Abstract
Physical activity has become an integral component of public health systems modeling the public health core functions of assessment, policy development, and assurance. However, people with disabilities have often not been included in public health efforts to assess, develop policies, or evaluate the impact of physical activity interventions to promote health and prevent disease among people with disabilities. Addressing the core function of assessment, current physical activity epidemiology, and surveillance among people with disabilities across the globe highlights the paucity of surveillance systems that include physical activity estimates among people with disabilities. The status of valid and reliable physical activity measures among people with condition-specific disabilities is explored, including self-report measures along with wearable devices, and deficiencies in measurement of physical activity. The core functions of policy development and assurance are described in the context of community-based intervention strategies to promote physical activity among people with disabilities. The identification of research gaps in health behavior change, policy, and environmental approaches to promoting physical activity among people with disabilities is explored, along with recommendations based on the principles of inclusive and engaged research partnerships between investigators and the members of the disability community.
1. Epidemiology and Surveillance of Physical Activity among People with Disabilities (PWD)
Background and rationale. Epidemiology and public health surveillance are a cornerstone of public health practice used to systematically monitor the population-level trends in health and behaviors, and to guide intervention priorities [1]. Existing surveillance systems for physical activity most often assess the aerobic physical activity (PA) behaviors of individuals and have been used to monitor secular changes in the population levels of PA over time [2,3]. Surveillance can also be used to monitor the factors that can influence changes in the PA levels. For example, the systems can be used to monitor supports for PA within the community and within various settings, such as workplaces. While PA surveillance systems, such as those existing in the United States and other high income countries (HIC) were primarily developed for national and state/region-specific monitoring of PA and inactivity among adults, their use can also be applied regionally and locally [4]. Sometimes the states/regions, but most often local, application of such data not only includes PA monitoring, but also intervention planning and program evaluation [5,6,7]. The expert panel results from a recent workshop conducted by the U.S. Centers for Disease Control and Prevention (CDC) sought to outline the current and future efforts within public health surveillance systems that need to be implemented in a timely, valid, and reliable manner to assess population-wide levels of PA and sedentary behaviors [8]. As examples, the national surveillance systems [2,9,10,11] along with the Behavioral Risk Factor Surveillance System (BRFSS) can be used to generate regional and even sometimes locally specific PA estimates [12]. In the case of the BRFSS, this system has been adapted for local applications by over-sampling in smaller geographic areas to generate locale-specific estimates of PA and related health behaviors [4,7,12]. The local public health practitioners can also use additional monitoring tools, such as community resource inventories [4] and environmental audits, to assess the PA needs and correlates of activity [13,14]. The objective measurements of PA have been demonstrated to be feasible surveillance and evaluation tools. Direct observation [15], accelerometers [16], and pedometers [17] have proven to be feasible, reliable, and valid measures of PA. When comparing these methods of PA assessment, each provides some advantages and disadvantages. In the case of direct observation, this is where trained observers, unobtrusively, record the number of people and their activity (from sedentary through vigorous) observed in various settings, e.g., parks, paths, playgrounds, and sidewalks. This method is valid and reliable (repeatability), but is labor intensive and requires the training of the observers—so is subject to inter-observer error [15]. Wearable devices, such as pedometers and accelerometers, have also demonstrated a good reliability and validity [8]. Pedometers measure the number of steps and need to be calibrated in accordance with the individual’s walking stride length. Accelerometers are more sophisticated measurement tools, and can measure general movement as well as electronically recording periods of sedentariness as well as movement [8]. The movement data from these wearables can be electronically downloaded into data spreadsheets. The cost of these wearables, unlike pedometers, is more expensive and labor intensive for both the subject wearing the device, often for 7 consecutive days, as well as the investigator. The use of such PA measures among PWD has been limited, since, in the case of wearables, the mode of activity is often walking/running and movement of the lower extremities, excluding use among PWD who have mobility impairments. Hence, further efforts to refine the use of accelerometers among PWD using upper extremities and/or trunk movements are currently being explored by investigators.
Finally, the information from the vital statistics and administrative data, such as hospital admission and discharge data, can be used to support the PA and health link [18]. The efforts to improve public health surveillance for PA can incorporate the same principles that are used to improve other public health surveillance efforts. The public health surveillance systems should have a clear purpose and are evaluated on their usefulness (contribution to prevention and control of disease) and their attributes. These attributes include simplicity, flexibility, data quality, acceptability, sensitivity, representativeness, timeliness, and stability (Table 1) [19].

Table 1.
Key attributes to consider when developing or evaluating public health surveillance systems *.
Status of global surveillance of PA among country-specific populations. Much has been accomplished over the past two decades regarding global efforts to measure physical activity prevalence and the impact of physical inactivity on health outcomes and mortality. Most of the current updates have been reported in The Lancet’s Global Health Physical Activity Series (LPAS 1, 2, and 3) in 2012, 2016, and 2021 [21,22,23,24,25,26,27,28,29]. A broader and more in-depth overview of the prevalence of physical activity worldwide is available through the Global Observatory for Physical Activity (GoPA!), and the release of their recent 2nd edition Global Physical Activity Almanac (Figure 1) [30].
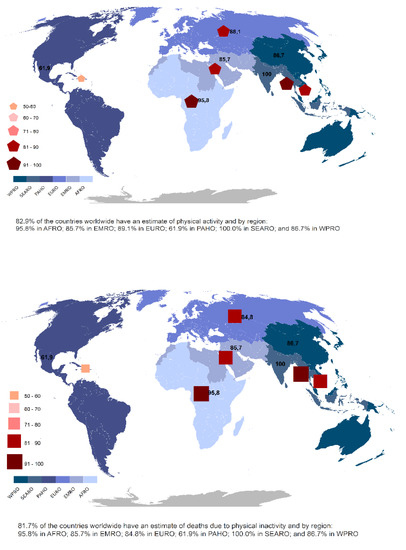
Figure 1.
Global prevalence of physical activity and global deaths due to physical inactivity. Adapted with permission from [30].
Current Status of global PA surveillance among PWD. In accordance with the recent review of Martin Ginis et al. [31], the following definitions have been used in this review, from studies of surveillance and assessment of PA among people with disabilities: (1) Disability, defined in light of the World Health Organization’s (WHO) International Classification of Functioning, Disability and Health (ICF) [32] and in accordance with the WHO Global Disability Plan 2014–2021: Better Health for All People with Disability [33], where estimates measure the domains of health and functioning, and/or domains and core questions of the Washington Group [34], which includes assessment among the respondents regarding difficulty with vision, hearing, walking or climbing steps, remembering or concentrating, self-care activities such as washing all over or dressing, communicating (understanding or being understood); (2) PA and physical inactivity are defined in accordance with the WHO Global Recommendations on Physical Activity for Health [35] and other national bodies, where the minimal amount of PA necessary to accrue health benefits for adults is 150 min of moderate aerobic PA per week or 75 min of vigorous PA per week and for children/youth, aged 6–18 years, 60 min of moderate to vigorous PA per day [35,36,37,38]. Persons are considered physically inactive if their levels of PA are less than these guidelines. More recently, Public Health England released a rapid evidence review summarizing the general health benefits of PA among adults with a disability [37]. Subsequently, WHO released the First Global Physical Activity and Sedentary Behavior Guidelines for People Living with Disability [35,39]. These guidelines provide evidence that doses of PA, tailored to the type of disability, along with guidelines limiting sedentary behavior provide significant health and improved function among PWD, similar to those benefits experienced by people without disability [35].
The current prevalence estimates of PA among people with disabilities comes almost exclusively from among the High Income Countries (HIC), such as those in North America, Western Europe, and Scandinavia [40,41,42,43]. There are prevalence estimates for PA among people with disabilities from Low to Middle Income Countries (LMIC), but these are limited to a small number of countries [44,45,46,47,48]. For adults living in HIC, the estimates among PWD meeting the WHO Guidelines range from 20.6 to 50%, while for PWD living in LMIC, the range is 23.4 to 50%. For children and adolescents, the estimates of those meeting the PA guidelines in HIC vary from 25 to 42%, while no systematic data exist for children and youth estimates in LMICs [49,50,51,52]. These contrast with PA prevalence estimates among children/adolescents and adults without disabilities in both HIC and LMIC of 40% to 60% and 50% to 80%, respectively [38,39,40,45,47,48,49,53]. The known efforts to measure PA and disability among children, adolescents, and adults concurrently across the globe in both HIC and LMIC are summarized in Table 2.

Table 2.
Prevalence Estimates of Physical Activity among people with disabilities from around the globe: children; adolescents; adults; and older adults.
Currently, comprehensive global estimates of PA patterns among people with disabilities do not exist [31]. The current international survey instruments and surveillance systems have either good measures for PA and sedentary behavior or good measures for disability and functional health, but seldom both. Finally, the Global Burden of Disease (GBD) reports estimates for PA in association with disability-adjusted life years (DALYS) and years lived with a disability (YLD) for specific ICD10 conditions/diseases/injuries [54]. However, it is unclear whether these measures are sufficiently sensitive for people with disabilities, or whether disability advocates find such measures acceptable.
Research Gaps and Recommendations. Current gaps in global epidemiology and surveillance of PA patterns—sedentary behavior through to high-intensity PA among people with disabilities—include a paucity of country-specific policies supporting improved access to places for PA among persons with disabilities. The current data come primarily from HIC, with little data from LMIC. The current global PA surveillance systems (e.g., WHO STEPs) for NCD do not include functioning and disability survey items. Often, disability surveillance instruments lack PA measures. This may be due in part to the lack of consensus regarding both reliable and valid measures of PA among PWD [31]. The national estimates for PA prevalence are the foundation of the PA action plans. They allow countries to track progress, ideally across all of the population groups and at all stages of the life course. The inclusion of PA prevalence estimates among adults and children with disabilities is now more frequent (e.g., USA, UK), reflecting the call by the WHO Global Action Plan on Physical Activity for “equity across the life course”. However, globally, and especially among LMIC, such data rarely exist, despite its obvious importance. Hence, the extent to which people with disabilities are included in the PA surveillance is remiss, because the national and international PA surveillance data across the globe rarely include people with a disability or classifies them as a group worthy of identification. Unless we understand the different levels of current activity and ability, any actions to shift the priority towards addressing disparities and reducing inequalities will remain both unevaluated and unachieved. The application of such strategies for PA surveillance among PWD require several important steps: (1) the continued evolution of more sensitive and specific PA measurement methods designed to capture the essential and functional PA among PWD, including electronic and other methods; (2) the intentional engagement of PWD in the design and development of PA measures that are adaptable and functionally acceptable; (3) the purposeful collaboration of public health organizations/practitioners with disability organizations and advocates to ensure the full integration of PWD into the mainstream of PA and public health. Thus, it is a priority that PA surveillance be inclusive at multiple levels. For example, action at the international level is critically needed to ensure that the WHO’s “STEP-wise approach to noncommunicable disease risk factor surveillance” data include people living with a disability. Specific strategies to improve physical activity surveillance that need expedient attention in general, fall into a series of categories that were generated by the recent CDC convening of PA and public health experts. 9 The research priorities were developed for each of the following strategies:
(1) Identify and prioritize PA constructs; (2) Assess the psychometric properties of instruments for PA surveillance; (3) Provide training and technical assistance for those collecting, analyzing, or interpreting surveillance data; (4) Explore accessing data from alternative sources; (5) Improve communication, translation, and dissemination of information about estimates of PA from surveillance systems. Although these strategies and research priorities were developed for physical activity surveillance in general, they are directly applicable to PWD, as part of an inclusive surveillance effort for PA [31].
2. Physical Activity Measures among People with Condition-Specific Disabilities: Research Gaps and Recommendations
Drawing on the systematic and scoping reviews presented by Martin Ginis et al., [31] which address the PA measures and intervention effects among persons living with a disability, a further search of the subsequent literature was conducted through several search engines, including Pubmed, Scopus, and Web of Science, providing both confirmation of the existing, and an update of the most recent, literature. Potentially disabling conditions were prioritized based on: (1) the prevalence of the condition across the global population; (2) the potential disabling impact of the condition over the course of the lifecycle; and (3) an existing evidence-base demonstrating a positive physical and/or mental health benefit among people living with a disability.
Persons with Spinal Cord Injury. The accurate measurement of PA in individuals with spinal cord injuries (SCI) has inherent limitations. The measures most used have include self-reported outcomes, such as the Physical Activity Recall Assessment for People with Spinal Cord Injury (PARA-SCI) [55], which has been validated for this population [56]. The PARA-SCI is a three-day PA questionnaire guided by an interview [57].
Accelerometry, which is less dependent on the recall of the activity level and intensity, has also been recommended as a measure of PA for individuals with SCI [58,59,60]. Accelerometers were placed on wheelchair spokes in various studies; however, this does not reflect upper extremity activity, and does not reflect the time that the wheelchair may be coasting or going downhill [60,61]. The placement of accelerometers on the upper extremities is therefore recommended, as well as individual calibration of the accelerometers for this population, to improve the accuracy [58,59]. The studies examining the agreement between accelerometers and the PARA-SCI have shown low levels of agreement. For example, resistance activities (upper body strengthening) and pushing a wheelchair uphill or on varied surfaces was reported higher on the PARA-SCI than with an accelerometer. Conversely, brief periods of activity and some of the activities of daily living may not be captured on the PARA-SCI, but are captured by accelerometry. This suggests that multiple measures may need to be utilized to capture a more complete picture of physical activity in this population [60]. Accurately capturing the amount of PA performed in this population is an area of research that will continue to evolve, but multiple measures combined will yield more accurate data.
Persons with stroke. A stroke is a condition/clinical event which can result in a wide variety of disability outcomes, both in terms of the systems affected as well as the severity and presents several significant PA measurement challenges. The focus here is on mobility impairments resulting from a stroke, whether thromboembolic or hemorrhagic. The physical activity levels of people with stroke are lower than their age-matched counterparts, even when they return to living in the community [62]. Regular PA in stroke survivors can improve the strength, balance, and HRQOL [63]. The methods to assess the duration, intensity, and frequency of exercise and stroke survivors, and its relationship to improving HRQOL, are sparse.
A recent systematic review [64] highlighted the lack of research that examines the measurement properties of the self-report PA assessment tools for stroke survivors. The validity and usefulness of these measures need to be examined in much greater depth, to assess if they are useful in research and in clinical practice.
The quantitative methods of monitoring PA following stroke were reviewed by [62], and examined the various methods and devices used for the measurement of PA. The objective measures included pedometers, actometers, accelerometers, and inertial measurement units (IMUs) which primarily used accelerometer data. The validity of many of the methods was not assessed and the studies that measured the validity ranged from poor to good, with better validity in more controlled environments, such as an in-patient setting where the daily routines are consistent. The reliability was examined to a higher degree, but there are limited data in real world environments.
The most recent systematic review [65] also examined the agreement between sensor-based measures of PA and clinical outcome measures, such as the National Institute of Health Stroke Scale, the Fugl-Meyer upper extremity motor assessment scale, Stroke Impairment Scale, etc., and reported that the sensor-based measures represent a different construct compared to the clinical scales [65].
Similar to other disabilities, no single device or method, such as patient-reported activity, was found to be ideal for quantifying PA after stroke [62]. The use of sensor-based measurements in combination with clinical outcome measures may yield the best information, similar to the other populations with disabilities. Obtaining accurate measures of activity duration, frequency, and intensity needs to be better refined for this population. What constitutes PA also varies between the studies and a more standardized definition of this would enhance the research in this field. The maintenance of PA after research trials also needs to be addressed for this population [66]. A Cochrane review [67] found only four small trials that examined the efficacy of activity monitors for increasing PA after stroke. The evidence for their usefulness in increasing PA to improve health and HRQOL and prevent a subsequent stroke should be a priority.
Persons with Parkinson’s Disease. The individuals with Parkinson’s disease (PD) have decreased levels of PA compared to age-matched controls [68]. This can be explained in part by the motor control issues due to akinesia and bradykinesia, tremor, and rigidity. A fear of falls has also been a factor limiting PA in this population [69]. The methods for the accurate assessment of PA for individuals with PD have been examined, but the data are limited, with studies that address reliability, validity, and clinical usefulness significantly lacking. The functional outcomes, such as recall of activities questionnaires, have been utilized but can also be affected by cognitive deficits [70].
The majority of the scales used have focused on the activities of daily living, and the measures of PA have not been developed specifically for this population, rather, the generic PA measures have traditionally been used, such as the Physical Activity Scale for the Elderly, International Physical Activity Questionnaire-Short Form, Exercise Self-Efficacy Scale, and others [71,72].
The progression of PD also makes it important to look at PA over time in the same cohorts of individuals, and how it affects HRQOL, including falls and depression. The data acquired from sensors, such as accelerometers, have increased as the cost of these devices has progressively decreased [73,74,75], but lack standardization and links to health-related measures. One study found that involuntary movements may increase the measures of PA [76], and may need to be factored in. There is a clear need to develop objective, reliable and validated tools for the measurement of PA in individuals with PD, as well PA questionnaires specifically for this population.
People with Cerebral Palsy. Cerebral palsy (CP) is a permanent disorder that commonly affects motor function and is frequently accompanied by comorbidities, such as cognitive and learning disabilities, epilepsy, and visual impairments. The functional limitations commonly seen with CP include difficulty with gait, balance, and increased muscle tone, which can create challenges to performing regular PA [77]. A lack of opportunity for regular PA is also problematic, as well as decreased self-efficacy for exercise. This, coupled with communication and behavioral issues in some of the individuals, compounds the problem. The guidelines for exercise and PA in individuals with cerebral palsy (CP) have been reported in the literature [78], however the majority of the literature has examined PA in children, with few studies on adults. Information is also lacking on how the habits developed in childhood may impact future PA habits, and how PA may impact health over the lifespan [78]. A systematic review examining the fitness measures for individuals with CP was conducted, and, of the over 800 articles they identified, less than one percent examined the reliability or validity of cardiovascular or strengthening measures for individuals with CP [79]. The outcomes’ measures that are based on standardized activity diaries and measures have been sparsely utilized in this population, and adaptations to these scales for the individuals with CP are lacking. While the PA questionnaire for older children (PAQ-C) has been used extensively in normal children, no studies have examined its usefulness in children with CP. The pediatric outcomes data-collection instrument is being used in one study [80], however, this is an ongoing trial. Other functional outcome measures, such as the timed-up-and-go and the child and adolescent scale of participation, have been used as a surrogate for physical activity, but have not been validated for this population. The international physical activity questionnaire has been utilized [81,82] and was found to not be a valid tool for the measurement of PA in individuals with CP [81]. The children’s assessment of participation and enjoyment was used to examine participation in leisure activities, and the reliability was examined but not the validity [83], and this scale does not address duration, intensity, dose, or frequency of PA.
Accelerometry has been used to a large extent in this population for ambulatory individuals, and has been shown to be reliable and valid [80,84,85,86] if adapted to the individual and their level of function. The individuals with cerebral palsy (CP) that are non-ambulatory and that require ambulation aids or wheelchairs have increased challenges in reaching the PA requirements. A few studies have examined physical activity in this population [87]. The quality measures to examine physical activity in individuals with CP are severely limited and need to be developed to better examine PA levels, and the effects of PA on HRQOL and non-communicable disease prevention [88]. The heterogeneity of this population makes the assessment of physical activity challenging without individual adaptations, probably contributing to this gap in the research.
3. Community-Based Interventions to Promote Physical Activity among People with Disabilities
Current Status. Martin Ginis et al. [31] recently conducted a systematic review of PA interventions among PWD. Their findings, which included both primary studies as well as other reviews and meta-analyses, found that most of the PA interventions conducted among PWD have addressed increases in leisure-time PA, were conducted primarily in HIC, and focused on intrapersonal factors and/or interpersonal factors [31]. However, their scoping review did identify several PA interventions delivered at community levels. Generally, such intervention strategies seek a change in the knowledge or practices among individuals, organizations, or community settings (e.g., neighborhoods, schools, parks, recreation centers). The examples include developing guidelines for the construction of accessible built and natural environments (e.g., trails, recreation centers, pools, outdoor venues), developing inclusiveness training programs for PA practitioners, and establishing programs that loan equipment for adapted physical activities [31]. The body of evidence for these types of interventions have produced mixed findings [31]. The examples include a nationwide Canadian study that found an educational intervention, designed to strengthen health care providers’ intentions to discuss LTPA with patients with physical disabilities, had no long-term effects [89]. Another example comes from the Netherlands, where staff training was provided to staff among 18 rehabilitation centers on how to deliver PA counselling with referrals made to hospital-based and community-based PA providers [90,91]. This national program reached 5873 patients with various disabilities and had a significant impact on PA participation over a three-year period [90,92].
The policy-level interventions include efforts to change legislation, laws, codes, regulations, rules, and practices that are developed and implemented by governments, government agencies, and nongovernmental organizations, such as businesses and schools. Some of the examples include policies to fund sports programs and equipment for PWD, to provide accessible transportation, and to ensure that built environments are accessible [93,94]. While some of the policy-level changes have proved to be effective for increasing PA in the general population [95], a paucity of studies exist that test the effectiveness of policy changes for increasing PA among PWD.
Such population-level interventions could be successful at encouraging/possibly changing behavior in the population, but with the unintended cost of widening the inequality gaps between the most vulnerable subgroups, including PWDs and the rest of the population. Hence, where the targeted approaches may not be feasible due to practical and/or political constraints, blended or so-called proportionate universal approaches should be considered by policy makers (e.g., refurbishing a park, or providing enhanced access to PA opportunities to those more in need).
The institutional-, community-, and policy-level approaches to promoting physical activity typically target entire communities or segments of communities [96]. At the institutional- and community-level, many of the organizations (e.g., schools, recreation centers, not-for-profit organizations) are responsible for delivering programs to increase physical activity participation in both the general population as well as those with disabilities. There is strong evidence that physical activity interventions carried out by various organizations, and that include informational, behavioral, and social strategies, can increase physical activity among people of all ages [25,97,98,99]. Unfortunately, very few studies have evaluated the physical activity and health impact of such community-based interventions among people with disabilities. The work of several groups have systematically reviewed the use and evidence of community-based intervention strategies among PWD, only to find a paucity of studies and those that exist are wanting in evidence of effectiveness [100,101,102,103].
The policy-level approaches represent rules, regulations, and practices that may influence physical activity through a variety of mechanisms, such as changing the built environment, providing incentives for exercising, or developing national or regional physical activity guidelines [104,105]. While there is sufficient evidence in support of various policy-level interventions to increase physical activity in the general population, representing both HIC and LMIC, [106,107,108] very few studies have examined the effects of these interventions on people with disabilities. Furthermore, the targets or moderators of policy-level interventions have not been well studied among the people with disabilities. For example, the policies that aim to increase physical activity by improving access to the pedestrian and bicycle infrastructure, or altering the environmental design and land use, have proven effective among the general population (see Table 3) [105,106,108,109,110]. The effects of such policy changes on the physical activity levels of people with disabilities have not been examined. Based on the descriptive studies, it is unclear whether the pedestrian infrastructure even plays a significant role in the physical activity levels of people with disabilities [109].

Table 3.
Overview of strategies to promote physical activity in communities.
Nevertheless, across the globe, many of the barriers to physical activity participation for people with disabilities could be alleviated by national/regional public and organizational policies [92,111,112,113,114]. These policies must align with, and target disability-specific influences on physical activity and be part of broader strategies that target multiple levels of influence [94]. The research has shown, for instance, that national policies supporting investments in major sporting events (e.g., the Paralympics and the Commonwealth Games) often have the intended purpose of enhancing the physical and social accessibility of facilities and venues to people with disabilities [102]. However, the benefits of such developments are unequal, poorly distributed, and do little to address the long-term systemic barriers faced by people with disabilities in the urban environment. For the people with disabilities to take advantage of the accessible recreational facilities, organizational and public policies are needed to alleviate transportation and financial barriers; institutional-, community- and interpersonal-level interventions are needed to address the negative societal attitudes toward physical activity for people with disabilities; and intrapersonal-level interventions are required to teach behavior change techniques [31,95].
4. Summary and Recommendations Addressing Research Gaps in PA and Public Health Efforts among People with Disabilities
Although much has been accomplished in the past decade to address the needs for PWD regarding the health-promoting benefits of PA, significant research gaps continue to exist. Such gaps currently limit the development of evidence-based approaches for promoting PA among PWD within a public health context. As has been reviewed in the preceding sections, these gaps fall into three major categories: (1) the need for adequate and inclusive measures of PA among children, youth, adults, and older adults who live with a disability across all of the public health surveillance systems—national, regional, and local; (2) the need for valid and reliable measures of PA among PWD specific to the type of disability and across multiple modes of assessment, including wearable devices, self-report measures, use of senser technology, and proxy measures; and (3) the need for research efforts to identify effective community-based PA promotion strategies that are both inclusive and adapted/tailored for PWD across a wide spectrum of disabilities.
The research recommendations to address these key components of public health efforts to promote PA among PWD have been enumerated within each of the preceding sections of this review. We have drawn heavily from the work of others to highlight the current status and research gaps, that, if filled through the next generation of research studies covering surveillance, PA measures, and community-based strategies to promote the healthful benefits of PA among PWD, will constitute significant health improvements for PWD across the globe. However, such efforts require significant input and partnership with members of the PWD community. These research partnerships have been identified and implemented across a number of research disciplines, and comprise a strategy that lends itself to addressing the research gaps covered within the context of this review [114]. One such research paradigm which has been used successfully to address the research development for PWD is Integrated Knowledge Translation (IKT) [115]. IKT consists of eight consensus-based principles: (1) Partners develop and maintain relationships based on trust, respect, dignity, and transparency; (2) Partners share in decision-making; (3) Partners foster open, honest, and responsive communication; (4) Partners recognize, value, and share their diverse expertise and knowledge; (5) Partners are flexible and receptive in tailoring the research approach to match the aims and context of the project; (6) Partners can meaningfully benefit by participating in the partnership; (7) Partners address ethical considerations; and (8) Partners respect the practical considerations and financial constraints of all of the partners. Although this model of research partnership with the PWD community was initially carried out in addressing the research efforts among people with a spinal cord injury, the success of this approach appears most applicable in providing important guidance in addressing the research gaps that exist for the full integration of PWD into the context of PA and public health [91,115].
5. Conclusions
Major gains have been made globally over the past decade in advancing the importance of the inclusion of people living with a disability into the fabric of public health policies, practice, and engagement. However, there remains significant research deficiencies addressing physical activity and public health among PWD. These research gaps include incomplete public health surveillance of PA, a lack of disability-specific PA measurement, and effective community-based promotion of physical activity among PWD. These research gaps can be overcome through an intentional partnership between the PA and public health research community, public health policy makers, and public health/prevention funding agencies/organizations in concert with people who live with a disability.
Author Contributions
G.W.H. and D.L. conceived the scope this review; G.W.H. and D.L. equally conducted the literature search; G.W.H. wrote the epidemiology and surveillance narrative; D.L. prepared the material addressing the measurement of physical activity among selected disabling conditions; All authors participated in reviewing the formative drafts. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
The authors wish to express appreciation and thanks to Andrea Ramirez and Jose David Pinzon Ortiz from the Universidad de los Andes, Colombia for creating Figure 1 for use with this publication.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Thacker, S.B.; Berkelman, R.L. Public health surveillance in the United States. Epidemiol. Rev. 1988, 10, 164–190. [Google Scholar] [CrossRef]
- Carlson, S.A.; Fulton, J.E.; Schoenborn, C.A.; Loustalot, F. Trend and prevalence estimates based on the 2008 Physical Activity Guidelines for Americans. Am. J. Prev. Med. 2010, 39, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.V.; Harris, C.D.; Carlson, S.A.; Kruger, J.; Fulton, J.E. Trends in no leisure-time physical activity--United States, 1988–2010. Res. Q. Exerc. Sport 2012, 83, 587–591. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R.M.; Wheeler, F.C.; Lee, P.R. Evaluation of the Heart To Heart Project: Lessons from a community-based chronic disease prevention project. Am. J. Health Promot. 1995, 9, 443–455. [Google Scholar] [CrossRef] [PubMed]
- Brownson, R.C.; Ballew, P.; Brown, K.L.; Elliott, M.B.; Haire-Joshu, D.; Heath, G.W.; Kreuter, M.W. The effect of disseminating evidence-based interventions that promote physical activity to health departments. Am. J. Public Health 2007, 97, 1900–1907. [Google Scholar] [CrossRef]
- Brownson, R.C.; Brennan, L.K.; Evenson, K.R.; Leviton, L.C. Lessons from a mixed-methods approach to evaluating Active Living by Design. Am. J. Prev. Med. 2012, 43, S271–S280. [Google Scholar] [CrossRef]
- Chomitz, V.R.; McDonald, J.C.; Aske, D.B.; Arsenault, L.N.; Rioles, N.A.; Brukilacchio, L.B.; Hacker, K.A.; Cabral, H.J. Evaluation results from an active living intervention in Somerville, Massachusetts. Am. J. Prev. Med. 2012, 43, S367–S378. [Google Scholar] [CrossRef]
- Fulton, J.E.; Carlson, S.A.; Ainsworth, B.E.; Berrigan, D.; Carlson, C.; Dorn, J.M.; Heath, G.W.; Kohl, H.W., 3rd; Lee, I.M.; Lee, S.M.; et al. Strategic Priorities for Physical Activity Surveillance in the United States. Med. Sci. Sports Exerc. 2016, 48, 2057–2069. [Google Scholar] [CrossRef]
- Crespo, C.J.; Keteyian, S.J.; Heath, G.W.; Sempos, C.T. Leisure-time physical activity among US adults. Results from the Third National Health and Nutrition Examination Survey. Arch. Intern. Med. 1996, 156, 93–98. [Google Scholar] [CrossRef]
- Carlson, S.A.; Densmore, D.; Fulton, J.E.; Yore, M.M.; Kohl, H.W., 3rd. Differences in physical activity prevalence and trends from 3 U.S. surveillance systems: NHIS, NHANES, and BRFSS. J. Phys. Act. Health 2009, 6 (Suppl. 1), S18–S27. [Google Scholar] [CrossRef]
- Buehler, R.; Pucher, J.; Merom, D.; Bauman, A. Active travel in Germany and the U.S. Contributions of daily walking and cycling to physical activity. Am. J. Prev. Med. 2011, 41, 241–250. [Google Scholar] [CrossRef]
- Wilcox, S.; Parrott, A.; Baruth, M.; Laken, M.; Condrasky, M.; Saunders, R.; Dowda, M.; Evans, R.; Addy, C.; Warren, T.Y.; et al. The Faith, Activity, and Nutrition program: A randomized controlled trial in African-American churches. Am. J. Prev. Med. 2013, 44, 122–131. [Google Scholar] [CrossRef] [PubMed]
- Foster, C.; Hillsdon, M. Changing the environment to promote health-enhancing physical activity. J. Sports Sci. 2004, 22, 755–769. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Kraft, K.; Linton, L.S. How the environment shapes physical activity: A transdisciplinary research agenda. Am. J. Prev. Med. 2002, 22, 208. [Google Scholar] [CrossRef]
- Ward, P.; McKenzie, T.L.; Cohen, D.; Evenson, K.R.; Golinelli, D.; Hillier, A.; Lapham, S.C.; Williamson, S. Physical activity surveillance in parks using direct observation. Prev. Chronic Dis. 2014, 11, 130147. [Google Scholar] [CrossRef][Green Version]
- Yang, L.; Griffin, S.; Chapman, C.; Ogilvie, D. The feasibility of rapid baseline objective physical activity measurement in a natural experimental study of a commuting population. BMC Public Health 2012, 12, 841. [Google Scholar] [CrossRef]
- Bassett, D.R., Jr.; Wyatt, H.R.; Thompson, H.; Peters, J.C.; Hill, J.O. Pedometer-measured physical activity and health behaviors in U.S. adults. Med. Sci. Sports Exerc. 2010, 42, 1819–1825. [Google Scholar] [CrossRef]
- Martin, S.L.; Heath, G.W. A six-step model for evaluation of community-based physical activity programs. Prev. Chronic Dis. 2006, 3, A24. [Google Scholar]
- German, R.R.; Lee, L.M.; Horan, J.M.; Milstein, R.L.; Pertowski, C.A.; Waller, M.N. Updated guidelines for evaluating public health surveillance systems: Recommendations from the Guidelines Working Group. MMWR Recomm. Rep. 2001, 50, 1–35, quiz CE31–CE37. [Google Scholar]
- Brownson, R.C.; Hoehner, C.M.; Day, K.; Forsyth, A.; Sallis, J.F. Measuring the built environment for physical activity: State of the science. Am. J. Prev. Med. 2009, 36, S99–S123.e12. [Google Scholar] [CrossRef]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Pratt, M.; Sarmiento, O.L.; Montes, F.; Ogilvie, D.; Marcus, B.H.; Perez, L.G.; Brownson, R.C. The implications of megatrends in information and communication technology and transportation for changes in global physical activity. Lancet 2012, 380, 282–293. [Google Scholar] [CrossRef]
- Kohl, H.W., 3rd; Craig, C.L.; Lambert, E.V.; Inoue, S.; Alkandari, J.R.; Leetongin, G.; Kahlmeier, S. The pandemic of physical inactivity: Global action for public health. Lancet 2012, 380, 294–305. [Google Scholar] [CrossRef]
- Sallis, J.F.; Bull, F.; Guthold, R.; Heath, G.W.; Inoue, S.; Kelly, P.; Oyeyemi, A.L.; Perez, L.G.; Richards, J.; Hallal, P.C. Progress in physical activity over the Olympic quadrennium. Lancet 2016, 388, 1325–1336. [Google Scholar] [CrossRef]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.M. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef]
- Ding, D.; Lawson, K.D.; Kolbe-Alexander, T.L.; Finkelstein, E.A.; Katzmarzyk, P.T.; van Mechelen, W.; Pratt, M. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet 2016, 388, 1311–1324. [Google Scholar] [CrossRef]
- Reis, R.S.; Salvo, D.; Ogilvie, D.; Lambert, E.V.; Goenka, S.; Brownson, R.C. Scaling up physical activity interventions worldwide: Stepping up to larger and smarter approaches to get people moving. Lancet 2016, 388, 1337–1348. [Google Scholar] [CrossRef]
- Van Sluijs, E.M.F.; Ekelund, U.; Crochemore-Silva, I.; Guthold, R.; Ha, A.; Lubans, D.; Oyeyemi, A.L.; Ding, D.; Katzmarzyk, P.T. Physical activity behaviours in adolescence: Current evidence and opportunities for intervention. Lancet 2021, 398, 429–442. [Google Scholar] [CrossRef]
- Ramirez Varela, A.; Hallal, P.; Pratt, M.; Bauman, A.; Borges, C.; Lee, I.-M.; Heath, G.; Powell, K.E.; Pedisic, Z.; Klepac Pogrmilovic, B.; et al. Global Observatory for Physical Activity (GoPA!): 2nd Physical Activity Almanac, Global Observatory for Physical Activity (GoPA!). Available online: http://globalphysicalactivityobservatory.com/ (accessed on 1 August 2022).
- Martin Ginis, K.A.; van der Ploeg, H.P.; Foster, C.; Lai, B.; McBride, C.B.; Ng, K.; Pratt, M.; Shirazipour, C.H.; Smith, B.; Vásquez, P.M.; et al. Participation of people living with disabilities in physical activity: A global perspective. Lancet 2021, 398, 443–455. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Functioning, Disability, and Health: Children & Youth Version: ICF-CY; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- World Health Organization. WHO Global Disability Action Plan 2014–2021; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Madans, J.H.; Loeb, M.E.; Altman, B.M. Measuring disability and monitoring the UN Convention on the Rights of Persons with Disabilities: The work of the Washington Group on Disability Statistics. BMC Public Health 2011, 11 (Suppl. 4), S4. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Powell, K.E.; King, A.C.; Buchner, D.M.; Campbell, W.W.; DiPietro, L.; Erickson, K.I.; Hillman, C.H.; Jakicic, J.M.; Janz, K.F.; Katzmarzyk, P.T.; et al. The Scientific Foundation for the Physical Activity Guidelines for Americans, 2nd Edition. J. Phys. Act. Health 2018, 16, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. Physical Activity for General Health Benefits in Disabled Adults: Summary of a Rapid Evidence Review for the UK Chief Medical Officers’ Update of the Physical Activity Guidelines; Public Health England: London, UK, 2018. [Google Scholar]
- Weggemans, R.M.; Backx, F.J.G.; Borghouts, L.; Chinapaw, M.; Hopman, M.T.E.; Koster, A.; Kremers, S.; van Loon, L.J.C.; May, A.; Mosterd, A.; et al. The 2017 Dutch Physical Activity Guidelines. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 58. [Google Scholar] [CrossRef] [PubMed]
- Carty, C.; van der Ploeg, H.P.; Biddle, S.J.H.; Bull, F.; Willumsen, J.; Lee, L.; Kamenov, K.; Milton, K. The First Global Physical Activity and Sedentary Behavior Guidelines for People Living With Disability. J. Phys. Act. Health 2021, 18, 86–93. [Google Scholar] [CrossRef]
- Brown, D.R.; Carroll, D.D.; Workman, L.M.; Carlson, S.A.; Brown, D.W. Physical activity and health-related quality of life: US adults with and without limitations. Qual. Life Res. 2014, 23, 2673–2680. [Google Scholar] [CrossRef]
- Carroll, D.D.; Courtney-Long, E.A.; Stevens, A.C.; Sloan, M.L.; Lullo, C.; Visser, S.N.; Fox, M.H.; Armour, B.S.; Campbell, V.A.; Brown, D.R.; et al. Vital signs: Disability and physical activity—United States, 2009–2012. Morb. Mortal. Wkly. Rep. 2014, 63, 407–413. [Google Scholar]
- De Hollander, E.L.; Proper, K.I. Physical activity levels of adults with various physical disabilities. Prev. Med. Rep. 2018, 10, 370–376. [Google Scholar] [CrossRef]
- Sport England. Active Lives Adult Survey; Sport England: London, UK, 2017. [Google Scholar]
- Temple, V.A.; Stanish, H.I. Physical activity and persons with intellectual disability: Some considerations for Latin America. Salud. Publica. Mex. 2008, 50 (Suppl. 2), 185–193. [Google Scholar] [CrossRef]
- Taechaboonsermsak, P.; Pitikultang, S.; Munsawaengsub, C.; Charupoonphol, P. Quality of life and health promoting behaviors among disabled people in two provinces of Thailand. J. Med. Assoc. Thai. 2009, 92 (Suppl. 7), S54–S58. [Google Scholar]
- Mat Rosly, M.; Halaki, M.; Hasnan, N.; Mat Rosly, H.; Davis, G.M.; Husain, R. Leisure time physical activity participation in individuals with spinal cord injury in Malaysia: Barriers to exercise. Spinal Cord 2018, 56, 806–818. [Google Scholar] [CrossRef]
- Ahmad, N.A.; Mohamad Kasim, N.; Mahmud, N.A.; Mohd Yusof, Y.; Othman, S.; Chan, Y.Y.; Abd Razak, M.A.; Yusof, M.; Omar, M.; Abdul Aziz, F.A.; et al. Prevalence and determinants of disability among adults in Malaysia: Results from the National Health and Morbidity Survey (NHMS) 2015. BMC Public Health 2017, 17, 756. [Google Scholar] [CrossRef] [PubMed]
- Oyeyemi, A.L.; Oyeyemi, A.Y.; Omotara, B.A.; Lawan, A.; Akinroye, K.K.; Adedoyin, R.A.; Ramírez, A. Physical activity profile of Nigeria: Implications for research, surveillance and policy. Pan Afr. Med. J. 2018, 30, 175. [Google Scholar] [CrossRef] [PubMed]
- Ng, K.; Tynjälä, J.; Sigmundová, D.; Augustine, L.; Sentenac, M.; Rintala, P.; Inchley, J. Physical Activity Among Adolescents With Long-Term Illnesses or Disabilities in 15 European Countries. Adapt. Phys. Activ. Q. 2017, 34, 456–465. [Google Scholar] [CrossRef]
- Wilson, P.B.; Haegele, J.A.; Zhu, X. Mobility Status as a Predictor of Obesity, Physical Activity, and Screen Time Use among Children Aged 5–11 Years in the United States. J. Pediatr. 2016, 176, 23–29.e21. [Google Scholar] [CrossRef] [PubMed]
- Arim, R.G.; Findlay, L.C.; Kohen, D.E. Participation in physical activity for children with neurodevelopmental disorders. Int. J. Pediatr. 2012, 2012, 460384. [Google Scholar] [CrossRef] [PubMed]
- GBD 2016 Stroke Collaborators. Global, regional, and national burden of stroke, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 439–458. [Google Scholar] [CrossRef]
- Chiu, T.Y.; Yen, C.F.; Escorpizo, R.; Chi, W.C.; Liou, T.H.; Liao, H.F.; Chou, C.H.; Fang, W.H. What is the gap in activity and participation between people with disability and the general population in Taiwan? Int. J. Equity Health 2017, 16, 136. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef]
- Ginis, K.A.; Latimer, A.E.; Hicks, A.L.; Craven, B.C. Development and evaluation of an activity measure for people with spinal cord injury. Med. Sci. Sports Exerc. 2005, 37, 1099–1111. [Google Scholar] [CrossRef]
- Latimer, A.E.; Ginis, K.A.; Craven, B.C.; Hicks, A.L. The physical activity recall assessment for people with spinal cord injury: Validity. Med. Sci. Sports Exerc. 2006, 38, 208–216. [Google Scholar] [CrossRef]
- Matin, P. Bone scintigraphy in the diagnosis and management of traumatic injury. Semin. Nucl. Med. 1983, 13, 104–122. [Google Scholar] [CrossRef]
- Murphy, S.L.; Kratz, A.L.; Zynda, A.J. Measuring Physical Activity in Spinal Cord Injury Using Wrist-Worn Accelerometers. Am. J. Occup. Ther. 2019, 73, 7301205090p1–7301205090p10. [Google Scholar] [CrossRef] [PubMed]
- McCracken, L.A.; Ma, J.K.; Voss, C.; Chan, F.H.; Martin Ginis, K.A.; West, C.R. Wrist Accelerometry for Physical Activity Measurement in Individuals with Spinal Cord Injury—A Need for Individually Calibrated Cut-Points. Arch. Phys. Med. Rehabil. 2018, 99, 684–689. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.K.; McCracken, L.A.; Voss, C.; Chan, F.H.N.; West, C.R.; Martin Ginis, K.A. Physical activity measurement in people with spinal cord injury: Comparison of accelerometry and self-report (the Physical Activity Recall Assessment for People with Spinal Cord Injury). Disabil. Rehabil. 2020, 42, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Brogioli, M.; Popp, W.L.; Schneider, S.; Albisser, U.; Brust, A.K.; Frotzler, A.; Gassert, R.; Curt, A.; Starkey, M.L. Multi-Day Recordings of Wearable Sensors Are Valid and Sensitive Measures of Function and Independence in Human Spinal Cord Injury. J. Neurotrauma 2017, 34, 1141–1148. [Google Scholar] [CrossRef] [PubMed]
- Fini, N.A.; Holland, A.E.; Keating, J.; Simek, J.; Bernhardt, J. How is physical activity monitored in people following stroke? Disabil. Rehabil. 2015, 37, 1717–1731. [Google Scholar] [CrossRef] [PubMed]
- Saunders, D.H.; Sanderson, M.; Hayes, S.; Johnson, L.; Kramer, S.; Carter, D.D.; Jarvis, H.; Brazzelli, M.; Mead, G.E. Physical fitness training for stroke patients. Cochrane Database Syst. Rev. 2020, 3, Cd003316. [Google Scholar] [CrossRef]
- Martins, J.C.; Aguiar, L.T.; Nadeau, S.; Scianni, A.A.; Teixeira-Salmela, L.F.; Faria, C. Measurement properties of self-report physical activity assessment tools for patients with stroke: A systematic review. Braz. J. Phys. Ther. 2019, 23, 476–490. [Google Scholar] [CrossRef]
- Bernaldo de Quirós, M.; Douma, E.H.; van den Akker-Scheek, I.; Lamoth, C.J.C.; Maurits, N.M. Quantification of Movement in Stroke Patients under Free Living Conditions Using Wearable Sensors: A Systematic Review. Sensors 2022, 22, 1050. [Google Scholar] [CrossRef]
- Machado, N.; Wingfield, M.; Kramer, S.; Olver, J.; Williams, G.; Johnson, L. Maintenance of Cardiorespiratory Fitness in People With Stroke: A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2022, 103, 1410–1421. [Google Scholar] [CrossRef]
- Lynch, E.A.; Jones, T.M.; Simpson, D.B.; Fini, N.A.; Kuys, S.S.; Borschmann, K.; Kramer, S.; Johnson, L.; Callisaya, M.L.; Mahendran, N.; et al. Activity monitors for increasing physical activity in adult stroke survivors. Cochrane Database Syst. Rev. 2018, 7, Cd012543. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.; Godfrey, A.; Galna, B.; Mhiripiri, D.; Burn, D.; Rochester, L. Ambulatory activity in incident Parkinson’s: More than meets the eye? J. Neurol. 2013, 260, 2964–2972. [Google Scholar] [CrossRef]
- Li, F.; Harmer, P.; Fitzgerald, K.; Eckstrom, E.; Stock, R.; Galver, J.; Maddalozzo, G.; Batya, S.S. Tai chi and postural stability in patients with Parkinson’s disease. N. Engl. J. Med. 2012, 366, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Ånfors, S.; Kammerlind, A.S.; Nilsson, M.H. Test-retest reliability of physical activity questionnaires in Parkinson’s disease. BMC Neurol. 2021, 21, 399. [Google Scholar] [CrossRef]
- Van Uem, J.M.T.; Cerff, B.; Kampmeyer, M.; Prinzen, J.; Zuidema, M.; Hobert, M.A.; Gräber, S.; Berg, D.; Maetzler, W.; Liepelt-Scarfone, I. The association between objectively measured physical activity, depression, cognition, and health-related quality of life in Parkinson’s disease. Parkinsonism Relat. Disord. 2018, 48, 74–81. [Google Scholar] [CrossRef]
- Urell, C.; Zetterberg, L.; Hellström, K.; Anens, E. Factors explaining physical activity level in Parkinson’s disease: A gender focus. Physiother. Theory Pract. 2021, 37, 507–516. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, S.; Kelly, V.E. Quantifying physical activity in early Parkinson disease using a commercial activity monitor. Parkinsonism Relat. Disord. 2019, 66, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Von Rosen, P.; Hagströmer, M.; Franzén, E.; Leavy, B. Physical activity profiles in Parkinson’s disease. BMC Neurol. 2021, 21, 71. [Google Scholar] [CrossRef] [PubMed]
- Breasail, M.; Biswas, B.; Smith, M.D.; Mazhar, M.K.A.; Tenison, E.; Cullen, A.; Lithander, F.E.; Roudaut, A.; Henderson, E.J. Wearable GPS and Accelerometer Technologies for Monitoring Mobility and Physical Activity in Neurodegenerative Disorders: A Systematic Review. Sensors 2021, 21, 8261. [Google Scholar] [CrossRef]
- Ito, H.; Yokoi, D.; Kobayashi, R.; Okada, H.; Kajita, Y.; Okuda, S. The relationships between three-axis accelerometer measures of physical activity and motor symptoms in patients with Parkinson’s disease: A single-center pilot study. BMC Neurol. 2020, 20, 340. [Google Scholar] [CrossRef]
- Johansen, M.; Rasmussen, H.M.; Lauruschkus, K.; Laugesen, B. Measurement of physical activity in children and adolescents with cerebral palsy: A scoping review protocol. JBI Evid. Synth. 2021, 19, 2339–2349. [Google Scholar] [CrossRef] [PubMed]
- Verschuren, O.; Peterson, M.D.; Balemans, A.C.; Hurvitz, E.A. Exercise and physical activity recommendations for people with cerebral palsy. Dev. Med. Child Neurol. 2016, 58, 798–808. [Google Scholar] [CrossRef] [PubMed]
- Lennon, N.; Thorpe, D.; Balemans, A.C.; Fragala-Pinkham, M.; O’Neil, M.; Bjornson, K.; Boyd, R.; Dallmeijer, A.J. The clinimetric properties of aerobic and anaerobic fitness measures in adults with cerebral palsy: A systematic review of the literature. Res. Dev. Disabil. 2015, 45–46, 316–328. [Google Scholar] [CrossRef] [PubMed]
- Fonvig, C.E.; Troelsen, J.; Dunkhase-Heinl, U.; Lauritsen, J.M.; Holsgaard-Larsen, A. Predictors of physical activity levels in children and adolescents with cerebral palsy: Clinical cohort study protocol. BMJ Open 2021, 11, e047522. [Google Scholar] [CrossRef] [PubMed]
- Lavelle, G.; Noorkoiv, M.; Theis, N.; Korff, T.; Kilbride, C.; Baltzopoulos, V.; Shortland, A.; Levin, W.; Ryan, J.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF) as a measure of physical activity (PA) in young people with cerebral palsy: A cross-sectional study. Physiotherapy 2020, 107, 209–215. [Google Scholar] [CrossRef]
- Kwon, K.B.; Choi, Y.; Sung, K.H.; Chung, C.Y.; Lee, K.M.; Kwon, S.S.; Cho, G.H.; Park, M.S. Correlation between Accelerometer and Questionnaire-Based Assessment of Physical Activity in Patients with Cerebral Palsy. Clin. Orthop. Surg. 2020, 12, 107–112. [Google Scholar] [CrossRef]
- Longo, E.; Badia, M.; Orgaz, B.M. Patterns and predictors of participation in leisure activities outside of school in children and adolescents with Cerebral Palsy. Res. Dev. Disabil. 2013, 34, 266–275. [Google Scholar] [CrossRef]
- Bjornson, K.F.; Belza, B.; Kartin, D.; Logsdon, R.; McLaughlin, J.; Thompson, E.A. The relationship of physical activity to health status and quality of life in cerebral palsy. Pediatr. Phys. Ther. 2008, 20, 247–253. [Google Scholar] [CrossRef]
- Buffart, L.M.; Roebroeck, M.E.; Rol, M.; Stam, H.J.; van den Berg-Emons, R.J. Triad of physical activity, aerobic fitness and obesity in adolescents and young adults with myelomeningocele. J. Rehabil. Med. 2008, 40, 70–75. [Google Scholar] [CrossRef]
- O’Neil, M.E.; Fragala-Pinkham, M.; Lennon, N.; George, A.; Forman, J.; Trost, S.G. Reliability and Validity of Objective Measures of Physical Activity in Youth With Cerebral Palsy Who Are Ambulatory. Phys. Ther. 2016, 96, 37–45. [Google Scholar] [CrossRef]
- Orlando, J.M.; Pierce, S.; Mohan, M.; Skorup, J.; Paremski, A.; Bochnak, M.; Prosser, L.A. Physical activity in non-ambulatory toddlers with cerebral palsy. Res. Dev. Disabil. 2019, 90, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Ryan, J.M.; Cassidy, E.E.; Noorduyn, S.G.; O’Connell, N.E. Exercise interventions for cerebral palsy. Cochrane Database Syst. Rev. 2017, 6, Cd011660. [Google Scholar] [CrossRef]
- Tomasone, J.R.; Martin Ginis, K.A.; Estabrooks, P.A.; Domenicucci, L. ‘Changing minds’: Determining the effectiveness and key ingredients of an educational intervention to enhance healthcare professionals’ intentions to prescribe physical activity to patients with physical disabilities. Implement. Sci. 2014, 9, 30. [Google Scholar] [CrossRef] [PubMed]
- Hoekstra, F.; Hoekstra, T.; van der Schans, C.P.; Hettinga, F.J.; van der Woude, L.H.V.; Dekker, R. The implementation of a physical activity counseling program in rehabilitation care: Findings from the ReSpAct study. Disabil. Rehabil. 2021, 43, 1710–1721. [Google Scholar] [CrossRef] [PubMed]
- Hoekstra, F.; Mrklas, K.J.; Khan, M.; McKay, R.C.; Vis-Dunbar, M.; Sibley, K.M.; Nguyen, T.; Graham, I.D.; Gainforth, H.L. A review of reviews on principles, strategies, outcomes and impacts of research partnerships approaches: A first step in synthesising the research partnership literature. Health Res. Policy Syst. 2020, 18, 51. [Google Scholar] [CrossRef] [PubMed]
- Hoekstra, F.; Roberts, L.; van Lindert, C.; Martin Ginis, K.A.; van der Woude, L.H.V.; McColl, M.A. National approaches to promote sports and physical activity in adults with disabilities: Examples from the Netherlands and Canada. Disabil. Rehabil. 2019, 41, 1217–1226. [Google Scholar] [CrossRef]
- Shikako-Thomas, K.; Law, M. Policies supporting participation in leisure activities for children and youth with disabilities in Canada: From policy to play. Disabil. Soc. 2015, 30, 381–400. [Google Scholar] [CrossRef]
- Martin Ginis, K.A.; Evans, M.B.; Mortenson, W.B.; Noreau, L. Broadening the Conceptualization of Participation of Persons With Physical Disabilities: A Configurative Review and Recommendations. Arch. Phys. Med. Rehabil. 2017, 98, 395–402. [Google Scholar] [CrossRef]
- Martin Ginis, K.A.; Ma, J.K.; Latimer-Cheung, A.E.; Rimmer, J.H. A systematic review of review articles addressing factors related to physical activity participation among children and adults with physical disabilities. Health Psychol. Rev. 2016, 10, 478–494. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef] [PubMed]
- Heath, G.W.; Brownson, R.C.; Kruger, J.; Miles, R.; Powell, K.E.; Ramsey, L.T. The Effectiveness of Urban Design and Land Use and Transport Policies and Practices to Increase Physical Activity: A Systematic Review. J. Phys. Act. Health 2006, 3, S55–S76. [Google Scholar] [CrossRef] [PubMed]
- Heath, G.W.; Parra, D.C.; Sarmiento, O.L.; Andersen, L.B.; Owen, N.; Goenka, S.; Montes, F.; Brownson, R.C. Evidence-based intervention in physical activity: Lessons from around the world. Lancet 2012, 380, 272–281. [Google Scholar] [CrossRef]
- Baker, P.R.; Francis, D.P.; Soares, J.; Weightman, A.L.; Foster, C. Community wide interventions for increasing physical activity. Cochrane Database Syst. Rev. 2015, 1, Cd008366. [Google Scholar] [CrossRef]
- Shields, N.; Synnot, A. Perceived barriers and facilitators to participation in physical activity for children with disability: A qualitative study. BMC Pediatr. 2016, 16, 9. [Google Scholar] [CrossRef]
- White, G.W.; Gonda, C.; Peterson, J.J.; Drum, C.E. Secondary analysis of a scoping review of health promotion interventions for persons with disabilities: Do health promotion interventions for people with mobility impairments address secondary condition reduction and increased community participation? Disabil. Health J. 2011, 4, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Shirazipour, C.H.; Evans, M.B.; Leo, J.; Lithopoulos, A.; Martin Ginis, K.A.; Latimer-Cheung, A.E. Program conditions that foster quality physical activity participation experiences for people with a physical disability: A systematic review. Disabil. Rehabil. 2020, 42, 147–155. [Google Scholar] [CrossRef]
- Adam, S.L.; Morgan, K.A. Meaningful components of a community-based exercise program for individuals with disabilities: A qualitative study. Disabil. Health J. 2018, 11, 301–305. [Google Scholar] [CrossRef]
- Sallis, J.F.; Bull, F.; Burdett, R.; Frank, L.D.; Griffiths, P.; Giles-Corti, B.; Stevenson, M. Use of science to guide city planning policy and practice: How to achieve healthy and sustainable future cities. Lancet 2016, 388, 2936–2947. [Google Scholar] [CrossRef]
- Giles-Corti, B.; Vernez-Moudon, A.; Reis, R.; Turrell, G.; Dannenberg, A.L.; Badland, H.; Foster, S.; Lowe, M.; Sallis, J.F.; Stevenson, M.; et al. City planning and population health: A global challenge. Lancet 2016, 388, 2912–2924. [Google Scholar] [CrossRef]
- Schmid, T.L.; Pratt, M.; Witmer, L. A Framework for Physical Activity Policy Research. J. Phys. Act. Health 2006, 3, S20–S29. [Google Scholar] [CrossRef]
- Bleich, S.N.; Sturm, R. Developing policy solutions for a more active nation: Integrating economic and public health perspectives. Prev. Med. 2009, 49, 306–308. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.; Sarmiento, O.L.; Stauber, C.; Zarama, R. The Ciclovia and Cicloruta programs: Promising interventions to promote physical activity and social capital in Bogotá, Colombia. Am. J. Public Health 2013, 103, e23–e30. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, Y.; Vanderbom, K.A.; Vasudevan, V. Does the built environment moderate the relationship between having a disability and lower levels of physical activity? A systematic review. Prev. Med. 2017, 95, S75–S84. [Google Scholar] [CrossRef] [PubMed]
- Community Preventive Services Task Force. Physical Activity: Built Environment Approaches Combining Transportation System Interventions with Land Use and Environmental Design. 2016. Available online: https://www.thecommunityguide.org/findings/physical-activity-built-environment-approaches (accessed on 1 August 2022).
- Bodde, A.E.; Seo, D.C. A review of social and environmental barriers to physical activity for adults with intellectual disabilities. Disabil. Health J. 2009, 2, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Blauwet, C.A.; Iezzoni, L.I. From the Paralympics to public health: Increasing physical activity through legislative and policy initiatives. PMR 2014, 6, S4–S10. [Google Scholar] [CrossRef] [PubMed]
- Bloemen, M.A.; Backx, F.J.; Takken, T.; Wittink, H.; Benner, J.; Mollema, J.; de Groot, J.F. Factors associated with physical activity in children and adolescents with a physical disability: A systematic review. Dev. Med. Child Neurol. 2015, 57, 137–148. [Google Scholar] [CrossRef]
- Calder, A.; Sole, G.; Mulligan, H. The accessibility of fitness centers for people with disabilities: A systematic review. Disabil. Health J. 2018, 11, 525–536. [Google Scholar] [CrossRef] [PubMed]
- Gainforth, H.L.; Hoekstra, F.; McKay, R.; McBride, C.B.; Sweet, S.N.; Martin Ginis, K.A.; Anderson, K.; Chernesky, J.; Clarke, T.; Forwell, S.; et al. Integrated Knowledge Translation Guiding Principles for Conducting and Disseminating Spinal Cord Injury Research in Partnership. Arch. Phys. Med. Rehabil. 2021, 102, 656–663. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).