Evaluation of Root Anatomy and Canal Configuration of Human Permanent Maxillary First Molar Using Cone-Beam Computed Tomography: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Focused Question
2.2. Inclusion Criteria
2.3. Exclusion Criteria
- Studies using any classifications other than Vertucci.
- Case reports, case series and reviews were excluded.
2.4. Search Strategy and Data Collection
2.5. Quality Assessment
3. Results
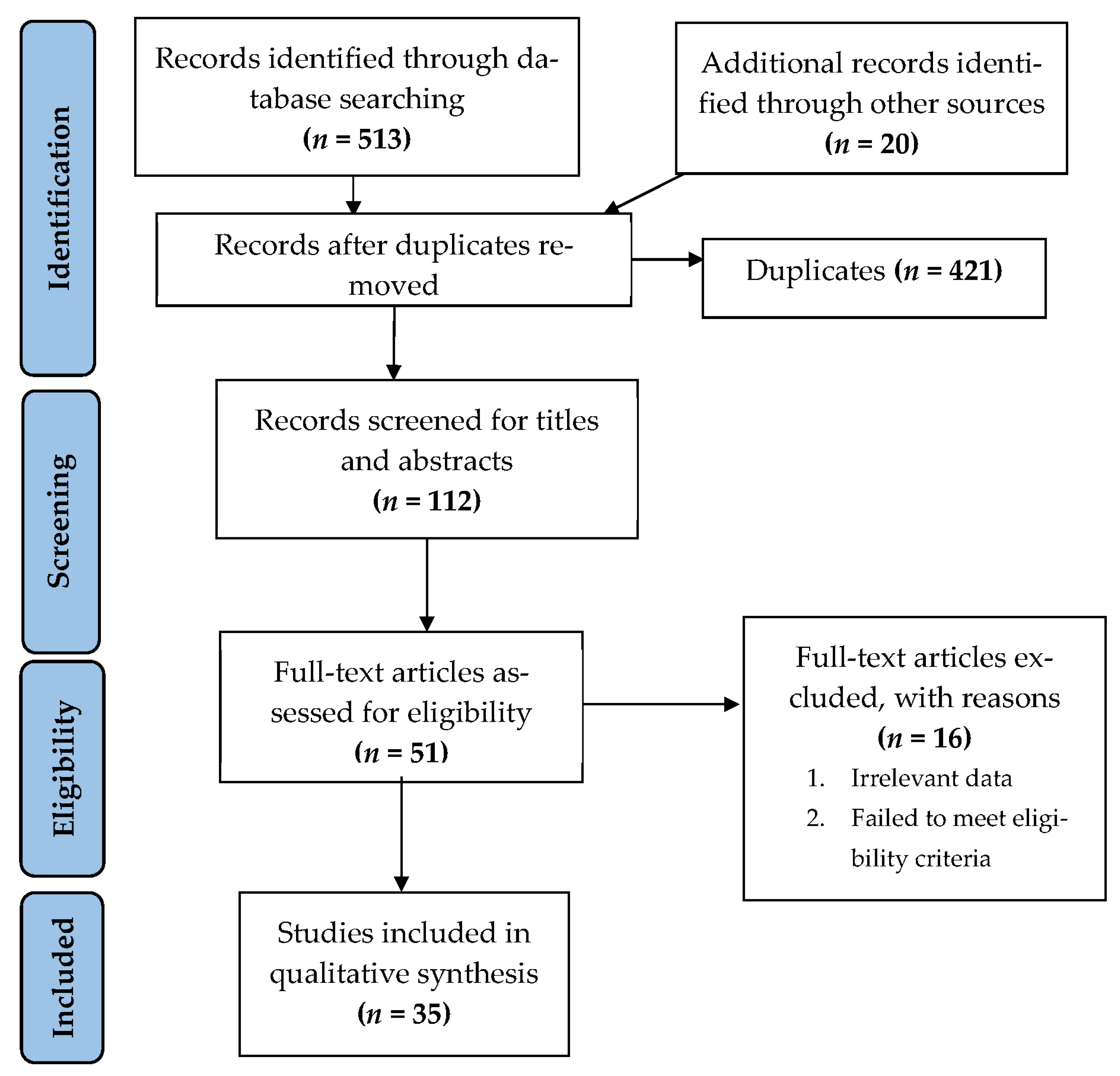
3.1. Search Selection and Results
3.2. Study Characteristics
3.3. Outcome
3.4. Prevalence of Canal Configuration of Mesiobuccal Root Based on Vertucci Classification
3.5. Prevalence of Canal Configuration of the Second Mesiobuccal Root Based on Vertucci Classification
3.6. Prevalence of Canal Configuration of the Distobuccal Root Based on Vertucci Classification
3.7. Frequency of Occurrence of Second Mesiobuccal Canal
3.8. Quality Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Selwitz, R.H.; Ismail, A.I.; Pitts, N.B. Dental Caries. Lancet 2007, 369, 51–59. [Google Scholar] [CrossRef]
- Schilder, H. Cleaning and Shaping the Root Canal. Dent. Clin. N. Am. 1974, 18, 269–296. [Google Scholar] [CrossRef]
- Iandolo, A.; Michele, S.; Stefano, O.; Sandro, R. 3D Cleaning, a Perfected Technique: Thermal Profile Assessment of Heated Naocl. G. Ital. Endod. 2017, 31, 58–61. [Google Scholar] [CrossRef]
- Iandolo, A.; Abdellatif, D.; Pantaleo, G.; Sammartino, P.; Amato, A. Conservative Shaping Combined with Three-Dimensional Cleaning Can Be a Powerful Tool: Case Series. J. Conserv. Dent. 2020, 23, 648–652. [Google Scholar] [CrossRef]
- Antunes, H.S.; Rôças, I.N.; Alves, F.R.F.; Siqueira, J.F. Total and Specific Bacterial Levels in the Apical Root Canal System of Teeth with Post-Treatment Apical Periodontitis. J. Endod. 2015, 41, 1037–1042. [Google Scholar] [CrossRef]
- Ricucci, D.; Siqueira, J.F. Fate of the Tissue in Lateral Canals and Apical Ramifications in Response to Pathologic Conditions and Treatment Procedures. J. Endod. 2010, 36, 1–15. [Google Scholar] [CrossRef]
- Siqueira, J.F. Aetiology of Root Canal Treatment Failure: Why Well-Treated Teeth Can Fail. Int. Endod. J. 2001, 34, 1–10. [Google Scholar] [CrossRef]
- Lin, L.M.; Rosenberg, P.A.; Lin, J. Do Procedural Errors Cause Endodontic Treatment Failure? J. Am. Dent. Assoc. 2005, 136, 187–193. [Google Scholar] [CrossRef]
- Ahmed, H.A.; Abu-bakr, N.H.; Yahia, N.A.; Ibrahim, Y.E. Root and Canal Morphology of Permanent Mandibular Molars in a Sudanese Population. Int. Endod. J. 2007, 40, 766–771. [Google Scholar] [CrossRef]
- Malagnino, V.; Gallottini, L.; Passariello, P. Some Unusual Clinical Cases on Root Anatomy of Permanent Maxillary Molars. J. Endod. 1997, 23, 127–128. [Google Scholar] [CrossRef]
- Weine, F.S.; Healey, H.J.; Gerstein, H.; Evanson, L. Canal Configuration in the Mesiobuccal Root of the Maxillary First Molar and Its Endodontic Significance. 1969. J. Endod. 2012, 38, 1305–1308. [Google Scholar] [CrossRef] [PubMed]
- Vertucci, F.J. Root Canal Anatomy of the Human Permanent Teeth. Oral. Surg Oral Med. Oral Pathol. 1984, 58, 589–599. [Google Scholar] [CrossRef]
- Sert, S.; Bayirli, G.S. Evaluation of the Root Canal Configurations of the Mandibular and Maxillary Permanent Teeth by Gender in the Turkish Population. J. Endod. 2004, 30, 391–398. [Google Scholar] [CrossRef]
- Ahmed, H.M.A.; Dummer, P.M.H. Advantages and Applications of a New System for Classifying Roots and Canal Systems in Research and Clinical Practice. Eur. Endod. J. 2018, 3, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Reit, C.; Petersson, K.; Molven, O. Diagnosis of Pulpal and Periapical Disease. In Textbook of Endodontology; Blackwell Munksgaard: Copenhagen, Denmark, 2003; pp. 9–18. [Google Scholar]
- Zheng, Q.; Wang, Y.; Zhou, X.; Wang, Q.; Zheng, G.; Huang, D. A Cone-Beam Computed Tomography Study of Maxillary First Permanent Molar Root and Canal Morphology in a Chinese Population. J. Endod. 2010, 36, 1480–1484. [Google Scholar] [CrossRef]
- Tu, M.-G.; Tsai, C.-C.; Jou, M.-J.; Chen, W.-L.; Chang, Y.-F.; Chen, S.-Y.; Cheng, H.-W. Prevalence of Three-Rooted Mandibular First Molars among Taiwanese Individuals. J. Endod. 2007, 33, 1163–1166. [Google Scholar] [CrossRef]
- Pinsky, H.M.; Dyda, S.; Pinsky, R.W.; Misch, K.A.; Sarment, D.P. Accuracy of Three-Dimensional Measurements Using Cone-Beam CT. Dentomaxillofac. Radiol. 2006, 35, 410–416. [Google Scholar] [CrossRef]
- Lo Giudice, G.; Iannello, G.; Terranova, A.; Lo Giudice, R.; Pantaleo, G.; Cicciù, M. Transcrestal Sinus Lift Procedure Approaching Atrophic Maxillary Ridge: A 60-Month Clinical and Radiological Follow-Up Evaluation. Int. J. Dent. 2015, 2015, 261652. [Google Scholar] [CrossRef]
- Blattner, T.C.; George, N.; Lee, C.C.; Kumar, V.; Yelton, C.D.J. Efficacy of Cone-Beam Computed Tomography as a Modality to Accurately Identify the Presence of Second Mesiobuccal Canals in Maxillary First and Second Molars: A Pilot Study. J. Endod. 2010, 36, 867–870. [Google Scholar] [CrossRef]
- Matherne, R.P.; Angelopoulos, C.; Kulild, J.C.; Tira, D. Use of Cone-Beam Computed Tomography to Identify Root Canal Systems In Vitro. J. Endod. 2008, 34, 87–89. [Google Scholar] [CrossRef]
- Martins, J.N.R.; Marques, D.; Silva, E.J.N.L.; Caramês, J.; Versiani, M.A. Prevalence Studies on Root Canal Anatomy Using Cone-Beam Computed Tomographic Imaging: A Systematic Review. J. Endod. 2019, 45, 372–386.e4. [Google Scholar] [CrossRef]
- Martins, J.N.R.; Versiani, M.A. CBCT and Micro-CT on the Study of Root Canal Anatomy. In The Root Canal Anatomy in Permanent Dentition; Versiani, M.A., Basrani, B., Sousa-Neto, M.D., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 89–180. [Google Scholar]
- Yousuf, W.; Khan, M.; Mehdi, H. Endodontic Procedural Errors: Frequency, Type of Error, and the Most Frequently Treated Tooth. Int. J. Dent. 2015, 2015, 673914. [Google Scholar] [CrossRef]
- Verma, P.; Love, R.M. A Micro CT Study of the Mesiobuccal Root Canal Morphology of the Maxillary First Molar Tooth. Int. Endod. J. 2011, 44, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 Statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Balk, E.M.; Chung, M.; Hadar, N.; Patel, K.; Yu, W.W.; Trikalinos, T.A.; Chang, L.K.W. Accuracy of Data Extraction of Non-English Language Trials with Google Translate; Report No.: 12-EHC056-EF; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2012.
- Martins, J.N.R.; Kishen, A.; Marques, D.; Nogueira Leal Silva, E.J.; Caramês, J.; Mata, A.; Versiani, M.A. Preferred Reporting Items for Epidemiologic Cross-Sectional Studies on Root and Root Canal Anatomy Using Cone-Beam Computed Tomographic Technology: A Systematized Assessment. J. Endod. 2020, 46, 915–935. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Yang, H.; Yu, X.; Wang, H.; Hu, T.; Dummer, P.M.H. Use of CBCT to Identify the Morphology of Maxillary Permanent Molar Teeth in a Chinese Subpopulation. Int. Endod. J. 2011, 44, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Lee, S.-J.; Woo, J. Morphology of Maxillary First and Second Molars Analyzed by Cone-Beam Computed Tomography in a Korean Population: Variations in the Number of Roots and Canals and the Incidence of Fusion. J. Endod. 2012, 38, 1063–1068. [Google Scholar] [CrossRef] [PubMed]
- Tocci, L.; Plotino, G.; Grande, N.M.; Testarelli, L.; Messineo, D.; Ciotti, M.; Gambarini, G. Analysis of root and root canal morphology of maxillary and mandibular molars in a Caucasian population: CBCT study in vivo. G. Ital. Endod. 2013, 27, 13–20. [Google Scholar] [CrossRef][Green Version]
- Guo, J.; Vahidnia, A.; Sedghizadeh, P.; Enciso, R. Evaluation of Root and Canal Morphology of Maxillary Permanent First Molars in a North American Population by Cone-Beam Computed Tomography. J. Endod. 2014, 40, 635–639. [Google Scholar] [CrossRef]
- Altunsoy, M.; Ok, E.; Nur, B.G.; Aglarci, O.S.; Gungor, E.; Colak, M. Root Canal Morphology Analysis of Maxillary Permanent First and Second Molars in a Southeastern Turkish Population Using Cone-Beam Computed Tomography. J. Dent. Sci. 2015, 10, 401–407. [Google Scholar] [CrossRef][Green Version]
- Abarca, J.; Gómez, B.; Zaror, C.; Monardes, H.; Bustos, L.; Cantin, M. Determinación de la Morfología de la Raíz Mesial y la Frecuencia del Canal MB2 en Molares Maxilares Usando Tomografía Computadorizada de Haz Cónico. Int. J. Morphol. 2015, 33, 1333–1337. [Google Scholar] [CrossRef]
- Kalender, A.; Celikten, B.; Tufenkci, P.; Aksoy, U.; Basmacı, F.; Kelahmet, U.; Orhan, K. Cone Beam Computed Tomography Evaluation of Maxillary Molar Root Canal Morphology in a Turkish Cypriot Population. Biotechnol. Biotechnol. Equip. 2016, 30, 145–150. [Google Scholar] [CrossRef]
- Naseri, M.; Safi, Y.; Akbarzadeh Baghban, A.; Khayat, A.; Eftekhar, L. Survey of Anatomy and Root Canal Morphology of Maxillary First Molars Regarding Age and Gender in an Iranian Population Using Cone-Beam Computed Tomography. Iran. Endod. J. 2016, 11, 298–303. [Google Scholar] [CrossRef]
- Tian, X.-M.; Yang, X.-W.; Qian, L.; Wei, B.; Gong, Y. Analysis of the Root and Canal Morphologies in Maxillary First and Second Molars in a Chinese Population Using Cone-Beam Computed Tomography. J. Endod. 2016, 42, 696–701. [Google Scholar] [CrossRef]
- Martins, J.N.R.; Marques, D.; Mata, A.; Caramês, J. Root and Root Canal Morphology of the Permanent Dentition in a Caucasian Population: A Cone-Beam Computed Tomography Study. Int. Endod. J. 2017, 50, 1013–1026. [Google Scholar] [CrossRef]
- Al-Kadhim, A.H.; Rajion, Z.A.; Malik, N.A.B.; Bin Jaafar, A. Morphology of Maxillary First Molars Analyzed by Cone-Beam Computed Tomography among Malaysian: Variations in the Number of Roots and Canals and the Incidence of Fusion. Int. Med. J. Malays. 2017, 16, 2. [Google Scholar] [CrossRef]
- Pérez-Heredia, M.; Ferrer-Luque, C.M.; Bravo, M.; Castelo-Baz, P.; Ruíz-Piñón, M.; Baca, P. Cone-Beam Computed Tomographic Study of Root Anatomy and Canal Configuration of Molars in a Spanish Population. J. Endod. 2017, 43, 1511–1516. [Google Scholar] [CrossRef]
- Zand, V.; Mokhtari, H.; Zonouzi, H.R.; Shojaei, S.N. Root Canal Morphologies of Mesiobuccal Roots of Maxillary Molars Using Cone Beam Computed Tomography and Periapical Radiographic Techniques in an Iranian Population. J. Contemp. Dent. Pract. 2017, 18, 745–749. [Google Scholar] [CrossRef]
- Ghobashy, A.M.; Nagy, M.M.; Bayoumi, A.A. Evaluation of Root and Canal Morphology of Maxillary Permanent Molars in an Egyptian Population by Cone-Beam Computed Tomography. J. Endod. 2017, 43, 1089–1092. [Google Scholar] [CrossRef]
- Al-Shehri, S.; Al-Nazhan, S.; Shoukry, S.; Al-Shwaimi, E.; Al-Sadhan, R.; Al-Shemmery, B. Root and Canal Configuration of the Maxillary First Molar in a Saudi Subpopulation: A Cone-Beam Computed Tomography Study. Saudi Endod. J. 2017, 7, 69. [Google Scholar] [CrossRef]
- Wang, H.; Ci, B.-W.; Yu, H.-Y.; Qin, W.; Yan, Y.-X.; Wu, B.-L.; Ma, D.-D. Evaluation of Root and Canal Morphology of Maxillary Molars in a Southern Chinese Subpopulation: A Cone-Beam Computed Tomographic Study. Int. J. Clin. Exp. 2017, 10, 7030–7039. Available online: https://e-century.us/files/ijcem/10/4/ijcem0045172.pdf (accessed on 14 July 2022).
- Khademi, A.; Zamani Naser, A.; Bahreinian, Z.; Mehdizadeh, M.; Najarian, M.; Khazaei, S. Root Morphology and Canal Configuration of First and Second Maxillary Molars in a Selected Iranian Population: A Cone-Beam Computed Tomography Evaluation. Iran. Endod. J. 2017, 12, 288–292. [Google Scholar] [CrossRef] [PubMed]
- Ghoncheh, Z.; Zade, B.M.; Kharazifard, M.J. Root Morphology of the Maxillary First and Second Molars in an Iranian Population Using Cone Beam Computed Tomography. J. Dent. 2017, 14, 115–122. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5694843/pdf/JOD-14-115.pdf (accessed on 17 July 2022).
- Martins, J.N.R.; Ordinola-Zapata, R.; Marques, D.; Francisco, H.; Caramês, J. Differences in Root Canal System Configuration in Human Permanent Teeth within Different Age Groups. Int. Endod. J. 2018, 51, 931–941. [Google Scholar] [CrossRef] [PubMed]
- Martins, J.N.R.; Gu, Y.; Marques, D.; Francisco, H.; Caramês, J. Differences on the Root and Root Canal Morphologies between Asian and White Ethnic Groups Analyzed by Cone-Beam Computed Tomography. J. Endod. 2018, 44, 1096–1104. [Google Scholar] [CrossRef] [PubMed]
- Razumova, S.; Brago, A.; Khaskhanova, L.; Barakat, H.; Howijieh, A. Evaluation of Anatomy and Root Canal Morphology of the Maxillary First Molar Using the Cone-Beam Computed Tomography among Residents of the Moscow Region. Contemp. Clin. Dent. 2018, 9, S133–S136. [Google Scholar] [CrossRef]
- Ratanajirasut, R.; Panichuttra, A.; Panmekiate, S. A Cone-Beam Computed Tomographic Study of Root and Canal Morphology of Maxillary First and Second Permanent Molars in a Thai Population. J. Endod. 2018, 44, 56–61. [Google Scholar] [CrossRef]
- Martins, J.N.R.; Marques, D.; Francisco, H.; Caramês, J. Gender Influence on the Number of Roots and Root Canal System Configuration in Human Permanent Teeth of a Portuguese Subpopulation. Quintessence Int. 2018, 49, 103–111. [Google Scholar] [CrossRef]
- Gomes Alves, C.R.; Martins Marques, M.; Stella Moreira, M.; Harumi Miyagi de Cara, S.P.; Silveira Bueno, C.E.; Lascala, C.Â. Second Mesiobuccal Root Canal of Maxillary First Molars in a Brazilian Population in High-Resolution Cone-Beam Computed Tomography. Iran. Endod. J. 2018, 13, 71–77. [Google Scholar] [CrossRef]
- Raja, M.; Pradeep, S.; Mohan, M. Root canal morphology of maxillary first molar using cone-beam computed tomography in south Indian population. J. Pharm. Res. 2018, 12, 4. [Google Scholar]
- Pan, J.Y.Y.; Parolia, A.; Chuah, S.R.; Bhatia, S.; Mutalik, S.; Pau, A. Root Canal Morphology of Permanent Teeth in a Malaysian Subpopulation Using Cone-Beam Computed Tomography. BMC Oral Health 2019, 19, 14. [Google Scholar] [CrossRef] [PubMed]
- Mohara, N.T.; Coelho, M.S.; de Queiroz, N.V.; Borreau, M.L.S.; Nishioka, M.M.; de Jesus Soares, A.; Frozoni, M. Root Anatomy and Canal Configuration of Maxillary Molars in a Brazilian Subpopulation: A 125-Μm Cone-Beam Computed Tomographic Study. Eur. J. Dent. 2019, 13, 82–87. [Google Scholar] [CrossRef] [PubMed]
- de Miranda Candeiro, G.T.; Gonçalves, S.D.S.; de Araújo Lopes, L.L.; de Freitas Lima, I.T.; Alencar, P.N.B.; Iglecias, E.F.; Silva, P.G.B. Internal Configuration of Maxillary Molars in a Subpopulation of Brazil’s Northeast Region: A CBCT Analysis. Braz. Oral Res. 2019, 33, e082. [Google Scholar] [CrossRef]
- Soh, N. Evaluation of Root Canal Morphology of Maxillary 1st Molars Using Cone Beam Computed Tomography in Chennai Population. J. Pharm. Sci. Res. 2019, 11, 2750–2754. Available online: https://jpsr.pharmainfo.in/Documents/Volumes/vol11issue07/jpsr11071948.pdf (accessed on 14 July 2022).
- Al Mheiri, E.; Chaudhry, J.; Abdo, S.; El Abed, R.; Khamis, A.H.; Jamal, M. Evaluation of Root and Canal Morphology of Maxillary Permanent First Molars in an Emirati Population; a Cone-Beam Computed Tomography Study. BMC Oral Health 2020, 20, 274. [Google Scholar] [CrossRef] [PubMed]
- Alsaket, Y.; El-ma’aita, A.; Aqrabawi, J.; Alhadidi, A. Prevalence and Configuration of the Second Mesiobuccal Canal in the Permanent Maxillary First Molar in Jordanian Population Sample. Iran. Endod. J. 2020, 15, 217–220. [Google Scholar] [CrossRef]
- Liu, Y.; Yang, W.; Wang, W.; Zhu, Y.; Lin, Z.; Zhu, M. Relationship between Canal Morphology and Isthmus in Mesio-Buccal Roots of Maxillary First Molars in 9- to 12-Year-Old Children: An In-Vivo Cone-Beam Computed Tomography Analysis. Arch. Oral Biol. 2020, 112, 104645. [Google Scholar] [CrossRef]
- Popović, M.; Živanović, S.; Vučićević, T.; Grujović, M.; Papić, M. Cone-Beam Computed Tomography Study of Tooth Root and Canal Morphology of Permanent Molars in a Serbian Population. Vojnosanit. Pregl. 2020, 77, 470–478. [Google Scholar] [CrossRef]
- Al-Saedi, A.; Al-Bakhakh, B.; Al-Taee, R.G. Using Cone-Beam Computed Tomography to Determine the Prevalence of the Second Mesiobuccal Canal in Maxillary First Molar Teeth in a Sample of an Iraqi Population. Clin. Cosmet. Investig. Dent. 2020, 12, 505–514. [Google Scholar] [CrossRef]
- Nikkerdar, N.; Asnaashari, M.; Karimi, A.; Araghi, S.; Seifitabar, S.; Golshah, A. Root and Canal Morphology of Maxillary Teeth in an Iranian Subpopulation Residing in Western Iran Using Cone-Beam Computed Tomography. Iran. Endod. J. 2020, 15, 31–37. [Google Scholar] [CrossRef]
- Peiris, R. Root and Canal Morphology of Human Permanent Teeth in a Sri Lankan and Japanese Population. Anthropol. Sci. 2008, 116, 123–133. [Google Scholar] [CrossRef]
- Campos Netto, P.D.A.; Dos Santos Accioly Lins, C.C.; Lins, C.V.; Lima, G.A.; Gomes Frazão, M.A. Study of the Internal Morphology of the Mesiobuccal Root of Upper First Permanent Molar Using Cone Beam Computed Tomography. Int. J. Morphol. 2011, 29, 617–621. [Google Scholar] [CrossRef]
- Buyukbayram, I.; Kartal, N. Evaluation of Complex Mesiobuccal Root Anatomy in Maxillary First Molar Teeth. Int. J. Morphol. 2018, 36, 460–464. [Google Scholar] [CrossRef]
- Rouhani, A.; Bagherpour, A.; Akbari, M.; Azizi, M.; Nejat, A.; Naghavi, N. Cone-Beam Computed Tomography Evaluation of Maxillary First and Second Molars in Iranian Population: A Morphological Study. Iran. Endod. J. 2014, 9, 190–194. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4099950/pdf/iej-9-190.pdf (accessed on 17 July 2022).
- Weng, X.-L.; Yu, S.-B.; Zhao, S.-L.; Wang, H.-G.; Mu, T.; Tang, R.-Y.; Zhou, X.-D. Root Canal Morphology of Permanent Maxillary Teeth in the Han Nationality in Chinese Guanzhong Area: A New Modified Root Canal Staining Technique. J. Endod. 2009, 35, 651–656. [Google Scholar] [CrossRef]
- Faraj, B.M. The Frequency of the Second Mesiobuccal Canal in Maxillary First Molars among a Sample of the Kurdistan Region-Iraq Population—A Retrospective Cone-Beam Computed Tomography Evaluation. J. Dent. Sci. 2021, 16, 91–95. [Google Scholar] [CrossRef]
- Martins, J.N.R.; Alkhawas, M.-B.A.M.; Altaki, Z.; Bellardini, G.; Berti, L.; Boveda, C.; Chaniotis, A.; Flynn, D.; Gonzalez, J.A.; Kottoor, J.; et al. Worldwide Analyses of Maxillary First Molar Second Mesiobuccal Prevalence: A Multicenter Cone-Beam Computed Tomographic Study. J. Endod. 2018, 44, 1641–1649.e1. [Google Scholar] [CrossRef]
- Betancourt, P.; Navarro, P.; Muñoz, G.; Fuentes, R. Prevalence and Location of the Secondary Mesiobuccal Canal in 1100 Maxillary Molars Using Cone Beam Computed Tomography. BMC. Med. Imaging 2016, 16, 66. [Google Scholar] [CrossRef]
- Sousa, T.O.; Haiter-Neto, F.; Nascimento, E.H.L.; Peroni, L.V.; Freitas, D.Q.; Hassan, B. Diagnostic Accuracy of Periapical Radiography and Cone-Beam Computed Tomography in Identifying Root Canal Configuration of Human Premolars. J. Endod. 2017, 43, 1176–1179. [Google Scholar] [CrossRef]
- Abuabara, A.; Baratto-Filho, F.; Aguiar Anele, J.; Leonardi, D.P.; Sousa-Neto, M.D. Efficacy of Clinical and Radiological Methods to Identify Second Mesiobuccal Canals in Maxillary First Molars. Acta Odontol. Scand. 2013, 71, 205–209. [Google Scholar] [CrossRef]
- Gaêta-Araujo, H.; Fontenele, R.C.; Nascimento, E.H.L.; do Carmo Chagas Nascimento, M.; Freitas, D.Q.; de Oliveira-Santos, C. Association between the Root Canal Configuration, Endodontic Treatment Technical Errors, and Periapical Hypodensities in Molar Teeth: A Cone-Beam Computed Tomographic Study. J. Endod. 2019, 45, 1465–1471. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, E.H.L.; Gaêta-Araujo, H.; Andrade, M.F.S.; Freitas, D.Q. Prevalence of Technical Errors and Periapical Lesions in a Sample of Endodontically Treated Teeth: A CBCT Analysis. Clin. Oral Investig. 2018, 22, 2495–2503. [Google Scholar] [CrossRef] [PubMed]
- Song, M.; Kim, H.-C.; Lee, W.; Kim, E. Analysis of the Cause of Failure in Nonsurgical Endodontic Treatment by Microscopic Inspection during Endodontic Microsurgery. J. Endod. 2011, 37, 1516–1519. [Google Scholar] [CrossRef] [PubMed]
| Study/Year of Publication | Country | CBCT Model | Voxel Size | FOV | Settings CBCT | Software Visualization |
|---|---|---|---|---|---|---|
| Zang R et al./2011 [27] | China | 3D Accuitomo scanner (Morita, Kyoto, Japan) | 0.125 mm | 40 mm or 60 mm | 80 kV and 5.0 mA, time 17 s | i-Dixel one volume viewer 1.5.0 and a Dell Precision T5400 workstation (Dell, Round Rock, TX, USA) |
| Kim Y et al./2012 [28] | Korea | Dinnova system (Willmed, Gwangmyeong, Korea) | 0.167-mm3 | 10 cm | 80 kVp, 9.0 mA | OnDemand3D software (Cybermed, Seoul, Korea). |
| Tocci L et al./2013 [29] | Italy | NewTom VGi Vertical Cone Beam (Verona, Italia) | 0.3 mm | 15 cm | 110 Kvp, 1–20 mAs, 15 mSv | NA |
| Guo J et al./2014 [30] | USA | Sirona Galileos device (Sirona Dental Systems, Inc, Long Island City, NY, USA) | 0.3/0.15 mm. | 15 cm | 85 kV and 5–7 mA | The Digital Imaging and Communications in Medicine (DICOM) format images were exported from Galileos and imported into InVivo Dental Application 5.1.6 software (Anatomage Inc., San Jose, CA, USA). |
| Altunsoy M et al./2014 [31] | Turkey | CBCT scanner (ICAT Vision; Imaging Science International, Hatfield, PA, USA) | 0.3 mm | NA | 120 kVp, and 18.54 mA, 8 s | NA |
| Abarca J. et al./2015 [32] | Chile | Gendex CB500 imaging system | 0.2 mm | NA | 120 kVp and 5 mA and 0.2 mm thickness of the cut | iCATVision software v 1.8.1.10 in a darkroom on 21” LCD monitors with a resolution of 1280 × 1024 pixels. |
| Kalender A et al./2015 [33] | Turkey | Newtom 3G: Quantitative Radiology s.r.l., Verona, Italy | NA | 9 inch | NA | NNT 4.6, QR Verona, Italy |
| Naseri M et al./2016 [34] | Iran | NewTom VGi (QR SRL Company, Verona, Italy) | 200 µm | 8 × 12 cm | 110 kVp and exposure time of 3.6 s | NewTom NNT software version 5.3 (Quantitative Radiology, Verona, Italy) |
| Tian X et al./2016 [35] | Chinese | NewTom VG; QR srl, Verona, Italy | 0.16 mm | 500 cm2 (20 × 25 cm) | 110 kVp and 10 mA, 18 s | NNT software version 2.21 (ImageWorks, Elmsford, NY, USA) |
| Martins J.N.R et al./2016(I) [36] | Portugal | Planmeca scanner (Planmeca Promax, Planmeca, Finland) | 0.2 mm | NA | 80 kv, 15 mA, 12 s | Planmeca Romexis, Planmeca |
| Al-Kadhim A et al./2017 [37] | Malaysia | NA | NA | NA | NA | One Data Viewer software (J. Morita Manufacturing Corp). |
| Perez M et al./2017 [38] | Spain | 9300 3D CBCT unit (Carestream Dental, Atlanta, GA, USA) | 0.18 mm | 10 × 10 cm | 90 kV, 4 mA, 8 s | Carestream software (CS 3D Imaging software 6.1.4) |
| Zand V et al./2017 [39] | Iran | NewTom GI CBCT (Verona/Italy) | NA | NA | 110 kVp, 18 s | NNT viewer software program |
| Ghobasby A et al./2017 [40] | Egypt | Cranex 3D (Soredex ,Tuusula, Finland) | 133-μm | NA | 80 kVp, 9.0 mA | NA |
| Al-Shehri S et al./2017 [41] | Saudi Arabia | 1. I-CAT (Imaging Science International, Hatfield, PA, USA), 2. Galileos (Sirona Dental Systems, Bensheim, Germany), 3.Carestream CS 9300 (Carestream Health, Inc., Rochester, NY, USA). | 0.3 mm (14-bit grayscale) | NA | 85 kV, 5–7 mA | OnDemand3D software (Cybermed, Seoul, Korea) |
| Wang H et al./2017 [42] | China | Planmeca Romexis 3D CBCT scanner (Planmeca, Finland) | 200 μm | NA | 84 kV and 14 mA,12 s, the minimum slice thickness was 0.2 mm. | The CBCT images were 3D-reconstructed by using a patented Feldkamp reconstruction algorithm, analysed with inbuilt software and ran in a 32-bit Windows 7 system. |
| Khademi A et al./2017 [43] | Iran | Galileos (Sirona Dental Systems Inc., Bensheim, Germany) | 150 μm | 150 × 150 or 75 × 150 mm | 85 kVp, 42 mA | SIDEXIS XG software version 3.7 (Sirona Dental System GmbH, Bensheim, Germany). |
| Ghoncheh Z/2017 [44] | Iran | NewTom VG CBCT system (Image Works, Verona, Italy) | 0.3 mm | (11 × 16 cm | 110 kV, 1–20 mA, 3.6–5.4 s. | NNT Viewer software (NNT 2.21; Image Works, Verona, Italy). |
| Martins J.N.R et al./2018(II) [45] | Portugal | Planmeca Promax, Planmeca, Helsinki, Finland | 0.20 mm | NA | 80 kV, 15 mA, 12 s | Romexis visualization software (Planmeca) |
| Martins J.N.R et al./2018(III) [46] | China | Kodak 9500 | 0.2 mm | Full Arch | 90 kV, 10 mA, 10.8 s | CS 900 3D imaging |
| Portugal | Planmeca Promax | 0.2 mm | Full Arch | 80 kV,15 mA, 12 s | Planmeca Romexis | |
| Razmuvo S et al./2018 [47] | Moscow | 3D eXam (KaVo, Biberach, Germany) | 0.3 mm | 23 cm × 17 cm | 110 kV, 1.6–20 s | g I-CAT viewer software (version 10, Hatfield, England). |
| Ratanajirasut et al./2018 [48] | Thai | 3D Accuitomo CBCT machine (J Morita Manufacturing Corp, Kyoto, Japan | 0.25 mm × 0.25 mm | 100.025 × 100.025 | 80 kVp,5 mA, 17.5 s | g One Volume Viewer software (J Morita Manufacturing Corp) |
| Martins J.N.R et al./2018(IV) [49] | Portugal | Planmeca Promax | 0.2 mm | 80 kV,15 mA, 12 s | Planmeca Romexis | |
| Alves CRG et al./2018 [50] | Brazil | Prexion 3D Elite model XP68 (PreXion Inc., San Mateo, California, USA), | 0.15 mm (for FOV 8) and 0.11 mm (for FOV 5) | 5 [5.6 cm × 5.2 cm (partial jaw) ] or 8 [8.1 cm × 7.5 cm (total jaw)] | 90 Kvp and 4 mA, 37 s | 3D software PreXion Image Analysis System (PreXion Inc. San Mateo, California, USA) |
| Raja M et al./2018 [51] | India | NA | NA | NA | The CBCT scanner was set at a constant slice thickness of 125 μm/slice | NA |
| Pan YJ et al./2019 [52] | Malaysia | KaVo 3D eXam imaging system (Imaging Sciences International, Hatfield, PA, USA). | 0.25 mm | NA | 121 kVp, 5 mA, 26.9 s | eXam Vision software version 1.9.3.13 (KaVo Dental GmbH, Biberach, Germany) |
| Mohara NT et al./2019 [53] | Brazil | a 3D Accuitomo 80 CBCT (J. Morita, Kyoto, Japan) | NA | 40 mm or 60 mm | 90 KVA, 8 mA, 18 s | i-Dixel (J Morita, Tokyo, Japan) |
| Candeiro GTM et al./2019 [54] | Brazil | Prexion 3D imaging device (Prexion, Inc., San Mateo, USA) | 0.125 mm | NA | 90 kVp and 4 mA | (Prexion, Inc., San Mateo, USA) was used on a Dell Precision T5400 (Dell, Round Rock, TX, USA) |
| Soh N et al./2019 [55] | India | NA | ||||
| Al Mheiri E et al./2019 [56] | United Arab Emirates | Planmeca ProMax CBCT scanner (Planmeca Oy, Helsinki, Finland) | 0.4 mm | 16 × 11 cm | 120 kVp, 18.54 mA, 8.9 s | iMAC computer ([27-in. screen size with Retina 5 K display, 5120 × 2880 resolution with support for 1 billion colors, 500 nits brightness], Apple, USA) in a room with controlled lighting using the Horos DICOM viewer |
| Alsaket YM et al./2020 [57] | Jordan | Carestream Dental, Rochester, NY, USA | NA | NA | NA | NA |
| Liu Y et al./2020 [58] | China | NewTom VG scanner (QR srl, Verona, Italy) | 0.125 mm | Small | NA | 3D reconstructed with an open source software platform 3D Slicer 4.8.1 from Slicer web site |
| Popovic M et al./2020 [59] | Serbia | Orthophos XG 3D device (Sirona Dental Systems GmbH, Bensheim, Germany) | 160 μm | 0.16 mm | NA | GALAXIS v1.9.4 (Sirona Dental Systems GmbH, Bensheim, Germany) |
| Al-Saedi A et al./2020 [60] | Iraq | Gendex (GXDP-7000) CBCT machine (Hatfield, PA, USA) | 200 µm | 80.0 × 80.0 × 60.0 mm | 90 kV,10 mA, 13 s | Software GxPicture; Kavo Dental, Biberach a der Riss, Germany built into the Invivo 5 dental viewer (Anatomage, San Jose, CA, USA) and run on a 64-bit Windows 7 system (Microsoft Corporation, Redmond, WA, USA) |
| Nikkerdar N et al./2020 [61] | Iran | New Tom VGi CBCT system (QR SRL Co., Verona, Italy) | 0.15 mm | 120 × 80 mm | 110 kVp, 10 mA, 5.4 s | NNT Viewer version 7.2 software on a 12.5-inch laptop (Asus) with 1080 × 1920 p resolution |
| Study/Year of Publication | Sample Size (n) | Population | MB2 Canals n (%) |
|---|---|---|---|
| Zang R et al./2011 [27] | 299 | China | 155 (52%) |
| Kim Y et al./2012 [28] | 814 | Korea | 510 (62.65%) |
| Tocci L et al./2013 [29] | 161 | Italy | 62 (40.3%) |
| Guo J et al./2014 [30] | 628 | USA | 428 (68.2%) |
| Abarca J. et al./2015 [32] | 802 | Chile | 802 (73.44%) |
| Tian X et al./2016 [35] | 1536 | China | 820 (53.9%) |
| Martins J.N.R et al./2016 (I) [36] | 421 | Malaysia | 191 (45.6%) |
| Al-Kadhim A et al./2017 [37] | 494 | Portugal | 350 (71.05%) |
| Zand V et al./2017 [39] | 156 | Iran | 86 (55.11%) |
| Ghobasby A et al./2017 [40] | 605 | Egypt | 451 (74.5%) |
| Al-Shehri S et al./2017 [41] | 330 | Saudi Arabia | 195 (55.6%) |
| Wang H et al./2017 [42] | 939 | China | 641 (68.3%) |
| Khademi A et al./2017 [43] | 389 | Iran | 272 (70.2%) |
| Ghoncheh Z/2017 [44] | 337 | Iran | 155 (46%) |
| Martins J.N.R et al./2018 (III) [46] | 239 | China | 552 (67.35%) |
| Razmuvo S et al./2018 [47] | 410 | Moscow | 382 (59.8%) |
| Ratanajirasut et al./2018 [48] | 476 | Thai | 303 (63.6%) |
| Alves CRG et al./2018 [50] | 362 | Brazil | 247 (68.23%) |
| Raja M et al./2018 [51] | 500 | Indian | 400 (80%) |
| Pan YJ et al./2019 [52] | 344 | Malaysia | 125 (36.3%) |
| Mohara NT et al./2019 [53] | 326 | Brazil | 209 (64.22%) |
| Candeiro GTM et al./2019 [54] | 700 | Brazil | 337 (48.21%) |
| Soh N et al./2019 [55] | 66 | India | 20 (30%) |
| Al Mheiri E et al./2019 [56] | 522 | United Arab Emirates | 418 (80.1%) |
| Alsaket YM et al./2020 [57] | 200 | Jordan | 174 (87%) |
| Total | 12,056 | 8223 (68.2%) |
| Sr. No. | Section Item | Total (n) | Percentage (%) |
|---|---|---|---|
| 1 | Title | 33 | 94.29 |
| Introduction | |||
| 2 | Keywords | 32 | 91.43 |
| 3 | Aim | 35 | 100.00 |
| Methods | |||
| 4 | Participants (in vivo assessment) | 33 | 94.29 |
| 5 | CBCT | 33 | 94.29 |
| 6 | Morphology concept & assessed teeth (variables) | 35 | 100.00 |
| 7 | Assessment | 35 | 100.00 |
| 8 | Observers | 27 | 77.14 |
| 9 | Potential sources of bias | 21 | 60.00 |
| 10 | Final sample size | 35 | 100.00 |
| 11 | Reliability | 25 | 71.43 |
| 12 | Statistical analysis | 33 | 94.29 |
| 13 | Ethics committee Results | 24 | 68.57 |
| 14 | Primary Outcomes | 34 | 97.14 |
| 15 | Other analysis | 28 | 80.00 |
| 16 | Visual documentation Support | 31 | 88.57 |
| Discussion | |||
| 17 | Outcome interpretation | 35 | 100.00 |
| 18 | Strength & limitations | 23 | 65.71 |
| 19 | Generalizability | 35 | 100.00 |
| 20 | Future research | 5 | 14.29 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbhai, S.; Shetty, R.; Joshi, P.; Mehta, V.; Mathur, A.; Sharma, T.; Chakraborty, D.; Porwal, P.; Meto, A.; Wahjuningrum, D.A.; et al. Evaluation of Root Anatomy and Canal Configuration of Human Permanent Maxillary First Molar Using Cone-Beam Computed Tomography: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 10160. https://doi.org/10.3390/ijerph191610160
Barbhai S, Shetty R, Joshi P, Mehta V, Mathur A, Sharma T, Chakraborty D, Porwal P, Meto A, Wahjuningrum DA, et al. Evaluation of Root Anatomy and Canal Configuration of Human Permanent Maxillary First Molar Using Cone-Beam Computed Tomography: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(16):10160. https://doi.org/10.3390/ijerph191610160
Chicago/Turabian StyleBarbhai, Sourabh, Rajesh Shetty, Poonam Joshi, Vini Mehta, Ankita Mathur, Tanvi Sharma, Damini Chakraborty, Priyanka Porwal, Aida Meto, Dian Agustin Wahjuningrum, and et al. 2022. "Evaluation of Root Anatomy and Canal Configuration of Human Permanent Maxillary First Molar Using Cone-Beam Computed Tomography: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 16: 10160. https://doi.org/10.3390/ijerph191610160
APA StyleBarbhai, S., Shetty, R., Joshi, P., Mehta, V., Mathur, A., Sharma, T., Chakraborty, D., Porwal, P., Meto, A., Wahjuningrum, D. A., Luke, A. M., & Pawar, A. M. (2022). Evaluation of Root Anatomy and Canal Configuration of Human Permanent Maxillary First Molar Using Cone-Beam Computed Tomography: A Systematic Review. International Journal of Environmental Research and Public Health, 19(16), 10160. https://doi.org/10.3390/ijerph191610160









