From Health Campaign to Interpersonal Communication: Does Traditional Diet Culture Hinder the Communication of the Chinese Gongkuai Campaign?
Abstract
:1. Introduction
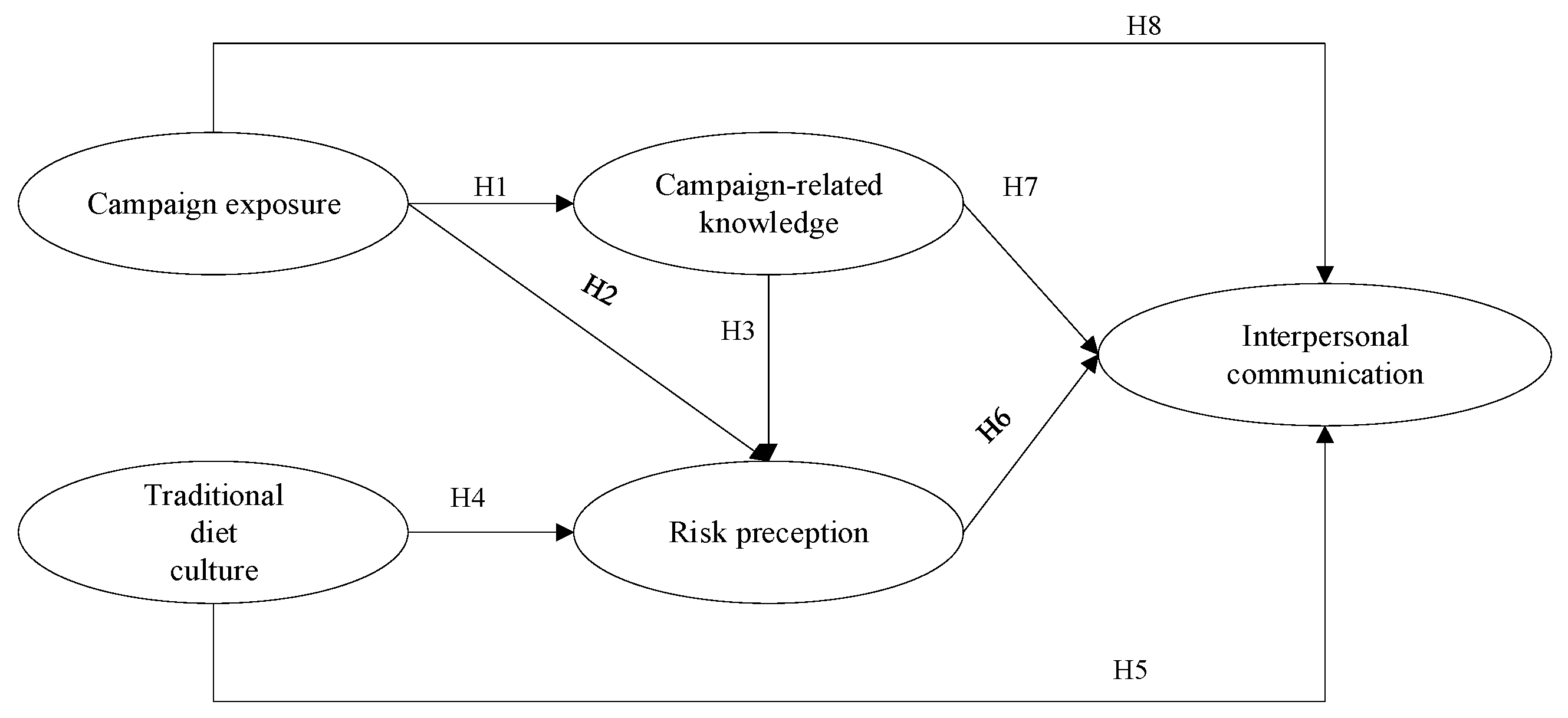
2. Theory and Hypotheses
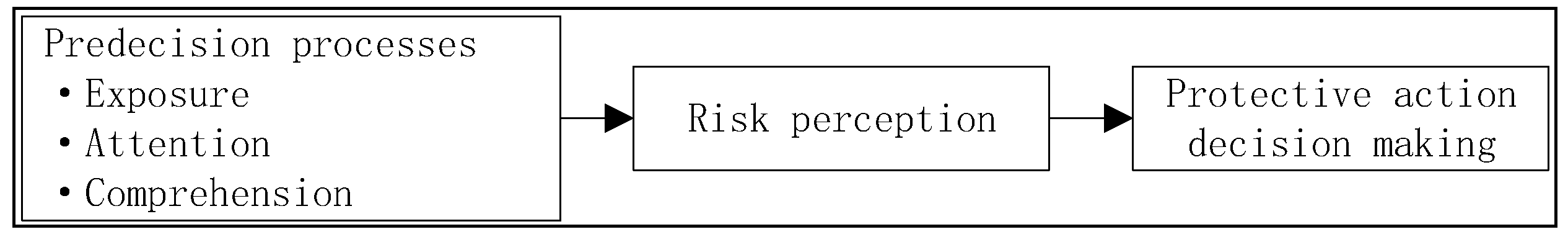
2.1. Interpersonal Communication and Protective Action Decision Model (PADM)
2.2. Campaign Exposure, Campaign-Related Knowledge, and Risk Perception
2.3. The Role of Traditional Diet Culture
2.4. Motivation for Campaign-Generated Interpersonal Communication
3. Research Method
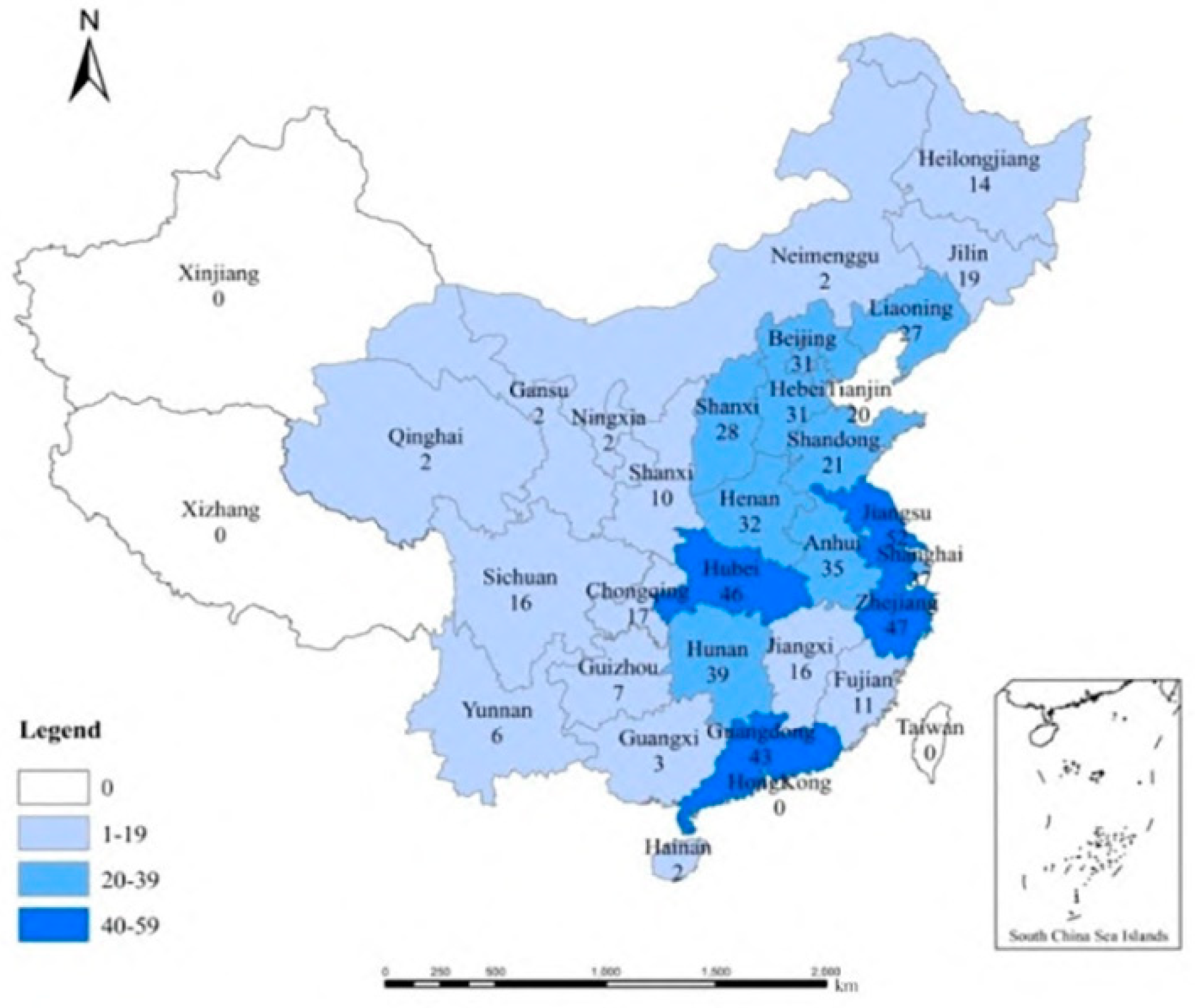
3.1. Data Collection and Samples
3.2. Measures
3.3. Descriptive Statistics and Correlations
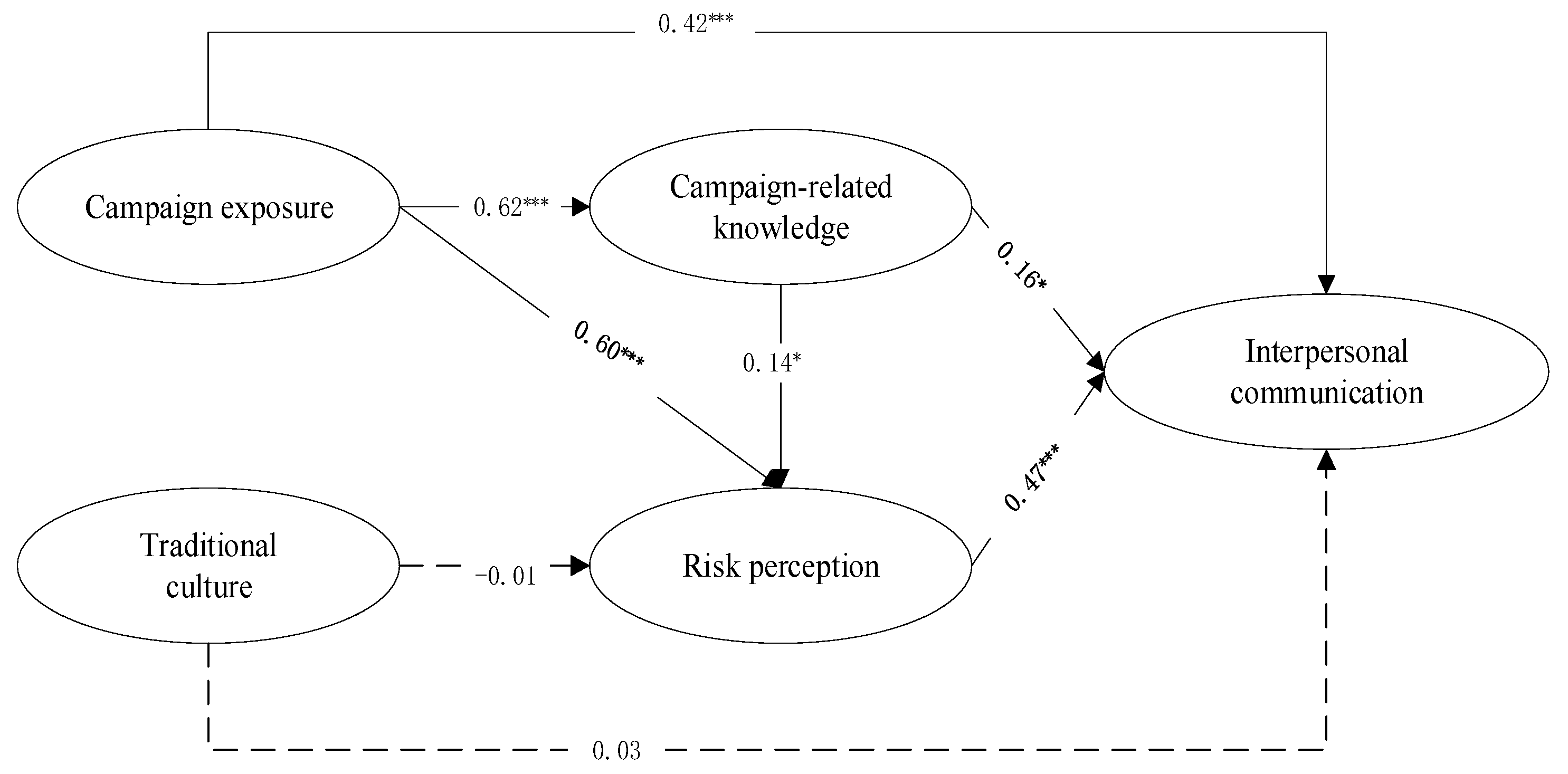
4. Results
4.1. Measurement Model
4.2. Structural Equation Model Analysis
5. Discussion and Implication
5.1. Discussion
5.2. Implications
5.3. Conclusions
6. Limitations and Future Directions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cheng, Y.; Yu, J.; Shen, Y.; Huang, B. Coproducing Responses to COVID-19 with Community-Based Organizations: Lessons from Zhejiang Province, China. Public Adm. Rev. 2020, 80, 866–873. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H. The SARS epidemic in Hong Kong: What lessons have we learned? J. R. Soc. Med. 2003, 96, 374. [Google Scholar]
- Tang, M.Y.L.; Chung, P.H.Y.; Chan, H.Y.; Tam, P.K.H.; Wong, K.K. Recent trends in the prevalence of Helicobacter Pylori in symptomatic children: A 12-year retrospective study in a tertiary centre. J. Pediatr. Surg. 2019, 54, 255–257. [Google Scholar] [CrossRef] [PubMed]
- Tam, K.-P.; Lau, I.Y.-M.; Chiu, C.-Y. Biases in the perceived prevalence and motives of severe acute respiratory syndrome prevention behaviors among Chinese high school students in Hong Kong. Asian J. Soc. Psychol. 2004, 7, 67–81. [Google Scholar] [CrossRef]
- Swierad, E.; Vartanian, L.R.; King, M. The Influence of Ethnic and Mainstream Cultures on African Americans’ Health Behaviors: A Qualitative Study. Behav. Sci. 2017, 7, 49. [Google Scholar] [CrossRef]
- Delport, W.; Merwe, S.W.V.D. The transmission of Helicobacter pylori: The effects of analysis method and study population on inference. Best Pract. Res. Clin. Gastroenterol. 2007, 21, 215–236. [Google Scholar] [CrossRef]
- Leung, W.; Sung, J.; Ling, T.; Siu, K.; Cheng, A. Does the use of chopsticks for eating transmit Helicobacter pylori? Lancet 1997, 350, 31. [Google Scholar] [CrossRef]
- Bagozzi, R.P.; Lee, K.-H.; Van Loo, M.F. Decisions to donate bone marrow: The role of attitudes and subjective norms across cultures. Psychol. Health 2001, 16, 29–56. [Google Scholar] [CrossRef]
- Zhang, J.; Zhao, A.; Ke, Y.; Huo, S.; Ma, Y.; Zhang, Y.; Ren, Z.; Li, Z.; Liu, K. Dietary Behaviors in the Post-Lockdown Period and Its Effects on Dietary Diversity: The Second Stage of a Nutrition Survey in a Longitudinal Chinese Study in the COVID-19 Era. Nutrients 2020, 12, 3269. [Google Scholar] [CrossRef]
- Wang, W.; Yu, N. Coping with a New Health Culture: Acculturation and Online Health Information Seeking Among Chinese Immigrants in the United States. J. Immigr. Minor. Health 2015, 17, 1427–1435. [Google Scholar] [CrossRef]
- Southwell, B.G.; Yzer, M.C. When (and Why) Interpersonal Talk Matters for Campaigns. Commun. Theory 2009, 19, 1–8. [Google Scholar] [CrossRef]
- Jeong, M.; Bae, R.E. The Effect of Campaign-Generated Interpersonal Communication on Campaign-Targeted Health Outcomes: A Meta-Analysis. Health Commun. 2017, 33, 988–1003. [Google Scholar] [CrossRef] [PubMed]
- Lindell, M.K.; Perry, R.W. The Protective Action Decision Model: Theoretical Modifications and Additional Evidence. Risk Anal. 2011, 32, 616–632. [Google Scholar] [CrossRef] [PubMed]
- Southwell, B.; Yzer, M.C. The Roles of Interpersonal Communication in Mass Media Campaigns. Ann. Int. Commun. Assoc. 2007, 31, 420–462. [Google Scholar] [CrossRef]
- Crook, B.; Stephens, K.K.; Pastorek, A.E.; Mackert, M.; Donovan, E.E. Sharing Health Information and Influencing Behavioral Intentions: The Role of Health Literacy, Information Overload, and the Internet in the Diffusion of Healthy Heart Information. Health Commun. 2015, 31, 60–71. [Google Scholar] [CrossRef]
- Yan, J.; Wei, J.; Zhao, D.; Vinnikova, A.; Li, L.; Wang, S. Communicating Online Diet-Nutrition Information and Influencing Health Behavioral Intention: The Role of Risk Perceptions, Problem Recognition, and Situational Motivation. J. Health Commun. 2018, 23, 1–10. [Google Scholar] [CrossRef]
- Lindell, M.K.; Hwang, S.N. Households’ Perceived Personal Risk and Responses in a Multihazard Environment. Risk Anal. 2008, 28, 539–556. [Google Scholar] [CrossRef]
- Lindell, M.K.; Mumpower, J.L.; Huang, S.-K.; Wu, H.-C.; Samuelson, C.D.; Wei, H.-L. Perceptions of protective actions for a water contamination emergency. J. Risk Res. 2016, 20, 887–908. [Google Scholar] [CrossRef]
- Wang, F.; Wei, J.; Huang, S.-K.; Lindell, M.K.; Ge, Y.; Wei, H.-L. Public reactions to the 2013 Chinese H7N9 Influenza outbreak: Perceptions of risk, stakeholders, and protective actions. J. Risk Res. 2016, 21, 809–833. [Google Scholar] [CrossRef]
- Yan, J.; Wei, J.; Ouyang, Z.; Vinnikova, A.; Zhao, D.; Zhang, H. The influence of parents’ information processing on childhood vaccine acceptance after a vaccine crisis in China. Health Risk Soc. 2019, 21, 284–303. [Google Scholar] [CrossRef]
- Tan, A.S.; Lee, C.-J.; Bigman, C. Public support for selected e-cigarette regulations and associations with overall information exposure and contradictory information exposure about e-cigarettes: Findings from a national survey of U.S. adults. Prev. Med. 2015, 81, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Jung, M.; Lin, L.; Viswanath, K. Associations between health communication behaviors, neighborhood social capital, vaccine knowledge, and parents’ H1N1 vaccination of their children. Vaccine 2013, 31, 4860–4866. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.O.; Denham, B.E.; Springston, J.K. Effects of Mass and Interpersonal Communication on Breast Cancer Screening: Advancing Agenda-Setting Theory in Health Contexts. J. Appl. Commun. Res. 2006, 34, 94–113. [Google Scholar] [CrossRef]
- Wang, S.; Wang, J.; Zhao, S.; Yang, S. Information publicity and resident’s waste separation behavior: An empirical study based on the norm activation model. Waste Manag. 2019, 87, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Salmon, C.T. Message Discrimination and the Information Environment. Commun. Res. 1986, 13, 363–372. [Google Scholar] [CrossRef]
- Murdock, M.R.; Rajagopal, P. The sting of social: How emphasizingsocial consequences in warning messages influences perception of risk. J. Mark. A Q. Publ. Am. Mark. Assoc. 2017, 81, 83–98. [Google Scholar] [CrossRef]
- Ferrer, R.A.; Portnoy, D.; Klein, W.M.P. Worry and Risk Perceptions as Independent and Interacting Predictors of Health Protective Behaviors. J. Health Commun. 2013, 18, 397–409. [Google Scholar] [CrossRef]
- Garfin, D.R.; Silver, R.C.; Holman, E.A. The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychol. 2020, 39, 355–357. [Google Scholar] [CrossRef]
- Seo, M.; Matsaganis, M.D. How Interpersonal Communication Mediates the Relationship of Multichannel Communication Connections to Health-Enhancing and Health-Threatening Behaviors. J. Health Commun. 2013, 18, 1002–1020. [Google Scholar] [CrossRef]
- Sudo, A.; Kuroda, Y. Media exposure, interactive health literacy, and adolescents’ susceptibility to future smoking. Int. J. Adolesc. Med. Health 2015, 29, 20150052. [Google Scholar] [CrossRef]
- Perettiwatel, P.; Raude, J.; Sagaonteyssier, L.; Constant, A.; Verger, P.; Beck, F. Attitudes toward vaccination and the H1N1 vaccine: Poor people’s unfounded fears or legitimate concerns of the elite? Soc. Sci. Med. 2014, 109, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Van Der Heide, I.; Uiters, E.; Rademakers, J.; Struijs, J.N.; Schuit, J.; Baan, C.A. Associations among Health Literacy, Diabetes Knowledge, and Self-Management Behavior in Adults with Diabetes: Results of a Dutch Cross-Sectional Study. J. Health Commun. 2014, 19, 115–131. [Google Scholar] [CrossRef] [PubMed]
- Andrews, J.C.; Netemeyer, R.G.; Burton, S.; Moberg, D.P.; Christiansen, A. Understanding Adolescent Intentions to Smoke: An Examination of Relationships among Social Influence, Prior Trial Behavior, and Antitobacco Campaign Advertising. J. Mark. 2004, 68, 110–123. [Google Scholar] [CrossRef]
- Kreuter, M.W.; McClure, S.M. The role of culture in health communication. Annu. Rev. Public Health 2004, 25, 439–455. [Google Scholar] [CrossRef]
- Schwartz, S.H. Universals in the Content and Structure of Values: Theoretical Advances and Empirical Tests in 20 Countries. Adv. Exp. Soc. Psychol. 1992, 25, 1–65. [Google Scholar] [CrossRef]
- Iwelunmor, J.; Newsome, V.; Airhihenbuwa, C.O. Framing the impact of culture on health: A systematic review of the PEN-3 cultural model and its application in public health research and interventions. Ethn. Health 2013, 19, 20–46. [Google Scholar] [CrossRef] [PubMed]
- Kumanyika, S.; Taylor, W.C.; Grier, S.A.; Lassiter, V.; Lancaster, K.J.; Morssink, C.B.; Renzaho, A.M. Community energy balance: A framework for contextualizing cultural influences on high risk of obesity in ethnic minority populations. Prev. Med. 2012, 55, 371–381. [Google Scholar] [CrossRef]
- Panicker, A.; Basu, K.; Chung, C.-F. Changing Roles and Contexts: Symbolic Interactionism in the Sharing of Food and Eating Practices between Remote, Intergenerational Family Members. Proc. ACM Hum.-Comput. Interact. 2020, 4, 1–19. [Google Scholar] [CrossRef]
- E Chapman, G.; Ristovski-Slijepcevic, S.; Beagan, B.L. Meanings of food, eating and health in Punjabi families living in Vancouver, Canada. Health Educ. J. 2010, 70, 102–112. [Google Scholar] [CrossRef]
- Rowe, J. Voices from the Inside: African American Women’s Perspectives on Healthy Lifestyles. Health Educ. Behav. 2010, 37, 789–800. [Google Scholar] [CrossRef]
- Arroyo, A.; Harwood, J. Exploring the Causes and Consequences of Engaging in Fat Talk. J. Appl. Commun. Res. 2012, 40, 167–187. [Google Scholar] [CrossRef]
- Frank, L.B.; Chatterjee, J.S.; Chaudhuri, S.T.; Lapsansky, C.; Bhanot, A.; Murphy, S.T. Conversation and Compliance: Role of Interpersonal Discussion and Social Norms in Public Communication Campaigns. J. Health Commun. 2012, 17, 1050–1067. [Google Scholar] [CrossRef] [PubMed]
- Basu, A.; Dutta, M.J. Sex Workers and HIV/AIDS: Analyzing Participatory Culture-Centered Health Communication Strategies. Hum. Commun. Res. 2009, 35, 86–114. [Google Scholar] [CrossRef]
- Brennan, E.; Durkin, S.J.; Wakefield, M.; Kashima, Y. Why Do Smokers Talk About Antismoking Campaigns? Predictors of the Occurrence and Content of Campaign-Generated Conversations. Health Commun. 2016, 32, 1539–1556. [Google Scholar] [CrossRef] [PubMed]
- Grasso, K.L.; Bell, R.A. Understanding Health Information Seeking: A Test of the Risk Perception Attitude Framework. J. Health Commun. 2015, 20, 1406–1414. [Google Scholar] [CrossRef]
- Helme, D.W.; Noar, S.M.; Allard, S.; Zimmerman, R.S.; Palmgreen, P.; McClanahan, K.J. In-Depth Investigation of Interpersonal Discussions in Response to a Safer Sex Mass Media Campaign. Health Commun. 2011, 26, 366–378. [Google Scholar] [CrossRef]
- Jepsen, A.L. Factors affecting consumer use of the Internet for information search. J. Interact. Mark. 2007, 21, 21–34. [Google Scholar] [CrossRef]
- Fu, H.; Dong, N.; Feng, D.; He, Z.; Tang, S.; Fu, Q.; Feng, Z. To Share or Not to Share: A Cross-Sectional Study on Health Information Sharing and Its Determinants Among Chinese Rural Chronic Patients. J. Health Commun. 2017, 22, 1–8. [Google Scholar] [CrossRef]
- Kim, J.-N.; Grunig, J.E. Problem Solving and Communicative Action: A Situational Theory of Problem Solving. J. Commun. 2011, 61, 120–149. [Google Scholar] [CrossRef]
- Fransen, M.P.; von Wagner, C.; Essink-Bot, M.-L. Diabetes self-management in patients with low health literacy: Ordering findings from literature in a health literacy framework. Patient Educ. Couns. 2012, 88, 44–53. [Google Scholar] [CrossRef]
- Dunlop, S.M.; Kashima, Y.; Wakefield, M. Predictors and Consequences of Conversations About Health Promoting Media Messages. Commun. Monogr. 2010, 77, 518–539. [Google Scholar] [CrossRef]
- Chatterjee, N. AIDS-related information exposure in the mass media and discussion within social networks among married women in Bombay, India. AIDS Care 1999, 11, 443–446. [Google Scholar] [CrossRef] [PubMed]
- Jeong, M.; Tan, A.; Brennan, E.; Gibson, L.; Hornik, R. Talking About Quitting: Interpersonal Communication as a Mediator of Campaign Effects on Smokers’ Quit Behaviors. J. Health Commun. 2015, 20, 1196–1205. [Google Scholar] [CrossRef] [PubMed]
- Parks, M.J.; Slater, J.S.; Rothman, A.J.; Nelson, C.L. Interpersonal Communication and Smoking Cessation in the Context of an Incentive-Based Program: Survey Evidence from a Telehealth Intervention in a Low-Income Population. J. Health Commun. 2015, 21, 125–133. [Google Scholar] [CrossRef]
- Si, H.; Shen, L.; Liu, W.; Wu, G. Uncovering people’s mask-saving intentions and behaviors in the post-COVID-19 period: Evidence from China. Sustain. Cities Soc. 2020, 65, 102626. [Google Scholar] [CrossRef]
- Shi, H.; Wang, S.; Zhao, D. Exploring urban resident’s vehicular PM2.5 reduction behavior intention: An application of the extended theory of planned behavior. J. Clean. Prod. 2017, 147, 603–613. [Google Scholar] [CrossRef]
- Shen, C.; Wang, M.P.; Wan, A.; Viswanath, K.; Chan, S.S.C.; Lam, T.H. Health information exposure from information and communication technologies and its associations with health behaviors: Population-based survey. Prev. Med. 2018, 113, 140–146. [Google Scholar] [CrossRef]
- Karletsos, D.; Hutchinson, P.; Leyton, A.; Meekers, D. The effect of interpersonal communication in tobacco control campaigns: A longitudinal mediation analysis of a Ghanaian adolescent population. Prev. Med. 2020, 142, 106373. [Google Scholar] [CrossRef]
- Gaspar, R.; Luís, S.; Seibt, B.; Lima, M.L.; Marcu, A.; Rutsaert, P.; Fletcher, D.; Verbeke, W.; Barnett, J. Consumers’ avoidance of information on red meat risks: Information exposure effects on attitudes and perceived knowledge. J. Risk Res. 2014, 19, 533–549. [Google Scholar] [CrossRef]
- James, W.L.; Hatten, K.J. Further evidence on the validity of the self-typing paragraph approach: Miles and snow strategic archetypes in banking. Strat. Manag. J. 1995, 16, 161–168. [Google Scholar] [CrossRef]
- Anderson, J.C.; Gerbing, D.W. Structural equation modeling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411–423. [Google Scholar] [CrossRef]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory. Am. Educ. Res. J. 1994, 5, 83. [Google Scholar]
- Yan, J.; Ouyang, Z.; Vinnikova, A.; Chen, M. Avoidance of the Threats of Defective Vaccines: How a Vaccine Scandal Influences Parents’ Protective Behavioral Response. Health Commun. 2020, 36, 962–971. [Google Scholar] [CrossRef] [PubMed]
- Fadyl, J.K. How can societal culture and values influence health and rehabilitation outcomes? Expert Rev. Pharm. Outcomes Res. 2020, 21, 5–8. [Google Scholar] [CrossRef] [PubMed]
| Demographic Characteristic | Frequency | % | |
|---|---|---|---|
| Gender | Male | 317 | 51.3 |
| Female | 301 | 48.7 | |
| Age | Less than 20 | 59 | 9.6 |
| 20–30 | 158 | 25.6 | |
| 31–40 | 188 | 30.4 | |
| 41–50 | 148 | 24.0 | |
| More than 50 | 65 | 10.4 | |
| Education | Senior high school or below | 109 | 17.6 |
| Associate or bachelor’s degree | 318 | 51.5 | |
| Master’s or higher degree | 191 | 30.9 | |
| Monthly Household income | Less than CNY 10,000 | 133 | 21.5 |
| CNY 10,000–15,000 | 208 | 33.6 | |
| CNY 15,001–20,000 | 161 | 26.1 | |
| More than CNY 20,000 | 116 | 18.8 | |
| Residential location | Urban | 257 | 41.6 |
| Suburban | 242 | 39.2 | |
| Rural | 119 | 19.2 | |
| Construct | Item | Measurement | Reference |
|---|---|---|---|
| Campaign exposure (CE) | CE1 | I often browsed or heard information about Gongkuai campaign in the past 2 months | [57,58] |
| CE2 | I often browse or hear information about Gongkuai campaign from traditional sources (e.g., television/radio/newspaper) | ||
| CE3 | I often browse or hear information about Gongkuai campaign from social media sites (e.g., Wechat/Weibo/TikTok) | ||
| Traditional diet culture (TDC) | TDC1 | I believe the shared use of chopsticks is an important traditional diet culture | [5,9] |
| TDC2 | Using serving chopsticks is very different from traditional customs. | ||
| TDC3 | I have a duty to uphold the traditional diet culture of dishes being shared communally | ||
| Campaign-related knowledge (CK) | CK1 | I know Gongkuai campaign policy | [20,59] |
| CK2 | I have knowledge of how to use serving chopsticks | ||
| CK3 | I know many of the negative aspects of not using serving chopsticks | ||
| Risk perception (RP) | RP1 | I worry about the danger of not using serving chopsticks | [13,20] |
| RP2 | It will be dangerous to dine outside if not using serving chopsticks | ||
| RP3 | Not using utensils will negatively influence my future health | ||
| Interpersonal communication (IC) | IC1 | In the past two months, I have had conversation with my family or friends about Gongkuai campaign | [49,58] |
| IC2 | In the past two months, I have had conversations with any relevant person about Gongkuai campaign | ||
| IC3 | In the past two months, I have actively looked for chances to share my knowledge and thoughts about Gongkuai campaign |
| Mean | Standard Deviation | CE | TDC | CK | RP | IC | ||
|---|---|---|---|---|---|---|---|---|
| CE | 3.69 | 0.72 | 1 | 0.83 | ||||
| TDC | 3.02 | 1.20 | −0.03 | 1 | 0.92 | |||
| CK | 3.75 | 0.77 | 0.55 ** | −0.04 | 1 | 0.77 | ||
| RP | 3.63 | 0.72 | 0.60 ** | −0.04 | 0.44 ** | 1 | 0.81 | |
| IC | 3.60 | 0.72 | 0.67 ** | −0.03 | 0.51 ** | 0.69 ** | 1 | 0.79 |
| Construct | Items | Loadings | Cronbach’s Alpha | Composite Reliability | AVE |
|---|---|---|---|---|---|
| Campaign exposure (CE) | CE1 | 0.876 | 0.87 | 0.87 | 0.69 |
| CE2 | 0.837 | ||||
| CE3 | 0.778 | ||||
| Traditional diet culture (TDC) | MC1 | 0.855 | 0.94 | 0.94 | 0.85 |
| MC2 | 0.971 | ||||
| MC3 | 0.914 | ||||
| Campaign-related knowledge (CK) | CK1 | 0.700 | 0.80 | 0.81 | 0.60 |
| CK2 | 0.775 | ||||
| CK3 | 0.833 | ||||
| Risk perception (RP) | RP1 | 0.822 | 0.85 | 0.85 | 0.65 |
| RP2 | 0.809 | ||||
| RP3 | 0.794 | ||||
| Interpersonal communication (IC) | IC1 | 0.771 | 0.83 | 0.84 | 0.63 |
| IC2 | 0.807 | ||||
| IC3 | 0.804 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yan, J.; Ji, J.; Gao, L. From Health Campaign to Interpersonal Communication: Does Traditional Diet Culture Hinder the Communication of the Chinese Gongkuai Campaign? Int. J. Environ. Res. Public Health 2022, 19, 9992. https://doi.org/10.3390/ijerph19169992
Yan J, Ji J, Gao L. From Health Campaign to Interpersonal Communication: Does Traditional Diet Culture Hinder the Communication of the Chinese Gongkuai Campaign? International Journal of Environmental Research and Public Health. 2022; 19(16):9992. https://doi.org/10.3390/ijerph19169992
Chicago/Turabian StyleYan, Jing, Jing Ji, and Lan Gao. 2022. "From Health Campaign to Interpersonal Communication: Does Traditional Diet Culture Hinder the Communication of the Chinese Gongkuai Campaign?" International Journal of Environmental Research and Public Health 19, no. 16: 9992. https://doi.org/10.3390/ijerph19169992
APA StyleYan, J., Ji, J., & Gao, L. (2022). From Health Campaign to Interpersonal Communication: Does Traditional Diet Culture Hinder the Communication of the Chinese Gongkuai Campaign? International Journal of Environmental Research and Public Health, 19(16), 9992. https://doi.org/10.3390/ijerph19169992





