Water, Sanitation, and Hygiene (WASH) Practices and Outreach Services in Settlements for Rohingya Population in Cox’s Bazar, Bangladesh, 2018–2021
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
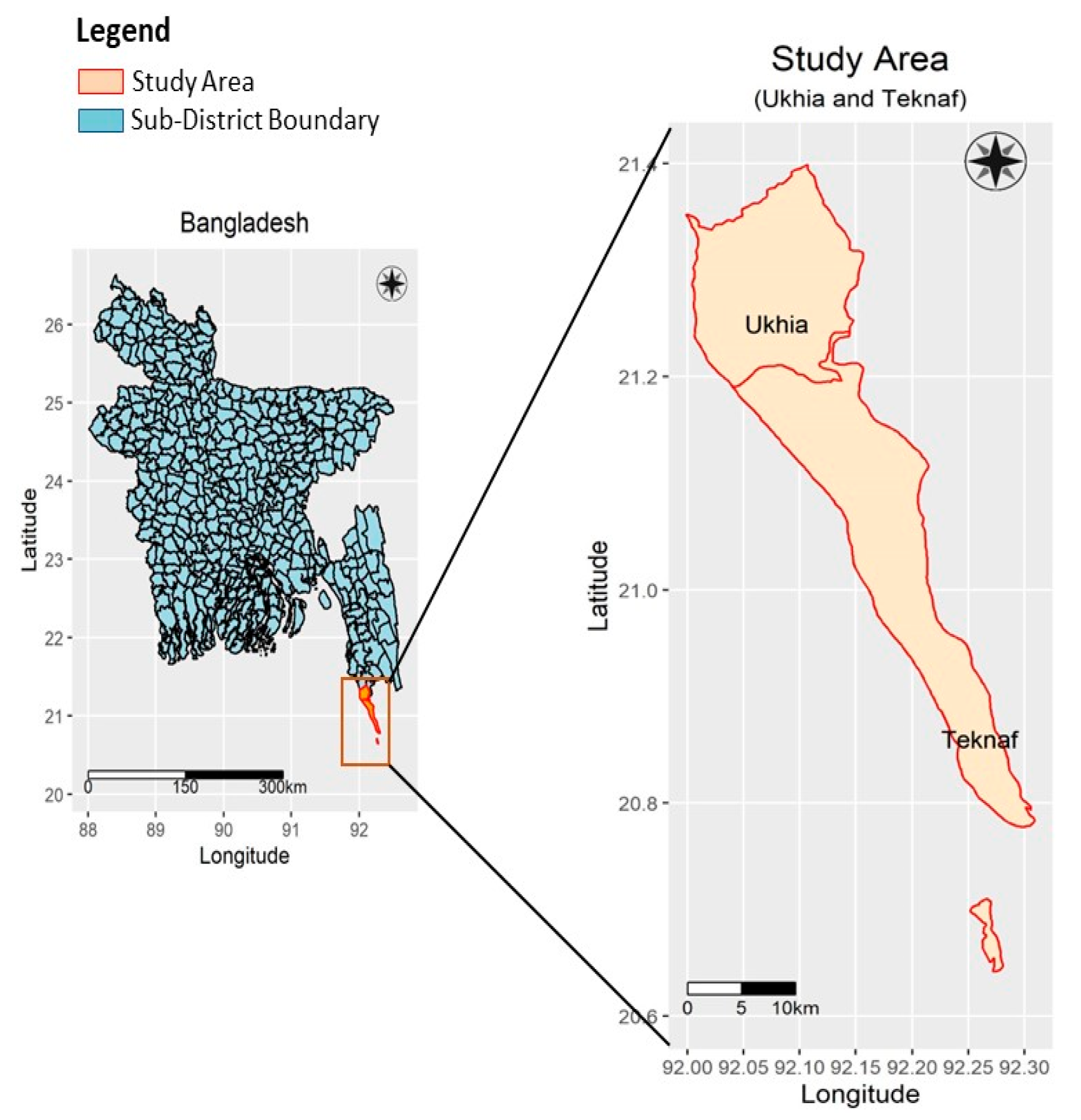
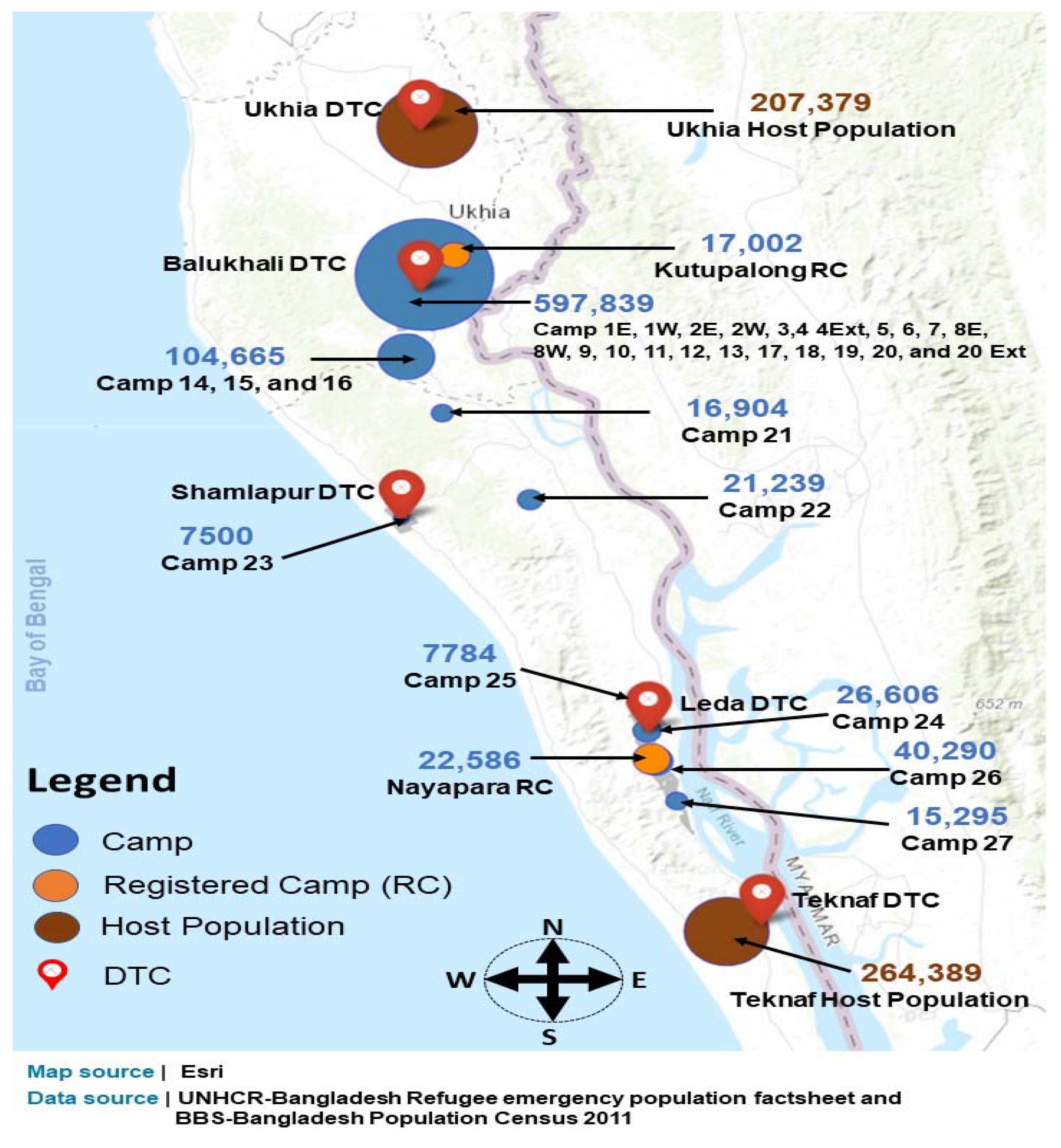
2.2. Study Site
2.3. Study Population
2.4. Operational Definitions
| Variables | Definitions |
| Diarrhea | According to World Health Organization, diarrhea is the passage of loose, watery stools, occurring three or more times in 24 h. |
| Water seal latrine | A toilet that has a squatting pan with a water seal with the pit lying immediately below. |
| Pit latrine | It has a squatting pan and simple pit in the ground lying directly below but without any water seal. |
| Tap water | A form of chlorinated public water supply to maximize drinking of safe water, while the water is acceptably free from pathogens that have potential to cause disease and often grow in water supply basins. |
| Shallow tube wells | Those having a depth that is drilled to ≤100 feet, generally easy to install, requiring little effort in maintenance, and giving easy access to drinking water, as they are installed in the neighborhood. |
| Deep tube wells | Those with depths of 500–700 feet, are expensive, difficult and time-consuming to install, and broadly located but give access to relatively safer drinking water. |
2.5. Data Collection
2.6. Statistical Analysis
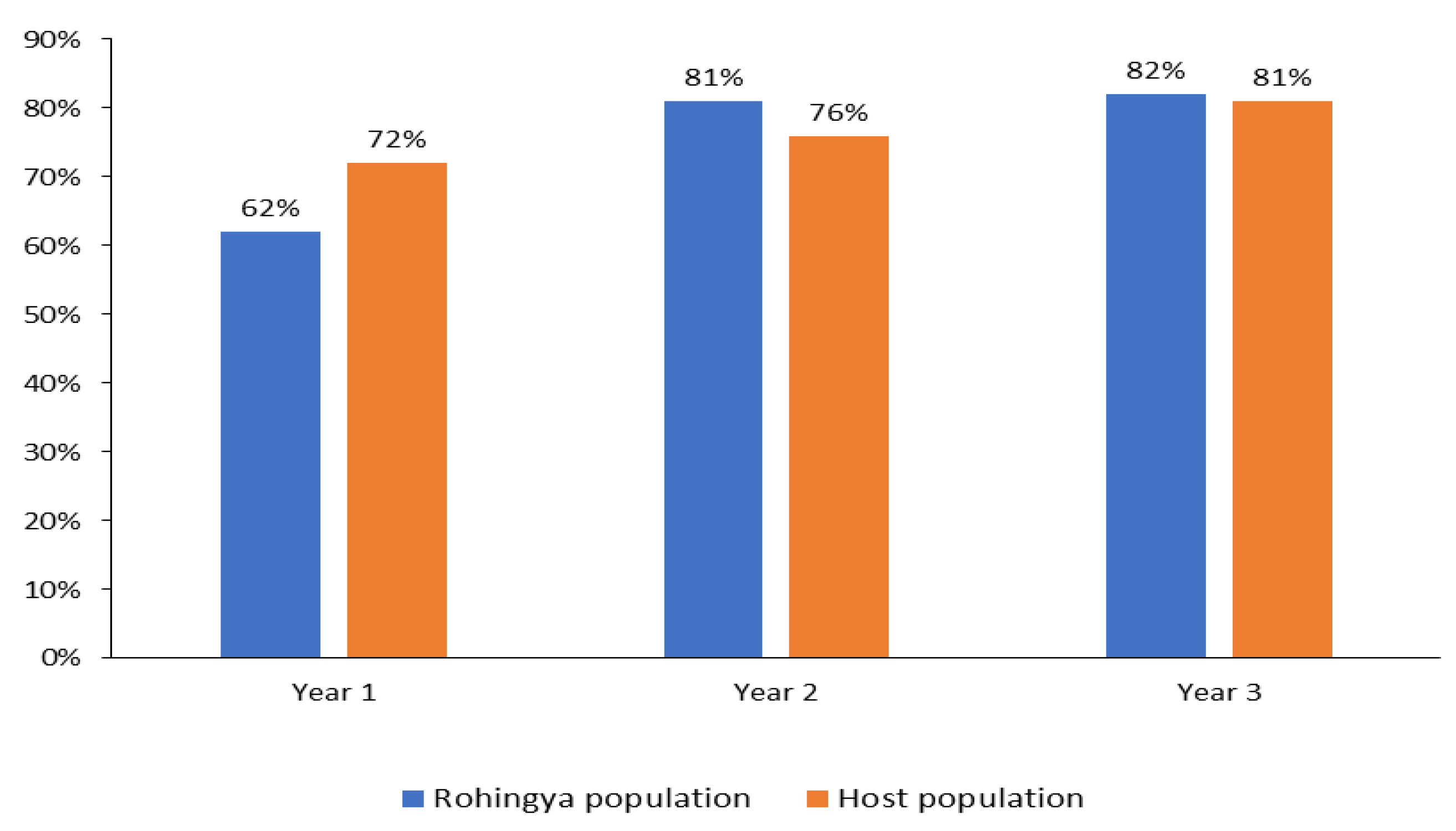
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| WASH | Water, sanitation and hygiene |
| DTCs | Diarrhea-treatment centers |
| ORS | Oral rehydration solutions |
| E. coli | Escherichia coli |
| icddr,b | International Centre for Diarrhoeal Disease Research, Bangladesh |
| UNICEF | United Nations Children’s Fund |
| NGO | Non-governmental organization |
| OCV | Oral cholera vaccine |
| EWARS | Early warning and alert response system |
| DDSS | Diarrheal Disease Surveillance System |
| WQS | Water-quality surveillance |
References
- Cash, R.A.; Halder, S.R.; Husain, M.; Islam, M.S.; Mallick, F.H.; May, M.A.; Rahman, M.; Rahman, M.A. Reducing the health effect of natural hazards in Bangladesh. Lancet 2013, 382, 2094–2103. [Google Scholar] [CrossRef]
- Ullah, A.A. Rohingya Refugees to Bangladesh: Historical Exclusions and Contemporary Marginalization. J. Immigr. Refug. Stud. 2011, 9, 139–161. [Google Scholar] [CrossRef]
- Schmitt, M.L.; Wood, O.R.; Clatworthy, D.; Rashid, S.F.; Sommer, M. Innovative strategies for providing menstruation-supportive water, sanitation and hygiene (WASH) facilities: Learning from refugee camps in Cox’s bazar, Bangladesh. Confl. Health 2021, 15, 10. [Google Scholar] [CrossRef] [PubMed]
- Faruque, A.S.G.; Khan, A.I.; Islam, S.M.R.; Nahar, B.; Hossain, M.N.; Widiati, Y.; Hasan, A.S.M.M.; Prajapati, M.; Kim, M.; Vandenent, M.; et al. Diarrhea treatment center (DTC) based diarrheal disease surveillance in settlements in the wake of the mass influx of forcibly displaced Myanmar national (FDMN) in Cox’s Bazar, Bangladesh, 2018. PLoS ONE 2021, 16, e0254473. [Google Scholar] [CrossRef]
- Bowden, M.; Crisp, J. Special Feature Rohingya Refugees in Bangladesh: The Humanitarian Response. Humanit Pract Netw ODI. 2018. Available online: https://odihpn.org/wp-content/uploads/2018/10/HE-73_web.pdf (accessed on 3 July 2022).
- Islam, M.M.; Nuzhath, T. Health risks of Rohingya refugee population in Bangladesh: A call for global attention. J. Glob. Health 2018, 8, 020309. [Google Scholar] [CrossRef]
- Pocock, N.S.; Mahmood, S.S.; Zimmerman, C.; Orcutt, M. Imminent health crises among the Rohingya people of Myanmar. BMJ 2017, 359, j5210. [Google Scholar] [CrossRef]
- Villasana, D. Picturing health: Rohingya refugees in Bangladesh. Lancet 2017, 390, 2233–2242. [Google Scholar] [CrossRef]
- UNHCR MUA. Fighting Water Scarcity in Cox’s Bazar Refugee Camps. 2019. Available online: https://www.unhcr.org/news/latest/2019/1/5c2fc16a4/fighting-water-scarcity-coxs-bazar-refugee-camps.html (accessed on 3 June 2022).
- Ayers, J.C.; George, G.; Fry, D.; Benneyworth, L.; Wilson, C.; Auerbach, L.; Roy, K.; Karim, R.; Akter, F.; Goodbred, S. Salinization and arsenic contamination of surface water in southwest Bangladesh. Geochem. Trans. 2017, 18, 4. [Google Scholar] [CrossRef]
- Shammi, M.; Rahman, M.; Bondad, S.E.; Doza, B. Impacts of Salinity Intrusion in Community Health: A Review of Experiences on Drinking Water Sodium from Coastal Areas of Bangladesh. Healthcare 2019, 7, 50. [Google Scholar] [CrossRef]
- Akhter, M.; Uddin, S.; Rafa, N.; Hridi, S.; Staddon, C.; Powell, W. Drinking Water Security Challenges in Rohingya Refugee Camps of Cox’s Bazar, Bangladesh. Sustainability 2020, 12, 7325. [Google Scholar] [CrossRef]
- Smith, A.H.; Lingas, E.O.; Rahman, M. Contamination of drinking-water by arsenic in Bangladesh: A public health emergency. Bull. World Health Organ. 2000, 78, 1093–1103. [Google Scholar] [PubMed]
- Mahmud, Z.H.; Islam, S.; Imran, K.M.; Hakim, S.A.I.; Worth, M.; Ahmed, A.; Hossan, S.; Haider, M.; Islam, M.R.; Hossain, F.; et al. Occurrence of Escherichia coli and faecal coliforms in drinking water at source and household point-of-use in Rohingya camps, Bangladesh. Gut Pathog. 2019, 11, 52. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Rohingya refugees in Bangladesh: Health sector bulletin no. 1. Health Sect. Bull. 2017, 1. Available online: https://cdn.who.int/media/docs/default-source/searo/bangladesh/bangladesh---rohingya-crisis---pdf-reports/health-sector-bulletin/health-sector-cxb-q1-2022.pdf?sfvrsn=f6f54efd_1 (accessed on 5 July 2022).
- Mahmud, Z.H.; Kabir, M.H.; Ali, S.; Moniruzzaman, M.; Imran, K.M.; Nafiz, T.N.; Islam, S.; Hussain, A.; Hakim, S.A.I.; Worth, M.; et al. Extended-Spectrum Beta-Lactamase-Producing Escherichia coli in Drinking Water Samples from a Forcibly Displaced, Densely Populated Community Setting in Bangladesh. Front. Public Health 2020, 8, 228. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, S. The Rohingya Crisis: A Health Situation Analysis of Refugee Camps in Bangladesh. 2019. Available online: https://www.orfonline.org/research/the-rohingya-crisis-a-health-situation-analysis-of-refugee-camps-in-bangladesh-53011/ (accessed on 6 July 2022).
- White, K. Rohingya in Bangladesh: An Unfolding Public Health Emergency. Lancet 2017, 390, 1947. [Google Scholar] [CrossRef][Green Version]
- UNICEF. UNICEF and WFP harness technology to strengthen food and hygiene distribution for Rohingyas. 2018. Available online: https://www.unicef.org/bangladesh/en/press-releases/unicef-and-wfp-harness-technology-strengthen-food-and-hygiene-distribution-rohingyas (accessed on 6 July 2022).
- Lam, E.; Al-Tamimi, W.; Russell, S.P.; Butt, M.O.-U.I.; Blanton, C.; Musani, A.S.; Date, K. Oral Cholera Vaccine Coverage during an Outbreak and Humanitarian Crisis, Iraq, 2015. Emerg. Infect. Dis. 2017, 23, 38–45. [Google Scholar] [CrossRef]
- Cambaza, E.; Mongo, E.; Anapakala, E.; Nhambire, R.; Singo, J.; Machava, E. Outbreak of Cholera Due to Cyclone Kenneth in Northern Mozambique, 2019. Int. J. Environ. Res. Public Health 2019, 16, 2925. [Google Scholar] [CrossRef]
- Jutla, A.; Khan, R.; Colwell, R. Natural Disasters and Cholera Outbreaks: Current Understanding and Future Outlook. Curr. Environ. Health Rep. 2017, 4, 99–107. [Google Scholar] [CrossRef]
- Jones, F.K.; Wamala, J.F.; Rumunu, J.; Mawien, P.N.; Kol, M.T.; Wohl, S.; Deng, L.; Pezzoli, L.; Omar, L.H.; Lessler, J.; et al. Successive epidemic waves of cholera in South Sudan between 2014 and 2017: A descriptive epidemiological study. Lancet Planet. Health 2020, 4, e577–e587. [Google Scholar] [CrossRef]
- Federspiel, F.; Ali, M. The cholera outbreak in Yemen: Lessons learned and way forward. BMC Public Health 2018, 18, 1338. [Google Scholar] [CrossRef]
- Qadri, F.; Azad, A.K.; Flora, M.S.; Khan, A.I.; Islam, T.; Nair, G.B.; Singh, P.K.; Clemens, J.D. Emergency deployment of oral cholera vaccine for the Rohingya in Bangladesh. Lancet 2018, 391, 1877–1879. [Google Scholar] [CrossRef]
- Khan, A.I.; Islam, M.T.; Siddique, S.A.; Ahmed, S.; Sheikh, N.; Siddik, A.U.; Islam, M.S.; Qadri, F. Post-vaccination campaign coverage evaluation of oral cholera vaccine, oral polio vaccine and measles-rubella vaccine among Forcibly Displaced Myanmar Nationals in Bangladesh. Hum. Vaccines Immunother. 2019, 15, 2882–2886. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, F.; Bhuiyan, T.R.; Akter, A.; Bhuiyan, M.S.; Khan, A.I.; Hossain, M.; Tauheed, I.; Ahmed, T.; Islam, S.; Rafique, T.A. Immunogenicity of a killed bivalent whole cell oral cholera vaccine in forcibly displaced Myanmar nationals in Cox’s Bazar, Bangladesh. PLoS Negl. Trop. Dis. 2020, 14, e0007989. [Google Scholar] [CrossRef]
- Ramesh, A.; Blanchet, K.; Ensink, J.H.J.; Roberts, B. Evidence on the Effectiveness of Water, Sanitation, and Hygiene (WASH) Interventions on Health Outcomes in Humanitarian Crises: A Systematic Review. PLoS ONE 2015, 10, e0124688. [Google Scholar] [CrossRef]
- Yates, T.; Zannat, H.; Khandaker, N.; Porteaud, D.; Bouvet, F.; Lantagne, D. Evidence summary of water, sanitation, and hygiene (WASH) coordination in humanitarian response. Disasters 2020, 45, 913–938. [Google Scholar] [CrossRef]
- Faruque, A.S.G.; Khan, A.I.; Nahar, B.; Islam, S.M.R.; Hossain, M.N.; Abdullah, S.A.; Khan, S.H.; Hossain, M.S.; Khan, F.H.; Prajapati, M. Cholera outbreak in Forcibly Displaced Myanmar National (FDMN) from a small population segment in Cox’s Bazar, Bangladesh, 2019. PLoS Negl. Trop. Dis. 2021, 15, e0009618. [Google Scholar] [CrossRef] [PubMed]
- Government of Bangladesh (GoB); United Nations High Commissioner for Refugees (UNHCR). March 2021: Joint Government of Bangladesh-UNHCR Population Factsheet. Available online: https://data2.unhcr.org/en/documents/details/86233 (accessed on 20 July 2022).
- Hanifi, S.; Sultana, A.; Mia, M.N.; Hoque, S.; Mahmood, S.S.; Iqbal, M.; Bhuiya, A. Chakaria Health and Demographic Surveillance System Report–2014: Focusing on the Sustainable Development Goals; icddr,b: Dhaka, Bangladesh, 2016. [Google Scholar]
- WHO. Diarrhoeal Disease. 2017. Available online: https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease (accessed on 20 July 2022).
- Parvin, I.; Shahunja, K.M.; Khan, S.H.; Alam, T.; Shahrin, L.; Ackhter, M.M.; Sarmin, M.; Dash, S.; Rahman, M.W.; Bin Shahid, A.S.M.S.; et al. Changing Susceptibility Pattern of Vibrio cholerae O1 Isolates to Commonly Used Antibiotics in the Largest Diarrheal Disease Hospital in Bangladesh during 2000–2018. Am. J. Trop. Med. Hyg. 2020, 103, 652–658. [Google Scholar] [CrossRef]
- Parvin, I.; Bin Shahid, A.S.M.S.; Das, S.; Shahrin, L.; Ackhter, M.M.; Alam, T.; Khan, S.H.; Chisti, M.J.; Clemens, J.D.; Ahmed, T.; et al. Vibrio cholerae O139 persists in Dhaka, Bangladesh since 1993. PLOS Negl. Trop. Dis. 2021, 15, e0009721. [Google Scholar] [CrossRef]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression; John Wiley & Sons: Hoboken, NJ, USA, 2013. [Google Scholar]
- Kahn, R.; Mahmud, A.S.; Schroeder, A.; Ramirez, L.H.A.; Crowley, J.; Chan, J.; Buckee, C.O. Rapid Forecasting of Cholera Risk in Mozambique: Translational Challenges and Opportunities. Prehospital Disaster Med. 2019, 34, 557–562. [Google Scholar] [CrossRef]
- Terkawi, A.S.; Bakri, B.; Alsadek, A.S.; Al-Hasan, A.H.; Alrahhal, M.S.; Alsaleh, F.M.; Alsatouf, F.A.; Arab, M.I.; Jnaid, H.; Hadid, A.A.; et al. Child and adolescent health in northwestern Syria: Findings from Healthy-Syria 2017 study. Avicenna J. Med. 2019, 9, 61–74. [Google Scholar] [CrossRef]
- Ataullahjan, A.; Gaffey, M.F.; Tounkara, M.; Diarra, S.; Doumbia, S.; Bhutta, Z.A.; Bassani, D.G. C’est vraiment compliqué: A case study on the delivery of maternal and child health and nutrition interventions in the conflict-affected regions of Mali. Confl. Health 2020, 14, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, Z.; Ataullahjan, A.; Gaffey, M.F.; Osman, M.; Umutoni, C.; Bhutta, Z.A.; Dalmar, A.A. Understanding the factors affecting the humanitarian health and nutrition response for women and children in Somalia since 2000: A case study. Confl. Health 2020, 14, 35. [Google Scholar] [CrossRef] [PubMed]
- Azman, A.S.; Rumunu, J.; Abubakar, A.; West, H.; Ciglenecki, I.; Helderman, T.; Wamala, J.F.; Vázquez, O.D.L.R.; Perea, W.; Sack, D.A.; et al. Population-Level Effect of Cholera Vaccine on Displaced Populations, South Sudan, 2014. Emerg. Infect. Dis. 2016, 22, 1067–1070. [Google Scholar] [CrossRef] [PubMed]
- Ngwa, M.C.; Alemu, W.; Okudo, I.; Owili, C.; Ugochukwu, U.; Clement, P.; Devaux, I.; Pezzoli, L.; Oche, J.A.; Ihekweazu, C.; et al. The reactive vaccination campaign against cholera emergency in camps for internally displaced persons, Borno, Nigeria, 2017: A two-stage cluster survey. BMJ Glob. Health 2020, 5, e002431. [Google Scholar] [CrossRef]
- Ozaras, R.; Leblebicioglu, H.; Sunbul, M.; Tabak, F.; Balkan, I.I.; Yemisen, M.; Sencan, I.; Ozturk, R. The Syrian conflict and infectious diseases. Expert Rev. Anti-Infect. Ther. 2016, 14, 547–555. [Google Scholar] [CrossRef]
- Desai, A.N.; Ramatowski, J.W.; Marano, N.; Madoff, L.C.; Lassmann, B. Infectious disease outbreaks among forcibly displaced persons: An analysis of ProMED reports 1996–2016. Confl. Health 2020, 14, 49. [Google Scholar] [CrossRef]
- Lantagne, D.; Lehmann, L.; Yates, T.; Gallandat, K.; Sikder, M.; Domini, M.; String, G. Lessons learned from conducting six multi-country mixed-methods effectiveness research studies on water, sanitation, and hygiene (WASH) interventions in humanitarian response. BMC Public Health 2021, 21, 560. [Google Scholar] [CrossRef]
- Milton, A.H.; Rahman, M.; Hussain, S.; Jindal, C.; Choudhury, S.; Akter, S.; Ferdousi, S.; Akter Mouly, T.; Hall, J.; Efird, J.T. Trapped in Statelessness: Rohingya Refugees in Bangladesh. Int. J. Environ. Res. Public Health 2017, 14, 942. [Google Scholar] [CrossRef]
- Cousins, S. “People will die” as monsoon approaches Rohingya refugee camps in Bangladesh. BMJ 2018, 361, k2040. [Google Scholar] [CrossRef]
- Grandi, F. Stateless Minorities and Their Search for Citizenship—UNHCR. 2017. Available online: https://www.unhcr.org/protection/statelessness/59f747404/home-stateless-minorities-search-citizenship.html (accessed on 25 July 2022).
- Mahmood, S.S.; Wroe, E.; Fuller, A.; Leaning, J. The Rohingya people of Myanmar: Health, human rights, and identity. Lancet 2017, 389, 1841–1850. [Google Scholar] [CrossRef]
- Hassan, M.M.; Smith, A.C.; Walker, K.; Rahman, M.K.; Southworth, J. Rohingya Refugee Crisis and Forest Cover Change in Teknaf, Bangladesh. Remote Sens. 2018, 10, 689. [Google Scholar] [CrossRef]
- Mukul, S.A.; Huq, S.; Herbohn, J.; Nishat, A.; Rahman, A.A.; Amin, R.; Ahmed, F.U. Rohingya refugees and the environment. Science 2019, 364, 138. [Google Scholar] [CrossRef] [PubMed]
- Karo, B.; Haskew, C.; Khan, A.S.; Polonsky, J.A.; Mazhar, M.K.A.; Buddha, N. World Health Organization Early Warning, Alert and Response System in the Rohingya Crisis, Bangladesh, 2017–2018. Emerg. Infect. Dis. 2018, 24, 2074–2076. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Report of Water Quality Surveillance in FDMN 2021—Community Point Source Round 2, 2021 (Cumulative Round 16) (9th January to 9th February 2021): Reliefweb. Available online: https://reliefweb.int/report/bangladesh/report-water-quality-surveillance-fdmn-2021-community-point-source-round-2-2021 (accessed on 25 July 2022).
- Karim, M. Purified Surface Water Meeting Demands of Rohingyas in Camps. The Daily Observer, 25 September 2021. [Google Scholar]
- Oregon Health Authority. Optimization, Training and Other Resources. Available online: https://www.oregon.gov/oha/PH/HEALTHYENVIRONMENTS/DRINKINGWATER/OPERATIONS/TREATMENT/Pages/index.aspx#treat (accessed on 25 July 2022).
- Kennedy, J.; McCoy, D. WHO and the health crisis among the Rohingya people of Myanmar. Lancet 2017, 389, 802–803. [Google Scholar] [CrossRef][Green Version]
- Inter Sectoral Coordination Group. 2020 Joint Response Plan for Rohingya humanitarian crisis: January–December 2020. Available online: www.humanitarianresponse.info/en/operations/bangladesh (accessed on 27 July 2022).
- World Vision Bangladesh. Three Years On: Rohingya Refugee Response Report 2020—Updated 22 August 2020. Available online: https://www.wvi.org/sites/default/files/2020-09/Rohingya_Refugee_Response_Annual_Report_2020.pdf (accessed on 27 July 2022).
- UNICEF. Bangladesh: Humanitarian Situation Report No. 56: 1 January to 31 March 2021. Available online: https://reliefweb.int/report/bangladesh/bangladesh-humanitarian-situation-report-no-56-1-january-31-march-2021 (accessed on 27 July 2022).
- WASH Sector, Cox’sbazar. WASH Sector Strategy for Rohingya Influx; March to December 2018, Cox’s Bazar: WASH Sector Cox’s Bazar 2018. Available online: https://reliefweb.int/sites/reliefweb.int/files/resources/wash_sector_cbx_mar_-_dec_2018_strategy.pdf (accessed on 31 July 2022).
| Name and Location of DTC | Health Facility Code | Starting Date | Ending Date | Capacity |
|---|---|---|---|---|
| Leda DTC | HF: 197 | 10 April 2018 | 31 March 2019 | 14 beds |
| Leda DTC (2nd Time) | HF: 197 | 8 October 2019 | 31 January 2020 | 14 beds |
| Leda DTC (3rd Time) | HF: 197 | 1 May 2020 | Continuing till now | 14 beds |
| Teknaf DTC | HF: 567 | 7 August 2018 | 30 April 2020 | 30 beds |
| Shamlyapur DTC | HF: 585 | 17 May 2018 | 31 March 2019 | 20 beds |
| Balukhali DTC | HF: 182 | 2 May 2018 | 31 December 2018 | 6 beds |
| Ukhia DTC | HF: 312 | 1 June 2018 | 31 December 2018 | 30 beds |
| Year 1 | Year 2 | Year 3 | ||||
|---|---|---|---|---|---|---|
| Indicator | n = 2355 (%) | n = 1636 (%) | n = 559 (%) | |||
| Water source | Rohingya population n = 860 (%) | Host population n = 1495 (%) | Rohingya population n = 463 (%) | Host population n = 1173 (%) | Rohingya population n = 268 (%) | Host population n = 291 (%) |
| Public tap | 331 (38.5) | 46 (3.1) | 392 (84.7) | 29 (2.5) | 244 (91.0) | 12 (4.1) |
| Deep tube well | 269 (31.3) | 638 (42.7) | 37 (8.0) | 445 (37.9) | 22 (8.2) | 187 (64.3) |
| Shallow tube well | 222 (25.8) | 699 (46.8) | 17 (3.7) | 580 (49.4) | 1 (0.4) | 49 (16.8) |
| Other | 38 (4.4) | 112 (7.5) | 17 (3.7) | 119 (10.1) | 1 (0.4) | 43 (14.8) |
| Year 1 | Year 2 | Year 3 | ||||
|---|---|---|---|---|---|---|
| Indicator | n = 2355 (%) | n = 1636 (%) | n = 559 (%) | |||
| Type of toilet | Rohingya population n = 860 (%) | Host population n = 1495 (%) | Rohingya population n = 463 (%) | Host population n = 1173 (%) | Rohingya population n = 268 (%) | Host population n = 291 (%) |
| Pit latrine, slab with water seal | 114 (13.3) | 376 (25.2) | 99 (21.4) | 315 (26.9) | 85 (31.7) | 128 (44.0) |
| Pit latrine, slab without water seal | 712 (82.8) | 814 (54.4) | 362 (78.2) | 664 (56.6) | 183 (68.3) | 160 (55.0) |
| Characteristics | AOR | 95% CI | p |
|---|---|---|---|
| Age | |||
| 5–14 years | 2.37 | 1.96–2.85 | <0.001 |
| 15+ years | 2.39 | 1.64–3.50 | <0.001 |
| Drinking non-tube well water | 0.42 | 0.36–0.50 | <0.001 |
| Use of no soap after using the toilet | 2.19 | 1.47–3.28 | <0.001 |
| Use of non-sanitary toilet facility | 0.49 | 0.41–0.58 | <0.001 |
| Father’s lack of schooling | 0.58 | 0.48–0.70 | <0.001 |
| Mother’s lack of schooling | 0.13 | 0.11–0.16 | <0.001 |
| Some dehydration | 0.44 | 0.31–0.62 | <0.001 |
| Severe dehydration | 0.52 | 0.36–0.74 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Faruque, A.; Alam, B.; Nahar, B.; Parvin, I.; Barman, A.K.; Khan, S.H.; Hossain, M.N.; Widiati, Y.; Hasan, A.M.; Kim, M.; et al. Water, Sanitation, and Hygiene (WASH) Practices and Outreach Services in Settlements for Rohingya Population in Cox’s Bazar, Bangladesh, 2018–2021. Int. J. Environ. Res. Public Health 2022, 19, 9635. https://doi.org/10.3390/ijerph19159635
Faruque A, Alam B, Nahar B, Parvin I, Barman AK, Khan SH, Hossain MN, Widiati Y, Hasan AM, Kim M, et al. Water, Sanitation, and Hygiene (WASH) Practices and Outreach Services in Settlements for Rohingya Population in Cox’s Bazar, Bangladesh, 2018–2021. International Journal of Environmental Research and Public Health. 2022; 19(15):9635. https://doi.org/10.3390/ijerph19159635
Chicago/Turabian StyleFaruque, ASG, Baharul Alam, Baitun Nahar, Irin Parvin, Ashok Kumar Barman, Soroar Hossain Khan, M Nasif Hossain, Yulia Widiati, ASM Mainul Hasan, Minjoon Kim, and et al. 2022. "Water, Sanitation, and Hygiene (WASH) Practices and Outreach Services in Settlements for Rohingya Population in Cox’s Bazar, Bangladesh, 2018–2021" International Journal of Environmental Research and Public Health 19, no. 15: 9635. https://doi.org/10.3390/ijerph19159635
APA StyleFaruque, A., Alam, B., Nahar, B., Parvin, I., Barman, A. K., Khan, S. H., Hossain, M. N., Widiati, Y., Hasan, A. M., Kim, M., Worth, M., Vandenent, M., & Ahmed, T. (2022). Water, Sanitation, and Hygiene (WASH) Practices and Outreach Services in Settlements for Rohingya Population in Cox’s Bazar, Bangladesh, 2018–2021. International Journal of Environmental Research and Public Health, 19(15), 9635. https://doi.org/10.3390/ijerph19159635







