x | x | x | x | x | x | x | |||||||||||||
| Thorsen (2020) [117] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||||
| Trindade (2018) [118] | x | x | x | x | x | x | ||||||||||||||||
| Trindade (2020) [119] | x | x | x | x | x | x | x | x | x | x | ||||||||||||
| Vliet (2017) [120] | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||||
| Ward (2020) [121] | x | x | x | x | x | x | x | |||||||||||||||
| Wijngaarden (2019) [122] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||
| Xanthopoulou (2019) [123] | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |||||||
| Frequency (%) (N = 58) | 39 | 22 | 26 | 17 | 32 | 32 | 18 | 21 | 46 | 35 | 33 | 14 | 50 | 38 | 38 | 21 | 10 | 15 | 34 | 16 | 18 | 11 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huizenga, J.; Scheffelaar, A.; Fruijtier, A.; Wilken, J.P.; Bleijenberg, N.; Van Regenmortel, T. Everyday Experiences of People Living with Mild Cognitive Impairment or Dementia: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 10828. https://doi.org/10.3390/ijerph191710828
Huizenga J, Scheffelaar A, Fruijtier A, Wilken JP, Bleijenberg N, Van Regenmortel T. Everyday Experiences of People Living with Mild Cognitive Impairment or Dementia: A Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(17):10828. https://doi.org/10.3390/ijerph191710828
Chicago/Turabian StyleHuizenga, Jacoba, Aukelien Scheffelaar, Agnetha Fruijtier, Jean Pierre Wilken, Nienke Bleijenberg, and Tine Van Regenmortel. 2022. "Everyday Experiences of People Living with Mild Cognitive Impairment or Dementia: A Scoping Review" International Journal of Environmental Research and Public Health 19, no. 17: 10828. https://doi.org/10.3390/ijerph191710828
APA StyleHuizenga, J., Scheffelaar, A., Fruijtier, A., Wilken, J. P., Bleijenberg, N., & Van Regenmortel, T. (2022). Everyday Experiences of People Living with Mild Cognitive Impairment or Dementia: A Scoping Review. International Journal of Environmental Research and Public Health, 19(17), 10828. https://doi.org/10.3390/ijerph191710828








