Psychological Distress in South African Healthcare Workers Early in the COVID-19 Pandemic: An Analysis of Associations and Mitigating Factors
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Participants, and Setting
2.2. Data Collection
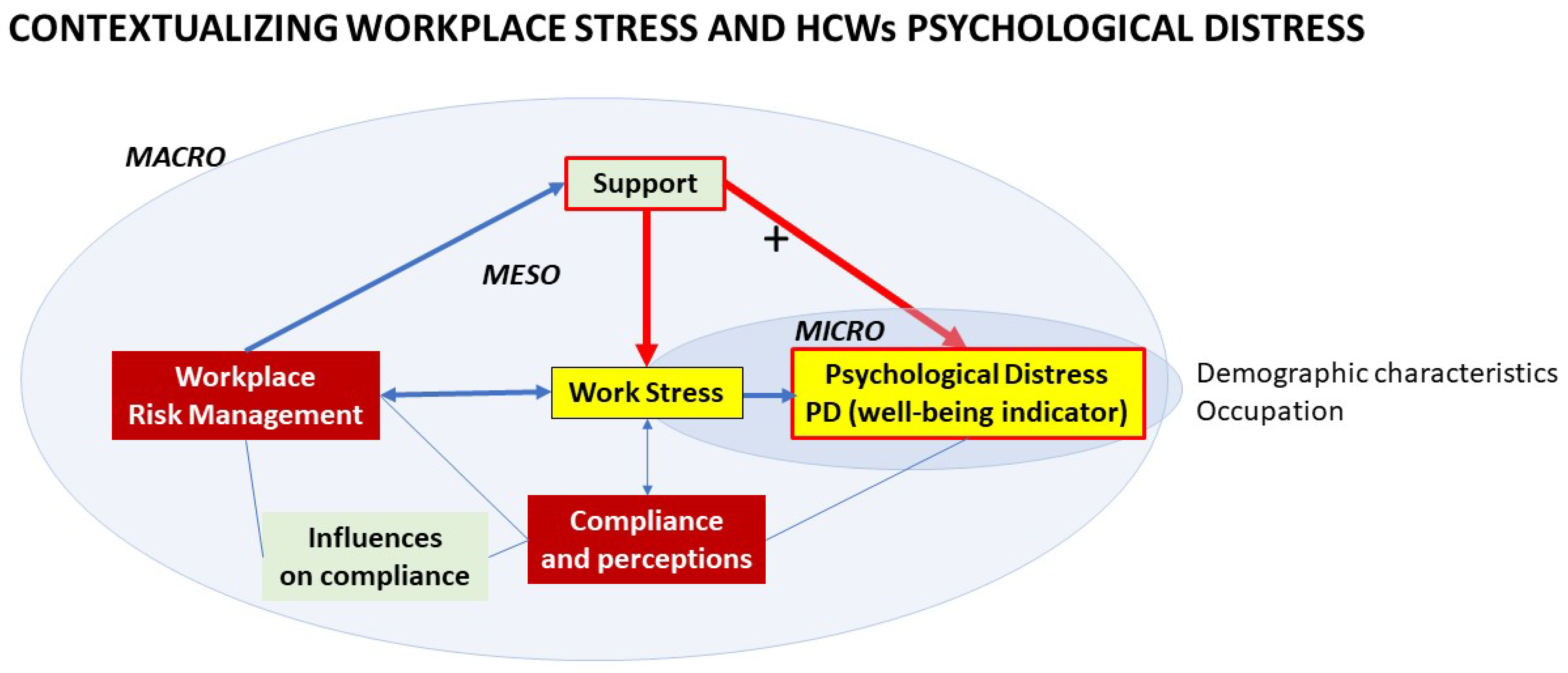
2.3. Variables and Conceptual Model
2.4. Instruments
2.4.1. General Health Questionnaire
2.4.2. Job-Related Tension Index
2.4.3. Perception of Risks Associated with COVID-19
2.4.4. Training-Related Questionnaire
2.4.5. Support
2.4.6. Questionnaire on Knowledge, Attitude, Practices, and Behaviour
2.5. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Psychological Distress
3.3. Work-Related Stress and Psychological Distress
3.4. Perception of Risks Associated with COVID-19 and Psychological Distress
3.5. Knowledge, Attitude, Practice and Behaviours during the COVID-19 Pandemic and Psychological Distress
3.6. Training, Supporting and Appreciation Sources and Psychological Distress
3.7. Correlation Analysis
3.8. The Risk or Protective Factors of Psychological Distress
3.9. Mediation and Moderation Analyses
4. Discussion
4.1. Strengths
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Announces COVID-19 Outbreak a Pandemic. Available online: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (accessed on 19 January 2022).
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 18 April 2022).
- Minister Zweli Mkhize Confirms 31 more Coronavirus COVID-19 Cases in South Africa. Available online: https://www.gov.za/speeches/dr-zweli-mkhize-confirms-116-more-coronavirus-covid-19-cases-south-africa-18-mar-2020-0000 (accessed on 19 January 2022).
- Statement by President Cyril Ramaphosa on Measures to Combat COVID-19 Epidemic. Available online: https://www.thepresidency.gov.za/press-statements/statement-president-cyril-ramaphosa-measures-combat-covid-19-epidemic (accessed on 19 January 2022).
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated with Mental Health Outcomes among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Rana, W.; Mukhtar, S.; Mukhtar, S. Mental health of medical workers in Pakistan during the pandemic COVID-19 outbreak. Asian J. Psychiatr. 2020, 51, 102080. [Google Scholar] [CrossRef] [PubMed]
- Xiaoming, X.; Ming, A.; Su, H.; Wo, W.; Jianmei, C.; Qi, Z.; Hua, H.; Xuemei, L.; Lixia, W.; Jun, C.; et al. The psychological status of 8817 hospital workers during COVID-19 Epidemic: A cross-sectional study in Chongqing. J. Affect. Disord. 2020, 276, 555–561. [Google Scholar] [CrossRef]
- Styra, R.; Hawryluck, L.; Mc Geer, A.; Dimas, M.; Sheen, J.; Giacobbe, P.; Dattani, N.; Lorello, G.; Rac, V.E.; Francis, T.; et al. Surviving SARS and living through COVID-19: Healthcare worker mental health outcomes and insights for coping. PLoS ONE 2021, 16, e0258893. [Google Scholar] [CrossRef]
- Robertson, L.J.; Maposa, I.; Somaroo, H.; Johnson, O. Mental health of healthcare workers during the COVID-19 outbreak: A rapid scoping review to inform provincial guidelines in South Africa. S. Afr. Med. J. 2020, 110, 1010–1019. [Google Scholar] [CrossRef]
- Goldblatt, D.; Johnson, M.; Falup-Pecurariu, O.; Ivaskeviciene, I.; Spoulou, V.; Tamm, E.; Wagner, M.; Zar, H.J.; Bleotu, L.; Ivaskevicius, R.; et al. Cross-sectional prevalence of SARS-CoV-2 antibodies in healthcare workers in paediatric facilities in eight countries. J. Hosp. Infect. 2021, 110, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Rees, K.; Dunlop, J.L.; Patel-Abrahams, S.; Struthers, H.; McIntyre, J.A. Primary healthcare workers at risk during COVID-19: An analysis of infections in HIV service providers in five districts of South Africa. S. Afr. Med. J. 2021, 111, 309–314. [Google Scholar] [CrossRef]
- WHO. Promoting Mental Health: Concepts, Emerging Evidence, Practice: Summary Report/a Report from the World Health Organization, Department of Mental Health and Substance Abuse in Collaboration with the Victorian Health Promotion Foundation and the University of Melbourne; World Health Organization: Geneva, Switzerland, 2004; p. 10. [Google Scholar]
- Väänänen, A.; Anttila, E.; Turtiainen, J.; Varje, P. Formulation of work stress in 1960–2000: Analysis of scientific works from the perspective of historical sociology. Soc. Sci. Med. 2012, 75, 784–794. [Google Scholar] [CrossRef]
- Ganster, D.C.; Rosen, C.C. Work Stress and Employee Health: A Multidisciplinary Review. J. Manag. 2013, 39, 1085–1122. [Google Scholar] [CrossRef]
- Sirois, F.M.; Owens, J. Factors Associated With Psychological Distress in Health-Care Workers during an Infectious Disease Outbreak: A Rapid Systematic Review of the Evidence. Front. Psychiatry 2020, 11, 589545. [Google Scholar] [CrossRef]
- Drapeau, A.; Marchand, A.; Beaulieu-Prévost, D. Epidemiology of Psychological Distress. In Mental Illnesses-Understanding, Prediction and Control; L’Abate, L., Ed.; IntechOpen: London, UK, 2012. [Google Scholar]
- Al-Hanawi, M.K.; Angawi, K.; Alshareef, N.; Qattan, A.M.N.; Helmy, H.Z.; Abudawood, Y.; Alqurashi, M.; Kattan, W.M.; Kadasah, N.A.; Chirwa, G.C.; et al. Knowledge, Attitude and Practice toward COVID-19 among the Public in the Kingdom of Saudi Arabia: A Cross-Sectional Study. Front. Public Health 2020, 8, 217. [Google Scholar] [CrossRef] [PubMed]
- Asemahagn, M.A. Factors determining the knowledge and prevention practice of healthcare workers towards COVID-19 in Amhara region, Ethiopia: A cross-sectional survey. Trop. Med. Health 2020, 48, 72. [Google Scholar] [CrossRef] [PubMed]
- Huynh, G.; Nguyen, T.N.H.; Tran, V.K.; Vo, K.N.; Vo, V.T.; Pham, L.A. Knowledge and attitude toward COVID-19 among healthcare workers at District 2 Hospital, Ho Chi Minh City. Asian Pac. J. Trop. Med. 2020, 13, 260–265. [Google Scholar] [CrossRef]
- Olum, R.; Chekwech, G.; Wekha, G.; Nassozi, D.R.; Bongomin, F. Coronavirus Disease-2019: Knowledge, Attitude, and Practices of Health Care Workers at Makerere University Teaching Hospitals, Uganda. Front. Public Health 2020, 8, 181. [Google Scholar] [CrossRef] [PubMed]
- Saqlain, M.; Munir, M.M.; Rehman, S.U.; Gulzar, A.; Naz, S.; Ahmed, Z.; Tahir, A.H.; Mashhood, M. Knowledge, attitude, practice and perceived barriers among healthcare workers regarding COVID-19: A cross-sectional survey from Pakistan. J. Hosp. Infect. 2020, 105, 419–423. [Google Scholar] [CrossRef]
- Zhang, M.; Zhou, M.; Tang, F.; Wang, Y.; Nie, H.; Zhang, L.; You, G. Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in Henan, China. J. Hosp. Infect. 2020, 105, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Manyaapelo, T.; Mokhele, T.; Sifunda, S.; Ndlovu, P.; Dukhi, N.; Sewpaul, R.; Naidoo, I.; Jooste, S.; Tlou, B.; Moshabela, M.; et al. Determinants of Confidence in Overall Knowledge About COVID-19 Among Healthcare Workers in South Africa: Results From an Online Survey. Front. Public Health 2021, 9, 614858. [Google Scholar] [CrossRef]
- Koh, D.; Lim, M.K.; Chia, S.E.; Ko, S.M.; Qian, F.; Ng, V.L.; Tan, B.H.; Wong, K.S.; Chew, W.M.; Tang, H.K.; et al. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare Workers in Singapore What can we Learn? Med. Care 2005, 43, 676–682. [Google Scholar] [CrossRef]
- Maunder, R.G.; Lancee, W.J.; Rourke, S.; Hunter, J.J.; Goldbloom, D.; Balderson, K.; Petryshen, P.; Steinberg, R.; Wasylenki, D.; Koh, D.; et al. Factors Associated With the Psychological Impact of Severe Acute Respiratory Syndrome on Nurses and Other Hospital Workers in Toronto. Psychosom. Med. 2004, 66, 938–942. [Google Scholar] [CrossRef]
- Hsu, C.-H.; Lin, H.-H.; Wang, C.-C.; Jhang, S. How to defend COVID-19 in Taiwan? Talk about people’s disease awareness, attitudes, behaviors and the impact of physical and mental health. Int. J. Environ. Res. Public Health 2020, 17, 4694. [Google Scholar] [CrossRef]
- Chatterjee, S.S.; Bhattacharyya, R.; Bhattacharyya, S.; Gupta, S.; Das, S.; Banerjee, B.B. Attitude, practice, behavior, and mental health impact of COVID-19 on doctors. Indian J. Psychiatry 2020, 62, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Heath, C.; Sommerfield, A.; von Ungern-Sternberg, B.S. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: A narrative review. Anaesthesia 2020, 75, 1364–1371. [Google Scholar] [CrossRef] [PubMed]
- Brisson, C.; Aubé, K.; Gilbert-Ouimet, M.; Duchaine, C.S.; Trudel, X.; Vézina, M. Organizational-level interventions and occupational health. In Handbook of Socioeconomic Determinants of Occupational Health: From Macro-Level to Micro-Level Evidence; Theorell, T., Ed.; Springer Nature: Cham, Switzerland, AG, 2020; pp. 505–536. [Google Scholar]
- Patridge, E.F.; Bardyn, T.P. Research Electronic Data Capture (REDCap). J. Med. Libr. Assoc. 2018, 106, 142–144. [Google Scholar] [CrossRef]
- Niskanen, T.; Louhelainen, K.; Hirvonen, M.L. A systems thinking approach of occupational safety and health applied in the micro-, meso- and macro-levels: A Finnish survey. Saf. Sci. 2016, 82, 212–227. [Google Scholar] [CrossRef]
- Jackson, C. The General Health Questionnaire. Occup. Med. 2007, 57, 79. [Google Scholar] [CrossRef]
- Quek, K.F.; Low, W.Y.; Razack, A.H.; Loh, C.S. Reliability and validity of the General Health Questionnaire (GHQ-12) among urological patients: A Malaysian study. Psychiatry Clin. Neurosci. 2001, 55, 509–513. [Google Scholar] [CrossRef]
- Makowska, Z.; Merecz, D. The usefulness of the Health Status Questionnaire: D. Goldberg’s GHQ-12 and GHQ-28 for diagnosis of mental disorders in workers. Med. Pr. 2000, 51, 589–601. [Google Scholar]
- Hankins, M. The reliability of the twelve-item general health questionnaire (GHQ-12) under realistic assumptions. BMC Public Health 2008, 8, 355. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Gater, R.; Sartorius, N.; Ustun, T.B.; Piccinelli, M.; Gureje, O.; Rutter, C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 1997, 27, 191–197. [Google Scholar] [CrossRef]
- Graetz, B. Multidimensional properties of the General Health Questionnaire. Soc. Psychiatry Psychiatr. Epidemiol. 1991, 26, 132–138. [Google Scholar] [CrossRef]
- Makowska, Z.; Merecz, D.; Mościcka, A.; Kolasa, W. The validity of general health questionnaires, GHQ-12 and GHQ-28, in mental health studies of working people. Int. J. Environ. Res. Public Health 2002, 15, 353–362. [Google Scholar]
- Gómez-Salgado, J.; Andrés-Villas, M.; Domínguez-Salas, S.; Díaz-Milanés, D.; Ruiz-Frutos, C. Related Health Factors of Psychological Distress During the COVID-19 Pandemic in Spain. Int. J. Environ. Res. Public Health 2020, 17, 3947. [Google Scholar] [CrossRef] [PubMed]
- Kahn, R.L.; Wolfe, D.M.; Quinn, R.P.; Snoek, J.D.; Rosenthal, R.A. Organizational Stress: Studies in Role Conflict and Ambiguity; John Wiley: Hoboken, NJ, USA, 1964. [Google Scholar]
- Rogers, R.E.; Li, E.Y.; Ellis, R. Perceptions of Organizational Stress among Female Executives in the U.S. Government: An Exploratory Study. Public Pers. Manag. 1994, 23, 593–609. [Google Scholar] [CrossRef]
- MacKinnon, N.J. Role strain: An assessment of a measure and its invariance of factor structure across studies. J. Appl. Psychol. 1978, 63, 321–328. [Google Scholar] [CrossRef]
- Rogers, R.E. Components of organizational stress among Canadian managers. J. Psychol. 1977, 95, 265. [Google Scholar] [CrossRef]
- Abush, R.; Burkhead, E.J. Job stress in midlife working women: Relationships among personality type, job characteristics, and job tension. J. Couns. Psychol. 1984, 31, 36–44. [Google Scholar] [CrossRef]
- Jamal, M. Job stress and job performance controversy: An empirical assessment. Organ. Behav. Hum. Decis. Process. 1984, 33, 1–21. [Google Scholar] [CrossRef]
- Wright, E.M.; Matthai, M.T.; Budhathoki, C. Midwifery Professional Stress and Its Sources: A Mixed-Methods Study. J. Midwifery Womens Health 2018, 63, 660–667. [Google Scholar] [CrossRef]
- Sallon, S.; Katz-Eisner, D.; Yaffe, H.; Bdolah-Abram, T. Caring for the Caregivers: Results of an Extended, Five-component Stress-reduction Intervention for Hospital Staff. Behav. Med. 2017, 43, 47–60. [Google Scholar] [CrossRef]
- Wooten, N.R.; Fakunmoju, S.B.; Kim, H.; LeFevre, A.L. Factor Structure of the Job-Related Tension Index Among Social Workers. Res. Soc. Work Pract. 2010, 20, 74–86. [Google Scholar] [CrossRef]
- Wu, P.; Fang, Y.; Guan, Z.; Fan, B.; Kong, J.; Yao, Z.; Liu, X.; Fuller, C.J.; Susser, E.; Lu, J.; et al. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychol. 2009, 54, 302–311. [Google Scholar] [CrossRef] [PubMed]
- House, J.S. Occupational Stress and the Mental and Physical Health of Factory Workers; Michigan, T.U.f., Ed.; The Institiute for Social Research, The University of Michigan: Ann Arbor, MI, USA, 1980; p. 319. [Google Scholar]
- Hedges, L.V. Distribution Theory for Glass’s Estimator of Effect size and Related Estimators. J. Educ. Stat. 1981, 6, 107–128. [Google Scholar] [CrossRef]
- Glen, S. Hedges’ g: Definition, Formula from StatisticsHowTo.com: Elementary Statistics for the Rest of Us! Available online: https://www.statisticshowto.com/hedges-g/ (accessed on 2 December 2021).
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 3rd ed.; Guilford Publications: New York, NY, USA, 2022; pp. 79–157, 233–281. [Google Scholar]
- International Standards Organization. Occupational Health and Safety Management—General Guidelines for Safe Working during the COVID-19 Pandemic. Available online: https://www.iso.org/obp/ui/#iso:std:iso:pas:45005:ed-1:v1:en (accessed on 28 July 2022).
- Saleem, F.; Malik, M.I.; Qureshi, S.S. Work Stress Hampering Employee Performance During COVID-19: Is Safety Culture Needed? Front. Psychol. 2021, 12, 655839. [Google Scholar] [CrossRef] [PubMed]
- d’Ettorre, G.; Ceccarelli, G.; Santinelli, L.; Vassalini, P.; Innocenti, G.P.; Alessandri, F.; Koukopoulos, A.E.; Russo, A.; d’Ettorre, G.; Tarsitani, L. Post-Traumatic Stress Symptoms in Healthcare Workers Dealing with the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 601. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Sun, L.; Du, Z.; Zhao, L.; Wang, L. A cross-sectional study of mental health status and self-psychological adjustment in nurses who supported Wuhan for fighting against the COVID-19. J. Clin. Nurs. 2020, 29, 4161–4170. [Google Scholar] [CrossRef]
- Barello, S.; Caruso, R.; Palamenghi, L.; Nania, T.; Dellafiore, F.; Bonetti, L.; Silenzi, A.; Marotta, C.; Graffigna, G. Factors associated with emotional exhaustion in healthcare professionals involved in the COVID-19 pandemic: An application of the job demands-resources model. Int. Arch. Occup. Environ. Health 2021, 94, 1751–1761. [Google Scholar] [CrossRef]
- Daniels, R.A.; Miller, L.A.; Mian, M.Z.; Black, S. One size does NOT fit all: Understanding differences in perceived organizational support during the COVID-19 pandemic. Bus. Soc. Rev. 2022, 127, 193–222. [Google Scholar] [CrossRef]
- Ran, L.; Wang, W.; Ai, M.; Kong, Y.; Chen, J.; Kuang, L. Psychological resilience, depression, anxiety, and somatization symptoms in response to COVID-19: A study of the general population in China at the peak of its epidemic. Soc. Sci. Med. 2020, 262, 113261. [Google Scholar] [CrossRef]
- Pieh, C.; Budimir, S.; Delgadillo, J.; Barkham, M.; Fontaine, J.R.J.; Probst, T. Mental Health during COVID-19 Lockdown in the United Kingdom. Psychosom. Med. 2021, 83, 328–337. [Google Scholar] [CrossRef]
- Gualano, M.R.; Lo Moro, G.; Voglino, G.; Bert, F.; Siliquini, R. Monitoring the impact of COVID-19 pandemic on mental health: A public health challenge? Reflection on Italian data. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 165–167. [Google Scholar] [CrossRef]
- Aljuaid, M.; Ilyas, N.; Altuwaijri, E.; Albedawi, H.; Alanazi, O.; Shahid, D.; Alonazi, W. Quality of Life among Caregivers of Patients Diagnosed with Major Chronic Disease during COVID-19 in Saudi Arabia. Healthcare 2022, 10, 523. [Google Scholar] [CrossRef] [PubMed]
- Shacham, M.; Hamama-Raz, Y.; Kolerman, R.; Mijiritsky, O.; Ben-Ezra, M.; Mijiritsky, E. COVID-19 Factors and Psychological Factors Associated with Elevated Psychological Distress among Dentists and Dental Hygienists in Israel. Int. J. Environ. Res. Public Health 2020, 17, 2900. [Google Scholar] [CrossRef] [PubMed]
- De Kock, J.H.; Latham, H.A.; Leslie, S.J.; Grindle, M.; Munoz, S.-A.; Ellis, L.; Polson, R.; O’Malley, C.M. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: Implications for supporting psychological well-being. BMC Public Health 2021, 21, 104. [Google Scholar] [CrossRef]
- Chen, J.; Farah, N.; Dong, R.K.; Chen, R.Z.; Xu, W.; Yin, A.; Chen, B.Z.; Delios, A.; Miller, S.; Wan, X.; et al. The Mental Health Under the COVID-19 Crisis in Africa: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 10604. [Google Scholar] [CrossRef]
- Batra, K.; Singh, T.P.; Sharma, M.; Batra, R.; Schvaneveldt, N. Investigating the Psychological Impact of COVID-19 among Healthcare Workers: A Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 9096. [Google Scholar] [CrossRef]
- Zhang, S.X.; Chen, R.Z.; Xu, W.; Yin, A.; Dong, R.K.; Chen, B.Z.; Delios, A.Y.; Miller, S.; McIntyre, R.S.; Ye, W.; et al. A Systematic Review and Meta-Analysis of Symptoms of Anxiety, Depression, and Insomnia in Spain in the COVID-19 Crisis. Int. J. Environ. Res. Public Health 2022, 19, 1018. [Google Scholar] [CrossRef]
- Sodi, T.; Modipane, M.; Oppong Asante, K.; Quarshie, E.N.-B.; Asatsa, S.; Mutambara, J.; Khombo, S. Mental health policy and system preparedness to respond to COVID-19 and other health emergencies: A case study of four African countries. S. Afr. J. Psychol. 2021, 51, 279–292. [Google Scholar] [CrossRef]
- Gao, F.; Luo, N.; Thumboo, J.; Fones, C.; Li, S.-C.; Cheung, Y.-B. Does the 12-item General Health Questionnaire contain multiple factors and do we need them? Health Qual. Life Outcomes 2004, 2, 63. [Google Scholar] [CrossRef][Green Version]
- Moonasar, D.; Pillay, A.; Leonard, E.; Naidoo, R.; Mngemane, S.; Ramkrishna, W.; Jamaloodien, K.; Lebese, L.; Chetty, K.; Bamford, L.; et al. COVID-19: Lessons and experiences from South Africa’s first surge. BMJ Glob. Health 2021, 6, e004393. [Google Scholar] [CrossRef]
- Mo, Y.; Deng, L.; Zhang, L.; Lang, Q.; Liao, C.; Wang, N.; Qin, M.; Huang, H. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. 2020, 28, 1002–1009. [Google Scholar] [CrossRef]
- Sun, N.; Wei, L.; Shi, S.; Jiao, D.; Song, R.; Ma, L.; Wang, H.; Wang, C.; Wang, Z.; You, Y.; et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am. J. Infect. Control. 2020, 48, 592–598. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Wei, J.; Zhu, H.; Duan, Y.; Geng, W.; Hong, X.; Jiang, J.; Zhao, X.; Zhu, B. A Study of Basic Needs and Psychological Wellbeing of Medical Workers in the Fever Clinic of a Tertiary General Hospital in Beijing during the COVID-19 Outbreak. Psychother. Psychosom. 2020, 89, 252–254. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liu, Y.; Hu, K.; Zhang, M.; Du, M.; Huang, H.; Yue, X. Healthcare workers’ stress when caring for COVID-19 patients: An altruistic perspective. Nurs. Ethics. 2020, 27, 1490–1500. [Google Scholar] [CrossRef] [PubMed]
- Maluleke, R. Quarterly Labour Force Survey (QLFS) Q4:2020. Available online: http://www.statssa.gov.za/publications/P0211/Presentation%20QLFS%20Q4_2020.pdf (accessed on 17 April 2022).
- Portugal, L.C.L.; Gama, C.M.F.; Gonçalves, R.M.; Mendlowicz, M.V.; Erthal, F.S.; Mocaiber, I.; Tsirlis, K.; Volchan, E.; David, I.A.; Pereira, M.G.; et al. Vulnerability and Protective Factors for PTSD and Depression Symptoms among Healthcare Workers during COVID-19: A Machine Learning Approach. Front. Psychiatry 2022, 12, 752870. [Google Scholar] [CrossRef]
- Liu, X.; Kakade, M.; Fuller, C.J.; Fan, B.; Fang, Y.; Kong, J.; Guan, Z.; Wu, P. Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Compr. Psychiatry 2012, 53, 15–23. [Google Scholar] [CrossRef]
- Cai, W.; Lian, B.; Song, X.; Hou, T.; Deng, G.; Li, H. A cross-sectional study on mental health among health care workers during the outbreak of Corona Virus Disease 2019. Asian J. Psychiatr. 2020, 51, 102111. [Google Scholar] [CrossRef]
- Moyo, I.; Mgolozeli, S.E.; Risenga, P.R.; Mboweni, S.H.; Tshivhase, L.; Mudau, T.S.; Ndou, N.D.; Mavhandu-Mudzusi, A.H. Experiences of Nurse Managers during the COVID-19 Outbreak in a Selected District Hospital in Limpopo Province, South Africa. Healthcare 2022, 10, 76. [Google Scholar] [CrossRef]
- Shanafelt, T.; Ripp, J.; Trockel, M. Understanding and Addressing Sources of Anxiety among Health Care Professionals During the COVID-19 Pandemic. JAMA 2020, 323, 2133–2134. [Google Scholar] [CrossRef]
- Maffoni, M.; Sommovigo, V.; Giardini, A.; Paolucci, S.; Setti, I. Dealing with ethical issues in rehabilitation medicine: The relationship between managerial support and emotional exhaustion is mediated by moral distress and enhanced by positive affectivity and resilience. J. Nurs. Manag. 2020, 28, 1114–1125. [Google Scholar] [CrossRef]
- Iosim, I.; Runcan, P.; Dan, V.; Nadolu, B.; Runcan, R.; Petrescu, M. The Role of Supervision in Preventing Burnout among Professionals Working with People in Difficulty. Int. J. Environ. Res. Public Health 2022, 19, 160. [Google Scholar] [CrossRef]
- Zungu, M.; Voyi, K.; Mlangeni, N.; Moodley, S.V.; Ramodike, J.; Claassen, N.; Wilcox, E.; Thunzi, N.; Yassi, A.; Spiegel, J.; et al. Organizational factors associated with health worker protection during the COVID-19 pandemic in four provinces of South Africa. BMC Health Serv. Res. 2021, 21, 1080. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total (N = 154) Valid/Total (%) | Final (N = 122) Valid/Total (%) |
|---|---|---|
| Gender | 134/154 (87.0%) | 106/122 (86.9%) |
| Female | 116 (86.6%) | 90 (84.9%) |
| Male | 18 (13.4%) | 16 (15.1%) |
| Age (years) | 150/154 (97.4%) | 119/122 (97.5%) |
| Median (IQR) | 44.00 (34.00, 54.00) | 34.00 (34.00, 44.00) |
| Job Title | 151/154 (98.1%) | 120/122 (98.4%) |
| Professional/Assistant/Staff nurses | 100 (66.2%) | 81 (67.5%) |
| Other professionals | 51 (33.8%) | 39 (32.5%) |
| Work Type | 120/154 (77.9%) | 95/122 (77.9%) |
| Inpatient | 112 (93.3%) | 89 (93.7%) |
| Outpatient only | 8 (6.7%) | 6 (6.3%) |
| Work Years | 126/154 (81.8%) | 99/122 (81.1%) |
| Median (IQ1, Q3) | 8.00 (2.00, 12.00) | 8.00 (2.00, 12.00) |
| Home Language | 142/154 (92.2%) | 113/122 (92.6%) |
| 1. English | 3 (2.1%) | 3 (2.7%) |
| 2. Ndebele | 8 (5.6%) | 8 (7.1%) |
| 3. Northern Sotho | 33 (23.2%) | 28 (24.8%) |
| 4. Southern Sotho | 6 (4.2%) | 2 (1.8%) |
| 5. Swati | 3 (2.1%) | 3 (2.7%) |
| 6. Tsonga | 15 (10.6%) | 13 (11.5%) |
| 7. Tswana | 47 (33.1%) | 34 (30.1%) |
| 8. Venda | 12 (8.5%) | 9 (8%) |
| 9. Xhosa | 4 (2.8%) | 4 (3.5%) |
| 10. Zulu | 11 (7.7%) | 9 (8%) |
| Prior COVID-19 infection | 145/154 (94.2%) | 113/122 (92.6%) |
| Yes | 15 (10.3%) | 12 (10.6%) |
| No | 130 (89.7%) | 101 (89.4%) |
| Received flu shot this season | 148/154 (96.1%) | 116/122 (95.1%) |
| Yes | 49 (33.1%) | 40 (34.5%) |
| No | 99 (66.9%) | 76 (65.5%) |
| Any MH/stress management workshops prior to COVID-19 | 140/154 (90.9%) | 109/122 (89.3%) |
| Yes | 53 (37.9%) | 43 (39.4%) |
| If yes, Attended any above workshops | ||
| Yes | 36 (69.2%) | 29 (69%) |
| No | 16 (30.8%) | 13 (31%) |
| No | 87 (62.1%) | 66 (60.6%) |
| Item | N b | Mean (SD) a | % Worse c |
|---|---|---|---|
| ANXIETY/DEPRESSION * | 2.31 | ||
| 5. Have you felt constantly under strain? | 152 | 2.57 (1.10) | 50.0 |
| 9. Have you been feeling unhappy or depressed? | 145 | 2.46 (1.18) | 49.0 |
| 2. Have your worries made you lose a lot of sleep? | 146 | 2.13 (0.98) | 32.1 |
| 6. Have you had the feeling that you could not overcome your difficulties? | 150 | 2.06 (0.96) | 30.6 |
| SOCIAL DYSFUNCTION * | 2.16 | ||
| 7. Have you been able to enjoy your normal day-to-day activities? | 147 | 2.41 (1.00) | 42.2 |
| 12. Have you been feeling reasonably happy all things considered? | 142 | 2.25 (1.00) | 33.1 |
| 1. Have you been able to concentrate well on what you were doing? | 151 | 2.14 (0.87) | 28.5 |
| 8. Have you been able to face up to your problems? | 148 | 2.11 (0.89) | 29.0 |
| 4. Have you felt capable of making decisions about things? | 151 | 2.09 (0.98) | 27.2 |
| 3. Have you felt that you are playing a useful part in things? | 150 | 1.91 (0.93) | 23.3 |
| SELF-CONFIDENCE * | 1.89 | ||
| 11. Have you been thinking of yourself as a worthless person? | 147 | 1.90 (1.13) | 29.3 |
| 10. Have you been losing confidence in yourself? | 148 | 1.89 (1.10) | 27.0 |
| Individual Scores (4-point scale)a | N b | Mean (SE) | |
| Average scale (all 12 questions answered) | 122 | 2.11 (0.06) | |
| Average scale (at least 10 questions answered) | 147 | 2.16 (0.05) | |
| Average scale (at least 6 questions answered) | 152 | 2.17 (0.05) | |
| Individual Scores (2-point scale with a total score of 12) d | N b | Mean (SD) d | |
| Average scale (all 12 questions answered) | 122 | 3.72 (3.23) | |
| Presence of psychological distress (individual 2pt score cut point ≥ 3) | Yes/No | 57.4%/42.6% |
| Items | Psychological Distress a | Effect Size | ||
|---|---|---|---|---|
| Yes | No | p | g | |
| 4. Feeling that you have too heavy a workload, one that you cannot possibly finish during an ordinary working day | 3.34 (1.28) | 2.71 (1.39) | 0.010 * | 0.476 |
| 13. Thinking that amount of work that you have to do may interfere with how well it gets done | 3.09 (1.27) | 2.43 (1.10) | 0.004 * | 0.545 |
| 5. Thinking that you will not be able to satisfy the conflicting demands of the various people over you | 3.04 (1.17) | 2.27 (1.06) | <0.001 * | 0.678 |
| 1. You have too little authority to carry out the responsibilities assigned to you | 2.99 (1.26) | 2.37 (1.09) | 0.007 * | 0.514 |
| 9. Having to decide things that affect the lives of individuals, people that you know | 2.94 (1.17) | 2.39 (1.28) | 0.015 * | 0.450 |
| 15. Feeling that your job tends to interfere with your family life | 2.91 (1.47) | 2.20 (1.31) | 0.006 * | 0.507 |
| 3. Not knowing what opportunities for advancement or promotion exist for you | 2.86 (1.51) | 2.39 (1.38) | 0.091 | |
| 14. Feeling that you have to do things on the job that go against your better judgement | 2.80 (1.26) | 2.29 (1.13) | 0.022 * | 0.422 |
| 7. Not knowing what your immediate supervisor thinks of you and how he or she evaluates your performance | 2.68 (1.14) | 2.45 (1.27) | 0.311 | |
| 11. Feeling unable to influence your immediate supervisor’s decisions that affect you | 2.62 (1.23) | 2.26 (1.31) | 0.132 | |
| 10. Feeling that you may not be liked or accepted by the people that you work with | 2.58 (1.13) | 2.08 (1.12) | 0.016 * | 0.444 |
| 12. Not knowing what the people that you work with expect of you | 2.44 (1.11) | 2.35 (1.14) | 0.639 | |
| 8. Not being able to get the necessary information to carry out your job | 2.35 (1.21) | 2.10 (1.20) | 0.280 | |
| 2. Being unclear on just what the scope and responsibilities of your job are doing | 2.18 (1.24) | 2.15 (1.24) | 0.879 | |
| 6. Feeling that you are not fully qualified to handle your job | 2.00 (1.23) | 1.46 (0.94) | 0.007 * | 0.480 |
| Average total score of 15 items (Mean, SD = 37.35, 12.37) | 40.39 (12.08) | 33.45 (11.77) | 0.006 * | 0.576 |
| Average score of 15 items b | 2.73 (0.76) | 2.25 (0.78) | 0.001 * | 0.610 |
| Psychological Distress a | p | Effect Size | ||
|---|---|---|---|---|
| Yes | No | g | ||
| Questions | Mean (SD) | Mean (SD) | ||
| 3. I am afraid of falling ill with COVID-19 | 4.93 (1.30) | 4.21 (1.52) | 0.007 * | 0.509 |
| 8. My family is worried they might get COVID-19 through me | 4.87 (1.50) | 4.40 (1.71) | 0.113 | |
| 4. I feel I have little control over whether I get infected or not | 4.79 (1.35) | 4.02 (1.69) | 0.008 * | 0.507 |
| 1. I believe that my job is putting me at great risk | 4.54 (1.69) | 4.21 (1.60) | 0.287 | |
| 2. I feel extra stress at work | 4.45 (1.47) | 3.18 (1.49) | <0.001 * | 0.852 |
| 7. I am afraid I will pass COVID-19 on to others | 4.43 (1.65) | 3.76 (1.77) | 0.036 * | 0.388 |
| 9. I feel altruistic working with COVID-19 | 4.33 (1.46) | 3.73 (1.72) | 0.049 * | 0.377 |
| 5. I feel I may be unlikely to survive if I get COVID-19 | 3.47 (1.84) | 2.92 (1.78) | 0.101 | |
| 6. I have thought about resigning because of COVID-19 | 2.93 (1.90) | 1.75 (1.13) | <0.001 * | 0.726 |
| Average score of 9 items b | 4.32 (1.00) | 3.58 (1.06) | <0.001 * | 0.713 |
| Psychological Distress | p | Effect Size | ||
|---|---|---|---|---|
| Yes | No | g | ||
| Items | Mean (SD) | Mean (SD) | ||
| Section 1. Concern about workplace hazards (higher scores meaning less risky and more protection in the workplace) | ||||
| 1. How hazardous do you feel your workplace is in general? | 1.37 (0.64) | 1.76 (0.77) | 0.003 * | −0.556 |
| (Risky to No risk, score from 1 to 4) | ||||
| 2. How hazardous do you feel your workplace is since the COVID-19 pandemic began? | 1.22 (0.54) | 1.48 (0.74) | 0.038 * | −0.409 |
| (Risky to No risk, score from 1 to 4) | ||||
| 3. Has your behaviour related to infection control changed since COVID-19 pandemic? | (%) | (%) | ||
| Yes (following the infection control protocol) | 29.90 | 18.80 | 0.176 | |
| No (Always maintained a high level of infection control/not exposed or at risk) | 70.10 | 81.30 | ||
| 4. From your perspective, is the supply of PPE available to you? | 1.57 (0.70) | 1.65 (0.56) | 0.496 | |
| (insufficient/adequate/sufficient, score from 1 to 3) | ||||
| Section 2. Compliance with protective practices-COVID-19 (from ‘Never’ to ‘Always’, score 1–5) | ||||
| 1. I use eye and face protection (other than prescription glasses) | 3.41 (1.38) | 3.80 (1.57) | 0.164 | |
| 2. I use a surgical mask when dealing with patients when an N95 is not available | 4.31 (1.15) | 4.10 (1.49) | 0.406 | |
| 3. I wear an N95 | 3.22 (1.56) | 4.06 (1.49) | 0.004 * | −0.545 |
| 4. I reuse my disposable masks | 2.61 (1.66) | 2.23 (1.66) | 0.234 | |
| 5. I wear a gown or apron | 3.61 (1.52) | 4.27 (1.19) | 0.011 * | −0.471 |
| 6. I wear gloves | 3.97 (1.37) | 4.40 (1.20) | 0.086 | |
| 7. Cleaning supplies are available | 3.80 (1.29) | 4.38 (1.12) | 0.015 * | −0.464 |
| Average score of 7 items a | 3.55 (0.84) | 3.90 (0.75) | 0.020 * | −0.438 |
| Section 3. Compliance with protective practices-non-COVID-19 (from ‘Never’ to ‘Always’, score 1 to 5) | ||||
| 1. I use a surgical mask | 4.29 (1.26) | 4.85 (0.55) | 0.001 * | −0.539 |
| 2. I wear gloves | 3.53 (1.45) | 4.14 (1.50) | 0.028 * | −0.414 |
| 3. I wear a gown/apron | 3.66 (1.37) | 4.06 (1.51) | 0.143 | |
| 4. I send them for testing if they report one symptom | 3.83 (1.40) | 4.08 (1.30) | 0.318 | |
| 5. I send them for testing if they report more than one symptom | 4.29 (1.18) | 4.39 (1.20) | 0.660 | |
| Average score of 5 items a | 3.92 (0.88) | 4.31 (1.00) | 0.029 * | −0.412 |
| Section 4. Workplace-participative, committed and trusting relationship when taking care of COVID-19 patients (from ‘Never’ to ‘Always’, score 1–5) | ||||
| 1. I make suggestions for correcting health and safety problems | 3.35 (1.43) | 3.88 (1.30) | 0.045 * | −0.378 |
| 2. I get clear supervision regarding safe work practices | 3.32 (1.37) | 4.33 (1.00) | <0.001 * | −0.813 |
| 3. I am encouraged to report injuries and illness at work | 3.93 (1.25) | 4.63 (0.86) | <0.001 * | −0.633 |
| 4. I trust my manager to make my workplace safe | 3.70 (1.31) | 4.55 (0.94) | <0.001 * | −0.726 |
| 5. I trust my health and safety committee to make my workplace safe | 3.12 (1.43) | 4.00 (1.19) | <0.001 * | −0.653 |
| Average score of 5 items a | 3.50 (1.03) | 4.29 (0.86) | <0.001 * | −0.815 |
| Section 5. Perceptions of barriers to infection control practices (from ‘Never’ to ‘Always’, score 1–5) | ||||
| 1. Not enough time/too much work | 3.74 (1.21) | 2.90 (1.25) | <0.001 * | 0.686 |
| 2. Poor availability of proper equipment | 3.71 (1.26) | 3.33 (1.45) | 0.129 | |
| 3. Lack of proper space | 3.61 (1.26) | 2.78 (1.42) | 0.001 * | 0.623 |
| 4. Do not feel the risk that requires it | 3.14 (1.32) | 2.40 (1.28) | 0.003 * | 0.567 |
| 5. Peer pressure | 2.83 (1.51) | 1.64 (1.06) | <0.001 * | 0.888 |
| 6. Not trained well enough | 3.13 (1.49) | 2.42 (1.33) | 0.009 * | 0.502 |
| 7. Proper supervision not provided | 2.91 (1.34) | 2.25 (1.28) | 0.010 * | 0.497 |
| 8. Not supported by my manager | 2.67 (1.34) | 2.00 (1.23) | 0.007 * | 0.512 |
| Average score of 8 items a | 3.22 (0.84) | 2.46 (0.94) | <0.001 * | 0.858 |
| Psychological Distress (Total Score ≥ 3) | ||
|---|---|---|
| Variables | Full Model | Final Model |
| OR (95% CI) | Adjusted OR (95%CI) | |
| Training | ||
| COVID-19 infection control | 0.37 (0.18, 0.74) ** | |
| Emergency procedures | 0.44 (0.27, 0.72) ** | 0.41 (0.21, 0.81) * |
| Perceived risks of COVID-19 | 1.99 (1.36, 2.93) ** | 2.35 (1.33, 4.17) ** |
| Job-Related Tension Index | 2.24 (1.35, 3.72) ** | |
| Social support | ||
| Immediate supervisor/boss | 0.56 (0.37, 0.86) ** | |
| Concern about workplace hazards | ||
| Feel workplace is hazardous in general | 0.46 (0.27, 0.79) ** | |
| Feel workplace is hazardous since the pandemic | 0.53 (0.29, 0.95) * | |
| Compliance with protective practices (COVID-19) | 0.57 (0.35, 0.92) * | |
| Compliance with protective practices (non-COVID-19) | 0.63 (0.41, 0.96) * | |
| Workplace relationships | 0.40 (0.25, 0.64) ** | 0.52 (0.27, 0.97) * |
| Perceptions of barriers to infection control practices | 2.67 (1.66, 4.29) ** | 2.16 (1.17, 3.98) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.-L.; Wilson, K.S.; Bernstein, C.; Naicker, N.; Yassi, A.; Spiegel, J.M. Psychological Distress in South African Healthcare Workers Early in the COVID-19 Pandemic: An Analysis of Associations and Mitigating Factors. Int. J. Environ. Res. Public Health 2022, 19, 9722. https://doi.org/10.3390/ijerph19159722
Lee H-L, Wilson KS, Bernstein C, Naicker N, Yassi A, Spiegel JM. Psychological Distress in South African Healthcare Workers Early in the COVID-19 Pandemic: An Analysis of Associations and Mitigating Factors. International Journal of Environmental Research and Public Health. 2022; 19(15):9722. https://doi.org/10.3390/ijerph19159722
Chicago/Turabian StyleLee, Hsin-Ling, Kerry S. Wilson, Colleen Bernstein, Nisha Naicker, Annalee Yassi, and Jerry M. Spiegel. 2022. "Psychological Distress in South African Healthcare Workers Early in the COVID-19 Pandemic: An Analysis of Associations and Mitigating Factors" International Journal of Environmental Research and Public Health 19, no. 15: 9722. https://doi.org/10.3390/ijerph19159722
APA StyleLee, H.-L., Wilson, K. S., Bernstein, C., Naicker, N., Yassi, A., & Spiegel, J. M. (2022). Psychological Distress in South African Healthcare Workers Early in the COVID-19 Pandemic: An Analysis of Associations and Mitigating Factors. International Journal of Environmental Research and Public Health, 19(15), 9722. https://doi.org/10.3390/ijerph19159722






