Improving the Treatment Outcome of Naso-Orbito-Ethmoido-Maxillary Fractures Using Virtual Three-Dimensional Anthropometric Data
Abstract
:1. Introduction
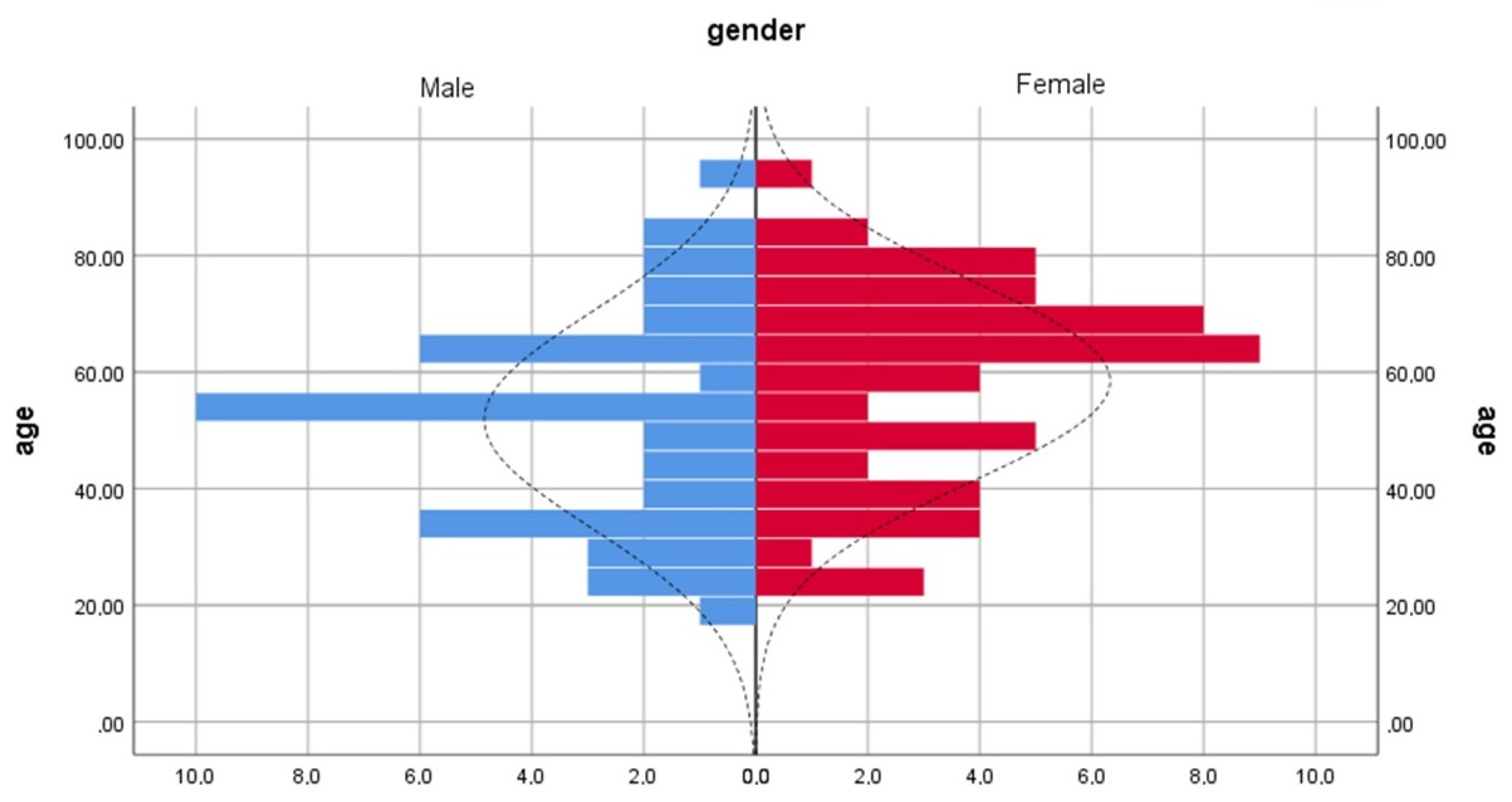
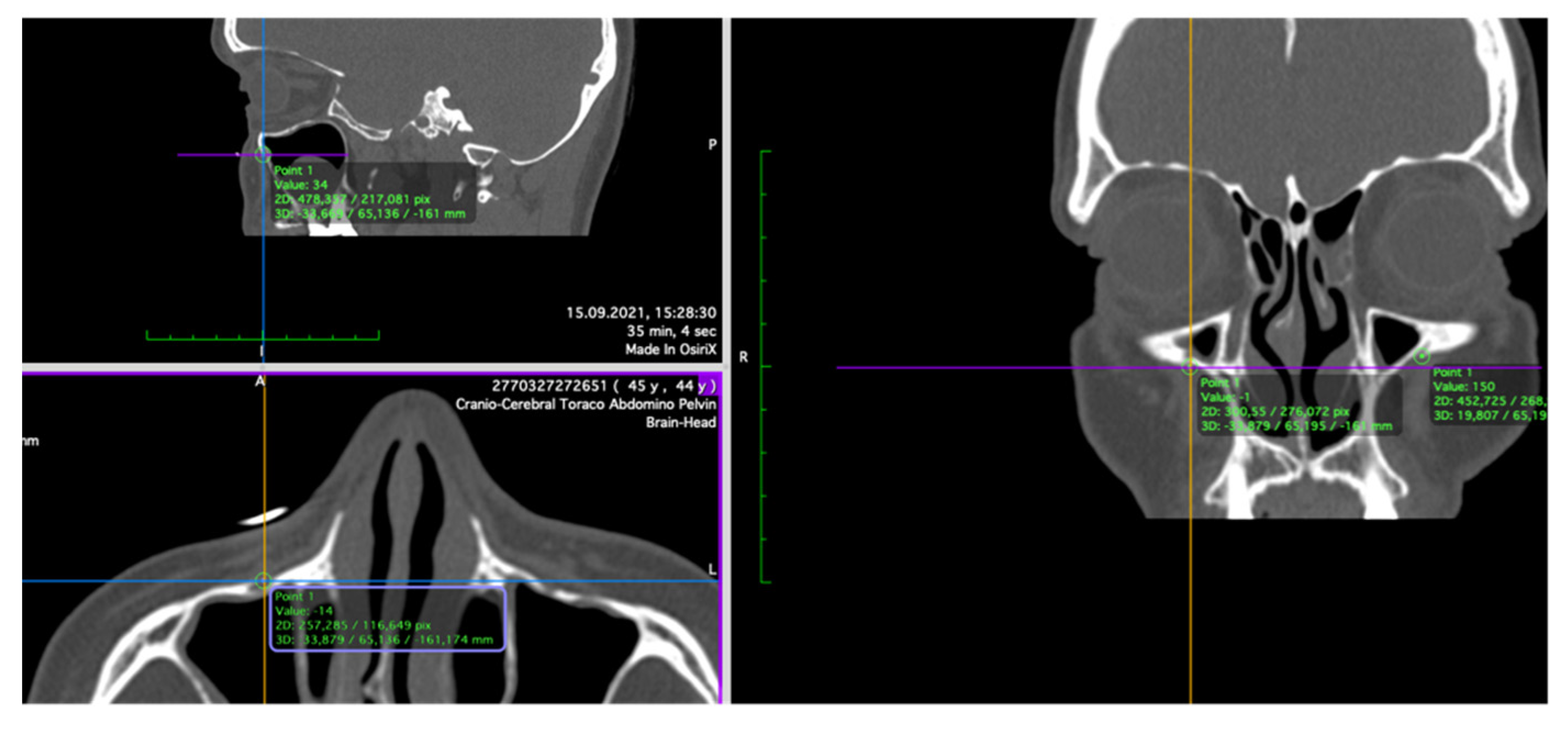
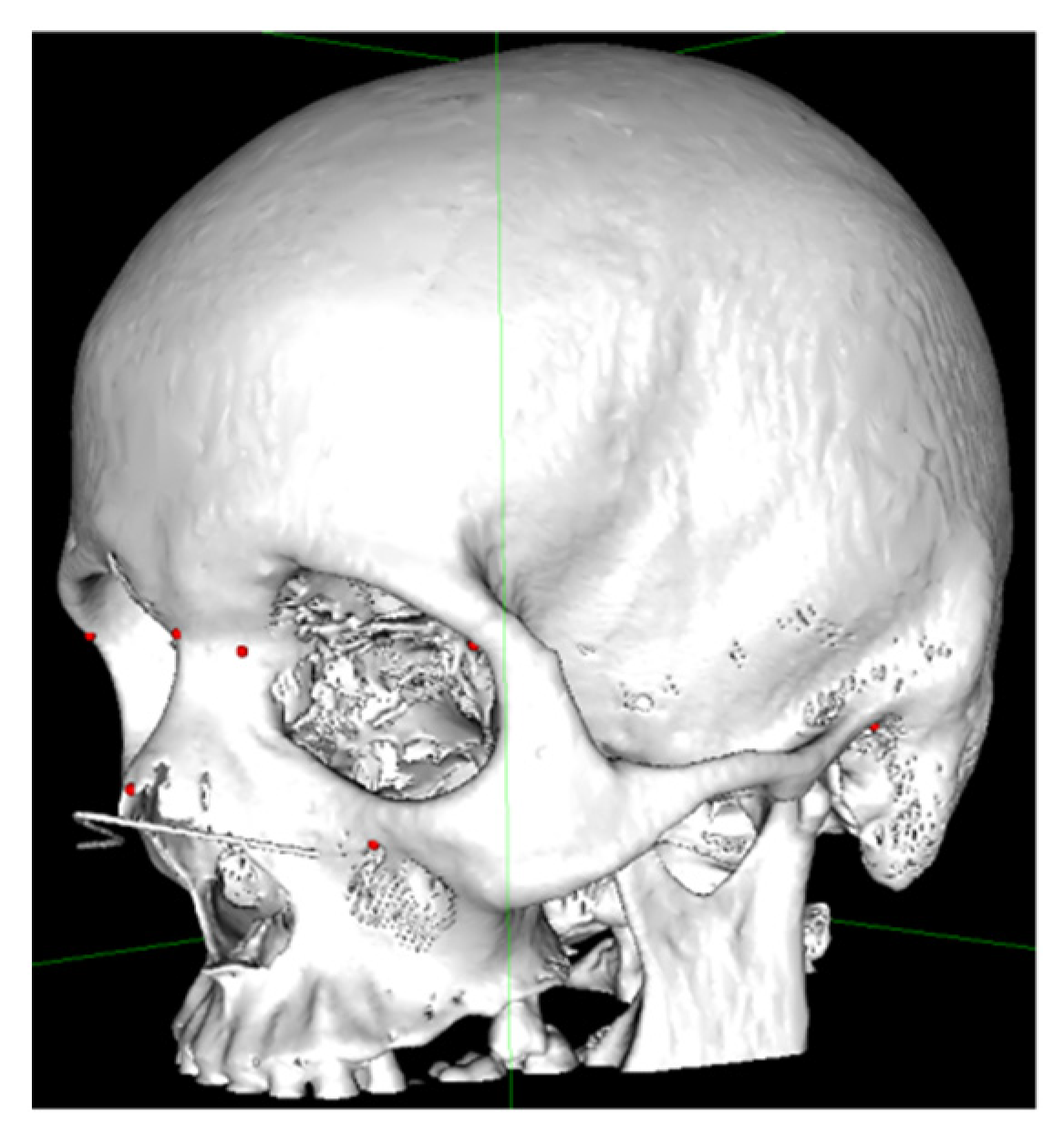
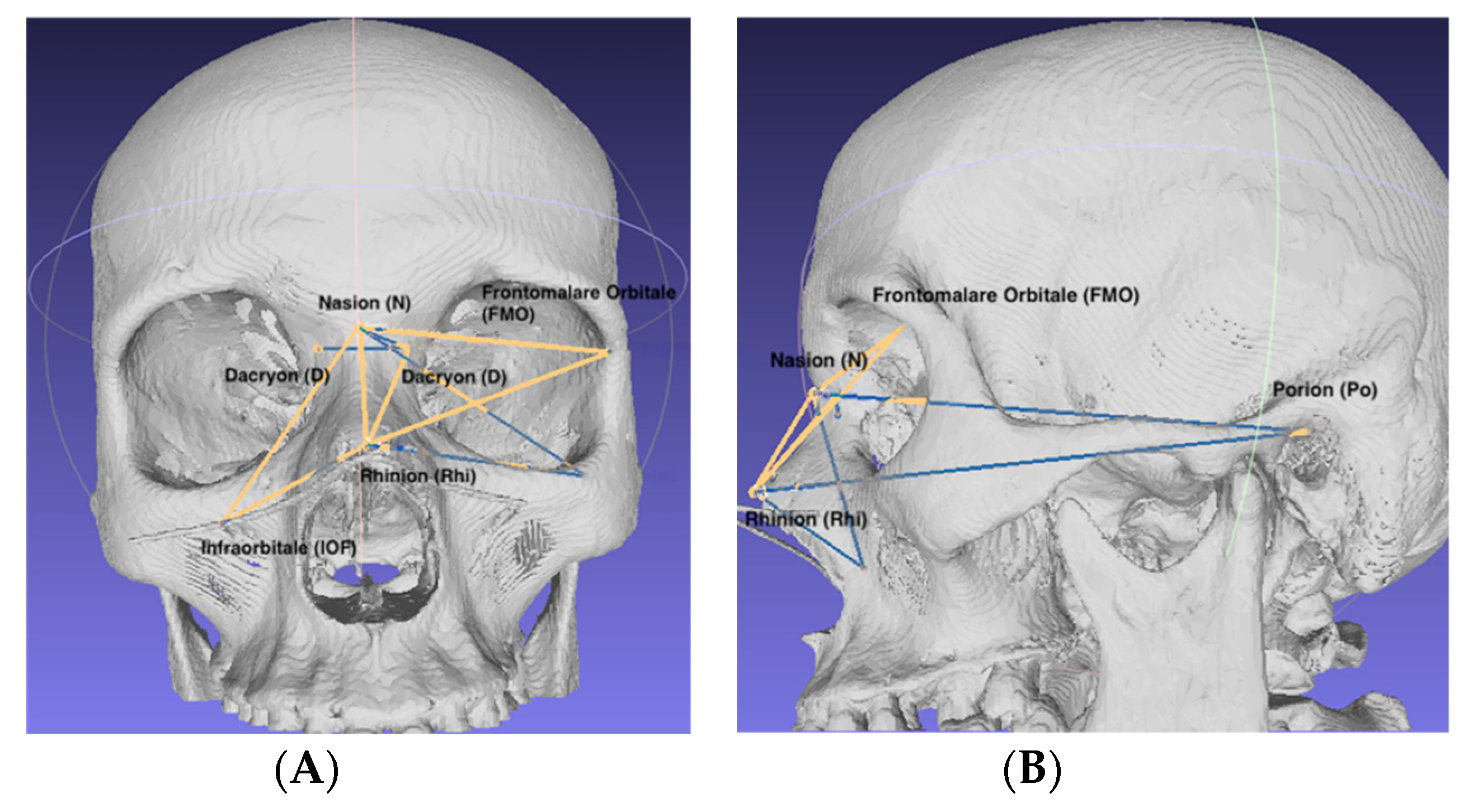
2. Materials and Methods
- Nasion (N): the most anterior point located at the middle line where the frontal and nasal bones meet [5];
- Dacryon (D): the point of junction of the maxillary, lacrimal and frontal bones [5];
- Infraorbital foramen (IOF): the anterior opening of the infraorbital canal;
- Rhinion (Rhi): the anterior tip of the nasal bones suture [5];
- Frontomalare Orbitale (FMO): the fronto-malar suture [6];
- Porion (Po): The most superior point on the upper margin of the external auditory meatus [6].
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Apinhasmit, W.; Chompoopong, S.; Methathrathip, D.; Sansuk, R.; Phetphunphiphat, W. Supraorbital notch/foramen, infraorbital foramen and mental foramen in Thais: Anthropometric measurements and surgical relevance. J. Med. Assoc. Thai 2006, 89, 675–682. [Google Scholar] [PubMed]
- Aziz, S.; Marchena, J.; Puran, A. Anatomic characteristics of the infraorbital foramen: A cadaver study. J. Oral Maxillofac. Surg. 2000, 58, 992–996. [Google Scholar] [CrossRef] [PubMed]
- Vigo, V.; Cornejo, K.; Nunez, L.; Abla, A.; Rubio, R.R. Immersive surgical anatomy of the craniometric points. Cureus 2020, 12, e8643. [Google Scholar] [CrossRef] [PubMed]
- Dias, P.; Santos, D.; Souza, D.; Santos, H.; Coelho, C.; Ferreira, M.T.; Santos, B.S. A new approach for 3D craniometric measurements using 3D skull models. In Proceedings of the 2013 17th International Conference on Information Visualisation, London, UK, 16–18 July 2013. [Google Scholar] [CrossRef]
- Damas, S.; Cordon, O.; Ibanez, O. Handbook on Cranifacial Superimposition; Springer: Cham, Switzerland, 2020; pp. 12–25. ISBN 978-3-319-11136-0. [Google Scholar]
- Caple, J.; Stephan, C.N. A standardized nomenclature for craniofacial and facial anthropometry. Int. J. Leg. Med. 2015, 130, 863–879. [Google Scholar] [CrossRef]
- Perry, M.; Holmes, S. Atlas of Operative Maxillofacial Trauma Surgery; Springer: London, UK; Heidelberg, Germany; New York, NY, USA; Dordrecht, The Netherlands, 2014; pp. 485–492. [Google Scholar]
- Varun Menon, P.; Surej Kumar, L.K.; Sherin, A.k. Naso-orbito-ethmoid fractures: An overview. J. Head Neck Physicians Surg. 2014, 2, 46–53. [Google Scholar]
- Sargent, L.A.; Rogers, G.F. Nasoethmoid orbital fractures: Diagnosis and management. J. Cranio-Maxillofac. Trauma 1999, 5, 19. [Google Scholar]
- Paskert, J.P.; Manson, P.N.; Iliff, N.T. Nasoethmoidal and orbital fractures. Clin. Plast. Sur. 1988, 15209–15223. [Google Scholar] [CrossRef]
- Etemadi, M.; Shahnaseri, S.; Soltani, P.; Kalantar, M.R. Management of nose-orbit-ethmoid fractures: A 10-year review. Trauma Mon. 2017, 22, e29230. [Google Scholar]
- Baril, S.E.; Yoon, M.K. Nose-orbito-ethmoidal (NOEM) fractures: A review. Int. Ophthalmol. Clin. 2013, 53, 149–155. [Google Scholar] [CrossRef]
- Fraioli, R.E.; Branstetter, B.; Deleyiannis, F.W. Facial fractures: Beyond Le Fort. Otolaryngol. Clin. N. Am. 2008, 41, 51–76. [Google Scholar] [CrossRef]
- Costan, V.V.; Popescu, E.; Sulea, D.; Stratulat, I.S. A new indication for barbedthreads: Static reanimation of the paralyzed face. J. Oral Maxillofac. Surg. 2018, 76, 639–645. [Google Scholar] [CrossRef] [PubMed]
- Naran, S.; Wes, A.M.; Mazzaferro, D.M.; Bartlett, S.P.; Taylor, J.A. More than meets the eye: The effect of intercanthal distance on perception of beauty and personality. J. Craniofac. Surg. 2018, 29, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Kun, H.; Fan, H.; YongSeok, N.; Seung Ho, H.; DaeJoong, K. Location and tension of the medial palpebral tendon. J. Craniofac. Surg. 2013, 24, 2119–2123. [Google Scholar] [CrossRef]
- Hierl, K.V.; Krause, M.; Kruber, D.; Sterker, I. 3-D cephalometry of the orbit regarding endocrine orbitopathy, exophthalmos, and sex. PLoS ONE 2022, 17, e0265324. [Google Scholar] [CrossRef] [PubMed]
- Siva Rama Krishna, L.; Balasany, U.K.; Venkatesh, S.R.; Potturi, A. Assessment of dimensional accuracy of reproducibility of cadaver skull by FDM additive manufacturing. In Learning and Analytics in Intelligent Systems, Proceedings of the International Conference on Emerging Trends in Engineering (ICETE), Online Event, 8–10 July 2020; Satapathy, S., Raju, K., Molugaram, K., Krishnaiah, A., Tsihrintzis, G., Eds.; Springer: Cham, Switzerland, 2020; Volume 2. [Google Scholar] [CrossRef]
- Farkas, L.G.; Katic, M.J.; Forrest, C.R.; Alt, K.W.; Bagic, I.; Baltadjiev, G.; Cunha, E.; Cvicelová, M.; Davies, S.; Erasmus, I.; et al. International anthropometric study of facial morphology in various ethnic groups/races. J. Craniofac. Surg. 2005, 16, 615–646. [Google Scholar] [CrossRef] [PubMed]
- Budai, M.; Farkas, L.G.; Tompson, B.; Katic, M.; Forrest, C.R. Relation between anthropometric and cephalometric measurements and proportions of the face of healthy young white adult men and women. J. Craniofac. Surg. 2003, 14, 154–163. [Google Scholar] [CrossRef]
- Przygocka, A.; Podgórski, M.; Jędrzejewski, K.; Topol, M.; Polguj, M. The location of the infraorbital foramen in human skulls, to be used as new anthropometric landmarks as a useful method for maxillofacial surgery. Morphol. Folia 2012, 71, 198–204. [Google Scholar]
- Zacharopoulos, G.V.; Manios, A.; Kau, C.H.; Velagrakis, G.; Tzanakakis, G.N.; de Bree, E. Anthropometric analysis of the face. J. Craniofac. Surg. 2016, 27, e71–e75. [Google Scholar] [CrossRef]
- Sharaf, B.A.; Morris, J.M.; Kuruoglu, D. EPPOCRATIS: A point-of-care utilization of virtual surgical planning and three-dimensional printing for the management of acute craniomaxillofacial trauma. J. Clin. Med. 2021, 10, 5640. [Google Scholar] [CrossRef]
- Rosu, A.; Sulea, D.; Rosu, O.; Cobzeanu, M.; Bandol, G.; Moisii, L.; Cobzeanu, L.; Costan, V.; Palade, D.; Cobzeanu, B. Anthropometric aspects used to treat fractures of the naso-orbito-ethmoido-maxillar (NOEM) complex in cases of facial trauma. Rom. J. Rhinol. 2022, 12, 71–77. [Google Scholar] [CrossRef]
- Boopathi, S.; Chakravarthy Marx, S.; Dhalapathy, S.; Anupa, S. Anthropometric analysis of the infraorbital foramen in South Indian population. Singap. Med. J. 2012, 51, 730–735. [Google Scholar]
- Kang, H.; Takahashi, Y.; Nakano, T.; Asamoto, K.; Ikeda, H.; Kakizaki, H. Medial canthal support structures: The medial retinaculum: A review. Ann. Plast. Surg. 2015, 74, 508–514. [Google Scholar] [CrossRef] [PubMed]
- Ozer, M.A.; Govsa, F.; Kazak, Z.; Erdogmus, S.; Celik, S. Redesign and treatment planning orbital floor reconstruction using computer analysis anatomical landmarks. Eur. Arch. Otorhinolaryngol. 2016, 273, 2185–2191. [Google Scholar] [CrossRef] [PubMed]
- Pagnoni, M.; Marenco, M.; Ramieri, V.; Terenzi, V.; Bartoli, D.; Amodeo, G.; Mazzoli, A.; Iannetti, G. Late treatment of orbital fractures: A new analysis for surgical planning. Acta Otorhinolaryngol. Ital. Organo Soc. Ital. Otorinolaringol. Chir. Cervico-Facc. 2014, 34, 439–445. [Google Scholar]
- Wi, J.M.; Sung, K.H.; Chi, M. ‘Orbital volume restoration rate after orbital fracture’; A CT-based orbital volume measurement for evaluation of orbital wall reconstructive effect. Eye 2017, 31, 713–719. [Google Scholar] [CrossRef]
- Shaye, D.A. The history of nasal reconstruction. Curr. Opin. Otolaryngol. Head Neck Surg. 2021, 29, 259–264. [Google Scholar] [CrossRef]
- Roşca, Ș.; Silistraru, I.; Bulgaru-Iliescu, D.; Severin, F.; Alexa, A.I.; Dorobăţ, C.; Ciureanu, I.A. Patient’s rights and patient’s data protection in the Romanian health system: Ready for the change? Int. J. Med. Dent. 2019, 23, 155–162. [Google Scholar]
- Gribel, B.F.; Gribel, M.N.; Frazão, D.C.; McNamara, J.A.; Manzi, F.R. Accuracy and reliability of craniometric measurements on lateral cephalometry and 3D measurements on CBCT scans. Angle Orthod. 2011, 81, 26–35. [Google Scholar] [CrossRef]
- Ross, A.H.; Williams, S. Testing repeatability and error of coordinate landmark data acquired from crania. J. Forensic Sci. 2008, 53, 782–785. [Google Scholar] [CrossRef]
- Campomanes-Álvarez, B.R.; Ibáñez, O.; Navarro, F.; Alemán, I.; Cordón, O.; Damas, S. Dispersion assessment in the location of facial landmarks on photographs. Int. J. Legal Med. 2014, 129, 227–236. [Google Scholar] [CrossRef]
- Bookstein, L. Morphometric Tools for Landmark Data: Geometry and Biology; Cambridge University Press: Cambridge, UK, 1991. [Google Scholar] [CrossRef]
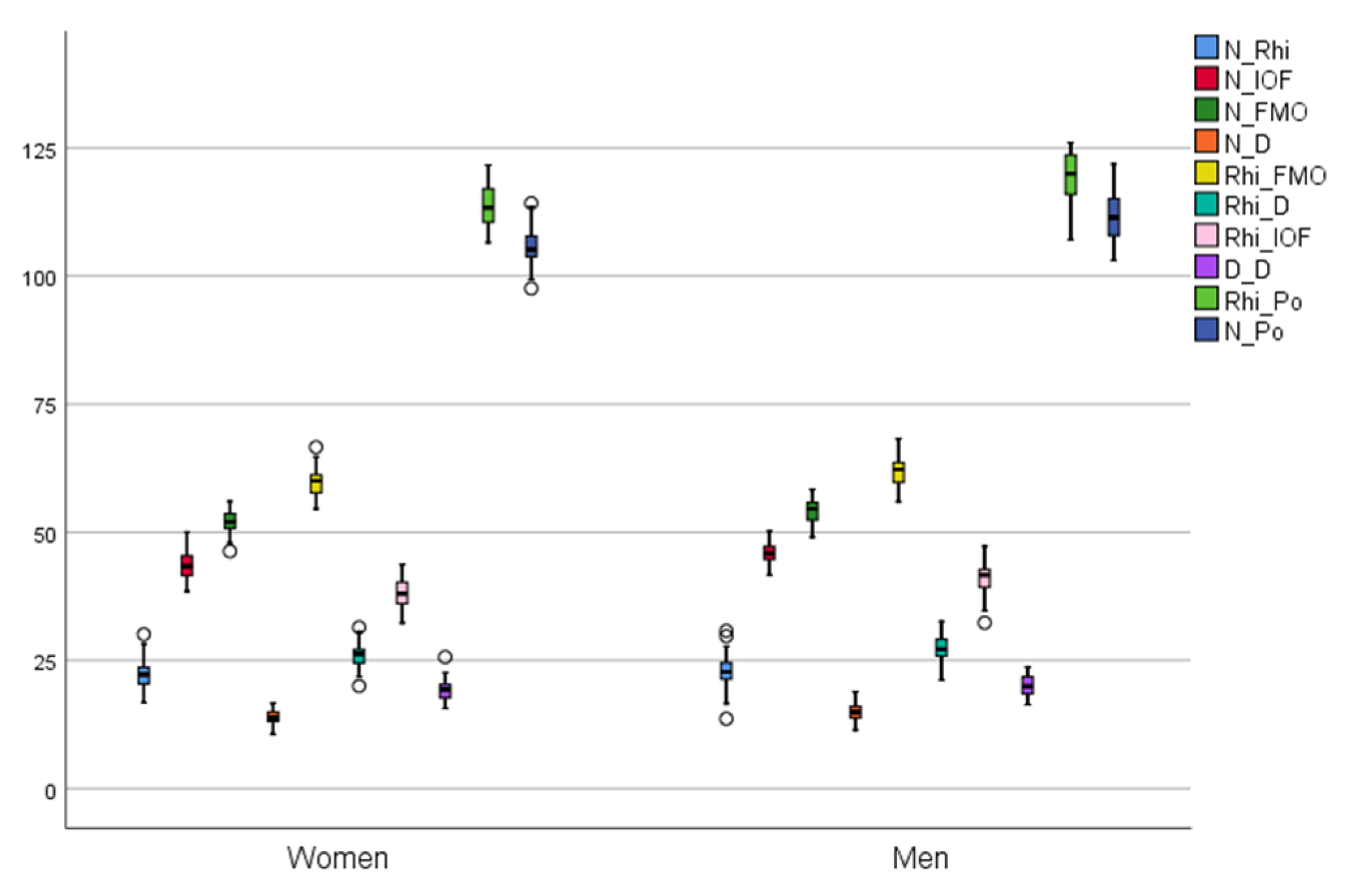
| Distance | Female (n = 55) Mean ± SD (Min–Max) | Male (n = 45) Mean ± SD (Min–Max) | Total (n = 100) Mean ± SD (Min–Max) | p-Value | 95% Confidence Interval of the Difference | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| N–FMO | 52.07 ± 1.98 (46.28–56.00) | 54.24 ± 2.19 (49.05–58.33) | 53.05 ± 2.34 (46.28–58.33) | 0.000 | 1.33 | 3.00 |
| N–Rhi | 22.18 ± 2.75 (16.75–30.09) | 22.88 ± 3.33 (13.61–30.76) | 22.50 ± 3.03 (13.61–30.76) | 0.254 | 0.50 | 1.90 |
| N–IOF | 43.43 ± 2.55 (38.48–50.05) | 46.10 ± 2.57 (41.65–56.01) | 44.63 ± 2.87 (38.48–56.01) | 0.000 | 1.64 | 3.69 |
| N–D | 13.92 ± 1.42 (10.60–16.64) | 15.01 ± 1.76 (11.43–18.87) | 14.41 ± 1.66 (10.60–18.87) | 0.001 | 0.45 | 1.72 |
| Rhi–FMO | 59.72 ± 2.52 (54.54–66.61) | 61.76 ± 2.90 (55.98–68.21 | 60.64 ± 2.87 (54.54–68.21) | 0.000 | 0.96 | 3.11 |
| Rhi–D | 25.99 ± 2.24 (19.99–31.45) | 27.21 ± 2.77 (21.19–32.57) | 26.54 ± 2.55 (19.99–32.57) | 0.016 | 0.22 | 2.22 |
| Rhi–IOF | 38.08 ± 2.68 (32.29–43.68) | 40.93 ± 3.13 (32.34–47.24) | 39.36 ± 3.21 (32.29–47.24) | 0.000 | 1.70 | 4.01 |
| D–D | 19.16 ± 1.93 (15.63–25.64) | 19.98 ± 1.94 (16.37–23.72) | 19.53 ± 1.97 (15.63–25.54) | 0.038 | 0.04 | 1.59 |
| Rhi–Po | 113.89 ± 3.87 (106.53–121.62) | 119.59 ± 4.67 (107.10–125.96) | 116.46 ± 5.10 (106.53–125–96) | 0.000 | 4.00 | 7.39 |
| N–Po | 105.80 ± 3.31 (97.56–114.21) | 111.47 ± 4.37 (103.08–121.82) | 108.35 ± 4.75 (97.56–121.82) | 0.000 | 4.14 | 7.20 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roșu, A.-M.; Șulea, D.; Bandol, G.; Cobzeanu, B.M.; Moisii, L.; Severin, F.; Cobzeanu, L.-M.; Negru, D.; Roșu, O.C.; Palade, D.O.; et al. Improving the Treatment Outcome of Naso-Orbito-Ethmoido-Maxillary Fractures Using Virtual Three-Dimensional Anthropometric Data. Int. J. Environ. Res. Public Health 2022, 19, 10412. https://doi.org/10.3390/ijerph191610412
Roșu A-M, Șulea D, Bandol G, Cobzeanu BM, Moisii L, Severin F, Cobzeanu L-M, Negru D, Roșu OC, Palade DO, et al. Improving the Treatment Outcome of Naso-Orbito-Ethmoido-Maxillary Fractures Using Virtual Three-Dimensional Anthropometric Data. International Journal of Environmental Research and Public Health. 2022; 19(16):10412. https://doi.org/10.3390/ijerph191610412
Chicago/Turabian StyleRoșu, Andrei-Mihail, Daniela Șulea, Geanina Bandol, Bogdan Mihail Cobzeanu, Liliana Moisii, Florentina Severin, Luiza-Maria Cobzeanu, Dragoș Negru, Oana Cristina Roșu, Dragoș Octavian Palade, and et al. 2022. "Improving the Treatment Outcome of Naso-Orbito-Ethmoido-Maxillary Fractures Using Virtual Three-Dimensional Anthropometric Data" International Journal of Environmental Research and Public Health 19, no. 16: 10412. https://doi.org/10.3390/ijerph191610412
APA StyleRoșu, A.-M., Șulea, D., Bandol, G., Cobzeanu, B. M., Moisii, L., Severin, F., Cobzeanu, L.-M., Negru, D., Roșu, O. C., Palade, D. O., Costan, V. V., & Cobzeanu, M. D. (2022). Improving the Treatment Outcome of Naso-Orbito-Ethmoido-Maxillary Fractures Using Virtual Three-Dimensional Anthropometric Data. International Journal of Environmental Research and Public Health, 19(16), 10412. https://doi.org/10.3390/ijerph191610412







