Current War in Ukraine: Lessons from the Impact of War on Combatants’ Mental Health during the Last Decade
Abstract
:1. Introduction
2. Materials and Methods
2.1. Database and Study Design
2.2. Statistical Analysis
3. Results
3.1. Anxiety Disorders Were Already Present in Peacetime, While a High Frequency of Psychoactive Substance Use Emerged with Acute Conflicts
3.2. An Increase in Psychological Stress Symptoms Could Be a Confounding Factor in Admissions Diagnosed as ‘Healthy’
3.3. The ICD-10 Category Depended on the War Period
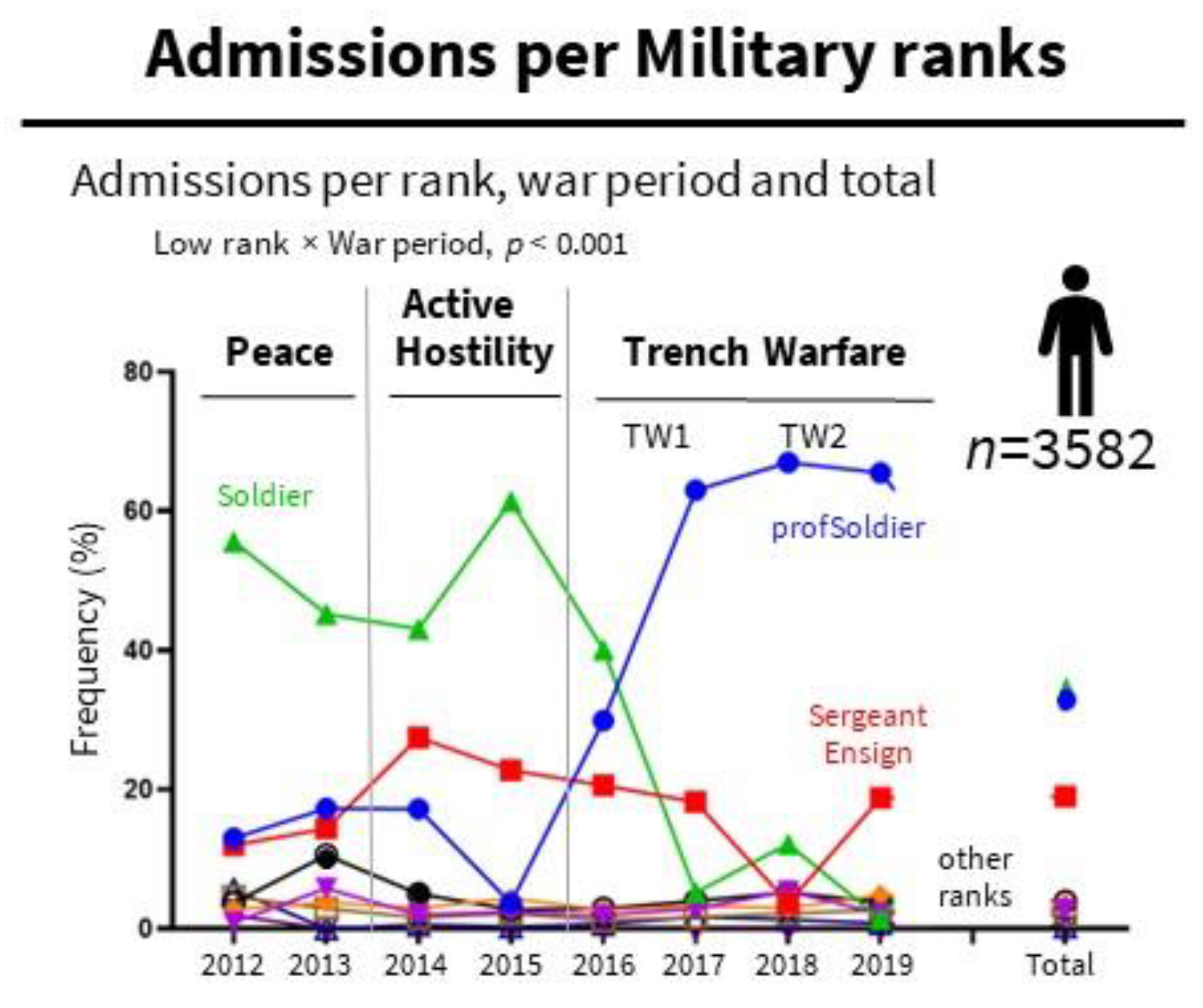
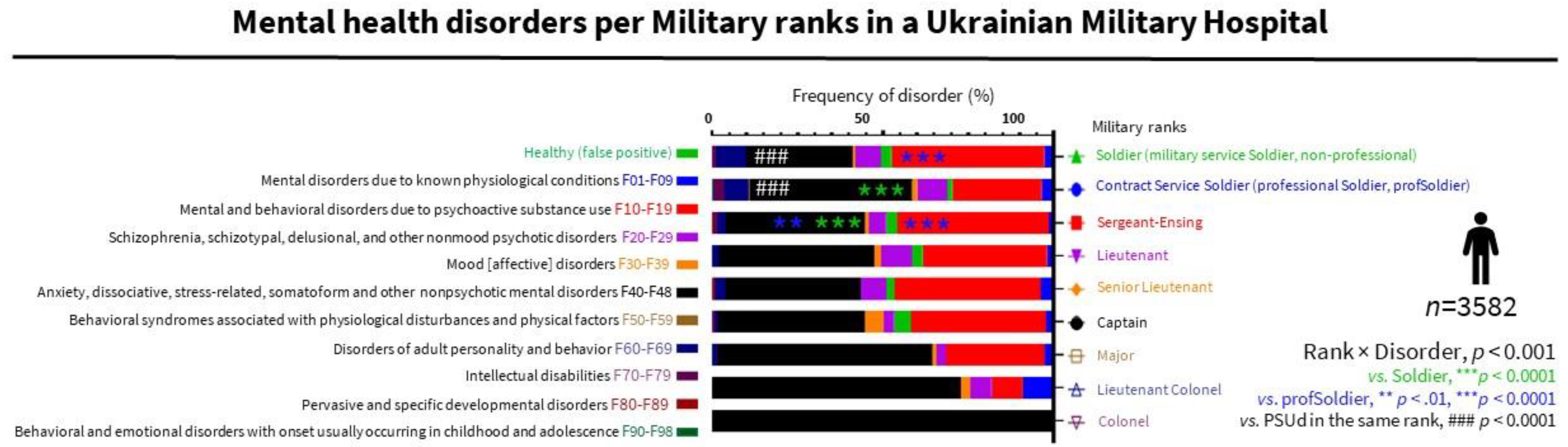
3.4. The Dramatic Increase in Admissions and the Specific Mental Health Profiles per Rank Put the Hospital’s Efficiency at Risk
3.5. The Specific Impact on PSUd in Nonprofessional Soldiers Is Relevant to the Current War, with the General Population of Ukraine Recruited for Defense and Combat
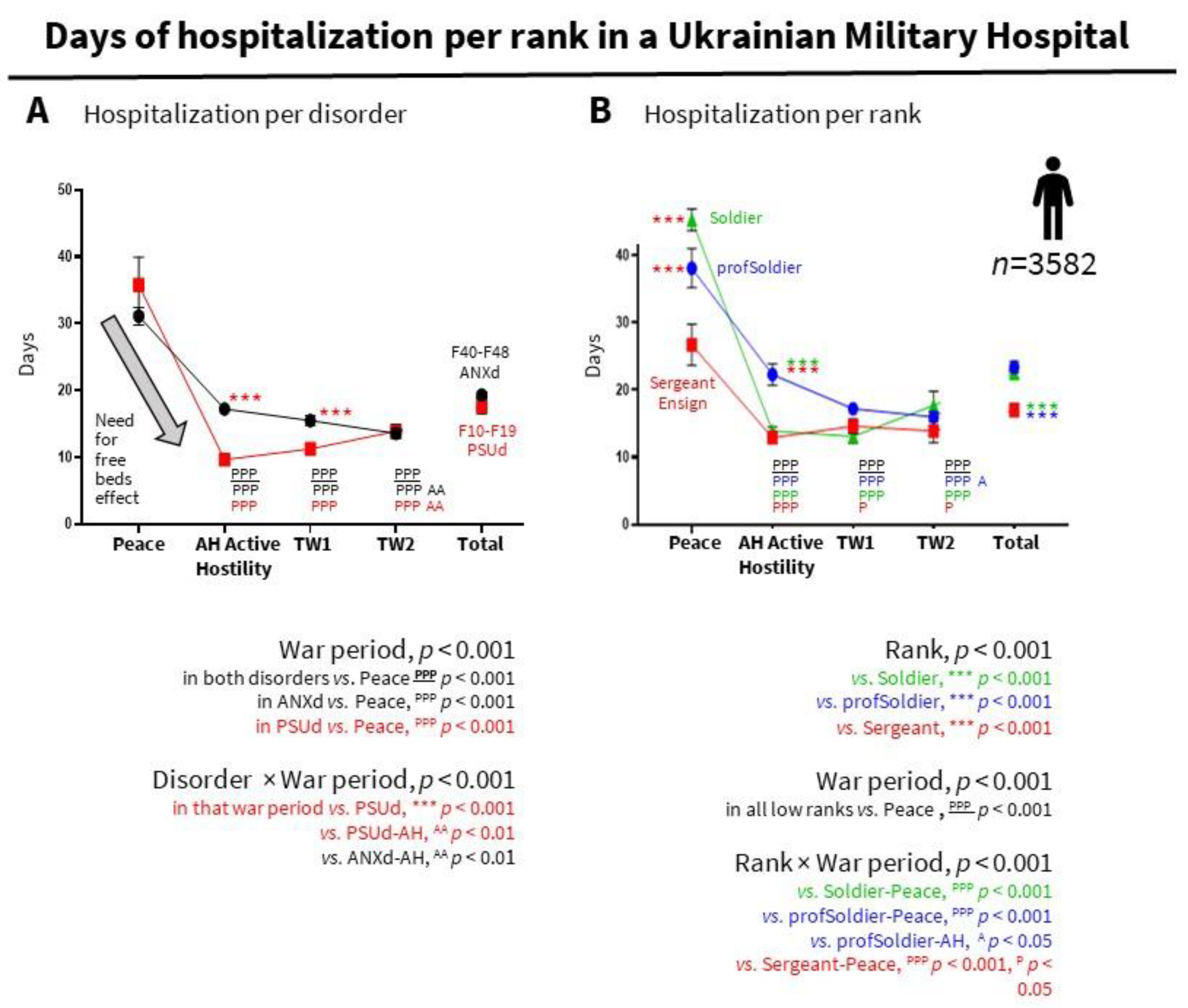
3.6. A ‘Need for Free Beds Effect’ Could Explain Shorter Hospital Stays during Active Conflict and Anticipate Similar Phenomena in the Current War
4. Discussion
5. Conclusions
- The dominance of ANXd, mainly among professional soldiers and high ranks, points to the need for rank-tailored psychological training in skills to reduce the ANXd burden.
- The large number of PSUd in nonprofessional soldiers during wartime dictates the need to strengthen the selection of military personnel, taking into account the tendency to addiction. In the current war, tightening the rules of sobriety in units and up to a ban on the sale of alcoholic beverages in areas where hostilities are taking place is recommended.
- Military operations multiply the hospitalizations in psychiatric hospitals. Admissions are heterogeneous and depend on the military rank (soldiers and professional soldiers spend more time than other low ranks). This is relevant to estimating and planning the need for hospital resources for the current situation where the general population has been recruited for defence and combat.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- OHCHR. Ukraine: Civilian Casualty Update 19 May 2022. Available online: https://www.ohchr.org/en/news/2022/05/ukraine-civilian-casualty-update-19-may-2022 (accessed on 27 June 2022).
- UN Refugee Agency. Ukraine Refugee Situation. 2022. Available online: https://data.unhcr.org/en/situations/ukraine (accessed on 1 August 2022).
- Sidney, C. Displacement in Ukraine: Insights from Survey Data IDMC, Internal Displacement Monitoring Centre. 2022. Available online: https://www.internal-displacement.org/expert-opinion/displacement-in-ukraine-insights-from-survey-data (accessed on 1 August 2022).
- Selyukh, A.; Hurt, A.; Jin, C.H.; Underwood, N. The Ripple Effects of Russia’s War in Ukraine are Changing the World. Available online: https://www.npr.org/2022/05/10/1093066817 (accessed on 27 June 2022).
- Chumachenko, D.; Chumachenko, T. Ukraine war: The humanitarian crisis in Kharkiv. BMJ 2022, 376, o796. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.S.; Erickson, T.B. The new humanitarian crisis in Ukraine: Coping with the public health impact of hybrid warfare, mass migration, and mental health trauma. Disaster Med. Public Health Prep. 2022; advance online publication. [Google Scholar] [CrossRef] [PubMed]
- Darden, J.T. In Ukraine and other conflicts, measuring the human cost is important. It’s also very difficult. The Washington Post. Available online: https://www.washingtonpost.com/politics/2022/03/11/ukraine-casualties (accessed on 27 June 2022).
- Blakey, S.M.; Griffin, S.C.; Grove, J.L.; Peter, S.C.; Levi, R.D.; Calhoun, P.S.; Elbogen, E.B.; Beckham, J.C.; Pugh, M.J.; Kimbrel, N.A. Comparing psychosocial functioning, suicide risk, and nonsuicidal self-injury between veterans with probable posttraumatic stress disorder and alcohol use disorder. J. Affect. Disord. 2022, 308, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Kurapov, A.; Pavlenko, V.; Drozdov, A.; Bezliudna, V.; Reznik, A.; Isralowitz, R. Toward an Understanding of the Russian-Ukrainian War Impact on University Students and Personnel. J. Loss Trauma 2022, 1–8. [Google Scholar] [CrossRef]
- Riad, A.; Drobov, A.; Krobot, M.; Antalová, N.; Alkasaby, M.A.; Peřina, A.; Koščík, M. Mental Health Burden of the Russian–Ukrainian War 2022 (RUW-22): Anxiety and Depression Levels among Young Adults in Central Europe. Int. J. Environ. Res. Public Health 2022, 19, 8418. [Google Scholar] [CrossRef] [PubMed]
- Cricenti, C.; Mari, E.; Barchielli, B.; Quaglieri, A.; Burrai, J.; Pizzo, A.; Lausi, G. Can Emotion Regulation Affect Aggressive Responses? A Study on the Ukrainian–Russian Conflict in a Non-Directly Exposed Sample. Int. J. Environ. Res. Public Health 2022, 19, 6189. [Google Scholar] [CrossRef] [PubMed]
- WHO. ICD-10. Available online: https://www.who.int/standards/classifications/classification-of-diseases (accessed on 25 June 2022).
- The Jamovi Project. Jamovi (Version 1.6) [Computer Software]. 2021. Available online: https://www.jamovi.org (accessed on 1 August 2022).
- Rozanov, V.; Frančišković, T.; Marinić, I.; Macarenco, M.; Letica-Crepulja, M.; Mužinić, L.; Jayatunge, R.; Sisask, M.; Vevera, J.; Wiederhold, B.; et al. Mental health consequences of war conflicts. In Advances in Psychiatry; Javed, A., Fountoulakis, K., Eds.; Springer: Cham, Switzerland, 2019. [Google Scholar] [CrossRef]
- Goldberg, J.; Eisen, S.A.; True, W.R.; Henderson, W.G. A twin study of the effects of the Vietnam conflict on alcohol drinking patterns. Am. J. Public Health 1990, 80, 570–574. [Google Scholar] [CrossRef] [PubMed]
- Schumm, J.A.; Chard, K.M. Alcohol and stress in the military. Alcohol Res. 2012, 34, 401–407. [Google Scholar] [PubMed]
- Alnahhas, H.; Mishori, R.; Heisler, M. Hospitals and healthcare workers must be protected from the waging of war. BMJ 2022, 376, o764. [Google Scholar] [CrossRef] [PubMed]
- Update: Mental health disorders and mental health problems, active component, U.S. Armed Forces, 2016–2020. MSMR 2021, 28, 2–9.
- Haydabrus, A.V. Dynamics of changes in the structure of mental illness among servicemen treated in the psychiatric ward of the military medical clinical center of the northern region. Psychiatry Neurol. Med. Psychol. 2020, 15. [Google Scholar] [CrossRef]
- Inoue, C.; Shawler, E.; Jordan, C.H.; Jackson, C.A. Veteran and military mental health issues. 2021 May 24. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Halperin, E.; Porat, R.; Tamir, M.; Gross, J.J. Can Emotion Regulation Change Political Attitudes in Intractable Conflicts? From the Laboratory to the Field. Psychol. Sci. 2013, 24, 106–111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacobson, I.G.; Ryan, M.A.; Hooper, T.I.; Smith, T.C.; Amoroso, P.J.; Boyko, E.J.; Gackstetter, G.D.; Wells, T.S.; Bell, N.S. Alcohol use and alcohol-related problems before and after military combat deployment. JAMA 2008, 300, 663–675. [Google Scholar] [CrossRef] [PubMed]
- Sharbafchi, M.R.; Heydari, M. Management of Substance Use Disorder in Military Services: A Comprehensive Approach. Adv. Biomed. Res. 2017, 6, 122. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haydabrus, A.; Santana-Santana, M.; Lazarenko, Y.; Giménez-Llort, L. Current War in Ukraine: Lessons from the Impact of War on Combatants’ Mental Health during the Last Decade. Int. J. Environ. Res. Public Health 2022, 19, 10536. https://doi.org/10.3390/ijerph191710536
Haydabrus A, Santana-Santana M, Lazarenko Y, Giménez-Llort L. Current War in Ukraine: Lessons from the Impact of War on Combatants’ Mental Health during the Last Decade. International Journal of Environmental Research and Public Health. 2022; 19(17):10536. https://doi.org/10.3390/ijerph191710536
Chicago/Turabian StyleHaydabrus, Andriy, Mikel Santana-Santana, Yuriy Lazarenko, and Lydia Giménez-Llort. 2022. "Current War in Ukraine: Lessons from the Impact of War on Combatants’ Mental Health during the Last Decade" International Journal of Environmental Research and Public Health 19, no. 17: 10536. https://doi.org/10.3390/ijerph191710536
APA StyleHaydabrus, A., Santana-Santana, M., Lazarenko, Y., & Giménez-Llort, L. (2022). Current War in Ukraine: Lessons from the Impact of War on Combatants’ Mental Health during the Last Decade. International Journal of Environmental Research and Public Health, 19(17), 10536. https://doi.org/10.3390/ijerph191710536






