Abstract
Fibromyalgia (FM) is a syndrome that involves chronic pain, fatigue, sleep disturbance and impaired quality of life and daily functioning. In addition to medical and psychological therapies, other therapies including acupuncture and dry needling aim to reduce pain and disability in patients with FM. The aim of this study was to investigate the efficacy of dry needling and acupuncture in patients with FM regarding pain, function and disability in both the short and the long term. MEDLINE, PubMed, SCOPUS and Web of Science databases were systematically searched for randomized controlled trial studies evaluating efficacy data of dry needling or/and acupuncture treatments to improve pain, fatigue, sleep disturbance and impaired quality of life and/or daily function. A qualitative analysis including the methodological quality and a systematic data synthesis was performed. A total of 25 studies addressed the selection criteria. Most studies had an acceptable methodological quality. Four studies assessed the effect of dry needling, and twenty-one studies assessed the effect of acupuncture. In general, both interventions improved pain, anxiety, depression, fatigue, stiffness, quality of sleep and quality of life. However, both techniques were not compared in any study. Acupuncture and dry needling therapies seems to be effective in patients with FM, since both reduced pain pressure thresholds, anxiety, depression, fatigue, sleep disturbances and disability in the short term. It is still required to compare both techniques and their application in the long term.
1. Introduction
Fibromyalgia (FM) is a condition that involves generalized chronic pain [1] associated with fatigue, sleep disturbance, depression and cognitive impairments [2,3]. This disease can affect people at different ages, but FM is most frequently found in middle-aged women [4]. In addition to gender and age, prior family history of FM increases the risk of suffering this condition. Therefore, this suggests a mixed genetic and lifestyle etiology [5], but the exact etiology is still unknown. Previous studies assessed the altered pain perception reporting a chronic and increased pain response to a painful stimulus (hyperalgesia) and pain caused by a stimulus which normally should not cause pain (allodynia) [6,7,8]. Gender differences were found in the intensity, frequency, duration and locations, female patients being more affected than male patients. Although pain perception is conditioned by subjective and personal experiences, these differences between genders could be explained by biologic features related to endogenous pain-relief mechanisms or the influence of gonadal hormones [9].
Some common treatments used for patients with FM to reduce fatigue, sleep disturbance and psychological and physical symptoms are psychological treatments (e.g., cognitive behavioral therapy) [10], aerobic exercise [10], and pharmacological treatment (e.g., amitriptyline, anticonvulsants, noradrenaline and serotonin reuptake inhibitors) [11]. However, these pharmacological options were demonstrated to be not effective at all [12] and to present adverse effects that make their use difficult in the long term, and a multidimensional approach including patient education, behavioral therapy, exercise and pain management is recommended [13]. Dry needling and acupuncture are complementary treatment options in this multidimensional approach that could be potentially used in the long term for reducing pain and disability in this population that have been widely studied in several conditions.
Dry needling is a therapeutic procedure that consists of a needle insertion with any pharmacological substance into a myofascial trigger point (MTrP) to inactivate it and reduce the pain [14]. This mechanism has been widely studied in several conditions (e.g., acute and chronic low back pain, myofascial pain syndrome and whiplash) [15] and showed a similar response to lidocaine injections in the treatment of MTrP symptoms (e.g., pain relief, increased range of movement and improved quality of life) [16]. On the other hand, acupuncture is a complementary and alternative medicine treatment that has been used to treat different conditions, including chronic pain, for over three millennia in China [17] and is used by up to 91% of the patients with FM [18]. Both techniques could base their analgesic effect on the neurotransmitter and hormone regulation on the central nervous system by stimulating nerve fibers (e.g., A delta afferences) and producing an activation in the cascade of pain-modulating endorphins, serotonin and noradrenaline, which contributes to analgesia [19].
Although dry needling and acupuncture are applied to decrease pain in different musculoskeletal conditions and several systematic reviews assessed the efficacy of acupuncture in patients with FM during the last 10 years [13,18,20,21], the inclusion of dry needling assessment for the management of pain, function and disability in patients with FM was not considered in any prior systematic review. Therefore, the current systematic review with meta-analysis evaluates the efficacy of both dry needling and acupuncture to improve pain, function and disability in the FM population.
2. Materials and Methods
2.1. Study Design
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [22]. The international OSF Registry registration link for this study is https://doi.org/10.17605/OSF.IO/Y4627 (registered on 25 October 2020).
2.2. Data Sources
Electronic literature searches were conducted on MEDLINE, PubMed, SCOPUS and Web of Science databases from their inception to 22 May 2022. Bibliographical search strategies were conducted with the assistance of an experienced health science librarian and FM management following the guidelines described by Greenhalgh [23]. Search strategies were based on a combination of Mesh terms and keywords following the PICO (Population, Intervention, Comparison, Outcome) question:
Population: Adults (older than 18 years old) with FM;
Intervention: Use of dry needling and/or acupuncture;
Comparator: Active control interventions;
Outcomes: Pain (e.g., subjective pain perception, pressure pain thresholds and/or pain questionnaires), Severity of the condition (e.g., fibromyalgia, anxiety, fatigue and/or depression severity indexes), and/or quality of life (e.g., quality of life, sleep disturbances and/or health questionnaires).
An example of the search strategy (PubMed database) is as follows Box 1:
Box 1. Example of the search strategy (PubMed database).
Filters: [Title/Abstract] |
#1 Fibromyalgia [MeSH]; #2 Fatigue Syndrome, Chronic [MeSH]; #3 Tender Points |
#4 #1 OR #2 OR #3 |
#5 Needling, Dry [MeSH]; #6 Acupuncture [MeSH]; #7 Acupuncture Therapy [MeSH]; #8 Acupuncture Analgesia [MeSH] |
#9 #5 OR #6 OR #7 OR #8 |
#10 Pain [MeSH]; #11 Chronic Pain [MesH]; #12 Pain Perception [MeSH]; #13 Pain Threshold [MeSH]; #14 Anxiety [MeSH]; #15 Depressive Disorder [MeSH]; #16 Fatigue [MeSH]; #17 Quality of Life [MeSH]; #18 Sleep [MeSH]; #19 Sleep Disorders |
#20 #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 |
2.3. Study Eligibility Criteria
Studies were eligible for inclusion if they evaluated the application of dry needling and/or acupuncture in adult patients with FM for the pain, disability, function and/or quality of life management and were published during the last 10 years in the English, Portuguese or Spanish languages. Animal studies, cadaveric studies, published proceedings, abstracts and studies with a sample size lower than 30 subjects were excluded for review. All included studies must have obtained approval from an ethics committee or institutional review board.
2.4. Study Appraisal and Synthesis Methods
The Mendeley Desktop v.1.19.4 for Mac OS (Glyph & Cog, LLC 2008) program was used to insert the search hits from the databases. First, the duplicates were removed. Second, title/abstracts of the articles were screened for potential eligibility by two authors. Third, the full text was analyzed to identify potentially eligible studies. Reviewers were required to agree in the inclusion/exclusion decision. In case of discrepancy between the initial two reviewers, a third reviewer participated in the process to reach the consensus for including the study in the systematic review or not.
A standardized data extraction form containing questions on study design, sample size, objectives, interventions, outcomes assessed, results and conclusions was used, following the main structure reported by Shokraneh et al. [24]. The methodological quality of the included studies was assessed using the PEDro scale, which consists of a checklist of 10 scored yes-or-no questions pertaining to the internal validity and the statistical information provided. Reported cut-offs for the scale interpretation are as follows: 0–3 score was interpreted as poor quality; 4–5 as fair quality; and 6–10 as high quality [25].
2.5. Level of Evidence
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used to evaluate the level of evidence [26]. The level of evidence was classified as high, moderate, low or very low based on study limitations, indirectness of evidence, unexplained heterogeneity, imprecision of the results and high probability of publication bias [27]. High-quality evidence was scored when all items were negative; moderate quality was scored when one item included serious risk, low quality was scored if two items showed serious risk or one item showed very serious risk; or very low quality was scored when three or more items had serious risk or two or more had very serious risk. This process was also performed by two authors, with the participation of a third one if disagreement occurred.
2.6. Data Analysis
Data analysis was performed with Review Manager statistical software (RevMan version 5.3). Data synthesis was presented by groups according to comparative groups, such as sham/control/placebo; manual therapy or other physical therapy intervention; and by follow-up, such as short- (0 to 3 months) and mid-term (>3months to <6 months), since long-term (≥6 months) data were not available. No other subgroup analysis was prespecified a priori.
Data extraction for the data analysis included sample size, means and standard deviations of the outcomes. When the trial reported standard errors, they were converted to standard deviations. Mean and standard deviations were estimated from graphs when needed. If data were expressed as median and interquartile range, they were converted to mean and standard deviation as needed [28].
The between-groups mean difference (MD) with the 95% confidence interval (CI) was calculated for those outcomes assessed with the same instrument, e.g., pain intensity and pressure pain thresholds. Between-groups mean differences were converted to SMD when different instruments were used for the same outcome, e.g., pain-intensity. A random-effects model was used to determine the effect sizes (SMD). An effect size (SMD) of ≥0.8 was considered large, between 0.5 and 0.8 was considered moderate and between 0.2 and 0.5 was considered small [29]. p-values < 0.05 were considered statistically significant.
Finally, when two subgroups included the same intervention, e.g., dry needling, the sample size was adjusted by dividing the sample size as the Cochrane textbook recommends for avoiding duplication in the overall effect [30].
The I2 statistic was applied to determine the heterogeneity between the included trials. We used the following interpretation: 0–40% represented no relevant heterogeneity; 30–60% represented moderate heterogeneity; 50–90% suggested substantial heterogeneity; and 75–100% suggested considerable heterogeneity [31].
3. Results
3.1. Study Selection
The electronic searches identified 695 potential studies for review. After removing 214 duplicated studies, 481 studies remained. Four hundred forty-six (n = 446) studies were excluded based on examination of their titles or abstracts, leaving 35 articles for full-text analysis. Eleven articles were excluded because they were not published in English or Spanish languages (n = 8), were protocols (n = 1) or had a case series design (n = 2) or retrospective observational design (n = 1). A total of twenty-four studies were included in this systematic review [6,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54]. The included articles investigated dry needling (n = 4) or acupuncture (n = 20), but none compared both techniques directly in the same study (Figure 1).
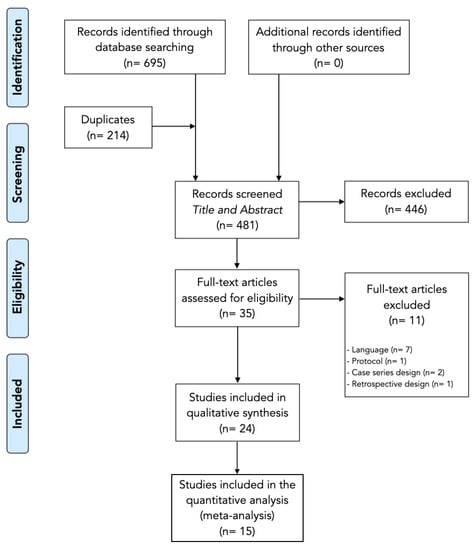
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Flowchart.
3.2. Methodological Quality Assessment
The methodological quality scores measured using the PEDro scale ranged from 5 to 9 (mean: 6.8; SD: 1.1) out of a maximum of 10 points (Table 1). The most consistent flaws were the blinding of all therapists administering the therapy (n = 22 studies out of 25), the blinding of the subjects to discriminate if they had or did not have the treatment (n = 19 out of 25), the concealed allocation (n = 10 out of 25) and the blinding of all assessors who measured at least one key outcome (n = 10 out of 25).

Table 1.
Methodological Quality Assessment using PEDro Scale of the Included Studies.
Overall, most of the studies specified the eligibility criteria (n = 25), allocated the subjects randomly to the groups (n = 23), had balanced group at baseline regarding the most important prognostic indicators (n = 21), obtained data from more than 85% of the subjects initially allocated in the groups (n = 20), participants received the treatment or control condition as allocated (n = 18), statistical comparisons between groups were reported (n = 25) and both point measures and measures of variability provided (n = 25). The methodological quality of studies assessing dry needling was higher (mean: 7.2; SD: 1.7) than that of acupuncture (mean: 6.6; SD: 1.0).
3.3. Dry Needling
Table 2 summarizes the four studies investigating the efficacy of dry needling in patients with FM. Just one study applied the technique in Tender Points (TP) [36] while three applied dry needling in MTrPs [6,42,50]. Comparative interventions selected for these studies were their ordinary medical treatment [30], taping applications [42], manual myofascial release techniques [6], and Transcutaneous Electrical Nerve Stimulation (TENS) [50]. The included studies had a total sample size of 312 patients with FM (35 men and 277 women).

Table 2.
Data Synthesis of the Studies applying Dry Needling in Patients with Fibromyalgia.
Although pain was a common outcome in all the included studies [6,36,42,50], the measurement instruments were not consistent in all the designs. Visual Analogue Scale (VAS) of pain was used in two studies [36,50], Pain Pressure Thresholds (PPTs) were reported in three of the studies for both TPs [36] and MTrPs [6,42] and McGill Pain Questionnaire and myalgic score in just one study [30]. In addition to pain outcomes, quality of life was assessed in two studies, including questionnaires, sleep quality, impact of fibromyalgia and fatigue [6,36]; psychological outcomes including depression and anxiety were assessed in one study [6]; spinal mobility was assessed in one study [42]; and finally, autonomic function including heart rate variability, galvanic skin response, oxygen saturation (SpO2) and photoplethysmography was assessed in one study [50].
In general, dry needling is shown to induce improvements in short-term subjective pain perception, pain pressure thresholds, mobility, fatigue, quality of life, physical function, physical role, general health, vitality, social function, emotional role and mental health.
3.4. Acupuncture
Twenty studies investigated the effects of acupuncture in patients with FM (Table 3). In the final qualitative analysis, four quasi-experimental studies [32,34,43,51], one experimental effectiveness comparative study [49] and sixteen controlled trials (of which fifteen were randomized [33,35,37,38,39,41,44,45,46,47,48,52,53,54], one non-randomized [40] and two double-blinded [38,41]) were included.

Table 3.
Data Synthesis of the Studies applying Acupuncture in Patients with Fibromyalgia.
This study selection compared acupuncture with dietary therapy with and without acupuncture [33,53], somatic and abdominal acupuncture [34], with scalp acupuncture [35,37], with moxibustion [37,40], with music and/or vibratory therapy [39], electroacupuncture [40], simulated acupuncture [46], patients’ education [47], TENS [48,49], core stability training [46] and physiotherapy [54]. However, the most selected comparator group was the application of sham acupuncture [37,38,41,44,45,46]. Most of the total participants (n = 1497) were women (n = 1481). Just two studies included a male sample (n = 16) [38,51].
The acupuncture points most commonly treated were PC-6 (Neiguan), LI-4 (Hegu), GB-34 (Yanglingquan), SP-6 (Sanyinjiao), Du-14 (Da Zhui), Si- 3 (Houxi), Si-4 (Wangu), Si-15 (Jian Zhong Shu), Li-4 (He Gu), Li-11 (Qu Chi), H-7 (Shen Men), P-6 (Nei Guan), Ren-6 (Qihai), Liv-3 (Tai Chong), St-36 (Zu San Li), LR-3 (Taichong), UB-11 (Tianzhu), UB-12 (Fengmen), UB-13 (Feishu), UB-14 (Jueyinshu), GB-21 (Jianjing), UB-62 (Shenmai), UB-64 (Jinggu), UB-65 (Shugu) and Sp-6 (San Yin Jiao) [32,33,34,35,37,38,39,40,41,43,44,45,46,47,48,49,51,54].
The most assessed outcomes were the effect of acupuncture on pain (seventeen studies) measured by using a VAS [32,33,34,35,37,38,39,41,43,44,45,46,48,49,54], the McGill Questionnaire [49], PPTs [40,48], the Pain Catastrophizing Scale [51], the Pain Detect Questionnaire [51] or the Wong-Baker Faces Pain Scale [34], and the effect on fibromyalgia severity (seventeen studies) was assessed by the Fibromyalgia Impact Questionnaire (FIQ) or the number of tender points [32,33,34,35,37,39,41,42,43,44,46,47,48,49,51,52,53,54]. Thus, psychological features (e.g., anxiety and depression) were assessed in seven studies [34,41,44,46,48,54], biomarkers in one study [43], balance in one study [52] and fatigue in four studies [44,47,52,53].
In general, acupuncture and scalp acupuncture showed to be effective in the treatment of fibromyalgia for reducing pain and disability in the short term if combined with other treatments, reducing the adverse effects and treatment costs. Although the placebo effect seems to play a relevant role in these improvements since sham acupuncture demonstrated significant reduction in pain and disability, real treatment seems to be more effective.
3.5. Meta-Analysis Results
3.5.1. Pain Intensity
Needle interventions exhibited an overall significant effect (MD −1.18, 95% CI −1.91 to −0.45; p = 0.002 Z = 3.15; SMD −0.55, 95% CI −0.89 to −0.21, N = 1033, n = 15 trials) for reducing pain after the intervention to 3 months follow-up vs. a comparison group but with substantial heterogeneity (I2 = 85%) between the trials (Figure 2). A significant effect was found in the dry needling subgroup (MD −2.36, 95% CI −3.27 to −1.46, p = 0.003, I2 = 78%; SMD −1.20, 95% CI −1.66 to −0.75, N = 322, n = 4 trials) but not for acupuncture (MD −0.70, 95% CI −1.54 to −0.14, p = 0.10, I2 = 84%; SMD −0.30, 95% CI −0.65 to −0.06, N = 711, n = 11 trials). Testing for subgroup differences showed significant differences between groups (p = 0.0008, I2 = 85.6%). The funnel plot did not present potential publication bias.
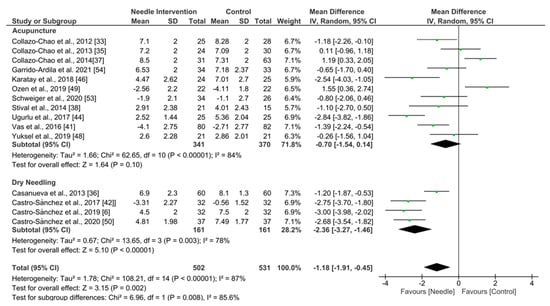
Figure 2.
Forest plot for Pain Intensity after 0–3 months.
Acupuncture exhibited an overall nonsignificant effect (MD −0.56, 95% CI −1.72 to 0.61; p = 0.35 Z = 0.94; SMD −0.26, 95% CI −0.82 to 0.29, N = 174, n = 3 trials) for reducing pain after 3 to 6 months of follow-up vs. a comparison group but with substantial heterogeneity (I2 = 70%) between the trials (Figure 3).
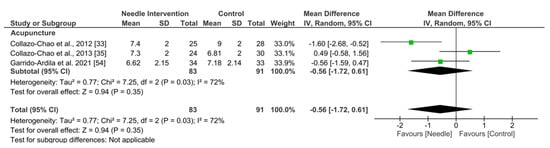
Figure 3.
Forest plot for Pain Intensity: 3 to 6 months.
Acupuncture exhibited an overall nonsignificant effect (MD −0.86, 95% CI −1.78 to 0.07; p = 0.07 Z = 1.82; SMD −0.42, 95% CI −0.88 to 0.04, N = 423, n = 35trials) for reducing pain after 6 months follow-up or more vs. a comparison group but with substantial heterogeneity (I2 = 81%) between the trials (Figure 4).
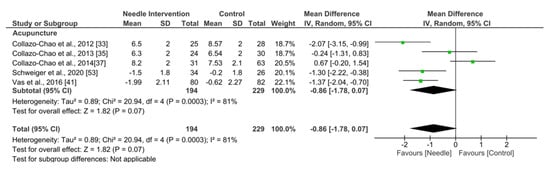
Figure 4.
Forest plot for Pain Intensity: +6 months.
3.5.2. Fibromyalgia Impact Questionnaire
Needle interventions exhibited an overall nonsignificant effect (MD −6.19, 95% CI −13.67 to 1.29; p = 0.10 Z = 1.62; SMD −0.36, 95% CI −0.77 to 0.05, N = 817, n = 11 trials) for FIQ after the intervention to 3 months follow-up vs. a comparison group but with substantial heterogeneity (I2 = 87%) between the trials (Figure 5). A significant effect was found in the dry needling subgroup (MD −16.03, 95% CI −28.20 to −3.86, p = 0.010, I2 = 73%; SMD −0.75, 95% CI −1.22 to −0.28, N = 184, n = 2 trials) but not for acupuncture (MD −0.70, 95% CI −1.54 to −0.14, p = 0.10, I2 = 84%; SMD −0.26, 95% CI −0.75 to 0.22, N = 633, n = 9 trials). Testing for subgroup differences did not show significant differences between groups (p = 0.11, I2 = 60.2%). The funnel plot did not present potential publication bias.
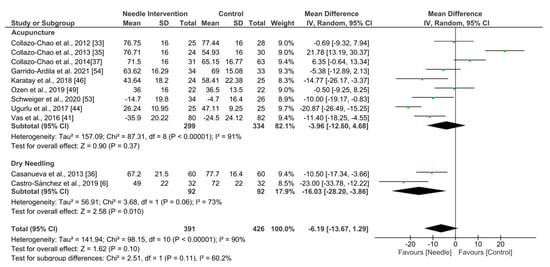
Figure 5.
Forest plot for FIQ after 0–3 months.
Acupuncture exhibited an overall nonsignificant effect (MD −4.08, 95% CI −18.08 to 9.93; p = 0.57 Z = 0.57; SMD −0.25, 95% CI −1.11 to 0.61, N = 107, n = 2 trials) for FIQ after 3 to 6 months follow-up vs. a comparison group but with substantial heterogeneity (I2 = 80%) between the trials (Figure 6).
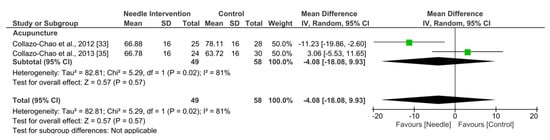
Figure 6.
Forest plot for FIQ: 3–6 months.
Acupuncture exhibited an overall nonsignificant effect (MD −7.57, 95% CI −14.92 to −0.22; p = 0.04 Z = 2.02; SMD −0.44, 95% CI −0.85 to −0.02, N = 423, n = 5 trials) for FIQ after 6 months or more follow-up vs. a comparison group but with substantial heterogeneity (I2 = 75%) between the trials (Figure 7).
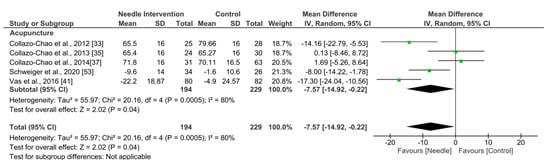
Figure 7.
Forest plot for FIQ after +6 months.
3.5.3. Sleeping/Resting Quality
Needle interventions exhibited an overall nonsignificant effect (SMD −0.38, 95% CI −0.78 to 0.02, N = 534, n = 6 trials) for sleep or rest after the intervention to 3 months follow-up vs. a comparison group but with substantial heterogeneity (I2 = 80%) between the trials (Figure 8). A significant effect was found in the dry needling subgroup (SMD −0.51, 95% CI −0.81 to −0.22, p = 0.0006, N = 184, n = 2 trials) but not for acupuncture (SMD −0.31, 95% CI −0.93 to 0.30, p = 0.32, I2 = 86%, N = 350, n = 4 trials). Testing for subgroup differences did not show significant differences between groups (p = 0.57, I2 = 0%).
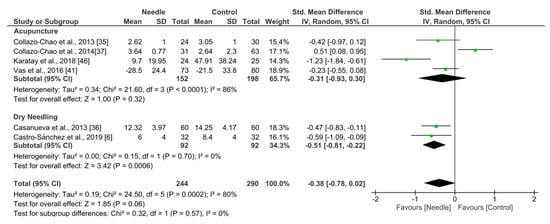
Figure 8.
Forest plot for Sleeping Quality after up to 3 months.
Acupuncture exhibited an overall nonsignificant effect (SMD −0.25, 95% CI −1.30 to 0.79, N = 107, n = 2 trials) for improving sleep after 3 to 6 months follow-up vs. a comparison group but with substantial heterogeneity (I2 = 86%) between the trials (Figure 9).
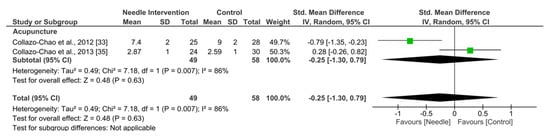
Figure 9.
Forest plot for Sleeping Quality after 3–6 months.
Acupuncture exhibited an overall nonsignificant effect (SMD −0.31, 95% CI −0.82 to 0.21, N = 423, n = 4 trials) for improving sleep after 6 months or more follow-up vs. a comparison group but with substantial heterogeneity (I2 = 81%) between the trials (Figure 10).
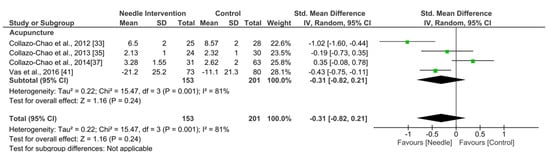
Figure 10.
Forest plot for Sleeping Quality after +6 months.
3.5.4. Depression
As shown in Figure 8, needle interventions exhibited an overall nonsignificant effect (SMD −0.52, 95% CI −0.90 to −0.14, p = 0.007, N = 512, n = 6 trials) for depression after the intervention to 3 months follow-up vs. a comparison group but with substantial heterogeneity (I2 = 76%) between the trials (Figure 11). A significant effect was found in the acupuncture subgroup (SMD −0.68, 95% CI −1.31 to −0.06, N = 328, n = 4 trials) and for dry needling (SMD −0.29, 95% CI −0.58 to 0.00, N = 184, n = 2 trials). Testing for subgroup differences did not show significant differences between groups (p = 0.26, I2 = 21.1%).
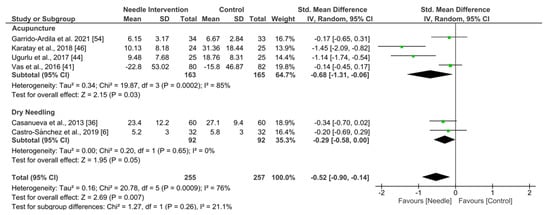
Figure 11.
Forest plot for Depression.
3.5.5. Pressure Pain Threshold
Needle interventions exhibited an overall nonsignificant effect (SMD 0.81, 95% CI −0.60 to 1.01, p < 0.00001, N = 406, n = 4 trials) for PPT after the intervention to 3 months follow-up vs. a comparison group but with substantial heterogeneity (I2 = 0%) between the trials (Figure 12).
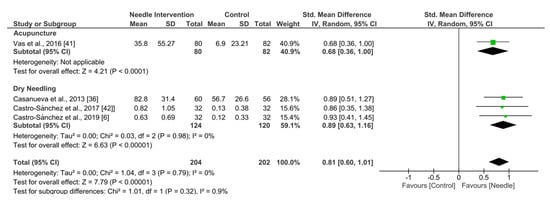
Figure 12.
Forest plot for PPTs.
3.6. Level of Evidence
The risk of bias, inconsistency of the results, indirectness of evidence, imprecision of results and publication bias for determining the level of evidence according to GRADE assessment are detailed in Table 4. The serious/very serious inconsistency of the results (heterogeneity) downgraded the evidence level of dry needling and acupuncture to low or moderate for most of the outcomes assessed, except for the pressure pain threshold in the short-term (with moderate to high quality evidence, especially for dry needling).

Table 4.
GRADE Evidence.
4. Discussion
The main findings of this meta-analysis were that dry needling could induce a short-term improvements in pain, quality of life, vitality, social function, psychological and severity in patients with FM in comparison with other techniques (e.g., manual myofascial release, cross tape) and that acupuncture, if combined with other treatments, is also an effective technique to reduce the ingestion of analgesics and to improve pain perception, quality of life, pain perception, depression and anxiety from the short-term to up to 12 months. Recent studies highlighted the importance of these outcomes in FM severity [55,56,57,58,59,60,61,62,63]. However, we could not find any study comparing the effectiveness of both techniques within the same research. Although the blinding process in studies including needling techniques is not always possible, the studies included in this review did not consider important methodological aspects regarding allocation concealing, the representative sample size or the inclusion of a proper comparator group, furthering the blinding of therapists, patients and assessors. Therefore, future studies should consider reducing methodological flaws including a greater patient recruitment to correct the patients lost during follow-up, especially in those with large follow-up times, and the inclusion of a blinded assessor to perform the measurements.
Although this is not the first meta-analysis comparing the application of dry needling and acupuncture for reducing pain and disability in patients with FM [64], the existing literature included a minor number of articles (including 14 studies for qualitative synthesis and 8 in the quantitative synthesis) and outcomes (i.e., FIQ, PPT and quality of life) in their analyses compared with this one, despite all types of invasive techniques being compared in their analyses.
One likely reason that could explain the limited number of studies applying dry needling in this population could be that dry needling focuses on MTrPs rather than tender points. MTrPs are defined as hyperirritable spots in skeletal muscles that are associated with hypersensitive palpable and painful nodules in a taut band that can induce referred pain, tenderness, motor dysfunction and autonomic phenomena, probably caused by the ischemia and hypoxia produced by the capillary vessels’ compression in these taut bands, and producing peripheral sensitization [65]. Low blood oxygen levels result in a significative pH reduction, an activation of acid-sensing ion channel receptors, acetylcholinesterase inhibition, ATP stimulation, bradykinin, tumor necrosis factor alfa, interleukins, serotonin, noradrenaline, P substance and calcitonin gen-related peptide [66]. On the other hand, tender points were defined by the American College of Rheumatology assessing the hypersensitivity of 18 specific locations to confirm the clinical diagnosis of FM [67].
Based on available literature to date, we found that dry needling induces a global subjective, pain, quality of life and disability improvement in the short-term up to 6 weeks after the treatment [36,50], reporting better results than TENS [50], manual myofascial release treatment [6] and cross tape for all the measured outcomes, except spinal mobility after cross tape treatment [42]. However, further research is needed to confirm these findings due to the lack of studies, the limited comparator groups and the limited follow-up time.
We also found that acupuncture is also an effective and safe tool for managing patients with FM if combined with other therapies (e.g., their usual medication or dietary therapy). Collazo-Chao et al. [32] reported a decrease in the analgesic intake, further improving disability, sleep quality and intensity of pain. All the acupuncture techniques assessed demonstrated similar results (e.g., somatic, abdominal and scalp) and agreed with these positive effects. However, there is enough evidence proposed by Webber et al. [39], Ugurlu et al. [44], Zucker et al. [45] and Karatay [46] to state the substantial role of the placebo effect, even if the verum acupuncture showed better results than sham acupuncture [41]. Further studies could compare the changes in serum serotonin and substance P levels both in the application of dry needling and acupuncture to explain analgesic mechanisms differences depending on the application procedures [46]. These conclusions must be interpreted carefully due to the methodological flaws found in these studies since most of them had no comparator groups or the group assignation was not randomized.
None of the studies assessed in the meta-analysis conducted by Deare et al. [18] nor Yang et al. [13] were included in this systematic review due to the publication date or the sample size. However, our conclusions are consistent with all the previous systematic reviews [13,18,21] since they reported low-to-moderate-level evidence that, compared with no treatment and standard therapy, acupuncture improves pain and stiffness in people with FM and moderate-level evidence that the effect of acupuncture does not differ from sham acupuncture for reducing FM symptoms. Thus, the methodological quality flaws that we found in this study are similar to those reported in these prior systematic reviews, this being the main reason for the level of evidence weakness.
Limitations
Finally, there are some limitations of the current systematic review. First, we have only included articles written in the English or Spanish language, so we have discarded some relevant published studies in other languages, such as Chinese, with a high number of potentially relevant acupuncture studies. Furthermore, we did not include those studies which were accepted but unpublished. Secondly, the limited number of studies assessing dry needling in FM populations as well the inclusion of quasi-experimental acupuncture studies with no comparative group in this review are the main reason to advise a careful interpretation of our conclusions. Further research with proper comparators and blinding is needed to reinforce to recommend the use of dry needling or acupuncture in patients with FM.
5. Conclusions
Due to the lack of studies assessing dry needling and the methodological quality flaws of the studies assessing acupuncture, this systematic review should be interpreted carefully. Overall, there is a low-to-moderate-quality level of evidence that suggests that dry needling is effective for improving pain, disability and quality of life in the short term (up to 6 weeks). The same level of evidence supports acupuncture as an effective complementary treatment to medication and exercise for improving FM severity and symptoms including pain, sleep quality, quality of life, depression, anxiety and fatigue. We did not find any research comparing both techniques in the same study. Further research is needed considering the inclusion of a proper comparator group, larger sample sizes and patient, therapist and/or assessor blinding, if possible, to make more consistent recommendations.
Author Contributions
Conceptualization, all authors; methodology, all authors; software, all authors; validation, all authors; formal analysis, all authors; investigation, all authors; resources, all authors; data curation, all authors; writing—original draft preparation, J.A.V.-C.; writing—review and editing, all authors; visualization, all authors; supervision, G.P.-M.; project administration, J.A.V.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data derived from this study are presented in the text.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.A.; Goldenberg, D.L.; Häuser, W.; Katz, R.L.; Mease, P.J.; Russell, A.S.; Russell, I.J.; Walitt, B. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin. Arthritis Rheum. 2016, 46, 319–329. [Google Scholar] [CrossRef]
- Clauw, D.J. Fibromyalgia: A clinical review. JAMA 2014, 311, 1547–1555. [Google Scholar] [CrossRef] [PubMed]
- Langhorst, J.; Klose, P.; Musial, F.; Irnich, D.; Häuser, W. Efficacy of acupuncture in fibromyalgia syndrome–A systematic review with a meta-analysis of controlled clinical trials. Rheumatology 2010, 49, 778–788. [Google Scholar] [CrossRef] [PubMed]
- Fitzcharles, M.A.; Ste-Marie, P.A.; Goldenberg, D.L.; Pereira, J.X.; Abbey, S.; Choinière, M.; Ko, G.; Moulin, D.E.; Panopalis, P.; Proulx, J.; et al. 2012 Canadian Guidelines for the diagnosis and management of fibromyalgia syndrome: Executive summary. Pain Res. Manag. 2013, 18, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Neumann, L.; Buskila, D. Epidemiology of fibromyalgia. Curr. Pain Headache Rep. 2003, 7, 362–368. [Google Scholar] [CrossRef]
- Castro Sánchez, A.M.; García López, H.; Fernández Sánchez, M.; Pérez Mármol, J.M.; Aguilar-Ferrándiz, M.E.; Luque Suárez, A.; Matarán Peñarrocha, G.A. Improvement in clinical outcomes after dry needling versus myofascial release on pain pressure thresholds, quality of life, fatigue, pain intensity, quality of sleep, anxiety, and depression in patients with fibromyalgia syndrome. Disabil. Rehabil. 2019, 41, 2235–2246. [Google Scholar] [CrossRef] [PubMed]
- Montoya, P.; Pauli, P.; Batra, A.; Wiedemann, G. Altered processing of pain-related information in patients with fibromyalgia. Eur. J. Pain 2005, 9, 293–303. [Google Scholar] [CrossRef] [PubMed]
- Desmeules, J.A.; Cedraschi, C.; Rapiti, E.; Baumgartner, E.; Finckh, A.; Cohen, P.; Dayer, P.; Vischer, T.L. Neurophysiologic evidence for a central sensitization in patients with fibromyalgia. Arthritis Rheum. 2003, 48, 1420–1429. [Google Scholar] [CrossRef] [PubMed]
- Maurer, A.J.; Lissounov, A.; Knezevic, I.; Candido, K.D.; Knezevic, N.N. Pain and sex hormones: A review of current understanding. Pain Manag. 2016, 6, 285–296. [Google Scholar] [CrossRef] [PubMed]
- Theoharides, T.C.; Tsilioni, I.; Arbetman, L.; Panagiotidou, S.; Stewart, J.M.; Gleason, R.M.; Russell, I.J. Fibromyalgia syndrome in need of effective treatments. J. Pharmacol. Exp. Ther. 2015, 355, 255–263. [Google Scholar] [CrossRef]
- Ablin, J.; Fitzcharles, M.A.; Buskila, D.; Shir, Y.; Sommer, C.; Häuser, W. Treatment of fibromyalgia syndrome: Recommendations of recent evidence-based interdisciplinary guidelines with special emphasis on complementary and alternative therapies. Evid. Based Complement. Altern. Med. 2013, 2013, 485272. [Google Scholar] [CrossRef]
- Macfarlane, G.J.; Kronisch, C.; Dean, L.E.; Atzeni, F.; Häuser, W.; Fluß, E.; Choy, E.; Kosek, E.; Amris, K.; Branco, J.; et al. EULAR revised recommendations for the management of fibromyalgia. Ann. Rheum. Dis. 2017, 76, 318–328. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Yi, G.; Hong, W.; Bo, C.; Wang, Z.; Liu, Y.; Xue, Z.; Li, Y. Efficacy of acupuncture on fibromyalgia syndrome: A meta-analysis. J. Tradit. Chin. Med. 2014, 34, 381–391. [Google Scholar] [CrossRef] [PubMed]
- Dunning, J.; Butts, R.; Mourad, F.; Young, I.; Flannagan, S.; Perreault, T. Dry needling: A literature review with implications for clinical practice guidelines. Phys. Ther. Rev. 2014, 19, 252–265. [Google Scholar] [CrossRef]
- Gattie, E.; Cleland, J.A.; Snodgrass, S. The Effectiveness of Trigger Point Dry Needling for Musculoskeletal Conditions by Physical Therapists: A Systematic Review and Meta-analysis. J. Orthop. Sports Phys. Ther. 2017, 47, 133–149. [Google Scholar] [CrossRef]
- Espejo-Antúnez, L.; Tejeda, J.F.; Albornoz-Cabello, M.; Rodríguez-Mansilla, J.; de la Cruz-Torres, B.; Ribeiro, F.; Silva, A.G. Dry needling in the management of myofascial trigger points: A systematic review of randomized controlled trials. Complement Ther. Med. 2017, 33, 46–57. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, Y.; Xing, J.J.; Li, J.; Zeng, B.Y.; Liang, F.R. History of acupuncture research. Int. Rev. Neurobiol. 2013, 111, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Deare, J.C.; Zheng, Z.; Xue, C.C.; Liu, J.P.; Shang, J.; Scott, S.W.; Littlejohn, G. Acupuncture for treating fibromyalgia. Cochrane Database Syst. Rev. 2013, 2013, CD007070. [Google Scholar] [CrossRef]
- Zhou, K.; Ma, Y.; Brogan, M.S. Dry needling versus acupuncture: The ongoing debate. Acupunct. Med. 2015, 33, 485–490. [Google Scholar] [CrossRef]
- Kim, J.; Kim, S.R.; Lee, H.; Nam, D.H. Comparing Verum and Sham Acupuncture in Fibromyalgia Syndrome: A Systematic Review and Meta-Analysis. Evid. Based Complement. Altern. Med. 2019, 2019, 8757685. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.C.; Chen, H.; Xu, W.T.; Song, Y.Y.; Gu, Y.H.; Ni, G.X. Acupuncture therapy for fibromyalgia: A systematic review and meta-analysis of randomized controlled trials. J. Pain Res. 2019, 12, 527–542. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T. Papers that summarise other papers (systematic reviews and meta-analyses). BMJ 1997, 315, 672–675. [Google Scholar] [CrossRef] [PubMed]
- Shokraneh, F.; Adams, C.E. Study-based registers of randomized controlled trials: Starting a systematic review with data extraction or meta-analysis. Bioimpacts 2017, 7, 209–217. [Google Scholar] [CrossRef] [PubMed]
- de Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Oxman, A.D.; Brozek, J.; Glasziou, P.; Bossuyt, P.; Chang, S.; Muti, P.; Jaeschke, R.; Guyatt, G.H. GRADE: Assessing the quality of evidence for diagnostic recommendations. BMJ Evid. Based Med. 2008, 13, 162–163. [Google Scholar] [CrossRef] [PubMed]
- Austin, T.M.; Richter, R.R.; Sebelski, C.A. Introduction to the GRADE approach for guideline development: Considerations for physical therapist practice. Phys. Ther. 2014, 94, 1652–1659. [Google Scholar] [CrossRef]
- Luo, D.; Wan, X.; Liu, J.; Tong, T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat. Methods Med. Res. 2018, 27, 1785–1805. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, G.M.; Feinn, R. Using Effect Size—Or Why the P Value Is Not Enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Deeks, J.J.; Higgins, J.P.T.; Douglas, G.; Altman, D.G. Analyzing data and undertaking metanalyses. In Cochrane Handbook for Systematic Reviews of Interventions Version 5.2.0 (Updated June 2017); Higgins, J.P.T., Churchill, R., Chandler, J., Cumpston, M.S., Eds.; Cochrane: London, UK, 2017. [Google Scholar]
- Huedo-Medina, T.B.; Sánchez-Meca, J.; Marín-Martínez, F.; Botella, J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol. Methods 2006, 11, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Collazo-Chao, E. Effectiveness of acupuncture therapy for pain relief in patients with fibromyalgia. Rev. Int. Acupunt. 2010, 4, 52–58. [Google Scholar] [CrossRef]
- Collazo-Chao, E.; Aragonés, M.A. Acupuncture and traditional Chinese dietary therapy in the treatment of patients with fibromyalgia. A randomized prospective study. Rev. Int. Acupunt. 2012, 6, 94–101. [Google Scholar]
- Iannuccelli, C.; Mannocci, F.; Guzzo, M.P.; Olivieri, M.; Gerardi, M.C.; Atzeni, F.; Sarzi-Puttini, P.; Valesini, G.; Di Franco, M. Complementary treatment in fibromyalgia: Combination of somatic and abdominal acupuncture. Clin. Exp. Rheumatol. 2012, 30, 112–116. [Google Scholar]
- Collazo-Chao, E.; Muñoz-Reina, M.D. Scalp acupuncture and acupuncture for treatment of patients with fibromyalgia. Prospective randomized study. Rev. Int. Acupunt. 2013, 7, 6–11. [Google Scholar]
- Casanueva, B.; Rivas, P.; Rodero, B.; Quintial, C.; Llorca, J.; González-Gay, M.A. Short-term improvement following dry needle stimulation of tender points in fibromyalgia. Rheumatol. Int. 2014, 34, 861–866. [Google Scholar] [CrossRef] [PubMed]
- Collazo-Chao, E.; Muñoz-Reina, M.D.; Aragonés, M.A.; Gómez, F. Randomized prospective study to assess the effectiveness of several therapeutic procedures of traditional Chinese medicine in alleviation of pain and improvement in the standard of living in patients with fibromyalgia. Rev. Int. Acupunt. 2014, 8, 121–128. [Google Scholar] [CrossRef]
- Stival, R.S.; Cavalheiro, P.R.; Stasiak, C.E.; Galdino, D.T.; Hoekstra, B.E.; Schafranski, M.D. Acupuntura na fibromialgia: Um estudo randomizado-controlado abordando a resposta imediata da dor [Acupuncture in fibromyalgia: A randomized, controlled study addressing the immediate pain response]. Rev. Bras. Reumatol. 2014, 54, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Weber, A.; Werneck, L.; Paiva, E.; Gans, P. Effects of music in combination with vibration in acupuncture points on the treatment of fibromyalgia. J. Altern. Complement. Med. 2015, 21, 77–82. [Google Scholar] [CrossRef]
- Días, P.A.; Guimarães, A.B.; Albuquerque Ade, O.; de Oliveira, K.L.; Cavalcante, M.L.; Guimarães, S.B. Short-term complementary and alternative medicine on quality of life in women with fibromyalgia. J. Integr. Med. 2016, 14, 29–35. [Google Scholar] [CrossRef]
- Li, D.; Yang, L.; Li, J. Fibromyalgia syndrome treated with acupuncture at the acupoints of the affected meridians and heavy moxibustion at painful points: A randomized controlled trial. Zhongguo Zhen Jiu 2016, 36, 147–151. [Google Scholar]
- Vas, J.; Santos-Rey, K.; Navarro-Pablo, R.; Modesto, M.; Aguilar, I.; Campos, M.Á.; Aguilar-Velasco, J.F.; Romero, M.; Párraga, P.; Hervás, V.; et al. Acupuncture for fibromyalgia in primary care: A randomised controlled trial. Acupunct. Med. 2016, 34, 257–266. [Google Scholar] [CrossRef]
- Castro-Sanchez, A.M.; Garcia-Lopez, H.; Mataran-Penarrocha, G.A.; Fernandez-Sanchez, M.; Fernandez-Sola, C.; Granero-Molina, J.; Aguilar-Ferrandiz, M.E. Effects of Dry Needling on Spinal Mobility and Trigger Points in Patients with Fibromyalgia Syndrome. Pain Physician 2017, 20, 37–52. [Google Scholar] [CrossRef]
- Iannuccelli, C.; Guzzo, M.P.; Atzeni, F.; Mannocci, F.; Alessandri, C.; Gerardi, M.C.; Valesini, G.; Di Franco, M. Pain modulation in patients with fibromyalgia undergoing acupuncture treatment is associated with fluctuations in serum neuropeptide Y levels. Clin. Exp. Rheumatol. 2017, 35, 81–85. [Google Scholar] [PubMed]
- Uğurlu, F.G.; Sezer, N.; Aktekin, L.; Fidan, F.; Tok, F.; Akkuş, S. The effects of acupuncture versus sham acupuncture in the treatment of fibromyalgia: A randomized controlled clinical trial. Acta Reumatol. Port. 2017, 42, 32–37. [Google Scholar] [PubMed]
- Zucker, N.A.; Tsodikov, A.; Mist, S.D.; Cina, S.; Napadow, V.; Harris, R.E. Evoked Pressure Pain Sensitivity Is Associated with Differential Analgesic Response to Verum and Sham Acupuncture in Fibromyalgia. Pain Med. 2017, 18, 582–1592. [Google Scholar] [CrossRef]
- Karatay, S.; Okur, S.C.; Uzkeser, H.; Yildirim, K.; Akcay, F. Effects of Acupuncture Treatment on Fibromyalgia Symptoms, Serotonin, and Substance P Levels: A Randomized Sham and Placebo-Controlled Clinical Trial. Pain Med. 2018, 19, 615–628. [Google Scholar] [CrossRef] [PubMed]
- Mist, S.D.; Jones, K.D. Randomized Controlled Trial of Acupuncture for Women with Fibromyalgia: Group Acupuncture with Traditional Chinese Medicine Diagnosis-Based Point Selection. Pain Med. 2018, 19, 1862–1871. [Google Scholar] [CrossRef]
- Yüksel, M.; Ayaş, Ş.; Cabıoğlu, M.T.; Yılmaz, D.; Cabıoğlu, C. Quantitative Data for Transcutaneous Electrical Nerve Stimulation and Acupuncture Effectiveness in Treatment of Fibromyalgia Syndrome. Evid. Based Complement. Altern. Med. 2019, 2019, 9684649. [Google Scholar] [CrossRef]
- Ozen, S.; Saracgil Cosar, S.N.; Cabioglu, M.T.; Cetin, N. A Comparison of Physical Therapy Modalities Versus Acupuncture in the Treatment of Fibromyalgia Syndrome: A Pilot Study. J. Altern. Complement. Med. 2019, 25, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Castro-Sánchez, A.M.; Garcia-López, H.; Fernández-Sánchez, M.; Perez-Marmol, J.M.; Leonard, G.; Gaudreault, N.; Aguilar-Ferrándiz, M.E.; Matarán-Peñarrocha, G.A. Benefits of dry needling of myofascial trigger points on autonomic function and photoelectric plethysmography in patients with fibromyalgia syndrome. Acupunct. Med. 2020, 38, 140–149. [Google Scholar] [CrossRef] [PubMed]
- Di Carlo, M.; Beci, G.; Salaffi, F. Acupuncture for Fibromyalgia: An Open-Label Pragmatic Study on Effects on Disease Severity, Neuropathic Pain Features, and Pain Catastrophizing. Evid Based Complement Alternat. Med. 2020, 2020, 9869250. [Google Scholar] [CrossRef] [PubMed]
- Garrido-Ardila, E.M.; González-López-Arza, M.V.; Jiménez-Palomares, M.; García-Nogales, A.; Rodríguez-Mansilla, J. Effectiveness of acupuncture vs. core stability training in balance and functional capacity of women with fibromyalgia: A randomized controlled trial. Clin. Rehabil. 2020, 34, 630–645. [Google Scholar] [CrossRef] [PubMed]
- Schweiger, V.; Secchettin, E.; Castellani, C.; Martini, A.; Mazzocchi, E.; Picelli, A.; Polati, E.; Donadello, K.; Valenti, M.T.; Dalle Carbonare, L. Comparison between Acupuncture and Nutraceutical Treatment with Migratens® in Patients with Fibromyalgia Syndrome: A Prospective Randomized Clinical Trial. Nutrients 2020, 12, 821. [Google Scholar] [CrossRef] [PubMed]
- Garrido-Ardila, E.M.; González-López-Arza, M.V.; Jiménez-Palomares, M.; García-Nogales, A.; Rodríguez-Mansilla, J. Effects of Physiotherapy vs. Acupuncture in Quality of Life, Pain, Stiffness, Difficulty to Work and Depression of Women with Fibromyalgia: A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 3765. [Google Scholar] [CrossRef]
- Úbeda-D’Ocasar, E.; Jiménez Díaz-Benito, V.; Gallego-Sendarrubias, G.M.; Valera-Calero, J.A.; Vicario-Merino, Á.; Hervás-Pérez, J.P. Pain and Cortisol in Patients with Fibromyalgia: Systematic Review and Meta-Analysis. Diagnostics 2020, 10, 922. [Google Scholar] [CrossRef] [PubMed]
- Úbeda-D’Ocasar, E.; Valera-Calero, J.A.; Hervás-Pérez, J.P.; Caballero-Corella, M.; Ojedo-Martín, C.; Gallego-Sendarrubias, G.M. Pain Intensity and Sensory Perception of Tender Points in Female Patients with Fibromyalgia: A Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 1461. [Google Scholar] [CrossRef] [PubMed]
- Cigarán-Méndez, M.I.; Pellicer-Valero, O.J.; Martín-Guerrero, J.D.; Varol, U.; Fernández-de-las-Peñas, C.; Navarro-Pardo, E.; Valera-Calero, J.A. Bayesian Linear Regressions Applied to Fibromyalgia Syndrome for Understanding the Complexity of This Disorder. Int. J. Environ. Res. Public Health 2022, 19, 4682. [Google Scholar] [CrossRef]
- Liew, B.X.W.; Valera-Calero, J.A.; Varol, U.; Nijs, J.; Arendt-Nielsen, L.; Plaza-Manzano, G.; Fernández-de-Las-Peñas, C. Distress and Sensitization as Main Mediators of Severity in Women with Fibromyalgia: A Structural Equation Model. Biomedicines 2022, 10, 1188. [Google Scholar] [CrossRef]
- Cigarán-Méndez, M.; Úbeda-D’Ocasar, E.; Arias-Buría, J.L.; Fernández-de-Las-Peñas, C.; Gallego-Sendarrubias, G.M.; Valera-Calero, J.A. The hand grip force test as a measure of physical function in women with fibromyalgia. Sci. Rep. 2022, 12, 3414. [Google Scholar] [CrossRef]
- Úbeda-D’Ocasar, E.; Valera-Calero, J.A.; Gallego-Sendarrubias, G.M.; Fernández-de-las-Peñas, C.; José Luis Arias-Buría, J.L.; Matilde Morales-Cabezas, M.; Lars Arendt-Nielsen, L.; Margarita Cigarán-Méndez, M. Association of Neuropathic Pain Symptoms with Sensitization Related Symptomatology in Women with Fibromyalgia. Biomedicines 2022, 10, 612. [Google Scholar] [CrossRef] [PubMed]
- Valera-Calero, J.A.; Úbeda-D’Ocasar, E.; Caballero-Corella, M.; Fernández-de-Las-Peñas, C.; Sendarrubias, G.M.G.; Arias-Buría, J.L. Cervical Multifidus Morphology and Quality Are Not Associated with Clinical Variables in Women with Fibromyalgia: An Observational Study. Pain Med. 2022, 23, 1138–1143. [Google Scholar] [CrossRef] [PubMed]
- Cigarán-Méndez, M.; Úbeda-D’Ocasar, E.; Arias-Buría, J.L.; Fernández-de-Las-Peñas, C.; Barbero, M.; Gallego-Sendarrubias, G.M.; Valera-Calero, J.A. Pain extent is associated with Central Sensitization Inventory but not widespread pressure pain sensitivity or psychological variables in women with fibromyalgia. Scand. J. Rheumatol. 2022, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Sarmiento-Hernández, I.; Pérez-Marín, M.L.Á.; Nunez-Nagy, S.; Pecos-Martín, D.; Gallego-Izquierdo, T.; Sosa-Reina, M.D. Effectiveness of Invasive Techniques in Patients with Fibromyalgia: Systematic Review and Meta-Analysis. Pain Med. 2020, 21, 3499–3511. [Google Scholar] [CrossRef] [PubMed]
- Fernández-de-las-Peñas, C.; Dommerholt, J. International Consensus on Diagnostic Criteria and Clinical Considerations of Myofascial Trigger Points: A Delphi Study. Pain Med. 2018, 19, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Valera-Calero, J.A. Percutaneous Electrolysis: A Potential Tool for Myofascial Pain Syndrome Treatment? Biomed. J. Sci. Tech. Res. 2020, 27, 21004–21005. [Google Scholar] [CrossRef]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.A.; Goldenberg, D.L.; Katz, R.S.; Mease, P.; Russell, A.S.; Russell, I.J.; Winfield, J.B.; Yunus, M.B. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. 2010, 62, 600–610. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).